Abstract
Objectives. To evaluate a community-level sodium-reduction intervention in Boston, Massachusetts. Reducing sodium in the food offerings of community settings may help reduce hypertension disparities.
Methods. We examined changes in the proportion of prepackaged foods with greater than 200 milligrams of sodium in 7 hospitals, 8 YMCAs, 4 community health centers, and 2 organizations serving homeless populations. Research assistants documented prepackaged items in cafeterias, kiosks, and vending machines before and after the intervention (2013–2015). We assessed intervention change via linear mixed models accounting for repeated observations.
Results. There were 161 access points at baseline (4347 facings) and 171 (4996 facings) at follow-up. The percentage of prepackaged products with greater than 200 milligrams of sodium decreased from 29.0% at baseline to 21.5% at follow-up (P = .003). Changes were driven by improvements in hospital cafeterias and kiosks (P = .003). The percentage of products with greater than 200 milligrams of sodium in YMCA vending decreased 58% (from 27.2% to 11.5%; P = .017); other organizations had nonsignificant declines.
Conclusions. We found modest reductions in the percentage of higher-sodium prepackaged products across community institutions. Community-level interventions may increase availability of lower-sodium products in the food supply.
Most Americans consume too much sodium, with an average intake of 3400 milligrams per day.1 The 2015 Dietary Guidelines for Americans recommend consuming less than 2300 milligrams each day in light of the strong evidence linking high sodium intake to hypertension, with even lower intakes recommended for children.1,2 Hypertension affects nearly 1 in 3 adults in the United States, is a major risk factor for heart disease and stroke, and is estimated to have a financial impact of $46 billion per year.3,4 Substantial racial/ethnic disparities also persist in the prevalence of hypertension.3,4 To address these trends in hypertension, the Institute of Medicine and National Salt Reduction Initiative have encouraged the food industry to reduce sodium in the food supply,5 as most of the sodium Americans consume (approximately 70%) is found in foods outside the home such as prepackaged, processed, and restaurant foods.6
Many prepackaged foods, including savory snacks such as chips, are among the top-10 foods from which Americans consume more than 40% of the sodium eaten each day.7 In 2016, the US Food and Drug Administration released a draft, voluntary guidance on standards for the food industry to reduce the sodium content in food categories including snack items, bakery products, and cereals, which are often served as prepackaged items.8 While such broad-reaching changes are under way, interventions addressing food offerings in community institutions can be important to both influence dietary patterns of consumers and influence food manufacturers to more rapidly adopt sodium-reduction standards.9 The Centers for Disease Control and Prevention (CDC) has successfully funded organizations to implement community- or institution-level procurement, reformulation, product placement, and consumer awareness strategies to reduce sodium content and improve their food environments.9
Much literature involving improvements in the healthfulness of prepackaged food products has focused on vending and competitive food changes in schools and worksites,10–13 with less (but growing) attention given to hospitals, other health care settings, and recreational community-based organizations (e.g., YMCAs).14–16 Such settings often serve as critical assets in a community and have missions aligned with healthy living. Hospitals, in particular, have been called on to be an example of health in the communities they serve.17 In many health care and community organizations, prepackaged food items are likely to be found in vending machines, as well as cafeterias and kiosks. It is estimated that hospitals (and nursing homes) make up approximately 8.2% of vending machines in the United States.18 Such organizations may be major employers and service providers to groups suffering disproportionately from chronic conditions. In addition, these organizations may have significant purchasing power such that their shift to healthier, lower-sodium food products may signal to the food industry an increase in the demand for such products.
Few studies have documented the healthfulness of food items in these community settings, but those that do generally show significant opportunity for improvement in the offerings within cafeterias, vending, and point-of purchase displays.19–22 For instance, a study assessing 15 health care facilities in California found the majority of items in the 96 vending machines would be classified as unhealthy according to the state’s school nutrition standards.16 Interventions to improve the food environment in other contexts have been successful, and modifications to the availability and presentation of healthier food items have been shown to influence food purchases in various settings.13,22,23 As most sodium is consumed outside the home,6 changing the sodium offerings in community settings is a critical population-level strategy.
