Abstract
Background
Adverse childhood experiences (ACEs) are associated with adult high-risk behaviors and diseases. There is value in screening parents for ACEs given the repercussions parental ACEs may have on parenting behaviors and child development. The primary aim of this study was to assess the feasibility of parental ACE screening in the home setting. A secondary aim was to evaluate whether or not maternal ACEs correlated with maternal mental health measures.
Methods
Two home visiting programs that support early childhood development and conduct parental mental health screening implemented ACE screening for parents of infants < 1 year of age. Descriptive statistics were produced for population surveillance of ACEs as well as standard-practice screens for depression, anxiety, substance use, and intimate partner violence. Logistic models were used to examine associations between ACE score and mental health measures.
Results
A total of 110 parents completed the ACE screen. All possible ACE score outcomes were represented (0–10). A trend toward association of positive prenatal maternal depression screen with ACE score was identified (p=0.05).
Conclusion
This novel prospective home-based screening program for parental ACEs was feasible and identified a trend toward increasing ACE score association with positive prenatal maternal depression screen.
Keywords: public health nursing practice, community-based nursing, adverse childhood experiences, advocacy, infant health, parent-child relationship, mental health, screening
Background
Adverse childhood experiences (ACEs) are traumatic events in an individual’s childhood such as physical, sexual, or emotional abuse, physical or emotional neglect, domestic violence, family separation, and family member substance use, mental illness, or incarceration. ACEs were first described in 1998 by Drs. Felitti and Anda, who found that stress related to ACEs had both short- and long-term health effects (Felitti et al., 1998).
Higher numbers of ACEs (i.e., higher “ACE scores”) are associated with increased likelihood of high-risk behaviors such as alcoholism, smoking, and increased number of sexual partners, as well as adult-onset diseases such as ischemic heart disease, chronic lung disease, and even cancer (Felitti et al., 1998). Disease relationships hold true after controlling for high-risk behaviors. Associations have also been found between childhood ACE scores and prevalence of physical, mental, and developmental health conditions between the ages of 0–17 years (Bright, Knapp, Hinojosa, Alford, & Bonner, 2016).
There is value in screening parents of young children for ACEs given the repercussions parental ACEs may have on parenting behaviors and child development (Szilagyi et al., 2016). When an adult experiences negative childhood events and later becomes a parent, their parenting style is likely to be affected by their past experiences. For example, they may copy the behaviors they observed in their own parents, such as physical, emotional, or sexual abuse (Chung et al., 2009; Narayan et al., 2017), thereby depriving their children of the safe, stimulating, and nurturing environment needed for optimal childhood growth and development (Suess & Sroufe, 2005). Alternatively, a parent with a high ACE score may experience health-related sequelae of childhood ACEs such as depression, heart disease, lung disease, or cancer (Cuijpers, Weitz, Karyotaki, Garber, & Andersson, 2015; Morris, Martini, & Preen, 2016), which may present a barrier to their ability to provide for their child either emotionally or physically. Child development and child-caregiver attachment proceeds rapidly in the first year of life (Adams & Cotgrove, 1995). Thus, being able to screen and refer families within this time period is crucial. One potential method to screen and intervene is to have home visiting professionals complete parental ACE screening. Home visitors already have relationships established with families and often complete other screening questionnaires in the home setting.
In addition to having potential repercussions on parenting behavior and child development, exposure to ACEs may affect maternal mental health. The relationship between ACEs and adult depression, anxiety, and substance use is well-documented (Choi, DiNitto, Marti, & Choi, 2016; Felitti et al., 1998). These studies, however, involved a majority of adults over the age of 50 and included both men and women. If pregnant and postpartum mothers demonstrate similar mental health sequelae of ACEs, this could impact the ACE score of the child and thereby predispose him or her to poorer health outcomes (Cuijpers et al., 2015; Felitti et al., 1998). Prenatal depression is also associated with adverse child outcomes (Accortt, Cheadle, & Dunkel Schetter, 2015; Davalos, Yadon, & Tregellas, 2012), and is not accounted for in the ACE score of the child.
Less is known about the relationship between ACEs and intimate partner violence (IPV), but it is thought that post-traumatic stress disorder, depression, and substance abuse play a role in connecting the two (Brown, Perera, Masho, Mezuk, & Cohen, 2015; Dennis & Vigod, 2013). IPV affects between 1.5–4 million U.S. women each year, and prevalence rates range between 1–38% depending on how IPV is defined and the population studied (Bailey, 2010; Sprague et al., 2014). Child health is disadvantaged from the beginning in these cases, as the risk for preterm birth and low birth weight are increased (Donovan, Spracklen, Schweizer, Ryckman, & Saftlas, 2016), and the child may become a witness to or even a victim of violence thereafter.
