Abstract
Background. Surveys in the United States and Europe have shown a plateau of new HIV cases, with certain regions and populations disproportionately affected by the disease. Ethnic minority women and socioeconomically disadvantaged groups are disproportionately affected by HIV. Previous reviews have focused on prevention interventions targeting ethnic minority men who have sex with men, have not accounted for socioeconomic status, or have included only interventions carried out in clinical settings.
Objectives. To review and assess the effectiveness of HIV prevention interventions targeting socioeconomically disadvantaged ethnic minority women in member states of the Organisation for Economic Co-operation and Development (OECD).
Search Methods. On March 31, 2014, we executed a search using a strategy designed for the MEDLINE (Ovid), CINAHL, Embase, Scopus, and Web of Knowledge databases. Additional searches were conducted through the Cochrane Library, CRD Databases, metaRegister of Controlled Trials, EURONHEED, CEA Registry, and the European Action Program for Health Inequities as well as in gray literature sources. No language or date restrictions were applied.
Selection Criteria. We selected studies assessing the effectiveness of interventions to prevent HIV among ethnic minority women of low socioeconomic status in which at least 80% of participants were reported to belong to an ethnic minority group and to have a low income or be unemployed. We included only studies that were conducted in OECD member states and were randomized controlled trials or quasi-experimental investigations with a comparison group.
Data Collection and Analysis. A data extraction form was developed for the review and used to collect relevant information from each study. We summarized results both qualitatively and quantitatively. The main outcomes were categorized into 3 groups: improved knowledge regarding transmission of HIV, behavior changes related to HIV transmission, and reductions in the incidence of sexually transmitted infections (STIs). We then performed meta-analyses to assess the effectiveness of the prevention interventions in terms of the 3 outcome categories.
Main Results. A total of 43 interventions were included, and 31 were judged to be effective, 7 were partially effective, and 5 were ineffective. The most frequently recurring characteristics of these interventions were cultural adaptation, a cognitive–behavioral approach, the use of small groups and trained facilitators, and a program duration of between 1 and 6 weeks. Our meta-analyses showed that the interventions improved knowledge of HIV transmission (odds ratio [OR] = 0.59; 95% confidence interval [CI] = 0.43, 0.75), increased the frequency of condom use (OR = 1.60; 95% CI = 1.16, 2.19), and significantly reduced the risk of STI transmission by 41% (relative risk = 0.59; 95% CI = 0.46, 0.75).
Conclusions. Our study demonstrates the feasibility and effectiveness of HIV prevention interventions targeting socioeconomically deprived ethnic minority women.
Public Health Implications. This is one of the first studies to include a meta-analysis assessing reductions in STI incidence among at-risk women who have participated in HIV prevention programs. The fact that our meta-analyses showed a statistically significant reduction in STI transmission provides important evidence supporting the overall effectiveness of directing prevention programming toward this vulnerable population. For policymakers, this review demonstrates the feasibility of working with multiple intervention components while at the same time facilitating more effective interventions that take into account the principal outcome measures of knowledge, behavior change, and STI transmission rates. The review also underscores the need for additional research outside the United States on the effectiveness of prevention interventions in this vulnerable group.
PLAIN-LANGUAGE SUMMARY
We reviewed HIV prevention interventions targeting socioeconomically deprived ethnic minority women in 34 countries starting from the beginning of the epidemic. We were able to identify 43 interventions and provide a thorough review of the characteristics and outcome measures of each. The most frequently recurring characteristics of these interventions were cultural adaptation, a cognitive–behavioral approach, the use of small groups and trained facilitators, and a program duration of between 1 and 6 weeks. The main outcome measures were categorized into 3 groups: improved knowledge regarding transmission of HIV, behavior changes related to HIV transmission, and reductions in STI incidence. A meta-analysis was then carried out on each of these outcome areas to assess the effectiveness of the reviewed interventions. We found statistically significant improvements in knowledge related to HIV transmission and condom usage. Notably, the reviewed interventions significantly reduced STI incidence by 41%, providing important evidence underscoring the effectiveness of prevention efforts in a population that continues to be disproportionately affected by HIV.
Years of research and community action have led to great advances in prevention and treatment options for the individuals and communities most affected by HIV and AIDS. However, the disease continues to be a significant threat to public health throughout the globe. In 2012, it was estimated that approximately 35.3 million people were living with the disease, with approximately 2.3 million new infections and 1.6 million deaths internationally. These numbers, although significant, represent a marked improvement, with a 33% reduction in new HIV cases since 2001 and a decrease of 700 000 deaths annually since the peak in 2005.1
Nevertheless, the burden of HIV is unequally distributed, and it has a much greater impact on certain vulnerable populations. In the countries that belong to the Organisation for Economic Co-operation and Development (OECD), a collection of 34 nation-states representing some of the world’s largest economies, there has been significant progress toward reducing the health burden of the disease.2 However, surveys in the United States and Europe have shown that new HIV cases have plateaued and that certain regions and populations are disproportionately affected by the disease.3,4 In particular, ethnic minority and socioeconomically disadvantaged groups are disproportionately affected, with studies showing that the immigrant sub-Saharan Africa community as well as the African American and Latino communities in the United States face unequal disease burdens.4–6
In the United States, for example, African American women are 20 times more likely to contract the disease than are White women, and Hispanic women are twice as likely as their White counterparts. The greater number of people living with HIV in African American and Hispanic/Latino communities and the fact that people tend to have sex with partners of the same ethnicity result in women from these communities facing a greater risk of HIV infection with each new sexual encounter.