In 2013, through funding from CDC’s Racial and Ethnic Approaches to Community Health (REACH) Demonstration Project, the Boston Public Health Commission (BPHC) in Boston, Massachusetts, set out to address racial/ethnic disparities in hypertension and obesity. We focused on the prepackaged sodium reduction component of this initiative, which aimed to reduce the percentage of products with greater than 200 milligrams of sodium per serving in various community institutions. This study adds to the limited evidence base by evaluating the effectiveness of a prepackaged sodium reduction initiative in important community settings including health care facilities, organizations serving homelessness populations, and YMCAs.
METHODS
In this study, we used a quasi-experimental pre–post design with no control group. The sample included 21 community institutions selected because they were located in, employed, or served residents in 5 priority neighborhoods—defined by BPHC as those with the highest proportion of Black and Latino residents and a disproportionate burden of chronic diseases. Site recruitment varied by sector; all Boston hospitals were invited to participate as they have a large employee base that includes many lower-wage workers who live in priority neighborhoods; community health centers and community-based organizations located within those 5 neighborhoods were invited to participate; and the YMCA, a core partner in the REACH Project, included all Boston-based branches. Organizations that chose to participate completed an initial pledge form stating their commitment. We estimate that approximately 78 000 people were reached by this intervention each week, on the basis of the number of employees and individuals served per week for each organization. This estimate is derived from information collected on the pledge form, an implementation survey, the Boston Redevelopment Authority, and a staff contact at the YMCA.
At each site, trained research assistants followed an audit protocol to document the prepackaged food items located in all access points at baseline (between fall 2013 and summer 2014) and follow-up (summer 2015). Access points represent the distinct locations in each site that served prepackaged snack items, such as vending machines, promotional stands or coolers within cafeterias, and smaller cafes or kiosks in other areas of the facility. We categorized the access points into 2 types: vending machines and cafeterias or kiosks. Research assistants recorded the brand and size of each product, counted the number of facings (spaces facing the consumer) in each vending machine or on a cafeteria or kiosk cooler or shelf, and took digital photographs, which could be used as a reference if needed. They included fruits that were not packaged (e.g., apples, bananas) but were served in access points similar to other prepackaged snack items.
The research assistants collected the majority of the nutrient information (e.g., sodium, calories), both per package and per serving, for each product from product packaging or the manufacturers’ Web sites or by contacting the manufacturer (98% of facings). They gathered information not obtained from the manufacturer or when not applicable (e.g., fruits) from the US Department of Agriculture Nutrient Database24 (< 2% of facings) or the Food Processor Nutrition Analysis Software (< 0.5% of facings; Esha Research, Salem, OR; SQL10.12; 2013), which provided estimated nutrients for combination foods (e.g., snacks containing cheese, crackers, and grapes).
Intervention
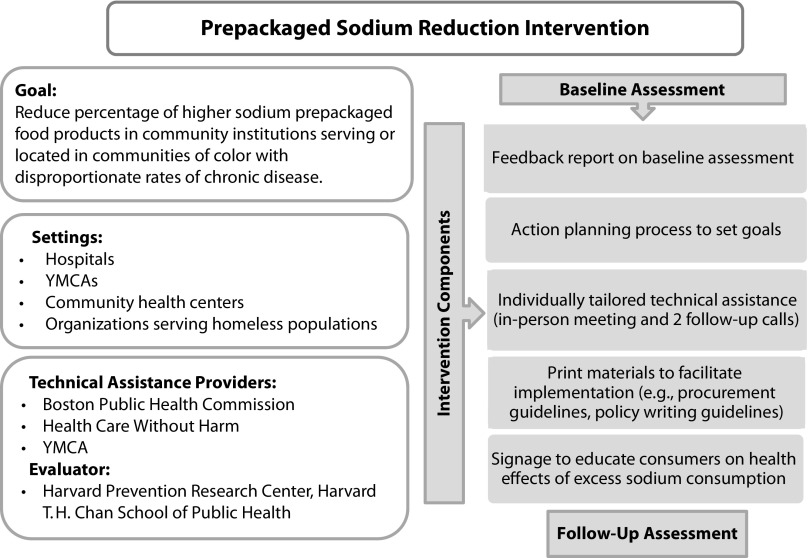
The prepackaged sodium-reduction intervention comprised
A feedback report on baseline assessment of current levels of sodium content in products and how they compared with other organizations in their sector (Figure A, available as a supplement to the online version of this article at http://www.ajph.org);
An action plan process that included setting goals for sodium reduction;
Individually tailored technical assistance;
Provision of materials such as decision aids, procurement guidelines, and policy-writing guides to support implementation strategies; and
Educational materials to identify healthy, lower-sodium options and increase consumer awareness of the health effects associated with excess sodium (Figure 1).
