Abstract
Objectives. To determine the effectiveness of a universal school-based depression education program.
Methods. In 2012–2015, we matched 6679 students from 66 secondary schools into pairs by state (Maryland, Delaware, Pennsylvania, Michigan, and Oklahoma) and randomized to the Adolescent Depression Awareness Program (ADAP; n = 3681) or to a waitlist control condition (n = 2998). Trained teachers delivered ADAP as part of the health education curriculum to students aged 14 to 15 years. The primary outcome was depression literacy. Secondary outcomes included mental health stigma and, in a subset of the sample, the receipt of mental health services. Follow-up was at 4 months.
Results. ADAP resulted in significantly higher levels of depression literacy among participating students than did waitlist controls, after adjusting for pretest assessment depression literacy (P < .001). Overall, ADAP did not significantly affect stigma (P = .1). After ADAP, students approached 46% of teachers with concerns about themselves or others. Of students who reported the need for depression treatment, 44% received treatment within 4 months of ADAP implementation.
Conclusions. ADAP is an effective public health intervention for improving depression literacy among students.
Trial Registration. Clinicaltrials.gov NCT02099305
Depression is prevalent, often disabling, and sometimes lethal, generating 10% to 11% of all medical burden and disabilities worldwide.1,2 In the United States in 2015, 12.5% of youths aged 12 to 17 (3 million adolescents) experienced at least 1 major depressive episode in the past year, and only 39% received treatment for depression.3
The risk of depression increases as children become adolescents.4 The onset of depression during adolescence is associated with poor academic performance, family and social dysfunction, poor physical health, substance use disorders, unemployment, early parenthood, and suicide.4–11 Adolescent depression has substantial continuity into adulthood, with impaired functioning in work, social, and family life5,6 and increased risk of depression and substance dependence in adulthood.7,9 These difficulties are also often evident in adolescents with subclinical levels of depression.12
Because depressive disorders are common, can be treated, and may begin early in life, the greatest opportunity for prevention is among young people.13 Compas et al.14 suggest conducting programs in early adolescence to precede the beginning of increased incidence. This approach shifts the focus to early identification, rather than waiting until depression is well established, has done considerable harm, or is potentially more difficult to treat.
Gulliver et al.15 found that poor mental health literacy is a key barrier preventing adolescents from seeking mental health treatment. Mental health literacy is defined by Jorm as “knowledge and beliefs about mental disorders which aid their recognition, management or prevention.”16(p182) Initiatives to increase mental health literacy have been linked with help seeking.17 Schools are an optimal setting to reach large populations of adolescents and are the place where most youths receive mental health treatment when they are treated.18,19 Previous research has advocated that mental health literacy be embedded within large-scale, universal school interventions as an essential strategy for early recognition of symptoms, the reduction of stigma, and improved adolescent help-seeking behaviors.17,20,21
The Adolescent Depression Awareness Program (ADAP) is a universal school-based depression education program developed in 1999 to increase depression literacy as the first step in encouraging depressed youths to seek treatment. ADAP delivers the core message that depression and bipolar disorder are treatable medical illnesses and that concerned individuals should seek help. ADAP is intended to be embedded in the standard high school health education curriculum and taught by trained school health education teachers over the course of two 90-minute or three 45- to 60-minute class periods. In a 1-group pre–post design study, students who received ADAP had a statistically significant increase in depression knowledge 6 weeks after ADAP implementation.22 Support for ADAP’s effectiveness was also found in a nonrandomized controlled study with students who received the ADAP intervention, compared with students who did not, showing a statistically significant increase in depression knowledge.23
Our aims were (1) to assess the effectiveness of ADAP in increasing depression literacy compared with the standard health education curriculum; (2) to assess the sustainability of depression literacy changes with a follow-up posttest conducted 4 months after ADAP; and (3) to assess whether the ADAP intervention had an influence on self-reported receipt of mental health treatment 4 months after ADAP compared with the standard health curriculum.
METHODS
We carried out our evaluation of ADAP using a school-based randomized effectiveness trial with a waitlist control design. Within region, we matched schools on school characteristics (community type [rural, urban, suburban], school type [public, private, charter, vocational, etc.], number of students, number of teaching faculty) and student characteristics (gender, race/ethnicity, proportion with free or reduced cost meals, median household income, average days absent, average total SAT scores, percentage who attend 2- and 4-year colleges). After matching schools into similar pairs within each region, we randomized 1 school in each pair to receive ADAP in year 1 and the other to receive ADAP in year 2. Schools who received ADAP in year 2 served as the control group for the schools who received ADAP in year 1. ADAP was not removed from schools after implementation.
