Abstract
This study evaluates knee joint loading during gait and step-up-and-over tasks in control subjects, subjects with early knee OA and those with established knee OA. Thirty-seven subjects with varying degrees of medial compartment knee OA severity (eighteen with early OA and sixteen with established OA), and nineteen healthy controls performed gait and step-up-and-over tasks. Knee joint moments, contact forces (KCF), the magnitude of contact pressures and center of pressure (CoP) location were analyzed for the three groups for both activities using a multi-body knee model with articular cartilage contact, 14 ligaments, and six degrees of freedom tibiofemoral and patellofemoral joints. During gait, the first peak of the medial KCF was significantly higher for patients with early knee OA (p = 0.048) and established knee OA (p = 0.001) compared to control subjects. Furthermore, the medial contact pressure magnitudes and CoP location were significantly different in both groups of patients compared to controls. Knee rotation moments (KRMs) and external rotation angles were significantly higher during early stance in both patient groups (p < 0.0001) compared to controls. During step-up-and-over, there was a high variability between the participants and no significant differences in KCF were observed between the groups. Knee joint loading and kinematics were found to be altered in patients with early knee OA only during gait. This is an indication that an excessive medial KCF and altered loading location, observed in these patients, is a contributor to early progression of knee OA.
Introduction
Osteoarthritis (OA) is a chronic degenerative and multifactorial [1,2] joint disease that most frequently affects the knee [3], causing pain and functional disability. To date, there are no therapeutic interventions that overcome or effectively delay the progression of this disease and symptoms can only be managed [4]. Identifying the contributing factors associated with early stages of OA is imperative to classify patients at high risk to develop established knee OA and better assess effective treatments to protect joint integrity before major structural damage occurs.
Although the cause of OA is still not completely understood, biomechanical factors are known to play an important role [5,6]. Aberrant knee joint loading has been identified as a factor affecting the progression of knee OA [7–9]. External joint moments can be readily calculated from motion analysis data and thus have been proposed to identify characteristics of OA patients. Elevated knee adduction moment (KAM), the external knee joint moment in the frontal plane, has been used as a parameter reflecting elevated medial tibiofemoral loading [10–17] and was associated with the presence of medial knee OA [18]. Reduced external knee flexion moment (KFM), the external knee joint moment in the sagittal plane, is commonly reported for OA patients as a consequence of quadriceps weakness [19–22]. However, some studies in patients with early stages of knee OA suggest that altered KAM and KFM are not risk factors in the initial development of knee OA [16,17,23,24]. Only a few studies examined the external knee rotation moment (KRM), the external moment in transverse plane, for patients with knee OA and they report contradictory findings of altered KRM [19,25–28] in patients with OA compared to healthy subjects. In addition, for KRM, no comparison between early and established OA patients is available to date. Consequently, the ability of external joint moments to identify the onset of OA is still under debate [17].
Knee joint moments depend only on kinematics and external forces and, therefore, do not account for muscle forces. Consequently, a reduction in peaks KAM does not necessarily indicate a reduction in medial contact load [14]. On the other hand, knee contact force (KCF), calculated using musculoskeletal modeling in combination with dynamic simulations, directly reflect cartilage loading by accounting for muscle and ligament forces.
A previous study from our group showed that in early stages of knee OA, overall KCFs were not different from those in control subjects [23], but were more elevated in subjects with established OA. By differentiating the loading on the medial and lateral compartment, Kumar et al. [16] found higher medial KCFs in patients with established OA (with Kellgren-Lawrence score (K&L) ≥ 2) than in healthy subjects. Marouane et al. [29], have recently reported KCFs and their respective location during the stance phase in both healthy subjects and subjects with established knee OA (K&L = 3 or 4) aiming to compare various approaches to compute the KCF locations in both groups. This study focused on subjects with demonstrated radiographic knee OA. Therefore, to date no information on the medio-lateral load distribution in terms of KCFs and/or alterations in contact location of loading in the joint are available in early OA patients. Alterations in cartilage surface contact location have been suggested to occur during gait and associated to the high incidence of medial knee OA after anterior cruciate ligament (ACL) injury [30]. Interestingly, advances in musculoskeletal modeling now enable evaluation of the pressure distribution in the joint and therefore can provide insight into the load-bearing regions of the knee joint [31,32]. As such, shifts in contact location during weight-bearing activities can be evaluated, an action mechanism often suggested to contribute to the onset of OA [2].
Most studies in literature have focused on knee loading during gait as a biomarker for OA onset and progression. However, subjects with knee OA initially present pain complaints in more demanding tasks, specifically weight-bearing activities that involve large knee flexion [33]. There are only a few studies that have reported joint moments [33–37] and muscle activations [38] during stair negotiation in patients with severe knee OA. Similar to stair negotiation (walking on a flight of stairs/steps), step-up-and-over requires an upward propulsive phase (as stair ascent) as well as a downward energy absorption phase (as stair descent), recruiting large knee motion and high muscle force. Studies have shown lower KFM [33,37] and indications of lower KAM during stair ascent and descent [35] in patients with knee OA compared to healthy subjects. So far, compartmental KCFs have not been described in patients with knee OA during higher demanding tasks. However, these metrics are extremely relevant, as demanding movements might explain mechanical alterations earlier and therefore may be more helpful in identifying early OA, enabling earlier screening and treatment.
The first aim of this study is to evaluate the magnitude of knee joint loading (KCF in the medial and lateral knee compartment, maximum contact pressures and centre of pressure locations in the medial compartment) during gait in patients with early knee OA, and those with established knee OA compared to healthy subjects. We hypothesize that these parameters are more helpful in detecting early altered knee joint loading, prior to the onset of structural degeneration. Secondly, this study evaluates knee joint loading during step-up-and-over task in early OA subjects. We hypothesize that this higher demanding activity may already cause larger alterations in the medial compartment loading, present prior to alterations during gait and, therefore, may be able to discriminate patients with early knee OA from healthy subjects.
Methods
The current study represents an extended analysis of the data set reported in [23].
Participants
Fifty-three participants (all women, mean age of 64.8±7.5, from 37 to 78 years) were recruited and separated into three groups: asymptomatic healthy subjects (n = 19) as control; patients with symptomatic early medial knee OA (n = 18), and patients with symptomatic established medial knee OA (n = 16). Participants were recruited between 2008 and 2011. Patients with OA were recruited by a rheumatologist or orthopedic surgeon during weekly consultations in the University Hospitals Leuven. Healthy participants were recruited from cultural and social organizations. All procedures were approved by the local ethics committee of Biomedical Science, KU Leuven, Belgium. Written informed consent was obtained from each subject. The current analysis is part of a larger study already published by Baert et al. [39–41] and Mahmoudian et al.[42–44].
Early medial knee OA was diagnosed based on novel classification criteria of Luyten et al. [45], including fulfillment of three criteria, namely knee pain, a K&L [46] grade 0, 1 or 2− (osteophytes only) and structural changes observed on MRI.
Established medial knee OA was diagnosed based on slightly adapted American College of Rheumatology classification criteria [47], including knee pain, morning stiffness of less than 30 min duration and crepitus, together with structural changes defined as presence of minimum grade 2+ (osteophytes and joint space narrowing) on K&L scale for at least the medial compartment on radiography.
A control group was also analyzed, which included asymptomatic healthy subjects with no history of knee OA or other pathology involving any lower extremity joints, and with a radiological score of 0 or 1 according to K&L score.
Participants were excluded if they had a prior significant trauma or surgery in lower limbs and/or low back, if they suffered from a neurological disease affecting coordination and/or balance during gait and/or musculoskeletal disorders other than knee OA in one of the limbs during the last six months prior to testing.
