Abstract
Aims
Recent data from the National Cardiovascular Data Registry indicate that women with ST-segment-elevation myocardial infarction (STEMI) continue to have higher mortality and reported delays in treatment compared to men. We aimed to determine whether the sex difference in mortality exists when treatment disparities are reduced.
Methods and Results
Using a prospective regional percutaneous-coronary-intervention (PCI)-based STEMI system database with a standardized STEMI protocol, we evaluated baseline characteristics, treatment and clinical outcomes of STEMI patients stratified by sex. From March 2003 to January 2016, 4918 consecutive STEMI patients presented to the Minneapolis Heart Institute at Abbott Northwestern Hospital regional STEMI system including 1416 (28.8%) women. Compared to men, women were older (68.4 vs 60.9 years) with higher rates of hypertension (66.7 vs 55.7%), diabetes (21.7 vs 17.4%) and cardiogenic shock (11.5 vs 8.0%) (all P<0.001). Pre-revascularization medications and PCI were performed with same frequencies, but women were less likely to receive statin or anti-platelet therapy at discharge. After age-adjustment, women had similar in-hospital mortality to men (5.1% vs 4.8%, P=0.60), despite slightly longer door-to-balloon time (95 vs 92 mins, P=0.004). Five-year follow-up confirmed absence of a sex disparity in age-adjusted survival post-STEMI.
Conclusions
Previously reported treatment disparities between men and women are diminished in a regional PCI-based STEMI system using a standardized STEMI protocol. No sex differences in short-term or long-term age-adjusted mortality are present in this registry despite some treatment disparities. These results suggest that STEMI healthcare disparities and mortality in women can be improved using STEMI protocols and systems.
Keywords: ST-elevation myocardial infarction, mortality, women
Introduction
Ischemic heart disease is the leading cause of mortality in women and is associated with significant morbidity related to the clinical consequences of myocardial infarction (MI) and ischemia, such as heart failure1, 2. Women with ST-elevation myocardial infarction (STEMI) have worse short-term and long-term mortality than men, although these sex differences are often attributed to increased age and higher cardiovascular risk profile in women3–6. Nevertheless, young women <65 years have higher mortality post-STEMI than age-matched men despite a lower prevalence of obstructive coronary artery disease (CAD)4, 7. Treatment disparities have been implicated, since women are less likely to receive guideline-recommended pharmacotherapy and reperfusion therapy compared to men and have longer times to treatment8–14. In addition, sex differences in the pathophysiology of STEMI (such as coronary plaque erosion and abnormal coronary vasomotor function) may lead to differences in administration of and response to guidelines-based STEMI therapy15. Whether the higher mortality in women is related to these treatment disparities remains controversial. We sought to determine whether a standardized STEMI protocol and organized transfer system reduces treatment disparities in addition to short-term and long-term mortality in women vs men.
Methods
We studied patients enrolled from March 2003 to January 2016 in the Minneapolis Heart Institute STEMI system registry, which is a comprehensive, prospective database of STEMI patients who presented to the Minneapolis Heart Institute at Abbott Northwestern Hospital regional STEMI system16, 17. The Minneapolis Heart Institute Level 1 MI program is a PCI-based regional STEMI system which includes 31 community hospitals and 10 clinics in Minnesota and Wisconsin using a standardized protocol and organized transfer system, designed to improve time to treatment and clinical outcomes. The design of the system and initial results have been previously described16–20. In addition to the PCI center, patients are transferred from Zone 1 which includes 11 hospitals within 60 miles of the PCI center and Zone 2 with 20 hospitals between 60 and 210 miles away treated with a pharmaco-invasive protocol using half-dose fibrinolysis20. Standardized protocols including a transfer plan (ambulance or helicopter) were implemented for each site. We obtained Institutional Review Board approval for data collection, follow-up, and data analysis.
Inclusion criterion was STEMI or new left bundle-branch block in patients with chest pain less than 24-hour duration. No patients were excluded from the protocol unless reperfusion therapy was considered inappropriate, for example in end-stage dementia or metastatic cancer. All STEMI patients, including those with out-of-hospital cardiac arrest, cardiogenic shock, advanced age and initially nondiagnostic 12-lead ECGs, were included in the registry. Demographic information, cardiovascular risk factors, door-to-balloon time (arrival at referral hospital to balloon at PCI center), STEMI characteristics, treatment, and clinical outcomes were recorded and stratified by sex. Patients were followed up for 5 years for survival analysis.
