Abstract
Significant progress has been made during the past decade towards the clinical adoption of cell-based therapeutics. However, existing cell-delivery approaches have shown limited success, with numerous studies showing fewer than 5% of injected cells persisting at the site of injection within days of transplantation. Although consideration is being increasingly given to clinical trial design, little emphasis has been given to tools and protocols used to administer cells. The different behaviours of various cell types, dosing accuracy, precise delivery, and cell retention and viability post-injection are some of the obstacles facing clinical translation. For efficient injectable cell transplantation, accurate characterisation of cellular health post-injection and the development of standardised administration protocols are required. This review provides an overview of the challenges facing effective delivery of cell therapies, examines key studies that have been carried out to investigate injectable cell delivery, and outlines opportunities for translating these findings into more effective cell-therapy interventions.
Introduction
Significant progress has been made during the past decade towards the clinical adoption of cell-based therapeutics. Pre-clinical studies have translated into clinical trials for conditions of the central nervous system (CNS), including Parkinson’s disease (PD),1 Huntington’s disease,2 amyotrophic lateral sclerosis (ALS)3 and stroke.4, 5 Clinical trials have focused on the delivery of purified cellular suspensions, for example, in spinal cord injuries and stroke.6–8 However, existing cell-delivery approaches have shown limited success, with numerous studies showing fewer than 5% of injected cells persisting at the site of injection within days of transplantation.
One of the main translational challenges to the implementation of injection-based cell therapy is the need to determine suitable delivery protocols to ensure sufficient accuracy, improved cell survival and reproducibility in administering cells for therapeutic efficacy.9 In this review, we identify critical considerations for the various stages of cell administration, outline studies that have measured functional performance of injected cells and discuss criteria for designing cell-delivery devices for minimally invasive cell therapy. The various approaches used to attempt to maximise cell viability and functionality in high accuracy cell-therapy applications are also described. We suggest that if the variables linked to optimal cell, survival can be recognised, cell loss may be reduced and efficacy of cellular therapies can be improved.
Cells as therapeutic agents: translational barriers in neurological applications
Three stages make up a typical cell-therapy procedure: (1) in vitro preparation of cell suspensions; (2) injection procedure; and (3) retention of the administered cells post-injection.10 Focusing on one stage only can yield optimised settings that are not favourable to the entire procedure, and therefore it is essential that a systematic investigation considers all three stages to outline optimal transplantation parameters (Fig. 1).
Fig. 1.
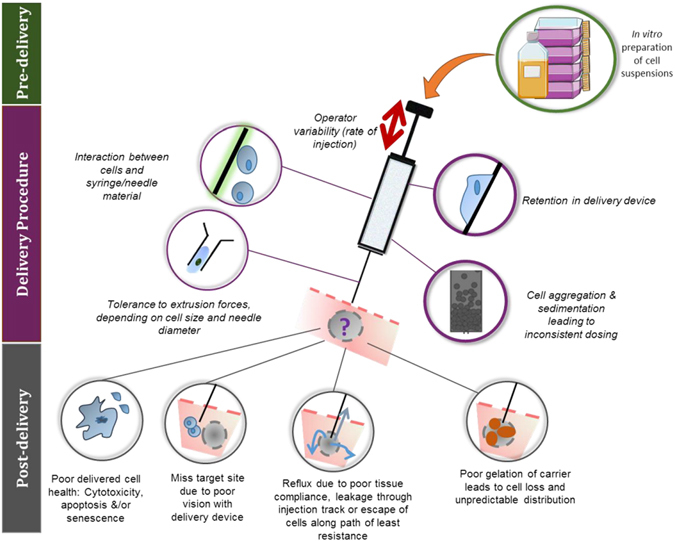
Common problems with injectable cell delivery and possible cell fates. Three stages make up a typical cell-therapy protocol: in vitro preparation (pre-delivery), injection (delivery) and subsequent retention (post-delivery) of injected cells
Cell loss has been reported to be observed post-transplantation,11, 12 with quantified survival rate of transplanted cells as low as 1%.13 Moreover, a large number of cells that have been originally retained die, possibly due to exposure of cells to the inflammatory microenvironment, washout, immune destruction, dispersion through impaired local vascular system,14, 15 apoptosis and anoikic cell death.16 Variable clinical outcomes observed in two trials for PD1, 17 have been partially ascribed to a failure to properly distribute cells to the target site.18 Attaining efficient delivery of an adequate number of cells without loss of functionality is therefore a key step in the development of regenerative medicine approaches.
The diverse behaviours of various cell types, choice of dosing density, administration protocol and cell viability post-injection are some of the obstacles facing clinical translation. This section will explore the various variables involved in the three stages of cell-therapy procedures.
Pre-delivery factors: scaling up pre-clinical models to human therapy
To overcome low cell transplantation efficiency, one popular approach to translational scale-up has been to deliver a large number of cells to a single site19 with doses ranging up to hundreds of millions of cells.19 This makes cell-therapy approaches technically complex and expensive, as well as offering limited control over site-specificity, as cells will potentially migrate to other sites.20
Determination of cell density. In cell transplantation studies, cell concentration within suspensions is often reported, with suspensions of over 100,000 cells/μL considered highly concentrated.21 As well as higher costs of cell processing, these suspensions can be viscous and may cause needle clogging and uneven injection flow. Moreover, as cell size varies widely, depending on the site or species of origin, the maximum concentration suspended within a certain volume will therefore vary. Hence, it is more accurate to express the cellular component as a volume fraction, which is the volume occupied by the cell fraction in a certain volume of suspension vehicle, as described by Rossetti et al.10
High-density cell suspensions may lead to cell death, attributable to limited oxygen and nutrient diffusion.22 The limited capacity to generate appropriately large numbers of standardised cells routinely, within a limited time frame, whereas adhering to quality standards has also led to small clinical trials. In addition, large doses of administered cells also pose higher safety risks of tumorigenesis23 and micro-embolism.24 Moreover, higher injected cell concentrations result in exposure to increased shear forces,25 yet may have a reduced tendency for sedimentation.10
No agreement exists regarding the optimal cell number to be transplanted, although this is likely to vary depending on cell type, disease and administration route. For example, 3–5 × 107 cells/kg mesenchymal stem cells (MSCs) were administered per multiple sclerosis patient,26 whereas in spinal cord injury, 5–6 × 106 cells/kg have been transplanted intrathecally.27 Taguchi et al.28 reported that the higher dose of 3.4 × 108 cells gave improved neurologic outcomes than the lower dose of 2.5 × 108 cells administered intravenously. A lower percentage loss of MSCs was exhibited with increasing concentrations being administered, possibly due to the finite number of cells being able to attach to the available inner surface of the device.29 However, a phase II trial using 5–10 million NT2N cells in stroke patients showed that patients receiving the lower dose performed better.4 A recent study also demonstrated that a suitable cell dose, rather than a higher one, can better aid the repair of injured tissue in stroke patients.30
Cell suspension vehicle. Suspension vehicles have been found to affect the viability of cells pre-delivery and their survival upon implantation.10, 31, 32 Preparing a cell suspension that maintains a homogeneous distribution and viability is essential to ensure effective clinical translation. Results suggested that MSCs viability is reduced to levels significantly below the permitted limit of 70% in a short time when stored in parenteral solutions, with other biological functions being slightly affected.31 Cells at different temperatures will also have different requirements for storage solutions.33
Injection volume. The human brain is 800–2300 times larger than that of rodents used for pre-clinical research.34 To enable scale-up to larger target volumes, cell distribution can be increased by making multiple, lower volume injections for improved engraftment.14 The adjustment of the needle/catheter for adequate cell distribution can lead to multiple needle tracks and entry points. Multiple transcortical brain penetrations have been used for a range of clinical trials.1, 17, 35 This is a cause for concern, as each penetration carries a risk of intracranial haemorrhage22 and damage to white matter tracts.
The shortage of human studies with lesion volume calculations, such as occur in human spinal cord injuries,36 make it challenging to decide on optimal injection volumes. A study by Gutierrez et al.37 evaluated the spinal cord’s tolerance to varying numbers and volumes of cell injections in Göttingen minipigs. Complete functional recovery was achieved by 2 weeks, even when injection volume and numbers were increased. However, histological analysis revealed tissue damage when large volumes (50 µL) of cell suspension were injected per site. Although increased numbers of injections did not cause an increase in tissue damage there was an optimal number of injections required to achieve the best engraftment.
In many clinical trials, doses are extrapolated from data of pre-clinical animal studies. Depending on how they are calculated, doses of 100 million or more cells may result in substantial volumes being required. Thus, it is vital that detailed dosing studies are carried out in animal models to establish the minimum effective and maximum tolerated doses.38
Cell-delivery challenges
Cell injector system design requirements and challenges. The main delivery platform for cell-based therapeutics has traditionally been a needle and syringe,39 with cell preparations delivered either systemically or directly.40 Although many clinical trials have used syringe/needle systems without cannulas,41–44 CNS cell transplantation trials have typically utilised a frame-based platform for the insertion of a stereotactically guided straight cell-delivery cannula or needle.1, 2, 17, 22, 35, 44–46 There is a growing recognition that conventional needle-based and catheter-based cell transplantation tools have considerable inadequacies that may affect clinical translation.47, 48 Insufficient pre-clinical testing of surgical tools and methods for cell delivery to the human brain and spinal cord may result in the failure of cell transplantation trials, despite the reliability of the basic biological concepts.49–51 Key considerations for clinical translation of cell-delivery devices include ease of loading and use, reproducibility of delivery, possibility of sterilisation, freedom from leachable and/or extractable contaminants, and ensuring no visual obstruction through a surgical microscope in high accuracy applications.
