Abstract
Purpose:
The purpose of this study is to assess the incidence, management, and outcomes for needle stick injuries (NSIs) in a tertiary eye-care hospital and provide appropriate recommendations for its prevention.
Methods:
This was a retrospective database review of NSI recorded between 2010 and 2015 at a tertiary eye care center. All staff members who had NSI were managed with standard treatment protocol. The mode, location, health-care workers affected and/or at risk for NSI were analyzed.
Results:
One hundred and forty NSI were reported between 2010 and 2015, with ophthalmic fellows under training encountering maximum needle pricks (n = 33; 24%), followed by nursing staff (n = 32; 23%), and consultants (n = 30; 21%). Location wise, the highest incidence of NSI was found in the operating room (n = 94; 67%), followed by the laboratory (n = 17; 12%), and patients’ ward (n = 14; 10%). Maximum pricks (n = 10; 20%) occurred while passing sharp instruments, anterior segment surgeons (n = 23; 79%) being affected more than posterior segment surgeons (n = 6; 21%). None of the NSI incidents was attributed to anti-VEGF injections. None of the subjects with NSI had seroconversion to hepatitis B surface antigen, human immunodeficiency virus, or hepatitis C virus in the 5-year study period.
Conclusions:
NSI is the most commonly encountered in the operating room among training personnel while passing sharp instruments, especially anterior segment surgeons. A proper needle/sharp disposal mechanism, documentation of adverse event, on-going staff training, and prompt prophylactic treatment are essential components of the protocol for NSI management.
Keywords: India, needle stick injury, ophthalmology
Needle stick injury (NSI) is defined as percutaneous exposure where the skin is breached by a needle or any sharp object contaminated by blood or other bodily fluid due to accidental pricks.[1] NSI is the second most common cause of occupational injury within the National Health Services.[2] It is known that 3–6 billion injections are given per year, of which 60% are unsafe.[3] The incidence of needle injury reported is about 100,000/year in the United Kingdom and about 600,000–1,000,000/year in the United States of America.[4] The reported authentic data of NSI in India are scarce due to infrequent reporting.[3] NSI poses a serious risk for occupational transmission of blood pathogens such as human immunodeficiency virus (HIV), hepatitis B virus and hepatitis C virus (HCV).[5] NSI can occur during various procedures such as needle recapping, operative procedures, blood collection, intravenous line administration, checking blood sugar, and due to improper sharps/needle disposal.[1]
Over the years, ophthalmology has evolved as a unique microsurgical practice and surgeons are at a constant risk of sustaining such injuries. The ophthalmic theater is the second most common reported location for NSI and accounts for 17% of high-risk sharp injuries as reported by the health practice authority of the United Kingdom in 2007.[2] With the advances in ophthalmic microsurgical instruments, sutures, and working under high magnification with dim room light, ophthalmic surgeons, and assistants are at great risk of sustaining sharp injuries. It is a attributed that special circumstances render an ophthalmologist at a greater risk of sustaining NSI as compared to other medical specialties.[4] The consequences of a sharp injury reach far beyond the immediate risk of blood-borne virus transmission, as such events are highly stressful and have the potential to affect an individual's career, family, and patients.[6,7,8,9,10,11,12]
The number of intravitreal injections performed has increased dramatically over the past decade, becoming one of the most commonly performed ophthalmic procedures as anti-inflammatory, antiviral, antibiotic, and anti-vascular endothelial growth factor inhibitor (anti-VEGF) therapies have emerged as the standard of care in ophthalmic practice and have also increased risk for the ophthalmic personal for NSI.[13]
There are very limited data for reported NSI in an ophthalmic setup. PubMed search for keywords “needle stick injury” “ophthalmology” revealed only three articles.[13,14,15] The purpose of this study was to determine the risk factors for NSI in a tertiary care ophthalmic practice over a 5-year period. The costs for conducting investigations for both the patient and the injured medical personnels and risk assessment for contamination with pathogens were also assessed.
