Abstract
Primary calcareous degeneration is a rare corneal disease. In the past 50 years, only four cases have been described. We present the case of a 26-year-old male patient with progressive calcium deposition in both eyes with negative laboratory parameters. For the first time, anterior segment optic coherence tomography was used to investigate and establish the proper treatment.
Keywords: Band keratopathy, calcareous degeneration, calcium, corneal transplantation
Band keratopathy, calcium salts in Bowman's layer, is the most classic form of corneal calcification seen in the clinical practice.[1] However, calcareous degeneration of the entire cornea is a very rare complication. Axenfeld, in the early 1900s, reported a bilateral case in an 8-year-old with a massive deposition of calcium phosphate located in the superficial and central strata of the parenchyma, slightly affecting Bowman's membrane and leaving the epithelium intact.[2] Secondary corneal calcium deposits were described due to hypercalcemic states, inherited and systemic diseases, anterior segment (AS) chronic inflammatory conditions, and chemical interaction (eyedrops with preservative).[3,4,5,6,7,8]
We describe a rare case of idiopathic bilateral calcareous degeneration of the cornea in a young adult, including AS optic coherence tomography (AS-OCT) and histopathological evaluation.
Case Report
A 26-year-old male Caucasian patient attended/presented at our Cornea and External Diseases Division with moderate visual loss in the right eye and severe visual loss in the left eye over the past 3 years. Visual acuity (Snellen) was 20/60 (0.48 logMAR) in the right eye and <20/400 (1.3 logMAR) in the left. The patient had no history of ocular or systemic disease, eyedrop use, trauma, familial visual impairment, or corneal dystrophy. Slit-lamp examination revealed a quiet and deep anterior chamber, no evidence of conjunctival inflammation, clear lenses, and deep and superficial crystalline corneal deposits without edema. Corneal deposits were mostly seen deeply in the posterior stromal/Descemet's from periphery to the center, central subepithelium, and Bowman's in the right eye [Fig. 1]. In the left eye, full-thickness deposits were noted [Fig. 2]. Epithelium was spared in both eyes. Pupil reflex, iris, intraocular pressure, and fundoscopy were normal.
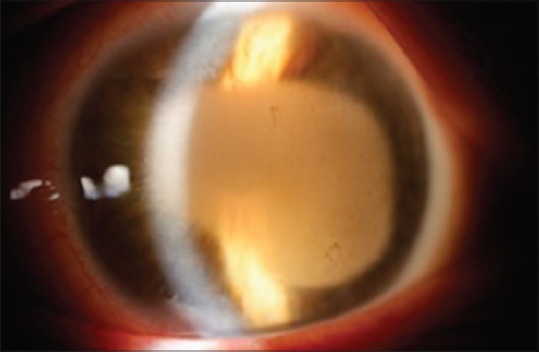
Figure 1.

Right eye biomicroscopic: Subepithelial and posterior stroma/Descemet's membrane calcium deposits
Figure 2.
Left eye biomicroscopy: Dense full-thickness calcium depositsmembrane
Laboratory parameters revealed a serum calcium level of 9.92 mg/dL (normal range, 8.5–10.5 mg/dL) and an alkaline phosphate concentration of 141 U/L (normal range, 37–147 U/L). We also performed 24-h urine calcium test that was also considered normal (97 mg/dL, normal range 25–300 mg/dL).
Penetrating keratoplasty was performed in the left eye. No complication was reported during the procedure. Six-month postoperative best-corrected visual acuity was 20/30 (0.18 logMar). No signs of inflammation, rejection, or reappearance of the deposits in the corneal graft were observed.
Anterior segment optic coherence tomography
The AS-OCT images showed hyperintense signal that corresponded to intense calcium deposition in the Bowman's layer and posterior central stroma adjacent to Descemet's membrane in the left eye [Fig. 3]. Diffuse stromal calcium deposition is also observed. The right eye presented mild deposits in the same location in relation to the left eye [Fig. 4]. Increased pachymetry was observed in both the eyes.
Figure 3.

Left eye anterior segment optic coherence tomography: Hyperintense signal mainly in Bowman's layer and posterior stroma/Descemet's membrane
Figure 4.