Subject characteristics are listed in Table 1. Knee pain was assessed through the Knee Injury and Osteoarthritis Outcome Score (KOOS) (Dutch version [48]). Knee joint alignment in the frontal plane was measured by a single experienced observer on full-leg, anterior-posterior, weight-bearing radiographs of the lower limbs (Oldelft, Triathlon, Agfa ADC M Compact Plus) [49].
Table 1. Characteristics of the groups.
Control (CO), early OA (EA) and established OA (ES).
| Task | Control | Early OA | Established OA | p |
p (CO-EA) |
p (CO- ES) |
p (EA- ES) |
|
|---|---|---|---|---|---|---|---|---|
| No. of subjects | Gait | 17 | 14 (6uni+8bi) | 16 (16bi) |
- | - | - | - |
| Step | 19 | 18 (8uni+19bi) | 16 (16bi) |
- | - | - | - | |
| Age, years (age range) |
Gait | 64.2±9.0 (37 to 78) |
63.3±7.7 (49 to 73) |
67.2±6.7 (54 to 78) |
0.362 | 0.985 | 0.619 | 0.449 |
| Step | 64.3±8.5 (37 to 78) |
63.3±7.0 (49 to 73) |
67.2±6.7 (54 to 78) |
0.305 | 0.965 | 0.598 | 0.351 | |
| Body mass, kg | Gait | 64.0±7.9 | 69.7±16.6 | 73.3±11.9 | 0.103 | 0.494 | 0.102 | 0.809 |
| Step | 64.6±7.7 | 70.0±15.5 | 73.3±12.0 | 0.103 | 0.440 | 0.109 | 0.813 | |
| Height, m | Gait | 1.61±0.1 | 1.62±0.1 | 1.61±0.1 | 0.828 | 0.971 | 0.993 | 0.903 |
| Step | 1.62±0.1 | 1.62±0.1 | 1.61±0.1 | 0.837 | 0.994 | 0.974 | 0.910 | |
| KOOS pain score | Gait | 100±0.0 | 82.9±17.7 | 73.3±19.4 | 0.000 | 0.005 | 0.000 | 0.203 |
| Step | 100±0.0 | 84.4±15.4 | 73.4±19.4 | 0.000 | 0.004 | 0.000 | 0.075 | |
| Speed, m/s | Gait | 1.21±0.2 | 1.26±0.2 | 1.20±0.2 | 0.426 | 0.623 | 0.992 | 0.524 |
| Step | 0.53±0.1 | 0.55±0.1 | 0.57±0.1 | 0.311 | 0.663 | 0.371 | 0.966 | |
| Knee Alignment in the frontal plane ° |
Gait | 0.50±2.3 (24) |
1.46±3.4 (15) |
3.66±3.5 (13) |
0.014 | 0.701 | 0.010 | 0.164 |
| Step | 0.45±2.5 (26) |
1.14±3.2 (18) |
4.03±3.5 (12) |
0.004 | 0.831 | 0.003 | 0.034 |
Values are the mean ± Standard Deviation (SD). ANOVA with Gabriel post hoc test. Significant difference p < 0.05 are indicated in bold.
For the knee alignment, positive values indicate varus (adduction) alignment and negative values indicate valgus (abduction) alignment.
Uni corresponds to the number of patients with unilateral OA and bi to those with bilateral OA.
For healthy subjects, both legs were analyzed. For symptomatic patients with unilateral knee OA, only data of the affected knee were analyzed. For those with bilateral knee OA, both legs were analyzed except if the less involved side presented with a K&L score ≤ 2 (Fig 1 and Table 1) for the established OA group.
Fig 1.
Flow charts of the limbs selection for gait (A) and step-up-and–over (B). The final number of the analyzed limbs are indicated in bold. During gait, 11%, 50% and 7% of the total knees diagnosed with early OA presented K&L of 0, 1 and 2, respectively. During step-up and -over, 17%, 47% and 6% of the total knees diagnosed with early OA presented K&L of 0, 1 and 2, respectively. Numerical problems are indicated as n.p.
All recruited subjects performed gait and step-up-and-over tasks. However, due to numerical problems during the simulation, six subjects were excluded from the gait analysis (Fig 1). More details about the participants’ selection and the total number of limbs included in each group are presented in Fig 1.
Motion analysis
An active 3D motion analysis system (Krypton, Metris) recorded the 3D position of 27 LEDs at a sampling frequency of 100 Hz placed according to an extended Helen Hayes protocol (consisting of 5 technical clusters and 12 anatomical landmarks). Marker data were labeled and smoothed using a spline routine [50] in Matlab R2010b (Mathworks, inc.) with cut-off at 6Hz. A force plate (Bertec Corporation, USA) measured ground reaction forces (GRF) sampled at 1000 Hz. GRF were filtered using a second order Butterworth low pass filter, with cut-off level at 30Hz.
Gait analysis consisted of barefoot level walking along a 10 m walkway at self-selected speed with the force plate embedded in the middle of the walkway. Subjects were required to perform 6 trials for each leg.
Step-up-and–over analysis consisted of barefoot [51] stepping onto a 20-cm-high step with one leg (stepping leg), while stepping over with the other leg (trailing leg) making contact on the other side of the step (Fig 2). The force plate was embedded in the ground under the step. Subjects performed a total of 3 trials for each leg.
Fig 2. A schematic illustrating the step-up-and-over task (adapted from Reid [52]).
The stepping leg (bold) is the leg considered for further analysis.
Musculoskeletal model
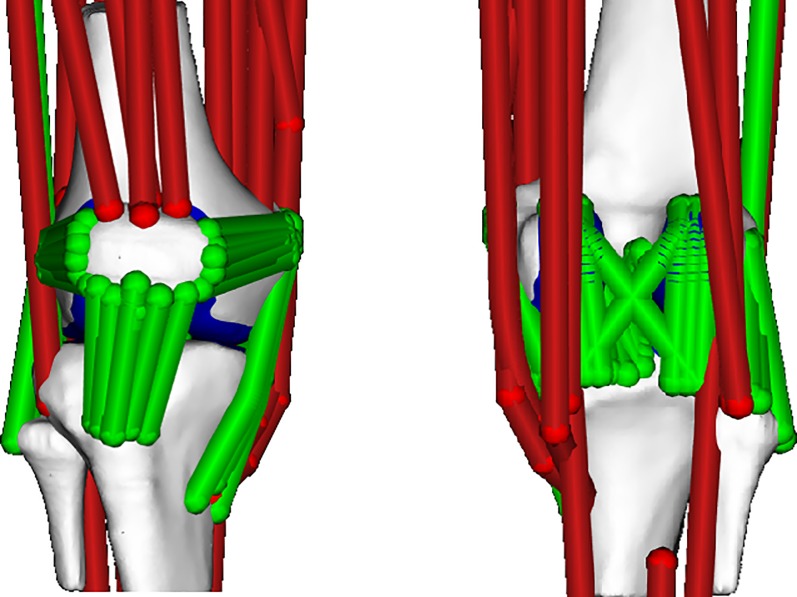
A multi-body knee model (Fig 3) with 6 degrees of freedom for the tibiofemoral and patellofemoral joints was used [53]. Fourteen ligaments were represented by bundles of nonlinear elastic springs. Cartilage surface contact pressures were computed using an elastic foundation formulation [54]. The knee model was integrated into an existing lower extremity musculoskeletal model [55], which included 44 musculotendon units crossing the hip, knee and ankle joints.
Fig 3. Multibody 12 degree of freedom knee model [53] including ligaments and an elastic foundation contact model.