In the European region, HIV diagnoses among migrants originating from sub-Saharan countries make up a disproportionate amount of cases resulting from heterosexual transmission.4 In Canada, another key member of the OECD bloc, Blacks and Aboriginals account for a disproportionate number of new AIDS cases, and women from these minority groups are more likely than their White counterparts to report HIV-associated stigma and less likely to receive HIV testing.7–9
As HIV incidence remains stubbornly in place, it is important to direct prevention efforts at those populations most affected by the disease to reduce transmission. Implemented interventions should incorporate techniques that are effective in terms of cost, geographic area covered, and adaptation to the populations most affected by the disease.10 Previous reviews have focused on prevention interventions targeting ethnic minority men who have sex with men, have not accounted for socioeconomic status, or have included only interventions carried out in clinical settings.11–15
We searched for and reviewed HIV prevention interventions targeting socioeconomically disadvantaged ethnic minority women in OECD countries. We used a standardized metric to evaluate the methodologies of the studies and the effectiveness of the interventions. The ultimate goal of this systematic review and meta-analysis was to identify, characterize, and assess the effectiveness of HIV prevention interventions for socioeconomically disadvantaged ethnic minority women.
METHODS
This study was part of a broader systematic review aiming to identify and analyze health care interventions designed to reduce social inequalities. The review and its procedures were planned, conducted, and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.16
Information Sources and Search Strategy
We designed specific search strategies for the MEDLINE (Ovid), CINAHL, Embase, Scopus, and Web of Knowledge databases. The strategy, which combined MeSH (Medical Subject Headings) terms and keywords, was initially designed for MEDLINE and afterward adapted and used in the other 4 databases. Other searches were also conducted with relevant keywords in different databases such as the Cochrane Library, CRD Databases, metaRegister of Controlled Trials, EURONHEED, CEA Registry, and the European Action Program for Health Inequities. Finally, we consulted various gray literature sources, as well as reviews of similar topics.
We executed the searches on March 31, 2014; no language or date restrictions were applied. A bibliographical database created through Reference Manager Professional Edition was used to store and manage the references. The full MEDLINE search strategy is described in Appendix A (available as a supplement to the online version of this article at http://www.ajph.org).
Study Selection
Our inclusion criteria were as follows. First, we included only studies assessing the effectiveness of interventions to prevent HIV among ethnic minority women of low socioeconomic status. Second, interventions were required to target populations in which at least 80% of the participants were reported to belong to an ethnic minority group and to have a low income or be unemployed. Third, studies had to have been conducted in OECD member states to ensure homogeneity among interventions targeting populations in countries with similar levels of development.17 Finally, studies were required to be randomized controlled trials or quasi-experimental investigations with comparison groups.
Studies focusing on drug-dependent ethnic minority women and addiction treatment or drug use were excluded. In addition, studies that targeted women who were already HIV positive were not included.
Two of the reviewers (M. M. and A. R.-G.) independently screened the titles and abstracts of the documents retrieved through the search to ascertain their eligibility. Those fulfilling the inclusion criteria were selected for full text assessments, after which a new independent assessment was performed to select studies to include in the review. Disagreements were solved through discussion with a third reviewer (I. R.-P.).
Assessment of Risk of Bias
We used the Cochrane Collaboration’s tool to assess the included studies with respect to risk of bias.18 Different sources of bias such as randomization, allocation, blinding, incomplete outcome data, and selective reporting were classified into 3 categories (low risk of bias, high risk of bias, unclear risk of bias). Two reviewers (M. M. and A. R.-G.) independently performed assessments of methodological quality, and again a third reviewer (I. R.-P.) was consulted to solve any disagreements.
Data Extraction and Synthesis of Results
A data extraction form was developed for the review and used to collect relevant information from each article, including information about the methods and population characteristics, interventions, comparators, outcomes, timing, settings, and study design. Two independent reviewers (M. M. and G. P.-M.) extracted the data, and the results were summarized both qualitatively and quantitatively. The qualitative summary included a description of the features and main outcomes of the interventions.
After a review of the included articles, we categorized the main outcomes into 3 groups: improved knowledge regarding transmission of HIV, behavior changes related to HIV transmission, and reductions in the incidence of sexually transmitted infections (STIs). However, we used different measures when studies included only 1 or 2 of the categories. We assessed the overall effectiveness of each intervention to determine whether significant postintervention improvements were observed in the experimental group relative to the control group. Interventions were determined to be effective when they achieved statistically significant improvements in all of the predetermined outcome measures. Partial effectiveness was defined as statistically significant changes in one or more but not all of the prevention intervention effectiveness measures. Interventions were deemed ineffective if there was no improvement in any of the outcome variables.
We performed our quantitative summary through 3 meta-analyses assessing the effectiveness of the prevention interventions in terms of the 3 measures of knowledge, behavior change, and STI transmission. Regarding the selection criteria for these analyses, studies were required to include calculations of differences between the experimental and control groups after the completion of the intervention in at least one of these 3 areas. According to these criteria, raw HIV knowledge score means and standard deviations were extracted and transformed into standardized mean differences with their 95% confidence intervals (CIs). Standardized mean differences were calculated as the ratio of the difference in mean outcomes between groups and the standard deviation of outcomes among participants.
We evaluated behavior change through the measure of condom usage, as it was the only outcome for which there was a sufficient number of studies with comparable results for the meta-analyses. Effect sizes were measured as odds ratios (ORs) for condom use in the intervention group as compared with the control group. In relation to STI incidence, we calculated the postintervention relative risk (RR) of STI transmission in intervention groups as compared with control groups for all eligible studies.
In all of our meta-analyses, we used a random effect model to combine individual effects. Heterogeneity was quantified via the I2 statistic, with I2 values of 50% or greater being considered evidence of substantial heterogeneity.19 Studies that contributed to heterogeneity were identified through a Galbraith chart. We performed the Begg and Egger test to quantitatively assess publication bias. All of our analyses were conducted with Stata version 11.2 (StataCorp LP, College Station, TX). We set the statistical significance level at a P level of less than .05.