Health education is a standard part of the high school curriculum required for graduation. In the participating schools, the ADAP intervention was added to the existing health education curriculum. The pretest was administered before starting the ADAP intervention, and the posttest was given 6 weeks after the intervention. Four months after the ADAP intervention, another posttest was administered to assess the sustainability of improvements in depression literacy and mental health stigma (defined as stigma regarding individuals with mental health problems). Students in the waitlist control condition were given the same assessments as the intervention schools.
In year 1, teachers from schools assigned to receive ADAP in year 1 attended instructor training. Teachers consented and completed knowledge and stigma measures at the start of the training day. The intervention schools implemented the ADAP curriculum in their classrooms (3 hours total given in 2–3 class periods). Trained teachers were encouraged to teach ADAP immediately after instructor training, but implementation timelines varied. Some schools taught health over the course of a full academic year, so they may have been trained in the fall and implemented ADAP in the spring semester. Schools randomized to year 2 had teacher training and implemented ADAP in the next academic year.
Because ADAP was implemented as part of the routine health curriculum as approved by the superintendents of the participating schools, parental consent was not required. In accordance with the program’s institutional review board exemption status, the pre-, post-, and follow-up tests were conducted for evaluative purposes. Teachers matched tests using a sign-in sheet with a prepopulated numeric identification number for each student that was destroyed after the follow-up tests were administered. Teachers provided informed consent because data were collected about their experiences teaching ADAP.
A total of 6679 high school students from 54 high schools in Maryland, Delaware, Pennsylvania, Michigan, and Oklahoma participated. School systems that agreed to the terms of the project, including randomization and data collection, were eligible to participate. Only 1 teacher in 1 of the schools selected for this project had previously received training on the ADAP intervention. We invited all 20 high schools within the Archdiocese of Baltimore to participate as well as 30 in New Castle County, Delaware; 5 in Adair County, Oklahoma; 8 in Washtenaw County, Michigan; and 28 in York County, Pennsylvania. Not all schools approached agreed to participate. Overall, 66 of 91 (75%) schools approached agreed to participate and 6 of the 66 schools dropped out of the study during the trial and therefore did not provide data.
In a subset of schools (in York County, PA), after receiving a complete description of the study, we obtained parental consent and adolescent assent for adolescents to participate in an online survey 4 months after the ADAP intervention about the receipt of mental health services. All teachers who taught ADAP participated in an online survey that asked about their experiences with ADAP.
The Adolescent Depression Awareness Program
ADAP is a school-based depression education program that educates high school students, teachers, counselors, and parents about adolescent depression. The curriculum is 3 hours long and is designed to be taught in 2 or 3 consecutive health classes. Multiple teaching modalities are employed with interactive lectures, videos, film assignments, homework, and group activities to reinforce key concepts. The curriculum is included in the standard teaching kit provided to all trained ADAP instructors. The kit also includes a detailed instructor’s manual and DVDs showing the curriculum being taught as well as all the materials needed to implement the ADAP curriculum (curriculum overheads or PowerPoint presentations, films, handouts, and group activity cards).
ADAP is delivered entirely by school personnel (usually trained health education teachers) as part of the standard high school health education curriculum (usually in 9th or 10th grade classes). It addresses knowledge about mood disorders as well as attitudes about treatment. The primary goal is to increase depression literacy. The core components include the following:
identifying symptoms of depression,
understanding the process of medical decision-making,
seeing parallels between depression and other medical illnesses,
recognizing suicide as a potential consequence of depression, and
understanding that depression is a treatable medical illness.
ADAP focuses on increasing depression literacy as the first step in encouraging youths to seek treatment.
Training
The ADAP instructor training includes an in-person training session (6 hours in length). The content of the in-person training includes the following:
education about the prevalence, diagnosis, and treatment of mood disorders in adolescence,
a review of ADAP’s development and rationale,
a parent’s perspective on adolescent depression,
first-person descriptions by adults whose mood disorders began in adolescence about the experience of living with a mood disorder, and
a detailed review of the ADAP curriculum content to supplement the training manual and DVDs.
Teachers received 6 hours of continuing education units for the training session. In addition to the resources available in their kit, refresher sessions were offered to teachers via online ADAP training modules located on the ADAP Web site.