Role of mechanical forces The mechanical forces that cells experience as they pass through the injection device is a factor influencing their subsequent viability and functionality post-transplantation. To comprehend the fluid dynamics in action, we must explore the mechanical forces exerted on the cells.
While flowing through a needle, cells may experience several types of mechanical forces, comprising shear forces characteristic of linear shear flow, a pressure drop across the cell and extensional (stretching) forces.52 The nature of flow, whether laminar or turbulent, should be confirmed at the ejection rate and syringe/needle size used for the transplantation procedure. This can be verified through the calculation of Reynold’s number (R e), which determines flow conditions (transitional level to turbulence is R e = 2100):
where ρ is the carrier fluid density (water at room temperature=999.97 kg/m3), Q is volumetric flow rate (mL/min), D is needle diameter and η is dynamic viscosity of the medium. Given that the flow is laminar, the velocity profile is parabolic across the diameter (Fig. 2a), with maximum velocity at the centre of the lumen. Cells and fluid in the middle of a cannula flow at a different velocity to those at the walls. This difference in velocity exposes cells to shear stress.25 Changes in shear rate and shear stress have been suggested to affect cell viability and function.52 Shear stress (τ) is calculated by Poiseuille’s equation,
where τ max is shear stress (dyn/cm2); Q is flow rate (cm3/s); η is dynamic viscosity of the medium; and R denotes needle radius. The magnitude of shear stress is maximal at the walls of the syringe/needle, zero at the centre and changes linearly with distance between those two. Even low levels of shear stress (10 dynes/cm2) have been stated to have a major influence on the activation of molecular cascades.53, 54 Any change in the system’s geometry, such as the sudden tapering of a syringe to the needle, can also result in cells experiencing extensional flow, an increase in velocity and, consequently, high shear.55 The range of shear stress values generated by clinicians may exceed physiological values. As a useful reference, average wall shear stress is 1–6 dyn/cm2 for venous circulation and 15 dyn/cm2 for arterial circulation.56, 57 However, previous reports have also stated that low shear forces of 3.5 58 and 15 dyn/cm2 59 can influence cells. Previous work has concluded that cell damage is based on the extent of shear stress as well as exposure time to zones of shear.25, 60 Damage may also occur due to collisions with the stationary surfaces of the device.61 Complete damage of the cell may not necessarily be the only adverse result. Investigations carried out on erythrocytes have shown that excessive stretching or deformation of the cell membrane might result in loss of function.62 Extensional flow also causes cells to experience stretching and deformation, leading to cell death.63, 64 A larger difference between diameters of the syringe and needle will result in larger extensional forces, whereas a longer needle will increase the time a cell is exposed to extensional forces. In addition, cell aggregation may intensify shear stress experienced by cells during delivery. Forces acting on cells during their administration may have two effects: cell destruction along with stretch pre-conditioning.65
Fig. 2.
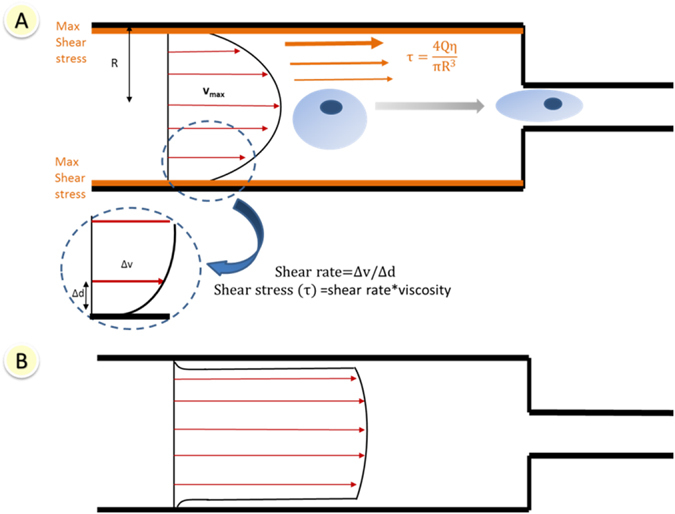
Schematic of a section of a syringe/needle lumen of radius R. a Shear stress and velocity distribution in delivery device for Newtonian fluid and laminar flow. The velocity profile across the diameter is parabolic. Shear stress (τ) is zero at the centre and increases linearly to its maximum value at the wall. As a cell flows from the syringe to the needle, it will experience increasing velocities along its length, causing it to stretch. b Plug flow behaviour—flow velocities are almost equal across the whole diameter. Shear-thinning materials display this behaviour when their flow in a capillary reaches a steady state
Biomaterial-assisted cell delivery (reviewed in detail in ‘Biomaterial-assisted delivery’ section) has the potential to mediate the impact of mechanical forces during cell delivery. Shear-thinning hydrogels are injectable materials that exhibit a viscosity decrease under shear strain; the viscosity returns to normal when the shear is removed. Shear-thinning materials typically display plug flow behaviour when their flow within a capillary reaches a steady state. They exhibit a central wide region, where material and cells experience little or no shear rate and a narrow zone of shear adjacent to the walls (Fig. 2b).
Needle characteristics Critical parameters in injectable cell delivery include needle characteristics and/or diameter of the tubing used.50 Needle characteristics include inner and outer diameters, length, stiffness and bevel design. Deep subcortical target structures, such as the caudate nucleus or corpus striatum, require a long, thin needle/cannula of sufficient rigidity to penetrate to the target site without injuring the overlying structure. This cannula can be 19 cm or more. Shorter needles (8–10 cm) would require direct brain exposure, which is more invasive.50
Various needle gauge sizes have been used for neurological applications, typically starting from 25 G.45, 66 Devices with needle sizes of 30 G have been developed for CNS applications,51, 67 and 30–34 G are typically used for applications requiring high accuracy.68, 69 However, smaller bore size needles, e.g.: 27–34 G, are more prone to obstruction by concentrated cell suspensions, especially when successive injections are required. Smaller gauge needles cause less tissue trauma, minimise leakage through the track created by needle insertion, and have been suggested to reduce gliosis.70 Mehta et al.71 reported a 53% headache rate with the use of a 22 G needle in neurological patients, and suggested that this high incidence could be caused by the large-bore spinal needle, which was used to prevent mechanical damage to the infused cells. Karussis et al.72 also reported a high incidence of headache with MSCs in multiple sclerosis and ALS patients, attributing this to the lumbar puncture itself; needle size was not reported. Care should be taken to choose the correct needle size that accounts for cell type, injection speed, site of transplantation and the viscosity of the suspension. Veraitch et al.73 reported that 45 passages through a bore of 500 µm diameter were needed before a significant reduction in viability was detected. Longer, finer needles have resulted in the delivery of a smaller volume50 and a lower percentage of the cell dose administered.60 However, loss of cell viability resulting from the use of smaller needle gauges was not substantial.25, 60, 74 Faster acceleration of fluid and cells within longer needles may be more prone to clogging, perhaps because there is less time for cells to dislodge from transient adhesions to other cells and the injector.50 Bevel angle and length may also influence injectate dispersion and direction.
Material employed for construction of delivery device Recent studies have shown that cells may be retained in the delivery device,60, 75 with this effect being more pronounced in glass cannulas than in metal.75 Whether the adherence of the cells to the walls of the syringe/cannula is due to chemical, physical or charge effects has not been studied, but all of these might possibly be manipulated to decrease adhesion and settling.75 In addition, coating the inner surface of the needle/catheter with proteins may reduce cell adhesion to the device.76 In addition to possible adherence to device materials, cells may encounter residual trace amounts of manufacturing agents that could induce apoptosis or undesired differentiation. The use of hydrophilic and siliconised coatings on internal walls of the cannula has also been suggested to decrease friction between the needle and tissue in vivo.75 Although glass cannulas present several advantages, including higher precision and minimal penetration injuries,21 glass may not be sufficiently rigid to endure injection pressure. Novel materials such as electroactive polymers and magnetorheological elastomers77 show promise for the development of tailored needles whose rigidity could be adjusted by current, magnetic field or temperature.
Sedimentation Uniformity of cell dosing may be affected by aggregation or sedimentation of cells in suspension over time, with clumping of cells being found to affect cell viability.78 The possibility of cell sedimentation during the course of the surgical procedure, especially in large diameter needles/cannula,75 and the potential for inconsistent cell dosing needs to be considered in designing cell-therapy protocols, particularly given that orientation will vary depending on application. In vertical cannulas, cells sediment towards the tip of the needle, with most cells appearing in the first 10–20% of the injectate. In horizontal cannulas, settling and adherence of cells on the side caused most of the cell dose to emerge in the final 10–20% of injectate75; similar effects of cell dose retention have been reported.74 A suspension medium should preferably have a density of ~2 g/cm3 and a viscosity >3 cP to reduce cell settling at 20–40% cell volume fraction.10 Negative impacts of cell sedimentation observed post cell therapy include graft-induced dyskinesias in PD trials which may have occurred due to formation of dopamine ‘hot spots’ in the brain, resulting in abnormal activation of neural circuits.79 Moreover, some cells, such as neural progenitor cells (NPCs), have a natural tendency to form clusters that may settle at the tip of the needle.50 Therefore, it is essential to maintain an even cell suspension using agitation or other approaches.
Administration protocols. As cell injections for neurological injuries move on to extensive clinical testing, procedural standardisation is necessary to reduce the probability of technical failures and measure the effects of interventions on patient outcome and other endpoints (e.g. injection-associated trauma, graft survival). Clinical trial design to enhance the final number of cells that integrate within the diseased tissue will require re-examining the current lack of optimisation of transplantation protocols. For a given clinical trial, optimum factors for cell implantation are normally estimated from pre-clinical research or the investigator’s judgement.80 Administration protocols will vary depending on cell type, disease and administration route. While inappropriately administered cells may in most cases result in no functional impact, in some cases, transplanted cells may result in undesirable side effects.