RESULTS
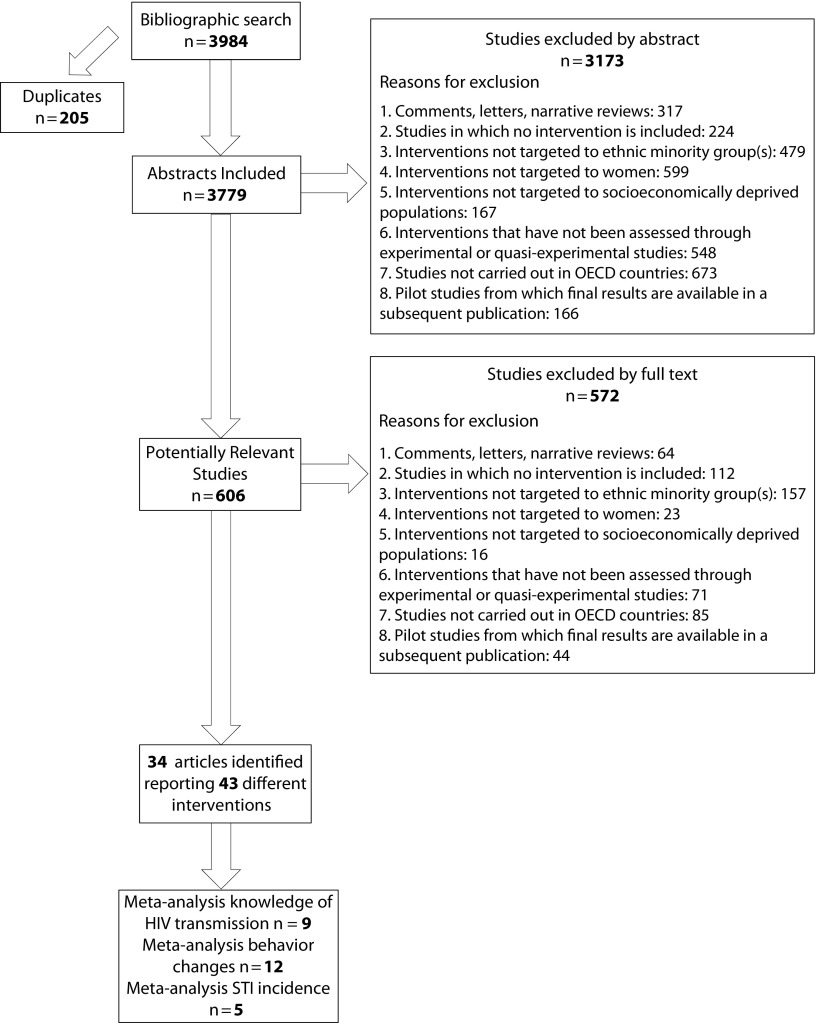
Our search results are summarized in the PRISMA flow diagram (Figure 1). A total of 3984 citations were identified in the initial search, 205 of which were duplicates. Title and abstract screening of the remaining 3779 citations resulted in the inclusion of 606 citations for further review. After examination of full-text articles, we included 34 articles.20–53
FIGURE 1—
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Flowchart of the Study Selection Process
Note. OECD = Organisation for Economic Co-operation and Development; STI = sexually transmitted infection.
Characteristics of the Studies
The characteristics of the included studies are summarized in Table 1. With regard to year of publication, the first study was published in 1993, and nearly half (15 studies) were published during or after 2010.22,23,25,27,31,32,35,38,40,44,47,50–53 Most (30 studies) were randomized controlled trials, and all of these trials were based on research performed in the United States.20–25,27,28,30,32–44,46–53 The studies included a variety of control groups that can be broken down into 3 large categories: no intervention, a standard health intervention, or an enhanced prevention intervention. The most frequently recurring comparison group was assigned to what was termed a standard health promotion or prevention intervention. These interventions usually addressed health in general or other topics not related to HIV/AIDS or STI transmission.
TABLE 1—
Study and Intervention Features: Review and Meta-Analysis of HIV Prevention Interventions Targeting Socioeconomically Deprived Ethnic Minority Women in Organisation for Economic Co-operation and Development Countries, 2014
| Feature | No. (%) or Mean (Range) |
| Study feature | |
| Study year | |
| 1993 | 1 (3) |
| 1994 | 2 (6) |
| 1996 | 1 (3) |
| 1997 | 2 (6) |
| 1999 | 2 (6) |
| 2000 | 3 (9) |
| 2001 | 2 (6) |
| 2002 | 2 (6) |
| 2003 | 1 (3) |
| 2005 | 2 (6) |
| 2007 | 1 (3) |
| 2010 | 1 (3) |
| 2011 | 4 (12) |
| 2012 | 5 (15) |
| 2013 | 4 (12) |
| 2014 | 1 (3) |
| Epidemiological design | |
| Randomized controlled trial | 28 (82) |
| Clustered randomized controlled trial | 2 (6) |
| Controlled trial | 4 (12) |
| Type of comparison group | |
| No intervention | 9 (27) |
| Standard prevention intervention | 17 (51) |
| Enhanced prevention intervention | 7 (21) |
| Intervention feature | |
| Setting | |
| Community-based organization | 7 (21) |
| Clinic | 7 (21) |
| Community health center | 4 (12) |
| Home | 1 (3) |
| Targeted geographic area | 4 (12) |
| School | 1 (3) |
| Prison | 1 (3) |
| Homeless shelter | 1 (3) |
| Not specified | 8 (24) |
| Duration (weeks) | 5.88 (1–52) |
| Type of prevention intervention | |
| Cognitive–behavioral | 23 (69) |
| Informational | 9 (27) |
| Community leadership development | 1 (3) |
| Counseling | 1 (3) |
| Culturally adapted | |
| Yes | 24 (72) |
| No | 9 (27) |
Note. The sample size was n = 13 318.