Our team offered to conduct a 90- to 120-minute open community forum on adolescent depression the evening before the full-day training for the school-based professionals in each community. This session included a presentation on adolescent mood disorders by ADAP’s director (a psychiatrist who specializes in mood disorders) as well as time for questions from community members and parents. Although all schools were offered parent nights, only 2 Maryland schools and 3 Oklahoma schools held parent nights. No parent nights were held in Delaware, Pennsylvania, or Michigan. Few parents and some teachers, administrators, and tribal leaders attended. Because so few parents participated, it is highly unlikely that these sessions influenced the results.
Study Outcome Assessments
The Adolescent Depression Knowledge Questionnaire (ADKQ)22 was developed to assess students’ knowledge about depression and help-seeking attitudes about the illness. Psychometric evidence supports the ADKQ as a measure to evaluate adolescent depression literacy from pre- to posttest and within several groups of interest (e.g., gender, facilitator).24 The questionnaire asks students to answer 13 yes or no questions to assess depression literacy and assess in 4 clinical vignettes whether each individual portrayed in the vignette “is having a rough time,” “has the medical illness of depression,” or “has the medical illness of bipolar disorder.” We defined depression literacy as correctly answering 80% or more of the 17 knowledge-based questions on the ADKQ. The ADKQ was administered to students on the first day of the curriculum as a pretest, 6 weeks postintervention, and 4 months postintervention.
A version of the Reported and Intended Behavior Scale (RIBS)25 modified with permission from the original author for use with adolescents was used. The RIBS is an 8-item tool that measures experiences and views in relation to people who have mental health problems. We used the RIBS to measure the effect of the intervention on students’ perceptions about people with mental illness. We coded mental health stigma as a binary variable whereby we categorized those with a RIBS score of 16 or higher as having high mental health stigma. We used this cutoff to make this outcome similar to the depression literacy outcome. Students self-administered the RIBS on the first day of the curriculum as a pretest, 6 weeks postintervention, and 4 months postintervention.
Among students in schools in York County, Pennsylvania, we assessed ADAP’s effect on the receipt of mental health services for depression and other conditions 4 months after ADAP was implemented among adolescents with parental consent. A modified version of the Child and Adolescent Services Assessment26–28 instrument was self-administered. Questions were also included on whether they received treatment for depression or another emotional problem after the ADAP intervention (e.g., “Did you seek help for depression or another emotional concern after the ADAP program?”) and whether a family member had ever been diagnosed with depression. Adolescents were also asked about their perceived need for depression treatment (e.g., “In the past 4 months, do you think you needed help for depression?”).
Teachers were asked to participate in an online survey after they taught the ADAP curriculum, which had questions about their experiences with the ADAP intervention, including whether students self-identified after they implemented ADAP.
Statistical Analyses
We used multilevel models29–32 to evaluate the impact of ADAP and to accommodate the hierarchical structure of the data. We estimated adjusted odds ratios (AORs), and 95% confidence intervals (CIs) using individual student-level data matching pre-, post-, and follow-up test results while taking into account the hierarchical and clustered structure of the data, with students clustered by school and within region. To explore the intervention impact on depression literacy and mental health stigma, we employed a linear mixed-effects model using the lme4 package in R33,34 with school as a random effect. We included gender and the school-level characteristics used for randomization as covariates.
Overall, there were no significant differences in loss to follow-up by gender in the postassessment (P = .47) and 4-month follow-up (P = .26). However, those who had achieved depression literacy were more likely to participate in the postassessment (P < .001) and 4-month follow-up (P < .001). With respect to the intervention arm, there were no significant differences in loss to follow-up by gender in the postassessment (P = .30), but girls were more likely to participate in the 4-month follow-up (P < .001). In the intervention arm, those who had achieved depression literacy were more likely to participate in the postassessment (P = .002) and in the 4-month follow-up (P = .08), though the latter finding did not achieve statistical significance.
To handle missing data, we calculated inverse probability weights. Inverse probability weighting provides a methodology for handing missing data when imputation is not preferred and list-wise deletion could introduce bias. We included intervention status, preassessments, school-level variables, state, and school in the equation used to create the inverse probability weights.
