Abstract
Background:
Lateral compartmental osteoarthritis (LCOA), a major complication after medial mobile-bearing unicompartmental knee arthroplasty (UKA), is highly associated with the increased stress of the lateral compartment. This study aimed to analyze the effects on the stress and load distribution of the lateral compartment induced by lower limb alignment and coronal inclination of the tibial component in UKA through a finite element analysis.
Methods:
Eight three-dimensional models were constructed based on a validated model for analyzing the biomechanical effects of implantation parameters on the lateral compartment after medial Oxford UKA: postoperative lower limb alignment of 3° valgus, neutral and 3° varus, and the inclination of tibial components placed in 4°, 2° valgus, square, and 2° and 4° varus. The contact stress of femoral and tibial cartilage and load distribution were calculated for all models.
Results:
In the 3° valgus lower limb alignment model, the contact stress of femoral (3.38 MPa) and tibial (3.50 MPa) cartilage as well as load percentage (45.78%) was highest compared to any other model, and was increased by 36.75%, 47.70%, and 27.63%, respectively when compared to 3° varus. In the condition of a neutral position, the outcome was comparable for the different tibial tray inclination models. The inclination did not greatly affect the lateral compartmental stress and load distribution.
Conclusions:
This study suggested that slightly varus (undercorrection) lower limb alignment might be a way to prevent LCOA in medial mobile-bearing UKA. However, the inclination (4° varus to 4° valgus) of the tibial component in the coronal plane would not be a risk factor for LCOA in neutral position.
Keywords: Finite Element Analysis, Lateral Compartmental Osteoarthritis, Lower Limb Alignment, Tibial Component Inclination, Unicompartmental Knee Arthroplasty
INTRODUCTION
Unicompartmental knee arthroplasty (UKA) has regained popularity in recent years as an excellent treatment for patients with single compartment knee osteoarthritis. With more of the functional anatomy unaffected, UKA offered a more rapid recovery and better restored the knee kinetics than total knee arthroplasty in selected patients.[1,2] The exceptional long-term survivorship and excellent function of UKA has been reported by a number of studies.[2,3,4] However, the progression of lateral compartmental osteoarthritis (LCOA) is one of the major downsides of UKA.[4,5] Other downsides to UKA are the wear of the polyethylene (PE) bearing, aseptic loosening, tibial femoral instability, fatigue failure of the tibia tray and infection.[5,6]
LCOA progression due to an altered stress pattern in the cartilage has been described in the literature.[7] Wear of lateral compartment has been attributed to abnormal cartilage stress, which can be strongly related with the postoperative lower limb alignment.[8,9] In addition, the tibial component inclination may affect the contact stress and load percentage in the lateral compartment.[10,11] Numerous finite element (FE) analyses of UKA have already advised on the postoperative lower limb alignment and inclination of the tibial component, but their results vary.[10,12,13] The aim of this study was to analyze the influence of the postoperative lower limb alignment and the tibial component coronal inclination on static knee biomechanics after mobile-bearing UKA using FE analysis.
METHODS
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of China-Japan Friendship Hospital. Informed written consent was obtained from the participate before enrollment in this study.
Intact knee model design
This study was conducted between November 2015 and June 2017 in China-Japan Friendship Hospital. An intact knee model was developed from computed tomography (CT), and magnetic resonance imaging (MRI) scans of the left knee joint of a 40-year-old healthy male (175 cm, 70 kg). CT (setting: 120 kV; 15 mA; slice thickness: 1 mm) was used to identify the bone structure. MRI (setting: Echo time 36 ms; repetition time 1300 ms; slice thickness: 1 mm; flip angle 90°) was used to generate cartilage, menisci, and four principal ligaments: lateral collateral ligament, medial collateral ligament, anterior cruciate ligament, and posterior cruciate ligament. Three-dimensional (3D) reconstruction and editing of the knee joint model were performed in Mimics 17.0 and 3-Matic 9.0 in-silico (Materialise Ltd., Leuven, Belgium). The initial graphics exchange specification files exported from Mimics were processed into Rapidform 2006 (INUS Technology, Inc., Seoul, Korea) to form solid models. These were imported into the FE analysis software Abaqus/Standard 6.14 (Dassault Systems Simulia Corp., Providence, RI, USA) for assembling [Figure 1a].