Intervention settings were diverse and included schools, churches, and prisons. However, the most frequent settings were community-based organizations (7), clinics (7), and community health centers (4). The total number of study participants was 13 318.
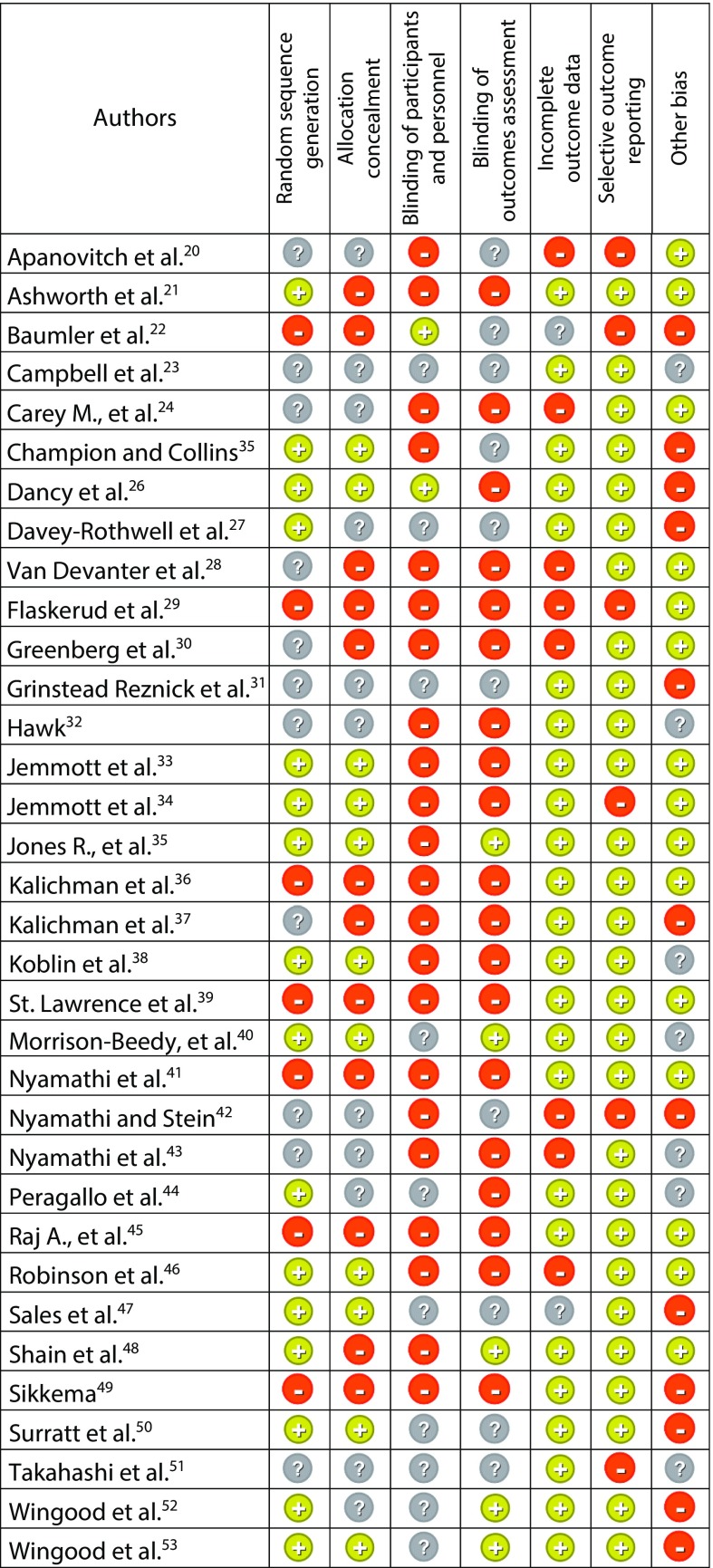
Risk of Bias
Data on risk of bias are presented in Figure 2. The most frequently encountered biases were random sequence generation, allocation concealment, and bias related to blinding. Ten studies did not provide complete data. Five studies were found to involve a high risk of bias.20,22,29,42,43
FIGURE 2—
Assessment of Risk of Bias: Review and Meta-Analysis of HIV Prevention Interventions Targeting Socioeconomically Deprived Ethnic Minority Women in Organisation for Economic Co-operation and Development Countries, 2014
Characteristics of the Interventions
The identified studies included 43 interventions (Table A, available as a supplement to the online version of this article at http://www.ajph.org). The majority of the interventions (22) were based on cognitive–behavioral theoretical models directed principally at reducing risky behaviors.22,23,25,27,28,31–33,37,39–45,47,50–53 Nine interventions were based on models aimed at behavior training in areas such as decision-making skills, partner communication, and correct condom use.29,30,33,34,45,48 Eight interventions consisted of educational models geared toward improving knowledge of HIV/AIDS transmission.20,21,34,35,38,46,49 Also, certain interventions included practice activities through demonstrations or role playing.27,33,34,44,50–52
The majority of interventions (32) were culturally adapted to the target population. Specifically, 18 interventions incorporated culturally adapted materials (e.g., materials adapted to the age and ethnicity of the study’s target population),21,29,32,33,35–37,39,41,42,46,51 7 interventions involved components that had been culturally adapted on the basis of previous research with the target population (e.g., prior knowledge of the population was analyzed and then used in the design of the intervention components),24,27,31,38,43,52,53 and 2 interventions incorporated a language adapted to the target population (the intervention was conducted in Spanish).44,48 In the case of 2 interventions, the adaptation was not specified.