The primary aim of this study was to assess the feasibility of implementing ACE screening of parents using home visiting professionals. A secondary aim was to evaluate how maternal ACEs correlated with maternal mental health measures including depression, anxiety, substance use, and IPV. Two home visiting programs that support pregnant mothers and early childhood development in Rochester, Minnesota were utilized for community implementation of the ACE screen and data retrieval.
Methods
Program 1: Early Head Start
Head Start is a nationwide program that offers free services to preschool children and their families. Families must meet the federal poverty guidelines to be eligible. Pregnant women, infants, toddlers, and children up to age five are eligible. Head Start programs provide education in the childcare setting and focus on building safe relationships within households, encouraging parents to be their child’s first source of guidance and supporting children’s mental and physical growth (“Office of Head Start,” 2016). Early Head Start (EHS) focuses on children up to the age of three. During 2016, there were 96 children in the Rochester EHS Program. The race distribution of participating children during the study period was 40% White, 33% Black, 10% multi-racial, 9% Asian, 5% Hispanic, and <1% American Indian/Alaska Native (Weis, 2016). While only 5% identified as Hispanic race, 35% identified as Hispanic/Latino ethnicity.
The EHS Home Visiting Program brings the educational model of EHS into the home. Children receive a minimum of 48 weekly visits per year. Each visit is 90 minutes long and focuses on parent education and child development. A home visitor (usually a social worker) will observe the child’s developmental progress and parent-child interactions, and make recommendations via the evidence-based Growing Great Kids/Growing Great Families curriculum (GGK/GGF) (“Growing Great Kids,” 2010–2015). The GGK/GGF curriculum focuses on developing six family strengths: nurturing and attachment, social and emotional competence of children, knowledge of parenting and child development, parental resilience, social connections, and concrete supports for parents.
Program 2: Olmsted County Public Health Services
The Olmsted County Public Health Services (OCPHS) Home Visiting Program targets families with risk factors for child maltreatment and poor infant brain development. Families are eligible to participate if they are pregnant or have a child up to five years of age. The race distribution of participating children during the study period was 65% White, 20% Black, 8% Asian, and 7% other. In terms of ethnicity, 15% identified as Hispanic and 85% identified as non-Hispanic (Swenson, 2017).
The OCPHS Home Visiting Program supports the parent-child relationship by focusing on family health, safety, child development, parental stress management, and social support. Home visits are provided by bachelor-prepared public health registered nurses. In 2012, OCPHS started integrating the Healthy Families America (HFA) model of family home visiting into all of its pregnancy and parenting home visiting programs. HFA is a nationally recognized evidence-based model of home visiting with the primary goal of preventing child maltreatment. Nurses use the GGK/GGF curriculum (“Growing Great Kids,” 2010–2015) to promote parental resiliency and help parents reach their parenting goals.
Study Instruments
The ACE screen was introduced by both programs in conjunction with this study. The Edinburgh Postnatal Depression Scale (EPDS) was part of standard practice by EHS, and the remaining screens below were part of standard practice by OCPHS.
ACE Screen
The ACE screen is a 10-item questionnaire that addresses past experiences of physical, sexual, or emotional abuse, physical or emotional neglect, domestic violence, family separation, and family member substance use, mental illness, or incarceration (Felitti et al., 1998). One point is assigned for each of the 10 possible ACEs, resulting in an ACE score between 0–10. There is no established cutoff value for a significantly high ACE score and no validation studies are available. The ACE screen was translated into Spanish, Somali, and Arabic for this study by institutional translation services.
EPDS
The Edinburgh Postnatal Depression Scale (EPDS) is a validated screen for postpartum depression (Cox, Holden, & Sagovsky, 1987). Mothers are asked 10 questions and told to choose the answer that best fits how they feel. The responses are scored 0–3, with a total possible score range of 0–30. A score of 10 or higher is considered significant. The final question is evaluated both in conjunction with the others and singularly, as it pertains to suicidal ideation.
PHQ-9
The PHQ-9 is a validated, nine-question depression screening tool (Kroenke, Spitzer, & Williams, 2001). Participants are asked how often in the past two weeks they felt a certain way and give a score of 0 (not at all), 1 (several days), 2 (more than half the days), or 3 (nearly every day). The responses are totaled and a score of 5 or higher is considered significant by home visitors.
GAD-7
The GAD-7 is a validated, seven-question screening instrument for generalized anxiety disorder (Lowe et al., 2008). Participants are asked how often in the past two weeks they were bothered by numerous things and give a score of 0 (not at all), 1 (several days), 2 (more than half the days), or 3 (nearly every day). The responses are totaled and a score of 5 or higher is considered significant by home visitors.
PHQ-4
The PHQ-4 is a validated screen that pulls two questions from the PHQ-9 and two questions from the GAD-7 (Lowe et al., 2010). This is done to simultaneously screen for anxiety and depression. A score of 1 or higher in either the depression or anxiety section is considered significant and leads to follow up screening with either the PHQ-9 or the GAD-7. This was the first screen given to all participating parents in the OCPHS group of this study, and a follow up PHQ-9 or GAD-7 was completed only if PHQ-4 screened positive for depression or anxiety.
CAGE
The CAGE screen is a validated tool to screen for alcohol abuse (Ewing, 1984). Patients are asked four questions related to their alcohol use. A score of 1 indicates a possible alcohol use disorder, and a score of 2 or higher indicates a probable alcohol use disorder.
CAGE-AID
The CAGE-AID expands upon the CAGE to screen for drug use (Couwenbergh, Van Der Gaag, Koeter, De Ruiter, & Van den Brink, 2009). The scoring is the same as for the CAGE.
HARK-C
The HARK-C is a validated screen for IPV which helps identify victims of physical, sexual, or emotional violence within a relationship, and whether or not a child was present during the violence (Sohal, Eldridge, & Feder, 2007). The tool includes five questions. The spouse/significant other is not present during this screen. A score of 1 or higher is considered significant.
Study Design
This was a prospective observational pilot study. De-identified data was sent electronically from EHS and OCPHS to research staff. Because the data was de-identified, the Institutional Review Board exempted the protocol from review.
Study Procedure: Early Head Start
Children were voluntarily registered in the EHS Home Visiting Program via recruitment, health care provider referral, school referral, or word of mouth. All parents with children under one year of age in the program during the study enrollment period were invited to participate in the study, regardless of how many home visits they had completed up to that point. The earliest that a family enrolled in the study was during their 4th home visit, and the latest a family enrolled was at their 36th home visit.
During the enrollment home visit, a preliminary video was shown to families about the original ACE study (Felitti et al., 1998), and an ACEs explanation pamphlet was provided. The pamphlet covered what types of questions the ACE screen would ask, explained that honesty was best when answering, and informed parents that this study would not share any personal protected health information with research staff (only demographic and screening data). A signature of consent was required prior to screening. Parents were given the ACE screen and EPDS by the home visitor and had the choice to fill out the questionnaires privately or to have the home visitor read and fill in the responses for them.
Based upon results of the ACE screen, teaching and referrals were put into action using a response algorithm, largely drawing from the GGK/GGF curriculum (“Growing Great Kids,” 2010–2015), as well as local mental health services. For example, if the answer to the ACE question regarding emotional abuse was positive, the home visitor would implement 2 GGK modules, 2 GGF modules, character building exercises, positive discipline home visiting modules, and a positive discipline parenting group.
The EPDS was offered to all mothers who enrolled in the program during pregnancy, and was completed during the 3rd trimester, 2 weeks after delivery, and 6 weeks after delivery. Mothers had the right to refuse the screen. If a mother scored 10 or higher on the EPDS, or if she scored positive on the single question pertaining to suicidal ideation, her primary obstetrician was notified to ensure proper referrals were made, and/or a note was made as to where she was already established with psychology/psychiatry care. If the score was 8 or 9 (i.e., borderline risk for developing depression), she was followed more closely by the EHS team with more frequent calls and visits.
Study Procedure: Olmsted County Public Health Services
Voluntary participation in the OCPHS Home Visiting Program was gained through referrals from Women, Infants, & Children (WIC), prenatal and postpartum facilities, other health care providers, and social services. Some participation was gained through recruitment and word of mouth.
At the first visit, an intake home visiting nurse completed an assessment to determine program eligibility as well as strengths and needs of the family. If eligible for the program during the study period, parents of children younger than one year of age were given the option to complete the ACE screen. When explaining the ACE questionnaire, the intake nurses described to families that they were participating in a grant project that would help determine whether ACE screening was feasible to complete during home visits, and especially the initial home visit. Families were told that completion of the screen was voluntary, and if they chose to participate they were given the option to do the questionnaire on their own or to have the intake nurse help them. All clients who did not speak English had an interpreter present to help translate the document. A verbal consent was required for study participation.
The remaining mental health screens – PHQ-4, follow up PHQ-9 and GAD-7 if indicated, CAGE, CAGE-AID, and HARK-C – were offered to all parents in the home visiting program. Parents had the right to refuse any of the screens.
The results of the ACE screen were addressed by both the intake and ongoing nurses. The intake nurse would thank parents for taking the time to complete the screen and also sharing the information they chose to share. The ongoing nurse would follow-up with the client at a later date to acknowledge that the intake nurse had shared the questionnaire with them and to acknowledge the experience of the client. If the client wanted to further discuss their results, the nurse would provide active listening and other interventions as needed, including modules from the GGK/GGF curriculum (“Growing Great Kids,” 2010–2015) and referrals to community resources (“Community Connections Family Resource Directory,” 2016–2017). The ongoing nurse was open to discussing the screening at any time if the client wished to do so, or if the nurse wished to relate a parenting behavior (positive or otherwise) to the results from the ACE screen during future home visits.
Analysis
EHS and OCPHS staff provided de-identified demographic data and screening results to research staff. The data was transcribed into a database for storage and analysis. Descriptive statistics of participant demographics and screening results were produced using Microsoft Excel 2011. A Wilcoxon non-parametric test was used to compare the distributions of ACE scores between the OCPHS and EHS populations. When multiple screening results were available for the same participant (e.g., for standard practice mental health outcome screens), only the first screen available was included in analysis for consistency. Due to the availability of a larger volume of data from OCPHS compared to EHS, logistic models of the association between ACE score and mental health screens in the OCPHS group were conducted using JMP Pro, Version 12.2.0.
Results
EHS Results
All 20 parents who were invited to participate agreed to complete the ACE screen (100% acceptance). Parents included 3 males and 17 females. Two of these were from the same family (one mother and one father). Eighty percent of parents reported an ACE score of at least 1, and 45% reported an ACE score of at least 4. The range of scores represented among the parents was 0–10, with mean ACE score 3.6 [standard deviation (SD) 3.1] and median score 3.0 [interquartile range (IQR) 5.0].
All 10 of the mothers asked to complete the EPDS per EHS protocol agreed to do so (100% acceptance). Of these, 3/10 (30%) screened positive for depression. The mean ACE score of mothers screening positive for depression was 4.0 (SD 2.0), while the mean ACE score of mothers screening negative for depression was 3.4 (SD 2.6).
OCPHS Results
Of the 94 parents invited to participate, 90 agreed to complete the ACE screen (96% acceptance). Parents included 6 males and 84 females. Data on how many of these mothers and fathers represented members of the same family were not available to research staff. Among the OCPHS respondents, 73% reported an ACE score of at least 1, and 33% reported an ACE score of at least 4. The range of scores represented among the parents was 0–9, with mean ACE score 2.8 (SD 2.7) and median score 2.0 (IQR 5.0).
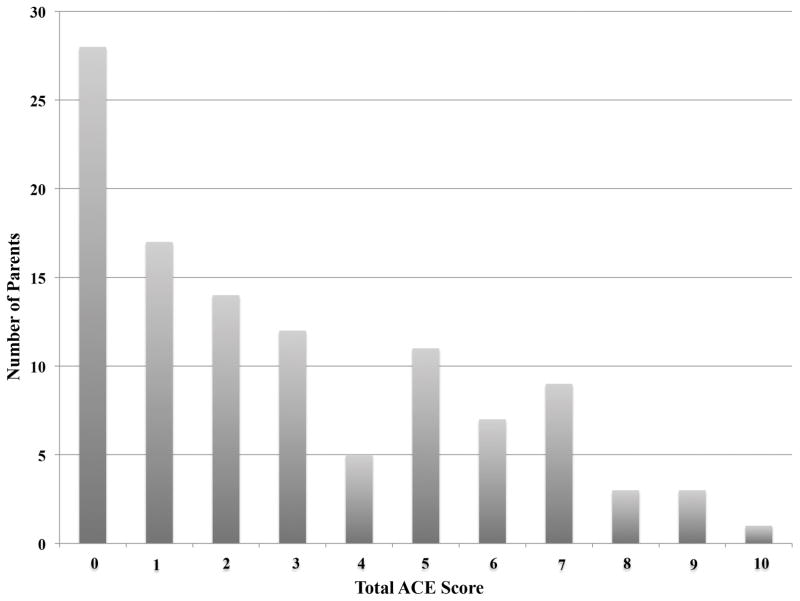
The ACE score responses from both EHS and OCPHS are combined in Figure 1. Distribution of ACE scores was skewed to the right, with more parents reporting lower ACE scores than higher ACE scores.
Figure 1.
A Wilcoxon non-parametric test was used to compare the distributions of ACE scores between the OCPHS and EHS populations, which was non-significant (p=0.40).
A subset of the 90 parents screened by OCPHS for ACEs also agreed to complete additional mental health screens per OCPHS protocol, including screens for depression (44 mothers; 49% acceptance), anxiety (42 mothers; 47% acceptance), alcohol/substance use (46 mothers, 2 fathers; 53% acceptance), and IPV (25 mothers; 28% acceptance). With the exception of 2 alcohol/substance use screens, all of these were completed by mothers rather than fathers.
Depression and anxiety screens were coded as either prenatal or postnatal. A subset of the postnatal screens (4 depression and 5 anxiety) were conducted after the traditional postpartum period of 6 weeks. The latest of these occurred when the child was 9 months of age. For simplicity, the term “postnatal” is used to describe all of the screens completed after birth, regardless of the age of the child. In addition, there were 9 mothers from the prenatal depression screening group and 7 from the prenatal anxiety screening group who later went on to be screened postnatally as part of OCPHS standard practice. These results are outlined separately below. None of the pre- or postnatal screens included in table 1 represent the same mother completing the screen twice.
Table 1.
Association between Mental Health Screens and ACE scores in OCPHS* Group
| Maternal Mental Health Screen | Number of Participants | % Screening Positive | ACE Score Median (IQR†) | P value | Odds Ratio |
|---|---|---|---|---|---|
| Depression – Prenatal | 29 | 48 | 2.0 (5.0) | 0.05 | 1.34 |
| Depression – Postnatal | 15 | 53 | 2.0 (3.0) | 0.95 | 0.98 |
| Depression – Overall | 44 | 50 | 2.0 (4.5) | 0.09 | 1.23 |
| Anxiety – Prenatal | 28 | 43 | 2.5 (5.5) | 0.15 | 1.22 |
| Anxiety – Postnatal | 14 | 50 | 2.5 (4.0) | 0.42 | 1.24 |
| Anxiety – Overall | 42 | 45 | 2.5 (4.0) | 0.10 | 1.22 |
| HARK-C | 25 | 32 | 2.0 (4.0) | 0.37 | 1.15 |
| CAGE and CAGE-AID‡ | 45 | 0 | 2.0 (5.0) | N/A | N/A |
OCPHS = Olmsted County Public Health Services
IQR = Interquartile Range
includes results from 2 fathers that completed the screens
In all, 44 mothers completed a screen for depression (29 prenatal and 15 postnatal). In the prenatal period, 48% screened positive for depression (14 positive/15 negative). In the postnatal period, 53% screened positive (8 positive/7 negative). The subset of 4 postnatal screens occurring after 6 weeks consisted of 3 positive screens and 1 negative. The average ACE score for mothers screening positive prenatally was 4.1 (SD 2.8), and for those screening negative prenatally 2.0 (SD 2.7). The average ACE score for mothers screening positive postnatally was 2.5 (SD 2.4), and for those screening negative postnatally also 2.5 (SD 2.0).
In all, 42 mothers completed a screen for anxiety (28 prenatal and 14 postnatal). In the prenatal period, 43% screened positive for anxiety (12 positive/16 negative). In the postnatal period, 50% screened positive (7 positive/7 negative). The subset of 5 postnatal screens occurring after 6 weeks consisted of 2 positive screens and 3 negative. The average ACE score for mothers screening positive prenatally was 4.0 (SD 3.1), and for those screening negative prenatally 2.4 (SD 2.7). The average ACE score for mothers screening positive postnatally was 3.0 (SD 2.3), and for those screening negative postnatally 2.4 (SD 2.0).
The subset of 9 mothers screened both prenatally and postnatally for depression consisted of 4 unchanged negatives, 1 unchanged positive, 3 positive-to-negatives, and 1 negative-to-positive. The subset of 7 mothers screened both prenatally and postnatally for anxiety consisted of 3 unchanged negatives, 1 unchanged positive, 1 positive-to-negative, and 2 negative-to-positives.
There were 48 parents (46 mothers and 2 fathers) who completed the CAGE and CAGE-AID screens for alcohol and substance abuse. All of these screens were negative. In addition, 25 mothers completed the HARK-C screen for IPV, and 32% screened positive. Data on the prenatal vs. postnatal timing of the CAGE, CAGE-AID, and HARK-C screens were not available to research staff.
Logistic modeling demonstrated that positive maternal depression screen trended toward association with increasing ACE score (p=0.09), driven primarily by prenatal screens (p=0.05) rather than postnatal screens (p=0.95). Similarly, but to a lesser extent, positive maternal anxiety screen trended toward association with increasing ACE score (p=0.10), driven more by prenatal screens (p=0.15) than postnatal screens (p=0.42). Increasing ACE score was not associated with IPV (p=0.36), and could not be determined for CAGE or CAGE-AID screens due to single response level (i.e., all screens were negative).
Discussion
This is the first report to our knowledge on prospective ACE screening of parents in the home setting. Our pilot study demonstrated that home-based screening for parents of infants in the first year of life is feasible, as demonstrated by availability of time and staff to complete the screening, as well as the high acceptability rates of the ACE screen by parents. Connecting families with resources during the first year of life is important given the rapid progression of child development and parent-child attachment in the early months. Our approach to home-based screening and referral differs from previously established interventions for adult survivors of ACEs, which primarily occur in the clinical setting (Korotana, Dobson, Pusch, & Josephson, 2016) and are not specifically targeted toward pregnant mothers and families with infants.
Our two home visiting programs conducted screening and referral in a similar fashion, but there were some differences worth noting. First, they differed in who conducted the screening: social workers for EHS and public health nurses for OCPHS. Second, OCPHS always conducted the screening at the initial intake home visit, whereas the timing for EHS screenings varied based on where the family was in the visit schedule at the time of study initiation, ranging between the 4th and 36th visit. Third, EHS used a standard intervention and referral response algorithm, while OCPHS used a more individualized approach. Both groups provided flexibility in how the parents filled out the screens – either privately or with the help of the home visitor – and both conducted screening and referral at home visits before the child’s first birthday.
There are a number of ways to carry out ACE screening. Our home visitors used written questionnaires completed by the parents either in coordination with the home visitor or in private. The same questionnaires can be used in a clinical practice setting (Glowa, Olson, & Johnson, 2016) to retrieve either an isolated ACE score or to record specific items screening positive. Whether one focuses on the total number of ACEs or the specific items screening positive may depend in part on whether the goal of screening is to identify the level of risk for development of mental or physical health conditions, or to intervene immediately with resources and referral.
It is worth noting that the current ACE screen emerged from a study of primarily Caucasian, college-educated, adult population, majority over 50 years of age (Felitti et al., 1998). It may not be generalizable to all groups such as new parents, single parent households, or refugee families. Some researchers are beginning to use the ACE screen with different populations (Giovanelli, Reynolds, Mondi, & Ou, 2016; Mersky, Topitzes, & Reynolds, 2013) and to ask different ACE questions, for example, pertaining to peer rejection and socioeconomic status (Finkelhor, Shattuck, Turner, & Hamby, 2013). This may help expand its scope of practice.
In all cases, the rationale for screening should be explained to parents before delivering the screen to alleviate potential concerns of judgment or bias based on the results, and screening should ideally be conducted by a professional who has rapport with the family. While our OCPHS home visitors conducted screening at the initial intake visit, EHS home visitors conducted screening weeks or months into the home visiting program. This may have contributed to the higher mean and median ACE score seen in the EHS group compared to the OCPHS group – that is, parents may feel more comfortable providing honest responses to sensitive questions when the person screening was familiar to them. This concept is supported by psychiatric literature showing that a strong therapeutic alliance may improve mental health outcomes (Howgego, Yellowlees, Owen, Meldrum, & Dark, 2003). That being said, there were differences between the two participant groups that may have contributed to the difference in ACE scores, such as the low-income requirement and higher percentage of racial minorities in the EHS group.
Our logistic analysis revealed a trend toward association between positive depression screen and ACE score, particularly driven by the prenatal rather than the postnatal screen. Further research is needed to evaluate whether this finding is replicable. Our ACE scores and rates of positive depression, anxiety, and IPV screens were higher than rates seen in the literature. While the original ACE study found that about 50% of their population had experienced ≥1 ACE and about 6% had experienced ≥4 ACEs, our EHS group demonstrated figures of 80% and 45%, and our OCPHS group demonstrated figures of 73% and 33%, respectively. In addition, we saw a positive prenatal depression screen rate of 48% (population estimate 5–13%) (Hasin, Goodwin, Stinson, & Grant, 2005) and a positive postnatal depression screen rate of 53% (population estimate 12–13%) (Craig & Howard, 2009). Our positive prenatal anxiety screen rate was 43% (population estimate 10%) (Baxter, Scott, Vos, & Whiteford, 2013), and our positive postnatal anxiety screen rate was 50% (population estimate 8.5%) (Goodman, Watson, & Stubbs, 2016). Our rate of IPV was on the high end at 32% (population estimate 1–38%) (Bailey, 2010; Sprague et al., 2014).
Our higher ACE scores and rates of positive depression, anxiety, and IPV screens may be attributable in part to the high-risk population we screened (i.e., participants were either from low-income families or at risk for child maltreatment). In addition, OCPHS used a score of 5 as a cutoff for a positive PHQ-9 or GAD-7, which is lower than the typical score of 10 used to indicate the need for intervention in the clinical setting (Kroenke et al., 2001; Lowe et al., 2008). This may have led to high false-positive screening results. Lastly, participants had the right to refuse any of the screens, and thus, may have chosen to opt-out if they did not have any mental health or IPV concerns.
In contrast to the elevated rates of depression, anxiety, and IPV seen in our population, CAGE and CAGE-AID screens identified no cases of alcohol or substance use disorders. The majority of these screens were completed by mothers rather than fathers. This is consistent with previous research which shows that women tend to turn inward with their stress, manifesting in higher rates of depression and anxiety, while men tend to turn outward, manifesting in higher rates of alcohol and substance use (Khan et al., 2013). It is also possible that public awareness of the dangers of alcohol and substance use during pregnancy and breastfeeding contributed to these low rates, or that this knowledge led to dishonest responses provided to the healthcare-focused home visitors.
This study has several limitations: (1) The very small sample size makes the associations between ACEs and mental health outcomes very limited and underpowered. This may have contributed to a type II statistical error in which a significant association was not found where one existed. Small sample size also precluded us from performing logistic analysis on the EHS data set. (2) Because prevalence data regarding ACEs in various regions and demographics nationally are lacking, particularly in minority populations, we were unable to compare our results to any pre-study predictions and assess the honesty of responses obtained. (3) Our postnatal group did not consist of strictly postpartum mothers within 6 weeks of birth. The mothers screened outside of this time period are specifically outlined above. (4) While the screens used were all validated to be predictive of diagnosis, they were not calibrated in our specific population and thus may not be generalizable to our participants. (5) There was no pre-or postnatal designation for the CAGE, CAGE-AID, or HARK-C data, so separate pre- and postnatal analyses could not be performed. (6) Our correlations were drawn from total ACE scores which precludes us from identifying which specific ACE items were correlated with mental health outcomes, and we did not adjust for potential confounding factors such as family income and social support.
Conclusion
The feasibility and efficacy observed in our ACE screening of parents in the community supports further expansion of this model of care. Through this model, we were able to facilitate connections between families, public health nurses, social workers, mental health providers, and community resources. In this pilot study, we were able to identify a trend in the relationship between increasing ACE score and positive prenatal depression screen. Opportunities for future research include expanding this prospective home-based screening model into communities with differing resources (e.g., healthcare, social, and mental health resources), developing ACE prevalence data for various regions and demographics across the nation, exploring further the potential relationships between specific ACE items and maternal mental health outcomes, and examining the impact of parental ACEs on childhood growth and development.
Acknowledgments
The authors would like to acknowledge the staff of the CCaTS statistical consultation service at Mayo Clinic, for their assistance with statistical methods. This publication was supported by Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), as well as a Community Access to Child Health Grant from the American Academy of Pediatrics. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or American Academy of Pediatrics.
Footnotes
Disclosure: The authors have no financial involvement with this manuscript and there are no conflicts of interest.
References
- Accortt EE, Cheadle AC, Dunkel Schetter C. Prenatal depression and adverse birth outcomes: an updated systematic review. Matern Child Health J. 2015;19(6):1306–1337. doi: 10.1007/s10995-014-1637-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams L, Cotgrove A. Promoting secure attachment patterns in infancy and beyond. Prof Care Mother Child. 1995;5(6):158–160. [PubMed] [Google Scholar]
- Bailey BA. Partner violence during pregnancy: prevalence, effects, screening, and management. Int J Womens Health. 2010;2:183–197. doi: 10.2147/ijwh.s8632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med. 2013;43(5):897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- Bright MA, Knapp C, Hinojosa MS, Alford S, Bonner B. The Comorbidity of Physical, Mental, and Developmental Conditions Associated with Childhood Adversity: A Population Based Study. Matern Child Health J. 2016;20(4):843–853. doi: 10.1007/s10995-015-1915-7. [DOI] [PubMed] [Google Scholar]
- Brown MJ, Perera RA, Masho SW, Mezuk B, Cohen SA. Adverse childhood experiences and intimate partner aggression in the US: sex differences and similarities in psychosocial mediation. Soc Sci Med. 2015;131:48–57. doi: 10.1016/j.socscimed.2015.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi NG, DiNitto DM, Marti CN, Choi BY. Association of adverse childhood experiences with lifetime mental and substance use disorders among men and women aged 50+ years. Int Psychogeriatr. 2016:1–14. doi: 10.1017/S1041610216001800. [DOI] [PubMed] [Google Scholar]
- Chung EK, Mathew L, Rothkopf AC, Elo IT, Coyne JC, Culhane JF. Parenting attitudes and infant spanking: the influence of childhood experiences. Pediatrics. 2009;124(2):e278–286. doi: 10.1542/peds.2008-3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Community Connections Family Resource Directory 2016–2017. 2016 Jul; Retrieved February 4, 2017, from http://www.co.olmsted.mn.us/OCPHS/reports/Documents/CommunityConnectionsFall2016_17.pdf.
- Couwenbergh C, Van Der Gaag RJ, Koeter M, De Ruiter C, Van den Brink W. Screening for substance abuse among adolescents validity of the CAGE-AID in youth mental health care. Subst Use Misuse. 2009;44(6):823–834. doi: 10.1080/10826080802484264. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Craig M, Howard L. Postnatal depression. BMJ Clin Evid. 2009;2009 [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Weitz E, Karyotaki E, Garber J, Andersson G. The effects of psychological treatment of maternal depression on children and parental functioning: a meta-analysis. Eur Child Adolesc Psychiatry. 2015;24(2):237–245. doi: 10.1007/s00787-014-0660-6. [DOI] [PubMed] [Google Scholar]
- Davalos DB, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch Womens Ment Health. 2012;15(1):1–14. doi: 10.1007/s00737-011-0251-1. [DOI] [PubMed] [Google Scholar]
- Dennis CL, Vigod S. The relationship between postpartum depression, domestic violence, childhood violence, and substance use: epidemiologic study of a large community sample. Violence Against Women. 2013;19(4):503–517. doi: 10.1177/1077801213487057. [DOI] [PubMed] [Google Scholar]
- Donovan BM, Spracklen CN, Schweizer ML, Ryckman KK, Saftlas AF. Intimate partner violence during pregnancy and the risk for adverse infant outcomes: a systematic review and meta-analysis. BJOG. 2016;123(8):1289–1299. doi: 10.1111/1471-0528.13928. [DOI] [PubMed] [Google Scholar]
- Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252(14):1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Shattuck A, Turner H, Hamby S. Improving the adverse childhood experiences study scale. JAMA Pediatr. 2013;167(1):70–75. doi: 10.1001/jamapediatrics.2013.420. [DOI] [PubMed] [Google Scholar]
- Giovanelli A, Reynolds AJ, Mondi CF, Ou SR. Adverse Childhood Experiences and Adult Well-Being in a Low-income, Urban Cohort. Pediatrics. 2016;137(4) doi: 10.1542/peds.2015-4016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glowa PT, Olson AL, Johnson DJ. Screening for Adverse Childhood Experiences in a Family Medicine Setting: A Feasibility Study. J Am Board Fam Med. 2016;29(3):303–307. doi: 10.3122/jabfm.2016.03.150310. [DOI] [PubMed] [Google Scholar]
- Goodman JH, Watson GR, Stubbs B. Anxiety disorders in postpartum women: A systematic review and meta-analysis. J Affect Disord. 2016;203:292–331. doi: 10.1016/j.jad.2016.05.033. [DOI] [PubMed] [Google Scholar]
- Growing Great Kids. 2010–2015 Retrieved February 4, 2017, from http://www.greatkidsinc.org/ggk-p36.html.
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Howgego IM, Yellowlees P, Owen C, Meldrum L, Dark F. The therapeutic alliance: The key to effective patient outcome? A descriptive review of the evidence in community mental health case management. Australian and New Zealand Journal of Psychiatry. 2003;37(2):169–183. doi: 10.1046/j.1440-1614.2003.01131.x. [DOI] [PubMed] [Google Scholar]
- Khan S, Okuda M, Hasin DS, Secades-Villa R, Keyes K, Lin KH, et al. Gender differences in lifetime alcohol dependence: results from the national epidemiologic survey on alcohol and related conditions. Alcohol Clin Exp Res. 2013;37(10):1696–1705. doi: 10.1111/acer.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korotana LM, Dobson KS, Pusch D, Josephson T. A review of primary care interventions to improve health outcomes in adult survivors of adverse childhood experiences. Clin Psychol Rev. 2016;46:59–90. doi: 10.1016/j.cpr.2016.04.007. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe B, Decker O, Muller S, Brahler E, Schellberg D, Herzog W, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Lowe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1–2):86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child Abuse Negl. 2013;37(11):917–925. doi: 10.1016/j.chiabu.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JN, Martini A, Preen D. The well-being of children impacted by a parent with cancer: an integrative review. Support Care Cancer. 2016;24(7):3235–3251. doi: 10.1007/s00520-016-3214-2. [DOI] [PubMed] [Google Scholar]
- Narayan AJ, Kalstabakken AW, Labella MH, Nerenberg LS, Monn AR, Masten AS. Intergenerational continuity of adverse childhood experiences in homeless families: Unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsychiatry. 2017;87(1):3–14. doi: 10.1037/ort0000133. [DOI] [PubMed] [Google Scholar]
- Office of Head Start. 2016 Aug 15; Retrieved February 4, 2017, from http://www.acf.hhs.gov/programs/ohs/about/head-start.
- Sohal H, Eldridge S, Feder G. The sensitivity and specificity of four questions (HARK) to identify intimate partner violence: a diagnostic accuracy study in general practice. BMC Fam Pract. 2007;8:49. doi: 10.1186/1471-2296-8-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprague S, Goslings JC, Hogentoren C, de Milliano S, Simunovic N, Madden K, et al. Prevalence of intimate partner violence across medical and surgical health care settings: A systematic review. Violence Against Women. 2014;20(1):118–136. doi: 10.1177/1077801213520574. [DOI] [PubMed] [Google Scholar]
- Suess GJ, Sroufe J. Clinical implications of the development of the person. Attach Hum Dev. 2005;7(4):381–392. doi: 10.1080/14616730500365886. [DOI] [PubMed] [Google Scholar]
- Swenson S. Public Health Nursing Manager at Olmsted County Public Health. 2017. [Google Scholar]
- Szilagyi M, Kerker BD, Storfer-Isser A, Stein RE, Garner A, O’Connor KG, et al. Factors Associated With Whether Pediatricians Inquire About Parents’ Adverse Childhood Experiences. Acad Pediatr. 2016;16(7):668–675. doi: 10.1016/j.acap.2016.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weis C. Health Services Coordinator at Families First of Minnesota. 2016. [Google Scholar]