The lower extremity model was scaled to subject-specific segment lengths as determined in a static calibration trial. The joint angles were computed using an inverse kinematics algorithm. The concurrent optimization of muscle activations and kinematics (COMAK) algorithm [31], was used to compute the secondary tibiofemoral (tibiofemoral translations and non-sagittal rotations) and patellofemoral kinematics, muscle and ligament forces, and KCFs by minimizing the muscle volume weighted sum of squared muscle activations plus the net knee contact energy. Tibiofemoral cartilage contact pressures were computed using a non-linear elastic foundation model in which pressure is assumed to be a function of the depth of penetration between meshes of the contacting cartilage surfaces. Depths of penetration for each triangle in a mesh were determined at each time step using ray-casting techniques [53]. At each triangle of the tibia plateau, the contact pressure was computed, in which cartilage was assumed to have an elastic modulus of 10 MPa, a Poisson's ratio of 0.45, and a uniform thickness of 2 mm for each surface (i.e. 4 mm total thickness) [54]. Subsequently, an inverse dynamics algorithm computed the external joint moments: KFM, KAM and KRM.
Total KCFs correspond to the resultant tibiofemoral contact forces in the entire joint, while medial and lateral KCFs correspond to contact forces in the medial and lateral compartment, respectively. KCFs are expressed in the tibia reference frame. Calculated KCFs were normalized to body weight (BW) and moments were normalized to the product of body weight and height (BW×Ht). All data were time normalized to the stance phase (i.e. from initial contact to toe off of the ipsilateral leg).
Data analysis
During gait, KCFs, moments and angles throughout the stance phase were averaged over the 6 trials for each leg. The peaks during the first and second half of the stance phase were determined for the total KCF, medial KCF, and lateral KCF, KFM and KRM. The minimum total, medial and lateral KCF and KFM during the single support (SS) phase, corresponding to the middle of the stance phase, occurring from toe-off until heel strike of the contralateral foot, between 25% and 75% of the gait cycle, were determined. For the KAM, only the first peak during early stance, corresponding to the highest peak during stance, was calculated. Although two peaks in KAM have been reported for healthy subjects and patients at early stages of OA, patients with advanced medial knee OA frequently present one peak during early stance and, therefore, a minimum value during SS and a second peak were not always clear [17,56–59]. A similar trend was found in our study, in which some patients with established knee OA did not show a distinct second peak.
During step-up-and-over, KCFs, joint moments and angles of the stepping leg were averaged across the 3 trials throughout the stance phase for each leg. The maximal values of total KCF, lateral KCF, KFM and KAM during the first and second half of the stance phase and the minimum values during the SS phase were determined (minimum total KCF, minimum lateral KCF, minimum KFM, and minimum KAM, respectively). In addition, the highest peak medial KCF during the stance phase was compared between groups. Due to the high variation in the individual KRM pattern observed in patients with established OA during this task, maximum values of KRM were not calculated and only the average curve is presented.
Furthermore, at the time instant of peak medial KCF, the maximum contact pressure magnitude and center of pressure (CoP) location in the medial tibial plateau were assessed and compared between the groups. The medial-lateral and anterior-posterior locations of CoP, calculated with respect to the tibia reference frame, were normalized to the tibia size and compared between the groups.
Statistical analysis
One-way analysis of variance (ANOVA), performed with SPSS Inc., v17.0, evaluated whether differences in peaks and minimum moments, KCF, contact pressures and CoP location were significantly different (p ≤ 0.05) between the three groups. As sample sizes were slightly different, Gabriel post hoc test was used to assess whether the differences were significant.
The effect size (Cohen's d) on these ANOVA tests were evaluated using G*Power 3.1.9.2 [60] based on the assumption of less than 5% Type I error. The effect size (f, from population means) for the F-test ANOVA were considered small for f = 0.10, medium for f = 0.25 and large for f = 0.40 with a minimum effect size (d, from standard deviations) of 0.80 considered acceptable [61].
Results
Subject characteristics
Age, body mass, height, and speed for gait and step-up-and–over did not differ significantly between the three groups (Table 1). Both OA groups reported significantly greater knee pain (p < 0.001) than controls, but no difference was found between the two groups of OA patients. Patients with established OA presented significantly higher varus alignment compared to controls in both gait and step-up-and-over (p = 0.010 and p = 0.003, respectively).
Knee joint loading during gait
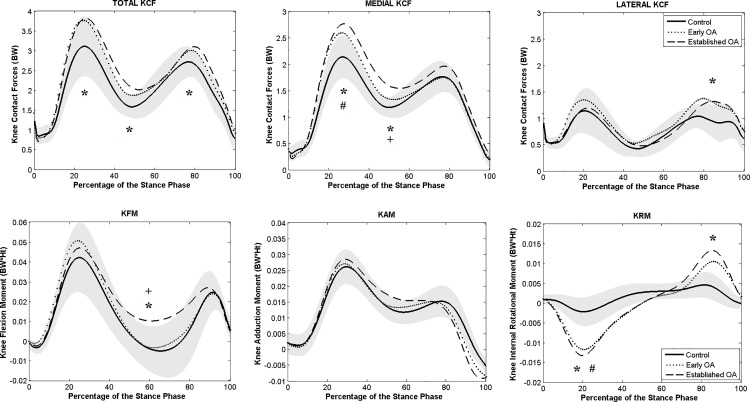
Only patients with established knee OA showed significantly higher peaks and higher minimum total KCF during the single support phase (Fig 4), when compared to controls (p = 0.012 and p = 0.013 during both first and second peak and p < 0.0001 during SS). No significant difference in total KCF was found between early OA and control subjects.
Fig 4. Averaged total, medial and lateral KCF (above) and knee moments (below) during stance phase of gait.
Knee moments in the sagittal, frontal and transversal planes are presented. The gray shaded area corresponds to the standard deviation of the control group. * indicates a significant difference between established OA and control group. # indicates a significant difference between early OA and control group. + indicates a significant difference between the early and established OA.
Both patient groups presented higher peak medial KCF compared to controls (p = 0.001, established OA and p = 0.048, early OA). Lateral compartment KCFs were higher in both OA groups during the second part of stance compared to healthy subjects (S1 Table) but only significantly for the established knee OA group (p = 0.009).
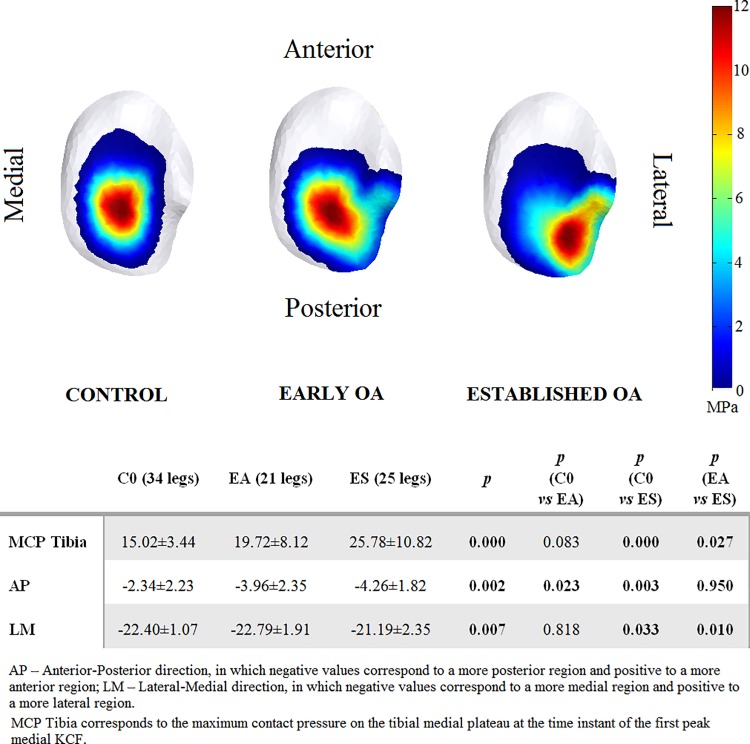
In Fig 5, the average contact pressure distribution on the tibial plateau at the time instant of the first peak medial KCF are presented for the three groups. Maximum contact pressure was significantly higher for subjects with established OA (25.78±10.82 MPa) compared to the control (15.02±3.44 MPa) and early OA (19.72±8.12 MPa) groups. In subjects with early knee OA, the medial compartment CoP at the time instant of the first peak medial KCF was shifted from central (as seen in the control subjects) to a significantly more posterior region, while a significantly more postero-lateral location of the CoP was found in subjects with established OA.
