Abstract
Objective
To examine disparities in disease prevalence related to age and race/ethnicity.
Study design
Retrospective observational study.
Methods
Eligible population included enrollees with largest insurer in Hawai‘i. Chronic diseases were identified from claims data (1999–2009) based on algorithms including diagnostic codes and pharmaceutical utilization. Relative risk of heart disease and its risk factors were calculated for Native Hawaiians and Asian sub-groups by age.
Results
Prevalence of heart disease and its risk factors differed substantially by age and race/ethnicity. Native Hawaiians and Filipinos had higher rates of hypertension and diabetes; Asians had highest rates of hyperlipidemia. Whites had the lowest prevalence of risk factors yet their risk of heart disease equaled other groups.
Conclusion
Prevalence curves began diverging at age 30 for risk factors and age 40 for heart disease. This suggests approaches to reduce the burden of disease for vulnerable groups need to begin in early adulthood if not sooner.
Keywords: Ethnic disparities, Native Hawaiian health, cardiovsascular disease, diabetes
Heart disease is the leading cause of death for all people in the United States, including Asians and Pacific Islanders (APIs). Risk factors include hyperlipidemia, hypertension, and diabetes mellitus. Although the number of APIs is increasing at the rapid rate of 4.5% per year, APIs’ health status remains under-explored.1 Historically, because APIs have been treated as one homogeneous group, with ethnicities as diverse as Native Hawaiians, Japanese, Chinese, Koreans, and Filipinos included in the API category, few ethnicity-specific data exist.2–4 The scant evidence that is available suggests large health disparities among API subgroups that are often masked by API group averages.5
Self-reported data from the Hawai‘i State Behavioral Risk Factor Surveillance Survey (BRFSS) reveal some of these health disparities within API subgroups.5 Forty-six percent of Japanese report being told they have high cholesterol compared with 37% of Whites, 36% of Filipinos, and 38% of Native Hawaiians. Only 5% of Whites report being told they have diabetes compared with 13% of Native Hawaiians, and 10% of Filipinos and Japanese. Similarly, 37% of Japanese have been told they have hypertension compared with 26% of Whites, 31% of Filipinos, and 36% of Native Hawaiians.
This study focuses on heart disease and three of its risk factors, hyperlipidemia, hypertension, and diabetes mellitus. Using administrative data from a large health plan in Hawai‘i, the goal was to examine how the prevalence of these conditions relates to age for Asian APIs (including Native Hawaiians, Japanese, Filipinos, Chinese, and Koreans) and Whites and to determine the extent of health disparities between groups.
The advantage of this approach is that it is based upon patient diagnoses submitted on medical claims rather than self-reported survey responses and contains information from a large study population. The large sample allows us to graph prevalence of condition by member age and examine whether racial and ethnic differences in prevalence are statistically significant.
Methods
The eligible population was selected from members enrolled with the largest insurer in Hawai‘i, which covers approximately half the population of Hawai‘i, in private business or through a Medicare cost contract. Private business includes state employees and retirees. Data on ethnicity were available from annual membership surveys conducted between 2002 and 2009. Each year, samples of approximately 100,000 members were surveyed with response rates in the range of 40–50%. The survey asked people to check all ethnicities that applied to them from a list of 14 categories. These categories were consistent with those the Hawai‘i State Department of Health uses in their health status surveys. Seventy-six percent of the respondents selected only one ethnicity. Members who selected more than one ethnicity were classified as “mixed race or ethnicity” and excluded from this study. The one exception was Native Hawaiians. In keeping with the approach used by Hawai‘i State Department of Health, we categorized as Hawaiian anyone who checked Hawaiian even if they checked more than one ethnicity. For instance, if someone checked Native Hawaiian and Japanese, they would be categorized as Native Hawaiian. This type of classification is common in research studies in Hawai‘i as there are so few people who are 100% Hawaiian.6
Our ethnic categories for this study included the six largest groups: Hawaiian/Part Hawaiian; Filipino; Japanese; Chinese; Korean; White. The only other eligibility criteria were enrollment with the insurer between 2002 and 2009 and being between ages 18 and 84.