Descriptive statistics are displayed as means and SDs for continuous variables; number and percentage with characteristic are given for categorical variables. When continuous variables had skewed distributions (door-to-balloon times and length of stay), data are summarized with medians and 25th and 75th percentiles. Categorical variables were analyzed using Pearson’s chi-square or Fisher’s exact tests. Continuous variables were analyzed using Student’s t-test for normally distributed variables or Wilcoxon rank-sum tests for continuous variables with non-normal distribution. A value of p<0.05 was considered significant, and p-values are two-sided where possible. For patients with known survival and event status, the fraction at each follow-up interval was estimated by Kaplan-Meier method. Cox regression models were used to adjust differences in age at presentation. Actual and expected surviving fractions were compared using the log-rank test. All statistical calculations and plots were done with Stata 14.1 (StataCorp. College Station, TX).
Results
Data from 4918 consecutive STEMI patients from March 2003 to January 2016 were analyzed including 28.8% women. Baseline characteristics for men and women are presented in Table 1. Women were older with higher rates of hypertension, diabetes, and cardiogenic shock but lower rates of prior smoking, history of CAD including previous MI and revascularization. Women had lower body mass index (BMI), peak creatine kinase (CK) and CK-MB levels. There were no significant sex differences in percentage of anterior MI or ejection fraction. Women were less likely to have a culprit artery (77.2% vs 83.3%, P<0.001) and consistent with this more frequently had TIMI 2/3 flow (54.8% vs 48.2%, P<0.001) at baseline angiography. There was no significant sex difference in pre-treatment with aspirin, thienopyridine, or other anti-thrombotic prior to PCI (Table 1).
Table 1.
Baseline demographic and angiographic information stratified by gender
| Men (n=3502) |
Women (n=1416) |
P-Value | |
|---|---|---|---|
| Age (Years), mean ± SD | 60.8 ± 13.3 | 68.4 ± 14.1 | <0.001 |
| BMI, mean ± SD | 29.1 ± 5.6 | 28.6 ± 7.2 | 0.002 |
| Hypertension, (%) | 1939 (55.7) | 934 (66.7) | <0.001 |
| Dyslipidemia, (%) | 1922 (56.1) | 754 (54.8) | 0.44 |
| Diabetes, (%) | 607 (17.4) | 305 (21.7) | <0.001 |
| History of CAD, (%) | 1102 (31.5) | 390 (27.7) | 0.009 |
| History of Stroke, (%) | 108 (3.1) | 55 (3.9) | 0.15 |
| History of Smoking, (%) | 2276 (65.5) | 728 (52.0) | <0.001 |
| Current Smoker, (%) | 1293 (37.2) | 421 (30.1) | <0.001 |
| History of PCI, (%) | 801 (23.0) | 253 (18.0) | <0.001 |
| History of MI, (%) | 761 (21.9) | 252 (17.9) | 0.002 |
| History of CABG, (%) | 275 (7.9) | 69 (4.9) | <0.001 |
| Killip Class | |||
| 1, (%) | 3079 (88.0) | 1169 (82.6) | <0.001 |
| 2/4, (%) | 419 (12.0) | 247 (17.4) | |
| Cardiac Arrest Pre-PCI, (%) | 374 (10.7) | 128 (9.0) | 0.084 |
| Cardiogenic Shock Pre-PCI, (%) | 281 (8.0) | 162 (11.5) | <0.001 |
| Anterior MI, (%) | 1234 (35.8) | 496 (35.4) | 0.78 |
| Ejection Fraction (%), mean ± SD | 47.9 ± 13.2 | 47.7 ± 14.7 | 0.52 |
| Culprit Artery | |||
| Graft, (%) | 86 (2.5) | 21 (1.5) | <0.001 |
| Left Main, (%) | 32 (0.9) | 16 (1.1) | |