Right eye anterior segment optic coherence tomography: Hyperintense signal on Bowman's layer and posterior stroma/Descemet's membrane. Central corneal thickness is enhanced
Histopathological findings
Receptor's cornea was fixed in 10% formalin for light microscopy. Paraffin sections were further processed with hematoxylin and eosin (H and E). The specimen was deparaffinized for ultrastructural study. For transmission electron microscopy, further processing included standard dehydration and embedding in epoxy resin. Multiple serial semithin sections (1 mm) were stained with paraphenylenediamine for phase-contrast microscopy. The ultrathin sections were doubly stained with uranyl acetate and lead citrate and examined with a transmission electron microscope. Corneal mineralization occurred more densely along the basement membrane and subepithelial stroma [Fig. 5]. Basophilic deposits stained with H and E were also observed in the posterior stroma and scattered in the central part of the stroma. Posterior stroma and Descemet's membrane detach resulted from the underlying deposit because of its brittleness. We consider that the cleft, especially that observed with mineralization or activated keratocytes, resulted from the weakening of adhesion in the posterior part of the corneal stroma.
Figure 5.

Histopathology (H and E). Subepithelial and Descemet's membrane basophilic deposits. Epithelium and endothelium are detached
Discussion
Calcareous degeneration of the cornea in which calcium carbonate and phosphate are deposited as granules in the superficial layers of the cornea may be of primary or secondary origin. Secondary calcareous degenerations are more common and may occur in old scars, leukoma, atheromatous ulcers, or hypercalcemic states, such as sarcoidosis or osteoporosis.[9] Primary calcareous degeneration with no evidence of hypercalcemia is comparatively rare, and its etiology is not known. It is not clear why in some cases the degeneration progresses and interferes with visual acuity. The mechanism of interface calcium salt precipitation in our case is purely speculative.
It is very important to distinguish calcareous degeneration from band keratopathy to indicate the correct treatment. The AS-OCT showed that deep anterior lamellar keratoplasty and surface debridement with ethylenediaminetetraacetic acid would not be the treatment of choice because calcium is seen in a significant quantity in posterior stroma and Descemet's membrane.
Conclusion
To the best of our knowledge, this is the first report of AS-OCT in this rare corneal condition. The deposits’ hyperintense signal practically excluded other clinical hypothesis and helped us to choose the correct treatment. Corneal histopathology and negative laboratory tests confirmed the diagnosis of primary calcareous degeneration of the cornea.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lavid FJ, Herreras JM, Calonge M, Saornil MA, Aguirre C. Calcareous corneal degeneration: Report of two cases. Cornea. 1995;14:97–102. [PubMed] [Google Scholar]
- 2.Mohan H, Gupta DK, Sen DK. Primary calcareous degeneration of the cornea. Br J Ophthalmol. 1969;53:195–7. doi: 10.1136/bjo.53.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schlötzer-Schrehardt U, Zagórski Z, Holbach LM, Hofmann-Rummelt C, Naumann GO. Corneal stromal calcification after topical steroid-phosphate therapy. Arch Ophthalmol. 1999;117:1414–8. doi: 10.1001/archopht.117.10.1414. [DOI] [PubMed] [Google Scholar]
- 4.Moisseiev E, Gal A, Addadi L, Caspi D, Shemesh G, Michaeli A, et al. Acute calcific band keratopathy: Case report and literature review. J Cataract Refract Surg. 2013;39:292–4. doi: 10.1016/j.jcrs.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 5.Jhanji V, Rapuano CJ, Vajpayee RB. Corneal calcific band keratopathy. Curr Opin Ophthalmol. 2011;22:283–9. doi: 10.1097/ICU.0b013e3283477d36. [DOI] [PubMed] [Google Scholar]
- 6.Bernauer W, Thiel MA, Kurrer M, Heiligenhaus A, Rentsch KM, Schmitt A, et al. Corneal calcification following intensified treatment with sodium hyaluronate artificial tears. Br J Ophthalmol. 2006;90:285–8. doi: 10.1136/bjo.2005.082792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taravella MJ, Stulting RD, Mader TH, Weisenthal RW, Forstot SL, Underwood LD. Calcific band keratopathy associated with the use of topical steroid-phosphatepreparations. Arch Ophthalmol. 1994;112:608–13. doi: 10.1001/archopht.1994.01090170052021. [DOI] [PubMed] [Google Scholar]
- 8.Freddo TF, Leibowitz HM. Bilateral acute corneal calcification. Ophthalmology. 1985;92:537–42. doi: 10.1016/s0161-6420(85)34000-9. [DOI] [PubMed] [Google Scholar]
- 9.Feist RM, Tessler H, Chandler JW. Transient calcific band-shaped keratopathy associated with increased serum calcium. Am J Ophthalmol. 1992;113:459–61. doi: 10.1016/s0002-9394(14)76177-x. [DOI] [PubMed] [Google Scholar]