Chronic diseases were identified from claims data that were available from 1999 through 2009. Patients with diabetes and heart disease, or both, were identified by algorithms used in disease management programs. Presence of diabetes and heart disease were confirmed whenever possible through contact with members and their physicians. A physician confirmation was required to exclude possible false positives. A diagnosis of either coronary artery disease or congestive heart failure was taken as evidence of heart disease. To identify hypertension and hyperlipidemia, algorithms were run quarterly examining claims in the past 12 months. Two claims with the respective diagnosis or one claim with the diagnosis and a prescription for a treatment medication were required for a member to be classified as having hypertension or hyperlipidemia. For all four chronic conditions, people were considered to have the condition from the first date they met the criteria for the condition, and assumed to have the condition from that date onward.
Prevalence was calculated by one-year age intervals. The days enrolled during an age for the entire eligible population was taken as the denominator. Members could contribute partial years of enrollment during an age if not enrolled for the full 12 months when they were that age. Numerators were calculated as the days enrolled while having a condition. In the age when they were first diagnosed patients contributed days of enrollment to the numerator for the condition from the date of first diagnosis until their next birthday. Using the Cochran-Mantel-Haenszel procedure, we calculated relative risks and confidence intervals for the prevalence of heart disease and its risk factors, relative to Whites. We analyzed the data using Statistical Analysis System (SAS) software package, version 9.1 (SAS Inc., Cary, NC).
Results
In our study, as is common in Hawai‘i, no one ethnic or racial group were in the majority. Forty percent of patients in the study were Japanese (n = 58,450), 22% were White (n = 31,569), 15% were Native Hawaiian (n = 22,373), 14% were Filipino (n = 19,914), 7% were Chinese (n = 10,924), and 2% were Korean (n = 2,853).
Mean age for people with heart disease was 69, for diabetes was 63, for hypertension was 61 and for hyperlipidemia was 59 (Table 1). Approximately 41% of patients with heart disease were female, compared with over 50% of people with diabetes, hypertension, and hyperlipidemia. A majority of patients with the conditions examined were Japanese. While Whites constituted only 14% of patients with diabetes, they accounted for 19 to 21% of patients with other conditions. Native Hawaiians accounted for 14% of patients with hyperlipidemia but over 18% of patients with diabetes. Chinese constituted between 9 and 10% and Koreans for approximately 2% of patients with heart disease and its risk factors.
Table 1.
CHARACTERISTICS OF THE STUDY POPULATION BY CONDITION
| Hyperlipidemia | Hypertension | Diabetes | Heart Disease | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Characteristic | Number | Mean ± SD or Percent |
Number | Mean ± SD or Percent |
Number | Mean ± SD or Percent |
Number | Mean ± SD or Percent |
| Age | 101,143 | 58.5 ± 13.5 | 88,780 | 60.4 ± 13.4 | 27,043 | 61.9 ± 12.8 | 21,074 | 67.9 ± 11.0 |
| Gender | ||||||||
| Female | 58,323 | 57.66 | 49,861 | 56.16 | 14,215 | 52.56 | 8,787 | 41.70 |
| Male | 42,820 | 42.34 | 38,919 | 43.84 | 12,828 | 47.44 | 12,287 | 58.30 |
| Ethnicity | ||||||||
| Caucasian | 18,134 | 17.93 | 14,366 | 16.18 | 2,934 | 10.85 | 3,642 | 17.28 |
| Chinese | 7,988 | 7.90 | 6,515 | 7.34 | 2,031 | 7.51 | 1,746 | 8.29 |
| Filipino | 13,444 | 13.29 | 12,484 | 14.06 | 4,205 | 15.55 | 2,368 | 11.24 |
| Hawaiian | 14,203 | 14.04 | 13,713 | 15.45 | 5,014 | 18.54 | 3,646 | 17.30 |
| Japanese | 45,269 | 44.76 | 40,150 | 45.22 | 12,361 | 45.71 | 9,296 | 44.11 |
| Korean | 2,105 | 2.08 | 1,552 | 1.75 | 498 | 1.84 | 376 | 1.78 |
Not surprisingly, the prevalence of heart disease and its risk factors increased with age for all racial and ethnic groups; however, the rate of increase differed according to ethnic group and risk factor or disease state.