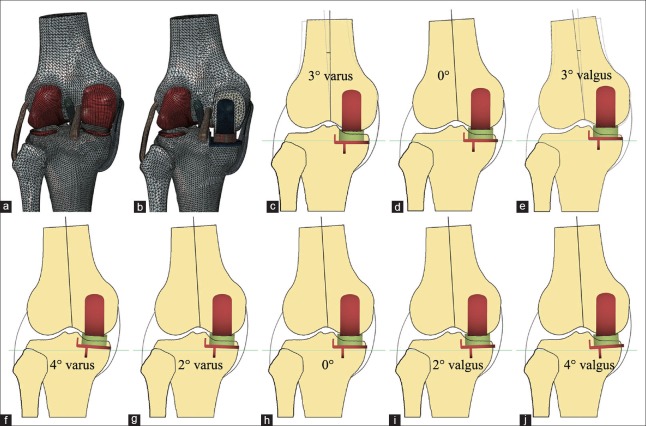
Figure 1.
The finite element models used in this study. (a) validated native knee model; (b) medial mobile-bearing UKA model with square (0°) inclination and neutral lower limb alignment; (c-e) medial mobile-bearing UKA models with the different lower limb alignments; (f-j) medial mobile-bearing UKA models with the different inclinations of the tibial tray. UKA: Unicompartmental knee arthroplasty.
Cartilage, menisci, cortical, and cancellous bone were all modeled as linear elastic isotropic material, as previously described [Table 1].[14] Ligament models were considered isotropic and hyperelastic materials to represent their nonlinear stress-strain relations, represented by an incompressible Neo-Hookean behavior with an energy density function of Ψ = C1× (I1− 3), where C1 is the initial shear modulus and I1 the first modified invariant of the right Cauchy-Green strain tensor.[11] C1 values were 6.06, 6.43, 5.83, and 6.06 MPa for the lateral collateral ligament, medial collateral ligament, anterior cruciate ligament, and posterior cruciate ligament, respectively.[15] The interfaces between cartilage and bones were modeled as fully bonded.[14] Both menisci were attached to the tibia at the horns.[15]
Table 1.
Material properties incorporated into the finite element models
| Items | Young’s modulus (MPa) | Poisson’s ratio |
|---|---|---|
| CoCrMo ally | 195,000.0 | 0.30 |
| UHMWPE | 685.0 | 0.40 |
| Cortical bone | 17,000.0 | 0.30 |
| Cancellous bone | 350.0 | 0.25 |
| Cartilage | 15.0 | 0.46 |
| Meniscus | 27.5 | 0.33 |
CoCrMo ally: Cobalt-chromium-molybdenum ally; UHMWPE: Ultra-high-molecular-weight-polyethylene.
Unicompartmental knee arthroplasty knee model definition
Solid models of Oxford UKA (Biomet UK Ltd., Swindon, UK) were offered by the manufacturer and imported into the intact knee model. Bones were trimmed and implanted virtually with the prostheses according to the standard surgical procedure for creating the UKA FE model in Abaqus/Standard 6.14.[3] Based on the dimensions of the femur and the tibia, size “M” was chosen for the femoral component and size “C” for the tibial tray. A bearing thickness of 4 mm was considered adequate for this study. The UKA was initially implanted whereby the femoral component, bearing, and tibial component all aligned with the long axis of the tibia. The neutrally aligned tibial tray was defined as having a square (0°) inclination in the coronal plane and a posterior slope of 7° in the sagittal plane [Figure lb].[11]
Next, a total of three different lower limb alignments were adopted and investigated [Figure 1c–1e]. The model with a neutral lower limb alignment was the model with square (0°) inclination of the UKA tibial tray. 3° valgus and 3° varus lower limb alignments were achieved by equivalent reposition of the mechanical axis of the femur. Furthermore, based on the square inclination position, the tibial tray and bearing were rotated around the stationary axis paralleled to the lateral edge of the tibial tray and passed through the center of the femoral component peg. A total of five different tibial tray positions were modeled in the coronal plane while maintaining a 7° posterior slope in the sagittal plane, and without changing the height of the joint surface. These additional models were: square inclination, 2° and 4° valgus inclination, and 2° and 4° varus inclination [Figure 1f–1j].