RESULTS
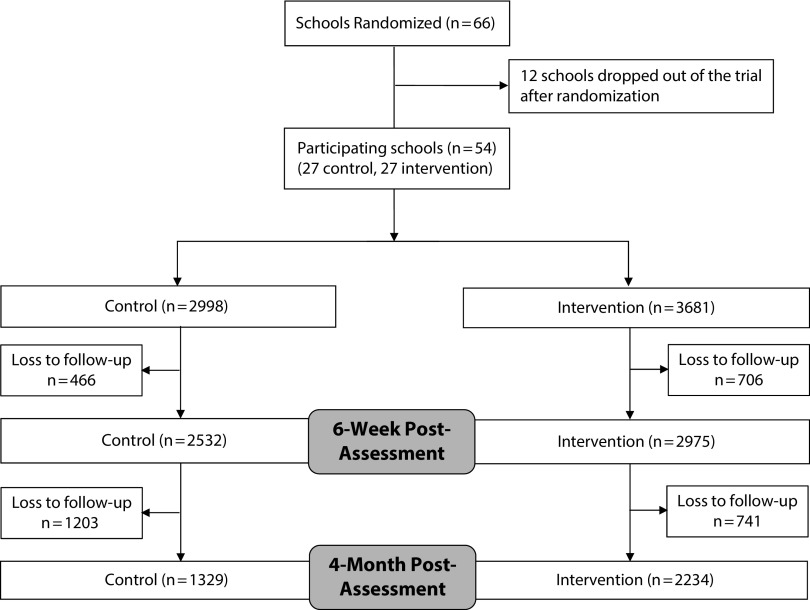
The consort table illustrates the progress through the phases of the study through enrollment, intervention allocation, and follow-up (Figure 1). Six schools were unable to follow study procedures and withdrew. We had to drop their matched-pair schools from the analysis. To test whether there were intervention and control group differences after randomization for the full sample and within each region, we analyzed differences between groups by gender and ADKQ pretest rates of depression literacy. In the Michigan only sample, there were significant differences by gender (P = .03); otherwise, there were no differences between the ADAP and control groups.
FIGURE 1—
Consolidated Standards of Reporting Trials (Consort) Flow Diagram Displaying the Progress of Participants Through the Trial: Randomized, School-based Effectiveness Trial of the Adolescent Depression Awareness Program (ADAP), 5 US States, 2012–2015
Note. The states studied were Maryland, Delaware, Michigan, Oklahoma, and Pennsylvania.
Depression Literacy and Mental Health Stigma
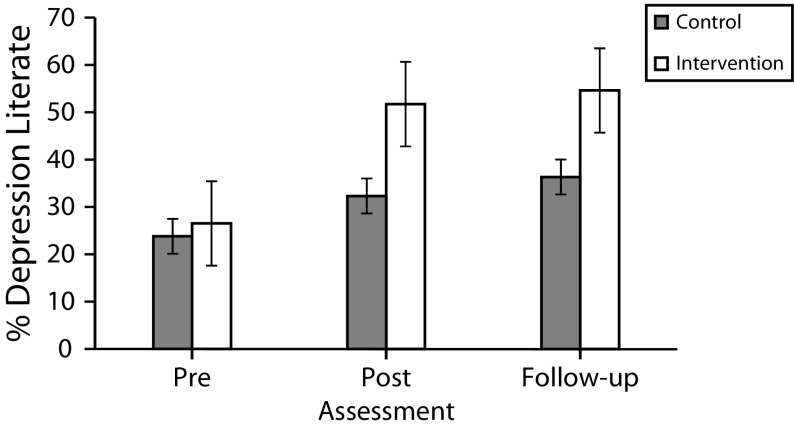
Intervention status was a significant predictor of depression literacy at the 6-week postassessment, controlling for depression literacy at the preassessment (ΑOR = 3.1; P < .001; 95% CI = 2.0, 5.0): those who received the ADAP intervention were more likely to be depression literate at the postassessment. Gender was also a significant predictor (ΑOR = 1.5; P < .001; 95% CI = 1.3, 1.6): girls were more likely to be depression literate at the postassessment than were boys. The intervention’s impact on the 4-month follow-up assessment was also explored in a linear mixed-effects model. Intervention status significantly predicted depression literacy at the 4-month follow-up assessment (ΑOR = 3.3; P < .001; 95% CI = 2.2, 5.0), while controlling for depression literacy at the preassessment (Table 1; Figure 2).
