Abstract
BACKGROUND
Outdoor air pollution has been considered as one of the most serious health concerns over the last decade. This study aimed to investigate the association between ambient air pollution and cardiovascular hospital admissions.
METHODS
This investigation was carried out from January 1, 2010 to December 31, 2015, in the urban population of Arak, Iran. Daily records of concentrations of air pollutants including particulate matter less than 10 µm (PM10), nitrogen dioxide (NO2), particulate matter less than 2.5 µm (PM2.5), ozone (O3), carbon monoxide (CO), and sulfur dioxide (SO2) as well as the daily number of hospital admissions due to cardiovascular disease were inquired from the Arak Department of Environment and two major hospitals, respectively. Time-series regression analysis was used to evaluate the effect of the pollutants on cardiovascular hospital admissions with different lag structures, controlling for weather variables, seasonality and long-term time trends, and day of the week.
RESULTS
Each 10 µg/m3 increase in PM10 and NO2 and 1 mg/m3 increase in CO concentrations at lag 0 (day) were significantly associated with an increase of 0.7% (P = 0.004), 3.3% (P = 0.006), and 9.4% (P < 0.001), respectively in overall cardiovascular hospital admissions. The elderly were more susceptible than those under 60 years to exposure to the pollutants (especially NO2) with regard to cardiovascular hospital admission.
CONCLUSION
The results of this study showed that hospital admission for cardiovascular disease is partly related to the levels of ambient air pollutions in Arak. Susceptibility to air pollutants varies by age groups and sex.
Keywords: Cardiovascular Diseases, Air Pollution, Hospital Admissions, Environmental Exposures, Iran
Introduction
Industrialization and urbanization over the last decades, along with rapid global economic growth has resulted in increase in ambient air pollution which is a serious threat to human health.1-3 Ambient air pollutants include complex mixtures of particles and gases such as carbon monoxide (CO), nitrogen dioxide (NO2), ozone (O3), sulfur dioxide (SO2), and particulate matter (PM).4,5 The World Health Organization (WHO) estimated that in 2012 ambient air pollution caused 3.7 million rural-and urban-premature deaths worldwide.6
Epidemiologic studies have indicated associations between ambient air pollution and adverse health effects such as respiratory hospital admission,7-10 respiratory mortality,11,12 and trauma.13 There is also growing epidemiological and clinical evidence showing that air pollution is associated with increased cardiovascular mortality and hospital admissions, and sudden cardiac arrest.14-19
Cardiovascular diseases (CVD) as a class of disorders involving the heart and blood vessels, are the leading cause of premature mortality in the world.20 Based on the WHO report, 17.5 million people died from CVD in 2012 which accounted for 31% of all global deaths. On the other hand, over 75% of CVD deaths occurred in low-income and middle-income countries.20
The underlying biological mechanisms linking air pollution and cardiovascular events have still remained unclear. Some researchers think that inhaled ultrafine particles diffuse in the blood circulation and can also modify the heart’s autonomic nervous control especially in people with existing cardiovascular disease.21,22
Various studies have showed that traffic related air pollution and residence within proximity of highways are related to myocardial infarction (MI).23,24 The results of a study conducted by Samoli et al. in London, UK demonstrated that traffic-related air pollution was associated with increased number of adult cardiovascular hospital admissions.25 Also, a Greek cohort conducted by Katsoulis et al. showed positive associations between traffic-related air pollution (PM10 and NO2 exposures) and ischemic heart disease and CVD morbidity, particularly among younger people (< 50 years) and women.26 Other studies conducted in the US and Italy also showed significant associations between air pollutants and cardiovascular admissions.27,28
Most studies on air pollution and CVD have been performed in developed countries, and there are few studies from developing countries and particularly the Middle East region, where air pollution is increasingly becoming a main public health and environmental problem.2,29 Researchers think that exhaust emissions from road vehicles and incomplete combustion of fossil fuels are the major sources of outdoor air pollution emissions in the Middle East region.2,30
Arak, is the capital city of the Markazi province located in central Iran, and is one of the industrial cities of the country31 with a population of over 600,000 people. The geographic coordinates of this city are 34.09 N and 49.69 E and it stands 1748 meters above sea level 31. The weather of the city is relatively warm and dry in summer, and cold and humid in winter. Due to intense industrial activities, urbanization and increased number of motor vehicles in the last decades, air pollution has had an ascending trend in this city. The objective of this study was to investigate the impact of short-term exposure to ambient air pollutants (SO2, PM2.5, CO, NO2, O3, and PM10) on cardiovascular hospital admissions in the urban population of Arak in a 6-year period.
Materials and Methods
This population-based ecological study was conducted from Jan 1, 2010 to Dec 31, 2015 in Arak. Daily data on cardiovascular hospital admissions were inquired from two major hospitals (Amir-al-Momenin and Amir Kabir) located in the urban area of Arak. These two governmental medical centers are the only referral centers and the main university affiliated hospitals in Arak, and admit people from various parts of this city. Another medical center is the Qods private hospital which has only 150 beds and admits much less patients. In this study, the daily number of cardiovascular hospital admissions was extracted from hospital admission records according to the tenth revision of the International Classification of Diseases (ICD-10), code I00-I99.
The daily ambient air pollution data were obtained from the Arak Department of Environment for the same time frame. The daily concentrations of 6 pollutants including CO, particulate matter less than 2.5 µm (PM2.5), particulate matter less than 10 µm (PM10), O3, NO2, and SO2 are measured daily in the four stationary centers located in different parts of the city. The daily concentrations of the pollutants used in this study were the average recorded results of these stations. The meteorological data including daily temperature, and relative humidity were inquired from the Arak Meteorological Organization for the same period.
This study (project number 95-249) was reviewed and approved by the Institutional Review Board of the Faculty of Health, Kerman University of Medical Sciences, Kerman, Iran, and was also approved by the Standing Committee on Ethics in Research of Arak University of Medical Sciences.
The short-term association between the number of cardiovascular admissions and air pollutant exposures (NO2, PM2.5, SO2, O3, PM10, and CO) was analyzed using a time-series regression model.32 As the daily number of CVD was approximately Poisson distributed, we used generalized linear models (GLM) within the family of Poisson distribution and distributed lag models (DLM) to estimate the association between CVD hospital admissions and air pollutant exposures. We adjusted for seasonality and long-term trend, temperature, relative humidity and day of the week (DOW).
We controlled for seasonality and long-term trend in the data with a flexible spline function of time with 7 degrees of freedom (df) per year.32 We also controlled for the effects of temperature and relative humidity as potential confounders that change from day to day with a natural cubic spline function with 4 df for each.32-34
Furthermore, in order to adjust for the day effect on hospital admissions, a DOW parameter was introduced in the model. The DLM was used with a range from zero to seven days, and presented the rate ratio (RR) of CVD admissions for increase in each pollutant.6 Finally, to reduce potential co-linearity between the air pollutants, the models were provided for each pollutant separately. Additionally, the association between ambient air pollution and cardiovascular hospital admissions was estimated according to sex and age separately. The final model was displayed as below:
Yt refers to the observed count for cardiovascular hospital admissions on day t, t is the day of the observation, s is a spline function, AP denotes to the daily level of the air pollutants (SO2, CO, O3, NO2, PM10 or PM2.5), indicates the lag days, time indicates the long-term trends and seasonality using the calendar time days, T and H are the average daily temperature (°C) and relative humidity (%), respectively and DOW is a categorical variable of the day of the week.
All statistical analyses were conducted by R software (version 3.3.1, R Foundation for Statistical Computing, Vienna, Austria) and statistical significance was considered when the P-value < 0.05. The effect was presented as RR and its 95% confidence interval (CI) for the daily cardiovascular hospital admissions, for each 1 mg/m3 increase in CO and each 10 μg/m3 increase in other pollutants, per day.
Results
The descriptive statistics of the pollutants concentrations, meteorological parameters, and mean of cardiovascular hospital admissions are shown in table 1. During the 6 years of study, there were a total of 32,089 cardiovascular hospital admissions. On average, there were 14.6 cardiovascular hospital admissions per day. More than half (53.1%) of the cardiovascular hospital admissions were men, and the sex ratio was 1.13:1 (17034:15055). The number of cardiovascular admissions was lower in the adult age group (19 to 60 years) and was 11,861 (only 37%).
Table 1.
Descriptive Statistics of air pollution levels, meteorological variables, and hospital admissions in Arak, Iran, 2010–2015
| Variables | Mean ± SD | Minimum | 25th percentile | Median | 75th percentile | Maximum |
|---|---|---|---|---|---|---|
| O3 (μg/m3) | 59.58 ± 26.70 | 1.50 | 41.47 | 55.97 | 72.82 | 186.03 |
| CO (mg/m3) | 2.89 ± 0.76 | 0.25 | 2.39 | 2.88 | 3.37 | 5.97 |
| SO2 (μg/m3) | 54.83 ± 33.30 | 1.59 | 37.49 | 47.87 | 61.91 | 566.85 |
| PM2.5 (μg/m3) | 24.30 ± 20.90 | 0.70 | 8.30 | 17.50 | 36.70 | 171.20 |
| PM10 (μg/m3) | 86.60 ± 44.30 | 2.30 | 62.10 | 82.04 | 99.30 | 536.30 |
| NO2 (μg/m3) | 53.45 ± 21.80 | 2.24 | 37.44 | 45.54 | 68.33 | 188.22 |
| Temperature (°C) | 14.80 ± 9.80 | -15.10 | 6.70 | 15.00 | 23.90 | 33.00 |
| Humidity (%) | 44.90 ± 21.10 | 12.00 | 26.00 | 42.00 | 61.00 | 99.00 |
| Cardiac admissions per day | ||||||
| All | 14.65 ± 7.30 | 0 | 9.00 | 14.00 | 20.00 | 43.00 |
| Men | 7.80 ± 4.40 | 0 | 5.00 | 7.00 | 11.00 | 26.00 |
| Women | 6.90 ± 4.00 | 0 | 4.00 | 6.00 | 9.00 | 24.00 |
| 0-18 years old | 0.28 ± 0.60 | 0 | 0.00 | 0.00 | 0.00 | 4.00 |
| 19-60 | 5.40 ± 3.50 | 0 | 3.00 | 5.00 | 8.00 | 18.00 |
| > 60 | 8.95 ± 4.70 | 0 | 6.00 | 9.00 | 12.00 | 31.00 |
SD: Standard deviation; CO: Carbon monoxide; NO2: Nitrogen dioxide; O3: Ozone; SO2: Sulfur dioxide; PM2.5: Particulate matter less than 2.5 μm; PM10: Particulate matter less than 10 μm
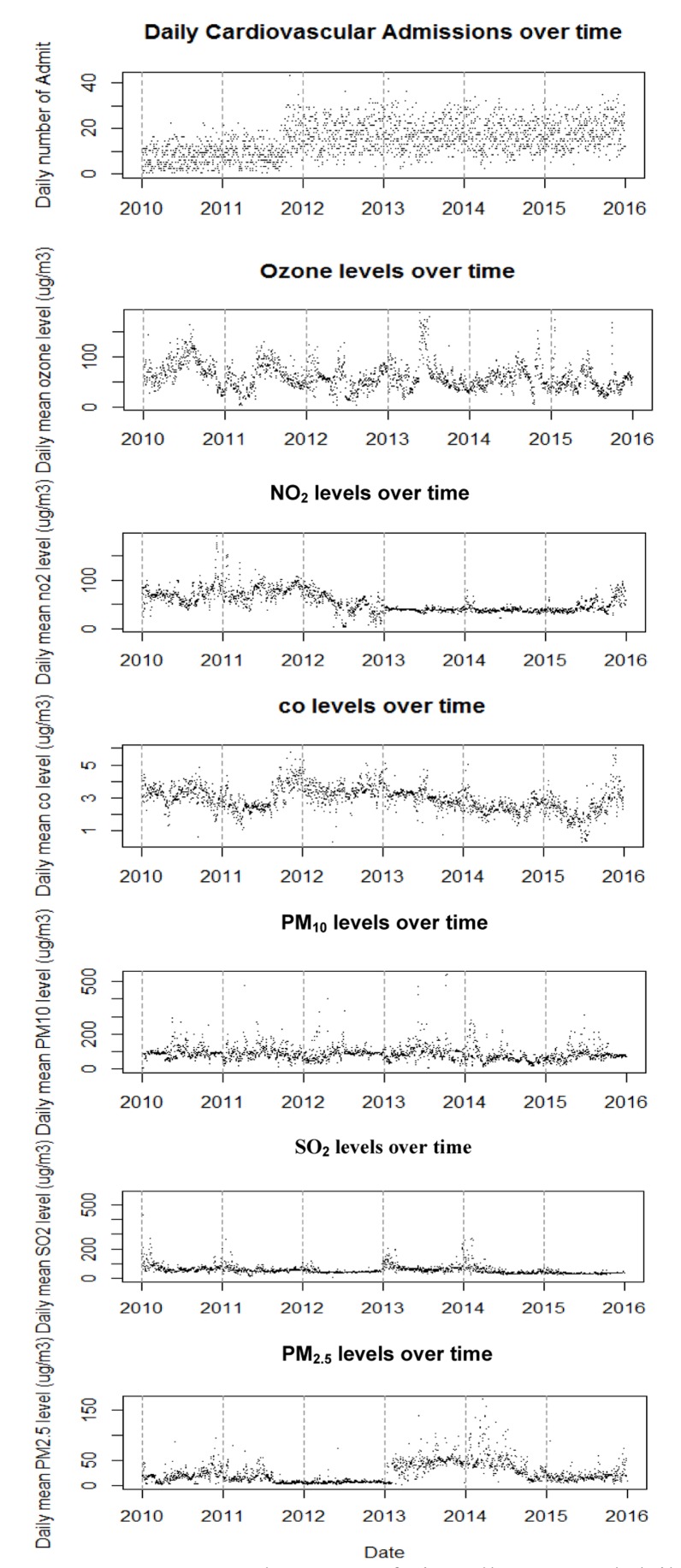
During the study period, the daily mean concentrations of PM10 and PM2.5 were 86.63 and 24.30 µg/m3, respectively which were higher than the correspondent WHO guidelines (25 and 50 μg/m3, Table 1).35 The temporal pattern of air pollutants and daily cardiovascular hospital admissions in the study period are shown in figure 1.