| LAD, (%) | 1109 (31.7) | 409 (28.9) | |
| LCx, (%) | 432 (12.4) | 154 (10.9) | |
| RCA, (%) | 1257 (35.9) | 492 (34.8) | |
| None/Unknown/Unclear, (%) | 583 (16.7) | 323 (22.8) | |
| Peak CK mg/dl, median(25th, 75th percentile) | 819 (284, 1807) | 538 (182, 1516) | <0.001 |
| Peak CKMB mg/dl, median(25th, 75th percentile) | 77 (21, 183) | 54 (16, 160) | <0.001 |
| TIMI Flow Pre PCI | |||
| 0/1, (%) | 1712 (51.8) | 602 (45.2) | <0.001 |
| 2/3, (%) | 1594 (48.2) | 729 (54.8) | |
| TIMI Flow Post PCI | |||
| 0/1, (%) | 73 (2.2) | 30 (2.3) | 0.93 |
| 2/3, (%) | 3233 (97.8) | 1302 (97.8) | |
| Pre-Revascularization Medication | |||
| Aspirin, (%) | 3474 (97.7) | 1361 (97.1) | 0.29 |
| Anti-thrombotic*, (%) | 3243 (95.3) | 1299 (95.4) | 0.86 |
| Thienopyridine, (%) | 1377 (93.9) | 566 (93.3) | 0.60 |
BMI = body mass index; CAD = coronary artery disease; PCI = percutaneous coronary intervention; MI = myocardial infarction; CABG = coronary artery bypass graft; LAD = left anterior descending; CK = creatine kinase; CKMB = creatine kinase MB
includes unfractionated heparin, low-molecular-weight heparin, or bivaluridin
When a culprit artery was identified, women had similar rates of PCI performed compared to men (94.4% vs 95.6%, P=0.10) but had longer door-to-balloon time (median 61 vs 55 minutes at a PCI facility, P<0.001; median 99 vs 94 at a Zone 1 facility, P<0.001) (Table 2). There was no significant sex difference in door-to-balloon time at the Zone 2 facility (median 124 vs 121, P=0.21). Overall, door-to-balloon within goal was achieved in fewer women than men for PCI and Zone 1 facilities, but not significantly different for Zone 2 facilities. The median length of stay was not clinically significantly different between women and men (3 days for both). Women who received PCI were slightly less likely to be discharged on an aspirin, statin, and other anti-platelet agent, compared to men (Table 2).
Table 2.
Clinical Outcomes
| Men (n=3502) |
Women (n=1416) |
P-Value | |
|---|---|---|---|
| *Intervention Performed, (%) | 2792 (95.6) | 1032 (94.4) | 0.10 |
| Length-of-stay (days) | 3 (2, 4) | 3 (2,5) | <0.001 |
| Door-to-Balloon (mins), median(25th, 75th percentile) | |||
| PCI Facility | 55 (40, 75) | 61 (44, 86) | <0.001 |
| Zone 1 | 94 (80, 117) | 99 (84, 124) | <0.001 |
| Zone 2 | 121 (100, 147) | 124 (101, 158) | 0.21 |
| PCI Door-to-Balloon ≤ 90 minutes, (%) | 789 (86.2) | 323 (79.0) | 0.001 |
| Zone 1 Door-to-Balloon ≤ 120 minutes, (%) | 1231 (78.3) | 424 (72.2) | 0.003 |
| Zone 2 Received fibrinolytic or Door-to-Balloon ≤ 120 minutes, (%) | 804 (84.2) | 319 (80.6) | 0.11 |
| Discharge Medications† | |||
| Aspirin, (%) | 2660 (98.3) | 948 (97.1) | 0.032 |
| Beta Blocker, (%) | 2569 (95.0) | 920 (94.6) | 0.55 |
| Statin, (%) | 2541 (93.9) | 889 (91.2) | 0.004 |
| Thienopyridine, (%) | 2636 (97.4) | 935 (95.7) | 0.009 |
Percent based on patients with a known culprit artery
Percent based on patients who received intervention
Compared to men, women had higher rates of unadjusted in-hospital mortality (7.6% vs 5.2%, P=0.001) and 30-day mortality (8.4% vs 5.9%, P=0.001) (Table 3). There were no significant sex differences in 30-day outcomes for myocardial infarction, stroke, and revascularization.