TABLE 1—
Proportion of Students with Depression Literacy and High Mental Health Stigma in the Intervention and Control Groups at Each Study Time Point: Randomized, School-Based Effectiveness Trial of the Adolescent Depression Awareness Program (ADAP), 5 US States, 2012–2015
| Variable | ADAP, % | Control, % | AOR (95% CI) |
| Male | 49.9 | 48.4 | |
| Depression literacy | |||
| Preassessment (n = 6679) | 26.5 | 23.8 | |
| Postassessment (n = 5507) | 51.7 | 32.3 | 3.10 (2.0, 5.0) |
| Follow-up assessment (n = 3563) | 54.6 | 36.3 | 3.30 (2.2, 5.0) |
| High mental health stigma | |||
| Preassessment (n = 6679) | 4.4 | 4.4 | |
| Postassessment (n = 5507) | 3.3 | 4.0 | 0.50 (0.2, 1.2) |
| Follow-up assessment (n = 3563) | 3.5 | 4.0 | 1.22 (0.5, 3.0) |
Note. AOR = adjusted odds ratio; CI = confidence interval. The χ2 test showed no significant difference in gender between ADAP and control (χ2 = 1.63, df = 1; P = .201). The states studied were Maryland, Delaware, Michigan, Oklahoma, and Pennsylvania.
FIGURE 2—
Proportions Depression Literate Among Students Who Received the Adolescent Depression Awareness Program (ADAP) Intervention and Control Students at Pretest, Posttest, and Follow-up Assessment: Randomized, School-Based Effectiveness Trial of ADAP, 5 US States, 2012–2015
Note. Posttest was 6 weeks after ADAP; follow-up assessment was 4 months after ADAP implementation. The states studied were Maryland, Delaware, Michigan, Oklahoma, and Pennsylvania.
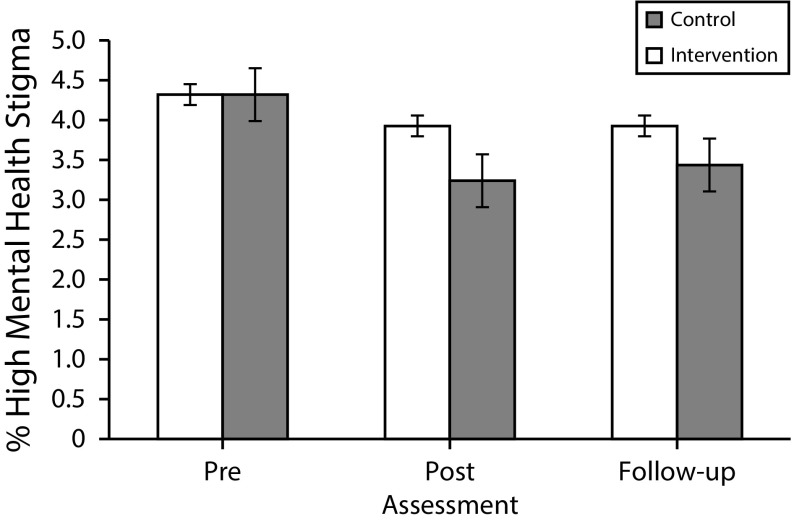
The ADAP intervention did not show a significant effect on postintervention stigma while controlling for preintervention stigma (ΑΟR = 0.5; P = .1; 95% CI = 0.2, 1.2). Gender was a significant predictor of postintervention mental health stigma (AOR = 0.5; P = .001; 95% CI = 0.3, 0.7): girls were less likely to have high mental health stigma at the postassessment. Similar results were found for the 4-month follow-up, with no significant impact of intervention on follow-up mental health stigma (ΑΟR = 1.2; P = .7; 95% CI = 0.5, 3.0; Figure 3).
FIGURE 3—
Proportions With High Mental Health Stigma Among Students Who Received the Adolescent Depression Awareness Program (ADAP) Intervention and Control Students at Pretest, Posttest, and Follow-up Assessment: Randomized, School-Based Effectiveness Trial of ADAP, 5 US States, 2012–2015
Note. Posttest was 6 weeks after ADAP; follow-up assessment was 4 months after ADAP implementation. The states studied were Maryland, Delaware, Michigan, Oklahoma, and Pennsylvania.
Online Surveys
Consent forms were distributed to 1427 families and received from 481 parents (34%), and 201 adolescents with parental consent (42%) completed the survey. Of those who completed the survey, 64% were girls, 55% were in 10th grade (mean age: 15.8 years), 77% self-reported White race, 13% had ever been diagnosed with depression, and 16% reported that they had sought help for depression or another emotional concern after the ADAP program.