Methods
This study was a retrospective database review of all needle prick injuries recorded between 2010 and 2015 at a tertiary eye care centre in India. The institution has six fully functional centers within the city, equipped for both outpatient (OP) and inpatient (IP) management. The institute has two mobile surgical units in buses for conducting cataract surgeries in the villages, which are accompanied by a well-equipped mobile pathology laboratory for sample blood collection and testing. The institute offers teaching and training to ophthalmic postgraduates, fellows (trainee doctors), nursing staff, optometrists, paramedical staff, and ophthalmic secretaries. This study was conducted according to the tenets of Helsinki Declaration. Prior Institutional Review Board approval was obtained. Each subject consented by signing a written informed consent.
The procedure for sharp needle and instrument disposal is followed as per standard protocol in all the centres. All the new recruits (staff and students) joining the institute were made aware of the protocols so as to minimize the rate of NSI. The protocol for handling sharp needle dictates minimal manipulation of needle or sharp instruments with hands or finger. Recapping of sharp instruments is avoided, and interindividual handling from one person to another during a surgical procedure is kept to a minimum. Particularly in the OP department (OPD), care is taken to dispose of needles in sharp disposal bins that are provided with colored labels in each room. Meanwhile, in the operating rooms, extreme caution is taken during surgery using trays to pass sharp instruments between the surgeon and nursing assistant. All needles are disposed of in the sharp-proof containers immediately after use in the operation theater (OT). A special area in the OT is designated for trolleys on which to place the sharp instruments. All syringes are disposed of in a separate container marked with a red-colored liner. The protocol in the event of an accidental NSI is described as follows in (sharp_injury_form.pdf): Three copies of the incident report form is raised by the concerned health-care worker, and one form each is sent to the main laboratory, the human resource department (HRD) and to the hospital infection control (HIC) committee. The patient flow is depicted in Fig. 1.
Figure 1.
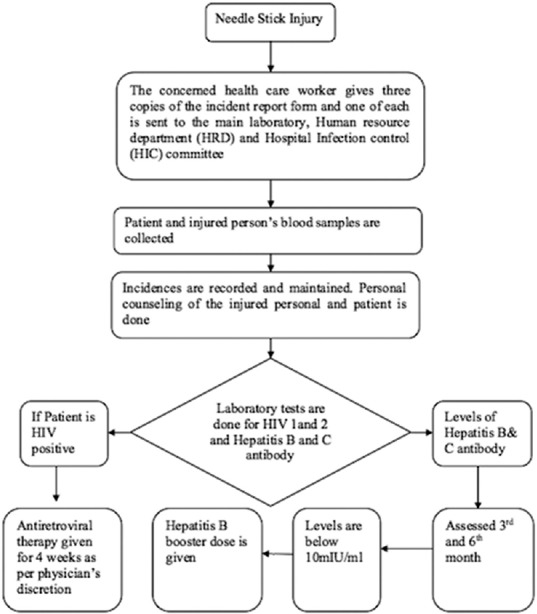
Flowchart describing the hospital protocol following needle stick injuries
The NSI analysis form is filled after investigating the cause of injury, and corrective and preventive action is taken in the manner subsequently described. After obtaining their consent, the patient's and the injured personnel's blood samples are collected. A record is kept in the HRD for further follow-up or analysis. Counseling of the patient and the injured personnel is done by the concerned physician. Laboratory tests are performed, including HIV screening, in the first 2 h of NSI, and postexposure prophylaxis is conducted within 72 h. If the patient tests HIV positive, antiretroviral therapy is started immediately and continued for 4 weeks in accordance with the National AIDS Control Organization guidelines.[7] The health-care worker (HCW) is counseled and assessed for HIV1 and 2 (enzyme-linked immunoassay) antibodies at 6-month-interval. Hepatitis B and C antibodies are tested within the first 2 h and then at third and 6th month intervals. The levels of hepatitis B antibodies are measured for the HCW at the third and 6th month, and if the levels are below 10 mIU/ml, a booster dose of hepatitis B vaccination is administered. Disposal of all sharps is done in yellow puncture-proof containers instilled with 1% sodium hypochlorite solution [Fig. 2].
Figure 2.