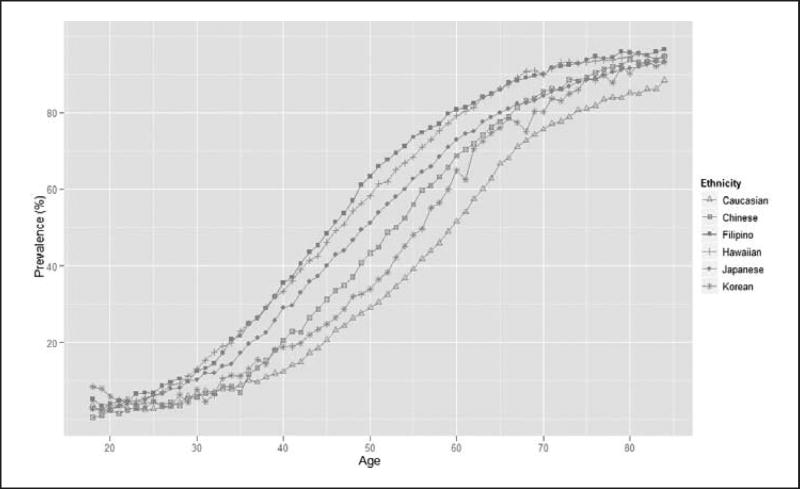
For hypertension, Filipinos tended to have the highest rates, particularly between the ages of 40 and 60, and Native Hawaiians had the second highest prevalence (Figure 1). Consistently across all age levels, Whites were least likely to have hypertension. At age 40, the prevalence of hypertension in Filipinos was approximately 40%, compared with 15% for Whites. For other groups, there appeared to be distinct, roughly parallel curves, with Japanese having the next highest rates, followed by Chinese and Koreans.
Figure 1.
Prevalence of hypertension related to age and ethnicity.
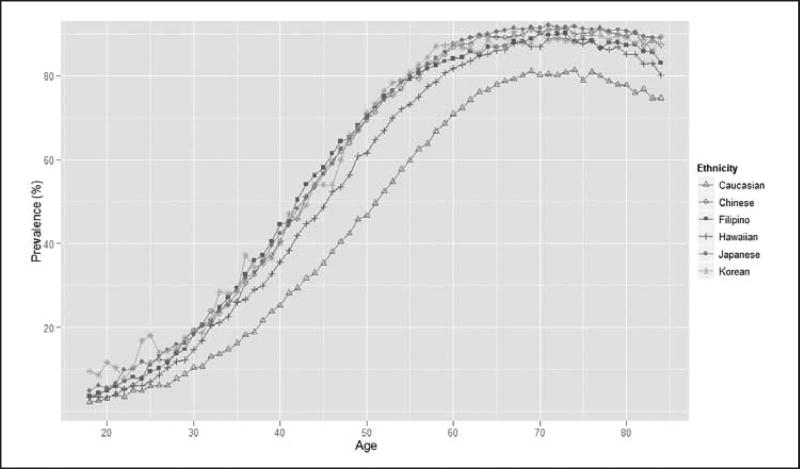
Similarly, the prevalence of hyperlipidemia for Whites was lower than that of all APIs (Figure 2). Rates for the three Asian groups were higher, and started to diverge among patients as young as 25 years of age. At age 40, the prevalence of hyperlipidemia for the three Asian sub-groups was approximately 45% compared with less than 25% for Whites. In contrast to results for hypertension, Native Hawaiians had the second lowest prevalence of hyperlipidemia.
Figure 2.
Prevalence of hyperlipidemia related to age and ethnicity.
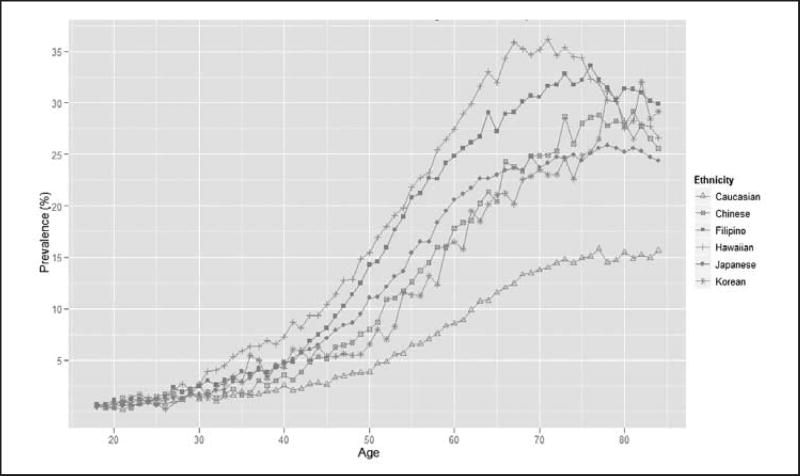
Whites also had the lowest prevalence of diabetes, and the disparities increased with age (Figure 3). Native Hawaiians had the highest prevalence of diabetes followed by Filipinos. At age 65, the prevalence of diabetes among Whites was about one third of that of Native Hawaiians (approximately 10% and 30%, respectively). Rates for Asians were in between those of Native Hawaiians and Whites.