Figure 1.
Temporal pattern of air pollutants and daily hospital admissions due to cardiovascular diseases during the study period
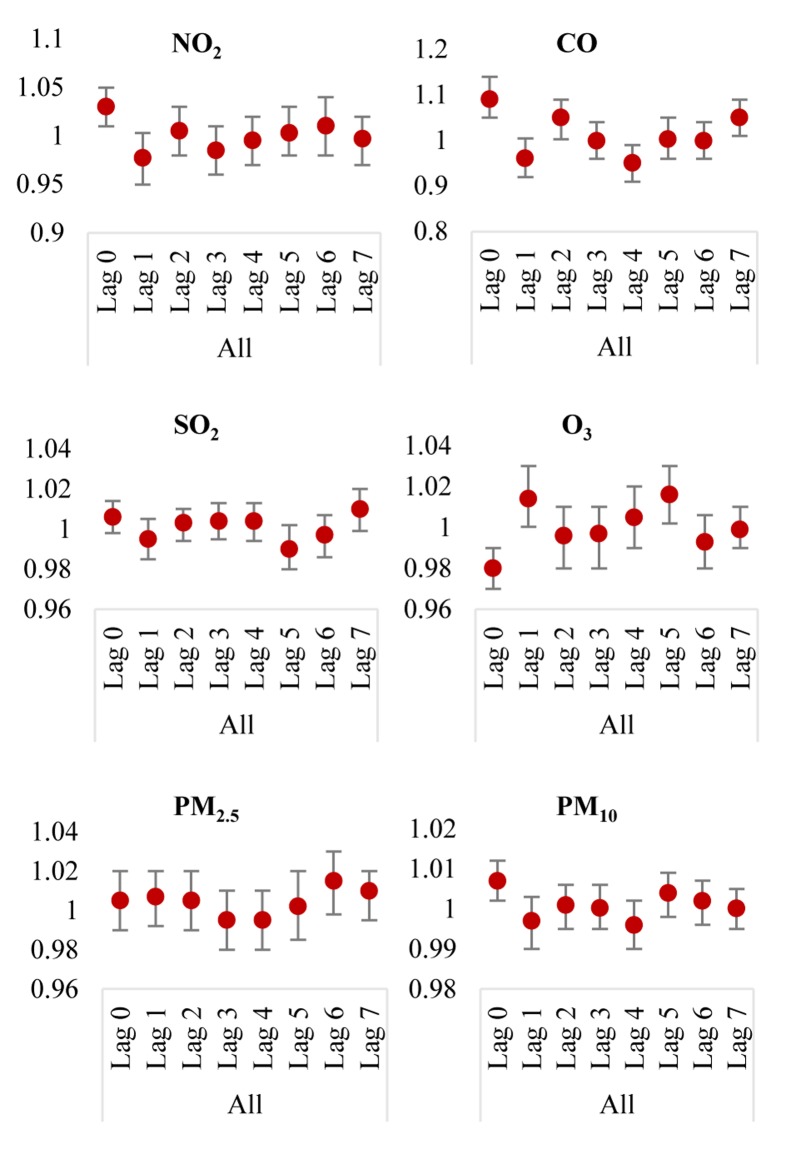
Table 2 and figure 2 show the effect of outdoor air pollutants on cardiovascular hospital admissions after controlling for long-term trend, DOW, and weather conditions for different lags in single-pollutant models. Significant direct effects were observed at lag 0 (day), for PM10 (RR = 1.007, P = 0.004), CO (RR = 1.094, P < 0.001) and NO2 (RR = 1.033, P = 0.006). Two air pollutants had significant direct lag effects, including CO at lag 2, and 7 ((RR = 1.094, P = 0.004), and (RR = 1.051, P = 0.004), respectively and O3 at lag 1 and 5 (RR = 1.014, P = 0.004) and (RR = 1.016, P = 0.004), respectively and shows that all pollutants significantly increased hospital admissions.
Table 2.
Rate ratios of cardiovascular admissions associated with 1 mg/m3 increase in CO or 10 μg/m3 increase in other air pollutants according to single lag, adjusted unconstrained and constrained distributed lag models for each air pollutant
| Pollutant All | Lag | Lag terms model one at a time RR (95% CI) | P | Adjusted unconstrained DLM RR (95% CI) | P | Adjusted constrained DLM RR (95% CI) | P |
|---|---|---|---|---|---|---|---|
| SO2 | Lag 0 | 1.006 (0.999-1.012) | 0.110 | 1.0060 (0.998-1.014) | 0.100 | 1.0050 (0.997-1.012) | 0.210 |
| Lag 1 | 1.001 (0.992-1.010) | 0.970 | 0.9950 (0.985-1.005) | 0.390 | 1.0003 (0.995-1.005) | 0.900 | |
| Lag 2 | 1.002 (0.995-1.009) | 0.520 | 1.0030 (0.994-1.01) | 0.630 | 1.0003 (0.995-1.005) | 0.900 | |
| Lag 3 | 1.002 (0.994-1.009) | 0.700 | 1.0040 (0.995-1.013) | 0.370 | 1.0005 (0.998-1.003) | 0.890 | |
| Lag 4 | 1.001 (0.993-1.008) | 0.770 | 1.0040 (0.994-1.013) | 0.490 | 1.0005 (0.998-1.003) | 0.890 | |
| Lag 5 | 0.995 (0.990-1.002) | 0.200 | 0.9920 (0.982-1.002) | 0.180 | 1.0005 (0.998-1.003) | 0.890 | |
| Lag 6 | 0.997 (0.990-1.005) | 0.510 | 0.9970 (0.986-1.007) | 0.710 | 1.0005 (0.998-1.003) | 0.890 | |
| Lag 7 | 1.002 (0.995-1.009) | 0.610 | 1.0100 (0.999-1.020) | 0.720 | 1.0005 (0.998-1.003) | 0.890 | |
| CO | Lag 0 | 1.070 (1.030-1.110) | < 0.001 | 1.0940 (1.051-1.140) | < 0.001 | 1.0820 (1.040-1.125) | < 0.001 |
| Lag 1 | 1.005 (0.971-1.040) | 0.800 | 0.9620 (0.920-1.005) | 0.410 | 0.9990 (0.975-1.025) | 0.620 | |
| Lag 2 | 1.040 (1.002-1.081) | 0.040 | 1.0500 (1.003-1.095) | 0.040 | 0.9990 (0.975-1.025) | 0.620 | |
| Lag 3 | 1.008 (0.971-1.045) | 0.630 | 0.9990 (0.960-1.044) | 0.970 | 1.0010 (0.990-1.013) | 0.760 | |
| Lag 4 | 0.975 (0.940-1.010) | 0.160 | 0.9500 (0.910-0.991) | 0.040 | 1.0010 (0.990-1.013) | 0.760 | |
| Lag 5 | 1.001 (0.966-1.040) | 0.940 | 1.0020 (0.960-1.050) | 0.970 | 1.0010 (0.990-1.013) | 0.760 | |
| Lag 6 | 1.020 (0.980-1.060) | 0.300 | 0.9990 (0.960-1.044) | 0.720 | 1.0010 (0.990-1.013) | 0.760 | |
| Lag 7 | 1.040 (0.999-1.071) | 0.051 | 1.0510 (1.010-1.094) | 0.040 | 1.0010 (0.990-1.013) | 0.760 | |
| NO2 | Lag 0 | 1.008 (0.992-1.025) | 0.320 | 1.0330 (1.010-1.055) | 0.006 | 1.0300 (1.007-1.050) | 0.009 |
| Lag 1 | 0.990 (0.973-1.010) | 0.210 | 0.9770 (0.951-1.003) | 0.065 | 0.9900 (0.980-1.001) | 0.070 | |
| Lag 2 | 0.990 (0.974-1.010) | 0.210 | 1.0050 (0.980-1.032) | 0.950 | 0.9900 (0.980-1.001) | 0.070 | |
| Lag 3 | 0.986 (0.970-1.002) | 0.080 | 0.9850 (0.960-1.012) | 0.360 | 0.9990 (0.995-1.005) | 0.450 | |
| Lag 4 | 0.990 (0.974-1.010) | 0.250 | 0.9950 (0.970-1.022) | 0.820 | 0.9990 (0.995-1.005) | 0.450 | |
| Lag 5 | 0.996 (0.980-1.012) | 0.620 | 1.0030 (0.980-1.030) | 0.870 | 0.9990 (0.995-1.005) | 0.450 | |
| Lag 6 | 0.998 (0.982-1.015) | 0.850 | 1.0100 (0.983-1.040) | 0.470 | 0.9990 (0.995-1.005) | 0.450 | |
| Lag 7 | 0.991 (0.975-1.008) | 0.320 | 0.9970 (0.975-1.020) | 0.450 | 0.9990 (0.995-1.005) | 0.450 | |
| O3 | Lag 0 | 0.985 (0.980-0.990) | 0.003 | 0.9800 (0.970-0.990) | < 0.001 | 0.9800 (0.970-0.990) | < 0.001 |
| Lag 1 | 0.997 (0.988-1.006) | 0.500 | 1.0140 (1.0003-1.030) | 0.045 | 1.0040 (0.998-1.010) | 0.230 | |
| Lag 2 | 0.996 (0.987-1.005) | 0.400 | 0.9960 (0.982-1.010) | 0.700 | 1.0040 (0.998-1.010) | 0.230 | |
| Lag 3 | 1.001 (0.992-1.029) | 0.900 | 0.9970 (0.983-1.011) | 0.360 | 1.0020 (0.999-1.005) | 0.090 | |
| Lag 4 | 1.005 (0.997-1.014) | 0.220 | 1.0050 (0.991-1.020) | 0.280 | 1.0020 (0.999-1.005) | 0.090 | |
| Lag 5 | 1.010 (0.999-1.020) | 0.070 | 1.0160 (1.002-1.030) | 0.010 | 1.0020 (0.999-1.005) | 0.090 | |
| Lag 6 | 0.999 (0.990-1.008) | 0.850 | 0.9930 (0.979-1.006) | 0.290 | 1.0020 (0.999-1.005) | 0.090 | |
| Lag 7 | 0.997 (0.990-1.005) | 0.460 | 0.9990 (0.990-1.011) | 0.870 | 1.0020 (0.999-1.005) | 0.090 | |
| PM2.5 | Lag 0 | 1.006 (0.992-1.020) | 0.360 | 1.0050 (0.990-1.020) | 0.630 | 1.0050 (0.990-1.020) | 0.560 |
| Lag 1 | 1.009 (0.996-1.022) | 0.180 | 1.0070 (0.992-1.022) | 0.220 | 1.0030 (0.994-1.010) | 0.490 | |
| Lag 2 | 1.004 (0.990-1.020) | 0.550 | 1.0050 (0.990-1.021) | 0.880 | 1.0030 (0.994-1.010) | 0.490 | |
| Lag 3 | 0.999 (0.986-1.014) | 0.990 | 0.9940 (0.978-1.010) | 0.720 | 1.0020 (0.998-1.007) | 0.230 | |
| Lag 4 | 0.999 (0.986-1.013) | 0.940 | 0.9950 (0.980-1.010) | 0.500 | 1.0020 (0.998-1.007) | 0.230 | |
| Lag 5 | 1.007 (0.993-1.021) | 0.280 | 1.0020 (0.985-1.020) | 0.670 | 1.0020 (0.998-1.007) | 0.230 | |
| Lag 6 | 1.015 (1.001-1.030) | 0.030 | 1.0150 (0.998-1.031) | 0.120 | 1.0020 (0.998-1.007) | 0.230 | |
| Lag 7 | 1.010 (0.997-1.024) | 0.140 | 1.0100 (0.995-1.021) | 0.540 | 1.0020 (0.998-1.007) | 0.230 | |
| PM10 | Lag 0 | 1.004 (0.999-1.010) | 0.090 | 1.0070 (1.002-1.012) | 0.004 | 1.0060 (1.001-1.010) | 0.010 |
| Lag 1 | 0.999 (0.995-1.004) | 0.760 | 0.9970 (0.991-1.003) | 0.280 | 0.9990 (0.996-1.002) | 0.330 | |
| Lag 2 | 0.999 (0.994-1.003) | 0.660 | 1.0010 (0.995-1.006) | 0.830 | 0.9990 (0.996-1.002) | 0.330 | |
| Lag 3 | 0.999 (0.994-1.003) | 0.630 | 1.0002 (0.995-1.006) | 0.700 | 1.0006 (0.999-1.002) | 0.860 | |
| Lag 4 | 0.998 (0.993-1.002) | 0.270 | 0.9960 (0.991-1.002) | 0.260 | 1.0006 (0.999-1.002) | 0.860 | |
| Lag 5 | 1.001 (0.997-1.005) | 0.530 | 1.0040 (0.998-1.009) | 0.240 | 1.0006 (0.999-1.002) | 0.860 | |
| Lag 6 | 1.002 (0.998-1.006) | 0.340 | 1.0020 (0.996-1.007) | 0.700 | 1.0006 (0.999-1.002) | 0.860 | |