A total of eight models were constructed in this study for FE analysis. Medial tibial plateau in each UKA model was fully covered by the same size of the tibial tray, and the component overhang was <3 mm in all models (additional overhang would cause the implant keel to break through the proximal tibia cortex).[13] The material of the femoral component and tibial tray was cobalt-chromium-molybdenum ally, and the bearing was ultra-high-molecular-weight-PE. All the materials were assumed to be linear elastic isotropic in all FE models [Table 1].[14]
Load and boundary conditions
The tibial tray and femoral component in these models were fully bonded to the femur and tibia bone respectively, simulating the use of cement.[16] The PE mobile-bearing was free to translate and rotate with respect to the surface of the tibial tray.[14,16] A Coulomb friction contact model (μ = 0.07) was used to simulate the contact surfaces between the bearing and metal components for all UKA models.[11]
A compressive axis load of 1000 N, consistent with the load magnitude in previous studies, was applied to the mid-point of the transepicondylar axis in the femur in the model validation step.[10,12,17] The femur was constrained only in flexion-extension while the tibia and fibula were completely fixed at their distal ends.[15,17] The results of load distribution, contact pressures, and contact areas were similar to the previous study.[17] Therefore, the UKA models founded in this study and the following analyses were considered reasonable. Then, the same load as above was once again applied to all UKA models, but this time, the femurs were only allowed to freely rotate in varus-valgus, referring to a previous in vitro experiment, while other boundary conditions remained the same.[18]
Finite element analysis
Abaqus/Standard version 6.14 was used to perform all the FE simulations. Bone structures in all models were meshed by tetrahedral elements; other structures were meshed by hexahedral elements with an approximate element size of 2 mm [Figure 1a]. Sensitivity analysis determined that increasing the element density did not influence the predictive power of the model and greatly increase analysis time owing to the nature of the explicit FE method. A convergence test was performed on element size for the tibial bone to ensure that peak von Mises stresses did not change by more than 5%.[19] Finally, the contact stress in the lateral compartment and load distribution between the medial and lateral compartment were calculated and shown on all surfaces of the 3D FE model.
RESULTS
The relative load distribution between the medial and lateral compartments of the knee joint was measured for the numerical models with a UKA in the different postoperative lower limb alignment and tibial tray inclination configurations. The values of contact stress and load percentages in the lateral compartments for all analyzed knee models are reported in Tables 2 and 3. It was particularly interesting to see a decrease in the values of femoral and tibial contact stresses and the load percentage from 3° valgus to 3° varus lower limb alignment [Table 2]. Yet, the values of contact stress and load percentage slightly increased from 4° valgus to 4° varus of tibial tray inclination [Table 3].
Table 2.
The values of contact stresses and load percentage in lateral compartments of different lower limb alignments after medial mobile-bearing unicompartmental knee arthroplasty
| Models | Contact stress of femoral cartilage (MPa) | Contact stress of tibial cartilage (MPa) | Lateral load percentage |
|---|---|---|---|
| 3° valgus | 3.38 | 3.50 | 45.78 |
| Neutral | 2.71 | 2.84 | 40.26 |
| 3° varus | 2.47 | 2.37 | 35.87 |
Table 3.
The values of contact stresses and load percentage in lateral compartments of different inclinations of the tibial tray after medial mobile-bearing unicompartmental knee arthroplasty
| Models | Contact stress of femoral cartilage (MPa) | Contact stress of tibial cartilage (MPa) | Lateral load percentage |
|---|---|---|---|
| 4° valgus | 2.61 | 2.71 | 39.79 |
| 2° valgus | 2.68 | 2.77 | 40.00 |
| 0° | 2.71 | 2.84 | 40.26 |
| 2° varus | 2.74 | 2.88 | 40.45 |
| 4° varus | 2.76 | 2.98 | 40.64 |
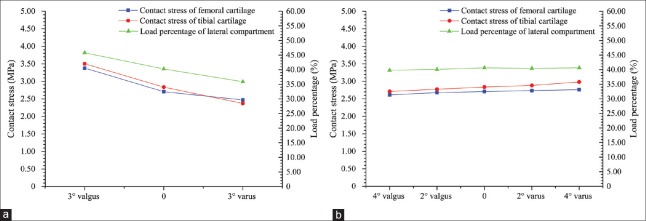
The changes in femoral and tibial cartilage contact stresses and the load distribution in the lateral compartment in each FE model are shown in Figure 2. The lateral contact stresses of femoral and tibial cartilage changed considerably especially in the 3° valgus, neutral, and 3° varus of the lower limb alignment. Figure 2a illustrates the contact stresses and load percentages in the lateral compartments and how they change with different lower limb alignments. In brief, the stress values of the femoral and tibial cartilage and load percentage in the lateral compartments were increased in the neutral position and higher in the 3° valgus lower limb alignment. However, the load percentages that were transferred through the lateral compartment remained almost unchanged by in the different inclinations of tibial component knee models. Similarly, also contact stresses were constant [Figure 2b].