Figure 3.
Prevalence of diabetes related to age and ethnicity.
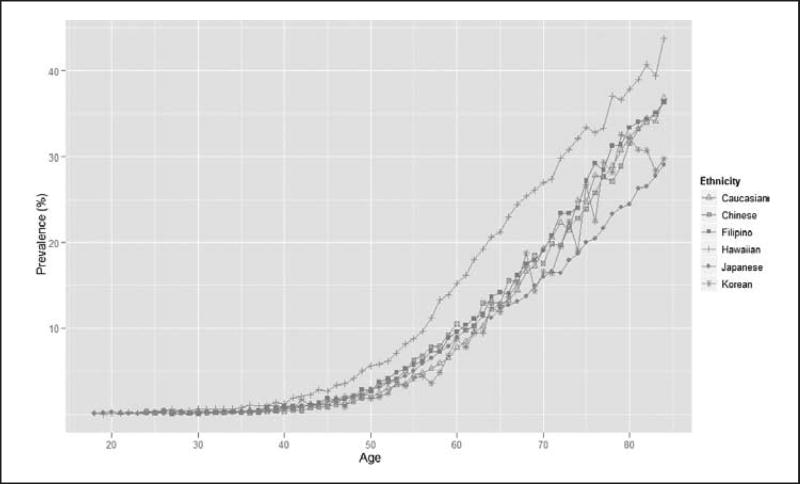
Beginning at age 45, the prevalence curve for heart disease for Native Hawaiians began to separate from those of other groups (Figure 4). By age 65, prevalence of heart disease for Native Hawaiians was 6 to 10 percentage points higher than that of other groups. Prior to age 65, rate of heart disease of Japanese was similar to that of other Asians and Whites; however, elderly Japanese had lowest rates of heart disease.
Figure 4.
Prevalence of heart disease related to age and ethnicity.
For Native Hawaiians, relative risks of having heart disease and its risk factors were all statistically significant relative to Whites (Table 2). Largest relative risks were found for diabetes and suggested that middle aged Native Hawaiians were more than three times as likely to have diabetes as Whites of similar age.
Table 2.
RELATIVE RISK OF CONDITION ACCORDING TO AGE AND ETHNICITY COMPARED TO CAUCASIANS
| Native Hawaiian | Japanese | Chinese | Filipino | Korean | ||
|---|---|---|---|---|---|---|
|
|
|
|
|
|
||
| Condition A | Age | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) |
| Hypertension | 18–34 | 1.95 (1.81, 2.10) | 1.54 (1.53, 1.55) | 0.96 (0.85, 1.08) | 2.14 (1.99, 2.31) | 1.26 (1.05, 1.51) |
| 35–49 | 2.15 (2.11, 2.20) | 1.90 (1.87, 1.94) | 1.42 (1.37, 1.46) | 2.23 (2.18, 2.27) | 1.22 (1.15, 1.29) | |
| 50–64 | 1.56 (1.55, 1.58) | 1.45 (1.44, 1.46) | 1.34 (1.33, 1.35) | 1.62 (1.61, 1.63) | 1.21 (1.18, 1.23) | |
| 65–85 | 1.14 (1.13, 1.15) | 1.09 (1.09, 1.10) | 1.11 (1.10, 1.11) | 1.15 (1.14, 1.15) | 1.08 (1.06, 1.09) | |
| Hyperlipidemia | 18–34 | 1.30 (1.23, 1.38) | 1.37 (1.37, 1.38) | 1.71 (1.58, 1.85) | 1.73 (1.63, 1.83) | 2.00 (1.78, 2.24) |
| 35–49 | 1.31 (1.29, 1.33) | 1.57 (1.55, 1.59) | 1.54 (1.51, 1.57) | 1.56 (1.53, 1.58) | 1.54 (1.49, 1.58) | |
| 50–64 | 1.18 (1.17, 1.19) | 1.28 (1.28, 1.29) | 1.26 (1.25, 1.27) | 1.25 (1.24, 1.25) | 1.27 (1.26, 1.28) | |
| 65–85 | 1.10 (1.09, 1.11) | 1.15 (1.15, 1.16) | 1.14 (1.13, 1.15) | 1.12 (1.11, 1.13) | 1.13 (1.11, 1.14) | |
| Diabetes | 18–34 | 2.13 (1.82, 2.49) | 2.38 (2.35, 2.42) | 1.27 (1.00, 1.62) | 1.87 (1.59, 2.21) | 1.61 (1.09, 2.37) |
| 35–49 | 3.41 (3.22, 3.60) | 2.31 (2.19, 2.44) | 1.71 (1.58, 1.85) | 2.51 (2.36, 2.66) | 1.87 (1.65, 2.12) | |
| 50–64 | 3.20 (3.13, 3.28) | 2.34 (2.29, 2.39) | 2.04 (1.97, 2.10) | 2.90 (2.83, 2.97) | 1.82 (1.73, 1.92) | |
| 65–85 | 2.20 (2.14, 2.27) | 1.69 (1.65, 1.74) | 1.85 (1.79, 1.91) | 2.14 (2.08, 2.21) | 1.78 (1.69, 1.88) | |