FIGURE 1—
Overview of Prepackaged Sodium Reduction Intervention Goal, Settings, and Components
Note. Sample intervention resources can be found at: http://www.bphc.org/whatwedo/healthy-eating-active-living/reach-project/Pages/sodium-reduction-initiative.aspx.
The intervention period ranged from 1 to 1.5 years depending on the site. We recruited sites and conducted baseline assessments between fall 2013 and summer 2014, and we conducted follow-up assessments for all sites during summer 2015. Technical assistance included an initial in-person meeting and 2 follow-up calls. We provided Webinars for site vendors and smaller organizations to educate them on the initiative and how they could support such changes. Two registered dietitians and other experienced staff from BPHC and Healthcare Without Harm were the technical assistance providers. Staff from the Harvard T. H. Chan School of Public Health’s Prevention Research Center conducted the evaluation, and the YMCA supported the overall intervention efforts. Intervention participants or leads at the respective sites included directors of food and nutrition services at the hospitals, operations or wellness directors at the YMCAs, and Special Supplemental Nutrition Program for Women, Infants, and Children program directors or business development managers at the other sites.
Measure
The main outcome of interest was the percentage of prepackaged foods with greater than 200 milligrams of sodium per serving within access points. At the study start, we convened registered dietitians and food service directors at participating sites to review national and local nutrition standards. The 200-milligram-per-serving cut-off was determined, and aligns with the Massachusetts School Nutrition Standards for Competitive Foods and Beverages.25 To better understand factors influencing implementation, we documented organizations’ goals and progress in site action plans, and conducted interviews with several implementation leaders at follow-up.
Statistical Analysis
Descriptive statistics included the number of organizations, access points, and facings. We used modified categories from the Food and Nutrient Database for Dietary Studies26 to assess percentage of facings falling into specified food categories. We assessed change in the percentage of prepackaged foods with sodium greater than 200 milligrams per serving from baseline to follow-up by using linear mixed models, accounting for clustering of access points within sites. We conducted stratified analyses to assess differences by access point type (i.e., vending machine vs cafeteria or kiosk) and sector-type (e.g., hospital, YMCA). We performed analyses with SAS version 9.4 (SAS Institute, Cary, NC) and a P value (2-tailed) of .05.
RESULTS
Twenty-one organizations set goals on action plans related to reducing sodium within their facilities (Table 1); there were 7 hospitals, 8 YMCA branches, 4 community health centers, and 2 organizations that served individuals experiencing homelessness. Sixty-six percent of organizations participated in the initial technical assistance meeting and at least 2 follow-ups, though more was available as needed. At baseline, these organizations contained 161 distinct access points (49 vending machines, 112 hospital cafeterias or kiosks), which contained 4347 food facings (1561 in vending machines, 2786 in hospital cafeterias or kiosks). At follow-up, there were 171 distinct access points (45 vending machines, 126 hospital cafeterias or kiosks), which contained 4996 individual food facings (1497 vending machines, 3499 hospital cafeterias or kiosks). Table 2 reflects the percentage of food facings categorized by food type. At baseline and follow-up, approximately one third of the food facings were categorized as salty snacks or chips (this categorization does not reflect the amount of sodium in a product). Fruits represented approximately 7% of facings at baseline, but 14% at follow-up.
TABLE 1—
Description of Organizations (n = 21) Participating in Racial and Ethnic Approaches to Community Health Prepackaged Sodium Reduction Intervention: Boston, MA, Fall 2013–Summer 2014 Through Summer 2015
| Characteristics | Baseline | Follow-Up |
| No. of organizations | ||
| Total no. | 21 | 21 |
| Hospitals | 7 | 7 |
| Community health centers | 4 | 4 |
| YMCAs | 8 | 8 |
| Homeless organizations | 2 | 2 |
| No. of access pointsa | ||
| Total no. | 161 | 171 |
| Hospital cafeterias and kiosks | 112 | 126 |
| Vending machines | 49 | 45 |
| Hospitals | 34 | 31 |
| YMCAs | 9 | 7 |
| Community health centers | 4 | 5 |
| Homeless organizations | 2 | 2 |
| No. of facingsb | ||
| Total no. | 4347 | 4996 |
| Hospital cafeterias and kiosks | 2786 | 3499 |
| Vending machines | 1561 | 1497 |
| Hospitals | 1106 | 1067 |
| YMCAs | 250 | 240 |
| Community health centers | 157 | 130 |
| Homeless organizations | 48 | 60 |
Access points refer to distinct locations in the setting that served prepackaged snack items such as vending machines, coolers, shelves, and kiosks.