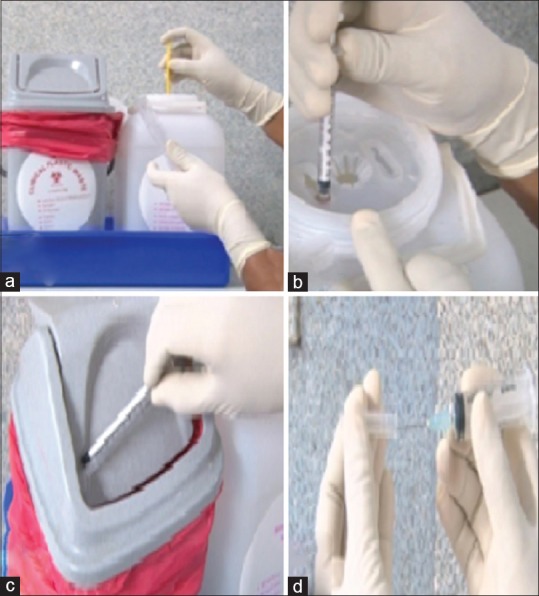
(a) The disposal of side-port needle (b) the disposal of needle hub in the container, and (c) disposal of the syringe in the red-labeled-colored container, and (d) not to recap needles
Every OPD, patient ward, and OT are provided with an adequate number of containers. Care is taken to avoid overfilling these containers, and they are handed over to the housekeeping staff once they are three-quarters full. All housekeeping staff are adequately trained in maintaining precaution while handling sharp instruments for disposal. All general waste is segregated and disposed of in white polythene biodegradable bags which are then placed in big bins designated for the same in the garbage area. The city corporation vehicles daily clear the waste. This is in accordance with the World Health Organization (WHO) protocol for the safe management of waste from health-care organizations.
Results
One hundred and forty NSI were reported over a period of 5 years from 2010 to 2015. Ophthalmic fellows, training in the institute, suffered maximum needle pricks (n = 33; 24%), followed by the nursing staff (n = 32; 23%), and consultants (n = 30; 21%). The postgraduates and biomedical staff accounted for (n = 14; 14%) and (n = 14; 10%), respectively. The least NSI was encountered by housekeeping/maintenance staff (n = 8; 6%), followed by the anesthesiologist, and staff secretaries (n = 2; 1%) as shown in Table 1.
Table 1.
Needle stick injuries in a tertiary eye-care hospital in India: Incidence amongst health-care workers (n=140)
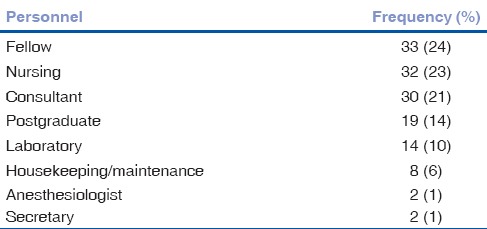
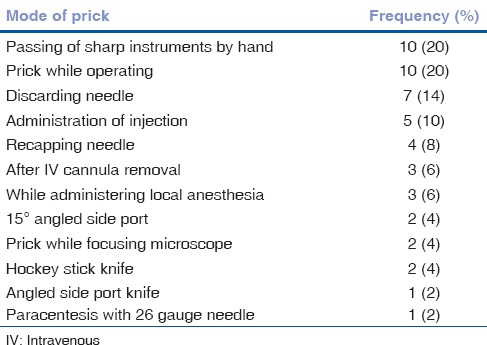
Table 2 shows the location-wise distribution of NSI, with the maximum number occurring in the OT (n = 94; 67%), followed by the laboratory (n = 1712%), and the ward (n = 14; 10%). The minimum number was reported in the OPD and needle disposal (n = 9; 6%) and (n = 6; 4%), respectively. Maximum pricks (n = 10; 20%) occurred while operating and passing the sharp instruments. The NSI encountered while discarding the needles and while administering injection was (n = 7; 14%) and (n = 5; 10%), respectively, as shown in Table 3.
Table 2.
Location-wise distribution of needle stick injuries in a tertiary eye-care hospital in India (n=140)

Table 3.
Needle stick injuries in a tertiary eye-care hospital in India: Mode of injury (n=50)
The cost for the first collection of blood sample for HIV 1, HIV2, HCV, and HBsAg (ELISA) were Rs. 1070, Rs. 430, and Rs. 580, respectively, and the cost of the antibody vaccination was Rs. 660. The total cost to the institute per staff members for the first sample was Rs. 2740. The cost for the second and third sample testing was Rs. 2080 per staff member. The same cost of second and third sample testing for the patients (Rs. 2080 per head) was borne by the hospital. The cost of the second dose of postexposure prophylactic vaccination for the staff was Rs. 180. The cost incurred by the hospital for testing one patient and one injured staff member was Rs. 9180. The overall cost incurred for managing all the 140 NSI amounted to Rs. 1285200.00 ($19219.38) as shown in Table 4.