| Heart Disease | 18–34 | 1.70 (1.17, 2.46) | 1.31 (1.29, 1.33) | 0.95 (0.49, 1.83) | 0.75 (0.46, 1.24) | NA |
| 35–49 | 1.89 (1.73, 2.07) | 0.93 (0.84, 1.02) | 0.62 (0.52, 0.74) | 0.95 (0.85, 1.06) | 0.93 (0.72, 1.20) | |
| 50–64 | 1.92 (1.87, 1.98) | 1.17 (1.14, 1.20) | 1.28 (1.23, 1.33) | 1.27 (1.23, 1.32) | 1.02 (0.94, 1.10) | |
| 65–85 | 1.23 (1.20, 1.26) | 0.81 (0.79, 0.82) | 0.99 (0.97, 1.02) | 1.01 (0.98, 1.04) | 0.93 (0.88, 0.98) |
CI = Confidence Interval
For both Japanese and Filipinos, the likelihood of having conditions was higher than for Whites except for heart disease (Table 2). For patients aged 35–49, differences in the prevalence of heart disease for both Japanese and Filipino patients were not statistically significant from Whites. For elderly Japanese, relative risk of heart disease compared with Whites was significantly less than 1 [RR = 0.81 (0.79, 0.82)].
Compared with Whites, Chinese patients were significantly more likely to have hypertension, hyperlipidemia, and diabetes (Table 2). The one exception was for hypertension for which the relative risk for Chinese younger than 35 years did not differ from Whites. Heart disease results were mixed. For two age groups (younger than 35 and older than 64), prevalence of heart disease did not differ between Chinese and Whites. For people aged 35–49, Chinese patients were less likely to have heart disease [RR = 0.62 (0.52, 0.74)], while for people aged 50–64, they were more likely to have heart disease [RR = 1.28 (1.23, 1.33)].
Compared with Whites, Korean patients were also significantly more likely to have one of the three risk factors for heart disease: hypertension, hyperlipidemia, and diabetes (Table 2); however, the only significant difference in the prevalence of heart disease was for patients over age 64 [RR = 0.93 (0.88, 0.98)] and their rate was unexpectedly lower than that of Whites.
Discussion
In our observational study of more than 146,000 health plan members in Hawai‘i, we found that the relationship between age and the prevalence of chronic conditions differed substantially according to race and ethnicity as well as the condition being examined. Whites had the lowest prevalence of the three risk factors examined: hypertension, hyperlipidemia, and diabetes. Native Hawaiians consistently had among the highest rates of heart disease and its risk factors. While disparities in disease prevalence among APIs have been documented in prior studies,7–23 our research went beyond previous work in examining how the prevalence changed with age for a number of API, including Native Hawaiians, Filipinos, Chinese, Japanese, and Koreans.