Injection rate Injection rates employed in clinical trials for cell injection are inconsistent. For neural cell transplantation, for instance, studies have used a rate of 5 µL/min,81 compared to 300 µL/min for spinal injury,82 and between 10 and 1000 µL/min for stroke.7, 83, 84 Rate of injection has been shown to be potentially vital in cellular delivery.50, 60, 74
Although small volume injections may be made over extended periods in the laboratory, clinical injections must be made within limited surgical duration. It has been suggested that delivering the required volume over a longer time will potentially reduce mechanical forces acting on the cells and the creation of damaging pressure gradients21; delivery of 44 nL in 5 min was linked to good tissue preservation.85 However, such a rate would be impractical, with 1 μL requiring over an hour to deliver. Notably, brain microinjections in rats at a rate >1 μL/min have been linked to tissue damage.86 Recently, intracarotid transplantation of glial-restricted precursors (GRPs) and MSCs through a microcatheter at an infusion rate of ≥1 mL/min resulted in stroke in 27/44 rats, even with a vehicle-only infusion. A lower rate (0.2 mL/min) was safe for the infusion of both vehicle and GRPs.87 Moreover, at high flow rates, backflow along the catheter shaft may occur if the applied force is removed from the plunger and affect delivery. It was determined that backflow can be avoided in grey matter with a 32 G catheter at rates <0.5 µL/min in a rat model.88 However, injection at a slow rate may lead to a lower percentage of the cell dose being delivered, higher apoptosis levels and influence the immunophenotype of delivered cells.60, 74
Cells employed Optimal injection parameters will vary depending on the morphological, physiological and growth characteristics of each cell type. Thus, it is not surprising that preparation and ejection protocols optimised for one type of cells are not necessarily applicable to others.32, 60, 74 When studying injection rates, smaller NIH-3T3 cells had an optimum ejection rate of 150 µL/min, whereby the maximum percentage of viable cell dose was delivered,60 whereas the relatively larger BMSCs had an optimal ejection rate of 300 µL/min.74 Some cell types, such as MSCs, may be especially disposed to clumping, leading to blockage of flow within the needle,49 whereas other cell types, e.g. NSCs, are sensitive to manipulation and undergo apoptosis easily. During handling, MSCs were observed to have a greater inclination than NPCs to come out of suspension and form tight clusters.49
Tissue compliance If injections are made into cavities, larger volumes can be introduced without generating large pressure gradients if fluid drainage from the cavity is adequate, i.e. match injection to lesion volumes.89, 90 Hydrodynamic injury will occur if intraparenchymal pressure surpasses the tensile limits of the parenchyma. Given that many microsyringes are manufactured to tolerate 1000 psi or more before failure, the likelihood of producing large tissue pressures during injection exists. Larger injection volumes also worsen the reflux of infused materials along the penetration tract,91 making cell dosing unpredictable in terms of numbers and final location, and contributing to injection-related injury.21 The low elastic modulus of brain tissue also provides little resistance to reflux of infusions.34
Post-delivery complications: functional performance of injected cells
Given the number of clinical trials that use needle-based systems or catheter-based systems for cell delivery, surprisingly few studies have focused on the impact of small-bore needle injection on cell function. Transplantation studies have focused on the outcome of the trial rather than the variables that affected results. Investigating viability and potency of transplanted cells at the time of delivery is crucial, as a small level of cell death within a concentrated cell population could have a significant effect on the remaining viable portion through the release of cytotoxic agents.92 To date, research has been carried out to evaluate the impact of injection on cell functionality.25, 29, 50, 52, 93–96 Studies have highlighted parameters needed to achieve an adequate cell density for therapy, such as the period between cell preparation and implantation,97 injection rate, needle length and bore size50 and cell concentration.70, 98
There has been wide variability in how the effects of delivery devices on cell performance are assessed. Therefore, it is vital to develop standardised assays to consistently characterise cellular therapy products. Discrepancies in the employed delivery devices and administration methodologies has complicated comparisons and led to contradictory results. This is illustrated in Table 1, with some studies demonstrating that cell manipulation through a needle did not significantly affect viability,25, 93, 95 whereas other studies show that it did exert a significant effect.94 In one study, ejection of NIH-3T3 cells at 150 µL/min exhibited the optimal percentage of dose delivered,60 whereas another study on hMSCs74 showed an optimal recovery at the highest flow rate under investigation (300 µL/min). A study by Heng et al.29 showed reduced cell recovery at the higher flow rate (1600 µL/min), with large variation in their samples.
Table 1.
Overview of investigations carried out to assess the effects of various injection parameters on cell viability and functionality
| Aim of study | Experimental design | Cell type | Syringe and needle | Flow rate(s) and other parameters | Brief description of results | Assays for assessment of cellular health | Refs. | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Viability | Apoptosis | Senescence | Others | |||||||
| Viability after cell transfusion: various needles and flow rates | In vitro | Bone marrow-derived mono-nuclear cells | Automatic injection pump and 16, 18, 22 G needles | 1 and 0.5 mm/s | No difference detected in viability ratios | √ | × | × | × | 95 |
| Changes in hMSCs by transcatheter injection | In vitro | hMSCs | 1-mL syringe and 26 G (155 cm) Nitinol needle | 400 or 1600 µL/min | Viability not affected by varying rate. Slightly altered gene expression, but effects not translated into significant differences in protein production | √ | × | × | Clonogenicity, gene expression profile and cytokine secretion | 29 |
| Response after manipulation in narrow-bore syringe system | In vitro | Murine MSCs | 10 μL syringes and 26, 25 or 22 G needles | Drawn up at 30 μL/min; ejected at 20, 5 and 1 μL/min; time within syringe | Needle bore size and time within the syringe affected viable cell density | √ | √ | × | Cell attachment and spreading | 94 |
| Effect of delivery via needles and catheters at multiple flow rates | In vitro | Rat and human MSCs | 20, 25 and 30 G needles, and SL-10 microcatheter | 60, 120, 240 and 500 mL/h | No significant effect on viability (>70%). Delayed drop in viability at 24 h. No change in cell surface markers or function | √ | √ | × | Immunophenotyping and multilineage differentiation | 25 |
| Small-bore size to deliver single/multiple cell injections | In vitro and in vivo (IV by tail vein injection) | hMSCs | 24, 25 and 26 G needles and 1 mL syringe. Multiple injections (10×): 26 G needle and 1 mL syringe | 2000 μL/min | 26 G needles can be safely used. Multiple injections were non-detrimental to cells (kept functional characteristics) | √ | × | √ | Morphology, immunophenotyping, trilineage differentiation, in vivo migration | 93 |
| Impact of manual handling procedures | In vitro | Mouse ESC cell lines | 20 mL syringes: one containing cell suspension, luer-locked to stainless steel capillary (500 µm D, 1 cm L) | Pass cells between syringes at 0.80 mL/s. Centrifugation: 300×g, 600×g and 1000×g.Inoculation cell density | Gentle cell handling and minimal variations in environmental conditions needed to maintain viability. Inoculation density and time exposed to ambient conditions impacted phenotype. | √ | × | × | Phenotyping | 73 |
| Impact of injection parameters in automated delivery for the brain | In vitro | Neural progenitor cells and bone marrow stromal cells | Automated injection device; 250 µL syringes with 20 G and 27 G needles, 3.8 or 15.2 cm in length | Flow rate of 1 µL or 10 µL/s; initial acceleration rate of 42 or 208 µL/s2.Delay between loading and injection | Longer, thinner cannulas and greater cell concentrations were harmful for delivery | √ | × | × | × | 50 |
| Effect of DMSO, cell density and needle size on viability in 3D hydrogels | In vitro | NIH-3T3 cells | 27 G needle | — | Viability of cryopreserved cells was significantly lower than freshly collected cells. Needle significantly reduced cell survival rates. Higher DMSO concentration and cell density lowered survival | √ | × | × | × | 96 |
| Effect of varying ejection rate, cell density and needle gauge on cell health | In vitro | NIH-3T3 cells | 30 and 34 G needles attached to 100 µL syringes | Drawn up at 300 µL/min, and ejected at 20–300 µL/min controlled using a syringe pump | Ejections at 150 μL/min resulted in highest percentage of dose delivered. Difference in proportions of apoptotic cells 48 h post-ejection was higher at slower rates | √ | √ | √ | Cytotoxicity | 60 |
| Investigation of cell suspensions in large injection cannulas oriented at various angles | In vitro | Primary rat embryonic cell suspensions of neural tissue | 18, 21 and 25 G metal cannulas. Glass cannulaswith nominal ID of 0.8 mm. Cannulas attached via a short siliconetubing to a 100-µL Hamilton syringe | 10 µL/min using a syringe pump. Delay of 20 mins between loading and injection | Cell behaviour was affected by cannula diameter, orientation (horizontal/vertical) and material | × | × | × | Mean cell counts | 75 |
| Effect of transcatheter injections on cell viability and cytokine release | In vitro | Mononuclear cells | Cell suspension was aspirated into a 5-mL syringe and then infused through a 25 G needle. Cells were passed through an Excelsior SL-10 catheter; Iodine and heparin exposure | 0.5–5 mL/min | Flow rates from 0.5–2 mL/min did not alter viability, but 5 mL/min reduced viability by 19%. Catheter delivery at 2 mL/min did not affect VEGF, IL-10 or IGF-1 levels. Iodine and low-dose heparin did not affect viability, but high-dose heparin caused cell death | √ | √ | × | Cellular function was assessed by production and release of VEGF, IL-10 and IGF-1 | 118 |
| Effect of ejection rate and needle gauge on cell health | In vitro | hMSCs | 30 and 34 G needles attached to 100 µL syringes | Drawn up at 300 µL/min, and ejected at 10–300 µL/min using a syringe pump | 300 μL/min resulted in highest viable cell recovery. Apoptosis levels at 10 µL/min were significantly higher than control. Downregulation of CD105 expression at 10 µL/min | √ | √ | √ | Immunophenotyping, trilineage differentiation | 74 |
CBF cerebral blood flow, G gauge, IV intravenous.