Facings refer to selection slots or spaces in access points facing the consumer.
TABLE 2—
Percentage of Prepackaged Snack Facings Across All Organizations (n = 21) Categorized by Food Type: Boston, MA, Fall 2013–Summer 2014 Through Summer 2015
| Food Type | Baseline, % | Follow-Up, % |
| Salty snacks or chips | 33.63 | 33.39 |
| Grains or granola bars | 24.39 | 16.96 |
| Sweets and candy | 12.56 | 10.87 |
| Grain-based sweets | 9.71 | 9.97 |
| Dairy | 8.74 | 10.87 |
| Fruits | 6.72 | 14.25 |
| Nuts and trail mixes | 3.89 | 2.94 |
| Miscellaneousa | 0.37 | 0.74 |
Note. Facings refer to selection slots or spaces in access points facing the consumer.
Miscellaneous includes items such as vegetables, meats, and items that did not fit into other categories.
Overall, the percentage of prepackaged food products with greater than 200 milligrams per serving of sodium changed after the implementation of the intervention (Table 3). When we adjusted for clustering of access points within organizations, access points contained an average of 29.0% of products with greater than 200 milligrams per serving of sodium at baseline and after the intervention there was an average of 21.5%, reflecting a statistically significant change from baseline to follow-up (–7.5 percentage points; P = .003). When we stratified by access point type, there was a significant change of −9.8 percentage points (P = .003) in the percentage of foods with greater than 200 milligrams per serving of sodium in cafeterias or kiosks, but no statistically significant change overall for vending machines (P = .54). When we further stratified vending machines by sector, there was a statistically significant 58% decrease from baseline to follow-up for access points within YMCAs (–15.8 percentage points; P = .02). There were also nonsignificant decreases for vending access points within community health centers (–6.2 percentage points; P = .20) and organizations serving homeless populations (–13.4 percentage points; P = .19), and a nonsignificant increase in the percentage of prepackaged foods with greater than 200 milligrams per serving of sodium across vending machine access points in hospitals (2.6 percentage points; P = .41). We found similar results when we examined the percentage of products defined by greater than 200 milligrams of sodium per package (Table A, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 3—
Change in the Percentage of Prepackaged Snack Facings With Greater Than 200 Milligrams of Sodium per Serving: Boston, MA, Fall 2013–Summer 2014 Through Summer 2015
| Organization and Access Point Type | Baseline (SE) | Follow-Up (SE) | Change (SE) | 95% CI | P |
| All organizations (n = 21) | 29.0 (2.0) | 21.5 (1.9) | −7.5 (2.5) | −12.4, −2.6 | .003 |
| Hospital cafeterias and kiosks (n = 7)a | 30.7 (2.5) | 20.9 (2.4) | −9.8 (3.3) | −16.3, −3.3 | .003 |
| All vending machines (n = 21)b | 25.0 (2.1) | 23.4 (2.2) | −1.5 (2.5) | −6.5, 3.4 | .54 |
| Hospital vending (n = 7) | 24.8 (3.1) | 27.4 (3.1) | 2.6 (3.1) | −3.7, 8.9 | .41 |
| YMCA vending (n = 8) | 27.2 (2.9) | 11.5 (3.6) | −15.8 (5.0) | −27.7, −3.9 | .017 |
| Community health center vending (n = 4) | 25.2 (3.2) | 19.0 (2.9) | −6.2 (4.1) | −17.5, 5.1 | .20 |
| Homeless organization vending (n = 2) | 40.0 (5.0) | 26.6 (5.0) | −13.4 (4.2) | −67.0, 40.2 | .19 |
Note. CI = confidence interval. Estimates account for clustering of access points within organizations.
Cafeterias and kiosks were only located in the 7 hospitals; no other sectors had cafeterias or kiosks.
Includes vending machines across all organizations including hospitals, community health centers, YMCAs, and homeless organizations.