Table 3.
In-hospital and 30 Day Outcomes
| Men (n=3502) |
Women (n=1416) |
P-Value | |
|---|---|---|---|
| Unadjusted Outcomes | |||
| In-hospital Death | 181 (5.2) | 108 (7.6) | 0.001 |
| 30 Day Outcomes | |||
| Myocardial Infarction, (%) | 48 (1.4) | 18 (1.3) | 0.78 |
| Stroke, (%) | 32 (0.9) | 20 (1.4) | 0.12 |
| Revascularization, (%) | 62 (1.8) | 23 (1.6) | 0.72 |
| Death, (%) | 207 (5.9) | 119 (8.4) | 0.001 |
| MACE (%) | 273 (7.8) | 150 (10.6) | 0.002 |
| Age-Adjusted Outcomes* | |||
| In-hospital Death | 4.8% (4.1 – 5.6) | 5.1% (4.1 – 6.3) | 0.66 |
| 30 Day Outcomes | |||
| Myocardial Infarction, (%) | 1.4% (1.0 – 1.8) | 1.3% (0.8 – 2.0) | 0.82 |
| Stroke, (%) | 0.9% (0.6 – 1.3) | 1.1% (0.7 – 1.8) | 0.45 |
| Revascularization, (%) | 1.8% (1.4 – 2.3) | 1.6% (1.1 – 2.5) | 0.75 |
| Death, (%) | 5.4% (4.7 – 6.6) | 5.4% (4.3 – 6.6) | 0.90 |
| MACE, (%) | 7.6% (6.7 – 8.5) | 7.8% (6.5 – 9.3) | 0.76 |
MACE= major adverse cardiac outcomes (myocardial infarction, stroke, or death);
Reported as Point Estimate (95% CI)
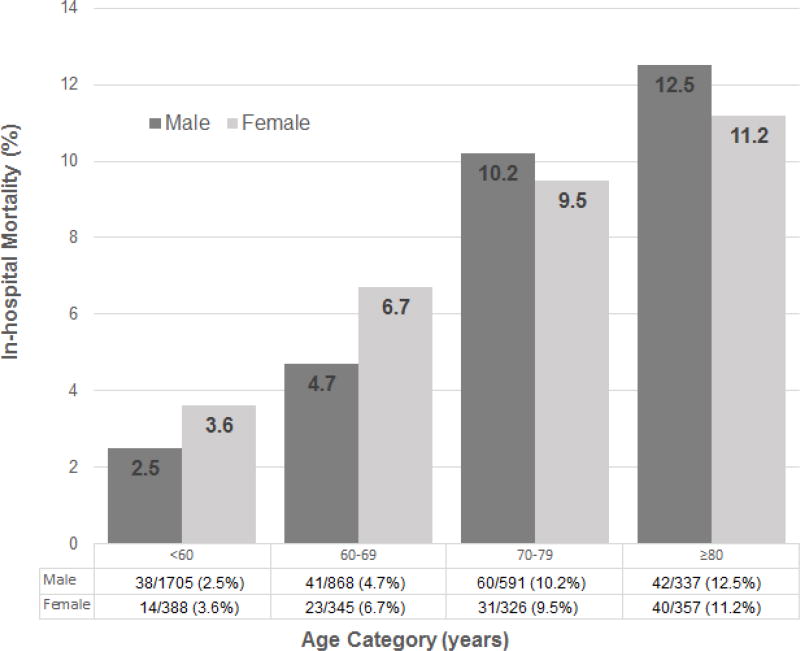
After age-adjustment, women continued to have similar outcomes to men including revascularization (95% vs 96%, P=0.43) and length of stay (2.9 vs 2.7 days, P=0.093), although door-to-balloon time (95 vs 92 minutes, P=0.004) and percentage of goal door-to-balloon ≤ 120 mins (71% vs 74%, P=0.04) remained slightly worse for women compared to men. In-hospital mortality was no longer significantly different when adjusted for age (5.1% vs 4.8%, P=0.60). Age-stratification demonstrated that in-hospital mortality was highest in the group of men and women age ≥80 years (Figure 1), but there was no significant sex difference in in-hospital mortality within each age sub-group, including young patients <60 years old. In addition, based on a multivariate model, female sex was not a significant predictor of in-hospital mortality (HR 1.042, 95% CI 0.860–1.261; P=0.68). Five-year follow-up data confirmed the absence of sex disparity in survival post-STEMI with age-adjustment (log-rank test: P=0.35) (Figure 2).