Another potential concern is the inadequate testing of many aspects of cellular health in most studies, thereby not providing the complete picture needed to develop appropriate clinical administration protocols. Table 1 provides a summary of the investigations carried out into the effects of injection-based administration of cells on various parameters of cell health. Conventional tests, such as propidium iodide, can reveal which cells are dead, but are not useful predictors of potential delayed damage to the cells. The transient exposure to shear forces when injected does not make membrane integrity measurements, such as trypan blue exclusion assay, a good method of uncovering delayed apoptotic and senescent responses triggered. This is evident in some studies that have only relied on the analysis of cell viability to conclude that cells were not affected by the injection parameters under investigation, as shown in Table 1.50, 95, 96 In addition, some studies have utilised a relatively small sample size of n ≤ 3 for their investigations.25, 29, 94 Moreover, different studies had different definitions of what constitutes effective cell transplantation. Although the Centre for Biologics Evaluation and Research (CBER) states that cellular therapy products should display ≥70% viability,99 a study by Kondziolka et al.,45 considered a reduction of almost 50% in viability of cells post-injection acceptable.
The aforementioned issues illustrate that an enhanced understanding of what happens to cellular therapeutics post-injection, specifically regarding vital cellular health parameters, will facilitate the development of more efficient administration and formulation approaches. This reinforces the need for defining crucial parameters and trial-specific pre-clinical good laboratory practice validation of any injection protocol before human application. One method to enhance cell functionality testing in pre-clinical and clinical studies is to assess the viability of a small aliquot of injected cells. Further investigations into proliferative capacity, phenotypic expressions, apoptotic responses and other transcription-level changes of the various cell types under clinical investigation is critical. Without this, the uncertainty of whether delivery was effective will undermine interpretations of efficacy.
Most investigations carried out on the impact of injection on cell functionality and viability are completely in vitro, and although these data are important, other issues can undermine cell viability in vivo. For example, reflux and rejection can eliminate grafts in animals. In vitro experiments presented in this review will need to be augmented with in vivo data. We cannot exclude the possibility that cells may experience significant biological changes on catheter/syringe/needle passage outside the conditions examined in studies cited in this review. Optimisation of injection protocols, materials from which delivery devices are constructed, injection rates and cell dose is therefore crucial to achieve higher efficacy and reduce variability using the smallest possible cell dose.
Approaches to improve injectability of cells
Improvement of neurological cell transplantation protocols and tools
To decrease variations encountered in manual injection, automated devices (e.g. computer-controlled syringe pumps) have been suggested to offer better control.49, 100 Automated brain injections were more reproducible compared to manual injections, with variability 2–20-fold higher in manual techniques.49 For cell aggregates or encapsulated cells, automated cell-delivery methods may prove useful to control the cell dose and preserve structure integrity. However, manual delivery is still often preferred to automated robot-assisted tools due to the lack of haptic feedback to the surgeon in the latter method.101
To overcome the need for multiple injections, Mendez et al.48 developed a two-hole cannula tip design, whereas Lim and colleagues created a system capable of radially branched deployment (RBD) of a catheter at adjustable angles.22, 34 Notably, cells at high density (6 × 107 cells/mL) were not damaged by transit at a high rate of delivery (50 µL/min, 99.6% viability).34 Although it represents an improvement, RBD still does not fully repeat the cell distribution achieved in pre-clinical models.
The use of syringe/cannula rotation during the injection procedure is a strategy described in the literature.45, 75, 102 In a clinical trial for Parkinson’s disease, the injection protocol incorporated rotations of the cannula between deposits, with transplant survival confirmed up to 12 months after surgery.48 Skewed distribution of cells in horizontally oriented cannulas can also be amended by rotation at regular intervals during the procedure.75 Robot-assisted surgery, image-based needle guidance systems can also facilitate accurate delivery. These include needles that automatically stop and lock into position by sensing drops in mechanical resistance.103 Technological improvements to platform and cannula design have reduced procedural invasiveness while improving injection accuracy, resulting in progress from single unilateral microinjections to multiple bilateral injections without long-term neurological consequences.51
Few clinical trials thoroughly optimise and state their cell transplantation protocols, and do not specify infusion volumes, rates or duration of administration, which may lead to variability and lower transplantation efficiency (Table 2). However, recent studies are beginning to recognise the importance of optimisation of transplantation protocols, both in pre-clinical and clinical trials.87, 98, 104–107 In a model of retinal dysfunction, photoreceptor integration was 20-fold to 30-fold increased by improved transplantation procedures including single and dual injections, and optimisation of the number of cells injected per µL.108 Another study defined optimised conditions for an autologous stem cell therapy to treat a craniofacial traumatic deficiency, regenerating 80% of the original jawbone deficiency in only 4 months vs. a minimum healing period of 6–8 months with typical protocols.104
Table 2.
Selection of clinical trials for neural applications carried out using injectable cell therapy
| Cells | Application | Route of administration | Injection device | Cell dose | Volume injected | Flow rate | Outcome | Refs. |
|---|---|---|---|---|---|---|---|---|
| MSCs | Amyotrophic lateral sclerosis | Intraspinal | Syringe with 18 G cannula needle mounted on a table fixed arm with a micrometric system. Cannula pre-modified to inject upwards and downwards | 110 × 106 cells. During treatment, different cell numbers were obtained in each subject. Only one patient received <15 × 106 cells | Cells suspended in about 1 mL of autologous CSF | Not stated | MSC transplantation into the spinal cord is safe, but no definitive conclusion about cell vitality after transplantation | 119 |
| Parkinson’s disease | Direct transplantation into the midbrain | Each patient was mounted with a Leksell stereotactic headframe. A 50 μL Hamilton syringe, fitted with a custom-made microinjector. Cell suspension was deposited along each of four putaminal trajectories | Final cell concentration of ≈80,000/μL. Total of 3.2 × 106 cells in one patient and about 4.8 × 106 cells in the other | E.g.: In the first patient, 40 μL injected along four tracks in the right postcommissural putamen, and 32 μL in the left | Not stated | Results demonstrate that such therapies can be effective in some patients at advanced stages of disease. Changes in methodology may result in better clinical outcome | 46 | |
| Chronic spinal cord injury | Intraarterial | Cobra 2 catheter (tubular, polyurethane 4 Fr and 65 cm long) | 2.5 × 106 CD 34+ cells/kg | Not stated | 10 mL/min | Recovery of somatosensory evoked response to peripheral stimuli in 67% of patients. During a 2.5-year follow-up, this protocol proved safe | 120 | |
| Intrathecal | Not stated | 5 × 106 to 10 × 106/kg of mononuclear cells | Not stated | Not stated | No statistical improvement demonstrated. One case of encephalomyelitis after 3rd injection. 24 patients developed neuropathic pain | 27 | ||
| LBS-neurons | Ischaemic or haemorrhagic stroke | Intracerebral | 0.9 mm-OD cannula with 20 µL. Cells were aspirated into 100 µL syringe | 5 × 106 or 1 × 107 cells | 10 µL was injected slowly at each site over 2 mins | 5 µL/min. Total time was around 150 min | A quantifiable improvement was noted in some patients but no evidence of significant value in motor function | 4 |
| MSCs and NSPCs | Ischaemic stroke | Either four IV injections of MSCs or one IV injection of MSCs followed by three injections of MSCs and NSPCs through the cerebellomedullary cistern | Not described | Either four IV injections of MSCs at 0.5 × 106/kg body weight; or one IV injection of MSCs at 0.5 × 106/kg followed by three injections at 5 × 106/patient and NSPCs at 6 × 106/patient | IV injections of MSCs in 250 mL saline; and the injections of MSCs and NSPCs in 10 mL saline | Not stated | No evidence of neurological deterioration, Infection or tumorigenesis at a 2-year follow-up. Neurological functions and disability levels were improved | 39 |
| NSI-566RSC (Neuralstem, Inc) | Amyotrophic lateral sclerosis | Intraspinal | Microinjection platform base attached to a custom self-retaining retractor system. Five sequential unilateral injections | 1 × 104 cells/mL | 5 injections of 10 µL at 4-mm intervals | Not stated | Delivery was well tolerated | 121 |
| Olfactory ensheathing cells | Complete, thoracic paraplegia | Intraspinal | 25 µL Hamilton syringe with 28 G bevelled needle | 80,000 cells/µL | Four injections of 1.1 µL during each penetration | Injections frame-assisted and freehand | Transplantations were feasible and safe up to 3 years post-implantation | 43, 122 |
| Chronic thoracic paraplegia | Intraspinal | Automatic micropump and 3D micromanipulator, with 25 μL glass syringe and 26 G bevelled needle | 30,000–200,000 cells/μL | Volume of single injections was 0.5 μL | 2 μL/min | Neurological improvements in the three patients, with confirmation of significance requiring larger sample | 42 |
This table is illustrative of the numerous clinical cell-therapy trials undertaken in the field of neurodegenerative diseases. Trials shown were selected to exemplify the range of therapies currently under investigation, and should not be taken as an indication of the quality of any particular trial.