DISCUSSION
In this study, we found evidence of effectiveness for a prepackaged sodium-reduction intervention in various community institutions. After implementation of the intervention, which included a baseline assessment feedback report, goal-setting process, tailored technical assistance, and provision of implementation and educational materials, the percentage of prepackaged foods with greater than 200 milligrams per serving of sodium decreased significantly across sites from 29.0% at baseline to 21.5% at follow-up. The change was primarily driven by reductions in the hospital cafeterias and kiosks. When we examined changes in vending machines by sector, YMCAs showed a statistically significant decline in the percentage of products that exceeded 200 milligrams per serving of sodium—going from 27.2% at baseline to 11.5% at follow-up. Community health centers and organizations serving homeless populations also had a decline, though the change was not significant likely because of the small number of access points in these settings.
While national efforts are under way to reduce sodium in the food supply, this study adds to the growing body of evidence showing that community-level efforts to reduce sodium can also be effective across a broad array of institutions.27,28 In addition, in this study, we directly observed the food environment and collected brand-specific and size information to more accurately assess the changes made instead of relying on general estimates or self-report from organizational staff. Our hospital sample included both self-managed operations and 2 different outside food-service vendors, which strengthens the generalizability of our results.
We found statistically significant changes in the cafeterias and kiosks located in hospitals, but not in hospital vending. One explanation for this finding may relate to organizational control. The cafeterias and kiosks, unlike vending machines, which may have strict multiyear contracts, could have more flexibility to add healthier items, remove less healthful items, or change presentation of food items. In addition, the sheer size of a hospital cafeteria may provide more flexibility in the space available to make changes or modify choice architecture to support healthier choices (e.g., placing fruit near check-out, creating large displays of healthy options). As there was a substantial change in the percentage of facings categorized as fruit from baseline (7%) to follow-up (14%), increasing the amount of fruit offered by adding fruit facings or entirely new access points in cafeterias and kiosks may have been one strategy used. Also, improving the healthfulness or number of lower-sodium “grab and go” items in cafeterias and kiosks may have contributed to the changes seen in these access points.
Challenges in making changes to the product offerings in vending machines have been noted previously in the literature. In health care facilities in Australia, an intervention to improve availability of healthier foods showed no change in the healthier foods items in vending machines.29 Similarly, Queensland health facilities found success in improving some food outlets, but found changing the snack vending machines to be problematic.30 Such challenges may result from contract stipulations, vendor sales goals tied to product mix, or even lack of knowledge of who controls the vending. Though directors or staff in the food and nutrition services department were frequently the lead implementers in this intervention, not all sites knew who controlled or had control over the vending machines in their organizations. In fact, 2 of the hospitals that had an increase in the percentage of higher-sodium products in their vending reported that they did not have control in making any vending changes—even though the vending was physically located in the food services section.
Although there was no significant change for vending machines overall, when we stratified by sector, we found a statistically significant decrease in the percentage of products with greater than 200 milligrams per serving of sodium in the YMCAs. The YMCAs had previously switched to a local vending company that marketed itself as healthy, although the vendor did not have any sodium standards to follow. The executive director of Healthy Living for the Greater Boston YMCA and the director of shared services, who leveraged the YMCA’s purchasing power in contract negotiations, engaged their food vendor to request that they adhere to the intervention’s nutrition standards. The company agreed and had ample products to meet those standards. The central control of vending at the YMCA association level allowed the YMCA to leverage its purchasing power to make a request that could have an impact on all of the respective branches—resulting in an approximate 58% reduction in the products exceeding the 200 milligrams per serving sodium cut-point.
Decreases in the percentage of products with greater than 200 milligrams of sodium per serving in vending machines were also found in the community health centers and the organizations serving the homeless population. These decreases were not statistically significant because of the small sample sizes, but the changes indicate that smaller organizations with more direct control of vending may be able to make effective changes to the sodium content offered at their sites. At the community health center with the greatest decrease in the percentage of higher-sodium products, the supervisor of nutrition services with support of the vice president engaged the staff through a wellness team to provide education on the initiative and get input on the nutrition guidelines. The vendor brought products meeting the guidelines to the wellness team so they could sample the products and have input on what would be included in the vending. Although changes were made, the intervention lead acknowledged that monitoring may be needed and that the long-term sustainability of the changes could easily go away with change in staff or vendor as it was not a formal policy change.