Figure 2.
The contact stress of cartilage and load percentage in the lateral compartment for (a) the different lower limb alignments, and (b) the different inclinations of the tibial tray.
DISCUSSION
Unicompartmental knee replacement offers better kinematics and function than total knee arthroplasty for patients with isolated single compartment knee disease. However, LCOA is a major cause of the revision in medial mobile-bearing UKA. The altered lateral contact stress and load distribution, probably influenced by the lower limb alignment and the tibial component inclination, was related to LCOA. Numerous FE analyses of UKA already advised on the postoperative lower limb alignment and inclination of the tibial component, but their results varied. Each of these studies also had some limitations such as baseline FE models only reporting on the proximal tibia without the femur bone, the use of invalidated models, and direct load application to the tibial tray.[10,12,13] In this study, the 3D models included bony and soft tissue structures which were much closer to the natural knee in vivo, and the models were validated in a previous study to analyze biomechanical effects on the lateral compartment by tibial component inclination and lower limb alignment.
Our FE study suggested that the static knee biomechanics can be greatly affected by the coronal lower limb alignments after mobile-bearing UKA. Valgus lower limb alignment (overcorrection) may lead to revision because of lateral compartment degeneration.[7,8,18] This concept is supported to some extent by the results of this study because the contact stress and load percentage in the lateral compartment significantly increased in 3° valgus lower limb alignment knee models [Figure 2a]. Minor varus alignment may prevent LCOA with reduced contact stress of femoral (26.87% reduction) and tibial (32.30% reduction) cartilage and load percentage (21.65% reduction) in the lateral compartment when compared to the 3° valgus model, which is in agreement with a previous study.[20] Vasso and colleagues[21] pointed minor varus (≤7°) lower limb alignment provide better clinical outcome and long-term survivorship of medial UKA. Zuiderbaan et al.[22] suggested a postoperative lower limb alignment of 1–4° varus to achieve knee pain relief. However, excessive varus alignment may cause the PE wear, knee pain, aseptic loosing. Several studies reported marked varus alignment (≥8–10°) is associated with PE wear and implant loosing.[21,23] Some even suggested to avoid more than 5–6° varus for tibial component loosing.[24,25] Considering the above studies, it is generally accepted that the lower limb alignment should be slightly varus (undercorrected) for UKA.
Some factors cause the lower limb alignment to change after UKA. First, excessive release of medial soft tissue can lead to valgus overcorrection in patients treated with medial UKA.[26] On the other hand, a change in lower limb alignment can also be as a result of overstuffed UKA. Heyse and colleagues[27] found that over stuffing after UKA can lead to significantly more valgus and higher strains in the superficial medial collateral ligament. Innocenti et al.[7] also reported that the load in the lateral compartment increased in subjectively balanced and over-stuffed UKA knees, and may be caused by more valgus lower limb alignment. Understuffing of the medial compartment, however, led to kinematics closest to the native knee. In fact, alignment is determined by proximal tibia resection level, ligament stability, preoperative deformity, implant thickness, and surgical technique.[21,28]
Many studies of UKA have focused on effects of varus-valgus inclination of tibial component on bone stress, PE wear, and postoperative pain in the medial compartment.[10,12,29] Zhu et al.[11] found that valgus inclination (>4°) was not recommended for avoiding the tibia pain and that varus inclination (>4°) was associated with LCOA.[11] Chatellard et al.[24] found a decreased survival of medial UKA with a greater than 3° change in tibial component obliquity. Inoue and colleagues found that valgus inclination of 3° and 6° increased the risk of medial tibial condylar fractures.[30] Sawatari et al.[10] concluded that a slight two to four degree valgus inclination of a UKA tibial component may be preferable to varus or square inclination in the coronal plane. In general, excessive varus inclination has been reported to potentially significantly worsen the survivorship of UKA.[24,30] In the present study, we found that the percentage of load transferred through the lateral compartment, as well as contact stresses, remained similar when comparing different inclinations of tibial component knee models in neutral alignment [Figure 2b]. Nevertheless, the values of contact stress and load slightly increased, but may not have a significant influence on the lateral compartment.