IV Intravenous.
Biomaterial-assisted delivery
Although many transplantation studies have employed a saline-based delivery vehicle, alternative cell carriers have included injectable hydrogels. Hydrogels are hydrated, polymeric networks with great potential as cell carriers.109, 110 Alternatives to saline vehicles have included cells embedded within hydrogels or microencapsulated within polymers, attached to the surfaces of microcarriers, or injected as multicellular aggregates.111 Injectable biomaterial scaffolds as cell carriers have demonstrated increased spatial and temporal administration compared to saline injections.112, 113 In addition, the use of biomaterials provides an opportunity to deliver growth factors alongside cells.
Hydrogels such as alginate may experience ‘shear banding’ along inner walls of the needle,52 whereby a layer of hydrogel shear-thins to form a fluid, acting as a lubricant, allowing the rest of the intact hydrogel to slip through the needle. The width of the plug flow region is dependent upon rigidity of the hydrogel and flow rate,114 therefore altering the hydrogel’s formulation may impact plug flow. This mechanical protection is independent of cell properties52 and is therefore applicable to different cell types. Aguado et al.52 tested 1% alginate with three different molecular weights, and demonstrated protective effects with optimised mechanical properties; human umbilical vein endothelial cells had significantly lower cell viability in phosphate-buffered saline or in non-crosslinked alginate compared to in crosslinked alginates.
Considerable research on hydrogel cell carriers has focused on their role post-delivery, including cell localisation,110 support of tissue growth115, 116 and protection from local inflammatory conditions.117 More focus is required on their role during the injection procedure, as opposed to post-delivery, where the presence of an optimised viscoelastic material may protect cells from damaging mechanical forces.52, 60 This has been only investigated on a small scale (Table 3), and needs to be explored further.
Table 3.
Selection of investigations carried out into potential protective mechanisms for cell cargos
| Aim of study | Cell type | Needle size | Flow rate | Brief description of results | Refs. |
|---|---|---|---|---|---|
| Use of hydrogels | |||||
| Improving viability during injection by alginate hydrogels | Human umbilical vein endothelial cells and adipose stem cells, rat MSCs, and mouse neural progenitor cells | 28 G needle on 1 mL syringes | 1000 µL/min | Crosslinked alginate hydrogel produced highest viability. Increasing or decreasing G′ reduced protective effect. Cells in non-crosslinked alginate exhibited lower viabilities than media. Data suggested extensional flow at needle entrance was chief cause of cell death | 52 |
| β-hairpin peptide hydrogel as carrier during syringe flow | MG63 | 26 G needle on 1 mL syringe | 4, 6 and 8 mL/h | Only gel at the capillary wall experienced a velocity gradient, whereas the rest was subject to minimal shear rate. Hydrogels had no apparent effect on viability of encapsulated cells | 114 |
| Injectable fibrin matrix to enhance vascularisation | Bone marrow mononuclear cells (BMMNCs) | 100 µL injection—Needle size not mentioned | Not mentioned | Device was constructed for simultaneous injection of fibrinogen and thrombin solutions. Implantation of BMMNCs in fibrin resulted in better tissue regeneration and neovascularisation | 123 |
| Growth factor supplemented matrigel for cell delivery | C2C12 myoblasts | Not mentioned | Slow-exact rate not mentioned | Results showed that the combination of matrigel as a cell carrier for myoblasts with growth factors is recommended for the generation of muscle in vivo | 124 |
| Use of microparticles | |||||
| PLGA particles for intracerebral delivery | Neural stem cells | 22 G needle on a 50 µL gastight Luer-tip syringe | 2 μL/min | Plasma polymerised allylamine-treated MPs were used. Cell attachment was influenced by curvature, material, electrostatic charge and surface motif of particles, and the number of cells in the culture | 125, 126 |
| Nerve growth factor (NGF)-releasing PLGA microparticles | Foetal rat (E16-E17) brain cells | 22s-G needle on a 10 µL syringe | <1 µL/min | Dose of NGF delivered can be modified by changing quantity of microparticles or NGF release rate. Activity of neo-tissues with NGF-enriched microenvironments increased in in vivo and in vitro | 127 |
| Automated vs. manual systems | |||||
| Compare manual and automated injection | Neural progenitor cells and bone marrow stromal cells | Automated device for μL syringes (MEDRAD Inc.) | — | Automated delivery resulted in less variability in amount delivered. No significant difference in viability attributable to method of injection | 49 |
G′ hydrogel storage modulus.
Concluding remarks and future outlook
The complexity of the cell injection process has resulted in a paucity of studies where combinations of process parameters have been evaluated. Nonetheless, these few studies demonstrate that interactions between cell preparation protocols and injection procedures are significant, and may substantially alter cell delivery. Studies also suggest that standardisation of injection parameters will be a critical aspect of designing and comparing clinical studies. In addition, factors such as choice of instrument, interval between filling of the cannula/needle and fixing to the stereotaxic frame prior to injection, and angles of delivery must be considered and empirically validated before use in clinical practice.
An integrated approach to the evaluation of cell-delivery success is needed to improve the assessment of delivery efficacy and to allow for sound interpretations of clinical results. Improved cell-delivery tools are also required to streamline the delivery of cell-based therapeutics from the donor to the patient without compromising quality. Finally, pre-clinical planning and testing of the desired administration protocol with cell-type specificity is essential to achieve good clinical trial design.
Acknowledgements
This work was supported by the Biotechnology and Biological Sciences Research Council; the Engineering and Physical Sciences Research Council; and the Medical Research Council (Grant Number MR/K026682/1) via the UK Regenerative Medicine Platform Hubs ‘Acellular Approaches for Therapeutic Delivery’. M.H.A. was funded by a University of Nottingham International Office scholarship and the ‘Faculty for the Future Program’ of the Schlumberger Foundation. L.J.W. was funded by a Marie Curie International Outgoing Fellowship under REA Grant Agreement No. 624841. M.M. is supported by NINDS (R01 NS082226).
Author Contributions
All authors researched, collated, and wrote this paper.
Competing interests
The authors declare that they have no competing financial interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Olanow CW, et al. A double-blind controlled trial of bilateral fetal nigral transplantation in Parkinson’s disease. Ann. Neurol. 2003;54:403–414. doi: 10.1002/ana.10720. [DOI] [PubMed] [Google Scholar]
- 2.Bachoud-Levi AC, et al. Effect of fetal neural transplants in patients with Huntington’s disease 6 years after surgery: a long-term follow-up study. Lancet Neurol. 2006;5:303–309. doi: 10.1016/S1474-4422(06)70381-7. [DOI] [PubMed] [Google Scholar]
- 3.Lunn JS, Sakowski SA, Hur J, Feldman EL. Stem cell technology for neurodegenerative diseases. Ann. Neurol. 2011;70:353–361. doi: 10.1002/ana.22487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kondziolka D, et al. Neurotransplantation for patients with subcortical motor stroke: a phase 2 randomized trial. J. Neurosurg. 2005;103:38–45. doi: 10.3171/jns.2005.103.1.0038. [DOI] [PubMed] [Google Scholar]
- 5.Bliss TM, Andres RH, Steinberg GK. Optimizing the success of cell transplantation therapy for stroke. Neurobiol. Dis. 2010;37:275–283. doi: 10.1016/j.nbd.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones LA, et al. A phase 2 autologous cellular therapy trial in patients with acute, complete spinal cord injury: pragmatics, recruitment, and demographics. Spinal Cord. 2010;48:798–807. doi: 10.1038/sc.2010.29. [DOI] [PubMed] [Google Scholar]
- 7.Steinberg GK, et al. Clinical outcomes of transplanted modified bone marrow-derived mesenchymal stem cells in stroke: a phase 1/2a study. Stroke. 2016;47:1817–1824. doi: 10.1161/STROKEAHA.116.012995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalladka D, et al. Human neural stem cells in patients with chronic ischaemic stroke (PISCES): a phase 1, first-in-man study. Lancet. 2016;388:787–796. doi: 10.1016/S0140-6736(16)30513-X. [DOI] [PubMed] [Google Scholar]
- 9.Srijaya TC, Ramasamy TS, Kasim NH. Advancing stem cell therapy from bench to bedside: lessons from drug therapies. J. Transl. Med. 2014;12:243. doi: 10.1186/s12967-014-0243-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rossetti T, Nicholls F, Modo M. Intra-cerebral cell implantation: preparation and characterization of cell suspensions. Cell Transplant. 2015;25:645–664. doi: 10.3727/096368915X690350. [DOI] [PubMed] [Google Scholar]
- 11.Karimi-Abdolrezaee S, Eftekharpour E, Wang J, Morshead CM, Fehlings MG. Delayed transplantation of adult neural precursor cells promotes remyelination and functional neurological recovery after spinal cord injury. J. Neurosci. 2006;26:3377–3389. doi: 10.1523/JNEUROSCI.4184-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paul C, Samdani AF, Betz RR, Fischer I, Neuhuber B. Grafting of human bone marrow stromal cells into spinal cord injury a comparison of delivery methods. Spine. 2009;34:328–334. doi: 10.1097/BRS.0b013e31819403ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hicks AU, et al. Transplantation of human embryonic stem cell-derived neural precursor cells and enriched environment after cortical stroke in rats: cell survival and functional recovery. Eur. J. Neurosci. 2009;29:562–574. doi: 10.1111/j.1460-9568.2008.06599.x. [DOI] [PubMed] [Google Scholar]
- 14.Hubschman JP, Reddy S, Schwartz SD. Age-related macular degeneration: current treatments. Clin. Ophthalmol. 2009;3:155–166. doi: 10.2147/OPTH.S2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang G, et al. Analysis of the indel at the ARMS2 3’UTR in age-related macular degeneration. Hum. Genet. 2010;127:595–602. doi: 10.1007/s00439-010-0805-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laflamme MA, Murry CE. Heart regeneration. Nature. 2011;473:326–335. doi: 10.1038/nature10147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freed CR, et al. Transplantation of embryonic dopamine neurons for severe Parkinson’s disease. N. Engl. J. Med. 2001;344:710–719. doi: 10.1056/NEJM200103083441002. [DOI] [PubMed] [Google Scholar]
- 18.Lindvall O, Bjorklund A. Cell therapy in Parkinson’s disease. NeuroRx. 2004;1:382–393. doi: 10.1602/neurorx.1.4.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selden NR, G. D., Huhn S. L., Koch T. K., Al-Uzri A., Steiner R. D. (eds) American Association of Neurological Surgeons Annual Meeting (AANS, 2010).