Figure 1. In-Hospital Mortality Stratified by Patient Age and Sex.
Age-stratification demonstrated that in-hospital mortality was not significantly different between women and men across age groups.
Figure 2. Age-Adjusted Mortality To Five Years Stratified by Sex.
Five-year follow-up confirmed absence of a sex disparity in survival post-STEMI.
Discussion
In this study, we demonstrate that in a regional PCI-based STEMI system using a standardized STEMI protocol and organized transfer system, treatment disparities in door-to-balloon time and discharge medications remained slightly worse for women compared to men, but prior reported sex disparities in STEMI in-hospital and five-year follow-up mortality are not observed when adjusted for age. Female sex was not a significant predictor of mortality in a multivariate model, suggesting that biological sex differences are not a major factor in the sex disparity in post-STEMI mortality when using a standardized PCI-based STEMI protocol. These results are important, as the recently published STEMI data from the National Cardiovascular Data Registry (NCDR) Acute Coronary Treatment and Intervention Outcomes Network Registry—Get With The Guidelines (ACTION-GWTG) demonstrated that 1) median contact-to-device time remains longer in women than men, 2) 32.5% of female STEMI patients did not meet the recommended target time ≤90 minutes compared with 24.4% of male patients, 3) longer reperfusion time was associated with increased mortality for both women and men, and importantly 4) adjusted mortality rate was higher in female STEMI patients than male STEMI patients12. We demonstrate that in a PCI-based STEMI system using a standardized STEMI protocol and reduced treatment disparities, female sex is no longer a predictor of mortality.
Sex differences in reperfusion time
Our findings are pertinent given the recent findings from two studies of contemporary young STEMI patients: 1) the “Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients” (VIRGO) study, which identified sex disparities in 1238 young patients (<55 years) with STEMI eligible for reperfusion from 2008 to 2012 in the United States11, and 2) the Nationwide Inpatient Sample database, which evaluated 632,930 patients <60 years with STEMI from 2004–2011 in the United States21. These two studies demonstrated that young women with STEMI were less likely to undergo coronary angiography and less likely to receive revascularization compared with young men in the United States. Of the patients who received revascularization, young women also experienced more delays in reperfusion than men, despite adjustment for sociodemographics, comorbidities, and clinical factors, with the most significant sex-specific delays being door-to-needle time for fibrinolytic therapy and door-to-balloon times for patients being transferred for PCI. In VIRGO, recommended timeframe guidelines were exceeded in more women than men, particularly for the transfer patients (door-to-balloon >120 min: 67% vs 44%, P<0.001)11. Older age is a known independent predictor of achieving goal reperfusion time13, which suggests a delay in younger patients —a group that may be more susceptible to sex-differences22.
Standardized protocols have been shown to improve reperfusion times with integrated transfer systems, which may in turn decrease sex discrepancy in reperfusion time16, 23. In the HORIZONS-AMI randomized trial of patients with STEMI undergoing primary PCI, door-to-balloon time was not significantly different in women vs men (102 vs 98 mins, P=0.19)24. Unfortunately, recent evaluation of over 14,000 STEMI patients in the NCDR ACTION-GWTG database showed that first medical contact to device time ≤ 120 minutes was not achieved in 35% patients who require transfer for primary PCI, even when restricting analysis to patients who are within 60-minutes of the PCI center13. In our study of the Minneapolis Heart Institute STEMI system registry, we identified minimal sex differences in door-to-balloon time and percentage of door-to-balloon within goal, but we had lower percentage of men (21.7%) and women (27.8%) surpassing door-to-balloon >120 min in Zone 1. This demonstrates that a standardized STEMI system reduces reperfusion delays and likely contributes to improved STEMI outcomes for women.