This study has some limitations. First, we only designed three alignments and limited the analysis to study the effect of the tibial inclination in the condition of neutral position (not best alignment) on the lateral compartment. In future work, we will need to identify the best lower limb alignment and tibial component inclination for the appropriate balance of the forces on the medial and lateral compartment. Second, the structures of the FE models were specific to the volunteer and constructed from CT and MRI data. This means that the data can only be extrapolated with the greatest care due to patient-dependent structure segmentation in CT and MRI sequences depending. Third, the static loading condition in this study represented only normal gait in the stance phase near full extension. It is inadequate for conditions where the point of loading moves as it does in vivo to determine the optimal position on the basis of a single case. The dynamic simulation of the knee joint at varying knee flexion angles will be the individuals of further study.
In conclusion, this study has demonstrated that there is a large increase of contact stress in the lateral compartment when postoperative lower limb alignment was overcorrected. This might be the cause of LCOA progression and correcting for it might help to reduce the revision rate of UKA. However, the inclination (4° valgus to 4° varus) of the tibial component in the coronal plane did not obviously affect the lateral compartmental stress and load distribution in neutral alignment. Thus, much care must be taken with postoperative lower limb alignment, as UKA is a technically demanding surgical procedure.
Financial support and sponsorship
This study was supported by grants from the National Natural Science Foundation of China (No. 81673776), and the capital health research and development of special, China (No. 2016-2-4062).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Qiang Shi
REFERENCES
- 1.Mochizuki T, Sato T, Tanifuji O, Kobayashi K, Koga Y, Yamagiwa H, et al. In vivo pre- and postoperative three-dimensional knee kinematics in unicompartmental knee arthroplasty. J Orthop Sci. 2013;18:54–60. doi: 10.1007/s00776-012-0322-9. doi: 10.1007/s00776-012-0322-9. [DOI] [PubMed] [Google Scholar]
- 2.Ma T, Tu YH, Xue HM, Wen T, Cai MW. Clinical outcomes and risks of single-stage bilateral unicompartmental knee arthroplasty via Oxford phase III. Chin Med J. 2015;128:2861–5. doi: 10.4103/0366-6999.168042. doi: 10.4103/0366-6999.168042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pandit H, Jenkins C, Barker K, Dodd CA, Murray DW. The oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br. 2006;88:54–60. doi: 10.1302/0301-620X.88B1.17114. doi: 10.1302/0301-620X.88B1.17114. [DOI] [PubMed] [Google Scholar]
- 4.Emerson RH, Alnachoukati O, Barrington J, Ennin K. The results of Oxford unicompartmental knee arthroplasty in the United States: A mean ten-year survival analysis. Bone Joint J. 2016;98-B:34–40. doi: 10.1302/0301-620X.98B10.BJJ-2016-0480.R1. doi: 10.1302/0301-620X.98B10.BJJ-2016-0480.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim KT, Lee S, Lee JI, Kim JW. Analysis and treatment of complications after unicompartmental knee arthroplasty. Knee Surg Relat Res. 2016;28:46–54. doi: 10.5792/ksrr.2016.28.1.46. doi: 10.5792/ksrr.2016.28.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van den Heever DJ, Scheffer C, Erasmus P, Dillon E. Contact stresses in a patient-specific unicompartmental knee replacement. Clin Biomech (Bristol, Avon) 2011;26:159–66. doi: 10.1016/j.clinbiomech.2010.09.007. doi: 10.1016/j.clinbiomech.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Innocenti B, Bilgen ÖF, Labey L, van Lenthe GH, Sloten JV, Catani F, et al. Load sharing and ligament strains in balanced, overstuffed and understuffed UKA. A validated finite element analysis. J Arthroplasty. 2014;29:1491–8. doi: 10.1016/j.arth.2014.01.020. doi: 10.1016/j.arth.2014.01.020. [DOI] [PubMed] [Google Scholar]
