Abstract
Background:
Sacroiliac (SI) screw fixation is a demanding technique, with a high rate of screw malposition due to the complex pelvic anatomy. TiRobot™ is an orthopedic surgery robot which can be used for SI screw fixation. This study aimed to evaluate the accuracy of robot-assisted placement of SI screws compared with a freehand technique.
Methods:
Thirty patients requiring posterior pelvic ring stabilization were randomized to receive freehand or robot-assisted SI screw fixation, between January 2016 and June 2016 at Beijing Jishuitan Hospital. Forty-five screws were placed at levels S1 and S2. In both methods, the primary end point screw position was assessed and classified using postoperative computed tomography. Fisher's exact probability test was used to analyze the screws’ positions. Secondary end points, such as duration of trajectory planning, surgical time after reduction of the pelvis, insertion time for guide wire, number of guide wire attempts, and radiation exposure without pelvic reduction, were also assessed.
Results:
Twenty-three screws were placed in the robot-assisted group and 22 screws in the freehand group; no postoperative complications or revisions were reported. The excellent and good rate of screw placement was 100% in the robot-assisted group and 95% in the freehand group. The P value (0.009) showed the same superiority in screw distribution. The fluoroscopy time after pelvic reduction in the robot-assisted group was significantly shorter than that in the freehand group (median [Q1, Q3]: 6.0 [6.0, 9.0] s vs. median [Q1, Q3]: 36.0 [21.5, 48.0] s; χ2 = 13.590, respectively, P < 0.001); no difference in operation time after reduction of the pelvis was noted (χ2 = 1.990, P = 0.158). Time for guide wire insertion was significantly shorter for the robot-assisted group than that for the freehand group (median [Q1, Q3]: 2.0 [2.0, 2.7] min vs. median [Q1, Q3]: 19.0 [15.5, 45.0] min; χ2 = 20.952, respectively, P < 0.001). The number of guide wire attempts in the robot-assisted group was significantly less than that in the freehand group (median [Q1, Q3]: 1.0 [1.0,1.0] time vs. median [Q1, Q3]: 7.0 [1.0, 9.0] times; χ2 = 15.771, respectively, P < 0.001). The instrumented SI levels did not differ between both groups (from S1 to S2, χ2 = 4.760, P = 0.093).
Conclusions:
Accuracy of the robot-assisted technique was superior to that of the freehand technique. Robot-assisted navigation is safe for unstable posterior pelvic ring stabilization, especially in S1, but also in S2. SI screw insertion with robot-assisted navigation is clinically feasible.
Keywords: Computer-Assisted, Pelvic Injuries, Percutaneous Screw Placement, Robotics, Sacroiliac Screw, Surgery
INTRODUCTION
Percutaneous sacroiliac (SI) screw fixation under fluoroscopic guidance for unstable pelvic ring fractures is becoming increasingly popular worldwide. It was first described by Routt and has steadily gained popularity, with advantages of minimal invasion to compromised soft tissue, limited blood loss, and decreased infection rates, compared to conventional open techniques.[1,2,3] However, it requires detailed knowledge and experience to accurately correlate the sacral osseous landmarks with their corresponding fluoroscopic images and find a secure screw corridor using rotating inlet, outlet, and lateral fluoroscopic views,[4] because incorrect placement of SI screws may result in implant-related and neurovascular complications.[5,6,7] Statistically, the rates for malposition of the screw under fluoroscopic guidance have been reported to range from 2% to 15%,[8,9] with an incidence of neurologic injury between 0.5% and 7.7%.[9] Given this, fluoroscopy and computer-assisted techniques have been widely used to achieve an accurate screw placement. Currently, the conventional freehand fluoroscopy technique is very common for intraoperative visualization realized via image intensifier, which is possible in only one plane at a time, meanwhile requiring complex hand-eye coordination.[10,11,12] As such, it is a highly demanding and challenging operative technique. Recently, computer-assisted orthopedic surgery, which potentially increases the accuracy and efficiency of percutaneous targeting, has utilized image navigation systems and purpose-built robots. The two-dimensional (2D) or 3D-fluoroscopy-based navigation system makes it possible for simultaneous representation in up to four planes, which means a substantial improvement for the operator.[13,14] Moreover, this advantage reduces the time of repeated C-arm movements during surgery and optimizes precise and simultaneous visualization of the surgical instruments in relation to the patient's anatomy in all the desired image planes. However, navigation does not solve the problem of precise manipulation of guide wire insertion and calculate the screw trajectory, which can be expediently alternated with a robot application. Robot-assisted orthopedic surgery is believed to potentially improve the precision of implant placement and decrease radiation and operative time. Several manufacturers research and produce hardware and software products for orthopedic surgery.[15] Notably, TiRobot™ is an orthopedic surgery robot which can be used for implantation of SI screws, especially useful in SI screw fixation for unstable pelvic injury. The method, studied in cadaver and cohort studies, has shown a high accuracy. To date, there has been no report describing a direct comparison of robot assistance with the freehand technique. This study is designed to evaluate the accuracy of robot-assisted placement of SI screws in comparison with the freehand conventional technique.