The interventions were principally directed toward women at risk of contracting HIV or other STIs, such as women with multiple sexual partners and those who have unprotected sex. In addition, 4 interventions were designed specifically for adolescent women,22,25,33,40 another 4 targeted women who were or had been addicted to drugs,23,41,43,51 3 were geared toward female sex workers,43,50,51 and 1 targeted women whose husbands were in prison.31
The interventions were typically delivered in small groups (29 interventions).22–28,30,32,33,36,37,39,40,43–45,47–49,51–53 Seven interventions were individually delivered,21,31,34,38,42 and 2 were delivered through videos.35,41 With regard to providers, 15 interventions were delivered by trained facilitators,24,25,27,30,32,33,37,39,44,49,51 9 by nurses,21,34,41–43 and 6 by peer educators.26,29,31,40,50,53 Two interventions were provided by health educators,47,52 2 by community leaders,45 and 2 by counselors.23,38
The interventions varied in length from 20 minutes to 15 hours; they also varied in duration in weeks, from a one-time session to a 1-year intervention. Thirteen interventions took place over 1 week,20,21,33,34,36,41–43 6 during 2 weeks,24,37,51 7 during 4 to 6 weeks,26,28,30,39,40,48,52 3 during 12 weeks,22,35,45 and 1 over the course of a year.49 In the case of 12 interventions, the duration was not specified.23,25,27,29,31,32,38,44,46,47,50,53
Effectiveness
Effectiveness was characterized on the basis of measurements of different outcomes that could be categorized into our 3 broad categories: increased knowledge of HIV transmission and prevention, behavior changes related to sexual practices, and reductions in STI incidence. These categories, identified after our review of the 34 included articles, reflect an evolving understanding of the assessment of prevention interventions. The different measures of effectiveness underscore the importance of relating improved knowledge to changes in behavior and then linking behavior changes to reductions in STI incidence. There was variability within each of these categories in that different authors used different knowledge areas, types of behaviors, and even types of STIs as effectiveness indicators.
Of the 43 interventions identified, 23 measured improved knowledge related to HIV/AIDS in general,21,22,24,32,39,41–44,47,51,53 5 focused more specifically on perceived vulnerability,26,37 2 focused on transmission knowledge,29,36 and 1 measured HIV vaccine knowledge.38 Forty-two interventions incorporated behavior change as an outcome measure, 32 measured changes in risk-related behavior,20–24,26–30,32–35,37–50,52,53 5 focused solely on HIV testing,20,31,36,42,50 and 1 focused on more general skill acquisition and use.51 Although STI incidence was an outcome measure in 10 interventions, only 6 of these studies included outcome information in their descriptions of results25,29,33,34,44,48 (Table A).
There were instances in which an intervention was judged to be partially effective, with improvements in, for example, knowledge but not risk-related behavior. Of the 43 interventions, 31 were judged to be effective,20–23,25–30,32–36,38–41,44,48–53 7 partially effective,24,29,31,33,43,45,47 and 5 not effective.37,46
Meta-Analysis Findings
Results from the Begg and Egger test ruled out the existence of publication bias in the 3 meta-analyses.
HIV knowledge.
In this meta-analysis, 9 interventions21,24,32,33,39 were included that provided sufficient information for between-intervention comparisons; the analysis was carried out to estimate combined effects on increased knowledge regarding HIV. A general increase of 0.59 was observed (95% CI = 0.43, 0.75), with moderate heterogeneity (I2 = 65%) (Figure A, available as a supplement to the online version of this article at http://www.ajph.org).
Behavior change.
In this meta-analysis, 12 studies were included that collected information regarding changes in condom use and provided the necessary information for interstudy comparisons.27–29,32,38–40,44,45,49,51,52 The pooled effect showed a statistically significant increase of 60% in postintervention frequency of condom use (OR = 1.60; 95% CI = 1.16, 2.19). Heterogeneity was measured at 80%. According to the Galbraith chart, the study authored by Van Devanter et al.28 was the greatest contributor to this measure, and when that study was eliminated from the analysis heterogeneity decreased to 55.5% (Figure B, available as a supplement to the online version of this article at http://www.ajph.org).
STI incidence.
Five studies provided the necessary information about STI incidence and were included in the meta-analysis.25,32,33,44,48 The combined obtained effect (RR = 0.59; 95% CI = 0.46, 0.75) indicated that preventive interventions significantly reduced the risk of STIs by 41%. No heterogeneity between study results was observed (Figure C, available as a supplement to the online version of this article at http://www.ajph.org).
DISCUSSION
This study represents the most recent review of the literature related to HIV prevention interventions among socioeconomically deprived ethnic minority women and provides, to our knowledge, the highest level of available evidence regarding the use of such interventions to reduce HIV transmission in that population. Also, given that we used the Cochrane assessment tool in our analyses, our study incorporated a rigorous measure of methodological quality.18
One of the principal observations highlighted by our review is the multifactorial impact of HIV prevention interventions as assessed via our 3 outcome measure categories. The review showed that the majority of the interventions were either partially or fully effective in attaining their goals of improved knowledge, behavior change, and reductions in STI transmission. The statistical significance of our meta-analysis results underscores the overall effectiveness of the interventions examined in this systematic review.
Of particular importance is the determination that these interventions translate into statistically significant reductions in STI incidence, an important marker of HIV transmission.54 It is noteworthy that our study is one of the first to analyze reductions in STI incidence among women who have participated in prevention programs. The fact that our meta-analyses showed a statistically significant reduction in STI transmission provides important evidence supporting the overall effectiveness of directing prevention programming toward this vulnerable population. This is particularly relevant given the ongoing public health challenge that STI transmission rates represent.