| Lag 7 | 1.001 (0.996-1.005) | 0.720 | 1.0001 (0.995-1.005) | 0.800 | 1.0006 (0.999-1.002) | 0.860 |
DLM: Distributed lag models; RR: Rate ratios; CI: Confidence interval; CO: Carbon monoxide; NO2: Nitrogen dioxide; O3: Ozone; SO2: Sulfur dioxide; PM2.5: Particulate matter less than 2.5 μm; PM10: Particulate matter less than 10 μm
Figure 2.
Rate ratio (RRs) (95% confidence interval) of cardiovascular admissions with an increase of 1 mg/m3 in CO or 10 μg/m3 in other air pollutants according to adjusted unconstrained models
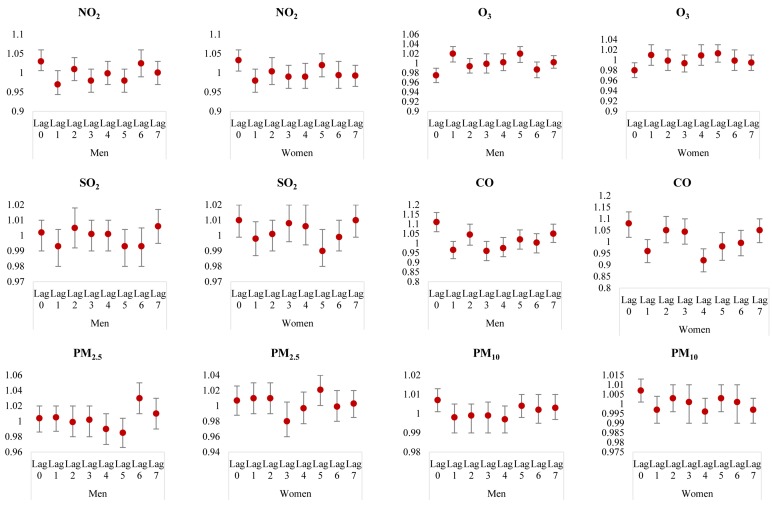
Table 3 and figure 3 show the effect of outdoor air pollutants on cardiovascular hospital admissions after controlling for confounders, among different genders. Significant effects were found for CO at lag 0 (RR = 1.08, P = 0.01), NO2 at lag 0 (RR = 1.033, P = 0.03), PM2.5 at lag 5 (RR = 1.021, P = 0.040) and PM10 at lag 0 (RR = 1.007, P = 0.014) in women, which shows these pollutants increase women hospital admissions. Also, men had a higher risk of cardiovascular admissions with an increase in PM10 on lag 0 (RR = 1.007, P = 0.020), CO at lag 0 (RR = 1.11, P < 0.001) and at lag 7 (RR = 1.053, P = 0.040), PM2.5 at lag 6 (RR = 1.03, P = 0.003), NO2 at lag 0 (RR = 1.033, P = 0.01), O3 at lag 1 (RR = 1.02, P = 0.023) and at lag 5 (RR = 1.02, P = 0.01).
Table 3.
Rate ratios of cardiovascular admissions associated with 1 mg/m3 increase in CO or 10 μg/m3 increase in other air pollutants according to single lag, adjusted unconstrained and constrained distributed lag models for each air pollutant in both genders
| Pollutant | Lag | Lag terms model one at a time RR (95% CI) | P | Adjusted unconstrained DLM RR (95% CI) | P | Adjusted constrained DLM RR (95% CI) | P | |
|---|---|---|---|---|---|---|---|---|
| Men | SO2 | Lag 0 | 1.0030 (0.996-1.012) | 0.350 | 1.002 (0.992-1.012) | 0.450 | 1.00100 (0.911-1.011) | 0.760 |
| Lag 1 | 0.9980 (0.990-1.007) | 0.720 | 0.993 (0.981-1.004) | 0.230 | 1.00010 (0.994-1.006) | 0.900 | ||
| Lag 2 | 1.0030 (0.995-1.011) | 0.430 | 1.005 (0.992-1.018) | 0.350 | 1.00010 (0.994-1.006) | 0.900 | ||
| Lag 3 | 0.9990 (0.991-1.008) | 0.860 | 1.001 (0.990-1.012) | 0.890 | 0.99900 (0.996-1.002) | 0.360 | ||
| Lag 4 | 1.0001 (0.991-1.010) | 0.990 | 1.001 (0.991-1.013) | 0.840 | 0.99900 (0.996-1.002) | 0.360 | ||
| Lag 5 | 0.9950 (0.985-1.004) | 0.230 | 0.993 (0.981-1.004) | 0.380 | 0.99900 (0.996-1.002) | 0.360 | ||
| Lag 6 | 0.9960 (0.987-1.005) | 0.380 | 0.994 (0.982-1.005) | 0.550 | 0.99900 (0.996-1.002) | 0.360 | ||
| Lag 7 | 0.9980 (0.990-1.007) | 0.700 | 1.006 (0.995-1.017) | 0.860 | 0.99900 (0.996-1.002) | 0.360 | ||
| CO | Lag 0 | 1.0900 (1.040-1.130) | < 0.001 | 1.111 (1.060-1.164) | < 0.001 | 1.10000 (1.050-1.151) | < 0.001 | |
| Lag 1 | 1.0150 (0.971-1.060) | 0.500 | 0.965 (0.920-1.014) | 0.080 | 0.99300 (0.965-1.023) | 0.310 | ||
| Lag 2 | 1.0350 (0.990-1.081) | 0.090 | 1.044 (0.991-1.100) | 0.240 | 0.99300 (0.965-1.023) | 0.310 | ||
| Lag 3 | 0.9900 (0.950-1.030) | 0.650 | 0.961 (0.912-1.012) | 0.180 | 1.00500 (0.991-1.020) | 0.710 | ||
| Lag 4 | 0.9910 (0.950-1.031) | 0.560 | 0.975 (0.930-1.030) | 0.430 | 1.00500 (0.991-1.020) | 0.710 | ||
| Lag 5 | 1.0200 (0.980-1.060) | 0.310 | 1.020 (0.970-1.072) | 0.470 | 1.00500 (0.991-1.020) | 0.710 | ||
| Lag 6 | 1.0310 (0.990-1.071) | 0.190 | 1.003 (0.953-1.056) | 0.830 | 1.00500 (0.991-1.020) | 0.710 | ||
| Lag 7 | 1.0400 (1.003-1.079) | 0.036 | 1.053 (1.004-1.104) | 0.040 | 1.00500 (0.991-1.020) | 0.710 | ||
| NO2 | Lag 0 | 1.0100 (0.990-1.030) | 0.400 | 1.033 (1.006-1.061) | 0.010 | 1.02600 (1.001-1.052) | 0.030 | |
| Lag 1 | 0.9900 (0.970-1.008) | 0.250 | 0.975 (0.944-1.006) | 0.090 | 0.98700 (0.972-1.002) | 0.100 | ||
| Lag 2 | 0.9900 (0.971-1.010) | 0.290 | 1.011 (0.980-1.040) | 0.830 | 0.98700 (0.972-1.002) | 0.100 | ||
| Lag 3 | 0.9850 (0.965-1.003) | 0.100 | 0.982 (0.951-1.013) | 0.320 | 1.00004 (0.994-1.006) | 0.780 | ||
| Lag 4 | 0.9900 (0.971-1.010) | 0.280 | 0.999 (0.977-1.031) | 0.850 | 1.00004 (0.994-1.006) | 0.780 | ||
| Lag 5 | 0.9910 (0.973-1.011) | 0.380 | 0.983 (0.952-1.015) | 0.220 | 1.00004 (0.994-1.006) | 0.780 | ||
| Lag 6 | 1.0050 (0.986-1.025) | 0.620 | 1.025 (0.993-1.600) | 0.110 | 1.00004 (0.994-1.006) | 0.780 | ||
| Lag 7 | 1.0001 (0.981-1.020) | 0.990 | 1.001 (0.974-1.030) | 0.840 | 1.00004 (0.994-1.006) | 0.780 | ||
| O3 | Lag 0 | 0.9860 (0.976-0.997) | 0.008 | 0.975 (0.961-0.990) | < 0.001 | 0.97800 (0.964-0.991) | 0.001 | |
| Lag 1 | 0.9980 (0.988-1.008) | 0.760 | 1.020 (1.003-1.035) | 0.020 | 1.00600 (0.998-1.014) | 0.180 | ||
| Lag2 | 0.9950 (0.985-1.005) | 0.370 | 0.994 (0.980-1.010) | 0.430 | 1.00600 (0.998-1.014) | 0.180 | ||
| Lag 3 | 1.0010 (0.991-1.011) | 0.830 | 0.999 (0.984-1.020) | 0.740 | 1.00100 (0.998-1.005) | 0.280 | ||
| Lag 4 | 1.0050 (0.995-1.015) | 0.320 | 1.002 (0.985-1.020) | 0.640 | 1.00100 (0.998-1.005) | 0.280 | ||
| Lag 5 | 1.0100 (0.999-1.020) | 0.110 | 1.020 (1.002-1.035) | 0.010 | 1.00100 (0.998-1.005) | 0.280 | ||
| Lag 6 | 0.9980 (0.988-1.008) | 0.700 | 0.987 (0.971-1.003) | 0.090 | 1.00100 (0.998-1.005) | 0.280 | ||
| Lag 7 | 0.9970 (0.987-1.007) | 0.590 | 1.002 (0.990-1.016) | 0.690 | 1.00100 (0.998-1.005) | 0.280 | ||
| PM2.5 | Lag 0 | 1.0050 (0.990-1.021) | 0.530 | 1.004 (0.986-1.022) | 0.810 | 1.00500 (0.987-1.023) | 0.650 | |
| Lag 1 | 1.0060 (0.990-1.022) | 0.420 | 1.005 (0.987-1.024) | 0.230 | 0.99900 (0.990-1.010) | 0.940 | ||
| Lag 2 | 0.9980 (0.982-1.014) | 0.840 | 0.999 (0.980-1.020) | 0.560 | 0.99900 (0.990-1.010) | 0.940 | ||
| Lag 3 | 1.0030 (0.987-1.020) | 0.720 | 1.002 (0.983-1.021) | 0.530 | 1.00300 (0.998-1.008) | 0.170 | ||
| Lag 4 | 0.9960 (0.980-1.012) | 0.630 | 0.990 (0.972-1.010) | 0.300 | 1.00300 (0.998-1.008) | 0.170 | ||
| Lag 5 | 0.9970 (0.982-1.014) | 0.780 | 0.985 (0.966-1.004) | 0.260 | 1.00300 (0.998-1.008) | 0.170 | ||
| Lag 6 | 1.0240 (1.008-1.040) | 0.003 | 1.030 (1.010-1.050) | 0.003 | 1.00300 (0.998-1.008) | 0.170 | ||
| Lag 7 | 1.0140 (0.998-1.030) | 0.090 | 1.010 (0.991-1.030) | 0.390 | 1.00300 (0.998-1.008) | 0.170 | ||