As the field moves forward with implementing environmental changes, sustainability is important to consider. Intervention leads indicated that it is possible the momentum built around the initiative may fade and the next steps toward formalizing it may not occur. Some participants noted the need for standard contract language that could be built into bids for vendors, and some noted that continual monitoring is necessary even if contracts are changed as those who stock machines may run out of certain products and fill it in with what is available. In this study, we also found that lower-sodium products were available to fill vending machines and stock cafeterias and kiosks. Therefore, with appropriate outreach to vendors and cafeteria staff, these changes were made relatively quickly. This shows the potential of community institutions to shift the food industry toward more healthful and lower-sodium products. Another important aspect of sustainability relates to leadership engagement. Though many intervention leads acknowledged that senior leadership was generally supportive of initiatives to improve the food environment, this was only 1 of many priorities, so leadership was usually not briefed on progress. Ensuring that there are clear feedback mechanisms to share progress made (or not) to senior leadership during such interventions may be important for creating a level of accountability for implementation leads and for overall sustainability of the initiative.
Limitations
Although this study adds to the evidence base on effective community-level sodium-reduction initiatives, there was no control group, which calls into question whether the effects observed were from the intervention or a reflection of secular trends. Although action plans and interviews that documented sites’ goals and activities provide evidence that intentional changes were made to produce the results found, it is important to acknowledge the broader environment that may have influenced the success of the initiative.5,8
Major food manufacturers have made public commitments to reduce sodium in their portfolios.31–33 Although these organizations do produce many prepackaged snack foods, the degree to which their sodium standards had an impact on the products in our study is not clear.31,32 A review of the National Salt Reduction Initiative from 2009 to 2014 found that sales-weighted mean sodium density declined significantly in the snack category, and though there was an increase in percentage of snack products meeting National Salt Reduction Initiative targets, it was fairly low overall.34 Another study examined the sodium content in a sample of 451 processed and restaurant foods from 2005 to 2015, and found a reduction in sodium of 4% over a 10-year period.35 Though only a few of the items in that analysis overlap with the prepackaged items in our study, this collection of evidence indicates that there may be some general trends toward lowering of sodium in the food supply.
The reductions observed in our study, a 7.5-percentage-point decrease, or 26% overall decrease, in the percentage of products exceeding 200 milligrams of sodium per serving are over a 1- to 1.5-year period, by contrast with the 5- and 10-year horizons described previously. In this study, there was a significant 19-milligram reduction in sodium per item (95% confidence interval = 13.57, 24.54; P < .001)—representing an overall 12% decrease in mean sodium from 154 milligrams at baseline to 135 milligrams at follow-up.
Another limitation is that we only examined changes in availability of higher-sodium products, and did not include any information on sales or consumption behaviors, which would be a more ideal marker of intervention effectiveness toward reducing sodium intake. However, evidence on vending changes has shown that increasing the availability of healthier options can lead to increased sales of these items.13,22,23 Finally, this intervention strategy was part of the REACH project aimed to reduce racial/ethnic disparities in hypertension. Though sites were selected to reach specific neighborhoods, we are uncertain of who will benefit most from these efforts. Understanding the impact of policy and environmental strategies on vulnerable populations is critical in ensuring such efforts do not unintentionally widen existing disparities.
Public Health Implications
Hypertension affects both quality of life and health care costs. While reducing sodium in the food supply is an ideal strategy to reduce population intake of sodium, community-level interventions may be important to help drive changes by food manufacturers. We present findings on the effectiveness of a sodium intervention that included goal setting and tailored technical assistance in reducing the percentage of higher-sodium prepackaged products in diverse community institutions. Future research should consider sales and consumption implications of introducing lower-sodium products, as well as who benefits from such initiatives.
ACKNOWLEDGMENTS
C. J. Brooks was supported by the Harvard T. H. Chan School of Public Health, Cardiovascular Disease Epidemiology Training Program in Behavior, the Environment, and Global Health (grant T32 HL098048); J. Barrett, J. Daly, R. Lee, N. Blanding, A. McHugh, and S. Gortmaker were supported by the US Centers for Disease Control and Prevention Racial and Ethnic Approaches to Community Health Demonstration Project Cooperative Agreement (1U58DP004726-01) with the Boston Public Health Commission; D. Williams is supported by the Harvard T. H. Chan School of Public Health.