- 8.Hernigou P, Deschamps G. Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2004;423:161–5. doi: 10.1097/01.blo.0000128285.90459.12. doi: 10.1097/01.blo.0000128285.90459.12. [DOI] [PubMed] [Google Scholar]
- 9.Borrego Paredes E, Barrena Sánchez P, Serrano Toledano D, Puente González AI, Fornell Pérez S, Domecq Fernández de Bobadilla G, et al. Total knee arthroplasty after failed unicompartmental knee arthroplasty. Clinical results, radiologic findings, and technical tips. J Arthroplasty. 2017;32:193–6. doi: 10.1016/j.arth.2016.06.035. doi: 10.1016/j.arth.2016.06.035. [DOI] [PubMed] [Google Scholar]
- 10.Sawatari T, Tsumura H, Iesaka K, Furushiro Y, Torisu T. Three-dimensional finite element analysis of unicompartmental knee arthroplasty – The influence of tibial component inclination. J Orthop Res. 2005;23:549–54. doi: 10.1016/j.orthres.2004.06.007. doi: 10.1016/j.orthres.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Zhu GD, Guo WS, Zhang QD, Liu ZH, Cheng LM. Finite element analysis of mobile-bearing unicompartmental knee arthroplasty: The influence of tibial component coronal alignment. Chin Med J. 2015;128:2873–8. doi: 10.4103/0366-6999.168044. doi: 10.4103/0366-6999.168044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iesaka K, Tsumura H, Sonoda H, Sawatari T, Takasita M, Torisu T, et al. The effects of tibial component inclination on bone stress after unicompartmental knee arthroplasty. J Biomech. 2002;35:969–74. doi: 10.1016/s0021-9290(01)00244-5. doi: 10.1016/s0021-9290(01)00244-5. [DOI] [PubMed] [Google Scholar]
- 13.Simpson DJ, Price AJ, Gulati A, Murray DW, Gill HS. Elevated proximal tibial strains following unicompartmental knee replacement – A possible cause of pain. Med Eng Phys. 2009;31:752–7. doi: 10.1016/j.medengphy.2009.02.004. doi: 10.1016/j.medengphy.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Kwon OR, Kang KT, Son J, Kwon SK, Jo SB, Suh DS, et al. Biomechanical comparison of fixed- and mobile-bearing for unicomparmental knee arthroplasty using finite element analysis. J Orthop Res. 2014;32:338–45. doi: 10.1002/jor.22499. doi: 10.1002/jor.22499. [DOI] [PubMed] [Google Scholar]
- 15.Peña E, Calvo B, Martínez MA, Doblaré M. A three-dimensional finite element analysis of the combined behavior of ligaments and menisci in the healthy human knee joint. J Biomech. 2006;39:1686–701. doi: 10.1016/j.jbiomech.2005.04.030. doi: 10.1016/j.jbiomech.2005.04.030. [DOI] [PubMed] [Google Scholar]
- 16.Hopkins AR, New AM, Rodriguez-y-Baena F, Taylor M. Finite element analysis of unicompartmental knee arthroplasty. Med Eng Phys. 2010;32:14–21. doi: 10.1016/j.medengphy.2009.10.002. doi: 10.1016/j.medengphy.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Bao HR, Zhu D, Gong H, Gu GS. The effect of complete radial lateral meniscus posterior root tear on the knee contact mechanics: A finite element analysis. J Orthop Sci. 2013;18:256–63. doi: 10.1007/s00776-012-0334-5. doi: 10.1007/s00776-012-0334-5. [DOI] [PubMed] [Google Scholar]
- 18.Chang TW, Yang CT, Liu YL, Chen WC, Lin KJ, Lai YS, et al. Biomechanical evaluation of proximal tibial behavior following unicondylar knee arthroplasty: Modified resected surface with corresponding surgical technique. Med Eng Phys. 2011;33:1175–82. doi: 10.1016/j.medengphy.2011.05.007. doi: 10.1016/j.medengphy.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 19.Kwon OR, Kang KT, Son J, Suh DS, Baek C, Koh YG, et al. Importance of joint line preservation in unicompartmental knee arthroplasty: Finite element analysis. J Orthop Res. 2017;35:347–52. doi: 10.1002/jor.23279. doi: 10.1002/jor.23279. [DOI] [PubMed] [Google Scholar]