| PM10 | Lag 0 | 1.0030 (0.998-1.008) | 0.180 | 1.007 (1.001-1.012) | 0.020 | 1.00600 (1.001-1.011) | 0.040 | |
| Lag 1 | 0.9980 (0.993-1.004) | 0.630 | 0.998 (0.991-1.005) | 0.510 | 0.99800 (0.995-1.001) | 0.210 | ||
| Lag 2 | 0.9970 (0.992-1.002) | 0.250 | 0.999 (0.992-1.005) | 0.810 | 0.99800 (0.995-1.001) | 0.210 | ||
| Lag 3 | 0.9970 (0.992-1.002) | 0.220 | 0.999 (0.990-1.006) | 0.440 | 1.00100 (0.999-1.003) | 0.800 | ||
| Lag 4 | 0.9970 (0.991-1.002) | 0.220 | 0.997 (0.990-1.004) | 0.290 | 1.00100 (0.999-1.003) | 0.800 | ||
| Lag 5 | 1.0010 (0.996-1.006) | 0.560 | 1.004 (0.998-1.010) | 0.180 | 1.00100 (0.999-1.003) | 0.800 | ||
| Lag 6 | 1.0030 (0.998-1.008) | 0.300 | 1.002 (0.995-1.010) | 0.950 | 1.00100 (0.999-1.003) | 0.800 | ||
| Lag 7 | 1.0030 (0.998-1.081) | 0.260 | 1.003 (0.997-1.010) | 0.540 | 1.00100 (0.999-1.003) | 0.800 | ||
| Women | SO2 | Lag 0 | 1.0100 (0.999-1.020) | 0.090 | 1.010 (0.999-1.020) | 0.052 | 1.01000 (0.999-1.020) | 0.052 |
| Lag 1 | 1.0020 (0.993-1.011) | 0.660 | 0.998 (0.987-1.009) | 0.800 | 1.00060 (0.994-1.007) | 0.850 | ||
| Lag 2 | 1.0010 (0.992-1.010) | 0.800 | 1.001 (0.990-1.011) | 0.900 | 1.00060 (0.994-1.007) | 0.850 | ||
| Lag 3 | 1.0040 (0.995-1.013) | 0.390 | 1.008 (0.996-1.020) | 0.180 | 1.00200 (0.999-1.005) | 0.460 | ||
| Lag 4 | 1.0020 (0.993-1.011) | 0.620 | 1.006 (0.994-1.020) | 0.320 | 1.00200 (0.999-1.005) | 0.460 | ||
| Lag 5 | 0.9950 (0.985-1.005) | 0.350 | 0.990 (0.980-1.004) | 0.180 | 1.00200 (0.999-1.005) | 0.460 | ||
| Lag 6 | 0.9990 (0.990-1.008) | 0.840 | 0.999 (0.990-1.012) | 0.900 | 1.00200 (0.999-1.005) | 0.460 | ||
| Lag 7 | 1.0060 (0.997-1.014) | 0.210 | 1.010 (0.999-1.020) | 0.400 | 1.00200 (0.999-1.005) | 0.460 | ||
| CO | Lag 0 | 1.0500 (1.010-1.100) | 0.020 | 1.080 (1.023-1.132) | 0.010 | 1.06300 (1.012-1.120) | 0.030 | |
| Lag 1 | 0.9950 (0.950-1.041) | 0.830 | 0.960 (0.910-1.013) | 0.100 | 1.00600 (0.975-1.040) | 0.860 | ||
| Lag 2 | 1.0400 (0.996-1.090) | 0.080 | 1.052 (0.996-1.112) | 0.110 | 1.00600 (0.975-1.040) | 0.860 | ||
| Lag 3 | 1.0310 (0.980-1.081) | 0.200 | 1.044 (0.990-1.100) | 0.140 | 0.99600 (0.982-1.011) | 0.380 | ||
| Lag 4 | 0.9600 (0.920-1.003) | 0.070 | 0.920 (0.871-0.973) | 0.009 | 0.99600 (0.982-1.011) | 0.380 | ||
| Lag 5 | 0.9810 (0.940-1.021) | 0.330 | 0.982 (0.930-1.040) | 0.460 | 0.99600 (0.982-1.011) | 0.380 | ||
| Lag 6 | 1.0100 (0.965-1.051) | 0.710 | 0.995 (0.942-1.051) | 0.730 | 0.99600 (0.982-1.011) | 0.380 | ||
| Lag 7 | 1.0250 (0.980-1.070) | 0.270 | 1.050 (0.997-1.100) | 0.190 | 0.99600 (0.982-1.011) | 0.380 | ||
| NO2 | Lag 0 | 1.0100 (0.990-1.030) | 0.420 | 1.033 (1.005-1.062) | 0.030 | 1.03100 (1.004-1.060) | 0.030 | |
| Lag 1 | 0.9900 (0.971-1.010) | 0.340 | 0.980 (0.950-1.011) | 0.210 | 0.99000 (0.974-1.005) | 0.120 | ||
| Lag 2 | 0.9900 (0.970-1.009) | 0.300 | 1.004 (0.971-1.040) | 0.890 | 0.99000 (0.974-1.005) | 0.120 | ||
| Lag 3 | 0.9870 (0.967-1.007) | 0.210 | 0.990 (0.960-1.021) | 0.610 | 0.99900 (0.993-1.006) | 0.340 | ||
| Lag 4 | 0.9910 (0.972-1.011) | 0.400 | 0.992 (0.960-1.025) | 0.570 | 0.99900 (0.993-1.006) | 0.340 | ||
| Lag 5 | 1.0010 (0.981-1.021) | 0.930 | 1.023 (0.990-1.060) | 0.330 | 0.99900 (0.993-1.006) | 0.340 | ||
| Lag 6 | 0.9910 (0.972-1.011) | 0.400 | 0.994 (0.961-1.030) | 0.850 | 0.99900 (0.993-1.006) | 0.340 | ||
| Lag 7 | 0.9830 (0.963-1.003) | 0.090 | 0.993 (0.965-1.021) | 0.270 | 0.99900 (0.993-1.006) | 0.340 | ||
| O3 | Lag 0 | 0.9900 (0.980-0.998) | 0.020 | 0.981 (0.966-0.995) | 0.007 | 0.98200 (0.970-0.995) | 0.006 | |
| Lag 1 | 0.9950 (0.984-1.006) | 0.380 | 1.011 (0.991-1.030) | 0.470 | 1.00300 (0.994-1.011) | 0.540 | ||
| Lag2 | 0.9970 (0.987-1.008) | 0.640 | 0.994 (0.981-1.020) | 0.820 | 1.00300 (0.994-1.011) | 0.540 | ||
| Lag 3 | 0.9990 (0.990-1.010) | 0.970 | 0.994 (0.977-1.011) | 0.210 | 1.00300 (0.999-1.006) | 0.090 | ||
| Lag 4 | 1.0060 (0.994-1.016) | 0.310 | 1.009 (0.991-1.030) | 0.170 | 1.00300 (0.999-1.006) | 0.090 | ||
| Lag 5 | 1.0080 (0.997-1.020) | 0.140 | 1.013 (0.996-1.031) | 0.090 | 1.00300 (0.999-1.006) | 0.090 | ||
| Lag 6 | 1.0010 (0.990-1.011) | 0.930 | 0.999 (0.982-1.020) | 0.900 | 1.00300 (0.999-1.006) | 0.090 | ||
| Lag 7 | 0.9960 (0.985-1.007) | 0.490 | 0.995 (0.980-1.010) | 0.470 | 1.00300 (0.999-1.006) | 0.090 | ||
| PM2.5 | Lag 0 | 1.0070 (0.990-1.025) | 0.380 | 1.007 (0.988-1.026) | 0.600 | 1.00500 (0.987-1.024) | 0.640 | |
| Lag 1 | 1.0120 (0.995-1.030) | 0.140 | 1.010 (0.992-1.031) | 0.370 | 1.00800 (0.997-1.020) | 0.260 | ||
| Lag 2 | 1.0100 (0.993-1.030) | 0.220 | 1.012 (0.992-1.033) | 0.390 | 1.00800 (0.997-1.020) | 0.260 | ||
| Lag 3 | 0.9960 (0.980-1.014) | 0.700 | 0.984 (0.964-1.005) | 0.200 | 1.00200 (0.996-1.008) | 0.560 | ||
| Lag 4 | 1.0040 (0.990-1.021) | 0.660 | 0.997 (0.977-1.018) | 0.900 | 1.00200 (0.996-1.008) | 0.560 | ||
| Lag 5 | 1.0200 (1.001-1.040) | 0.030 | 1.021 (1.0006-1.041) | 0.040 | 1.00200 (0.996-1.008) | 0.560 | ||
| Lag 6 | 1.0070 (0.990-1.024) | 0.530 | 0.999 (0.980-1.020) | 0.720 | 1.00200 (0.996-1.008) | 0.560 | ||
| Lag 7 | 1.0070 (0.990-1.023) | 0.450 | 1.003 (0.985-1.022) | 0.860 | 1.00200 (0.996-1.008) | 0.560 | ||
| PM10 | Lag 0 | 1.0040 (0.999-1.010) | 0.140 | 1.007 (1.001-1.013) | 0.014 | 1.00600 (0.999-1.011) | 0.360 | |
| Lag 1 | 0.9990 (0.994-1.005) | 0.900 | 0.997 (0.990-1.004) | 0.250 | 1.00020 (0.996-1.004) | 0.740 | ||
| Lag 2 | 1.0010 (0.996-1.007) | 0.640 | 1.003 (0.996-1.010) | 0.530 | 1.00020 (0.996-1.004) | 0.740 | ||
| Lag 3 | 1.0010 (0.996-1.007) | 0.620 | 1.001 (0.994-1.010) | 0.860 | 0.99900 (0.998-1.001) | 0.980 | ||
| Lag 4 | 0.9980 (0.992-1.004) | 0.590 | 0.996 (0.990-1.003) | 0.430 | 0.99900 (0.998-1.001) | 0.980 | ||
| Lag 5 | 1.0010 (0.995-1.007) | 0.670 | 1.003 (0.996-1.010) | 0.540 | 0.99900 (0.998-1.001) | 0.980 | ||
| Lag 6 | 1.0010 (0.996-1.007) | 0.600 | 1.001 (0.994-1.010) | 0.540 | 0.99900 (0.998-1.001) | 0.980 | ||
| Lag 7 | 0.9980 (0.993-1.004) | 0.550 | 0.997 (0.990-1.003) | 0.280 | 0.99900 (0.998-1.001) | 0.980 |
DLM: Distributed lag models; RR: Rate ratios; CI: Confidence interval; CO: Carbon monoxide; NO2: Nitrogen dioxide; O3: Ozone; SO2: Sulfur dioxide; PM2.5: Particulate matter less than 2.5 μm; PM10: Particulate matter less than 10 μm
Figure 3.