Table 4.
Cost of laboratory tests for staff and patients for needle stick injuries
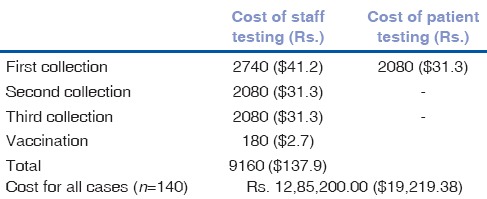
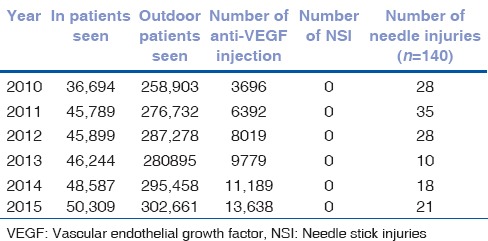
Table 5 shows the year-wise incidence of NSI and rate of seroconversion per year. The maximum number of pricks (n = 35; 25%) were observed in 2011, followed by (n = 28; 20%) NSI in 2010 and 2012 each, respectively. The least (n = 10; 7%) NSI were observed in 2013 while 2014 and 2015 accounted (n = 18; 13%) and (n = 21; 15.0%), respectively. None of the reported subjects with NSI had seroconversion to HBsAg, HIV, and HCV in the 5 years. Table 6 shows the comparison of numbers of IP and OP patients per year and the number of anti-VEGF injection given per year versus the number of NSI per year. The data delineate the negligible number of NSI occurring in our institute even with the steady increase in the number of IP and OP patients per year.
Table 5.
Needle stick injuries in a tertiary eye-care hospital in India: Year-wise incidence and rate of conversion (n=140)
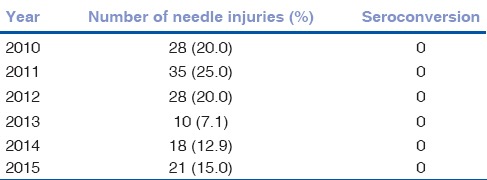
Table 6.
The comparison of number of inpatient and outdoor patients and the number of anti-vascular endothelial growth factor injection given per year versus the number of needle stick injuries per year
Discussion
This study provides significant data regarding the self-reported risk for NSI among health workers in a tertiary eye care ophthalmic practice in India. In our study, the highest incidence of NSI was observed among the training fellows in the institute, accounting for (n = 34; 24%) of the total number. This was followed by the nursing staff and consultants, each accounting for (n = 32; 23%) and (n = 29; 23%) of the total NSI. Ghauri et al. and Alshihry observed most NSI being reported among the nursing staff, 54% and 50% respectively, followed by doctors accounting for 40% and 19%, respectively, in their study.[4,16] Jayanth et al. conducted a study of needle prick injury in a tertiary hospital and observed that nursing staff accounted for 28% of the NSI and interns/trainees accounted for 9%.[5] For us, the maximum NSI was observed among the fellows and can be attributed to the fact that our hospital is a tertiary ophthalmic institute and provides training to a large number of fellows and postgraduates in varying ophthalmic subspecialties. The high volume of surgical assistance work and relatively limited wet laboratory experience and surgical learning curve could contribute to such a risk. The individual incidence of NSI among different working staff members is difficult to calculate due to the large volume of surgeries being done in the institute using the electronic medical record system and assigning each surgery a specific code, which makes it difficult for such an analysis. It could also be due to the fact that training fellows go through rotations within the hospital in different sub specialties.
The incidence of NSI in the 5-year study period was noted to be 0.07/1000 surgeries. Sharma et al. had reported an 3.47% per annum occurrence rate of NSI in a tertiary hospital in India, and Pournaras et al. found a similar incidence of 2.4% per year in a Greek hospital. A large multinational study by the WHO on the global burden of sharps injury estimated the average number of injuries per HCW to be 0.2–4.7 per year.[16]
In our study, the highest number of needle pricks (n = 94; 67%) occurred in the OT, followed by the laboratory and ward, accounting (n = 17; 12%) and (n = 14; 10%), respectively. Ghauri et al. and Alshihry each reported 52% and 55% of NSI in the ophthalmic theater and this corresponds with our results.[4,6] This can be attributed to the fact that most ophthalmic procedures are conducted in the OT and ours being a tertiary care center, the number of surgeries are higher on a per day basis and thus increases the chances of NSI in both the OT and the ward.