For policymakers, our review demonstrates the feasibility of working with multiple intervention components while at the same time facilitating more effective interventions that take into account the principal outcome measures of knowledge, behavior change, and STI transmission rates. We hope that the results of this review will encourage a focus on the key effectiveness indicators for HIV prevention interventions while highlighting crucial intervention characteristics such as cultural adaptation.
Limitations and Strengths
One possible limitation of our review is the absence of published studies from outside the United States and the difficulty in generalizing the results to other countries. Given the diversity of ethnic minority groups in Canada, Europe, and other OECD member states, we believe that additional information is needed to determine the effectiveness of HIV prevention interventions in other cultural contexts. The lack of studies from outside the United States underscores the need for additional research on HIV prevention interventions in other countries where socioeconomically deprived ethnic minority women continue to be at increased risk of contracting the disease. At the same time, our review can provide a framework for prevention intervention development in other countries and for the types of outcome measurements that can best assess intervention effectiveness.
Another limitation of our study is the lack of standardization of the socioeconomic status variable, which is an inherent methodological challenge in systematic reviews and any secondary data analyses in which variables have already been defined. We used the definition of low socioeconomic status or low income level outlined by the authors themselves when defining their sample. This criterion has been used in previous systematic reviews. The definition was explicit in some cases and not explicit in others, making it apparent that variability was likely to exist. However, such variability is frequently seen in studies of health inequalities when there is not a globally accepted definition. In addition, the utility of prevention interventions would be further strengthened by an analysis of cost-effectiveness, which would provide important evidence related to the affordability of preventing HIV transmission.
A principal strength of our review is the exhaustive search, which extended back to the beginning of the HIV/AIDS epidemic and covered a wide geographic area. However, this systematic review is subject to the same publication bias as other systematic reviews, and such bias may have led to overestimations of intervention effectiveness.18
In the process of selecting studies to evaluate preventive interventions among socioeconomically disadvantaged ethnic minority women, we encountered many studies in which populations with different characteristics were analyzed without disaggregation. As a result, we adopted strict inclusion criteria and included only interventions that targeted populations in which at least 80% of the participants were reported to belong to an ethnic minority group and to have a low income or be unemployed. By reducing the participation percentage required to meet our inclusion criteria, we could have included other potential interventions with different approaches or outcome measurements; however, that strategy would have led to greater variability in our study population, thereby affecting the internal validity of our results.
Conclusions
Our study demonstrates the feasibility and effectiveness of developing HIV prevention interventions targeting socioeconomically deprived ethnic minority women. Additional research in this area is necessary in countries outside the United States, and there is also a need to determine the cost-effectiveness of such interventions.
ACKNOWLEDGMENTS
This study was supported by the National Institute of Health Carlos III (study identification number PS09/00747) in partnership with the Andalusian Regional Ministry of Health (study identification number PI-0152).
HUMAN PARTICIPANT PROTECTION
No protocol approval was needed for this study because no human participants were involved.
REFERENCES
- 1.Joint United Nations Programme on HIV/AIDS. Report on the global AIDS epidemic. Available at: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Global_Report_2013_en_1.pdf. Accessed August 26, 2017.
- 2.Organisation for Economic Co-operation and Development. AIDS incidence and HIV prevalence. Available at: http://www.oecd-ilibrary.org/docserver/download/8111101ec015.pdf?expires=1503955084&id=id&accname=guest&checksum=A655E31F13FACDD7137D96D6BC63E63A. Accessed August 26, 2017.
- 3.Centers for Disease Control and Prevention. HIV surveillances report. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf. Accessed August 26, 2017.
- 4.European Centre for Disease Prevention and Control/World Health Organization Regional Office for Europe. HIV/AIDS Surveillance in Europe 2012. Stockholm, Sweden: European Centre for Disease Prevention and Control; 2013. [Google Scholar]
- 5.Dodds C, Hickson F, Chinouya M, Chwaula J, Weatherburn P. Plan of action to meet the HIV prevention needs of Africans living in England. Available at: https://researchonline.lshtm.ac.uk/1396/1/report2008a.pdf. Accessed August 26, 2017.
- 6.Johnson AS, Beer L, Sionean C et al. HIV infection—United States, 2008 and 2010. MMWR Suppl. 2013;62(3):112–119. [PubMed] [Google Scholar]
- 7.Hall HI, Geduld J, Boulos D et al. Epidemiology of HIV in the United States and Canada: current status and ongoing challenges. J Acquir Immune Defic Syndr. 2009;51(suppl 1):S13–S20. doi: 10.1097/QAI.0b013e3181a2639e. [DOI] [PubMed] [Google Scholar]
- 8.Loutfy MR, Logie CH, Zhang Y et al. Gender and ethnicity differences in HIV-related stigma experienced by people living with HIV in Ontario, Canada. PLoS One. 2012;7(12):e48168. doi: 10.1371/journal.pone.0048168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh Setia M, Quesnel-Vallee A, Curtis S, Lynch J. Assessing the role of individual and neighbourhood characteristics in HIV testing: evidence from a population based survey. Open AIDS J. 2009;3:46–54. doi: 10.2174/1874613600903010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gilbert L, Goddard-Eckrich D, Hunt T et al. Efficacy of a computerized intervention on HIV and intimate partner violence among substance-using women in community corrections: a randomized controlled trial. Am J Public Health. 2016;106(7):1278–1286. doi: 10.2105/AJPH.2016.303119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hemmige V, McFadden R, Cook S, Tang H, Schneider JA. HIV prevention interventions to reduce racial disparities in the United States: a systematic review. J Gen Intern Med. 2012;27(8):1047–1067. doi: 10.1007/s11606-012-2036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 13.Crepaz N, Horn AK, Rama SM et al. The efficacy of behavioral interventions in reducing HIV risk sex behaviors and incident sexually transmitted disease in black and Hispanic sexually transmitted disease clinic patients in the United States: a meta-analytic review. Sex Transm Dis. 2007;34(6):319–332. doi: 10.1097/01.olq.0000240342.12960.73. [DOI] [PubMed] [Google Scholar]
- 14.Althoff MD, Grayson CT, Witt L, Holden J, Reid D, Kissinger P. A meta-analysis of the efficacy of behavioral interventions to reduce risky sexual behavior and decrease sexually transmitted infections in Latinas living in the United States. Health Educ Behav. 2015;42(6):709–718. doi: 10.1177/1090198114540461. [DOI] [PubMed] [Google Scholar]
- 15.Herbst JH, Kay LS, Passin WF et al. A systematic review and meta-analysis of behavioral interventions to reduce HIV risk behaviors of Hispanics in the United States and Puerto Rico. AIDS Behav. 2007;11(1):25–47. doi: 10.1007/s10461-006-9151-1. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Organisation for Economic Co-operation and Development. List of OECD member countries: ratification of the convention on the OECD. Available at: http://www.oecd.org/about/membersandpartners/list-oecd-member-countries.htm. Accessed August 26, 2017.