We thank all participating organizations and partners for their contribution to this intervention and research.
HUMAN PARTICIPANT PROTECTION
No human participants were involved in this study. The research was part of a larger project approved by the Harvard T. H. Chan School of Public Health institutional review board.
Footnotes
See Galea and Vaughan, p. 1867.
REFERENCES
- 1.2015–2020 Dietary Guidelines for Americans. 8th ed. Washington, DC: US Department of Health and Human Services, US Department of Agriculture; 2015. [Google Scholar]
- 2.He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev. 2013;(4):CD004937. doi: 10.1002/14651858.CD004937.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin EJ, Go AS et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 4.Yoon S, Fryar C, Carroll M. Atlanta, GA: National Center for Health Statistics; 2015. Hypertension prevalence and control among adults, United States, 2011–2014. NCHS Data Brief no. 220. [Google Scholar]
- 5.Institute of Medicine. Strategies to Reduce Sodium Intake in the United States. Washington, DC: The National Academies Press; 2010. [Google Scholar]
- 6.Harnack LJ, Cogswell ME, Shikany JM et al. Sources of sodium in US adults from 3 geographic regions. Circulation. 2017;135(19):1775–1783. doi: 10.1161/CIRCULATIONAHA.116.024446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quader ZS, Zhao L, Gillespie C et al. Sodium intake among persons aged ≥2 years—United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2017;66(12):324–328. doi: 10.15585/mmwr.mm6612a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Food and Drug Administration. Draft guidance for industry: voluntary sodium reduction goals: target mean and upper bound concentrations for sodium in commercially processed, packaged, and prepared foods. Available at: http://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/ucm494732.htm. Accessed September 8, 2016.
- 9.Mugavero K, Losby JL, Gunn JP, Levings JL, Lane RI. Reducing sodium intake at the community level: the sodium reduction in communities program. Prev Chronic Dis. 2012;9:E168. doi: 10.5888/pcd9.120081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffman JA, Rosenfeld L, Schmidt N et al. Implementation of competitive food and beverage standards in a sample of Massachusetts schools: the NOURISH Study (Nutrition Opportunities to Understand Reforms Involving Student Health) J Acad Nutr Diet. 2015;115(8):1299–1307.e2. doi: 10.1016/j.jand.2015.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.French SA, Story M, Fulkerson JA, Gerlach AF. Food environment in secondary schools: a la carte, vending machines, and food policies and practices. Am J Public Health. 2003;93(7):1161–1167. doi: 10.2105/ajph.93.7.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greves HM, Rivara FP. Report card on school snack food policies among the United States’ largest school districts in 2004–2005: room for improvement. Int J Behav Nutr Phys Act. 2006;3:1. doi: 10.1186/1479-5868-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grech A, Allman-Farinelli M. A systematic literature review of nutrition interventions in vending machines that encourage consumers to make healthier choices. Obes Rev. 2015;16(12):1030–1041. doi: 10.1111/obr.12311. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Under Pressure: Strategies for Sodium Reduction in the Hospital Environment. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion; 2011. [Google Scholar]
- 15.Naylor PJ, Olstad DL, Therrien S. An intervention to enhance the food environment in public recreation and sport settings: a natural experiment in British Columbia, Canada. Child Obes. 2015;11(4):364–374. doi: 10.1089/chi.2014.0148. [DOI] [PubMed] [Google Scholar]
- 16.Lawrence S, Boyle M, Craypo L, Samuels S. The food and beverage vending environment in health care facilities participating in the healthy eating, active communities program. Pediatrics. 2009;123(suppl 5):S287–S292. doi: 10.1542/peds.2008-2780G. [DOI] [PubMed] [Google Scholar]
- 17.A Call to Action: Creating a Culture of Health. Chicago, IL: American Hospital Association; 2011. [Google Scholar]
- 18.Refermat E. Annual Report State of the Industry. Automatic Merchandiser. Available at: http://media.cygnus.com/files/base/AUTM/document/2015/06/2015_State_of_the_Vending_Industry.pdf. Accessed October 6, 2016.