In our study, the two most common scenarios for NSI in the operating room were while passing sharp instruments by hand, and while operating, each accounting for (n = 10; 20%). This was comparable with the results obtained in the study by Alshihry where they observed the maximum number (31%) of NSI while handling instruments during operating procedures.[6] Ghauri et al. observed 46%, and Alshihry observed 21% cases of NSI while discarding the needles in comparison to (n = 7; 14%). Needle discarding procedures are the second most common cause of NSI in our study.[4] The other causes of NSI as observed by Alshihry during various surgical steps/procedures were while recapping the needles (55%), passing the instrument (35%), unpacking the instrument sets, and uncovering the needles (5%). Dissimilar results were observed in comparison with our study as needle recapping accounted for 8% of NSI. This can be attributed to the initial training course given in sharp disposal to all staff members at the time of joining the institute.
In our study, the highest number of NSI was observed among anterior segment surgeons (n = 23; 79%) in comparison to the posterior segment surgeons accounting for (n = 6; 21%). The incidence of NSI among anterior and posterior segment sugeons in our study was noted to be 0.13% and 0.83%, respectively. No references were available in literature on the difference in prevalence of NSI between anterior and posterior segment surgeons. It could be attributed to the higher frequency of anterior segment surgeries performed in a day by a single surgeon as compared to posterior segment surgery and faster handling of sharp instruments, exposing them to a higher risk.
The average cost of the postexposure for staff in our institute, inclusive of the vaccination and patient blood sample, is Rs. 9180 ($144). Thus, the total expense for 171 NSI was Rs. 1285200.00 ($19219.38). The cost of a similar single NSI treatment in the United States ranges between $500 and $3000. The annual economic burden for NSI in the United States is estimated to be between 118 million and 591 million dollars.[8,9] In the United Kingdom, the cost for initial testing and treatment is €3500 while the long-term cost of treating HCV and HIV is €700,000.[7] The short-term cost at a tertiary care hospital in Mumbai is Rs. 9000 for each HCW per needle prick.[3]
In the current study, the year-wise incidence of NSI with maximum number of pricks (n = 35; 25%) was observed in 2011, followed by (n = 28; 20%) NSI in 2010 and 2012, respectively, with a decrease in frequency (n = 10; 7%) in 2013, 2014 (13%), and 2015 (15%). This can be attributed to the intensified training of staff and new recruits by showing them preventive videos and demonstrating how to discard sharp instruments by the HIC committee. The training initiative for NSI prophylaxis was started in 2012 in our institute. Even with the best efforts at educating the staff on a periodic basis, accidental NSI does occur, thus necessitating the need for repetitive and regular training for proper disposal of needles and highlighting the emphasis required for extreme precaution in handling sharps. We observed no seroconversion in all 5 years for the staff members exposed to NSI. The Center for Disease Control and Prevention estimated the seroconversion rate for HBsAg, HCV and HIV to be 22%–31%, 0.5%, and 0.3%, respectively. The worldwide reported incidence of HIV seroconversion was 296 cases after occupational exposure, of which 56 are documented while 138 were possibly occupationally acquired. In India, two possible cases of occupationally acquired HIV infection have been reported from Chandigarh.[5]
Table 6 describes the year-wise frequency of anti-VEGF injection versus the number of NSI in the span of 5 years. We reported no cases of NSI due to anti-VEGF injections, even after an exponential increase in the use of anti-VEGF injections per year. There is scarce literature of NSI related to anti-VEGF. Shah et al. described the use of intravitreal bevacizumab as being widely prevalent among retina specialists in the United States and conducted a cross-sectional survey study for the assessment of needle prick injury associated with anti-VEGF injection. The survey concluded that at least one-third of the retina specialists perceive the practice of direct application of adhesive stickers to syringes as a risk for NSI. About 8% of retinal physicians had experienced at least one NSI while performing intravitreal injection. In our study, we reported no NSI related to anti-VEGF injection, as the drug is drawn from a single bevacizumab vial with a minispike (Braun™) into multiple individuals.[13]