- 18.Higgins JPT, Altman DG, Gotzsche PC et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. London, England: Cochrane Collaboration; 2011. [Google Scholar]
- 20.Apanovitch AM, McCarthy D, Salovey P. Using message framing to motivate HIV testing among low-income, ethnic minority women. Health Psychol. 2003;22(1):60–67. doi: 10.1037//0278-6133.22.1.60. [DOI] [PubMed] [Google Scholar]
- 21.Ashworth CS, DuRant RH, Gaillard G, Rountree J. An experimental evaluation of an AIDS educational intervention for WIC mothers. AIDS Educ Prev. 1994;6(2):154–162. [PubMed] [Google Scholar]
- 22.Baumler E, Glassman J, Tortolero S et al. Examination of the relationship between psychosocial mediators and intervention effects in It’s Your Game: an effective HIV/STI/pregnancy prevention intervention for middle school students. AIDS Res Treat. 2012;2012:298494. doi: 10.1155/2012/298494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campbell AN, Tross S, Hu MC, Pavlicova M, Kenney J, Nunes EV. Female condom skill and attitude: results from a NIDA clinical trials network gender-specific HIV risk reduction study. AIDS Educ Prev. 2011;23(4):329–340. doi: 10.1521/aeap.2011.23.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carey MP, Braaten LS, Maisto SA et al. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women: a second randomized clinical trial. Health Psychol. 2000;19(1):3–11. doi: 10.1037//0278-6133.19.1.3. [DOI] [PubMed] [Google Scholar]
- 25.Champion JD, Collins JL. Comparison of a theory-based (AIDS risk reduction model) cognitive behavioral intervention versus enhanced counseling for abused ethnic minority adolescent women on infection with sexually transmitted infection: results of a randomized controlled trial. Int J Nurs Stud. 2012;49(2):138–150. doi: 10.1016/j.ijnurstu.2011.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dancy BL, Marcantonio R, Norr K. The long-term effectiveness of an HIV prevention intervention for low-income African American women. AIDS Educ Prev. 2000;12(2):113–125. [PubMed] [Google Scholar]
- 27.Davey-Rothwell MA, Tobin K, Yang C, Sun CJ, Latkin CA. Results of a randomized controlled trial of a peer mentor HIV/STI prevention intervention for women over an 18 month follow-up. AIDS Behav. 2011;15(8):1654–1663. doi: 10.1007/s10461-011-9943-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Devanter N, Gonzales V, Merzel C, Parikh NS, Celantano D, Greenberg J. Effect of an STD/HIV behavioral intervention on women’s use of the female condom. Am J Public Health. 2002;92(1):109–115. doi: 10.2105/ajph.92.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flaskerud JH, Nyamathi AM, Uman GC. Longitudinal effects of an HIV testing and counseling programme for low-income Latina women. Ethn Health. 1997;2(1–2):89–103. doi: 10.1080/13557858.1997.9961818. [DOI] [PubMed] [Google Scholar]
- 30.Greenberg J, Hennessy M, MacGowan R et al. Modeling intervention efficacy for high-risk women: the WINGS Project. Eval Health Prof. 2000;23(2):123–148. doi: 10.1177/016327870002300201. [DOI] [PubMed] [Google Scholar]
- 31.Grinstead Reznick O, Comfort M, McCartney K, Neilands TB. Effectiveness of an HIV prevention program for women visiting their incarcerated partners: the HOME Project. AIDS Behav. 2011;15(2):365–375. doi: 10.1007/s10461-010-9770-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hawk M. The Girlfriends Project: results of a pilot study assessing feasibility of an HIV testing and risk reduction intervention developed, implemented, and evaluated in community settings. AIDS Educ Prev. 2013;25(6):519–534. doi: 10.1521/aeap.2013.25.6.519. [DOI] [PubMed] [Google Scholar]
- 33.Jemmott JB, III, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: a randomized controlled trial. Arch Pediatr Adolesc Med. 2005;159(5):440–449. doi: 10.1001/archpedi.159.5.440. [DOI] [PubMed] [Google Scholar]
- 34.Jemmott LS, Jemmott JB, III, O’Leary A. Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings. Am J Public Health. 2007;97(6):1034–1040. doi: 10.2105/AJPH.2003.020271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones R, Hoover DR, Lacroix LJ. A randomized controlled trial of soap opera videos streamed to smartphones to reduce risk of sexually transmitted human immunodeficiency virus (HIV) in young urban African American women. Nurs Outlook. 2013;61(4):205–215.e3. doi: 10.1016/j.outlook.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kalichman SC, Kelly JA, Hunter TL, Murphy DA, Tyler R. Culturally tailored HIV-AIDS risk-reduction messages targeted to African-American urban women: impact on risk sensitization and risk reduction. J Consult Clin Psychol. 1993;61(2):291–295. doi: 10.1037//0022-006x.61.2.291. [DOI] [PubMed] [Google Scholar]