Fig 5. Group-averaged contact pressure distributions on the articular surfaces of medial tibial plateau at the time instant of the first peak medial KCF.
To obtain these averaged contact pressure distribution maps, the average contact pressure was calculated for every triangle of the medial tibial surface mesh and presented on a representative surface model. Results are presented for the control group (C0, on the left), the early knee OA group (EA, in the middle), and the established knee OA group (ES, on the right).
No significant differences were found in peak KFM or KAM between the three groups. During SS, patients with established knee OA presented significantly higher KFM compared to control and early OA groups (S1 Table). First peak KRM was significantly higher in early (p < 0.0001) and established OA (p < 0.0001) groups compared to healthy subjects. Only established OA showed significantly higher second peak KRM (Fig 4).
At the time instant of the first peak medial KCF, the tibia was significantly more externally rotated with higher variation for both OA groups (rotation angle means and respective standard deviations of –7.4°±14.0° and –14.6°±14.3°, respectively, for early and established OA) compared to the controls (rotation angle mean and respective standard deviation of +0.3°±5.1°) (S1 Fig and S1 Table).
For all reported significant differences, the effect size f was large or medium to large (f ≥ 0.34) and d ranged from acceptable (d ≥ 0.80) to very high (d ≥ 0.95) (S1 Table). Only for the second peak KRM a d lower than 0.80 was found.
Knee joint loading during step-up-and-over
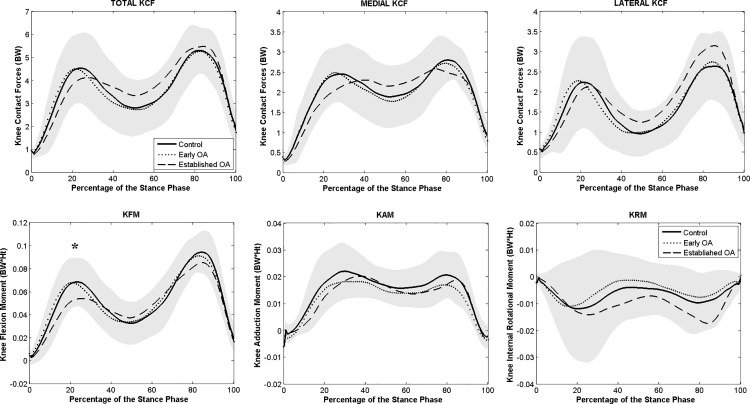
No significant differences in KCF, either medial or lateral, were observed between the groups (Fig 6). Due to the high variability in terms of joint angles (S2 Fig), moments and KCFs (S2 Table) between subjects during the step-up-and-over task, f values were small to medium and d did not achieve the acceptable minimum. Therefore, the contact pressure data was not further analyzed.
Fig 6. Averaged total, medial and lateral KCF (above) and knee moments (below) during stance phase of step-up-and-over.
Knee moments in the sagittal, frontal and transversal planes are presented. The gray shaded area corresponds to the standard deviation of the control group. *indicates a significant difference between established OA and control groups.
Patients with established knee OA did present significantly lower first peak KFM compared to controls (p = 0.038) (S2 Table). No significant differences were observed in terms of KAM between the three groups (Fig 6).
Discussion
This study investigated magnitude and location of knee loading during gait and step-up-and-over in subjects with early and established medial knee OA. We evaluated loading differences, both KCFs and contact pressure distributions, between patients with early OA compared to healthy subjects and patients with established OA aiming to identify whether early changes in knee loading are already present in these patients.
Knee joint loading during gait
Our study shows that in patients at early stages of OA, altered medial compartment knee loading is found when using a musculoskeletal model which calculates compartmental joint loading. An elevated overall mechanical loading during gait, assessed by the total KCF, is only present in more advanced stages of the disease as observed in patients with established knee OA and not in early stages. Likewise, although the maximum contact pressures were more elevated in both groups of OA patients compared to controls, it was only significant in patients with established OA. This partially confirms our first hypothesis, in which medial KCF during gait showed to be helpful in detecting early changes in knee loading. Nevertheless, both patients groups with knee OA showed a shifted CoP at the first peak medial KCF which, in combination with higher external rotation of the tibia than healthy subjects during early stance, shows that patients with knee OA tend to load a more posterior (both groups) and lateral (established OA) cartilage region of the medial tibia plateau, which is not loaded in healthy subjects (Fig 5). This suggests that, although excessive loading is not revealed by the total KCF in the early phase of the disease, the medial-lateral force and pressure distributions are altered. Only when clear structural degeneration is present (KL>2), as in the established OA group, changes in gait mechanics result in excessive total knee loading compared to healthy controls. The abnormal transverse plane kinematics, particularly the more elevated external rotation found in patients with OA than in controls, shifted the normal load bearing contact to regions in the cartilage which are less predisposed for higher loads and therefore might influence the initiation of knee OA. If the normal load bearing contact has shifted to a region less predisposed for higher and repetitive loading during walking, due to ligament-deficiency or -injury, there is the potential for a degenerative pathway to be initiated [62].
In regards to the external joint moments during gait, only peak KRMs were significantly different between patients with early knee OA and healthy subjects. Patients with established OA showed higher midstance KFM, but no differences in peak KAM or KFM compared to the other two groups, confirming our previous study [23]. First peak KRM was higher in patients with knee OA than in healthy subjects. For patients with established OA, the excessive rotation moments persisted during late stance. Although KRM has received much less attention in the literature than KAM or KFM, and less consistence has been found between studies assessing patients with knee OA [19,25,26,63,64], our findings confirm the study of Gok et al. [25] and Wilson et al. [26], who found higher rotation moments in patients with knee OA compared to healthy subjects.
Comparing to previous literature, similar patterns of joint moments were observed in the present study [16,19,23,25,26,63,64]. In terms of magnitudes, studies show more differences in knee joint moments between each other, depending on the group of participants and techniques used to calculate knee moments. Magnitudes of peak KFM as well as moments in the other two planes of movement in healthy subjects and subjects with OA were in general comparable to those presented by Gok et al. [25] and Kumar et al. [16]. Significant differences in peak KAM have been previously reported [65–69] and are in contrast with the present study. Previous studies have used more simplified knee models, presenting less degrees of freedom and calculated knee kinematics using the transepicondylar axis (TEA), therefore not accounting for load-dependency effects on knee angle calculations. More simplified knee models can induce differences in the calculated kinematics and, ultimately, in KAM compared to more complex knee models. Firstly, large errors in the calculation of the secondary kinematics (varus-valgus angle) are expected when using TEA to calculate knee angles [70–74]. Secondly, by tracking the secondary kinematics, models do not take load-dependency effects into account [54,74–77] that may be relevant especially in patients with knee OA [74] as they normally present more joint instability [78]. Indeed, in a previous study [74], the effect of the knee axis on the calculated KAM was assessed, which underlined the sensitivity of KAM to knee axis definition. The current knee model includes six degrees of freedom in the tibiofemoral and six in the patellofemoral joints and accounts for load-dependent effects in the moment calculation that may explain the differences in angles and moments compared to previous studies.