Conclusions
The most common risk factors for NSI in an ophthalmic tertiary care hospital include training personnel performing or assisting in anterior segment surgeries, especially while exchanging sharp instruments. It is in this view that all hospital personnel should be made aware of the risks for NSI, protocol for incident reporting, safe instrument handling, needle disposal mechanisms, and participation in ongoing staff training to reduce and prevent this occupational hazard. Further prospective studies are necessary to evaluate the incidence of NSI among staff workers in an ophthalmic eye hospital and taking active steps in preventing the occurrence of NSI.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bidira K, Woldie M, Nemera G. Prevalence and predictors of needle stick injury among nurses in public hospitals of Jimma Zone, South West Ethiopia. Int J Nurs Midwifery. 2014;30(6):90–6. [Google Scholar]
- 2.Adams S, Stojkovic SG, Leveson SH. Needlestick injuries during surgical procedures: A multidisciplinary online study. Occup Med (Lond) 2010;60:139–44. doi: 10.1093/occmed/kqp175. [DOI] [PubMed] [Google Scholar]
- 3.Muralidhar S, Singh PK, Jain RK, Malhotra M, Bala M. Needle stick injuries among health care workers in a tertiary care hospital of India. Indian J Med Res. 2010;131:405–10. [PubMed] [Google Scholar]
- 4.Ghauri AJ, Amissah-Arthur KN, Rashid A, Mushtaq B, Nessim M, Elsherbiny S. Sharps injuries in ophthalmic practice. Eye (Lond) 2011;25:443–8. doi: 10.1038/eye.2011.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jayanth ST, Kirupakaran H, Brahmadathan KN, Gnanaraj L, Kang G. Needle stick injuries in a tertiary care hospital. Indian J Med Microbiol. 2009;27:44–7. [PubMed] [Google Scholar]
- 6.Al Shihri AM. Pattern of Sharps Injuries in Ophthalmic Practice. Epidemiol. 3:128. doi: 10.4172/2161-1165.1000128. [Google Scholar]
- 7.Prüss-Ustün A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005;48:482–90. doi: 10.1002/ajim.20230. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Workbook for Designing, Implementing and Evaluating a Sharps Injury Prevention Program 2004. 2007. [Last accessed on 2017 Sep 01]. p. 9130. Available from: http://www.cdc.gov/sharpssafety/pdf/sharpsworkbook_2008.pdf .
- 9.U.S. Public Health Service. Updated U.S. Public Health Service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep. 2001;50:1–52. [PubMed] [Google Scholar]
- 10.Marcus R. Surveillance of health care workers exposed to blood from patients infected with the human immunodeficiency virus. N Engl J Med. 1988;319:1118–23. doi: 10.1056/NEJM198810273191703. [DOI] [PubMed] [Google Scholar]
- 11.International Review of Modern Surgery. Infection control: The rising cost of needle stick injuries. Becton, Dickinson: U.K Limited; 2005. [Google Scholar]
- 12.Rodrigues C. Needle stick injuries &the health care worker – The time to act is now. Indian J Med Res. 2010;131:384–6. [PubMed] [Google Scholar]
- 13.Shah SU, Koenig MJ, Dacquay Y, Mozayan A, Hubschman JP. Assessment of the risk of needlestick injuries associated with intravitreal injections. Retina. 2014;34:781–4. doi: 10.1097/IAE.0b013e3182a2f523. [DOI] [PubMed] [Google Scholar]
- 14.Trottmann F, Mojon D. Pattern of injuries to the surgical team during ophthalmosurgical interventions. Klin Monbl Augenheilkd. 2013;230:150–6. doi: 10.1055/s-0032-1327957. [DOI] [PubMed] [Google Scholar]
- 15.Mansour AM. Needlestick injuries in ophthalmology. Ophthalmic Surg. 1989;20:367–9. [PubMed] [Google Scholar]
- 16.Sharma R, Rasania S, Verma A, Singh S. Study of prevalence and response to needle stick injuries among health care workers in a tertiary care hospital in Delhi, India. Indian J Community Med. 2010;35:74–7. doi: 10.4103/0970-0218.62565. [DOI] [PMC free article] [PubMed] [Google Scholar]