- 37.Kalichman SC, Rompa D, Coley B. Experimental component analysis of a behavioral HIV-AIDS prevention intervention for inner-city women. J Consult Clin Psychol. 1996;64(4):687–693. doi: 10.1037//0022-006x.64.4.687. [DOI] [PubMed] [Google Scholar]
- 38.Koblin BA, Bonner S, Hoover DR et al. A randomized trial of enhanced HIV risk-reduction and vaccine trial education interventions among HIV-negative, high-risk women who use noninjection drugs: the UNITY study. J Acquir Immune Defic Syndr. 2010;53(3):378–387. doi: 10.1097/QAI.0b013e3181b7222e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.St. Lawrence JS, Wilson TE, Eldridge GD, Brasfield TL, O’Bannon RE., III Community-based interventions to reduce low income, African American women’s risk of sexually transmitted diseases: a randomized controlled trial of three theoretical models. Am J Community Psychol. 2001;29(6):937–964. doi: 10.1023/A:1012919700096. [DOI] [PubMed] [Google Scholar]
- 40.Morrison-Beedy D, Jones SH, Xia Y, Tu X, Crean HF, Carey MP. Reducing sexual risk behavior in adolescent girls: results from a randomized controlled trial. J Adolesc Health. 2013;52(3):314–321. doi: 10.1016/j.jadohealth.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nyamathi A, Flaskerud J, Bennett B, Leake B, Lewis C. Evaluation of two AIDS education programs for impoverished Latina women. AIDS Educ Prev. 1994;6(4):296–309. [PubMed] [Google Scholar]
- 42.Nyamathi AM, Stein JA. Assessing the impact of HIV risk reduction counseling in impoverished African American women: a structural equations approach. AIDS Educ Prev. 1997;9(3):253–273. [PubMed] [Google Scholar]
- 43.Nyamathi AM, Kington RS, Flaskerud J, Lewis C, Leake B, Gelberg L. Two-year follow-up of AIDS education programs for impoverished women. West J Nurs Res. 1999;21(3):405–425. doi: 10.1177/01939459922043956. [DOI] [PubMed] [Google Scholar]
- 44.Peragallo N, Gonzalez-Guarda RM, McCabe BE, Cianelli R. The efficacy of an HIV risk reduction intervention for Hispanic women. AIDS Behav. 2012;16(5):1316–1326. doi: 10.1007/s10461-011-0052-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Raj A, Amaro H, Cranston K et al. Is a general women’s health promotion program as effective as an HIV-intensive prevention program in reducing HIV risk among Hispanic women? Public Health Rep. 2001;116(6):599–607. doi: 10.1093/phr/116.6.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Robinson BBE, Uhl G, Miner M et al. Evaluation of a sexual health approach to prevent HIV among low income, urban, primarily African American women: results of a randomized controlled trial. AIDS Educ Prev. 2002;14(suppl A):81–96. doi: 10.1521/aeap.14.4.81.23876. [DOI] [PubMed] [Google Scholar]
- 47.Sales JM, Brown JL, DiClemente RJ, Rose E. Exploring factors associated with nonchange in condom use behavior following participation in an STI/HIV prevention intervention for African-American adolescent females. AIDS Res Treat. 2012;2012:231417. doi: 10.1155/2012/231417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shain RN, Piper JM, Newton ER et al. A randomized, controlled trial of a behavioral intervention to prevent sexually transmitted disease among minority women. N Engl J Med. 1999;340(2):93–100. doi: 10.1056/NEJM199901143400203. [DOI] [PubMed] [Google Scholar]
- 49.Sikkema K. HIV prevention among women in low-income housing developments: issues and intervention outcomes in a place-based randomized controlled trial. Ann Am Acad Pol Soc Sci. 2005;599(1):52–70. [Google Scholar]
- 50.Surratt HL, O’Grady C, Kurtz SP, Levi-Minzi MA, Chen M. Outcomes of a behavioral intervention to reduce HIV risk among drug-involved female sex workers. AIDS Behav. 2014;18(4):726–739. doi: 10.1007/s10461-014-0723-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Takahashi LM, Tobin KE, To S et al. Chieh Mei Ching Yi: a randomized controlled trial of a culturally tailored HIV prevention intervention for Chinese massage parlor women in Los Angeles. AIDS Educ Prev. 2013;25(6):508–518. doi: 10.1521/aeap.2013.25.6.508. [DOI] [PubMed] [Google Scholar]
- 52.Wingood GM, Di Clemente RJ, Villamizar K et al. Efficacy of a health educator-delivered HIV prevention intervention for Latina women: a randomized controlled trial. Am J Public Health. 2011;101(12):2245–2252. doi: 10.2105/AJPH.2011.300340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wingood GM, Robinson L, Braxton ND et al. Comparative effectiveness of a faith-based HIV intervention for African American women: importance of enhancing religious social capital. Am J Public Health. 2013;103(12):2226–2233. doi: 10.2105/AJPH.2013.301386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hayes R, Watson-Jones D, Celum C, van de Wijgert J, Wasserheit J. Treatment of sexually transmitted infections for HIV prevention: end of the road or new beginning? AIDS. 2010;24(suppl 4):S15–S26. doi: 10.1097/01.aids.0000390704.35642.47. [DOI] [PMC free article] [PubMed] [Google Scholar]