Of those who completed the survey, 42% had a family member diagnosed with depression. When asked about their perceived need for depression treatment, 38 (19%) said they needed help, and, of these, 44% obtained services for depression after ADAP.
Teachers were given an online survey about their experiences with ADAP. Of those approached, 75% (65 of 87 teachers) completed the survey. In response to “Did students self-identify after ADAP (or approach you on behalf of a friend)?” 46% (30 of 65 total respondents) said that at least 1 student self-identified or approached them on behalf of a friend.
DISCUSSION
To our knowledge, this was the first universal randomized controlled effectiveness trial to increase depression literacy. The results show that ADAP, a short school-based intervention (3 hours over the course of 2 or 3 course periods), significantly increased depression literacy in both boys and girls. ADAP did not have an effect on mental health stigma. The RIBS mental health stigma measure had a limited range, with less than 4.5% of the sample having high stigma at preassessment. It could be that our sample did not have enough range to detect any impact of ADAP on mental health stigma. It could also be that, to have an effect on stigma reduction, interventions must go beyond education.
The finding that students approached 46% of teachers with concerns about themselves or others after ADAP implementation indicates that teachers who implement ADAP should be prepared to link students with school mental health professionals. Of those who reported the need for depression treatment, 44% received treatment within 4 months of ADAP implementation.
Limitations and Strengths
Several study limitations should be acknowledged. After randomization, 6 schools were unable to follow study procedures and withdrew. We had to drop their 6 matched-pair schools from the analysis. There was considerable attrition during the 4-month follow-up because many schools had quarter-based marking periods; thus, students were disbursed to new classes after 8 weeks. The school regions we included are not broadly generalizable to schools throughout the United States. The receipt of mental health treatment after ADAP was assessed in only 1 region (York County, PA); the results of the student survey were uncontrolled and could not be directly linked with their depression literacy and mental health stigma measures because parental consent was waived for the school-based components of the study. Collecting identifiers requires parental consent; this likely would have resulted in reduced student participation and a much smaller and less generalizable sample. Of those who completed the online survey, 42% reported a family member diagnosed with depression, which could indicate differential participation among a sample enriched for depression.
This study also has a number of notable strengths. Foremost are the trial’s large sample size and the random allocation of schools to the intervention and waitlist control condition. Teachers implemented ADAP as part of the standard health education curriculum, which does not compete for academic time and encourages sustainability. Interventions administered by mental health professionals are likely to be less scalable to widespread use in school settings. Delivery at schools within the school day ensures access to the program for the majority of youths.35 The intervention is also practical, easy to implement, unobtrusive (it fits into the current health education curriculum), ready to use, highly relevant, and well received by schools. The participating schools are diverse, with broad ethnic representation and diversity by low-income status (percentage free lunch status), type of school (public, private, parochial, charter, alternative), school size, location (urban, rural, suburban), and mental health services available within schools. Five schools with large proportions of Native American students (40%–100%) in Adair County, Oklahoma, participated in this trial. We did not adapt the intervention for these schools, but ADAP seemed to have high relevance and applicability.
Conclusions
Adding ADAP to the standard high school health education curriculum implemented by health education teachers in 54 schools in multiple states resulted in significantly higher levels of student depression literacy. In addition, 46% of teachers reported that at least 1 student self-identified as needing depression treatment after ADAP implementation. Universal programs such as ADAP avoid stigmatizing targeted groups and have the potential to benefit large numbers of recipients who may not be symptomatic at the time of the intervention but could be in the future. There is untapped potential for embedding evidence-based interventions into health education class. The evaluation of programs under such conditions is important in determining the program’s long-term dissemination and sustainability potential.35 Future directions of ADAP include adaptation for younger students.
ACKNOWLEDGMENTS
This work was funded by the National Institute of Mental Health (grants R01MH095855 to H. C. W. and K23MH090246 to L. M.). G. Thornicroft is supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London at King’s College London Foundation Trust; the Department of Health via the (NIHR) Biomedical Research Centre and Dementia Unit awarded to South London and Maudsley National Health Service (NHS) Foundation Trust in partnership with King’s College London and King’s College Hospital NHS Foundation Trust; and the European Union Seventh Framework Programme (grant FP7/2007-2013) Emerald project.