The present study provides important insight into the altered medial loading magnitude and medial pressure location which were found to be already present in patients at early stages of medial knee OA, but was not revealed by the total KCF. With progression of structural degeneration, alterations in gait mechanics led to elevated overall joint loading, affecting both the medial and lateral compartment. Therefore, medial KCF rather than KAM or total KCF during gait provides the most helpful marker for early OA.
Knee joint loading during step-up-and-over
High variations in movement strategies between subjects, particularly in those having knee OA, were observed during step-up-and-over. Due to these high variations, the effect size was low. Consequently, step-up-and-over does not generate large differences in kinematics and loading patterns, which might be due to the difficulty of standardizing the movement execution. As a more demanding task, step-up-and-over seems to motivate subjects, particularly those with knee OA, to search more for alternative movement strategies to deal with and, therefore, generating elevated variations.
In contrast to our second hypothesis, no significant differences were observed in knee loading between patients with early knee OA and healthy subjects during step-up-and-over. However, most patients with established knee OA presented a different timing of the highest peak medial KCF compared with the other two groups. This difference in the loading pattern observed in patients with established OA needs further analysis.
Interestingly, during step-up-and-over, no significant differences in peak KAM were found between early OA and healthy subjects, or even between established OA and controls, although the high variation in the data indicates larger subject numbers may be necessary to effectively study this task. Nevertheless, patients with established knee OA showed reduced first peak KFM compared to the control group and also to the early knee OA group during the upward propulsive phase (step ascent). This finding is in line with previous studies in stair negotiation [21,22,36,79], in which patients with established knee OA also presented altered movement strategies in the sagittal plane.
Limitations of this study
These results have to be interpreted in view of some methodological limitations, as inherent to the model used [54]. Firstly, we used a single generic knee model that was scaled to represent the anthropometry of the subjects instead of considering the subject-specific articular geometries, including those of the tibia plateau. Our model does not account for OA induced changes in the articular geometry, such as thickness and mechanical properties of the cartilage, or changes in the muscle and ligament properties. Consequently, the reported differences in KCF and contact pressures only result from altered kinematic and kinetic behavior. Bone deformities, ligament laxity or changes in cartilage induced by joint degeneration were not taken into account and they might produce an effect on contact pressures [80]. However, the effect of having a 2-mm constant cartilage thickness instead of a variable thickness on tibiofemoral contact pressure during gait has been previously assessed and showed limited effect on the observed peak contact pressure (about 4%) [80]. Secondly, although the secondary tibiofemoral kinematics and patellofemoral kinematics were calculated as a function of muscle and ligament forces, and cartilage contact and only knee flexion was tracked in the gait simulation, the method may still present some sensitivity to soft tissue artifacts. Thirdly, although the validation of the model has shown a good agreement between the calculated and experimental kinematics and contact forces in healthy subjects and patients following total knee replacement [54], this validation cannot easily be extended to an OA population. The presence of increased co-contraction, bone deformities or changes in cartilage mechanical properties, and the potential presence of ligament laxity induced by joint degeneration were not evaluated. Therefore, this model might present specific limitations when used in patients with knee OA, especially those known to present increased co-contraction (KL≥2) resulting in an underestimation of the joint loading [81,82]. Compared to previous literature in subjects with instrumented prosthesis [63,64], the magnitude of KCF in healthy subjects and those with OA seen in the present study were higher for both walking and step-up-and-over. Our controls exhibited an averaged peak total resultant KCF of 3.16 BW and 4.94 BW (walking and step-up, respectively), while our patients with knee OA exhibited a peak KCF of 3.91 BW and 4.49 BW, respectively. Reported values in instrumented knee studies range from 2.20 to 2.8 BW for walking and from 2.50 BW to 3.5 BW for stair negotiation [63,64,83–86]. However, KCF measured from instrumented prostheses cannot be expected to be similar to those estimated in healthy and patients with OA, as the surgical procedure involves articular surface replacement, changes in the bone structure, and re-alignment of the mechanical knee axis [87] that dramatically change the gait pattern [88]. In other computational studies [16,23,89], also higher KCFs were observed in healthy and patients with OA. Healthy subjects exhibited a peak total resultant KCF range from 3.00 to 4.35 BW [16,23,89,90], and patients with severe knee OA range from 4.0 to 4.5 BW during walking [16,23,89]. Finally, only females participated in the study and, therefore, no conclusions can be drawn for male patients affected with OA.
Conclusions
Altered knee joint loading and pressure location during gait were found to be already present in early OA, as confirmed in the elevated medial KCFs and a shift in the center of pressure. Our findings indicate that medial KCF predicted by a novel musculoskeletal simulation routine provides a more helpful metric than the KAM used by previous researchers to identify early knee OA development prior to the onset of radiographic evidences. This reinforces the importance of considering the muscle and ligament forces when assessing knee loading rather than only the external knee adduction moment. Consequently, KCF might be used as feedback signal during gait retraining sessions aiming at controlling knee loading in patients with knee osteoarthritis. Excessive medial KCF seems to be already present in early stages of OA.
As more muscular demanding, step-up-and-over resulted in higher total knee contact force compared to walking in controls, and caused patients to present a large variability in their movement execution, possibly aiming to reduce knee loading. Therefore, step-up-and-over was not the best task to induce higher loading in order to discriminate loading profiles between patients with early knee OA from healthy subjects.
Supporting information
The gray shaded area corresponds to the standard deviation of the control group. * indicates a significant difference between established OA and control groups. # indicates a significant difference between early OA and control group.
(TIF)
The gray shaded area corresponds to the standard deviation of the control group.
(TIF)
Peak and minima SS values of the KCF, KFM, KAM and KRM during the stance phase of gait, as well as rotation angles (RAngle in degrees). at the time instant of the first peak MKCF, for control (C0), early OA (EA) and established OA (ES) groups.
(DOCX)
Peak and SS values of the KCF, KFM and KAM during the stance phase of step-up-and-over for control (C0), early OA (EA) and established OA (ES) groups.
(DOCX)
First and second peaks of the KCF during gait, and minimum values during midstance (SS).
(DOCX)
First and second peaks of the KCF during step-up-and-over, and minimum values during midstance (SS) of step-up-and-over.
(DOCX)
Peaks of the KAM, KFM and KRM during gait, and minimum value during midstance (SS).
(DOCX)
Peaks of the KAM and KFM during step-up-and-over, and minimum value during midstance (SS).
(DOCX)
(DOCX)
(DOCX)
Data Availability
Individual data points for each individual subject are provided in the paper's Supporting Information files (S3 Table, S4 Table, S5 Table, S6 Table, S7 Table and S8 Table). All motion data are available from Open Science Framework at the following URL: https://osf.io/8edy3/.
Funding Statement
Integrated in Move-Age program funded by the European Commission as part of the Erasmus Mundus program. Research was supported by funding of the KU Leuven research council (OT/13/083).
References
- 1.Lories RJ, Luyten FP. The bone-cartilage unit in osteoarthritis. Nat Rev Rheumatol 2011; 7(1):43–49. doi: 10.1038/nrrheum.2010.197 [DOI] [PubMed] [Google Scholar]
- 2.Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng 2004; 32(3):447–457. [DOI] [PubMed] [Google Scholar]
- 3.Buckwalter JA, Martin JA. Osteoarthritis. Adv Drug Deliv Rev 2006; 58(2):150–67. doi: 10.1016/j.addr.2006.01.006 [DOI] [PubMed] [Google Scholar]
- 4.McAllindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil 2014; 22:363–88. doi: 10.1016/j.joca.2014.01.003 [DOI] [PubMed] [Google Scholar]
- 5.Nuki G, Salter D. The impact of mechanical stress on the pathophysiology of osteoarthritis. In: Sharm K & Berenbaum F (eds). Osteoarthritis. Philadelphia: Mosby; 2007. p. 33–52.