Prevalence rates from our studied differed from those obtained from the BFRSS for hyperlipidemia and hypertension. Data from BRFSS show Japanese as more likely to have hypertension than Filipinos and as likely as Native Hawaiians. In our study, Native Hawaiians and Filipinos were more likely to have hypertension than Japanese. Moreover while in the BRFSS Japanese had considerably higher rates of hyperlipidemia than other subgroups, in our study, the Asian subgroups had similar rates of this condition. Differences in methodology, in terms of data source (self-reported vs. administrative data) and sample (population vs. enrollees in a health plan), might explain this disparity; however, further research is needed to determine which more accurately reflects the true prevalence rates in the community.
Our study highlights the importance of examining prevalence rates of disease and risk factors separately for API sub-groups and reveals the extent to which health disparities emerge at an early age. By age 30, Asian Americans and Pacific Islanders had a higher prevalence of hyperlipidemia than Whites. By age 35, Filipinos, Native Hawaiians, Japanese, and Koreans had higher rates of hypertension than Whites. By age 40, Native Hawaiians were at higher risk for diabetes and by age 50, they were at higher risk for heart disease than other groups. Hence, while the Centers for Medicare and Medicaid Services (CMS) are spurring efforts to improve the quality of care in order to reduce the burden of disease in the elderly, our study suggests that efforts to lessen disparities need to start at a younger age.24
For Asian and White groups, the expected relationship between risk factors and prevalence of heart disease was not evident. While Filipinos had the highest rates of hypertension and hyperlipidemia, along with rates of diabetes only slightly lower than Native Hawaiians, the rate of heart disease in Filipinos was much lower than that of Native Hawaiians and similar to that of other Asians who were much less likely to have diabetes, hypertension, and hyperlipidemia. Similarly, while Whites had considerably lower rates of all risk factors, their prevalence of heart disease was similar to that of Asians who seemed to be at higher risk based on the risk factors we examined. Hence, these descriptive data raise several interesting questions. Why do Whites have the lowest risk of hyperlipidemia, hypertension, and diabetes, but comparable risk of heart disease? How is it that Japanese Americans have the highest prevalence of hyperlipidemia but the lowest rate of heart disease, particularly among the elderly? To what extent do these differences result from receiving appropriate evidence-based care and coherent treatment? Some evidence suggests there is greater adherence by Japanese Americans to recommended treatment guidelines, but further research is needed.25,26
There are several limitations to our study. First, data are from a single large health plan in Hawai‘i and may not be generalizable to other areas or to uninsured or Medicaid populations. We know from the BRFSS that Filipinos are less likely to have insurance than Whites (90.9% vs. 94.2%, respectively).6 Hence, they are less likely to be represented in our study. If rates of heart disease are higher among the uninsured than the insured population, our results might underestimate the prevalence of disease in Filipinos living in Hawai‘i. Second, race/ethnicity information was only available for a subset of the population who had filled out a member satisfaction survey. Third, our information on health conditions came from administrative claims data. There may be people who have a diagnosis in claims that really do not have the disease as well as people who have the disease who do not have a diagnosis in the claims (i.e. false positives as well as false negatives). Additionally, we were not able to adjust for obesity and socioeconomic status.
The main goal of this study was to examine and document disparities in the prevalence of heart disease and its risk factors among APIs. Subsequent studies are needed to better understand and interpret these results. We agree with the assessment by the National Heart, Lung, And Blood Institute Workshop on heterogeneity in cardiometabolic risk in Asian Americans as to the need for further research in this area. We need to better understand whether these differences stem from genetics, lifestyle choices, system factors, or environmental influences.
Specific programs may need to target the most vulnerable groups and these groups may differ by condition or risk factor. To promote cardiovascular health among APIs, the National Heart, Lung, and Blood Institute (NHLBI) has launched the ASPIRE for Healthy Hearts Project.19 Findings from the ASPIRE project suggest that a family-based approach to health promotion is an important component of effective outreach strategies for APIs. Moreover, the approach needs to be culturally appropriate and to take into account the level of acculturation.27–31 Furthermore, as seen in other populations, there may also be issues with health literacy and access to care that need to be addressed.32
Acknowledgments
This study was funded by the Hawai‘i Medical Service Association.
Contributor Information
Deborah T. Juarez, University of Hawaii College of Pharmacy.
James W. Davis, Clinical Research Center.