- 20.Silva EA, Kim ES, Kong HJ, Mooney DJ. Material-based deployment enhances efficacy of endothelial progenitor cells. Proc. Natl Acad. Sci. USA. 2008;105:14347–14352. doi: 10.1073/pnas.0803873105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guest J, Benavides F, Padgett K, Mendez E, Tovar D. Technical aspects of spinal cord injections for cell transplantation. Clinical and translational considerations. Brain Res. Bull. 2011;84:267–279. doi: 10.1016/j.brainresbull.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 22.Potts MB, Silvestrini MT, Lim DA. Devices for cell transplantation into the central nervous system: design considerations and emerging technologies. Surg. Neurol. Int. 2013;4:S22–S30. doi: 10.4103/2152-7806.109190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwartz SD, Anglade E, Lanza R, Ocata Macular Disease Investigator Group. Stem cells in age-related macular degeneration and Stargardt’s macular dystrophy—authors’ reply. Lancet. 2015;386:30. doi: 10.1016/S0140-6736(15)61203-X. [DOI] [PubMed] [Google Scholar]
- 24.Borlongan CV, Weiss MD. Baby STEPS: a giant leap for cell therapy in neonatal brain injury. Pediatr. Res. 2011;70:3–9. doi: 10.1203/PDR.0b013e31821d0d00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walker PA, et al. Effect of needle diameter and flow rate on rat and human mesenchymal stromal cell characterization and viability. Tissue Eng. Part. C. Methods. 2010;16:989–997. doi: 10.1089/ten.tec.2009.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yamout B, et al. Bone marrow mesenchymal stem cell transplantation in patients with multiple sclerosis: a pilot study. J. Neuroimmunol. 2010;227:185–189. doi: 10.1016/j.jneuroim.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 27.Kishk NA, et al. Case control series of intrathecal autologous bone marrow mesenchymal stem cell therapy for chronic spinal cord injury. Neurorehabil. Neural Repair. 2010;24:702–708. doi: 10.1177/1545968310369801. [DOI] [PubMed] [Google Scholar]
- 28.Taguchi A, et al. Intravenous autologous bone marrow mononuclear cell transplantation for stroke: phase1/2a clinical trial in a homogeneous group of stroke patients. Stem Cells Dev. 2015;24:2207–2218. doi: 10.1089/scd.2015.0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heng BC, et al. Transcatheter injection-induced changes in human bone marrow-derived mesenchymal stem cells. Cell Transplant. 2009;18:1111–1121. doi: 10.3727/096368909X12483162197006. [DOI] [PubMed] [Google Scholar]
- 30.Shehadah A, et al. Human placenta-derived adherent cell treatment of experimental stroke promotes functional recovery after stroke in young adult and older rats. PLoS ONE. 2014;9:e86621. doi: 10.1371/journal.pone.0086621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen Y, et al. Effects of storage solutions on the viability of human umbilical cord mesenchymal stem cells for transplantation. Cell Transplant. 2013;22:1075–1086. doi: 10.3727/096368912X657602. [DOI] [PubMed] [Google Scholar]
- 32.Watts C, Caldwell MA, Dunnett SB. The development of intracerebral cell-suspension implants is influenced by the grafting medium. Cell Transplant. 1998;7:573–583. doi: 10.1177/096368979800700608. [DOI] [PubMed] [Google Scholar]
- 33.Mathew AJ, Baust JM, Van Buskirk RG, Baust JG. Cell preservation in reparative and regenerative medicine: evolution of individualized solution composition. Tissue Eng. 2004;10:1662–1671. doi: 10.1089/ten.2004.10.1662. [DOI] [PubMed] [Google Scholar]
- 34.Silvestrini MT, et al. Radially branched deployment for more efficient cell transplantation at the scale of the human brain. Stereotact. Funct. Neurosurg. 2013;91:92–103. doi: 10.1159/000343213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breeze RE, Wells TH, Jr., Freed CR. Implantation of fetal tissue for the management of Parkinson’s disease: a technical note. Neurosurgery. 1995;36:1044–1047. doi: 10.1227/00006123-199505000-00027. [DOI] [PubMed] [Google Scholar]
- 36.Miyanji F, Furlan JC, Aarabi B, Arnold PM, Fehlings MG. Acute cervical traumatic spinal cord injury: MR imaging findings correlated with neurologic outcome—prospective study with 100 consecutive patients. Radiology. 2007;243:820–827. doi: 10.1148/radiol.2433060583. [DOI] [PubMed] [Google Scholar]
- 37.Gutierrez J, et al. Preclinical validation of multilevel intraparenchymal stem cell therapy in the porcine spinal cord. Neurosurgery. 2015;77:604–612. doi: 10.1227/NEU.0000000000000882. [DOI] [PubMed] [Google Scholar]
- 38.Usvald D, et al. Analysis of dosing regimen and reproducibility of intraspinal grafting of human spinal stem cells in immunosuppressed minipigs. Cell Transplant. 2010;19:1103–1122. doi: 10.3727/096368910X503406. [DOI] [PubMed] [Google Scholar]
- 39.Qiao LY, et al. A two-year follow-up study of cotransplantation with neural stem/progenitor cells and mesenchymal stromal cells in ischemic stroke patients. Cell Transplant. 2014;23:S65–72. doi: 10.3727/096368914X684961. [DOI] [PubMed] [Google Scholar]
- 40.Miljan EA, Sinden JD. Stem cell treatment of ischemic brain injury. Curr. Opin. Mol. Ther. 2009;11:394–403. [PubMed] [Google Scholar]
- 41.Lammertse DP, et al. Autologous incubated macrophage therapy in acute, complete spinal cord injury: results of the phase 2 randomized controlled multicenter trial. Spinal Cord. 2012;50:661–671. doi: 10.1038/sc.2012.39. [DOI] [PubMed] [Google Scholar]
- 42.Tabakow P, et al. Transplantation of autologous olfactory ensheathing cells in complete human spinal cord injury. Cell Transplant. 2013;22:1591–1612. doi: 10.3727/096368912X663532. [DOI] [PubMed] [Google Scholar]
- 43.Feron F, et al. Autologous olfactory ensheathing cell transplantation in human spinal cord injury. Brain. 2005;128:2951–2960. doi: 10.1093/brain/awh657. [DOI] [PubMed] [Google Scholar]
- 44.Knoller N, et al. Clinical experience using incubated autologous macrophages as a treatment for complete spinal cord injury: phase I study results. J. Neurosurg-Spine. 2005;3:173–181. doi: 10.3171/spi.2005.3.3.0173. [DOI] [PubMed] [Google Scholar]
- 45.Kondziolka D, Steinberg GK, Cullen SB, McGrogan M. Evaluation of surgical techniques for neuronal cell transplantation used in patients with stroke. Cell Transplant. 2004;13:749–754. doi: 10.3727/000000004783983350. [DOI] [PubMed] [Google Scholar]
- 46.Mendez I, et al. Cell type analysis of functional fetal dopamine cell suspension transplants in the striatum and substantia nigra of patients with Parkinson’s disease. Brain. 2005;128:1498–1510. doi: 10.1093/brain/awh510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bjarkam CR, et al. Safety and function of a new clinical intracerebral microinjection instrument for stem cells and therapeutics examined in the Gottingen minipig. Stereotact. Funct. Neurosurg. 2010;88:56–63. doi: 10.1159/000268743. [DOI] [PubMed] [Google Scholar]
- 48.Mendez I, Hong M, Smith S, Dagher A, Desrosiers J. Neural transplantation cannula and microinjector system: experimental and clinical experience. J. Neurosurg. 2000;92:493–499. doi: 10.3171/jns.2000.92.3.0493. [DOI] [PubMed] [Google Scholar]
- 49.Gobbel GT, Kondziolka D, Fellows-Mayle W, Uram M. Manual vs automated delivery of cells for transplantation: accuracy, reproducibility, and impact on viability. Neurosurgery. 2010;67:1662–1668. doi: 10.1227/NEU.0b013e3181f9b1e2. [DOI] [PubMed] [Google Scholar]
- 50.Kondziolka D, Gobbel GT, Fellows-Mayle W, Chang YF, Uram M. Injection parameters affect cell viability and implant volumes in automated cell delivery for the brain. Cell Transplant. 2011;20:1901–1906. doi: 10.3727/096368911X566190. [DOI] [PubMed] [Google Scholar]
- 51.Riley JP, Raore B, Taub JS, Federici T, Boulis NM. Platform and cannula design improvements for spinal cord therapeutics delivery. Neurosurgery. 2011;69:ons147–154. doi: 10.1227/NEU.0b013e3182195680. [DOI] [PubMed] [Google Scholar]
- 52.Aguado BA, Mulyasasmita W, Su J, Lampe KJ, Heilshorn SC. Improving viability of stem cells during syringe needle flow through the design of hydrogel cell carriers. Tissue Eng. Part. A. 2012;18:806–815. doi: 10.1089/ten.tea.2011.0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grellier M, Bareille R, Bourget C, Amedee J. Responsiveness of human bone marrow stromal cells to shear stress. J. Tissue Eng. Regen. Med. 2009;3:302–309. doi: 10.1002/term.166. [DOI] [PubMed] [Google Scholar]
- 54.Stolberg S, McCloskey KE. Can shear stress direct stem cell fate? Biotechnol. Prog. 2009;25:10–19. doi: 10.1002/btpr.124. [DOI] [PubMed] [Google Scholar]
- 55.Bird, R. B., Stewart, W. E. & Lightfoot, E. N. Transport Phenomena (Wiley, 2007).