METHODS
Ethical approval
The ethics committee of Beijing Jishuitan Hospital Ethics Committee approved the present clinical study (No. 20150504). All patients gave written informed consent before the study.
Patient selection
All the thirty patients received treatment in the Department of Orthopedic Trauma at Beijing Jishuitan Hospital between January 2016 and June 2016. They were all polytrauma patients having fallen from a height of more than 2 m (9 patients) or injured because of a motor vehicle accident (21 patients) and classified according to Tile criteria. A multidisciplinary team of professionals made the diagnosis. Each patient included in this study had to fulfill the following criteria: (1) aged older than 18 years, (2) indication for posterior pelvic ring stabilization using SI screws, and (3) informed consent to participate in the study. Patients were randomized to conventional fluoroscopy-assisted freehand SI screw placement or robot-assisted SI screw placement in a 1:1 ratio (ClinicalTrials.gov identifier: NCT02890043).
Three experienced trauma orthopedic surgeons familiar with both techniques, that is, conventional freehand SI screw implantation and the robot-assisted implantation, performed the surgical procedures in equal proportions.
Study design
Based on random, open, parallel-controlled design, this study adopted an electronic interactive web response system for central randomization to separate the participants into a robot-assisted group and a freehand group. The robot-assisted group received the robot-assisted implantation of SI screws in comparison with the freehand group using freehand conventional technique. The surgical record covered the duration of surgeries and planning, radiation exposure, number of guide wire attempts, and other indicators. Another experienced surgeon, who did not attend this study, carried out the review process, based on the screw's position in the image after the surgery. The statistical calculation was run based on these indicators to analyze the strengths of robot-assisted and freehand conventional surgeries.
Conventional freehand sacroiliac screw implantation
For conventional freehand SI pedicle screw implantation, inlet, outlet, and lateral fluoroscopic views were used during the procedure. The upper posterior quadrant, forming an intersection between a line parallel to the femoral diaphysis and another line perpendicular to the anterior superior iliac spine, was the site of insertion. Under imaging control, a guide wire was passed from the lateral edge of the ilium, perpendicular to the SI joint toward the body of the first sacral vertebra. Lateral views of the sacrum were taken to confirm the correct positioning of the guide wire within the safe zone, avoiding the placement of an “in-out-in” screw, as described by Routt et al.[2] A 7.0-mm cannulated screw was then inserted and directed perpendicularly to the SI articulation while chondral surfaces were avoided. Following placement of the first screw, a second screw was used as necessary.
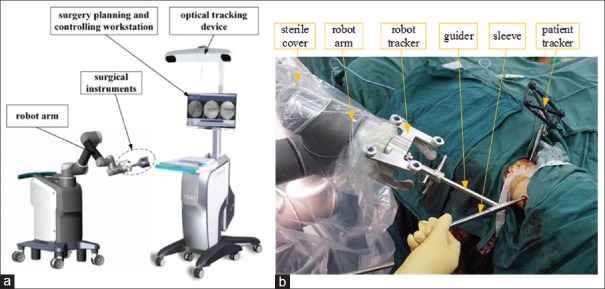
Robot component
Orthopedic surgery robot, TiRobot™ (TINAVI Medical Technologies Co., Ltd., Beijing, China), consists of a robot arm, an optical tracking device, a surgical planning and controlling workstation, and surgical instruments [Figure 1].
Figure 1.
Main components of TiRobot™: a robot arm, an optical tracking device, a surgical planning and controlling workstation, and some surgical instruments (a); surgical instruments: robot arm is isolated by the sterile cover, and robot tracker and patient tracker are fixed, respectively, at the distal end of the robot arm and on the patient, guider attaches to the robot arm and firmly holds the sleeve; the sleeve can slide along the guider and invade patient (b).
The robot arm is an actuator for trajectory positioning in this system with 6 degrees-of-freedom. The optical tracking device is a binocular camera based on infrared light, whose positioning error is <0.3 mm. The robot tracker and the patient tracker with reflection balls are fixed. The optical tracking device locates the spatial position of the robot arm and the patient through the robot tracker and patient tracker correspondingly. The calibrator is used for acquiring mapping relation between the imaging space and the surgical space through fluoroscopic images’ matching coordinates in the calibrator images. The planning and controlling workstation is used for image processing, trajectory planning, coordinate calculating, data saving, and controlling robot arm movements.