Rate ratios (RR, 95% confidence intervals) of cardiovascular admissions with an increase of 1 mg/m3 in CO or 10 μg/m3 in other air pollutants according to adjusted unconstrained distributed lag models for each air pollutant in both genders CO: Carbon monoxide; NO2: Nitrogen dioxide; O3: Ozone; SO2: Sulfur dioxide; PM2.5: Particulate matter less than 2.5 μm; PM10: Particulate matter less than 10 μm
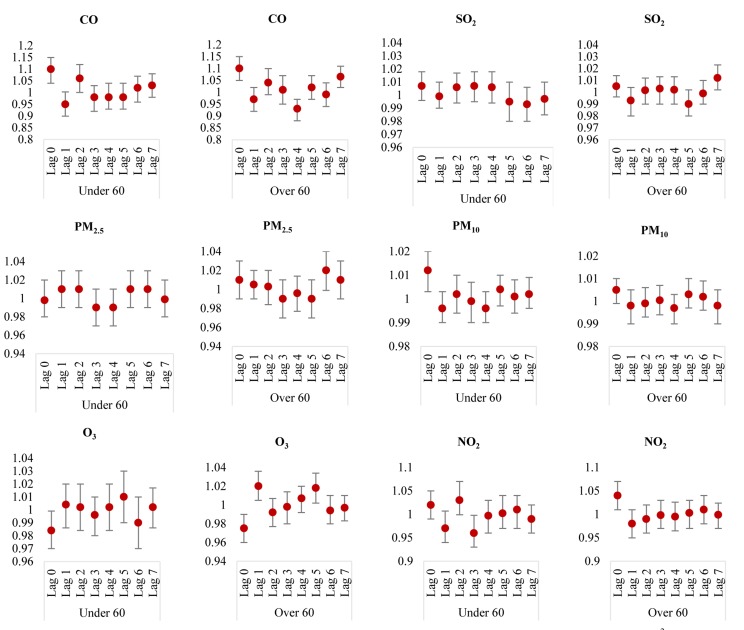
Table 4 and figure 4 show the effect of outdoor air pollutants on cardiovascular disease hospital admissions after controlling for long-term trend, DOW, and weather conditions for different lags in single-pollutant models among different age groups.
Table 4.
Rate ratios of cardiovascular admissions associated with 1 mg/m3 increase in CO or 10 μg/m3 increase in other air pollutants according to single lag, adjusted unconstrained and constrained distributed lag models for each air pollutant among two age groups
| Pollutant | Lag | Lag terms model one at a time RR (95% CI) | P | Adjusted unconstrained DLM RR (95% CI) | P | Adjusted constrained DLM RR (95% CI) | P | |
|---|---|---|---|---|---|---|---|---|
| Over 60 | SO2 | Lag 0 | 1.0050 (0.997-1.013) | 0.240 | 1.0050 (0.996-1.014) | 0.200 | 1.00500 (0.997-1.014) | 0.220 |
| Lag 1 | 0.9960 (0.988-1.005) | 0.370 | 0.9930 (0.982-1.004) | 0.270 | 0.99800 (0.990-1.003) | 0.430 | ||
| Lag 2 | 0.9900 (0.990-1.006) | 0.630 | 1.0020 (0.991-1.012) | 0.970 | 0.99800 (0.99-1.003) | 0.430 | ||
| Lag 3 | 0.9970 (0.990-1.006) | 0.550 | 1.0030 (0.992-1.013) | 0.710 | 1.00100 (0.998-1.004) | 0.990 | ||
| Lag 4 | 0.9980 (0.990-1.006) | 0.580 | 1.0020 (0.991-1.013) | 0.710 | 1.00100 (0.998-1.004) | 0.990 | ||
| Lag 5 | 0.9950 (0.986-1.003) | 0.260 | 0.9900 (0.980-1.002) | 0.180 | 1.00100 (0.998-1.004) | 0.990 | ||
| Lag 6 | 1.0010 (0.992-1.010) | 0.870 | 0.9990 (0.990-1.010) | 0.750 | 1.00100 (0.998-1.004) | 0.990 | ||
| Lag 7 | 1.0070 (0.999-1.015) | 0.070 | 1.0120 (1.002-1.023) | 0.030 | 1.00100 (0.998-1.004) | 0.990 | ||
| CO | Lag 0 | 1.0750 (1.030-1.120) | < 0.001 | 1.1000 (1.050-1.150) | < 0.001 | 1.08400 (1.040-1.140) | 0.001 | |
| Lag 1 | 1.0100 (0.971-1.050) | 0.530 | 0.9710 (0.923-1.021) | 0.180 | 1.00200 (0.973-1.030) | 0.810 | ||
| Lag 2 | 1.0400 (0.996-1.080) | 0.070 | 1.0410 (0.990-1.100) | 0.170 | 1.00200 (0.973-1.030) | 0.810 | ||
| Lag 3 | 1.0210 (0.980-1.060) | 0.460 | 1.0140 (0.963-1.070) | 0.800 | 1.00200 (0.990-1.015) | 0.880 | ||
| Lag 4 | 0.9650 (0.930-1.005) | 0.090 | 0.9300 (0.880-0.974) | 0.009 | 1.00200 (0.990-1.015) | 0.880 | ||
| Lag 5 | 1.0100 (0.971-1.051) | 0.660 | 1.0200 (0.970-1.070) | 0.600 | 1.00200 (0.990-1.015) | 0.880 | ||
| Lag 6 | 1.0200 (0.981-1.060) | 0.310 | 0.9900 (0.941-1.041) | 0.530 | 1.00200 (0.990-1.015) | 0.880 | ||
| Lag 7 | 1.0500 (1.010-1.090) | 0.020 | 1.0650 (1.020-1.116) | 0.020 | 1.00200 (0.990-1.015) | 0.880 | ||
| NO2 | Lag 0 | 1.0100 (0.992-1.030) | 0.280 | 1.0400 (1.010-1.070) | 0.005 | 1.04000 (1.014-1.064) | 0.004 | |
| Lag 1 | 0.9900 (0.971-1.007) | 0.240 | 0.9800 (0.950-1.010) | 0.170 | 0.98300 (0.970-0.997) | 0.010 | ||
| Lag 2 | 0.9860 (0.970-1.004) | 0.120 | 0.9900 (0.960-1.020) | 0.340 | 0.98300 (0.970-0.997) | 0.010 | ||
| Lag 3 | 0.9900 (0.971-1.007) | 0.230 | 0.9980 (0.970-1.030) | 0.770 | 1.00200 (0.996-1.007) | 0.980 | ||
| Lag 4 | 0.9930 (0.975-1.011) | 0.450 | 0.9950 (0.965-1.026) | 0.910 | 1.00200 (0.996-1.007) | 0.980 | ||
| Lag 5 | 0.9980 (0.980-1.016) | 0.840 | 1.0030 (0.973-1.034) | 0.840 | 1.00200 (0.996-1.007) | 0.980 | ||
| Lag 6 | 1.0020 (0.984-1.020) | 0.840 | 1.0100 (0.980-1.041) | 0.480 | 1.00200 (0.996-1.007) | 0.980 | ||
| Lag 7 | 0.9960 (0.980-1.014) | 0.680 | 0.9990 (0.973-1.024) | 0.690 | 1.00200 (0.996-1.007) | 0.980 | ||
| O3 | Lag 0 | 0.9870 (0.977-0.997) | 0.010 | 0.9750 (0.960-0.990) | < 0.001 | 0.97500 (0.964-0.990) | < 0.001 | |
| Lag 1 | 1.0001 (0.990-1.010) | 0.970 | 1.0200 (1.005-1.036) | 0.015 | 1.00600 (0.998-1.013) | 0.130 | ||
| Lag2 | 0.9990 (0.990-1.008) | 0.790 | 0.9920 (0.977-1.007) | 0.500 | 1.00600 (0.998-1.013) | 0.130 | ||
| Lag 3 | 1.0030 (0.993-1.013) | 0.470 | 0.9980 (0.980-1.014) | 0.550 | 1.00300 (0.999-1.006) | 0.052 | ||
| Lag 4 | 1.0100 (0.998-1.020) | 0.110 | 1.0070 (0.992-1.020) | 0.250 | 1.00300 (0.999-1.006) | 0.052 | ||
| Lag 5 | 1.0100 (1.001-1.020) | 0.040 | 1.0180 (1.002-1.034) | 0.010 | 1.00300 (0.999-1.006) | 0.052 | ||
| Lag 6 | 0.9990 (0.990-1.010) | 0.970 | 0.9940 (0.980-1.010) | 0.370 | 1.00300 (0.999-1.006) | 0.052 | ||
| Lag 7 | 0.9970 (0.986-1.007) | 0.550 | 0.9970 (0.983-1.011) | 0.830 | 1.00300 (0.999-1.006) | 0.052 | ||
| PM2.5 | Lag 0 | 1.0080 (0.993-1.024) | 0.290 | 1.0100 (0.992-1.030) | 0.400 | 1.01000 (0.993-1.030) | 0.300 | |
| Lag 1 | 1.0070 (0.991-1.022) | 0.390 | 1.0050 (0.990-1.023) | 0.320 | 1.00050 (0.990-1.011) | 0.880 | ||
| Lag 2 | 0.9990 (0.984-1.016) | 0.980 | 1.0030 (0.984-1.021) | 0.840 | 1.00050 (0.990-1.011) | 0.880 | ||
| Lag 3 | 0.9970 (0.982-1.013) | 0.750 | 0.9940 (0.976-1.013) | 0.750 | 1.00300 (0.998-1.008) | 0.380 | ||
| Lag 4 | 0.9980 (0.983-1.014) | 0.830 | 0.9960 (0.977-1.014) | 0.650 | 1.00300 (0.998-1.008) | 0.380 | ||
| Lag 5 | 1.0010 (0.984-1.020) | 0.970 | 0.9940 (0.975-1.013) | 0.570 | 1.00300 (0.998-1.008) | 0.380 | ||
| Lag 6 | 1.0200 (1.002-1.033) | 0.030 | 1.0200 (0.999-1.040) | 0.130 | 1.00300 (0.998-1.008) | 0.380 | ||
| Lag 7 | 1.0130 (0.998-1.030) | 0.090 | 1.0100 (0.993-1.030) | 0.250 | 1.00300 (0.998-1.008) | 0.380 | ||
| PM10 | Lag 0 | 1.0020 (0.997-1.007) | 0.320 | 1.0050 (0.999-1.011) | 0.080 | 1.00500 (0.999-1.014) | 0.080 | |
| Lag 1 | 0.9990 (0.994-1.004) | 0.820 | 0.9980 (0.992-1.005) | 0.480 | 0.99900 (0.996-1.003) | 0.490 | ||
| Lag 2 | 0.9980 (0.990-1.004) | 0.640 | 0.9990 (0.993-1.006) | 0.870 | 0.99900 (0.996-1.003) | 0.490 | ||
| Lag 3 | 0.9990 (0.990-1.004) | 0.710 | 1.0004 (0.994-1.007) | 0.600 | 1.00040 (0.999-1.002) | 0.840 | ||
| Lag 4 | 0.9980 (0.993-1.003) | 0.420 | 0.9970 (0.990-1.003) | 0.280 | 1.00040 (0.999-1.002) | 0.840 | ||
| Lag 5 | 1.0010 (0.996-1.006) | 0.650 | 1.0030 (0.997-1.010) | 0.260 | 1.00040 (0.999-1.002) | 0.840 | ||
| Lag 6 | 1.0020 (0.997-1.007) | 0.380 | 1.0020 (0.996-1.009) | 0.640 | 1.00040 (0.999-1.002) | 0.840 | ||
| Lag 7 | 0.9990 (0.995-1.004) | 0.980 | 0.9980 (0.992-1.005) | 0.480 | 1.00040 (0.999-1.002) | 0.840 | ||
| Under 60 | SO2 | Lag 0 | 1.0070 (0.998-1.016) | 0.120 | 1.0100 (0.996-1.020) | 0.120 | 1.00400 (0.994-1.014) | 0.370 |