- 56.Reneman RS, Hoeks AP. Wall shear stress as measured in vivo: consequences for the design of the arterial system. Med. Biol. Eng. Comput. 2008;46:499–507. doi: 10.1007/s11517-008-0330-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Malek AM, Alper SL, Izumo S. Hemodynamic shear stress and its role in atherosclerosis. JAMA. 1999;282:2035–2042. doi: 10.1001/jama.282.21.2035. [DOI] [PubMed] [Google Scholar]
- 58.Korenaga R, et al. Negative transcriptional regulation of the VCAM-1 gene by fluid shear stress in murine endothelial cells. Am. J. Physiol. 1997;273:C1506–C1515. doi: 10.1152/ajpcell.1997.273.5.c1506. [DOI] [PubMed] [Google Scholar]
- 59.Wang H, et al. Shear stress induces endothelial differentiation from a murine embryonic mesenchymal progenitor cell line. Arterioscler. Thromb. Vasc. Biol. 2005;25:1817–1823. doi: 10.1161/01.ATV.0000175840.90510.a8. [DOI] [PubMed] [Google Scholar]
- 60.Amer MH, White LJ, Shakesheff KM. The effect of injection using narrow-bore needles on mammalian cells: administration and formulation considerations for cell therapies. J. Pharm. Pharmacol. 2015;67:640–650. doi: 10.1111/jphp.12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Doran, P. M. in Bioprocess Engineering Principles 2nd edn. 1–919 (Elsevier, 2013).
- 62.Sutera SP. Flow-induced trauma to blood cells. Circ. Res. 1977;41:2–8. doi: 10.1161/01.RES.41.1.2. [DOI] [PubMed] [Google Scholar]
- 63.Lee SS, Yim Y, Ahn KH, Lee SJ. Extensional flow-based assessment of red blood cell deformability using hyperbolic converging microchannel. Biomed. Microdevices. 2009;11:1021–1027. doi: 10.1007/s10544-009-9319-3. [DOI] [PubMed] [Google Scholar]
- 64.Tanzeglock T, Soos M, Stephanopoulos G, Morbidelli M. Induction of mammalian cell death by simple shear and extensional flows. Biotechnol. Bioeng. 2009;104:360–370. doi: 10.1002/bit.22405. [DOI] [PubMed] [Google Scholar]
- 65.Muller-Ehmsen J, et al. Survival and development of neonatal rat cardiomyocytes transplanted into adult myocardium. J. Mol. Cell Cardiol. 2002;34:107–116. doi: 10.1006/jmcc.2001.1491. [DOI] [PubMed] [Google Scholar]
- 66.Mazzini L, et al. Human neural stem cell transplantation in ALS: initial results from a phase I trial. J. Transl. Med. 2015;13:17. doi: 10.1186/s12967-014-0371-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Riley J, et al. Intraspinal stem cell transplantation in amyotrophic lateral sclerosis: a phase I safety trial, technical note, and lumbar safety outcomes. Neurosurgery. 2012;71:405–416. doi: 10.1227/NEU.0b013e31825ca05f. [DOI] [PubMed] [Google Scholar]
- 68.Ballios BG, Cooke MJ, van der Kooy D, Shoichet MS. A hydrogel-based stem cell delivery system to treat retinal degenerative diseases. Biomaterials. 2010;31:2555–2564. doi: 10.1016/j.biomaterials.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 69.van Asten F, et al. Are intravitreal injections with ultrathin 33-G needles less painful than the commonly used 30-G needles? Retina. 2015;35:1778–1785. doi: 10.1097/IAE.0000000000000550. [DOI] [PubMed] [Google Scholar]
- 70.Nikkhah G, et al. A microtransplantation approach for cell suspension grafting in the rat Parkinson model: a detailed account of the methodology. Neuroscience. 1994;63:57–72. doi: 10.1016/0306-4522(94)90007-8. [DOI] [PubMed] [Google Scholar]
- 71.Mehta T, et al. Subarachnoid placement of stem cells in neurological disorders. Transplant. Proc. 2008;40:1145–1147. doi: 10.1016/j.transproceed.2008.03.026. [DOI] [PubMed] [Google Scholar]
- 72.Karussis D, et al. Safety and immunological effects of mesenchymal stem cell transplantation in patients with multiple sclerosis and amyotrophic lateral sclerosis. Arch. Neurol. 2010;67:1187–1194. doi: 10.1001/archneurol.2010.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Veraitch FS, Scott R, Wong JW, Lye GJ, Mason C. The impact of manual processing on the expansion and directed differentiation of embryonic stem cells. Biotechnol. Bioeng. 2008;99:1216–1229. doi: 10.1002/bit.21673. [DOI] [PubMed] [Google Scholar]
- 74.Amer MH, Rose FR, White LJ, Shakesheff KM. A detailed assessment of varying ejection rate on delivery efficiency of mesenchymal stem cells using narrow-bore needles. Stem Cells Transl. Med. 2016;5:366–378. doi: 10.5966/sctm.2015-0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Torres EM, Trigano M, Dunnett SB. Translation of cell therapies to the clinic: characteristics of cell suspensions in large-diameter injection cannulae. Cell Transplant. 2015;24:737–749. doi: 10.3727/096368914X685429. [DOI] [PubMed] [Google Scholar]
- 76.Heaton JT, et al. Modification and testing of a pneumatic dispensing device for controlled delivery of injectable materials. Laryngoscope. 2012;122:2023–2028. doi: 10.1002/lary.23468. [DOI] [PubMed] [Google Scholar]
- 77.Guo BL, Finne-Wistrand A, Albertsson AC. Molecular architecture of electroactive and biodegradable copolymers composed of polylactide and carboxyl-capped aniline trimer. Biomacromolecules. 2010;11:855–863. doi: 10.1021/bm9011248. [DOI] [PubMed] [Google Scholar]
- 78.Bayoussef Z, Dixon JE, Stolnik S, Shakesheff KM. Aggregation promotes cell viability, proliferation, and differentiation in an in vitro model of injection cell therapy. J. Tissue Eng. Regen. Med. 2012;6:e61–73. doi: 10.1002/term.482. [DOI] [PubMed] [Google Scholar]
- 79.Ma Y, et al. Dyskinesia after fetal cell transplantation for parkinsonism: a PET study. Ann. Neurol. 2002;52:628–634. doi: 10.1002/ana.10359. [DOI] [PubMed] [Google Scholar]
- 80.Borlongan CV, et al. Potential of stem/progenitor cells in treating stroke: the missing steps in translating cell therapy from laboratory to clinic. Regen. Med. 2008;3:249–250. doi: 10.2217/17460751.3.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Glass JD, et al. Lumbar intraspinal injection of neural stem cells in patients with amyotrophic lateral sclerosis: results of a phase I trial in 12 patients. Stem Cells. 2012;30:1144–1151. doi: 10.1002/stem.1079. [DOI] [PubMed] [Google Scholar]
- 82.Yoon SH, et al. Complete spinal cord injury treatment using autologous bone marrow cell transplantation and bone marrow stimulation with granulocyte macrophage-colony stimulating factor: phase I/II clinical trial. Stem Cells. 2007;25:2066–2073. doi: 10.1634/stemcells.2006-0807. [DOI] [PubMed] [Google Scholar]
- 83.Misra V, Lal A, El Khoury R, Chen PR, Savitz SI. Intra-arterial delivery of cell therapies for stroke. Stem Cells Dev. 2012;21:1007–1015. doi: 10.1089/scd.2011.0612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rosado-de-Castro PH, Pimentel-Coelho PM, da Fonseca LM, de Freitas GR, Mendez-Otero R. The rise of cell therapy trials for stroke: review of published and registered studies. Stem Cells Dev. 2013;22:2095–2111. doi: 10.1089/scd.2013.0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Myers RD. Injection of solutions into cerebral tissue - relation between volume and diffusion. Physiol. Behav. 1966;1:171–174. doi: 10.1016/0031-9384(66)90064-3. [DOI] [Google Scholar]
- 86.Peterson SL. Drug microinjection in discrete brain regions. Kopf Carrier. 1998;50:1–6. [Google Scholar]
- 87.Janowski M, et al. Cell size and velocity of injection are major determinants of the safety of intracarotid stem cell transplantation. J. Cerebr. Blood Flow Metab. 2013;33:921–927. doi: 10.1038/jcbfm.2013.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Morrison PF, Chen MY, Chadwick RS, Lonser RR, Oldfield EH. Focal delivery during direct infusion to brain: role of flow rate, catheter diameter, and tissue mechanics. Am. J. Physiol. 1999;277:R1218–1229. doi: 10.1152/ajpregu.1999.277.4.R1218. [DOI] [PubMed] [Google Scholar]
- 89.Massensini AR, et al. Concentration-dependent rheological properties of ECM hydrogel for intracerebral delivery to a stroke cavity. Acta Biomater. 2015;27:116–130. doi: 10.1016/j.actbio.2015.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nicholls FJ, Ling W, Ferrauto G, Aime S, Modo M. Simultaneous MR imaging for tissue engineering in a rat model of stroke. Sci. Rep. 2015;5:14597. doi: 10.1038/srep14597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yin D, et al. Optimal region of the putamen for image-guided convection-enhanced delivery of therapeutics in human and non-human primates. Neuroimage. 2011;54:S196–203. doi: 10.1016/j.neuroimage.2009.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Agashi, K. The Analysis of Cell Fate Post-Ejection through Parenteral Devices and the Development of Systems that Aid the Transportation of Cell Therapy Products. PhD thesis, University of Nottingham (2010).