In the past 36 months, L. Townsend’s spouse has received research support, acted as a consultant, or served on a speaker’s bureau for Actavis, Akili, Alcobra, Amerex, American Academy of Child & Adolescent Psychiatry, American Psychiatric Press, Bracket, CogCubed, Cognition Group, Coronado Biosciences, Elsevier, Epharma Solutions, Forest, Genentech, GlaxoSmithKline, Guilford Press, Ironshore, Johns Hopkins University Press, KemPharm, Lundbeck, Medgenics, Merck, NIH, Neurim, Novartis, Otsuka, PCORI, Pfizer, Physicians Postgraduate Press, Purdue, Rhodes Pharmaceuticals, Roche, Sage, Shire, Sunovion, Supernus Pharmaceuticals, Syneurx, Takeda, Teva, TouchPoint, Tris, Validus, and WebMD.
Note. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
HUMAN PARTICIPANT PROTECTION
The Johns Hopkins School of Medicine institutional review board approved this study.
REFERENCES
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9525):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
- 4.Nock MK, Green JG, Hwang I et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cicchetti D, Toth SL. The development of depression in children and adolescents. Am Psychol. 1998;53:221–241. doi: 10.1037//0003-066x.53.2.221. [DOI] [PubMed] [Google Scholar]
- 6.Bayer JK, Sanson AV. Preventing the development of emotional mental health problems from early childhood: recent advances in the field. Int J Ment Health Promot. 2003;5(3):4–16. [Google Scholar]
- 7.Merry S, McDowell H, Wild CJ, Bir J, Cunliffe R. A randomized placebo-controlled trial of a school-based depression prevention program. J Am Acad Child Adolesc Psychiatry. 2004;43(5):538–547. doi: 10.1097/00004583-200405000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002;59(3):225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 9.McGorry PD, Purcell R, Hickie IB, Jorm AF. Investing in youth mental health is a best buy. Med J Aust. 2007;187(7, suppl):S5–S7. doi: 10.5694/j.1326-5377.2007.tb01335.x. [DOI] [PubMed] [Google Scholar]
- 10.Cairns KE, Yap MBH, Pilkington PD, Jorm AF. Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2014;169:61–75. doi: 10.1016/j.jad.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Auerbach RP, Millner AJ, Stewart JG, Esposito EC. Identifying differences between depressed adolescent suicide ideators and attempters. J Affect Disord. 2015;186:127–133. doi: 10.1016/j.jad.2015.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gotlib IH, Lewinsohn PM, Seeley JR. Symptoms versus a diagnosis of depression: differences in psychosocial functioning. J Consult Clin Psychol. 1995;63(1):90–100. doi: 10.1037//0022-006x.63.1.90. [DOI] [PubMed] [Google Scholar]
- 13.March J, Silva S, Curry J et al. The Treatment for Adolescents with Depression Study (TADS): outcomes over 1 year of naturalistic follow-up. Am J Psychiatry. 2009;166(10):1141–1149. doi: 10.1176/appi.ajp.2009.08111620. [DOI] [PubMed] [Google Scholar]
- 14.Compas BE, Oppedisano G, Connor JK et al. Gender differences in depressive symptoms in adolescence: comparison of national samples of clinically referred and nonreferred youths. J Consult Clin Psychol. 1997;65(4):617–626. doi: 10.1037//0022-006x.65.4.617. [DOI] [PubMed] [Google Scholar]
- 15.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. “Mental health literacy”: a survey of the public’s ability to recognize mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. 1997;166(4):182. doi: 10.5694/j.1326-5377.1997.tb140071.x. [DOI] [PubMed] [Google Scholar]
- 17.Rüsch N, Evans-Lacko SE, Henderson C, Flach C, Thornicroft G. Knowledge and attitudes as predictors of intentions to seek help for and disclose a mental illness. Psychiatr Serv. 2011;62(6):675–678. doi: 10.1176/ps.62.6.pss6206_0675. [DOI] [PubMed] [Google Scholar]
- 18.Wilson CJ, Deane FP, Marshall KL, Dalley A. Reducing adolescents’ perceived barriers to treatment and increasing help-seeking intentions: effects of classroom presentations by general practitioners. J Youth Adolesc. 2008;37(10):1257–1269. [Google Scholar]