- 6.Radin EL, Rose RM. Role of subchondral bone in the initiation and progression of cartilage damage. Clin Orthop Relat Res 1986; 213:34–40. [PubMed] [Google Scholar]
- 7.Fregly BJ, Reinbolt JA, Rooney KL, Mitchell KH, Chmielewski TL. Design of patient-specific gait modifications for knee osteoarthritis rehabilitation. IEEE Trans Biomed Eng 2007; 54:1687–1695. doi: 10.1109/TBME.2007.891934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mundermann A, Asay JL, Mundermann L, Andriacchi. Implications of increased medio-lateral trunk sway for ambulatory mechanics. J Biomech 2008; 41:165–170. doi: 10.1016/j.jbiomech.2007.07.001 [DOI] [PubMed] [Google Scholar]
- 9.Hurwitz DE, Ryals AR, Block JA, Sharma L, Schnitzer TJ, Andriacchi TP. Knee pain and joint loading in subjects with osteoarthritis of the knee. J Orthop Res 2000; 18:572–579. doi: 10.1002/jor.1100180409 [DOI] [PubMed] [Google Scholar]
- 10.Andriacchi T. Dynamics of knee malalignment. Orthop Clin North Am, 1994; 25:395 [PubMed] [Google Scholar]
- 11.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis 2002; 61:617–622. doi: 10.1136/ard.61.7.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baliunas A, Hurwitz D, Ryals A, Karrar A, Case JP, Block JA, Andriacchi TP. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthr Cartil 2002; 10:573–579. [DOI] [PubMed] [Google Scholar]
- 13.Meyer AJ, D’Lima DD, Besier TF, Lloyd DG, Colwell CW, Fregly BJ. Are external knee load and EMG measures accurate indicators of internal knee contact forces during gait?, J Orthop Res 2013; 31(6); 921–9. doi: 10.1002/jor.22304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walter JP, D'Lima DD, Colwell CW Jr., Fregly BJ. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. J Orthop Res 2010; 28(10):1348–1354. doi: 10.1002/jor.21142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kutzner I, Trepczynski A, Heller MO, Bergmann G. Knee adduction moment and medial contact force—facts about their correlation during gait, PLoS One 2013; 2;8(12):e81036 doi: 10.1371/journal.pone.0081036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar D, Manal KT, Ridolph KS. Knee joint loading during gait in healthy controls and individuals with knee osteoarthritis. Osteoarthr Cartil 2013; 21, 298–305. doi: 10.1016/j.joca.2012.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baert IA, Jonkers I, Staes F, Luyten FP, Truijen S, Verschueren S. Gait characteristics and lower limb muscle strength in women with early and established knee osteoarthritis. Clin Biomech (Bristol, Avon) 2013; 28(1):40–7. [DOI] [PubMed] [Google Scholar]
- 18.Sharma L, Hurwitz DE, Thonar EJMA, Sum JA, Lenz ME, Dunlop DD, Schnitzer TJ, Kirwan-Mellis G, Andriacchi TP. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum 1998; 41:1233–40. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L [DOI] [PubMed] [Google Scholar]
- 19.Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Knee biomechanics of moderate OA patients measured during gait at a self-selected and fast walking speed, J Biomech 2007; 40: 1754–1761. doi: 10.1016/j.jbiomech.2006.08.010 [DOI] [PubMed] [Google Scholar]
- 20.Roos EM, Herzog W, Block JA, Bennell KL. Muscle weakness, afferent sensory dysfunction and exercise in knee osteoarthritis. Nat. Rev. Rheumatol. 2011; 7:57–63. doi: 10.1038/nrrheum.2010.195 [DOI] [PubMed] [Google Scholar]
- 21.Hurley MV. 1998. Quadriceps weakness in osteoarthritis. Curr Opin Rheumatol 10:246–250. [DOI] [PubMed] [Google Scholar]
- 22.Slemenda C, Brandt KD, Heilman DK, et al. 1997. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med 127: 97–104. [DOI] [PubMed] [Google Scholar]
- 23.Meireles S, Groote FD, Reeves ND, Verschueren S, Maganaris C, Luyten F, Jonkers I. Knee contact forces are not altered in early knee osteoarthritis, Gait Posture 2016; 45:115–120. doi: 10.1016/j.gaitpost.2016.01.016 [DOI] [PubMed] [Google Scholar]
- 24.Duffell LD, Southgate DFL, Gulati V, McGregor AH. Balance and gait adaptations in patients with early knee Osteoarthritis, Gait Posture 2014; 39: 1057–61. doi: 10.1016/j.gaitpost.2014.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gok H, Ergin S, Yavuzer G. Kinetic and kinematic characteristics of gait in patients with medial knee arthrosis. Acta Orthop Scand 2002; 73:647–52. doi: 10.1080/000164702321039606 [DOI] [PubMed] [Google Scholar]
- 26.Wilson JLA, Hatfield G, Stanish WD, Hubley-Kozey. Asymptomatic individuals with radiographic evidence of knee osteoarthritis walk with different knee mechanics patterns than symptomatic individuals with the same radiographic evidence. Osteoarthr Cartil, 2013; 21:S9–S62. [Google Scholar]
- 27.Harding GT, Hubley-Kozey CL, Dunbar MJ, Stanish WD, Wilson ALA. Body mass index affects knee joint mechanics during gait differently with and without moderate knee osteoarthritis, Osteoarthr Cartil 2012; 20:1234–1242. doi: 10.1016/j.joca.2012.08.004 [DOI] [PubMed] [Google Scholar]
- 28.Kang SH, Lee SJ and Zhang L-Q. Real-time tracking of knee adduction moment in patients with knee osteoarthritis, J Neurosci Methods 2014; 231:9–17. doi: 10.1016/j.jneumeth.2013.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marouane H, Shirazi-Adl A and Adouni M. Alterations in knee contact forces and centers in stnce phase of gait: a detailed lower extremity musculoskeletal model, J Biomech 2016; 49:185–192. doi: 10.1016/j.jbiomech.2015.12.016 [DOI] [PubMed] [Google Scholar]
- 30.Andriacchi TP, Briant PL, Bevill SL, and Koo S. Rotational changes at the knee after ACL injury cause cartilage thinning, Clin Orthop Rel Res 2006; 442:39–44. [DOI] [PubMed] [Google Scholar]
- 31.Smith CR, Choi KW, Negrut D and Thelen DG. Efficient computation of cartilage contact pressures within dynamic simulations of movement, Comput Methods Biomech Biomed Eng: Imaging Vis, 2016. [DOI] [PMC free article] [PubMed]
- 32.Koo, S, EJ Alexander, GE Gold, NJ Giori, and TP Andriacchi. Morphological thickness in tibial and femoral cartilage are influenced by gait characteristics in healthy and osteoarthritic knees. In: Proceedings of the 2003 ASME Summer Conference, Miami, FL, 2003.