- 19.Derrick JW, Bellini SG, Spelman J. Using the Hospital Nutrition Environment Scan to evaluate health initiative in hospital cafeterias. J Acad Nutr Diet. 2015;115(11):1855–1860. doi: 10.1016/j.jand.2015.06.378. [DOI] [PubMed] [Google Scholar]
- 20.Winston CP, Sallis JF, Swartz MD, Hoelscher DM, Peskin MF. Consumer nutrition environments of hospitals: an exploratory analysis using the Hospital Nutrition Environment Scan for Cafeterias, Vending Machines, and Gift Shops, 2012. Prev Chronic Dis. 2013;10:E110. doi: 10.5888/pcd10.120335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naylor PJ, Bridgewater L, Purcell M, Ostry A, Wekken SV. Publically funded recreation facilities: obesogenic environments for children and families? Int J Environ Res Public Health. 2010;7(5):2208–2221. doi: 10.3390/ijerph7052208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olstad DL, Goonewardene LA, McCargar LJ, Raine KD. If we offer it, will children buy it? Sales of healthy foods mirrored their availability in a community sport, commercial setting in Alberta, Canada. Child Obes. 2015;11(2):156–164. doi: 10.1089/chi.2014.0131. [DOI] [PubMed] [Google Scholar]
- 23.Roy R, Kelly B, Rangan A, Allman-Farinelli M. Food environment interventions to improve the dietary behavior of young adults in tertiary education settings: a systematic literature review. J Acad Nutr Diet. 2015;115(10):1647–1681.e1. doi: 10.1016/j.jand.2015.06.380. [DOI] [PubMed] [Google Scholar]
- 24.US Department of Agriculture. USDA food composition databases. Available at: https://ndb.nal.usda.gov/ndb. Accessed June 1, 2016.
- 25.Massachusetts Department of Health and Human Services. Massachusetts School nutrition standards for competitive foods and beverages. 2014. Available at: http://www.mass.gov/eohhs/docs/dph/mass-in-motion/school-nutrition-glance.pdf. Accessed September 8, 2016.
- 26.US Department of Agriculture. What we eat in America food categories. Available at: https://www.ars.usda.gov/northeast-area/beltsville-md/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/dmr-food-categories. Accessed June 1, 2016.
- 27.Trieu K, McLean R, Johnson C et al. The science of salt: a regularly updated systematic review of the implementation of salt reduction interventions (November 2015 to February 2016) J Clin Hypertens (Greenwich) 2016;18(12):1194–1204. doi: 10.1111/jch.12909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moran A, Krepp EM, Johnson Curtis C, Lederer A. An intervention to increase availability of healthy foods and beverages in New York City hospitals: the Healthy Hospital Food Initiative, 2010–2014. Prev Chronic Dis. 2016;13:E77. doi: 10.5888/pcd13.150541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bell C, Pond N, Davies L, Francis JL, Campbell E, Wiggers J. Healthier choices in an Australian health service: a pre–post audit of an intervention to improve the nutritional value of foods and drinks in vending machines and food outlets. BMC Health Serv Res. 2013;13:492. doi: 10.1186/1472-6963-13-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miller J, Lee A, Obersky N, Edwards R. Implementation of A Better Choice Healthy Food and Drink Supply Strategy for staff and visitors in government-owned health facilities in Queensland, Australia. Public Health Nutr. 2015;18(9):1602–1609. doi: 10.1017/S1368980013003455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tahiri M. Our promise to lower sodium. General Mills. 2015. Available at: http://www.blog.generalmills.com/2015/12/our-promise-to-lower-sodium-2. Accessed October 18, 2016.
- 32.American Heart Association. Food giant Mars to lower sodium, urges FDA to issue guidelines. 2016. Available at: http://news.heart.org/food-giant-mars-to-lower-sodium-urges-fda-to-issue-guidelines. Accessed October 18, 2016.
- 33. Nestlé. Nestlé policy on sodium (salt). 2017. Available at: https://www.nestle.com/asset-library/documents/library/documents/about_us/nestle-policy-salt.pdf. Accessed October 18, 2016.
- 34.Curtis CJ, Clapp J, Niederman SA, Ng SW, Angell SY. US food industry progress during the national salt reduction initiative: 2009–2014. Am J Public Health. 2016;106(10):1815–1819. doi: 10.2105/AJPH.2016.303397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jacobson M. Salt Assault: Brand-Name Comparisons of Processed Foods. 4th ed. Washington, DC: Center for Science in the Public Interest; 2016. [Google Scholar]