S. Kalani Brady, Departments of Native Hawaiian Health.
Richard S. Chung, John A. Burns School of Medicine at the University of Hawai‘i, Honolulu, Hawai‘i, and APS Healthcare.
Notes
- 1.Lin-Fu J. Asian and Pacific Islander Americans: an overview of demographic characteristics and health care issues. Asian Am Pac Isl J Health. 1993 Summer;1(1):20–36. [PubMed] [Google Scholar]
- 2.Tamir A, Cachola S. Hypertension and other cardiovascular risk factors. In: Zane NWS, Takeuchi DT, Young KNJ, editors. Confronting critical health issues of Asian and Pacific Islander Americans. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- 3.Hong B, Bayat N. National Asian American and Pacific Islander cardiovascular health action plan: eliminating racial and ethnic disparities in cardiovascular health. Washington, DC: Health Resources and Services Administration; 2011. [Google Scholar]
- 4.Srinivasan S, Guillermo T. Toward improved health: disaggregating Asian American and Native Hawaiian/Pacific Islander data. Am J Public Health. 2000 Nov;90(11):1731–4. doi: 10.2105/ajph.90.11.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naravan KM, Aviles-Santa L, Oza-Frank R, et al. Report of a National Heart, Lung, and Blood Institute Workshop: heterogeneity in cardiometabolic risk in Asian Americans in the U.S. Opportunities for research. J Am Coll Cardiol. 2010 Mar 9;55(10):966–73. doi: 10.1016/j.jacc.2009.07.075. [DOI] [PubMed] [Google Scholar]
- 6.State of Hawai‘i Department of Health. Hawai‘i behavioral risk factor surveillance system. Honolulu, HI: State of Hawai‘i Department of Health; 2010. [Google Scholar]
- 7.Steinbrecher A, Morimoto Y, Heak S, et al. The preventable proportion of type 2 diabetes by ethnicity: the multiethnic cohort. Ann Epidemiol. 2011 Jul;21(7):526–35. doi: 10.1016/j.annepidem.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grandinetti A, Kaholokula JK, Theriault AG, et al. Prevalence of diabetes and glucose intolerance in an ethnically diverse rural community of Hawai‘i. Ethn Dis. 2007 Spring;17(2):250–5. [PubMed] [Google Scholar]
- 9.Grandinetti A, Chang HK, Mau MK, et al. Prevalence of glucose intolerance among Native Hawaiians in two rural communities. Native Hawaiian Health Research (NHHR) Project. Diabetes Care. 1998 Apr;21(4):549–54. doi: 10.2337/diacare.21.4.549. [DOI] [PubMed] [Google Scholar]
- 10.Maskarinec G, Grandinetti A, Matsuura G, et al. Diabetes prevalence and body mass index differ by ethnicity: the multiethnic cohort. Ethn Dis. 2009 Winter;19(1):49–55. [PMC free article] [PubMed] [Google Scholar]
- 11.Kim HS, Park SY, Grandinetti A, et al. Major dietary patterns, ethnicity, and prevalence of type 2 diabetes in rural Hawai‘i. Nutrition. 2008 Nov-Dec;24(11–12):1065–72. doi: 10.1016/j.nut.2008.05.008. Epub 2008 Jun 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mau MK, Grandinetti A, Arakaki R, et al. Insulin resistance syndrome in Native Hawaiians. Diabetes Care. 1997 Sep;20(9):1376–80. doi: 10.2337/diacare.20.9.1376. [DOI] [PubMed] [Google Scholar]
- 13.Patrick SL, Kadohiro JK, Waxman SH, et al. IDDM incidence in a multiracial population. The Hawai‘i IDDM Registry, 1980–1990. Diabetes Care. 1997 Jun;20(6):983–7. doi: 10.2337/diacare.20.6.983. [DOI] [PubMed] [Google Scholar]
- 14.Klatsky A, Armstrong MA. Cardiovascular risk factors among Asian Americans living in northern California. Am J Public Health. 1991 Nov;81(11):1423–8. doi: 10.2105/ajph.81.11.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curb JD, Aluli NE, Kautz JA, et al. Cardiovascular risk factor levels in ethnic Hawaiians. Am J Public Health. 1991 Feb;81(2):164–7. doi: 10.2105/ajph.81.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braun KL, Look MA, Tsark JA. High mortality rates in Native Hawaiians. Hawaii Med J. 1995 Sep;54(9):723–9. [PubMed] [Google Scholar]