- 19.Chisholm KE, Patterson P, Torgerson C, Turner E, Birchwood M. A randomised controlled feasibility trial for an educational school-based mental health intervention: study protocol. BMC Psychiatry. 2012;12:23. doi: 10.1186/1471-244X-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skre I, Friborg O, Breivik C, Johnsen LI, Arnesen Y, Wang CEA. A school intervention for mental health literacy in adolescents: effects of a non-randomized cluster controlled trial. BMC Public Health. 2013;13:873. doi: 10.1186/1471-2458-13-873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust. 2007;187(7 suppl):S26–S30. doi: 10.5694/j.1326-5377.2007.tb01332.x. [DOI] [PubMed] [Google Scholar]
- 22.Swartz KL, Kastelic EA, Hess SG et al. The effectiveness of a school-based adolescent depression education program. Health Educ Behav. 2010;37(1):11–22. doi: 10.1177/1090198107303313. [DOI] [PubMed] [Google Scholar]
- 23.Ruble AE, Leon PJ, Gilley-Hensley L, Hess SG, Swartz KL. Depression knowledge in high school students: effectiveness of the adolescent depression awareness program. J Affect Disord. 2013;150(3):1025–1030. doi: 10.1016/j.jad.2013.05.033. [DOI] [PubMed] [Google Scholar]
- 24.Hart SR, Kastelic EA, Wilcox HC et al. Achieving depression literacy: the Adolescent Depression Knowledge Questionnaire (ADKQ) School Ment Health. 2014;6(3):213–223. doi: 10.1007/s12310-014-9120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evans-Lacko S, Rose D, Little K et al. Development and psychometric properties of the Reported and Intended Behaviour Scale (RIBS): a stigma related behaviour measure. Epidemiol Psychiatr Sci. 2011;20(3):263–271. doi: 10.1017/s2045796011000308. [DOI] [PubMed] [Google Scholar]
- 26.Burns CD, Cortell R, Wagner BM. Treatment compliance in adolescents after attempted suicide: a 2-year follow-up study. J Am Acad Child Adolesc Psychiatry. 2008;47(8):948–957. doi: 10.1097/CHI.0b013e3181799e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ascher BH, Farmer EMZ, Burns BJ, Angold A. The child and adolescent services assessment (CASA) description and psychometrics. J Emot Behav Disord. 1996;4(1):12–20. [Google Scholar]
- 28.Farmer EM, Angold A, Burns BJ, Costello EJ. Reliability of self-reported service use: test–retest consistency of children’s responses to the Child and Adolescent Services Assessment (CASA) J Child Fam Stud. 1994;3(3):307–325. [Google Scholar]
- 29.Bryk AS, Raudenbush SW. Hierarchical Linear Models for Social and Behavioural Research: Applications and Data Analysis Methods. Newbury Park, CA: Sage; 1992. [Google Scholar]
- 30.Hedeker D, Gibbons RD. A random-effects ordinal regression model for multilevel analysis. Biometrics. 1994;50(4):933–944. [PubMed] [Google Scholar]
- 31.Hedeker D, Gibbons RD. MIXOR: a computer program for mixed-effects ordinal regression analysis. Comput Methods Programs Biomed. 1996;49(2):157–176. doi: 10.1016/0169-2607(96)01720-8. [DOI] [PubMed] [Google Scholar]
- 32.Hedeker D, Gibbons RD. MIXREG: a computer program for mixed-effects regression analysis with autocorrelated errors. Comput Methods Programs Biomed. 1996;49(3):229–252. doi: 10.1016/0169-2607(96)01723-3. [DOI] [PubMed] [Google Scholar]
- 33.Bates D, Sarkar D, Bates MD, Matrix L. The lme4 package. R package version 2007 [computer program]. Available at: http://ftp.auckland.ac.nz/software/CRAN/doc/packages/lme4.pdf. Accessed September 19, 2017.
- 34.Pinheiro J, Bates D, DebRoy S, Sarkar D. nlme: linear and nonlinear mixed effects models. R package version 3.1–117 [computer program]; 2014. Available at http://CRAN.R-project.org/package=nlme. Accessed September 19, 2017.
- 35.Calear AL, Christensen H, Mackinnon A, Griffiths KM, O’Kearney R. The YouthMood Project: a cluster randomized controlled trial of an online cognitive behavioral program with adolescents. J Consul Clin Psychol. 2009;77(6):1021–1032. doi: 10.1037/a0017391. [DOI] [PubMed] [Google Scholar]