Reperfusion time and mortality
The sex disparities in reperfusion time for young STEMI patients may explain why these prior studies have shown a higher mortality in young women with STEMI than men. The VIRGO analysis found that 1-month and 1-year mortality rate was higher in young patients who exceeded the recommended reperfusion goals (including nontransfer and transfer door-to-balloon times for PCI and fibrinolysis door-to-needle times) than patients who met the recommended reperfusion guidelines, although the mortality rates were low and thus could not be adjusted for sex or age. The Zwolle Myocardial Infarction Study Registry, which studied 6746 STEMI patients referred for primary PCI from 1998–2008 in the Netherlands, also demonstrated sex differences in reperfusion time and 1-year mortality in young patients <65 years4. While our study is underpowered for analysis of sex-differences in young STEMI patients, we did not see a statistically significant sex difference in mortality for patients <60 years old.
Improved reperfusion times translate to lower mortality rates24–26. In our analysis of the Minneapolis Heart Institute regional STEMI system database, we did not find a significant sex difference for in-hospital mortality or 5-year mortality when adjusted for age. The lack of significant sex differences when stratified by age may be due to the standardized treatment strategies with very high rates of guideline based medications pre-revascularization and at discharge, although we did find a slightly lower percentage of women receiving statin, aspirin, and other anti-platelet agents at discharge. Our findings are consistent with those of the HORIZONS-AMI trial, which determined that female sex was not an independent predictor of long-term major adverse cardiovascular events at 3 years after adjusting for differences in baseline and treatment characteristics24.
Sex differences in cardiovascular risk markers and post-discharge management
While the studies above emphasize sex differences in reperfusion as important modifiable predictors of STEMI mortality, sex-related differences in cardiovascular risk markers should not be dismissed as factors contributing to mortality and post-discharge treatment disparities. Our finding that women with STEMI have poorer baseline cardiovascular risk profile (specifically hypertension and diabetes) is consistent with prior studies and may be related to age27. Nevertheless, sex-related biological differences include increased mortality associated with diabetes and higher risk of ischemic heart disease if smoking28. Sex-differences in cardiac enzymes and STEMI symptoms may also contribute to suboptimal prediction of a woman’s STEMI risk –and thus STEMI management29. Given the lower total infarct size (as measured by CKMB) and the higher pre-PCI TIMI flow in women, women may be expected to have lower mortality than men. However, women had a smaller BMI than men, and the post-PCI TIMI flow rates were not different between women and men in our study. Women have also been reported to have worse morbidity than men following STEMI, including short-term and long-term bleeding and major adverse cardiovascular events24. Finally, female sex has also been associated with the underutilization of ACE inhibitors, beta-blockers, statin, and cardiac rehabilitation utilization post-MI2. Indeed, of the patients who received PCI in our STEMI registry, guidelines-based pharmacotherapies (antiplatelet and statin) were less frequently prescribed in women compared to men at the time of discharge. We did not determine whether sex differences in bleeding complications, cholesterol levels, or statin intolerance contributed to the mild disparity in discharge prescription rates of these guidelines-based pharmacotherapies. Although we did not find a difference in age-adjusted 30-day or 5-year mortality, physicians and the community should be educated regarding sex-related differences in cardiovascular risk, morbidity and pharmacotherapy to ultimately improve long-term cardiovascular outcomes30, 31.
Limitations
Since our study included only STEMI patients enrolled in the registry, we do not have a contemporary control group that did not participate in the standardized STEMI protocol. Thus, our comparison of sex disparities are based on historic control data from prior published STEMI studies. We also did not perform subgroup analysis for STEMI patients younger than 60 given the small sample size in this age group. All patients with STEMI were included in our outcomes analysis, including patients with coronary artery spasm, Takotsubo cardiomyopathy, and spontaneous coronary artery dissection, which are conditions that are more common in women and may have different management and prognosis compared to STEMI from ruptured plaque32–36. Treatment times are also included for all patients including complex situations such as patients who developed ST-elevation after the initial EKG or patients with prolonged resuscitation. There is a possible oversampling of men, as there were approximate 2.5× more men than women in our registry. However, this is consistent with the proportion of women in other STEMI registries. In addition, race and ethnicity were typical of a Minnesota population (95% white, 2–3% African American, 1% Asian, 1% Hispanic, and ~1% other). While there was no statistical difference across groups, the demographics of our population may not be reflective of the United States population. Finally, our 5-year survival analysis was adjusted for age and not adjusted for other baseline characteristics.