| Lag 1 | 1.0070 (0.997-1.016) | 0.150 | 0.9990 (0.987-1.011) | 0.880 | 1.00400 (0.998-1.010) | 0.170 | ||
| Lag 2 | 1.0100 (1.001-1.020) | 0.040 | 1.0060 (0.994-1.017) | 0.310 | 1.00400 (0.998-1.010) | 0.170 | ||
| Lag 3 | 1.0100 (0.999-1.020) | 0.080 | 1.0070 (0.995-1.019) | 0.190 | 1.00001 (0.996-1.004) | 0.750 | ||
| Lag 4 | 1.0070 (0.997-1.016) | 0.150 | 1.0060 (0.994-1.018) | 0.390 | 1.00001 (0.996-1.004) | 0.750 | ||
| Lag 5 | 0.9950 (0.985-1.005) | 0.320 | 0.9950 (0.983-1.010) | 0.420 | 1.00001 (0.996-1.004) | 0.750 | ||
| Lag 6 | 0.9910 (0.981-1.002) | 0.110 | 0.9930 (0.980-1.006) | 0.720 | 1.00001 (0.996-1.004) | 0.750 | ||
| Lag 7 | 0.9910 (0.981-1.002) | 0.110 | 0.9970 (0.985-1.010) | 0.130 | 1.00001 (0.996-1.004) | 0.750 | ||
| CO | Lag 0 | 1.0650 (1.020-1.110) | 0.005 | 1.1000 (1.040-1.151) | 0.004 | 1.08000 (1.024-1.140) | 0.010 | |
| Lag 1 | 0.9900 (0.950-1.041) | 0.760 | 0.9500 (0.900-1.003) | 0.100 | 0.99700 (0.965-1.030) | 0.530 | ||
| Lag 2 | 1.0400 (0.990-1.090) | 0.100 | 1.0600 (1.001-1.120) | 0.030 | 0.99700 (0.965-1.030) | 0.530 | ||
| Lag 3 | 0.9970 (0.951-1.040) | 0.920 | 0.9770 (0.923-1.034) | 0.790 | 1.00050 (0.986-1.016) | 0.710 | ||
| Lag 4 | 0.9900 (0.951-1.031) | 0.670 | 0.9840 (0.930-1.041) | 0.690 | 1.00050 (0.986-1.016) | 0.710 | ||
| Lag 5 | 0.9900 (0.946-1.035) | 0.650 | 0.9810 (0.927-1.040) | 0.500 | 1.00050 (0.986-1.016) | 0.710 | ||
| Lag 6 | 1.0160 (0.970-1.061) | 0.490 | 1.0200 (0.960-1.075) | 0.900 | 1.00050 (0.986-1.016) | 0.710 | ||
| Lag 7 | 1.0160 (0.970-1.062) | 0.480 | 1.0300 (0.980-1.085) | 0.680 | 1.00050 (0.986-1.016) | 0.710 | ||
| NO2 | Lag 0 | 1.0050 (0.983-1.030) | 0.650 | 1.0220 (0.992-1.053) | 0.100 | 1.01200 (0.984-1.041) | 0.260 | |
| Lag 1 | 0.9900 (0.970-1.012) | 0.380 | 0.9720 (0.940-1.007) | 0.090 | 0.99700 (0.980-1.014) | 0.600 | ||
| Lag 2 | 0.9970 (0.976-1.020) | 0.780 | 1.0350 (0.999-1.072) | 0.130 | 0.99700 (0.980-1.014) | 0.600 | ||
| Lag 3 | 0.980 0(0.960-1.002) | 0.070 | 0.9640 (0.930-0.998) | 0.040 | 0.99700 (0.990-1.003) | 0.140 | ||
| Lag 4 | 0.9860 (0.964-1.008) | 0.210 | 0.9970 (0.961-1.032) | 0.820 | 0.99700 (0.990-1.003) | 0.140 | ||
| Lag 5 | 0.9910 (0.970-1.013) | 0.430 | 1.0020 (0.970-1.040) | 0.900 | 0.99700 (0.990-1.003) | 0.140 | ||
| Lag 6 | 0.9920 (0.971-1.014) | 0.480 | 1.0100 (0.970-1.040) | 0.680 | 0.99700 (0.990-1.003) | 0.140 | ||
| Lag 7 | 0.9840 (0.963-1.006) | 0.150 | 0.9900 (0.960-1.020) | 0.350 | 0.99700 (0.990-1.003) | 0.140 | ||
| O3 | Lag 0 | 0.987 (0.976-0.998) | 0.020 | 0.9840 (0.970-0.999) | 0.040 | 0.98400 (0.970-0.998) | 0.040 | |
| Lag 1 | 0.9920 (0.981-1.003) | 0.160 | 1.0040 (0.986-1.022) | 0.770 | 1.00200 (0.993-1.011) | 0.790 | ||
| Lag 2 | 0.9920 (0.982-1.004) | 0.210 | 1.0020 (0.984-1.020) | 0.790 | 1.00200 (0.993-1.011) | 0.790 | ||
| Lag 3 | 0.9960 (0.985 -1.007) | 0.470 | 0.9960 (0.980-1.013) | 0.310 | 1.00100 (0.998-1.005) | 0.520 | ||
| Lag 4 | 1.0010 (0.990-1.012) | 0.800 | 1.0020 (0.984-1.020) | 0.560 | 1.00100 (0.998-1.005) | 0.520 | ||
| Lag 5 | 1.0050 (0.994 -1.015) | 0.390 | 1.0130 (0.995-1.031) | 0.100 | 1.00100 (0.998-1.005) | 0.520 | ||
| Lag 6 | 0.9980 (0.987-1.010) | 0.780 | 0.9920 (0.974-1.010) | 0.370 | 1.00100 (0.998-1.005) | 0.520 | ||
| Lag 7 | 0.9970 (0.986-1.008) | 0.560 | 1.0020 (0.986-1.017) | 0.950 | 1.00100 (0.998-1.005) | 0.520 | ||
| PM2.5 | Lag 0 | 1.0030 (0.985-1.021) | 0.760 | 0.9980 (0.980-1.020) | 0.760 | 0.99700 (0.978-1.017) | 0.750 | |
| Lag 1 | 1.0130 (0.995-1.031) | 0.140 | 1.0110 (0.991-1.030) | 0.280 | 1.00800 (0.996-1.020) | 0.250 | ||
| Lag 2 | 1.0110 (0.993-1.030) | 0.210 | 1.0100 (0.990-1.030) | 0.590 | 1.00800 (0.996-1.020) | 0.250 | ||
| Lag 3 | 1.0040 (0.986-1.022) | 0.640 | 0.9930 (0.973-1.015) | 0.820 | 1.00200 (0.996-1.010) | 0.220 | ||
| Lag 4 | 1.0010 (0.983-1.020) | 0.870 | 0.9910 (0.970-1.012) | 0.490 | 1.00200 (0.996-1.010) | 0.220 | ||
| Lag 5 | 1.0200 (1.002-1.040) | 0.030 | 1.0140 (0.993-1.035) | 0.100 | 1.00200 (0.996-1.010) | 0.220 | ||
| Lag 6 | 1.0120 (0.994-1.030) | 0.190 | 1.0100 (0.990-1.031) | 0.330 | 1.00200 (0.996-1.010) | 0.220 | ||
| Lag 7 | 1.0050 (0.990-1.020) | 0.560 | 0.9990 (0.980-1.020) | 0.760 | 1.00200 (0.996-1.010) | 0.220 | ||
| PM10 | Lag 0 | 1.0060 (1.001-1.011) | 0.040 | 1.0120 (1.003-1.020) | 0.004 | 1.00700 (1.002-1.013) | 0.010 | |
| Lag 1 | 0.9990 (0.993-1.005) | 0.790 | 0.9960 (0.990-1.003) | 0.240 | 0.99900 (0.995-1.003) | 0.320 | ||
| Lag 2 | 0.9990 (0.994-1.005) | 0.810 | 1.0020 (0.994-1.010) | 0.830 | 0.99900 (0.995-1.003) | 0.320 | ||
| Lag 3 | 0.9990 (0.993-1.004) | 0.660 | 0.9990 (0.992-1.007) | 0.950 | 1.00100 (0.999-1.003) | 0.560 | ||
| Lag 4 | 0.9000 (0.991-1.003) | 0.290 | 0.9960 (0.990-1.003) | 0.470 | 1.00100 (0.999-1.003) | 0.560 | ||
| Lag 5 | 1.0020 (0.996-1.007) | 0.550 | 1.0040 (0.997-1.011) | 0.470 | 1.00100 (0.999-1.003) | 0.560 | ||
| Lag 6 | 1.0020 (0.996-1.007) | 0.510 | 1.0010 (0.994-1.008) | 0.920 | 1.00100 (0.999-1.003) | 0.560 | ||
| Lag 7 | 1.0020 (0.997-1.008) | 0.470 | 1.0020 (0.996-1.009) | 0.600 | 1.00100 (0.999-1.003) | 0.560 |
DLM: Distributed lag models; RR: Rate ratios; CI: Confidence interval; CO: Carbon monoxide; NO2: Nitrogen dioxide; O3: Ozone; SO2: Sulfur dioxide; PM2.5: Particulate matter less than 2.5 μm; PM10: Particulate matter less than 10 μm
Figure 4.
Rate ratios (95% confidence intervals) of cardiovascular admissions with an increase of 1 mg/m3 in CO or 10 μg/m3 in other air pollutants according to adjusted unconstrained distributed lag models for each air pollutant among two age groups CO: Carbon monoxide; NO2: Nitrogen dioxide; O3: Ozone; SO2: Sulfur dioxide; PM2.5: Particulate matter less than 2.5 μm; PM10: Particulate matter less than 10 μm
Direct and statistically significant associations were found with SO2 at lag 7 (RR = 1.012, P = 0.030), CO at lag 0 (RR = 1.10, P < 0.001) and lag-7 (RR = 1.065, P = 0.02), NO2 at lag 0 (RR = 1.04, P = 0.005) and O3 at lag 1 (RR = 1.02, P = 0.015) and lag 5 (RR = 1.018, P = 0.010) in the elderly (aged > 60) group. The effect of CO and NO2 was the strongest in the elderly (aged > 60) group. In the under 60 years age group, we found direct significant associations with CO at lag 0 (RR = 1.10, P = 0.004) and at lag 2 (RR = 1.06, P = 0.03); and PM10 at lag 0 (RR = 1.012, P = 0.004). In this study, the age group of > 60 years were more susceptible to air pollutants with regard to cardiovascular hospital admissions.