Robot-assisted operation principles
The robot-assisted surgical system has two major designs: (1) spatial guidance: to obtain the spatial coordinates of the planned surgical trajectory, (2) trajectory positioning: to control the movement of the robot according to the spatial coordinates of the planned trajectory and move the cannula system to the surgical position.
The system collects two fluoroscopic images using C-arm in different directions during the surgery for screw trajectory planning and spatial positioning. The imaging principle of C-arm conforms to the imaging principle of a pinhole camera, to acquire the spatial location of the surgical trajectory through a biplane localization algorithm. In controlling the movement of each joint of the robot arm, the sleeve fixed at the distal end of the robot arm will move exactly in reference to the planned trajectory. Firmly holding the sleeve, the operator can place guide wires along the sleeve, after which the cannulated screws can be inserted.
Robot-assisted sacroiliac screw implantation
Possessing the only registered license from the Food-Drug Administration in China, TiRobot™ has been certified for use in orthopedic surgery, including SI screw implantation. At the beginning of the surgical procedure, the patient was prepared through positioning, sterilizing, and draping. The patient tracker was fixed on the contralateral anterior superior iliac spine of the surgical side and a C-arm was placed on the same side of the patient. All parts of the robot were placed on the distal side of the patient, while the robot tracker and calibrator were assembled at the distal end of the robot arm. After the calibrator was fixed, pelvic inlet, outlet, and lateral intraoperative fluoroscopic images were taken. The fluoroscopic images were automatically imported into the planning and controlling workstation. Based on these fluoroscopic images, the surgeon planned the surgical trajectory for SI screw insertion and generated spatial positioning orders for the robot arm. The arm was moved automatically according to orders from the surgical planning and controlling workstation and completed the surgical trajectory positioning.
During the positioning process, the surgeon controlled accuracy through adjusting the screw trajectory on the fluoroscopic image, as necessary. When the positioning accuracy was <1.00 mm, the guide wire was placed into the sleeve. The instrumentation was then concluded through implantation and fixation of the SI screw over the guide wire without the assistance of the robot. Following the implantation, the surgeon verified accuracy through a comparison between the inserted screw's position and the intraoperative planned screw's position through fluoroscopy.
Study parameters
The primary end point of the study was the position of the SI screws, assessed using a postoperative computed tomography (CT) scan. Experts not involved in the treatment evaluated all cases, using a double-blind method. According to Gras et al.,[16] the evaluation criteria of screw placement can be set as follows: excellent, entirely within the cortical margins of the sacrum with no contact to any cortical border of the sacrum; good, partially contact the cortical bone without piercing, and; poor, penetrating the cortical bone. The quality rating of screw placement in this study was evaluated using this system.
As secondary end points, the duration of trajectory planning, the duration of surgery after reduction of the pelvis, the insertion time of the guide wire during surgery (if the number of implant screws was greater than one in one case, the mean value was calculated), the number of guide wire attempts made during surgery (if the number of implant screws was greater than one in one case, the mean value was calculated), and the radiation exposure after pelvic reduction were assessed.
Furthermore, patients’ sex, age, levels of instrumentation, and number of instrumented levels were acquired.
Statistical analysis
In this study, statistical software (IBM SPSS Statistics 22; SPSS Inc., Chicago, Illinois, USA) was used for all statistical analyses. Comparisons of sex and the number of screws per level between groups were undertaken using a Chi-square test. Patient's age and some quantitative indexes, involving operation time, guide wire insertion time, and intraoperative radiation exposure time were compared using a Kruskal-Wallis H-test. Additionally, Fisher's exact probability test was used to analyze the screw positions. A 5% significance level was applied for all tests (P < 0.05). The clinical data were represented as median (Q1, Q3).
RESULTS
In the study, thirty patients were included and randomized in a 1:1 ratio for conventional freehand or robot-assisted SI screw implantation. Patient data are summarized in Table 1. In brief, there were no significant differences regarding median patient age (43.0 (35.0, 52.0) years vs. 36.0 (25.0, 47.0) years; χ2 = 0.911, P = 0.340) and the male/female ratio (χ2 = 0.556, P = 0.710) between both the groups.
Table 1.