Conclusions
The previously reported treatment disparities between men and women are diminished in a regional PCI-based STEMI system using a standardized STEMI protocol, with no sex differences in age-adjusted mortality. These results suggest that STEMI healthcare disparities and mortality in women can be improved using STEMI protocols and systems. Larger datasets with fully risk-adjusted models and longer follow-up are needed to assess mortality differences in younger women and longer term mortality.
Acknowledgments
Funding:
This work was supported by contracts from the National Heart, Lung and Blood Institutes [K23HL105787 and T32HL116273]; grants from the Edythe L. Broad and the Constance Austin Women’s Heart Research Fellowships, Cedars-Sinai Medical Center, Los Angeles, California; the Barbra Streisand Women’s Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest:
Wei J, Grey E, Garberich RF: none declared; Mehta PK: Research/Research Grants - General Electric, Gilead; Hauser RG: Officer, Director, Trustee, or Other Fiduciary Role - Cardiac Insights; Bairey Merz CN: Consultant Fees/Honoraria – Lecture (AACE, AAC-AZ, Florida Hospital, Mayo, NAMS, Practice Point Communications, Pri-Med) Scripps Clinic, Vox Media, VBWG, ULCA, University of Chicago, Northwestern, Radcliffe Institute, UCSF), Consulting (Amgen, Medscape, Pfizer); Grant Review (Gilead, NIH-SEP); Research/Research Grants (FAMRI, Microvascular, Normal Control, RWISE, WISE CVD); Henry TD: none declared.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics C, Stroke Statistics S. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wenger NK. Women and coronary heart disease: a century after Herrick: understudied, underdiagnosed, and undertreated. Circulation. 2012;126(5):604–11. doi: 10.1161/CIRCULATIONAHA.111.086892. [DOI] [PubMed] [Google Scholar]
- 3.Jneid H, Fonarow GC, Cannon CP, Hernandez AF, Palacios IF, Maree AO, Wells Q, Bozkurt B, Labresh KA, Liang L, Hong Y, Newby LK, Fletcher G, Peterson E, Wexler L Get With the Guidelines Steering C, Investigators. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118(25):2803–10. doi: 10.1161/CIRCULATIONAHA.108.789800. [DOI] [PubMed] [Google Scholar]
- 4.Otten AM, Maas AH, Ottervanger JP, Kloosterman A, van 't Hof AW, Dambrink JH, Gosselink AT, Hoorntje JC, Suryapranata H, de Boer MJ Zwolle Myocardial Infarction study G. Is the difference in outcome between men and women treated by primary percutaneous coronary intervention age dependent? Gender difference in STEMI stratified on age. European heart journal Acute cardiovascular care. 2013;2(4):334–41. doi: 10.1177/2048872612475270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaccarino V, Horwitz RI, Meehan TP, Petrillo MK, Radford MJ, Krumholz HM. Sex differences in mortality after myocardial infarction: evidence for a sex-age interaction. Archives of internal medicine. 1998;158(18):2054–62. doi: 10.1001/archinte.158.18.2054. [DOI] [PubMed] [Google Scholar]
- 6.Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, Goldberg RJ. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Annals of internal medicine. 2001;134(3):173–81. doi: 10.7326/0003-4819-134-3-200102060-00007. [DOI] [PubMed] [Google Scholar]
- 7.Shao YH, Croitor SK, Moreyra AE, Wilson AC, Kostis WJ, Cosgrove NM, Kostis JB, Group MS. Comparison of hospital versus out of hospital coronary death rates in women and men. The American journal of cardiology. 2010;106(1):26–30. doi: 10.1016/j.amjcard.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 8.Kaul P, Armstrong PW, Sookram S, Leung BK, Brass N, