Summary
Background
Documentation of the demographic and geographical details of changes in cause-specific neonatal (younger than 1 month) and 1–59-month mortality in India can guide further progress in reduction of child mortality. In this study we report the changes in cause-specific child mortality between 2000 and 2015 in India.
Methods
Since 2001, the Registrar General of India has implemented the Million Death Study (MDS) in 1.3 million homes in more than 7000 randomly selected areas of India. About 900 non-medical surveyors do structured verbal autopsies for deaths recorded in these homes. Each field report is assigned randomly to two of 404 trained physicians to classify the cause of death, with a standard process for resolution of disagreements. We combined the proportions of child deaths according to the MDS for 2001–13 with annual UN estimates of national births and deaths (partitioned across India’s states and rural or urban areas) for 2000–15. We calculated the annual percentage change in sex-specific and cause-specific mortality between 2000 and 2015 for neonates and 1–59-month-old children.
Findings
The MDS captured 52 252 deaths in neonates and 42 057 deaths at 1–59 months. Examining specific causes, the neonatal mortality rate from infection fell by 66% from 11.9 per 1000 livebirths in 2000 to 4.0 per 1000 livebirths in 2015 and the rate from birth asphyxia or trauma fell by 76% from 9.0 per 1000 livebirths in 2000 to 2.2 per 1000 livebirths in 2015. At 1–59 months, the mortality rate from pneumonia fell by 63% from 11.2 per 1000 livebirths in 2000 to 4.2 per 1000 livebirths in 2015 and the rate from diarrhoea fell by 66% from 9.4 per 1000 livebirths in 2000 to 3.2 per 1000 livebirths in 2015 (with narrowing girl–boy gaps). The neonatal tetanus mortality rate fell from 1.6 per 1000 livebirths in 2000 to less than 0.1 per 1000 livebirths in 2015 and the 1–59-month measles mortality rate fell from 3.3 per 1000 livebirths in 2000 to 0.3 per 1000 livebirths in 2015. By contrast, mortality rates for prematurity or low birthweight rose from 12.3 per 1000 livebirths in 2000 to 14.3 per 1000 livebirths in 2015, driven mostly by increases in term births with low birthweight in poorer states and rural areas. 29 million cumulative child deaths occurred from 2000 to 2015. The average annual decline in mortality rates from 2000 to 2015 was 3.3% for neonates and 5.4% for children aged 1–59 months. Annual declines from 2005 to 2015 (3.4% decline for neonatal mortality and 5.9% decline in 1–59-month mortality) were faster than were annual declines from 2000 to 2005 (3.2% decline for neonatal mortality and 4.5% decline in 1–59-month mortality). These faster declines indicate that India avoided about 1 million child deaths compared with continuation of the 2000–05 declines.
Interpretation
To meet the 2030 Sustainable Development Goals for child mortality, India will need to maintain the current trajectory of 1–59-month mortality and accelerate declines in neonatal mortality (to >5% annually) from 2015 onwards. Continued progress in reduction of child mortality due to pneumonia, diarrhoea, malaria, and measles at 1–59 months is feasible. Additional attention to low birthweight is required.
Funding
National Institutes of Health, Disease Control Priorities Network, Maternal and Child Epidemiology Estimation Group, and University of Toronto.
Introduction
Progress in reduction of the current global total of 6 million child (younger than age 5 years) deaths depends greatly on India, which accounts for about a fifth of the global total.1 India’s child mortality rate per thousand livebirths has fallen by 62% from 125 per thousand livebirths in 1990 to 47 per thousand livebirths in 2015, slightly short of the 2015 Millennium Development Goal of a 66% reduction.1 Annual declines in child mortality rates were faster during 2000–15 than during 1990–2000. Fertility also fell: the average number of children born per woman aged 15–49 years decreased from 3.3 children per woman to 2.4 children per woman from 2000 to 2015.2 The next goals—the Sustainable Development Goals (SDGs), which the Government of India has accepted—call for India to achieve another halving of child mortality rates from 2015, reaching 25 per thousand livebirths by 2030.3 The SDGs also call for reduction by more than half of neonatal (first 28 days of life) mortality rates per thousand livebirths from 27 per thousand livebirths in 2015 to 12 per thousand livebirths in 2030.
In the last decade, the Government of India has modestly increased its traditionally low level of public spending on health, mostly through the National Health Mission (NHM; previously called the National Rural Health Mission, which concentrated on 18 states, including the nine poorest).4,5 To improve maternal and child health, the Government also launched a conditional cash transfer programme to encourage pregnant women to deliver in hospitals and a targeted campaign for a second dose of measles vaccine.4,6 Understanding of the effect of these investments and the prospects for India to achieve the SDGs requires reliable documentation of the demographic and geographical trajectories in cause-specific mortality, separately for neonates and ages 1–59 months. Moreover, a need exists to understand the changes in cause-specific mortality by sex given that, until recently, India has had much higher mortality at ages 1–59 months among girls than among boys.7 In this study we report the 2000–15 changes in cause-specific child mortality from the ongoing Million Death Study (MDS).
Methods
Study design and participants
Most deaths in India occur at home and without medical attention.8 Hence, deaths are not routinely registered and their causes remain unknown. In the absence of complete registration and medical certification of deaths, the Registrar General of India (RGI) has implemented the MDS in 1.3 million homes since 2001 within its Sample Registration System (SRS), a continuous demographic surveillance system in operation since 1971. After each census, the RGI partitions India into 1 million small areas (rural villages or urban census enumeration blocks, each with typically 150–300 homes). The SRS randomly selects and monitors several thousand units from these areas for the next decade, capturing about 140 000 births and 46 000 deaths annually. This study relied on 6671 units drawn from the 1991 census and 7597 drawn from the 2001 census.8 Approximately 900 trained non-medical RGI surveyors do two rounds per year of interviews of household members or close associates of people who have died since the last round using a modified version of the 2011 WHO verbal autopsy questionnaire. The interview uses structured checklist questions about key symptoms and a half-page local language narrative that captures events and their chronology.
Each field report is converted to electronic format and assigned to two of 404 trained physicians using an online system developed for the MDS.9 These physicians receive standardised training and pass an exam with questions randomly allocated. Assignment is random to the physicians, who classify the underlying causes of death according to the International Classification of Diseases, tenth revision (ICD-10; appendix pp 6–7),10 using strict coding guidelines.11 Initial differences in coding (about 30%) are reconciled by both physicians, each anonymously receiving the other’s notes justifying a particular ICD-10 code.12 One of 40 senior physicians adjudicates persisting differences (about 10%).12 The fieldwork, data capture, physician coding, and other steps are subjected to various quality assurance checks.9,11–16 Independent teams resampled about 3% of the deaths in 2001–03, yielding similar results to the original survey.12,13
Statistical analysis
We calculated the age-specific and sex-specific mortality proportions using 3 year backward-moving averages for each disease, weighted by the SRS sampling probability for enrolled populations in rural and urban areas of 35 states and union territories. We applied these weighted cause-specific proportions for 2001–13 deaths from the MDS to estimated child deaths (0–28 days, 29 days to 11 months, and 1–4 years) in India and its 35 states and union territories by rural and urban residence and by sex as determined by 1998–2014 SRS vital statistics and the 2001 and 2011 censuses. The SRS undercounts male deaths at older than age 5 years by about 1–4% and female deaths at these ages by about 8–11%, but comparison with full birth histories in household surveys shows high consistency of mortality of those aged younger than 5 years between the different data sources.2,17,18 We adjusted the final totals to match the national birth totals as determined by the UN Population Division and death totals as determined by the UN Population Division’s Inter-agency Group for Child Mortality Estimation (IGME), for 2000–15.1,2,19 This adjustment had the benefit of accounting for any residual undercounts in the SRS and the approximate 5% of deaths that were missed during the fieldwork, mostly from the household being unavailable or migration from the local area.11,12
We adopted the IGME’s 90% CIs for the total child mortality envelopes.1,19 The major uncertainty in our analyses, however, is not the demographic totals, but the cause of death classification. Hence, the lower bounds for the mortality rates for major causes correspond to the rates if both physicians immediately agreed on the ICD-10 code and the upper bounds correspond to the rates if only one physician assigned that code. We fitted cubic spline polynomial curves to 2001–13 cause-specific mortality rates of the rural–urban and poorer–richer state strata to extrapolate to 2000 and 2014–15. We calculated the simple annual percentage change in sex-specific and cause-specific mortality averaged for three 6-year time periods, including a 1-year overlap: 2000–05 (before the start of the NHM), 2005–10 (during the NHM’s early implementation), and 2010–15 (during the NHM’s full implementation). We stratified analyses by sex, age (neonatal [younger than 1 month (0–28 days)] and 1–59 month), rural or urban residence, and the nine poorer (low resources and spending)20 states: Assam, Bihar, Jharkhand, Madhya Pradesh, Chhattisgarh, Odisha, Rajasthan, Uttarakhand, and Uttar Pradesh.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
From 2000 to 2015, the mortality rates among neonates, 1–59-month-olds, and all those younger than 5 years of age fell (table; appendix p 9). The average annual decline in mortality rates from 2000 to 2015 was 3.3% for neonates and 5.4% at ages 1–59 months. This average annual mortality decline provides a useful benchmark to compare declines in various subpopulations of region, age, sex, and conditions for the three specified time periods. The annual mortality declines were faster at ages 1–59 months than during the neonatal period. For both age groups, annual mortality declines were fastest during 2010–15. Among neonates, the fastest annual mortality declines were seen in urban areas and the richer states. At ages 1–59 months, the average annual decline in mortality rates from 2000 to 2015 was 6.0% for girls and 4.6% for boys. From 2000 to 2015, the rural-to-urban ratio of mortality rates decreased at ages 1–59 months from 1.7 to 1.3, but increased for neonatal deaths from 1.7 to 2.1 (appendix p 9).
Table.
Annual mortality of those aged younger than 5 years in India, 2000–15
| Deaths in 2015 (thousands) | Mortality rate per 1000 livebirths
|
Average annual change (%)*
|
||||||
|---|---|---|---|---|---|---|---|---|
| 2000† | 2005‡ | 2010§ | 2015¶ | 2000–05 | 2005–10 | 2010–15 | ||
| Neonatal | 696 | 45.0 (41.9–48.6) | 38.1 (35.3–41.3) | 32.8 (30.0–35.5) | 27.0 (24.0–31.6) | −3.2% | −3.0% | −3.8% |
| Girls | 328 | 41.1 | 36.8 | 31.1 | 26.8 | −2.2% | −3.3% | −2.9% |
| Boys | 368 | 48.5 | 39.3 | 34.3 | 27.1 | −4.1% | −2.7% | −4.6% |
| Rural | 598 | 49.7 | 42.4 | 37.2 | 31.1 | −3.1% | −2.6% | −3.6% |
| Urban | 98 | 28.8 | 24.2 | 19.6 | 15.0 | −3.4% | −4.1% | −5.3% |
| Poorer states‖ | 483 | 51.9 | 44.2 | 38.4 | 31.8 | −3.2% | −2.8% | −3.7% |
| Richer states | 213 | 36.0 | 30.0 | 25.0 | 20.1 | −3.6% | −3.6% | −4.3% |
|
| ||||||||
| 1–59 months | 505 | 45.2 (42.9–49.6) | 35.8 (33.3–39.6) | 27.2 (23.9–30.7) | 19.6 (14.7–25.6) | −4.5% | −5.3% | −6.4% |
| Girls | 260 | 54.2 | 41.2 | 32.1 | 21.2 | −5.4% | −4.8% | −7.9% |
| Boys | 245 | 37.0 | 31.0 | 22.8 | 18.1 | −3.4% | −5.9% | −4.5% |
| Rural | 402 | 49.6 | 39.5 | 29.6 | 20.9 | −4.5% | −5.6% | −6.8% |
| Urban | 103 | 30.0 | 23.8 | 20.2 | 15.8 | −4.4% | −3.2% | −4.7% |
| Poorer states‖ | 371 | 56.2 | 44.2 | 33.8 | 24.4 | −4.7% | −5.2% | −6.3% |
| Richer states | 134 | 31.0 | 24.5 | 18.1 | 12.6 | −4.6% | −.8% | −7.0% |
|
| ||||||||
| Younger than 5 years of age | 1201 | 90.1 (88.0–94.7) | 74.0 (71.6–77.9) | 60.0 (56.6–63.4) | 46.6 (42.4–53.3) | −3.9% | −4.1% | −5.0% |
| Girls | 588 | 95.3 | 78.0 | 63.2 | 48.0 | −3.9% | −4.1% | −5.3% |
| Boys | 613 | 85.5 | 70.4 | 57.2 | 45.2 | −3.8% | −4.1% | −4.6% |
| Rural | 1000 | 99.3 | 81.9 | 66.8 | 51.9 | −3.8% | −4.0% | −4.9% |
| Urban | 201 | 58.8 | 48.1 | 39.8 | 30.8 | −3.9% | −3.7% | −5.0% |
| Poorer states‖ | 854 | 108.1 | 88.4 | 72.2 | 56.2 | −3.9% | −4.0% | −4.9% |
| Richer states | 347 | 67.1 | 54.6 | 43.1 | 32.7 | −4.0% | −4.6% | −5.4% |
|
| ||||||||
| Neonatal causes | .. | .. | .. | .. | .. | .. | .. | .. |
| Prematurity or low birthweight | 370 | 12.3 | 12.5 | 14.3 | 14.3 | 0.4% | 2.8% | 0 |
| Neonatal infections** | 103 | 11.9 | 8.1 | 5.7 | 4.0 | −7.5% | −6.7% | −6.8% |
| Birth asphyxia or trauma | 57 | 9.0 | 6.5 | 3.9 | 2.2 | −6.5% | −9.4% | −10.9% |
| Non-communicable | 52 | 2.4 | 2.5 | 2.2 | 2.0 | 0.7% | −2.2% | −2.1% |
| Congenital | 28 | 1.8 | 1.7 | 1.4 | 1.1 | −2.0% | −3.3% | −5.1% |
| Other conditions†† | 41 | 3.2 | 3.2 | 2.4 | 1.6 | 0.4% | −5.4% | −8.2% |
| Injuries | 13 | 0.3 | 0.4 | 0.3 | 0.5 | 6.9% | −2.6% | 10.1% |
| Tetanus | 0.6 | 1.6 | 1.3 | 0.7 | <0.1 | −4.9% | −10.2% | −43.5% |
| Ill-defined | 6 | 0.8 | 0.7 | 0.5 | 0.2 | −1.3% | −7.5% | −14.7% |
|
| ||||||||
| 1–59 months causes | .. | .. | .. | .. | .. | .. | .. | .. |
| Pneumonia | 108 | 11. | 8.3 | 6.2 | 4.2 | −5.8% | −5.6% | −7.6% |
| Diarrhoea | 82 | 9.4 | 7.2 | 5.3 | 3.2 | −5.3% | −5.9% | −9.7% |
| Injuries | 69 | 2.3 | 2.4 | 2.2 | 2.7 | 1.0% | −1.6% | 4.2% |
| Non-communicable | 54 | 3.5 | 2.8 | 2.6 | 2.1 | −4.4% | −1.8% | −4.0% |
| Other infections | 53 | 3.4 | 3.3 | 2.9 | 2.1 | −0.5% | −3.0% | −6.3% |
| Nutritional | 29 | 1.5 | 1.8 | 1.7 | 1.1 | 3.4% | −1.2% | −7.4% |
| Malaria | 28 | 2.0 | 1.6 | 1.3 | 1.1 | −4.3% | −3.9% | −3.1% |
| Congenital | 26 | 1.4 | 1.3 | 1.2 | 1.0 | −1.0% | −1.8% | −3.5% |
| Meningitis or encephalitis | 22 | 2.1 | 1.9 | 1.2 | 0.8 | −2.0% | −8.5% | −7.3% |
| Acute bacterial sepsis or severe infection | 8 | 1.6 | 1.1 | 0.5 | 0.3 | −7.7% | −13.3% | −9.7% |
| Measles | 7 | 3.3 | 1.7 | 0.9 | 0.3 | –12.0% | –11.0% | –21.8% |
| Ill-defined‡‡ | 20 | 3.4 | 2.5 | 1.2 | 1.1 | –6.1% | –13.0% | –2.3% |
Data in parentheses are 90% CIs. We adjusted subnational estimated livebirths and deaths of those aged younger than 5 years to match the UN Inter-agency Group for Child Mortality Estimation estimates. 2015 Inter-agency Group for Child Mortality Estimation estimates substantially revised the 2005 mortality totals. Hence, the neonatal and 1–59-month mortality rates for 2005 differ from those published previously using 2001–03 data.15
Average of simple annual rates of changes in mortality.
27.9 million livebirths.
27.6 million livebirths.
26.6 million livebirths.
25.8 million livebirths.
Low-income states where approximately half of India’s population lives: Assam, Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Odisha, Rajasthan, Uttarakhand, and Uttar Pradesh.
Neonatal infections consist of, in descending proportions, pneumonia, sepsis, and meningitis or encephalitis.
Other conditions consist of, in descending proportions, other infections, other perinatal conditions, and nutritional conditions.
Ill-defined conditions at ages 1–59 months include the few deaths coded as perinatal before 2005.
The MDS captured 94309 child deaths (52252 neonatal deaths and 42057 deaths at ages 1–59 months) from 2001 to 2013, which revealed substantial variation in mortality rates for specific conditions. Neonatal infection mortality rates (comprising mostly neonatal pneumonia and sepsis) fell across the three time periods (table; the appendix [pp 11–17] provides mortality rates for various conditions in the three time periods). Birth asphyxia or trauma mortality rates declined annually during 2010–15. Tetanus mortality rates declined sharply annually during 2010–15. By contrast, prematurity or low birthweight mortality rates rose by 1% annually from 2000 to 2015, with the largest increase during 2005–10 and plateauing during 2010–15.
At ages 1–59 months, mortality rates for all causes except for injuries declined (table). Declines in mortality rates from pneumonia and diarrhoea accelerated during 2010–15, but declines in malaria mortality rates slowed after 2010. Measles mortality rates declined substantially in each time period, but notably so during 2010–15. Mortality rates for the major neonatal and 1–59-month causes stratified by sex (appendix pp 12–13), residence (appendix pp 16–17), and poorer or richer states (appendix pp 14–15) are shown in the appendix.
India’s births have declined only slightly from about 28 million to about 26 million from 2000 to 2015 (appendix p 10). Hence, the approximate halving of child mortality rates (table) has approximately halved absolute child deaths, from about 2.5 million in 2000 to about 1.2 million in 2015 (appendix p 10). In 2015, the largest absolute numbers of child deaths were in rural areas (about 1.0 million) and the nine poorer states (about 0.85 million), reflecting a growing proportion of national total births and slower declines in neonatal mortality rates in rural areas than in urban areas. Neonatal deaths were 50% of all child deaths in 2000, but this proportion rose to 58% by 2015. Three causes—prematurity or low birthweight, neonatal infections, and birth asphyxia or trauma—accounted for more than three-quarters of neonatal deaths (appendix p 18). Pneumonia and diarrhoea constituted more than one-third of 1–59-month deaths. During the study period, little change occurred in the rank order of the major neonatal causes of death in the three time periods. By contrast, marked change occurred in rank order at 1–59 months from 2000 to 2015, with measles deaths falling from fifth to 11th rank because of a more than 90% reduction. Deaths from injuries rose from the sixth rank to third rank. 17000 (25%) of 69000 injury deaths in 2015 were due to falls and about 14000 (20%) were due to drowning.
Neonatal mortality rates in rural and urban areas declined, but the rates in rural areas remained more than two-thirds higher than those in urban areas throughout the entire period (figure 1). At ages 1–59 months, the girl–boy relative mortality narrowed substantially from a 47% excess in girls in 2000 to a 17% excess in 2015. The girl–boy gap in pneumonia and diarrhoea mortality rates narrowed substantially. As a check for possible misclassifications, we compared mortality trends using the strictest definition—when the two reviewing physicians immediately agreed on the cause of death—with trends using all of the data, and the results were similar (appendix pp 11–17). The mortality rates from ill-defined causes fell from 2000 to 2015 among neonates as well as among 1–59-month-olds (table).
Figure 1. Mortality rates in children aged younger than 5 years in India, 2000–15.
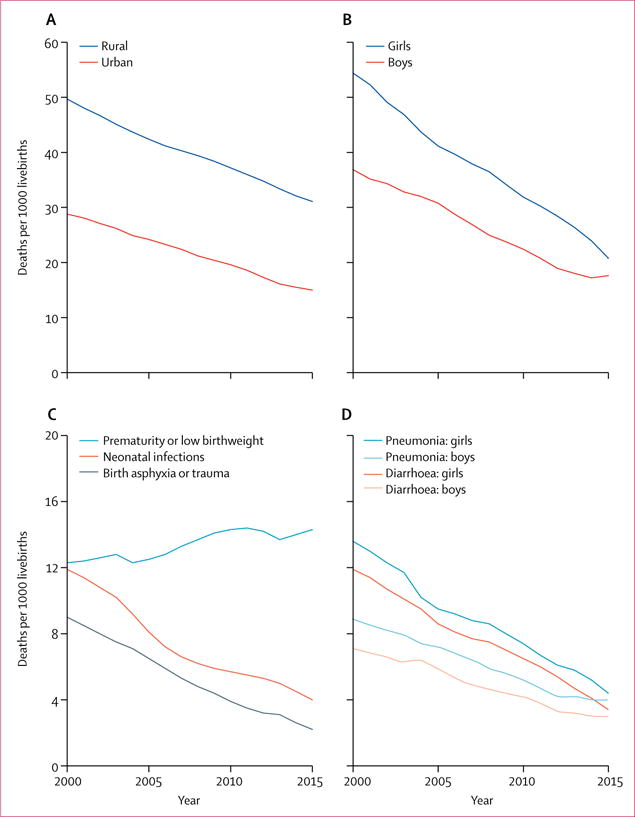
All-cause mortality rates for neonates by rural and urban residence (A) and those aged 1–59 months by sex (B). Cause-specific mortality rates for neonates (C) and 1–59 months by sex (D).
The absolute number of neonatal deaths from prematurity or low birthweight rose modestly from 342000 deaths in 2000 to about 370000 by 2015 (figure 2). With declines in other causes in neonates, prematurity or low birthweight are a rising proportion of a shrinking total. At ages 1–59 months, substantial decreases occurred in the absolute number of deaths from pneumonia, diarrhoea, and other infectious or nutritional conditions, but no demonstrable change occurred in the absolute number of deaths from non-communicable diseases and injuries.
Figure 2. Estimated deaths of children aged younger than 5 years in India, 2000–15.
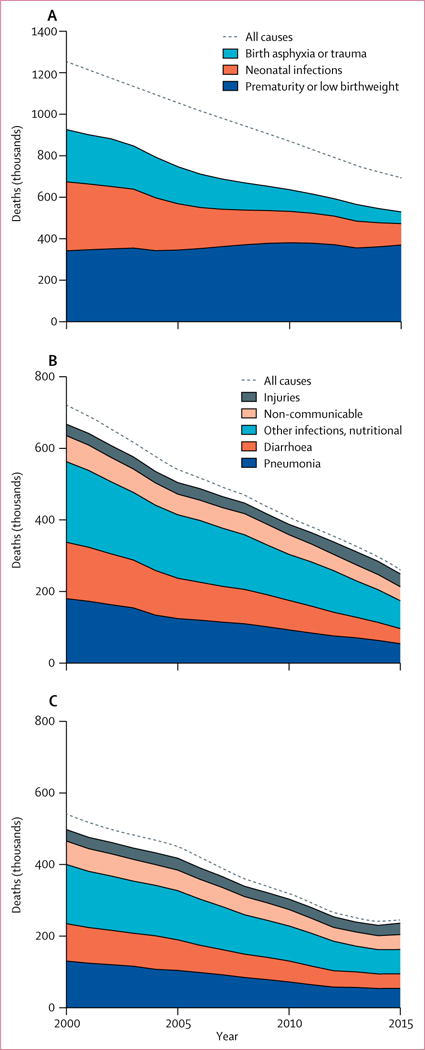
Neonates (A), 1–59-month-old girls (B), and 1–59-month-old boys (C).
Declines in mortality rates varied by urban or rural residence and state (figure 3). Neonatal infections and birth asphyxia or trauma fell in rural and urban areas and in richer and poorer states. Prematurity or low birthweight mortality rates rose in rural areas (from 13.2 per 1000 livebirths in 2000 to 17.0 per 1000 livebirths in 2015) and in poorer states (from 11.3 per 1000 livebirths in 2000 to 17.8 per 1000 livebirths in 2015), but fell in urban areas and in richer states. Prematurity or low birthweight deaths occurred less often on days 0–1 (when most birth asphyxia or trauma deaths occurred) than on other days. Infants dying from prematurity or low birthweight also had fever reported less often than did those dying from infection (data not shown). Most of the increase in prematurity or low birthweight deaths was in term births with low birthweight, not in preterm births (data not shown). The SRS records stillbirths, but their implied rates are probably underestimates.8,21 Declines in reported stillbirth rates correlated with declines in prematurity or low birthweight mortality rates in the poorer states (data not shown), consistent with the main increase being of term births with low birthweight. Pneumonia and diarrhoea mortality rates at ages 1–59 months fell substantially across rural and urban areas and richer and poorer states, but injury mortality rates did not decline, except slightly in richer states (figure 3). Hence, in urban and richer states, injuries are now killing about the same number of children as is diarrhoea at ages 1–59 months.
Figure 3.
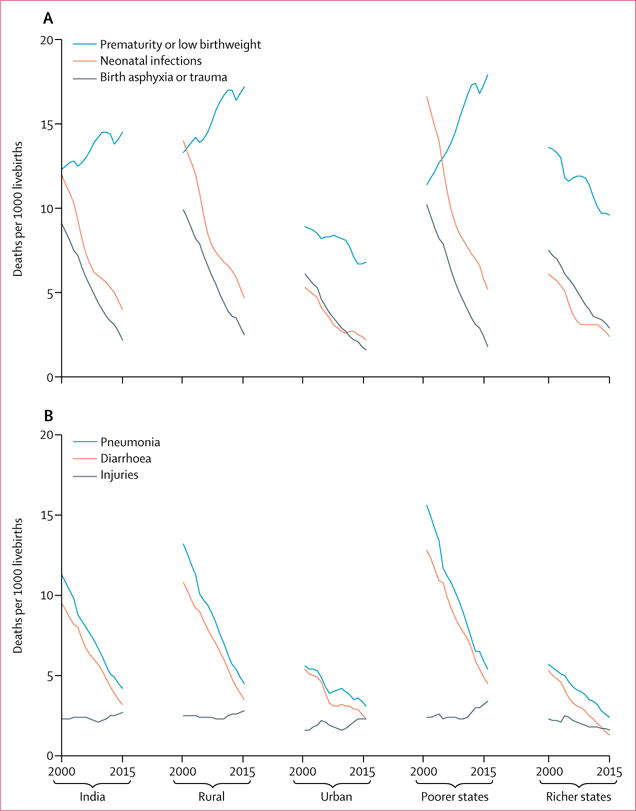
Cause-specific mortality rates for neonates (A) and those aged 1–59 months (B) by residence and poorer or richer state in India, 2000–15
We restricted analyses of state-specific declines in cause-specific mortality to the study years of 2001–13 when causes of death were directly collected (figure 4, appendix p 19). We observed quite marked variation in the trends in mortality rates from prematurity or low birthweight, with increases in Madhya Pradesh, Uttar Pradesh, Rajasthan, Bihar, Punjab, and Haryana, but declines in Odisha and Assam and most of the richer states. Birth asphyxia or trauma mortality rates fell surprisingly fast in Uttar Pradesh, Rajasthan, and Bihar. Thus, by 2013, these three states had slightly lower birth asphyxia or trauma mortality rates than did Delhi. Declines in 2001–13 mortality rates from diarrhoea conformed broadly to the expected patterns: higher baseline rates in the poorer states than in the richer states.
Figure 4. Cause-specific child mortality rates for selected causes in poorer and richer states of India, 2001–13.
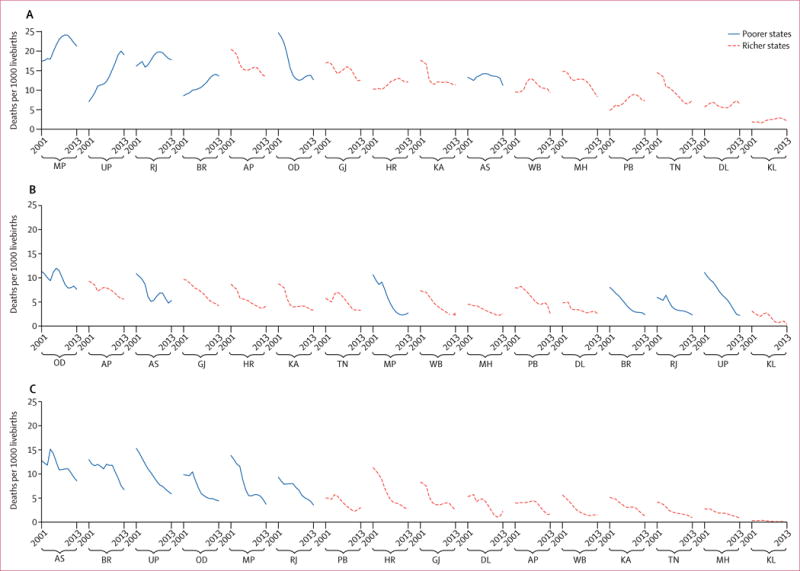
Neonatal prematurity or low birthweight (A), neonatal birth asphyxia or trauma for neonates (B), and diarrhoea for 1–59-month-old children (C). States are sequenced by their 2013 mortality rate. Jharkand, Chhattisgarh, and Uttarakhand are not included because the number of deaths for these states was too small for trends analysis. AP=Andhra Pradesh. AS=Assam. BR=Bihar. DL=Delhi. GJ=Gujarat. HR=Haryana. KA=Karnataka. KL=Kerala. MH=Maharashtra. MP=Madhya Pradesh. OD=Odisha. PB=Punjab. RJ=Rajasthan. TN=Tamil Nadu. UP=Uttar Pradesh. WB=West Bengal.
The faster declines in child mortality after 2005 (average annual decline of 3.4% for neonatal mortality and 5.9% for 1–59-month mortality) than before 2005 (3.2% decline in annual neonatal mortality and 4.5% decline in 1–59-month mortality) suggest that India has avoided about 1 million more child deaths than it would have at 2000–05 rates of progress (figure 5). If all states of India had achieved the declines seen in Tamil Nadu, Karnataka, and Maharashtra, nearly all states of India would have met the 2015 Millennium Development Goals.
Figure 5. Child deaths for all causes since 2000 in India.
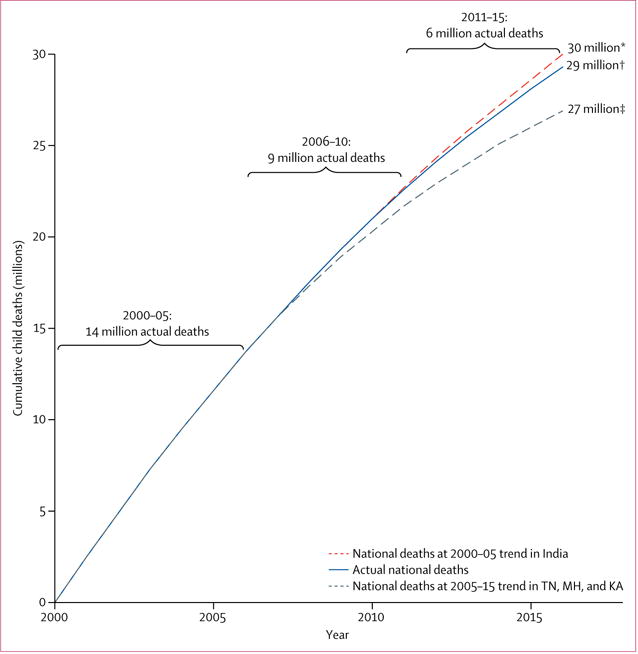
We calculated cumulative numbers of deaths for each scenario for 2000–15. 2000–05 covers 6 years, whereas 2006–10 and 2011–15 cover 5 years each. KA=Karnataka. MH=Maharashtra. TN=Tamil Nadu. *Estimated cumulative number of deaths had all of India followed its 2000–05 trend. †Estimated cumulative number of deaths by 2015. ‡Estimated cumulative number of deaths had all of India followed the average 2005–15 trend in KA, MH, and TN.
Discussion
Child mortality rates in India have substantially reduced since 2000, with the steepest decline in 2010–15. The 1–59-month decline exceeded the decline among neonates, driven by a nearly two-thirds reduction in the mortality rates from pneumonia and diarrhoea at ages 1–59 months. A steeper decline among girls has sharply narrowed the girl–boy gap in mortality rates at ages 1–59 months, which was prominent in previous analyses of 2001–03.7,15 Notably, almost equal numbers of boys and girls died in 2015. The rural–urban gap in 1–59-month mortality rates has also narrowed, but neonatal mortality is still substantially higher in rural than in urban areas.
About 1 million additional child deaths have been avoided in India since 2005. Although this study was not designed to attribute declines in specific causes to the NHM or any other programme, our results enable cause-specific analysis to guide future efforts. India’s next challenge is to meet the 2030 SDGs for child and neonatal mortality.20 Accomplishment of these goals will require an average annual decline from 2015 onwards of 4.1% in child mortality and 5.3% in neonatal mortality. We have shown a 3% or greater annual decline in all-cause mortality in those aged younger than 5 years of age in several subpopulations by sex, by urban or rural residence, across states, and from specific causes for 2010–15. By contrast, few subpopulations reached a 5% annual decline in all-cause neonatal mortality.
The biggest target to reduce neonatal mortality is prematurity or low birthweight deaths, especially in poorer states. Prematurity and low birthweight, and in particular, low birthweight, are strongly linked to largely modifiable maternal and prenatal factors, such as antenatal care, education, nutrition, anaemia, oral tobacco use, and other factors.22–24 India’s recently launched Newborn Action Plan25 will require specific attention to the early neonatal period, including ensuring early home visits for all births by a health professional and more intervention research for prematurity or low birthweight than has been done so far.22,26,27 We provide evidence of avoidability of these deaths: prematurity or low birthweight mortality rates fell in the richer and urban areas. Even poorer states, where safe delivery coverage has improved, saw substantial declines in birth asphyxia or trauma mortality rates.
At ages 1–59 months, about 225 000 annual deaths persist from pneumonia, diarrhoea, malaria, and measles. Immunisation schemes added pentavalent vaccine in 2015, rotavirus in 2016, and pneumococcal vaccine in 2017 and might enable continued progress in reduction of mortality due to pneumonia and diarrhoea. The eastern and northeastern states in particular need more effective malaria control than at present.28 Beyond the SDGs, our analyses suggest other plausible public health goals. In 2015, WHO declared that India had eliminated neonatal tetanus, meaning less than one case per 1000 livebirths. The 91% decline in the 1–59-month measles mortality rate meant that only 7000 deaths occurred in 2015 and a similar decline in the neonatal tetanus mortality rate meant that only 600 deaths occurred. Hence, elimination of deaths from both infections is now achievable.
Inherent uncertainties exist in classification of verbal autopsies. In particular, the declines in mortality rates from birth asphyxia or trauma occurred in many states concurrent with an increase in mortality rates from term births with low birthweight. However, use of dual physician coding and the distinct pregnancy length, day of death, and symptom patterns limited misclassification between these causes. Nonetheless, inevitably some misclassification within the major neonatal causes will have occurred, but such error has probably not changed over time, even as an increasing proportion of births occur in facilities compared with in homes. When mortality trends using the strictest definition were compared with those using all of the data, results were similar. The proportion of ill-defined deaths, which is a good test of the performance of verbal autopsy,12 remained low for both neonatal and 1–59-month deaths. Unlike the Global Burden of Disease,29 we retain ill-defined codes to provide a transparent check on the quality of overall cause of death systems. The MDS fieldwork missed some deaths, but we have taken into account possible undercounts by adjusting our totals to match IGME totals. Our assumption is that any missing deaths are distributed similarly to recorded deaths. Had the MDS missed many girl deaths, we would not observe a narrowing of the girl–boy gap in 1–59-month deaths.
The MDS reinforces the importance of direct measurement of causes of death. Indirect model-based methods, including the Global Burden of Disease29 and WHO’s Global Health Estimates,30 complement but do not substitute for annual nationally representative data for causes of death. Moreover, model-based estimates cannot separate trends due to changes in model assumptions from those due to actual changes in mortality rates.31 Forthcoming, more detailed analyses than this study of the MDS in partnership with the Indian Council of Medical Research should provide additional details of cause-specific mortality patterns in the country. Vital registration systems and medical cause of death reporting to document these basic data still need to improve in many countries in Africa and Asia.31,32 Direct mortality statistics are essential to plan strategies to meet the 2030 SDGs for child (and adult) health.33
Supplementary Material
Research in context.
Evidence before this study
We searched the PubMed, Embase, and Popline databases for original studies of mortality of children aged younger than 5 years in India published from Jan 1, 2000, to March 23, 2017, with no language restrictions. 32 studies reported mortality distribution for at least five causes and more than 100 deaths. The Registrar General of India Million Death Study (MDS) was the only source of directly measured causes at the national level. Small studies examined cause-specific mortality for home deaths in select states (n=16) or were limited to health facilities (n=9). Four model-based studies relied on MDS and facility-based data. None could distinguish whether trends in cause-specific mortality arose from changes in modelling assumptions or were due to actual changes in mortality.
Added value of this study
This study is, to our knowledge, the first to directly quantify cause-specific time trends for child deaths in India from 2000 to 2015. The variation in mortality rates by sex, urban and rural areas, and poorer and richer states also provides a crude assessment of the effect of the National Health Mission programmes. Our analyses show substantial declines in mortality rates at ages 1–59 months from pneumonia, diarrhoea, measles, and acute bacterial sepsis or severe infection and among neonates in rates from infection, birth asphyxia or trauma, and tetanus. However, mortality rates for prematurity or low birthweight rose (mostly comprising term births with low birthweight) modestly in rural areas and poorer states. The rates of progress for various conditions help identify pathways to and challenges for achievement of the 2030 Sustainable Development Goals (SDGs).
Implications of all the available evidence
India has avoided about 1 million child deaths since 2005, but could have feasibly avoided about 3 million if national progress matched that achieved by some states. Continued rapid progress in neonatal and 1–59-month mortality is required to achieve the SDGs. Specific attention to low birthweight births is required. Our MDS helps to define feasible public health goals, such as a reduction in the 225 000 deaths at ages 1–59 months from pneumonia, diarrhoea, malaria, and measles. Elimination of measles and tetanus deaths is also achievable. Direct monitoring of changes in causes of death with use of nationally representative studies continues to be essential to achievement of the SDGs for child (and adult) mortality.
Acknowledgments
The Registrar General of India established the Sample Registration System in 1971, has continued it ever since, and is collaborating with several of the authors. The academic partners in India (Million Death Study Collaborators) planned the Million Death Study in close collaboration with the Office of the Registrar General of India. External funding is from the Fogarty International Center of the National Institutes of Health (grant R01 TW05991-01), Dalla Lana School of Public Health of the University of Toronto, Maternal and Child Epidemiology Estimation Group, and Disease Control Priorities Network. The opinions expressed in this paper are those of the authors and do not necessarily represent those of the Government of India, WHO, or the UN.
Footnotes
Contributors
PJ conceived the Million Death Study. PJ, RK, SA, and RR conceived the child mortality study and provided overall guidance. The Registrar General of India collected data. SAF and WS analysed the data. SAF, RR, HG, and PJ interpreted the data and wrote the initial drafts. PG, UR, and FR provided complementary demographic or survey data. SAF and LN did the literature review. All other authors reviewed results, reviewed the drafts, and contributed to the report.
Declaration of interests
PJ is supported by the Canada Research Chair Programme and the University of Toronto. All other authors declare no competing interests.
References
- 1.You D, Hug L, Ejdemyr S, et al. Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet. 2015;386:2275–86. doi: 10.1016/S0140-6736(15)00120-8. [DOI] [PubMed] [Google Scholar]
- 2.UN Population Division. World population prospects: the 2015 revision. New York: United Nations; 2015. [Google Scholar]
- 3.UN. Transforming our world: the 2030 agenda for sustainable development. New York: United Nations; 2015. [Google Scholar]
- 4.Government of India, Ministry of Health and Family Welfare. National rural health mission: meeting people’s health needs in rural areas, framework for implementation 2005–2012. New Delhi: Government of India, Ministry of Health and Family Welfare; 2005. [Google Scholar]
- 5.WHO. Global health expenditure database. http://apps.who.int/nha/database/Select/Indicators/en (accessed July 13, 2017)
- 6.Centers for Disease Control and Prevention. Progress in implementing measles mortality reduction strategies—India, 2010–2011. Morb Mortal Wkly Rep. 2011;60:1315–19. [PubMed] [Google Scholar]
- 7.Ram U, Jha P, Ram F, et al. Neonatal, 1–59 month, and under-5 mortality in 597 Indian districts, 2001 to 2012: estimates from national demographic and mortality surveys. Lancet Glob Health. 2013;1:e219–26. doi: 10.1016/S2214-109X(13)70073-1. [DOI] [PubMed] [Google Scholar]
- 8.Registrar General of India. Sample Registration System statistical report 2015. New Delhi: Office of the Registrar General of India; 2016. [Google Scholar]
- 9.Jha P, Jacob B, Gajalakshmi V, et al. A nationally representative case-control study of smoking and death in India. N Engl J Med. 2008;358:1137–47. doi: 10.1056/NEJMsa0707719. [DOI] [PubMed] [Google Scholar]
- 10.WHO. ICD-10: international statistical classification of diseases and related health problems 10th revision. Geneva: World Health Organization; 1992. [Google Scholar]
- 11.Jha P, Gajalakshmi V, Gupta PC, et al. Prospective study of one million deaths in India: rationale, design, and validation results. PLoS Med. 2006;3:e18. doi: 10.1371/journal.pmed.0030018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aleksandrowicz L, Malhotra V, Dikshit R, et al. Performance criteria for verbal autopsy-based systems to estimate national causes of death: development and application to the Indian Million Death Study. BMC Med. 2014;12:21. doi: 10.1186/1741-7015-12-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ram U, Dikshit R, Jha P. Level of evidence of verbal autopsy. Lancet Glob Health. 2016;4:e368–69. doi: 10.1016/S2214-109X(16)30045-6. [DOI] [PubMed] [Google Scholar]
- 14.Patel V, Ramasundarahettige C, Vijayakumar L, et al. Suicide mortality in India: a nationally representative survey. Lancet. 2012;379:2343–51. doi: 10.1016/S0140-6736(12)60606-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Million Death Study Collaborators. Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet. 2010;376:1853–60. doi: 10.1016/S0140-6736(10)61461-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris SK, Awasthi S, Khera A, et al. Rotavirus mortality in India: estimates based on a nationally representative survey of diarrhoeal deaths. Bull World Health Organ. 2012;90:720–27. doi: 10.2471/BLT.12.101873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mari Bhat PN. Completeness of India’s sample registration system: an assessment using the general growth balance method. Popul Stud (Camb) 2002;56:119–34. doi: 10.1080/00324720215930. [DOI] [PubMed] [Google Scholar]
- 18.Gerland P. UN Population Division’s methodology in preparing base population for projections: case study for India. Asian Popul Stud. 2014;10:274–303. [Google Scholar]
- 19.UN Inter-agency Group for Child Mortality Estimation. Levels and trends in child mortality: report 2015. New York: United Nations Children’s Fund; 2015. [Google Scholar]
- 20.Jha P, Laxminarayan R. Choosing health: an entitlement for all Indians. Toronto: Centre for Global Health Research; 2009. [Google Scholar]
- 21.Jha P, Kumar R, Vasa P, Dhingra N, Thiruchelvam D, Moineddin R. Low female-to-male sex ratio of children born in India: national survey of 1.1 million households. Lancet. 2006;367:211–18. doi: 10.1016/S0140-6736(06)67930-0. [DOI] [PubMed] [Google Scholar]
- 22.Lassi ZS, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst Rev. 2015;3:CD007754. doi: 10.1002/14651858.CD007754.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suliankatchi RA, Sinha DN. The human cost of tobacco chewing among pregnant women in India: a systematic review and meta-analysis. J Obstet Gynaecol India. 2016;66:161–66. doi: 10.1007/s13224-015-0821-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sebastian T, Yadav B, Jeyaseelan L, Vijayaselvi R, Jose R. Small for gestational age births among south Indian women: temporal trend and risk factors from 1996 to 2010. BMC Pregnancy Childbirth. 2015;15:7. doi: 10.1186/s12884-015-0440-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Government of India, Ministry of Health and Family Welfare. India newborn action plan. New Delhi: Government of India, Ministry of Health and Family Welfare; 2014. [Google Scholar]
- 26.Fadel SA, Ram U, Morris SK, et al. Facility delivery, postnatal care and neonatal deaths in India: nationally-representative case-control studies. PLoS One. 2015;10:e0140448. doi: 10.1371/journal.pone.0140448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sankar MJ, Neogi SB, Sharma J, et al. State of newborn health in India. J Perinatol. 2016;36:S3–8. doi: 10.1038/jp.2016.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dhingra N, Jha P, Sharma VP, et al. Adult and child malaria mortality in India: a nationally representative mortality survey. Lancet. 2010;376:1768–74. doi: 10.1016/S0140-6736(10)60831-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Global Burden of Disease Pediatrics Collaboration. Kyu HH, Pinho C, et al. Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: findings from the Global Burden of Disease 2013 Study. JAMA Pediatr. 2016;170:267–87. doi: 10.1001/jamapediatrics.2015.4276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO. Global health estimates for 2000–2015: cause-specific mortality. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html (accessed Feb 27, 2017)
- 31.Jha P. Reliable direct measurement of causes of death in low- and middle-income countries. BMC Med. 2014;12:19. doi: 10.1186/1741-7015-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385:430–40. doi: 10.1016/S0140-6736(14)61698-6. [DOI] [PubMed] [Google Scholar]
- 33.Grove J, Claeson M, Bryce J, et al. Maternal, newborn, and child health and the Sustainable Development Goals—a call for sustained and improved measurement. Lancet. 2015;386:1511–14. doi: 10.1016/S0140-6736(15)00517-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