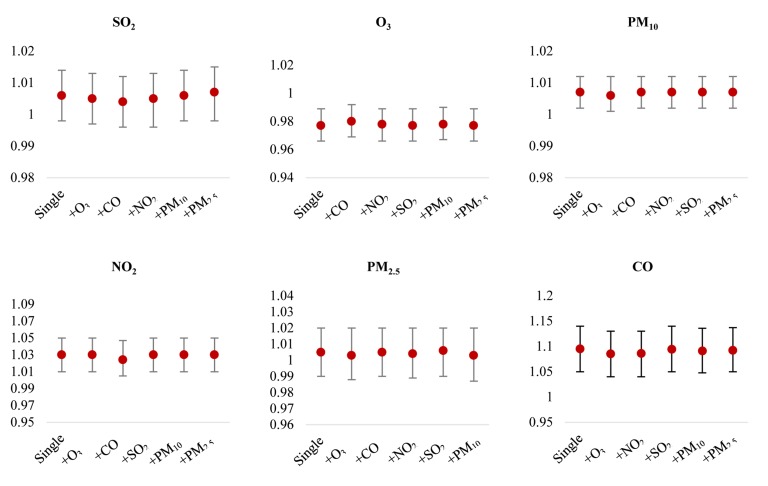
Figure 5 depicts the effect of outdoor air pollutants on cardiovascular hospital admissions after controlling for other air pollutants. When investigating the association between cardiovascular hospital admissions and NO2, while adjusted for CO, the estimated RR decreased to 1.05 (95% Cl 1.002-1.100), but remained significant. Almost all effects of air pollutants on cardiovascular hospital admissions were relatively constant after controlling for other air pollutants, and indicated that the evidence for the association between air pollutants and cardiovascular hospital admissions are relatively robust.
Figure 5.
Rate ratios (95% confidence intervals) of cardiovascular admissions with an increase of 1 mg/m3 in CO or 10 μg/m3 in other air pollutants in two-pollutant models CO: Carbon monoxide; NO2: Nitrogen dioxide; O3: Ozone; SO2: Sulfur dioxide; PM2.5: Particulate matter less than 2.5 μm; PM10: Particulate matter less than 10 μm
Discussion
In the present study, the short-term effect of air pollutions on cardiovascular hospital admissions in an industrial city from Iran was evaluated. This study provides evidence of an association between ambient NO2, PM10, SO2 and CO and cardiovascular hospital admissions.
In the present study, CO presented a significant effect on cardiovascular hospital admissions. This effect remained significant after adjustment for other air pollutants. These results are consistent with several previous studies.36-39 Bell et al.28 explored the association between short-term exposure to ambient CO and risk of cardiovascular disease hospital admissions in 126 urban counties in the US in 2009, and showed that daily cardiovascular admission increased by 0.96% for each 1 ppm increase in same-day CO levels.
Researchers stated that the risk of cardiovascular hospitalization persisted after adjustment for NO2 and even at low CO concentrations (< 1 ppm).28 Shahi et al. found evidence for a consistent positive association between short-term exposure to CO and cardiovascular hospital admissions in Tehran, Iran.38 A systematic review and meta-analysis including 34 studies conducted by Mustafic et al. in 2012 showed that the risk of MI increased by 4.8% for each increment of 1 mg/m3 in CO levels.36 In London, Ontario, Canada short-term exposure to CO and cardiovascular hospital admissions were significantly related and cardiovascular hospital admissions increased by 8.0% (95% CI 1.5-11.5) for an increase equal to the interquartile range in CO levels.37 A study done by Pereira Filho et al. in 2008, in Sao Paulo, Brazil investigated the effects of air pollution on CVD and diabetes and reported a direct effect of CO on cardiovascular emergency room (ER) visits for non-diabetic individuals.39
Our analysis showed significant increases in cardiovascular hospital admissions among women and the elderly for SO2. Martins et al. in 2006 reported a significant effect of SO2 on cardiovascular hospitalizations in the elderly in Sao Paulo, and this effect was higher among women.40 The results of the present study were also comparable to the study of Milojevic et al. in 2014, which did not find a significant effect of SO2 on cardiovascular hospital admissions in any age in England and Wales, UK.41 The association between air pollution and cardiovascular hospital admissions among individuals aged above 18 was also investigated by Jevtic et al. in 2014 in Novi Sad, Serbia, but they showed that SO2 was not significantly associated with the daily number of cardiovascular hospital admissions (RR = 0.972, 95% CI 0.908-1.040).42 Also in Taipei, Taiwan43 and Kerman, Iran44 researchers did not find a positive association between SO2 and cardiovascular hospital admissions. However, a study done by Xie et al. in 2014 reported that each 10 μg/m3 increase in SO2 concentration on the same day was positively associated with a 0.9% increase for total ER visits for coronary heart disease (CHD) in Shanghai, China.45 Mustafic et al.’s study in 2012 showed the risk of MI increased by 1% for each increment of 10 μg/m3 in SO2 levels.36 A study done in 2014 in Tianjin, China suggested that there was a positive association between SO2 and cardiovascular hospitalization and there was a 0.43% (95% CI 0.03-0.84) increase for each 10 μg/m3 increase in 2-day average concentrations of SO2.46 In Sao Paulo researchers also reported the positive effects of SO2 on cardiovascular ER visits.39
The results of this study are mainly consistent with previous studies indicating significant effects of ambient PM10 on cardiovascular hospital admissions. For example, a study by Zhang et al. in 2015 found 1.39% increased risk of cardiovascular emergency admissions for each 10 μg/m3 increase in PM10 at lag 5 and 1.72% increased risk for each 10 μg/m3 increase in PM10 for lag 0.35 In our study, the effect estimate was slightly smaller, with 0.7% (95% CI 1.002-1.010) increase in cardiovascular hospital admissions per 10 μg/m3 increase in PM10. A study from Seoul, Korea also reported that cardiovascular hospital admissions increased by 1.3% for each 10 μg/m3 increase in PM10 levels.47 In Sao Paulo significant associations were found between PM10 and cardiovascular hospitalizations for the elderly.40 In Shanghai, China a 1.1% increased risk of total CHD emergency visits was reported for each 10 μg/m3 increase in PM10 concentrations.45 In addition, Mustafic et al. also showed that the risk of MI increased by 0.6% for each 10 μg/m3 increment in PM10 levels.36 However, some studies have reported non-significant associations between PM10 concentrations and CVD. For example, the findings of Milojevic et al.’s study in 2014 from England and Wales,41 Willocks et al.’s study in 2012 from Scotland,48 and Hashemi et al.’s study in 2016 from Iran,44 did not show a direct significant association between PM10 and cardiovascular hospital admissions.
The results of Milojevic et al. reported that PM2.5 concentrations was not significantly associated with an increase in cardiovascular hospital admissions.41 However, some other studies have shown significant associations between PM2.5 concentrations and cardiovascular hospital admissions. For example, Dominici et al. in 2006 in the US found an increased risk of cardiovascular hospital admissions associated with exposure to PM2.5.49 Zanobetti et al. in 2009 in the US reported that admissions of cardiovascular diseases increased by 1.89% for each 10 μg/m3 increase in 2-day averaged PM2.5 levels.50 In this study, the effect of PM2.5 on daily hospital admissions for CVD in men and women were significant at lag 6 and lag 5.
In the current study, NO2 showed a significant association with hospital admissions for CVD. Several previous studies are in line with these results.27,36,41,45 Xie et al. reported that ER visits for CHD increased by 1.44% for each 10 μg/m3 increase in NO2 concentrations.45 A systematic review and meta-analysis study reported that each 10 μg/m3 increase in NO2 concentration was directly associated with an increase of 1.1% for MI.36 Milojevic et al. reported that only NO2 was associated with a raised risk of admission for CVD.41 Colais et al. also reported that hospital admissions for CVD were associated with exposure to NO2 in Italy.27 In Sao Paulo, direct associations were found between NO2 and cardiovascular ER visits for non-diabetic and diabetic individuals.39 The findings of Jevtic et al.’s study from Serbia showed positive associations between NO2 and daily admissions for CVD with RR = 1.047 (95% CI 1.007-1.089).42 However, a study from China reported that there was no association between NO2 and cardiovascular morbidity or cardiovascular hospitalization.46
In this study, distributed lag model suggested that ozone had a significant positive association with cardiovascular admissions at lag 1 and lag 5. Some studies have not shown a significant association between ozone and cardiovascular admissions. A systematic review and meta-analysis in 2013, including 35 articles reported that exposure to ozone did not have a significant adverse effect on heart failure hospitalizations.18 Another systematic review and meta-analysis done in 2012, including 34 studies also suggested that short-term exposure to ozone was not significantly associated with an increase in MI. In this review, each 10 μg/m3 increase in O3 concentration was associated with a 0.3% increase in MI risk but was not significant (P = 0.36).36 In Italy, no effect was reported for ozone on hospital admissions for cardiac diseases.27 On the other hand, some studies have reported adverse effects of ozone on cardiovascular hospital admissions.38,44 For example in Tehran researchers reported that each 10 μg/m3 increase in O3 was associated with a 0.2% increase in cardiovascular hospitalization on the same day (lag 0) in urban areas.38 Findings from Kerman also reported significant association between increase in ozone concentrations and cardiovascular hospital admissions.44
Some previous studies reported different effects of air pollutants between two genders and age groups with regard to cardiovascular diseases. The present study also explored the associations between air pollutants and human health, among different age groups and sexes, in terms of cardiovascular hospitalization. This study found significant positive associations for CO, NO2 and PM10 at lag 0 in women. Also, a higher risk of cardiovascular admissions was seen in older adults (> 60 years) for PM10 at lag 0, CO at lag 0 and lag 7, NO2 at lag 0, SO2 at lag 7, and O3 at lag 1 and lag 5. This result demonstrated that older adults (> 60 years) were more susceptible to exposure to air pollutants than younger adults (< 60 years) regarding CVD. Jalaludin et al. in 2006 in Sydney, reported a significant direct association between PM10, PM2.5, NO2, and CO and cardiovascular ER visits among the elderly (> 65 years).51
One of the limitations of the present study was the fact that we used aggregated data and thus the results cannot be directly inferred to individuals. Moreover, we were not able to control potential individual confounders such as socioeconomic status, occupation, eating habits, smoking, and migration that may affect cardiovascular hospital admissions.
Conclusion
Ambient air pollution is associated with cardiovascular disease hospital admissions in Arak. The elderly are more vulnerable to air pollution.
Acknowledgments
This study was funded by Kerman University of Medical Sciences (Grant No 95-249). The authors thank Kerman University of Medical Sciences (Ethical Code: IR.KMU.REC.1395.249), Arak University of Medical Sciences (Ethical Code: IR.ARAKMU.REC.1395.80), and the Arak Department of Environment and Meteorological Organization for their cooperation in this study.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Xu Q, Li X, Wang S, Wang C, Huang F, Gao Q, et al. Fine particulate air pollution and hospital emergency room visits for respiratory disease in urban areas in Beijing, China, in 2013. PLoS One. 2016;11(4):e0153099. doi: 10.1371/journal.pone.0153099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nasser Z, Salameh P, Nasser W, Abou Abbas, Elias E, Leveque A. Outdoor particulate matter (PM) and associated cardiovascular diseases in the Middle East. Int J Occup Med Environ Health. 2015;28(4):641–61. doi: 10.13075/ijomeh.1896.00186. [DOI] [PubMed] [Google Scholar]
- 3.Daryanoosh SM, Goudarzi G, Omidi Khaniabadi, Armin H, Bassiri H, Omidi Khaniabadi. Effect of Exposure to PM10 on Cardiovascular Diseases Hospitalizations in Ahvaz, Khorramabad and Ilam, Iran During 2014. Iranian Journal of Health, Safety & Environment, 2016;3(1):428–33. [Google Scholar]
- 4.Pope CA, Dockery DW. Health effects of fine particulate air pollution: Lines that connect. J Air Waste Manag Assoc. 2006;56(6):709–42. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- 5.Mohammadi A, Azhdarpoor A, Shahsavani A, Tabatabaee H. Investigating the health effects of exposure to criteria pollutants using airQ2.2.3 in Shiraz, Iran. Aerosol Air Qual Res. 2016;16(4):1035–43. [Google Scholar]
- 6.World Health Organization. Ambient (outdoor) air quality and health [Online]. 2014. Available from: URL: http://www.who.int/mediacentre/factsheets/fs313/en.