- 93.Mamidi MK, et al. Impact of passing mesenchymal stem cells through smaller bore size needles for subsequent use in patients for clinical or cosmetic indications. J. Transl. Med. 2012;10:229. doi: 10.1186/1479-5876-10-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Agashi K, Chau DYS, Shakesheff KM. The effect of delivery via narrow-bore needles on mesenchymal cells. Regen. Med. 2009;4:49–64. doi: 10.2217/17460751.4.1.49. [DOI] [PubMed] [Google Scholar]
- 95.Tol M, Akar AR, Durdu S, Ayyildiz E, Ilhan O. Comparison of different needle diameters and flow rates on bone marrow mononuclear stem cell viability: an ex vivo experimental study. Cytotherapy. 2008;10:98–99. doi: 10.1080/14653240701762356. [DOI] [PubMed] [Google Scholar]
- 96.Chen X, Thibeault S. Effect of DMSO concentration, cell density and needle gauge on the viability of cryopreserved cells in three dimensional hyaluronan hydrogel. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2013;2013:6228–6231. doi: 10.1109/EMBC.2013.6610976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gobbel GT, Kondziolka D, Fellows-Mayle W, Uram M. Cellular transplantation for the nervous system: impact of time after preparation on cell viability and survival. J. Neurosurg. 2010;113:666–672. doi: 10.3171/2009.10.JNS09252. [DOI] [PubMed] [Google Scholar]
- 98.Nikkhah G, et al. Microtransplantation of dopaminergic cell suspensions: further characterization and optimization of grafting parameters. Cell Transplant. 2009;18:119–133. doi: 10.3727/096368909788341324. [DOI] [PubMed] [Google Scholar]
- 99.Center for Biologics Evaluation and Research. Guidance for FDA Reviewers and Sponsors: Content and Review of Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs) (Food and Drug Administration, US Department of Health and Human Services, 2008).
- 100.Richard PL, et al. A first semimanual device for clinical intramuscular repetitive cell injections. Cell Transplant. 2010;19:67–78. doi: 10.3727/096368909X578812. [DOI] [PubMed] [Google Scholar]
- 101.Okamura AM. Haptic feedback in robot-assisted minimally invasive surgery. Curr. Opin. Urol. 2009;19:102–107. doi: 10.1097/MOU.0b013e32831a478c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Brundin P, et al. Bilateral caudate and putamen grafts of embryonic mesencephalic tissue treated with lazaroids in Parkinson’s disease. Brain. 2000;123:1380–1390. doi: 10.1093/brain/123.7.1380. [DOI] [PubMed] [Google Scholar]
- 103.Schwartz SG. Re: Awh et al.: CFH and ARMS2 Genetic polymorphisms predict response to antioxidants and zinc in patients with age-related macular degeneration (Ophthalmology 2013;120:2317–2323) Ophthalmology. 2014;121:e38. doi: 10.1016/j.ophtha.2013.12.046. [DOI] [PubMed] [Google Scholar]
- 104.Rajan A, et al. Optimized cell survival and seeding efficiency for craniofacial tissue engineering using clinical stem cell therapy. Stem Cells Transl. Med. 2014;3:1495–1503. doi: 10.5966/sctm.2014-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zakaria N, et al. Results of a phase I/II clinical trial: standardized, non-xenogenic, cultivated limbal stem cell transplantation. J. Transl. Med. 2014;12:58. doi: 10.1186/1479-5876-12-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Reyes S, Tajiri N, Borlongan CV. Developments in intracerebral stem cell grafts. Expert Rev. Neurother. 2015;15:381–393. doi: 10.1586/14737175.2015.1021787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Harting MT, Sloan LE, Jimenez F, Baumgartner J, Cox CS., Jr. Subacute neural stem cell therapy for traumatic brain injury. J. Surg. Res. 2009;153:188–194. doi: 10.1016/j.jss.2008.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pearson RA, et al. Restoration of vision after transplantation of photoreceptors. Nature. 2012;485:99–103. doi: 10.1038/nature10997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Guarino V, Gloria A, Raucci MG, Ambrosio L. Hydrogel-based platforms for the regeneration of osteochondral tissue and intervertebral disc. Polymers. 2012;4:1590–1612. doi: 10.3390/polym4031590. [DOI] [Google Scholar]
- 110.Seif-Naraghi SB, Salvatore MA, Schup-Magoffin PJ, Hu DP, Christman KL. Design and characterization of an injectable pericardial matrix gel: a potentially autologous scaffold for cardiac tissue engineering. Tissue Eng. Part A. 2010;16:2017–2027. doi: 10.1089/ten.tea.2009.0768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bidarra SJ, Barrias CC, Granja PL. Injectable alginate hydrogels for cell delivery in tissue engineering. Acta Biomater. 2014;10:1646–1662. doi: 10.1016/j.actbio.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 112.Slaughter BV, Khurshid SS, Fisher OZ, Khademhosseini A, Peppas NA. Hydrogels in regenerative medicine. Adv. Mater. 2009;21:3307–3329. doi: 10.1002/adma.200802106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tan HP, Marra KG. Injectable, biodegradable hydrogels for tissue engineering applications. Materials. 2010;3:1746–1767. doi: 10.3390/ma3031746. [DOI] [Google Scholar]
- 114.Yan C, et al. Injectable solid peptide hydrogel as a cell carrier: effects of shear flow on hydrogels and cell payload. Langmuir. 2012;28:6076–6087. doi: 10.1021/la2041746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kong HJ, Smith MK, Mooney DJ. Designing alginate hydrogels to maintain viability of immobilized cells. Biomaterials. 2003;24:4023–4029. doi: 10.1016/S0142-9612(03)00295-3. [DOI] [PubMed] [Google Scholar]
- 116.Bible E, et al. Non-invasive imaging of transplanted human neural stem cells and ECM scaffold remodeling in the stroke-damaged rat brain by (19)F- and diffusion-MRI. Biomaterials. 2012;33:2858–2871. doi: 10.1016/j.biomaterials.2011.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zeng Q, Chen W. The functional behavior of a macrophage/fibroblast co-culture model derived from normal and diabetic mice with a marine gelatin-oxidized alginate hydrogel. Biomaterials. 2010;31:5772–5781. doi: 10.1016/j.biomaterials.2010.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.El Khoury R, et al. The effect of transcatheter injections on cell viability and cytokine release of mononuclear cells. AJNR. 2010;31:1488–1492. doi: 10.3174/ajnr.A2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mazzini L, et al. Mesenchymal stem cell transplantation in amyotrophic lateral sclerosis: a phase I clinical trial. Exp. Neurol. 2010;223:229–237. doi: 10.1016/j.expneurol.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 120.Cristante AF, et al. Stem cells in the treatment of chronic spinal cord injury: evaluation of somatosensitive evoked potentials in 39 patients. Spinal Cord. 2009;47:733–738. doi: 10.1038/sc.2009.24. [DOI] [PubMed] [Google Scholar]
- 121.Riley J, et al. Intraspinal stem cell transplantation in amyotrophic lateral sclerosis: a phase I trial, cervical microinjection, and final surgical safety outcomes. Neurosurgery. 2014;74:77–87. doi: 10.1227/NEU.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 122.Mackay-Sim A, et al. Autologous olfactory ensheathing cell transplantation in human paraplegia: a 3-year clinical trial. Brain. 2008;131:2376–2386. doi: 10.1093/brain/awn173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ryu JH, et al. Implantation of bone marrow mononuclear cells using injectable fibrin matrix enhances neovascularization in infarcted myocardium. Biomaterials. 2005;26:319–326. doi: 10.1016/j.biomaterials.2004.02.058. [DOI] [PubMed] [Google Scholar]
- 124.Barbero A, et al. Growth factor supplemented matrigel improves ectopic skeletal muscle formation--a cell therapy approach. J. Cell Physiol. 2001;186:183–192. doi: 10.1002/1097-4652(200102)186:2<183::AID-JCP1020>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 125.Bible E, et al. Attachment of stem cells to scaffold particles for intra-cerebral transplantation. Nat. Protoc. 2009;4:1440–1453. doi: 10.1038/nprot.2009.156. [DOI] [PubMed] [Google Scholar]
- 126.Bible E, et al. The support of neural stem cells transplanted into stroke-induced brain cavities by PLGA particles. Biomaterials. 2009;30:2985–2994. doi: 10.1016/j.biomaterials.2009.02.012. [DOI] [Google Scholar]
- 127.Mahoney MJ, Saltzman WM. Transplantation of brain cells assembled around a programmable synthetic microenvironment. Nat. Biotechnol. 2001;19:934–939. doi: 10.1038/nbt1001-934. [DOI] [PubMed] [Google Scholar]