- 33.Hensor E, Dube B, Kingsbury SR, Tennat A, Conaghan PG. Toward a clinical definition of early osteoarthritis: onset of patient-reported knee pain begins on stairs. Data from the osteoarthritis initiative. Arthritis Care & Res 2015; 67, 1: 40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo M, Axe MJ, Manal K. The influence of foot progression angle on the knee adduction moment during walking and stair climbing in pain free individuals with knee osteoarthritis. Gait Posture 2007; 26:436–441. doi: 10.1016/j.gaitpost.2006.10.008 [DOI] [PubMed] [Google Scholar]
- 35.Asay JL, Mundermann A and Andriacchi TP. Adaptive patterns of movement during stair climbing in patients with knee osteoarthritis, J Orthopaedic Res 2009; 325–329. [DOI] [PubMed] [Google Scholar]
- 36.Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech 2001; 34:907–15. [DOI] [PubMed] [Google Scholar]
- 37.Igawa T and Katsuhira J. Biomechanical Analysis of Stair Descent in Patients with Knee Osteoarthritis. J Phys Ther Sci 2014; 26:629–631. doi: 10.1589/jpts.26.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liikavaino T. Biomechanics of gait and physical function in patients with knee osteoarthritis: thigh muscle properties and joint loading assessment. Publ. Univ. Eastern Finland. Dissertations in Health Sciences 2010; 13:98. [Google Scholar]
- 39.Baert IA, Jonkers I, Staes F, Luyten FP, Truijen S, Verschueren SM. Gait characteristics and lower limb muscle strength in women with early and established knee osteoarthritis, Clin Biomech 2013a; 40–47. [DOI] [PubMed] [Google Scholar]
- 40.Baert IA, Mahmoudian A, Nieuwenhuys A, Jonkers I, Staes F, Luyten FP, Truijen S, Verschueren SM. Proprioceptive accuracy in women with early and established knee osteoarthritis and its relation to functional ability, postural control, and muscle strength Clin Rheumatol 2013b; 32(9): 1365–74. [DOI] [PubMed] [Google Scholar]
- 41.Baert IA, Staes F, Truijen S, Mahmoudian A, Noppe N, Vaderschueren G, Luyten FP, Verschueren SM. Weak associations between structural changes on MRI and symptoms, function and muscle strength in relation to knee osteoarthritis, Knee Sur Sports Traumatol Athrosc 2014; 22(9): 2013–25. [DOI] [PubMed] [Google Scholar]
- 42.Mahmoudian A, van Dieen JH, Bruijn SM, Baert IA, Faber GS, Luyten FP, Verschueren SM. Varus thrust in women with early medial knee osteoarthritis and its relation with the external knee adduction moment, Clin Biomech 2016a; 39: 109–114. [DOI] [PubMed] [Google Scholar]
- 43.Mahmoudian A, van Dieen JH, Baert IA, Jonkers I, Bruijn SM, Luyten FP, Faber GS, Verschueren SM. Changes in proprioceptive weighting during quiet standing in women with early and established knee osteoarthritis compared to healthy controls, Gait Posture 2016b; 44: 184–8. [DOI] [PubMed] [Google Scholar]
- 44.Mahmoudian A, van Dieen JH, Bruijn SM, Baert IA, Faber GS, Luyten FP, Verschueren SM. Dynamic and static knee alignment at baseline predict structural abnormalities on MRI associated with medial compartment knee osteoarthritis after 2 years, Gait Posture 2017; 57: 46–51. doi: 10.1016/j.gaitpost.2017.05.024 [DOI] [PubMed] [Google Scholar]
- 45.Luyten FP, Denti M, Filardo G, Kon E, Engebretsen L. Definition and classification of early osteoarthritis of the knee. Knee Surg. Sports Traumatol Arthrosc 2012; 20: 401–406. doi: 10.1007/s00167-011-1743-2 [DOI] [PubMed] [Google Scholar]
- 46.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 1986; 29:1039–1049. [DOI] [PubMed] [Google Scholar]
- 48.De Groot IB, Favejee MM, Reijman M, Verhaar JA, Terwee CB. The Dutch version of the Knee Injury and Osteoarthritis Outcome Score: a validation study. Health Qual. Life Outcomes 2008; 6: 16 doi: 10.1186/1477-7525-6-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 2001; 286:188–195. [DOI] [PubMed] [Google Scholar]
- 50.Woltring HJ. A Fortran package for generalized, cross-validatory spline smoothing and differentiation. Adv Eng Softw 1986; 8:104–113. [Google Scholar]
- 51.Reid S, Stair negotiation in an older adult population: analysis of the lower limb (doctoral thesis). Queen’s University, 2010.
- 52.Shakoor N, Block JA. Walking barefoot decreases loading on the lower extremity joints in knee osteoarthritis. Arthritis Rheum 2006; 54:2923–2927. doi: 10.1002/art.22123 [DOI] [PubMed] [Google Scholar]
- 53.Bei Y, and Fregly BJ. Multibody dynamic simulation of knee contact mechanics. Med. Eng. Phys. 2004; 26:777–789. doi: 10.1016/j.medengphy.2004.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lenhart RL, Kaiser J, Smith CR, Thelen DG. Prediction and validation of load-dependent behavior of the tibiofemoral and patellofemoral joints during movement, Ann Biomed Eng. 2015; 43(11): 2675–2685. doi: 10.1007/s10439-015-1326-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Arnold E. M., Ward S. R., Lieber R. L., and Delp S. L. A model of the lower limb for analysis of human movement. Ann. Biomed. Eng. 38: 269–279, 2010. doi: 10.1007/s10439-009-9852-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Butler RJ, Barrios JA, Royer T, Davis IS. Frontal-plane gait mechanics in people with medial knee osteoarthritis are different from those in people with lateral knee osteoarthritis, Physical Therapy 2011; 91(8): 1235–1243. doi: 10.2522/ptj.20100324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kito N, Shinkoda K, Yamasaki T, Kanemura N, Anan M, Okanishi N, et al. Contribuition of knee adduction moment impulse to pain and disability in Japenese women with medial knee osteoarthritis, Clin Biomech 2010; 25: 914–919. [DOI] [PubMed] [Google Scholar]
- 58.Baliunas AJ, Hurwits DE, Ryals AB, Karrar A, Case JP, Block JA and Andriacchi TP. Increased knee joint loads during walking are present in subjects with knee osteoarthritis, Osteoarthr Cartil 2002; 10: 573–579. [DOI] [PubMed] [Google Scholar]
- 59.Astephen JL, Deluzio KJ, Caldwell GE, Dunhar MJ. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis, J Orthopaedic Res 2008; 332–341. [DOI] [PubMed] [Google Scholar]
- 60.Faul F, Erdfelder E, Lang A- G, and Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007; 39: 175–191. [DOI] [PubMed] [Google Scholar]
- 61.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 62.Andriacchi TP, Koo S, Scnlan SF. Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee, J Bone Joint Surg Am. 2009, 91 Suppl 1: 95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kutzner I, Heinlein B, Graichen F, Bender A, Rohlmann A, Halder A, Beier A, Bergmann, G. Loading of the knee joint during activities of daily living measured in vivo in five subjects, J Biomech 2010; 43: 2164–2173. doi: 10.1016/j.jbiomech.2010.03.046 [DOI] [PubMed] [Google Scholar]
- 64.Heinlein B, Kutzner I, Graichen F, Bender A, Rohlmann A, Halder AM, Beier A and Bergmann G. ESB clinical biomechanics award 2008: Complete data of total knee replacement loading for level walking and stair climbing measured in vivo with a follow-up of 6–10 months, Clin. Biomech. 2009; 24(4), 315–326. [DOI] [PubMed] [Google Scholar]
- 65.Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res 2002; 20(1):101e7. [DOI] [PubMed] [Google Scholar]