- 7.Vahedian M, Khanjani N, Mirzaee M, Koolivand A. Associations of short-term exposure to air pollution with respiratory hospital admissions in Arak, Iran. J Environ Health Sci Eng. 2017;15:17. doi: 10.1186/s40201-017-0277-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rezaei S, Khanjani N, Mohammadi Senjedkooh, Darabi Fard. The effect of air pollution on respiratory disease visits to the emergency department in Kerman, Iran. J Health Dev. 2015;4(4):306–14. [Google Scholar]
- 9.Hoek G, Brunekreef B, Goldbohm S, Fischer P, van den Brandt PA. Association between mortality and indicators of traffic-related air pollution in the Netherlands: A cohort study. Lancet. 2002;360(9341):1203–9. doi: 10.1016/S0140-6736(02)11280-3. [DOI] [PubMed] [Google Scholar]
- 10.Pope CA, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, et al. Cardiovascular mortality and long-term exposure to particulate air pollution: Epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004;109(1):71–7. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- 11.Khanjani N, Ranadeh Kalankesh, Mansouri F. Air pollution and respiratory deaths in Kerman, Iran (from 2006 till 2010). Iran J Epidemiol. 2012;8(3):58–65. [Google Scholar]
- 12.Dadbakhsh M, Khanjani N, Bahrampour A. "Death from respiratory diseases and air pollutants in Shiraz, Iran (2006-2012). Journal of Environment Pollution and Human Health. 2015;3(1):4–11. [Google Scholar]
- 13.Dastoorpoor M, Idani E, Khanjani N, Goudarzi G, Bahrampour A. Relationship between air pollution, weather, traffic, and traffic-related mortality. Trauma Mon. 2016;21(4):e37585. doi: 10.5812/traumamon.37585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hashemi SY, Khanjani N, Soltaninejad Y, Momenzadeh R. Air pollution and cardiovascular mortality in Kerman from 2006 to 2011. American Journal of Cardiovascular Disease Research. 2014;2(2):27–30. [Google Scholar]
- 15.Hoek G, Brunekreef B, Fischer P, van Wijnen J. The association between air pollution and heart failure, arrhythmia, embolism, thrombosis, and other cardiovascular causes of death in a time series study. Epidemiology. 2001;12(3):355–7. doi: 10.1097/00001648-200105000-00017. [DOI] [PubMed] [Google Scholar]
- 16.Kang SH, Heo J, Oh IY, Kim J, Lim WH, Cho Y, et al. Ambient air pollution and out-of-hospital cardiac arrest. Int J Cardiol. 2016;203:1086–92. doi: 10.1016/j.ijcard.2015.11.100. [DOI] [PubMed] [Google Scholar]
- 17.Dadbakhsh M, Khanjani N, Bahrampour A. Death from cardiovascular diseases and air pollution in Shiraz, Iran (March 2006-March 2012). J Epid Prev Med. 2016;2(1):114. [Google Scholar]
- 18.Shah AS, Langrish JP, Nair H, McAllister DA, Hunter AL, Donaldson K, et al. Global association of air pollution and heart failure: A systematic review and meta-analysis. Lancet. 2013;382(9897):1039–48. doi: 10.1016/S0140-6736(13)60898-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma Y, Zhang H, Zhao Y, Zhou J, Yang S, Zheng X, et al. Short-term effects of air pollution on daily hospital admissions for cardiovascular diseases in western China. Environ Sci Pollut Res Int. 2017;24(16):14071–9. doi: 10.1007/s11356-017-8971-z. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. Cardiovascular diseases (CVDs) [Online]. 2016. Available from: URL: http://www.who.int/mediacentre/factsheets/fs317/en.
- 21.Ukehaxhaj A, Gjorgjev D, Ramadani M, Krasniqi S, Gjergji T, Zogaj D. Air pollution in pristina, influence on cardiovascular hospital morbidity. Med Arch. 2013;67(6):438–41. doi: 10.5455/medarh.2013.67.438-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Franchini M, Mannucci PM. Short-term effects of air pollution on cardiovascular diseases: Outcomes and mechanisms. J Thromb Haemost. 2007;5(11):2169–74. doi: 10.1111/j.1538-7836.2007.02750.x. [DOI] [PubMed] [Google Scholar]
- 23.Beelen R, Hoek G, van den, Goldbohm RA, Fischer P, Schouten LJ, et al. Long-term effects of traffic-related air pollution on mortality in a Dutch cohort (NLCS-AIR study). Environ Health Perspect. 2008;116(2):196–202. doi: 10.1289/ehp.10767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tonne C, Melly S, Mittleman M, Coull B, Goldberg R, Schwartz J. A case-control analysis of exposure to traffic and acute myocardial infarction. Environ Health Perspect. 2007;115(1):53–7. doi: 10.1289/ehp.9587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samoli E, Atkinson RW, Analitis A, Fuller GW, Green DC, Mudway I, et al. Associations of short-term exposure to traffic-related air pollution with cardiovascular and respiratory hospital admissions in London, UK. Occup Environ Med. 2016;73(5):300–7. doi: 10.1136/oemed-2015-103136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katsoulis M, Dimakopoulou K, Pedeli X, Trichopoulos D, Gryparis A, Trichopoulou A, et al. Long-term exposure to traffic-related air pollution and cardiovascular health in a Greek cohort study. Sci Total Environ. 2014;490:934–40. doi: 10.1016/j.scitotenv.2014.05.058. [DOI] [PubMed] [Google Scholar]
- 27.Colais P, Serinelli M, Faustini A, Stafoggia M, Randi G, Tessari R, et al. Air pollution and urgent hospital admissions in nine Italian cities. Results of the EpiAir Project. Epidemiol Prev. 2009;33(6 Suppl 1):77–94. [PubMed] [Google Scholar]
- 28.Bell ML, Peng RD, Dominici F, Samet JM. Emergency hospital admissions for cardiovascular diseases and ambient levels of carbon monoxide: Results for 126 United States urban counties, 1999-2005. Circulation. 2009;120(11):949–55. doi: 10.1161/CIRCULATIONAHA.109.851113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nasser Z, Salameh P, Dakik H, Elias E, Abou AL, Leveque A. Outdoor air pollution and cardiovascular diseases in Lebanon: A case-control study. J Environ Public Health. 2015;2015:810846. doi: 10.1155/2015/810846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Waked A, Afif C. Emissions of air pollutants from road transport in Lebanon and other countries in the Middle East region. Atmos Environ. 2012;61:446–52. [Google Scholar]
- 31.Solgi E. Assessment of copper and zinc contamination in soils of industrial estates of Arak region (Iran). Iran J Toxicol. 2015;9(28):1277–83. [Google Scholar]
- 32.Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42(4):1187–95. doi: 10.1093/ije/dyt092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ye X, Peng L, Kan H, Wang W, Geng F, Mu Z, et al. Acute effects of particulate air pollution on the incidence of coronary heart disease in Shanghai, China. PLoS One. 2016;11(3):e0151119. doi: 10.1371/journal.pone.0151119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Phung D, Hien TT, Linh HN, Luong LM, Morawska L, Chu C, et al. Air pollution and risk of respiratory and cardiovascular hospitalizations in the most populous city in Vietnam. Sci Total Environ. 2016;557-558(322):30. doi: 10.1016/j.scitotenv.2016.03.070. [DOI] [PubMed] [Google Scholar]
- 35.Zhang Y, Wang SG, Ma YX, Shang KZ, Cheng YF, Li X, et al. Association between ambient air pollution and hospital emergency admissions for respiratory and cardiovascular diseases in Beijing: A time series study. Biomed Environ Sci. 2015;28(5):352–63. doi: 10.3967/bes2015.049. [DOI] [PubMed] [Google Scholar]
- 36.Mustafic H, Jabre P, Caussin C, Murad MH, Escolano S, Tafflet M, et al. Main air pollutants and myocardial infarction: A systematic review and meta-analysis. JAMA. 2012;307(7):713–21. doi: 10.1001/jama.2012.126. [DOI] [PubMed] [Google Scholar]
- 37.Fung KY, Luginaah I, Gorey KM, Webster G. Air pollution and daily hospitalization rates for cardiovascular and respiratory diseases in London, Ontario. Int J Environ Stud. 2005;62(6):677–85. doi: 10.1080/00207230500367879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shahi AM, Omraninava A, Goli M, Soheilarezoomand HR, Mirzaei N. The Effects of Air Pollution on Cardiovascular and Respiratory Causes of Emergency Admission. Emerg (Tehran) 2014;2(3):107–14. [PMC free article] [PubMed] [Google Scholar]
- 39.Pereira Filho, Pereira LA, Arbex FF, Arbex M, Conceiēćo GM, Santos UP, et al. Effect of air pollution on diabetes and cardiovascular diseases in Sćo Paulo, Brazil. Braz J Med Biol Res. 2008;41(6):526–32. doi: 10.1590/s0100-879x2008005000020. [DOI] [PubMed] [Google Scholar]
- 40.Martins LC, Pereira LA, Lin CA, Santos UP, Prioli G, Luiz OC, et al. The effects of air pollution on cardiovascular diseases: Lag structures. Rev Saude Publica. 2006;40(4):677–83. doi: 10.1590/s0034-89102006000500018. [DOI] [PubMed] [Google Scholar]
- 41.Milojevic A, Wilkinson P, Armstrong B, Bhaskaran K, Smeeth L, Hajat S. Short-term effects of air pollution on a range of cardiovascular events in England and Wales: Case-crossover analysis of the MINAP database, hospital admissions and mortality. Heart. 2014;100(14):1093–8. doi: 10.1136/heartjnl-2013-304963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jevtic M, Dragic N, Bijelovic S, Popovic M. Cardiovascular diseases and air pollution in Novi Sad, Serbia. Int J Occup Med Environ Health. 2014;27(2):153–64. doi: 10.2478/s13382-014-0239-y. [DOI] [PubMed] [Google Scholar]
- 43.Chang CC, Tsai SS, Ho SC, Yang CY. Air pollution and hospital admissions for cardiovascular disease in Taipei, Taiwan. Environ Res. 2005;98(1):114–9. doi: 10.1016/j.envres.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 44.Hashemi SY, Khanjani N. Air Pollution and Cardiovascular Hospital Admissions in Kerman, Iran. J Heart Cardiol. 2016;2(2):1–6. [Google Scholar]
- 45.Xie J, He M, Zhu W. Acute effects of outdoor air pollution on emergency department visits due to five clinical subtypes of coronary heart diseases in shanghai, china. J Epidemiol. 2014;24(6):452–9. doi: 10.2188/jea.JE20140044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tong L, Li K, Zhou Q. Promoted relationship of cardiovascular morbidity with air pollutants in a typical Chinese urban area. PLoS One. 2014;9(9):e108076. doi: 10.1371/journal.pone.0108076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leem JH, Kim ST, Kim HC. Public-health impact of outdoor air pollution for 2(nd) air pollution management policy in Seoul metropolitan area, Korea. Ann Occup Environ Med. 2015;27:7. doi: 10.1186/s40557-015-0058-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Willocks LJ, Bhaskar A, Ramsay CN, Lee D, Brewster DH, Fischbacher CM, et al. Cardiovascular disease and air pollution in Scotland: No association or insufficient data and study design? BMC Public Health. 2012;12:227. doi: 10.1186/1471-2458-12-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dominici F, McDermott A, Daniels M, Zeger SL, Samet JM. Revised analyses of the National Morbidity, Mortality, and Air Pollution Study: Mortality among residents of 90 cities. J Toxicol Environ Health A. 2005;68(13-14):1071–92. doi: 10.1080/15287390590935932. [DOI] [PubMed] [Google Scholar]
- 50.Zanobetti A, Franklin M, Koutrakis P, Schwartz J. Fine particulate air pollution and its components in association with cause-specific emergency admissions. Environ Health. 2009;8:58. doi: 10.1186/1476-069X-8-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jalaludin B, Morgan G, Lincoln D, Sheppeard V, Simpson R, Corbett S. Associations between ambient air pollution and daily emergency department attendances for cardiovascular disease in the elderly (65+ years), Sydney, Australia. J Expo Sci Environ Epidemiol. 2006;16(3):225–37. doi: 10.1038/sj.jea.7500451. [DOI] [PubMed] [Google Scholar]