Abstract
Objectives
Schoolchildren in developing countries are at greater risk of intestinal parasitic infections. This study aimed to estimate the prevalence and assess the risk factors of intestinal parasite infection among schoolchildren in rural areas of Peru.
Methods
A volunteer team from the Korea International Cooperation Agency (KOICA) conducted a campaign for parasite eradication called “Chao parasitos” at five schools in the peripheral highland regions of Huanuco in October 2013. The study collected questionnaires and stool samples from children of participating schools. Entamoeba coli, Iodamoeba buschii, and Chilomastix mesnil were classified as nonpathogenic parasites.
Results
The overall prevalence of intestinal parasite infection in the students was 100% (185/185). Among them, 25.9% (48/185) were infected only with nonpathogenic parasites whereas 74.1% (137/185) were infected with at least one pathogenic parasite. Ascaris lumbricoides was the most commonly detected (37.3%, 69/185), followed by Giardia lamblia (15.1%, 28/185) and I. buschii (11.9%, 22/185). Among lifestyle practices associated with parasitic infection, the rate of washing hands before meals was significantly lower in the students with pathogenic parasites compared to those with nonpathogenic parasites (77.4%, 106/137 vs. 93.8%, 45/48, p = 0.025).
Conclusion
The prevalence of intestinal parasite was 100%. Both personal hygiene and water supply facilities are required to eradicate parasite infection in rural areas of Peru.
Keywords: parasites, volunteers, Peru
INTRODUCTION
Intestinal parasite infections are a major public health issue in the developing world [1]. It has been estimated that over 3.5 billion people are infected with intestinal parasites globally. People in developing countries are at greater risk for these infections due to poor hygiene and a lack of sanitation facilities [2]. Schoolchildren are particularly vulnerable to intestinal parasitic infections because of their poor hygiene, hand-mouth activity, and immature immune system [3].
Peru is a well-known developing country on the central pacific coast of South America. Despite a fast-growing economy, approximately 40% of the population still lives under poor socioeconomic conditions. The bottom 50% of the population, in terms of income, contributes only 13% of the gross domestic product, and 65% of nationals cannot take advantage of health insurance [4]. Additionally, people in poor regions have limited access to sanitation facilities, and young children in such regions suffer from parasitic infections that can cause malnutrition, stunting, and even death [5].
The Korea International Cooperation Agency (KOICA) is a government agency that provides Official Development Assistance (ODA) work and dispatches volunteers including health professionals to Peru [4]. The health sector is one of the principal ODA strategies of the KOICA in Peru; therefore, several campaigns on health promotion have been conducted by volunteers particularly in poor regions [4]. In 2013, KOICA volunteers in Huanuco, a province located in the Andean highland, noticed that many schoolchildren were suffering from parasite infections and organized a campaign for parasite eradication which was called “Chao parasitos.” There are few studies on intestinal parasite infections among schoolchildren in Peru and no relevant statistics for the Huanuco province [5,6].
The objective of this study was to estimate the prevalence and to assess the risk factors of intestinal parasite infections among schoolchildren in the peripheral highland regions of Huanuco, Peru based on data collected from the campaign.
MATERIALS AND METHODS
1. Study setting and population
This study was performed in the highland areas of the Amarilis district located in the peripheral region of Huanuco, Peru (Figure 1). The KOICA volunteer team conducted a campaign for parasite eradication, “Chao parasitos,” in October 2013. Five schools in this area (Cachuna, Matamarca, Sariapampa, Sharicancha, and Paucar) were selected. Primaria students (similar to elementary school aged) from all five schools (n = 222) and secundaria students (similar to middle and high school aged) from one school (Sariapampa, n = 32) participated in this campaign. The campaign program was as follows:
Figure 1.
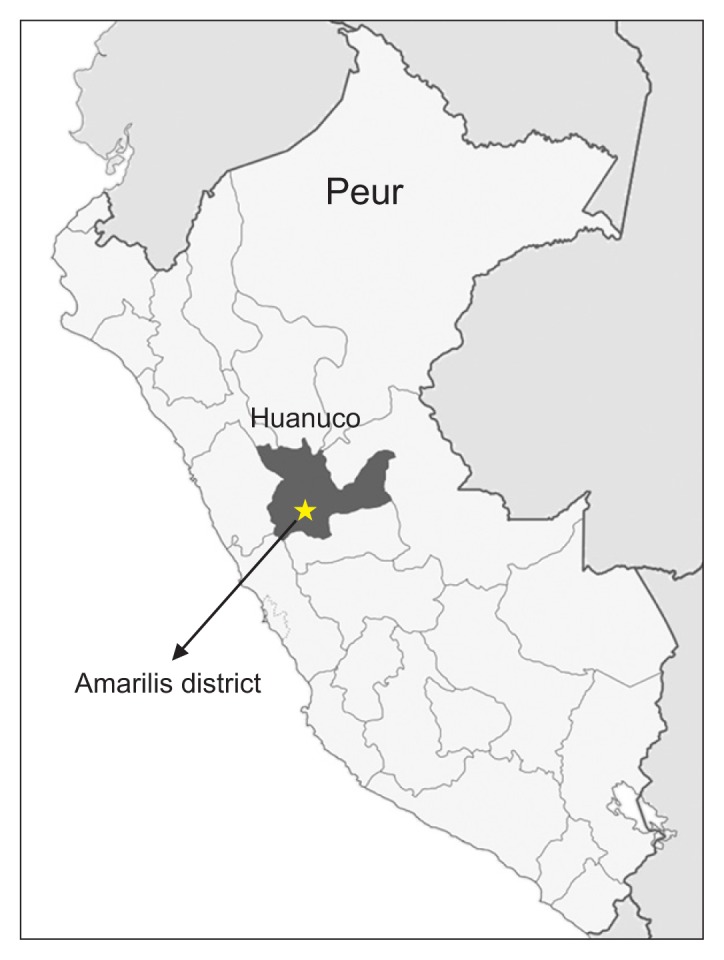
Map of the Huanuco region. The arrow shows the Amarilis district where the study was conducted.
Day 1
The KOICA volunteer team visited each school and gave an introduction to all the students that included a description of the proper way to collect a stool sample. Then, they measured the height and weight of each student. Labeled plastic stool containers and questionnaires were distributed thereafter.
Day 2
Stool samples and questionnaires were collected by the KOICA volunteer team. They transported the collected stool samples to the laboratory of Centro de Salud (public health center), Peru-Corea, for parasitological examination.
Day 3
The KOICA volunteer team explained the results of the parasitological examination to the students and distributed anthelmintic drugs (albendazole, metronidazole, or praziquantel) according to the detected parasite species. Subsequently, education on prevention measures against parasite infections was provided to the students and teachers.
Students who completed questionnaire and submitted proper stool sample were enrolled in this study. We classified Entamoeba coli, Iodamoeba buschii, and Chilomastix mesnil as nonpathogenic parasites and others as pathogenic parasites.
2. Laboratory analysis and data collection
All collected stool samples were examined using direct smear method with light microscopy. Lugol’s iodine was applied on direct smear slide for the identification of protozoan parasites. All positive results were confirmed by a second observer.
The questionnaire included demographic information (gender, age, weight, height), lifestyle practices associated with parasite infection (number of family members, raising animal at home, washing hands before meals, wearing shoes, drinking water sources, eating raw vegetables, using latrine, cultivating vegetable garden, using fertilizers with human feces) and parent’s knowledge of parasite infection (parasite transmission route, parasite infection state in their children).
3. Statistical analysis
IBM SPSS Statistics version 24.0 for Windows (IBM Co., Armonk, NY, USA) was used for the statistical analysis. Categorical variables were analyzed by the chi-square test or Fisher’s exact test. Continuous variables were analyzed by the independent t-test. A p-value of < 0.05 by a two-tailed test was considered to be significant.
4. Ethics statement
The study protocol was approved by the institutional review boards of Eulji University Hospital (IRB number: 2017-04-019), and the requirement for written informed consent from patients was waived.
RESULTS
Overall demographic data of participants is shown in Table 1. The average age was 10.1 ± 2.9 years. Approximately half of the participants were male (51.4%, 95/185) and the average body mass index (BMI) was 17.2 ± 2.4 kg/m2. All of the subjects were infected with at least one parasite (100%, 185/185). Among them, 25.9% (48/185) of the subjects were infected with nonpathogenic parasites, and 74.1% (137/185) were infected with at least one pathogenic parasite. Monoparasitism was observed in 91.9% (170/185), and more than two parasites were observed in 8.1% (15/185). Ten parasite species (3 nonpathogenic parasites and 7 pathogenic parasites) were found in the stool samples: Ascaris lumbricoides was the most commonly detected (37.3%, 69/185), followed by Giardia lamblia (15.1%, 28/185), I. buschii (11.9%, 22/185) and E. coli (10.3%, 19/185) (Table 2).
Table 1.
Descriptive analysis of demographic data (n = 185)
| Data | |
|---|---|
| Gender | |
| Male | 95 (51.4) |
| Female | 90 (48.6) |
| Age (y) | 10.1 ± 2.9 |
| Body mass index (kg/m2) | 17.2 ± 2.4 |
| Participating schools | |
| Paucar | 48 (25.9) |
| Sarapampa primaria | 33 (17.8) |
| Sarapampa scundaria | 32 (17.3) |
| Sharicancha | 32 (17.3) |
| Cachuna | 22 (11.9) |
| Matamarca | 18 (9.7) |
| Parasite infections | |
| Pathogenic parasite infections | 137 (74.1) |
| Nonpathogenic parasite infectionsa | 48 (25.9) |
Values are presented as number (%) or mean ± standard deviation.
Infected only with Entamoeba coli, Iodamoeba buschii, or Chilomastix mesnil.
Table 2.
Parasitological findings
| Monoparasitism (n = 170) | Polyparasitism (n = 15) | Total (n = 185) | Prevalence (%)a | |
|---|---|---|---|---|
| Nonpathogenic parasite | ||||
| Entamoeba coli | 11 | 8 | 19 | 10.3 |
| Chilomastix mesnili | 16 | 1 | 17 | 9.2 |
| Iodamoeba buschii | 19 | 3 | 22 | 11.9 |
| Subtotal | 46 | 12 | 58 | 31.4 |
| Pathogenic parasite | ||||
| Ascaris lumbricoides | 62 | 7 | 69 | 37.3 |
| Blastocystis hominis | 8 | 2 | 10 | 5.4 |
| Enterobius vermicularis | 1 | 1 | 2 | 1.1 |
| Giardia lamblia | 22 | 6 | 28 | 15.1 |
| Hymenolepis nana | 14 | 1 | 15 | 8.1 |
| Strongyloides stercoralis | 6 | 0 | 6 | 3.2 |
| Trichuris trichiura | 11 | 1 | 12 | 6.5 |
| Subtotal | 124 | 18 | 142 | 76.8 |
| Total | 170 | 30 | 200 | 100 |
Percentage of children with positive results divided by the total number of children (n = 185).
Risk factors of pathogenic parasite infection are shown in Table 3. There was no difference in average BMI between students with pathogenic parasite and students with nonpathogenic parasite (17.2 ± 2.4 kg/m2 and 17.3 ± 2.3 kg/m2, respectively; p = 0.687). Among lifestyle practices associated with parasite infection, the rate of washing hands before meals was significantly lower in the students with pathogenic parasite compared to those with nonpathogenic parasite (77.4%, 106/137 and 93.8%, 45/48, respectively; p = 0.025). There was no significant difference between the two groups in number of family members, raising animals at home, wearing shoes, drinking water sources, eating raw vegetables, using latrine and cultivating vegetable garden. The rate of using fertilizers with human feces was approximately two-fold higher in the students with pathogenic parasites; however, this was not statistically significant (13.9%, 19/137 and 6.3%, 3/48, respectively; p = 0.144). There were no significant differences between the two groups on parent’s knowledge of parasite transmission route (21.2%, 29/137 and 22.9%, 11/48, respectively; p = 0.874) as well as on parent’s knowledge of parasite infection state in their children (31.4%, 43/137 and 31.3%, 15/48, respectively; p = 0.891)
Table 3.
Risk factors of pathogenic parasite infection
| Variable | Students with | Total (n = 185) | p-value | |
|---|---|---|---|---|
| Pathogenic parasite (n = 137) | Nonpathogenic parasite (n = 48) | |||
| Body mass index (kg/m2) | 17.2 ± 2.4 | 17.3 ± 2.3 | 17.2 ± 2.4 | 0.687 |
| Number of family members | 5.7 ± 2.1 | 5.1 ± 1.8 | 5.5 ± 2.0 | 0.119 |
| Raising animals at home | 132 (96.4) | 48 (100) | 180 (97.3) | 0.547 |
| Washing hands before meals | 106 (77.4) | 45 (93.8) | 151 (81.6) | 0.025 |
| Wearing shoes | 87 (63.5) | 32 (66.7) | 119 (64.3) | 0.875 |
| Drinking water sources | 0.804 | |||
| Natural water | 75 (54.7) | 28 (58.3) | 103 (55.7) | |
| Mineral water | 3 (2.2) | 0 (0.0) | 3 (1.6) | |
| Boiled water | 27 (19.7) | 9 (18.8) | 36 (19.5) | |
| Tap water | 27 (19.7) | 11 (22.9) | 38 (20.5) | |
| Non-response | 5 (3.6) | 0 (0) | 5 (2.7) | |
| Eating raw vegetables | 75 (54.7) | 26 (54.2) | 101 (54.6) | 0.790 |
| Using latrine | 76 (55.5) | 30 (62.5) | 106 (57.3) | 0.518 |
| Cultivating vegetable garden | 119 (86.9) | 44 (91.7) | 163 (88.1) | 0.663 |
| Using fertilizers with human feces | 19 (13.9) | 3 (6.3) | 22 (11.9) | 0.144 |
| Parent’s knowledge of parasite transmission route | 29 (21.2) | 11 (22.9) | 40 (21.6) | 0.874 |
| Parent’s knowledge of parasite infection state in their children | 43 (31.4) | 15 (31.3) | 58 (31.4) | 0.891 |
Values are presented as mean ± standard deviation or number (%).
DISCUSSION
In the present study, the overall prevalence of intestinal parasite infections was 100% among schoolchildren in the peripheral highland regions of Huanuco. It was higher than the 91.2% prevalence in a previous study conducted in other Peruvian rural highland communities [7]. Furthermore, it seems to be higher compared to that in rural regions of other countries in South America. The prevalence of intestinal parasite infections was 53.4% among agricultural settlements in the Amazon region of Brazil [8], 77% among an indigenous group in the Bolivian Amazon region [9], and 69% among rural public school students in Colombia [10]. In addition, the prevalence of pathogenic parasites in the highland regions of Huanuco was higher than that of the highland regions of Puno (76.8% and 19.8%, respectively). According to Maco Flores et al. [7], Hymenolepis nana (6.6%) showed the highest prevalence in the rural highland areas of Puno, followed by Entamoeba histolytica (5.5%), G. lamblia (3.3%), Taenia sp. (2.2%) and A. lumbricoides (2.2%). Additionally, A. lumbricoides and Trichuris trichiura, common soil-transmitted helminths that are known to be highly relevant to malnutrition and growth retardation [11], comprised a great proportion of the intestinal parasite infections in the study area (43.8%, 81/185). Specifically, the prevalence of A. lumbricoides in Huanuco was higher compared to other South American countries such as Brazil (5.8%) [8], Bolivia (7%) [9], and Colombia (21%) [10], as well as other Peruvian provinces (2.2%) [7].
The high prevalence of pathogenic parasite infections may have an important role in the nutritional status of the study region. It is well known that intestinal parasite infections decrease appetite and cause several gastrointestinal symptoms including vomiting, diarrhea, and abdominal pain, which have a detrimental impact on the growth rate, school attendance and cognitive performance of schoolchildren [12]. The nutritional status of the schoolchildren can be classified into four categories according to their BMI; severe malnutrition (< 15.9 kg/m2), moderate malnutrition (16–16.9 kg/m2), mild malnutrition (17–18.4 kg/m2), and normal (18.5–25 kg/m2) [13]. With this standard, the average nutritional status of the participants was mild malnutrition (BMI, 17.2 ± 2.4 kg/m2).
We suggest that use of infected water is the primary cause of the high prevalence of intestinal parasite infections in the study region [14]. The majority of the participants drank natural or tap water (76.2%, 141/185) rather than boiled or mineral water (21.1%, 39/185). Unfortunately, the study area does not have a standardized water supply system, and unfiltered water is delivered to each household. Moreover, the water is likely to be contaminated by human and animal feces. In fact, about 40% of the participants (42.7%, 79/185) did not use latrines, and it is possible they might defecate in the open.
Parents’ lack of knowledge about parasite infections was another serious problem in the study region; parents who knew about parasite transmission routes and the parasite infection status of their children were only 21.6% and 31.4%, respectively. Several studies in other countries have shown that an especially low maternal education level is highly correlated with the risk of parasitic infection in children [15–17]. Mothers with a low educational level tend to be less knowledgeable about the controllability of parasitic infections and believe that infections are inevitable in their children [15], and because of this, children are exposed to risky family habits and environments as well as a poor sense of hygiene. Additionally, parents’ lack of knowledge about parasite infections disrupts taking prompt, proper measures for their children’s infections. Therefore, improving the knowledge and behavior of the parents is necessary to control parasitic infections.
The level of personal hygiene is an important risk factor of parasitic infection. Interestingly, a significantly lower handwashing rate before meals was observed among the schoolchildren with pathogenic parasites compared to those without nonpathogenic parasites in this study. Additionally, hand washing is one of the most effective and simple methods to reduce the risk of infectious diseases; handwashing with plain soap can reduce 53% of gastrointestinal infections in developing countries [18].
Taken together, establishing adequate water supply facilities and education on personal hygiene are essential for the eradication of parasite infections in the study region. To achieve this goal more effectively, cooperation between the Peruvian government and the international community is necessary. In this regard, the role of the KOICA is important. The KOICA began to dispatch volunteers to Peru since 1996, and the health sector has been providing the principal ODA strategies in this country [4]. With support of the Korean government, the KOICA constructed five public health centers and one hospital in Peru; one of these exists in Huanuco. For this reason, Huanuco became a strategic region for the KOICA, and several health professionals including international cooperation doctors have been dispatched to achieve these ODA works [4]. We expect further sophisticated support for this region.
There are limitations to this study. First, we collected data using written questionnaires. Children who have parents with a low education level may not have completed the questionnaire and thus were excluded from this study. To minimize such bias, we obtained help from local teachers if the parents of students were illiterate. Second, the parasitological examination was performed with samples from the participants, and we could not assess the surrounding environment. Thus, the transmission route was not verified. Further research is necessary to provide additional insight on parasitic infection in this region.
Despite these limitations, this is the first study on prevalence and risk factor analysis of intestinal parasite infections among schoolchildren in the peripheral highland regions of Huanuco, Peru. The prevalence of intestinal parasites was 100% in this region. Both personal hygiene and water supply facilities are required to eradicate parasite infections in this area. Further cooperation between the Peruvian government and international organizations including the KOICA is essential to improve public health in rural Peruvian areas.
ACKNOWLEDGMENTS
The authors thank Eun Jung Jung, Eun Ah Go, and Ji Eun Yoo, volunteers of the KOICA and Dr. Javier Miranda, director of Centro de Salud, Peru-Corea, for their cooperation in the campaign “Chao Parasitos.” The KOICA funded the campaign “Chao Parasitos.”
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Kucik CJ, Martin GL, Sortor BV. Common intestinal parasites. Am Fam Physician. 2004;69:1161–8. [PubMed] [Google Scholar]
- 2.World Health Organization. Informal consultation on intestinal helminth infections [Internet] Geneva: World Health Organization; 1990. [cited 2017 Jun 20]. Available from: http://apps.who.int/iris/handle/10665/62188. [Google Scholar]
- 3.Tyoalumun K, Abubakar S, Christopher N. Prevalence of intestinal parasitic infections and their association with nutritional status of rural and urban pre-school children in Benue State, Nigeria. Int J MCH AIDS. 2016;5:146–52. [PMC free article] [PubMed] [Google Scholar]
- 4.Kim B. Review for the Korean health professionals and international cooperation doctors dispatched to Peru by the Korea International Cooperation Agency (KOICA) Osong Public Health Res Perspect. 2015;6:133–9. doi: 10.1016/j.phrp.2015.02.004. https://doi.org/10.1016/j.phrp.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casapía M, Joseph SA, Núñez C, et al. Parasite risk factors for stunting in grade 5 students in a community of extreme poverty in Peru. Int J Parasitol. 2006;36:741–7. doi: 10.1016/j.ijpara.2006.03.004. https://doi.org/10.1016/j.ijpara.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Cabada MM, Morales ML, Lopez M, et al. Hymenolepis nana impact among children in the highlands of Cusco, Peru: an emerging neglected parasite infection. Am J Trop Med Hyg. 2016;95:1031–6. doi: 10.4269/ajtmh.16-0237. https://doi.org/10.4269/ajtmh.16-0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maco Flores V, Marcos Raymundo LA, Terashima Iwashita A, et al. [Distribution of entero-parasitic infections in the Peruvian Highland: study carried out in six rural communities of the department of Puno, Peru]. Rev Gastroenterol Peru. 2002;22:304–9. In Spanish. [PubMed] [Google Scholar]
- 8.de Souza EA, da Silva-Nunes M, Malafronte Rdos S, et al. Prevalence and spatial distribution of intestinal parasitic infections in a rural Amazonian settlement, Acre State, Brazil. Cad Saude Publica. 2007;23:427–34. doi: 10.1590/S0102-311X2007000200019. https://doi.org/10.1590/S0102-311X2007000200019. [DOI] [PubMed] [Google Scholar]
- 9.Tanner S, Leonard WR, McDade TW, et al. Influence of helminth infections on childhood nutritional status in lowland Bolivia. Am J Hum Biol. 2009;21:651–6. doi: 10.1002/ajhb.20944. https://doi.org/10.1002/ajhb.20944. [DOI] [PubMed] [Google Scholar]
- 10.Wilson WM, Dufour DL, Staten LK, et al. Gastrointestinal parasitic infection, anthropometrics, nutritional status, and physical work capacity in Colombian boys. Am J Hum Biol. 1999;11:763–71. doi: 10.1002/(SICI)1520-6300(199911/12)11:6<763::AID-AJHB6>3.0.CO;2-M. https://doi.org/10.1002/(SICI)1520-6300(199911/12)11:6<763::AID-AJHB6>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 11.Bethony J, Brooker S, Albonico M, et al. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet. 2006;367:1521–32. doi: 10.1016/S0140-6736(06)68653-4. https://doi.org/10.1016/S0140-6736(06)68653-4. [DOI] [PubMed] [Google Scholar]
- 12.Papier K, Williams GM, Luceres-Catubig R, et al. Childhood malnutrition and parasitic helminth interactions. Clin Infect Dis. 2014;59:234–43. doi: 10.1093/cid/ciu211. https://doi.org/10.1093/cid/ciu211. [DOI] [PubMed] [Google Scholar]
- 13.Amare B, Ali J, Moges B, et al. Nutritional status, intestinal parasite infection and allergy among school children in northwest Ethiopia. BMC Pediatr. 2013;13:7. doi: 10.1186/1471-2431-13-7. https://doi.org/10.1186/1471-2431-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slifko TR, Smith HV, Rose JB. Emerging parasite zoonoses associated with water and food. Int J Parasitol. 2000;30:1379–93. doi: 10.1016/S0020-7519(00)00128-4. https://doi.org/10.1016/S0020-7519(00)00128-4. [DOI] [PubMed] [Google Scholar]
- 15.Omoigberale AI, Airauhi LU. Aspects of the epidemiology of intestinal parasitoses (IP) in children: knowledge, practices and perceptions of mothers. Niger J Clin Pract. 2006;9:109–13. [PubMed] [Google Scholar]
- 16.Quihui L, Valencia ME, Crompton DW, et al. Role of the employment status and education of mothers in the prevalence of intestinal parasitic infections in Mexican rural schoolchildren. BMC Public Health. 2006;6:225. doi: 10.1186/1471-2458-6-225. https://doi.org/10.1186/1471-2458-6-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nematian J, Nematian E, Gholamrezanezhad A, et al. Prevalence of intestinal parasitic infections and their relation with socio-economic factors and hygienic habits in Tehran primary school students. Acta Trop. 2004;92:179–86. doi: 10.1016/j.actatropica.2004.06.010. https://doi.org/10.1016/j.actatropica.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Luby SP, Agboatwalla M, Feikin DR, et al. Effect of handwashing on child health: a randomised controlled trial. Lancet. 2005;366:225–33. doi: 10.1016/S0140-6736(05)66912-7. https://doi.org/10.1016/S0140-6736(05)66912-7. [DOI] [PubMed] [Google Scholar]