Study parameters for conventional freehand or robot-assisted Sacroiliac screw implantation
| Items | Freehand (n = 22) | Robot assisted (n = 23) | χ2 | P |
|---|---|---|---|---|
| Age (years), median (Q1, Q3) | 43.0 (35.0, 52.0) | 36.0 (25.0, 47.0) | 0.911 | 0.340 |
| Sex (male/female), n | 8/7 | 10/5 | 0.556 | 0.710 |
| Median planning time (min) | Not applicable | 7.8 | – | – |
| Operation time (min), median (Q1, Q3) | 104.0 (60.0, 154.0) | 150.0 (75.0, 230.0) | 1.990 | 0.158 |
| Guide wire insertion time (min), median (Q1, Q3) | 19.0 (15.5, 45.0) | 2.0 (2.0, 2.7) | 20.952 | <0.001 |
| Number of guide wire attempts, median (Q1, Q3) | 7.0 (2.0, 9.0) | 1.0 (1.0, 1.0) | 15.771 | <0.001 |
| Intraoperative radiation exposure (s), median (Q1, Q3) | 36.0 (21.5, 48.0) | 6.0 (6.0, 9.0) | 13.590 | <0.001 |
The median duration of intraoperative planning of screw trajectories using TiRobot™ software was 7.8 min for robot-assisted group, whereas no planning time was necessary for the freehand group. Surprisingly, the median operation time from the end of pelvic reduction to the end of the operation was not different between the freehand group and the robot-assisted group (150.0 (75.0, 230.0) min vs. 104.0 (60.0, 154.0) min; χ2 = 1.990, P = 0.158). Although the operation time after reduction of the pelvis was not significantly different, the median surgical time for the guide wire implantation was significantly shorter in the robot-assisted group than that in the freehand group (2.0 [2.0, 2.7] min vs. 19.0 [15.5, 45.0] min; χ2 = 20.952, P < 0.001). During the guide wire implantation, the number of the lead wire attempts was significantly different between the freehand group and the robot-assisted group (7.0 [2.0, 9.0] times vs. 1.0 [1.0, 1.0] time; χ2 = 15.771, P < 0.001). The number of guide wire attempts in the robot-assisted group was significantly less than that in the freehand group.
The robot-assisted group required additional planning for fluoroscopic radiography, which was not necessary for the freehand group. Nevertheless, after pelvic reduction, the median time of intraoperative radiation needed was 6.0 (6.0, 9.0) s in the robot-assisted group and 36.0 (21.5, 48.0) s in the freehand group (χ2 = 13.590, P < 0.001). This suggested that the differences between the two groups had statistical significance. The intraoperative fluoroscopy time required for the robot-assisted group was significantly shorter than that of the freehand group.
There were no differences in the instrumented iliosacral levels between the two groups, which were from S1 to S2 [χ2 = 4.760, P = 0.093; Table 2].
Table 2.
Number of screws per level and group
| Instrumented SVB | Freehand (n = 22) | Robot assisted (n = 23) | Total (n = 45) | χ2 | P |
|---|---|---|---|---|---|
| S1 (single) | 13 | 9 | 22 | 4.760 | 0.093 |
| S2 (single) | 9 | 10 | 19 | ||
| S1 (double) | 0 | 4 | 4 |
SVB: Sacral vertebral body.
Screw positions, according to the classifications used by Gras and Marintschev, are summarized in Table 3. Of 45 implanted screws, 22 were implanted in patients from the freehand group and 23 were implanted in patients from the robot-assisted group. There were no postoperative complications including nerve palsy and revisions in the two groups. The excellent and good rate of screw placement in the robot-assisted group was 100% and higher than 95% in the freehand group. Furthermore, P = 0.009, based on comparisons between the screw distributions in the two groups, which meant that the screw distribution of the robot-assisted group was better than that of the freehand group.
Table 3.
Comparison of screw positions utilizing the Florian Gras and Ivan Marintschev classification
| Screw position | Freehand (n = 22) | Robot assisted (n = 23) | Total (n = 45) | P |
|---|---|---|---|---|
| Excellent | 16 | 23 | 39 | 0.009 |
| Good | 5 | 0 | 5 | |
| Poor | 1 | 0 | 1 |
Illustrative clinical case 1
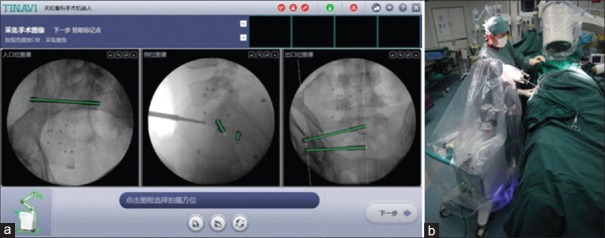
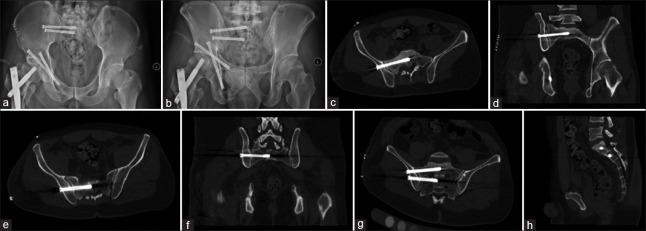
A 33-year-old male patient sustained pelvic fractures in a car accident. The preoperative X-ray film and CT scan showed a C3-type injury involving sacral fractures combined with separation of the SI joint [Figure 2]. The patient was treated with SI screw fixation using TiRobot™ [Figure 3]. Different from conventional freehand technique, the workstation of the robot can plan and calculate the surgical trajectory of the SI screw. To verify the accuracy of robotic planning intraoperatively, fluoroscopy verification for guide wire insertion was necessary [Figure 4]. Postoperative images showed that the positioning of the S1 and S2 screws had been excellent according to evaluation criterion [Figure 5].
Figure 2.
The patient was examined preoperatively by X-ray and computed tomography scan, the result was sacral fractures combined with separation of the sacroiliac joint.
Figure 3.
Planning image of the sacroiliac screw on pelvis inlet, outlet, and lateral sides (a); Implantation of sacroiliac screws with the robot (b).
Figure 4.
Verifying the location of guide wires and sacroiliac screws intraoperatively. (a) Inlet view of guide wires’ location, (b) outlet view of guide wires’ location, (c) inlet view of SI screws’ location, (d) outlet view of SI screws’ location, (e) lateral view of sacroiliac screws’ location.
Figure 5.
The patient was examined by X-ray and computed tomography scan postoperatively. (a) Inlet view, (b) outlet view, (c) S1 axial computed tomography scan, (d) S1 coronal computed tomography scan, (e) S2 axial computed tomography scan, (f) S2 coronal computed tomography scan, (g) angled sacral coronal computed tomography scan, (h) sacral sagittal computed tomography scan.
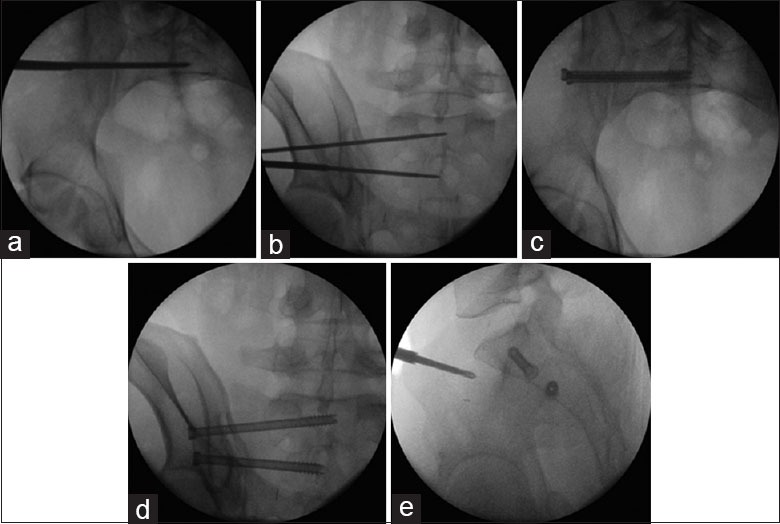
Illustrative clinical case 2
A 24-year-old female patient was admitted for surgery four days after a car accident injury. According to the preoperative examination, there were sacral fractures combined with separation of the SI joint. The operator implanted screws using the freehand technique, but the S1 screw passed in-out-in between the sacrum and the ilium, which was found in the postoperative X-ray image and CT scan [Figure 6]. However, there were no postoperative complications including nerve palsy and revision.
Figure 6.
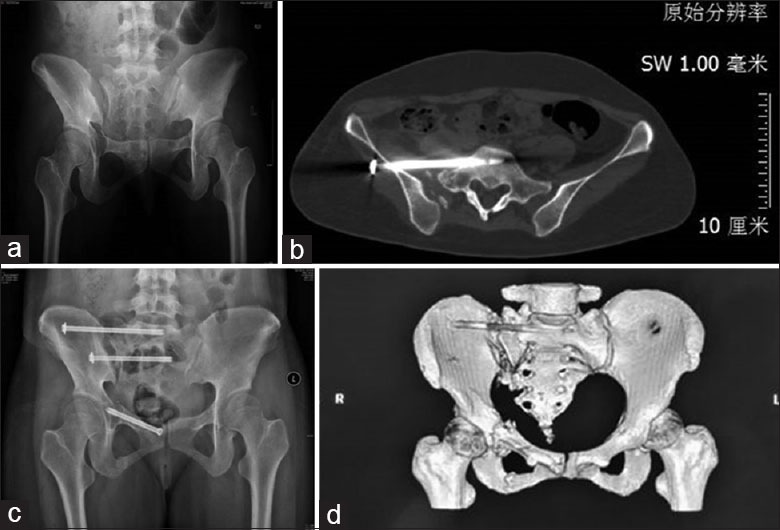
By contrast between pre- and post-operative images, the S1 screw passing “in-out-in” between the sacrum and the ilium was found. (a) Preoperative outlet view, (b) postoperative computed tomography image, (c) postoperative outlet view, (d) postoperative reconstruction computed tomography image.
DISCUSSION
Over several years, novel medical robotics, as well as computer-assisted surgery equipment and instrumentation, have been continuously introduced into orthopedic surgery rooms throughout the world, but lately their clinical benefits have been strongly challenged.[15,16] Frequently, considerable financial investment is required to serve a somewhat limited field of applications, such as total joint replacement or spine pedicle screw placement. As a result, the future of these devices is unpredictable. The most common application of computer-assisted orthopedic surgery in trauma is in the placement of iliosacral screws. Pelvic fixation “opportunity tunnels” are narrow and multiplanar images are necessary to avoid damage to vulnerable nearby neurovascular structures, such as the L5 and S1 nerve roost, cauda equina at the level of the first sacral vertebra, and the crossing of the femoral vein and artery superior to the superior pubic bone.[17] Pelvic ring injuries that are treated with iliosacral screws, using image-guided navigation, show 96% of well-placed screws in postoperative radiographs and CT scans,[18,19] but a medical robotic system has not yet been established for percutaneous iliosacral screw placement. In contrast to navigation, robots not only allow the surgeon to know the alignment of the guide wire in real time corresponding to intraoperative fluoroscopy, but also guide or assist the surgeon to perform the operation. Medical robotic systems for orthopedic surgery have been developed, but most studies about robot-assisted iliosacral surgery are based on studies using cadavers.[19,20] In this prospective study, in terms of a relatively large number of patients, we aimed to determine whether the percutaneous iliosacral screw implantation could be optimized, through evaluating the grade of position and whether the intraoperative radiation exposure could be reduced using a robot-assisted technique.[20,21,22]
The central finding of this study is that the accuracy of the robot-assisted technique was superior to the conventional freehand technique. Furthermore, intraoperative radiation exposure was reduced with robotic assistance. Surprisingly, the operation time after pelvic reduction was not different between the groups. This finding indicates that the setup of the TiRobot™ navigation system is not cumbersome or tends to take up too much additional time, (usually only 5 min), which we propose is an acceptable amount of time for a new technique. Moreover, the time for guide wire implantation was significantly shorter in the robot-assisted group than in the freehand group, owing to a reduced number of guide wire attempts and an increase in stable, precise manipulation in the robot-assisted group. As proven in the current study, for S1 and S2 instrumentation, robot-assisted navigation can increase the accuracy of the implant position and reduce intraoperative radiation exposure. In addition, the robot-assisted navigation system has the advantages of avoiding: (1) multiple false passages that may be of potential harm to patients (e.g., an error in positioning the sacral passage could result in nerve root damage); (2) multiple drill holes that may lead to screw loosening; and (3) joint penetration through inaccurate measurement and positioning of the implant. Therefore, several aspects may have contributed to the superior results of our study.
The most important safety aspect of TiRobot™ was derived from the electro-optical camera and the robot arm, based on a specific biplane orientation algorithm to realize a high-precision and stable operation. The novel biplane algorithm can calculate the screw trajectory, depending on two intraoperative fluoroscopy images. According to the calculated surgical trajectory, the robot arm moves automatically to the right position and maintains a precise and steady sleeve. During the robot arm movement, the electro-optical navigation system can monitor the sleeve over the planning trajectory in real time. Therefore, an excellent intraosseous screw position was found in most complete cases with TiRobot™ assistance, which is likely due to fluoroscopy-based navigation in combination with the semi-active robot guide. Another safety aspect of using the applicable and modularized design of the robot structure is avoiding complications in the assembly process, which lead to reducing the setup time of the TiRobot™. Generally, it is not necessary to repeatedly verify the surgical trajectory using intraoperative fluoroscopy. The high precision of the specific biplane orientation software, based on two intraoperative fluoroscopy images, could explain the reduction of radiation exposure to the robot-assisted group.
Most studies reporting robot use in pelvic trauma were performed on saw bone or cadaveric bone. That is a different scenario from real life, with no soft-tissue tethers. The safety and accuracy of robot-assisted orthopedic surgery, measured through the number of drilling attempts, screw positioning, and radiation time, have been shown to be superior to conventional techniques. However, there are some disadvantages with the robot-assisted navigation system: (1) the surgeon must be constantly aware of the position of the navigation machine and should avoid the path between the trackers and the detector. Blocking the field of view of these cameras will cause loss of tool reference, which might be frustrating, but is not critical for the operation; (2) inserting trackers in the iliac spine for registration is an extra step that must be undertaken. It carries minimal risk but definite discomfort to the patient. It has to be undertaken so as not to be on the placement site of the implant and also it has to be placed for the navigation machine to detect it at all times; and (3) using a robot-assisted navigation system adds to the cost of the surgery, including the cost of the machine, the cost of the personnel responsible to operate the machine, and the cost of replacing trackers when they have decreased sensitivity. However, the technology may be already implemented in other hospital service lines, such as neurosurgery or arthroplasty, and a transfer to orthopedic use is likely to be less demanding in that case.
There are some limitations to this study. We demonstrate a comparative study between a robot-assisted technique and a conventional freehand technique. However, the required image-aided navigation technique has not been involved in the present study. The second limitation is the lack of long-term functional outcome results. Our study does confirm the superior accuracy and efficiency of the TiRobot™ system in SI screw fixation for unstable pelvic injury, thus warranting future studies to further define its potential clinical role.
Financial support and sponsorship
This study was supported by grants from the National Natural Science Foundation of China (No. F010401) and the National Key Research and Development Program of China during the 13th Five-Year Plan Period (No. 2016YFC0105802).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank Mr. Zhen-Dong Guo from the Medical Robotic Engineering Laboratory for assistance in providing the photographs of the TiRobot™. The data analysis was supported, in part, by Xi Chen from the Medical Robotic Engineering Laboratory, TINAVI Medical Technology Co., Ltd.
Footnotes
Edited by: Ning-Ning Wang
REFERENCES
- 1.Schweitzer D, Zylberberg A, Córdova M, Gonzalez J. Closed reduction and iliosacral percutaneous fixation of unstable pelvic ring fractures. Injury. 2008;39:869–74. doi: 10.1016/j.injury.2008.03.024. doi: 10.1016/j.injury.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 2.Routt ML, Jr, Nork SE, Mills WJ. Percutaneous fixation of pelvic ring disruptions. Clin Orthop Relat Res. 2000;375:15–29. doi: 10.1097/00003086-200006000-00004. doi: 10.1097/00003086-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Routt ML, Jr, Simonian PT, Mills WJ. Iliosacral screw fixation: Early complications of the percutaneous technique. J Orthop Trauma. 1997;11:584–9. doi: 10.1097/00005131-199711000-00007. doi: 10.1097/00005131-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Giannoudis PV, Tzioupis CC, Pape HC, Roberts CS. Percutaneous fixation of the pelvic ring: An update. J Bone Joint Surg Br. 2007;89:145–54. doi: 10.1302/0301-620X.89B2.18551. doi: 10.1302/0301-620X.89B2.18551. [DOI] [PubMed] [Google Scholar]
- 5.Altman DT, Jones CB, Routt ML., Jr Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma. 1999;13:220–7. doi: 10.1097/00005131-199903000-00011. doi: 10.1097/00005131-199903000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Stephen DJ. Pseudoaneurysm of the superior gluteal arterial system: An unusual cause of pain after a pelvic fracture. J Trauma. 1997;43:146–9. doi: 10.1097/00005373-199707000-00037. doi: 10.1097/00005373-199707000-00037. [DOI] [PubMed] [Google Scholar]
- 7.Stöckle U, König B, Hofstetter R, Nolte LP, Haas NP. Navigation assisted by image conversion. An experimental study on pelvic screw fixation. Unfallchirurg. 2001;104:215–20. doi: 10.1007/s001130050717. doi: 10.1007/s001130050717. [DOI] [PubMed] [Google Scholar]
- 8.Hinsche AF, Giannoudis PV, Smith RM. Fluoroscopy-based multiplanar image guidance for insertion of sacroiliac screws. Clin Orthop Relat Res. 2002;395:135–44. doi: 10.1097/00003086-200202000-00014. doi: 10.1097/00003086-200202000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Templeman D, Schmidt A, Freese J, Weisman I. Proximity of iliosacral screws to neurovascular structures after internal fixation. Clin Orthop Relat Res. 1996;329:194–8. doi: 10.1097/00003086-199608000-00023. doi: 10.1097/00003086-199608000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Salari P, Moed BR, Bledsoe JG. Supplemental S1 fixation for type C pelvic ring injuries: Biomechanical study of a long iliosacral versus a transsacral screw. J Orthop Traumatol. 2015;16:293–300. doi: 10.1007/s10195-015-0357-8. doi: 10.1007/s10195-015-0357-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bastian JD, Jost J, Cullmann JL, Aghayev E, Keel MJ, Benneker LM. Percutaneous screw fixation of the iliosacral joint: Optimal screw pathways are frequently not completely intraosseous. Injury. 2015;46:2003–9. doi: 10.1016/j.injury.2015.06.044. doi: 10.1016/j.injury.2015.06.044. [DOI] [PubMed] [Google Scholar]
- 12.Zwingmann J, Konrad G, Kotter E, Südkamp NP, Oberst M. Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin Orthop Relat Res. 2009;467:1833–8. doi: 10.1007/s11999-008-0632-6. doi: 10.1007/s11999-008-0632-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang JQ, Zhao CP, Su YG, Zhou L, Hu L, Wang TM, et al. Computer-assisted navigation systems for insertion of cannulated screws in femoral neck fractures: A comparison of bi-planar robot navigation with optoelectronic navigation in a Synbone hip model trial. Chin Med J. 2011;124:3906–11. doi: 10.3760/cma.j.issn. 0366-6999.2011.23.014. [PubMed] [Google Scholar]
- 14.Wu T, Chen W, Zhang Q, Zheng ZL, Lyu HZ, Cui YW, et al. Biomechanical comparison of two kinds of internal fixation in a type C zone II pelvic fracture model. Chin Med J. 2015;128:2312–7. doi: 10.4103/0366-6999.163377. doi: 10.4103/0366-6999.163377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lang JE, Mannava S, Floyd AJ, Goddard MS, Smith BP, Mofidi A, et al. Robotic systems in orthopaedic surgery. J Bone Joint Surg Br. 2011;93:1296–9. doi: 10.1302/0301-620X.93B10.27418. doi: 10.1302/0301-620X.93B10.27418. [DOI] [PubMed] [Google Scholar]
- 16.Gras F, Marintschev I, Wilharm A, Klos K, Mückley T, Hofmann GO. 2D-fluoroscopic navigated percutaneous screw fixation of pelvic ring injuries – A case series. BMC Musculoskelet Disord. 2010;11:153. doi: 10.1186/1471-2474-11-153. doi: 10.1186/1471-2474-11-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu XB, Wang JQ, Zhao CP, Sun X, Shi Y, Zhang ZA, et al. Printed three-dimensional anatomic templates for virtual preoperative planning before reconstruction of old pelvic injuries: Initial results. Chin Med J. 2015;128:477–82. doi: 10.4103/0366-6999.151088. doi: 10.4103/0366-6999.151088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ringel F, Stüer C, Reinke A, Preuss A, Behr M, Auer F, et al. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: A prospective randomized comparison to conventional freehand screw implantation. Spine (Phila Pa 1976) 2012;37:E496–501. doi: 10.1097/BRS.0b013e31824b7767. doi: 10.1097/BRS.0b013e31824b7767. [DOI] [PubMed] [Google Scholar]
- 19.Zwingmann J, Konrad G, Mehlhorn AT, Südkamp NP, Oberst M. Percutaneous iliosacral screw insertion: Malpositioning and revision rate of screws with regards to application technique (navigated vs. Conventional) J Trauma. 2010;69:1501–6. doi: 10.1097/TA.0b013e3181d862db. doi: 10.1097/TA. 0b013e3181d862db. [DOI] [PubMed] [Google Scholar]
- 20.Oszwald M, Westphal R, Bredow J, Calafi A, Hufner T, Wahl F, et al. Robot-assisted fracture reduction using three-dimensional intraoperative fracture visualization: An experimental study on human cadaver femora. J Orthop Res. 2010;28:1240–4. doi: 10.1002/jor.21118. doi: 10.1002/jor.21118. [DOI] [PubMed] [Google Scholar]
- 21.Pieske O, Landersdorfer C, Trumm C, Greiner A, Wallmichrath J, Gottschalk O, et al. CT-guided sacroiliac percutaneous screw placement in unstable posterior pelvic ring injuries: Accuracy of screw position, injury reduction and complications in 71 patients with 136 screws. Injury. 2015;46:333–9. doi: 10.1016/j.injury.2014.11.009. doi: 10.1016/j.injury.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Takao M, Nishii T, Sakai T, Yoshikawa H, Sugano N. Iliosacral screw insertion using CT-3D-fluoroscopy matching navigation. Injury. 2014;45:988–94. doi: 10.1016/j.injury.2014.01.015. doi: 10.1016/j.injury.2014.01.015. [DOI] [PubMed] [Google Scholar]