- 17.Palaniappan L, Wang Y, Fortmann SP. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol. 2004 Aug;14(7):499–506. doi: 10.1016/j.annepidem.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 18.Curb JD, Aluli NE, Huang BJ, et al. Hypertension in elderly Japanese Americans and adult Native Hawaiians. Public Health Rep. 1996;111(Suppl 2):53–5. [PMC free article] [PubMed] [Google Scholar]
- 19.National Institutes of Health. Addressing cardiovascular health in Asian Americans and Pacific Islanders—a background report. Bethesda, MD: National Institutes of Health; 2000. (Publication no. 00-3647) [Google Scholar]
- 20.Novotny R, Davis J, Ross P, et al. Adiposity and blood pressure in a multiethnic population of women in Hawaii. Ethn Health. 1998 Aug;3(3):167–73. doi: 10.1080/13557858.1998.9961859. [DOI] [PubMed] [Google Scholar]
- 21.Stavig GR, Igra A, Leonard AR. Hypertension among Asians and Pacific Islanders in California. Am J Epidemiol. 1984 May;119(5):677–91. doi: 10.1093/oxfordjournals.aje.a113789. [DOI] [PubMed] [Google Scholar]
- 22.Angel A, Armstrong MA, Klatsky AL. Blood pressure among Asian Americans living in northern California. Am J Cardiol. 1989 Jul 15;64(3):237–40. doi: 10.1016/0002-9149(89)90468-2. [DOI] [PubMed] [Google Scholar]
- 23.Heiss G, Tamir I, Davis CE, et al. Lipoprotein-cholesterol distributions in selected North American population: the lipid research clinics program prevalence study. Circulation. 1980 Feb;61(2):302–15. doi: 10.1161/01.cir.61.2.302. [DOI] [PubMed] [Google Scholar]
- 24.Iglehart JK. Linking compensation to quality—Medicare payments to physicians. N Engl J Med. 2005 Sep 1;353(9):870–2. doi: 10.1056/NEJMp058194. [DOI] [PubMed] [Google Scholar]
- 25.Taira DA, Gelber RP, Davis J, et al. Antihypertensive adherence and drug class among Asian Pacific Americans. Ethn Health. 2007 Jun;12(3):265–81. doi: 10.1080/13557850701234955. [DOI] [PubMed] [Google Scholar]
- 26.Lee R, Taira DA. Adherence to oral hypoglycemic agents in Hawaii. Prev Chronic Dis. 2005 Apr;2(2):A09. Epub 2005 Mar 15. [PMC free article] [PubMed] [Google Scholar]
- 27.Mokuau N, Hughes CK, Tsark JU. Heart disease and associated risk factors among Hawaiians: culturally responsive strategies. Health Soc Work. 1995 Feb;20(1):46–51. doi: 10.1093/hsw/20.1.46. [DOI] [PubMed] [Google Scholar]
- 28.Huang B, Rodriguez BL, Burchfiel CM, et al. Acculturation and prevalence of diabetes among Japanese-American men in Hawaii. Am J Epidemiol. 1996 Oct 1;144(7):674–81. doi: 10.1093/oxfordjournals.aje.a008980. [DOI] [PubMed] [Google Scholar]
- 29.Marmot MG, Syme SL. Acculturation and coronary heart disease in Japanese Americans. Am J Epidemiol. 1976 Sep;104(3):225–47. doi: 10.1093/oxfordjournals.aje.a112296. [DOI] [PubMed] [Google Scholar]
- 30.Kaholokula JK, Nacapoy AH, Grandinetti A, et al. Association between acculturation modes and type 2 diabetes among Native Hawaiians. Diabetes Care. 2008 Apr;31(4):698–700. doi: 10.2337/dc07-1560. [DOI] [PubMed] [Google Scholar]
- 31.Chun KM, Chesla CA, Kwan CM. “So we adapt step by step”: acculturation experiences affecting diabetes management and perceived health for Chinese American immigrants. Soc Sci Med. 2011 Jan;72(2):256–64. doi: 10.1016/j.socscimed.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liao Y, Bang D, Cosgrove S, et al. Surveillance of health status in minority communities—Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. MMWR Surveill Summ. 2011 May 20;60(6):1–44. [PubMed] [Google Scholar]