- 66.Fregly BJ, Reinbolt JA, Rooney KL, Mitchell KH, Chmielewski TL. Design of patient-specific gait modifications for knee osteoarthritis rehabilitation. IEEE Trans Biomed Eng 2007; 54:1687–1695. doi: 10.1109/TBME.2007.891934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Andriacchi TP, Natarajan RN, Hurwitz DE. Musculoskeletal dynamics, locomotion, and clinical applications In: Mow VC, Hayes WC, Eds. Basic Orthopaedic Biomechanics. Philadelphia: Lippincott-Raven; 1997; 37–68. [Google Scholar]
- 68.Baliunas A, Hurwitz D, Ryals A, Karrar A, Case JP, Block JA, Andriacchi TP. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage 2002; 10:573–579. [DOI] [PubMed] [Google Scholar]
- 69.Lewek M, Rudolph KS, Snyder-Mackler L. Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthr Cartil 2004; 12(9):745–51. doi: 10.1016/j.joca.2004.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Baudet A, Morisset C, d'Athis P, Maillefert JF, Casillas JM, Ornetti P, Laroche D. Cross-talk correction method for knee kinematics in gait analysis using principal component Analysis (PCA): A New Proposal. Plos One 2014; 9(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Marin F, Mannel H, Claes L, Dürselen L. Correction of axis misalignment in the analysis of knee rotations. Hum. Mov. Sci, 2003; 22, 285–296. [DOI] [PubMed] [Google Scholar]
- 72.Robinson MA and Vanrenterghem J. An evaluation of anatomical and functional knee axis definition in the context of side-cutting. J Biomech 2012; 45: 1941–46. doi: 10.1016/j.jbiomech.2012.05.017 [DOI] [PubMed] [Google Scholar]
- 73.Van Campen A, De Groote F, Bosmans L, Scheys L, Jonkers I, De Schutter J. Functional knee axis based on isokinetic dynamometry data: Comparison of two methods, MRI validation, and effect on knee joint kinematics. J Biomech 2011; 44: 2595–2600. doi: 10.1016/j.jbiomech.2011.08.022 [DOI] [PubMed] [Google Scholar]
- 74.Meireles S, De Groote F, Van Rossom S, Verschueren S and Jonkers I. Differences in knee adduction moment between healthy subjects and patients with osteoarthritis depend on the knee axis definition, Gait & Posture 53, 2017: 104–109. [DOI] [PubMed] [Google Scholar]
- 75.Dyrby CO, and Andriacchi TP. Secondary motions of the knee during weight bearing and non-weight bearing activities. J. Orthop. Res. 2004; 22:794–800. doi: 10.1016/j.orthres.2003.11.003 [DOI] [PubMed] [Google Scholar]
- 76.Li G, Rudy T, Sakane M, Kanamori A, Ma C, and Woo SLY. The importance of quadriceps and hamstring muscle loading on knee kinematics and in situ forces in the ACL. J. Biomech. 1999; 32: 395–400. [DOI] [PubMed] [Google Scholar]
- 77.Westphal CJ, Schmitz A, Reeder SB, and Thelen DG. Load-dependent variations in knee kinematics measured with dynamic MRI. J. Biomech. 2013; 46: 2045–2052. doi: 10.1016/j.jbiomech.2013.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Knoop J, van der Leeden M, van der Esch M, Thorstensson CA, Gerritsen M, Voorneman RE, Lems WF, Roorda LD, Dekker J, and Steultjens MP. Association of lower muscle strength with self-reported knee instability in osteoarthritis of the knee: results from the Amsterdam Osteoarthritis cohort. Arthritis Care Res 2012; 64 (1): 38–45. [DOI] [PubMed] [Google Scholar]
- 79.O’Reilly SC, Jones A, Muir KR, Doherty M. Quadriceps weakness in knee osteoarthritis: the effect on pain and disability, Ann Rheum Dis 1998; 57(10): 588–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Smith CR, Lenhart R, Kaiser J, Choi K, Thelen D. The effect of cartilage thickness on tibiofemoral contact pressure during gait, 2015 Annual Meeting of the Orthopaedic Research Society.
- 81.Hubley-Kozey C, Deluzio K, Dunbar M. Muscle co-activation patterns during walking in those with severe knee osteoarthritis. Clin Biomech 2008; 23:71–80. [DOI] [PubMed] [Google Scholar]
- 82.Schmitt LC, Rudolph KS. Muscle stabilization strategies in people with medial knee osteoarthritis: the effect of instability. J Orthop Res 2008; 26:1180–5. doi: 10.1002/jor.20619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.D’Lima DD, Patil S, Steklov N, Slamin JE, Colwell CW Jr. The Chitranjan Ranawat Award: in vivo knee forces after total knee arthroplasty. Clin Orthop Relat Res 2005; 440: 45–9. [DOI] [PubMed] [Google Scholar]
- 84.D’Lima DD, Patil S, Steklov N, Slamin JE, Colwell CW Jr. Tibial forces measured in vivo after total knee arthroplasty. J Arthroplasty 2006; 21: 255–62. doi: 10.1016/j.arth.2005.07.011 [DOI] [PubMed] [Google Scholar]
- 85.Mundermann A, Dyrby CO, D’Lima DD, Colwell CW Jr, Andriacchi TP. In vivo knee loading characteristics during activities of daily living as measured by an instrumented total knee replacement. J Orthop Res 2008; 26, 1167–1172. doi: 10.1002/jor.20655 [DOI] [PubMed] [Google Scholar]
- 86.Zhao D, Banks SA, D’Lima DD, Colwell CW, Fregly BJ. In vivo medial and lateral tibial loads during dynamic and high flexion activites. J Orthop Res 2007; 25, 593–602. doi: 10.1002/jor.20362 [DOI] [PubMed] [Google Scholar]
- 87.Benedetti MG, Catani F, Bilotta TW, Marcacci M, Mariani E, Giannini S. Muscle activation pattern and gait biomechanics after total knee replacement. Clin Biomech (Bristol, Avon) 2003; 18: 871–6. [DOI] [PubMed] [Google Scholar]
- 88.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech 2008; 23:320–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Richards C, and Higginson JS. Knee contact force in subjects with symmetrical OA grades: Differences between OA severities. J Biomech 2010; 43:2595–2600. doi: 10.1016/j.jbiomech.2010.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Winby CR, Lloyd DG, Besier TF, and Kirk TB. Muscle and external load contribution to knee joint contact loads during normal gait. J Biomech 2009; 42(14): 2294–2300. doi: 10.1016/j.jbiomech.2009.06.019 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The gray shaded area corresponds to the standard deviation of the control group. * indicates a significant difference between established OA and control groups. # indicates a significant difference between early OA and control group.
(TIF)
The gray shaded area corresponds to the standard deviation of the control group.
(TIF)
Peak and minima SS values of the KCF, KFM, KAM and KRM during the stance phase of gait, as well as rotation angles (RAngle in degrees). at the time instant of the first peak MKCF, for control (C0), early OA (EA) and established OA (ES) groups.
(DOCX)
Peak and SS values of the KCF, KFM and KAM during the stance phase of step-up-and-over for control (C0), early OA (EA) and established OA (ES) groups.
(DOCX)
First and second peaks of the KCF during gait, and minimum values during midstance (SS).
(DOCX)
First and second peaks of the KCF during step-up-and-over, and minimum values during midstance (SS) of step-up-and-over.
(DOCX)
Peaks of the KAM, KFM and KRM during gait, and minimum value during midstance (SS).
(DOCX)
Peaks of the KAM and KFM during step-up-and-over, and minimum value during midstance (SS).
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
Individual data points for each individual subject are provided in the paper's Supporting Information files (S3 Table, S4 Table, S5 Table, S6 Table, S7 Table and S8 Table). All motion data are available from Open Science Framework at the following URL: https://osf.io/8edy3/.