- 20.Mullaji AB, Shetty GM, Kanna R. Postoperative limb alignment and its determinants after minimally invasive Oxford medial unicompartmental knee arthroplasty. J Arthroplasty. 2011;26:919–25. doi: 10.1016/j.arth.2011.03.008. doi: 10.1016/j.arth.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 21.Vasso M, Del Regno C, D’Amelio A, Viggiano D, Corona K, Schiavone Panni A, et al. Minor varus alignment provides better results than neutral alignment in medial UKA. Knee. 2015;22:117–21. doi: 10.1016/j.knee.2014.12.004. doi: 10.1016/j.knee.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 22.Zuiderbaan HA, van der List JP, Chawla H, Khamaisy S, Thein R, Pearle AD, et al. Predictors of subjective outcome after medial unicompartmental knee arthroplasty. J Arthroplasty. 2016;31:1453–8. doi: 10.1016/j.arth.2015.12.038. doi: 10.1016/j.arth.2015.12.038. [DOI] [PubMed] [Google Scholar]
- 23.Manzotti A, Cerveri P, Pullen C, Confalonieri N. Computer-assisted unicompartmental knee arthroplasty using dedicated software versus a conventional technique. Int Orthop. 2014;38:457–63. doi: 10.1007/s00264-013-2215-8. doi: 10.1007/s00264-013-2215-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chatellard R, Sauleau V, Colmar M, Robert H, Raynaud G, Brilhault J, et al. Medial unicompartmental knee arthroplasty: Does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res. 2013;99:S219–25. doi: 10.1016/j.otsr.2013.03.004. doi: 10.1016/j.otsr.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 25.Barbadoro P, Ensini A, Leardini A, d’Amato M, Feliciangeli A, Timoncini A, et al. Tibial component alignment and risk of loosening in unicompartmental knee arthroplasty: A radiographic and radiostereometric study. Knee Surg Sports Traumatol Arthrosc. 2014;22:3157–62. doi: 10.1007/s00167-014-3147-6. doi: 10.1007/s00167-014-3147-6. [DOI] [PubMed] [Google Scholar]
- 26.Tashiro Y, Matsuda S, Okazaki K, Mizu-Uchi H, Kuwashima U, Iwamoto Y, et al. The coronal alignment after medial unicompartmental knee arthroplasty can be predicted: Usefulness of full-length valgus stress radiography for evaluating correctability. Knee Surg Sports Traumatol Arthrosc. 2014;22:3142–9. doi: 10.1007/s00167-014-3248-2. doi: 10.1007/s00167-014-3248-2. [DOI] [PubMed] [Google Scholar]
- 27.Heyse TJ, El-Zayat BF, De Corte R, Scheys L, Chevalier Y, Fuchs-Winkelmann S, et al. Balancing UKA: Overstuffing leads to high medial collateral ligament strains. Knee Surg Sports Traumatol Arthrosc. 2016;24:3218–28. doi: 10.1007/s00167-015-3848-5. doi: 10.1007/s00167-015-3848-5. [DOI] [PubMed] [Google Scholar]
- 28.Kim KT, Lee S, Kim TW, Lee JS, Boo KH. The influence of postoperative tibiofemoral alignment on the clinical results of unicompartmental knee arthroplasty. Knee Surg Relat Res. 2012;24:85–90. doi: 10.5792/ksrr.2012.24.2.85. doi: 10.5792/ksrr.2012.24.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Innocenti B, Pianigiani S, Ramundo G, Thienpont E. Biomechanical effects of different varus and valgus alignments in medial unicompartmental knee arthroplasty. J Arthroplasty. 2016;31:2685–91. doi: 10.1016/j.arth.2016.07.006. doi: 10.1016/j.arth.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 30.Inoue S, Akagi M, Asada S, Mori S, Zaima H, Hashida M, et al. The valgus inclination of the tibial component increases the risk of medial tibial condylar fractures in unicompartmental knee arthroplasty. J Arthroplasty. 2016;31:2025–30. doi: 10.1016/j.arth.2016.02.043. doi: 10.1016/j.arth.2016.02.043. [DOI] [PubMed] [Google Scholar]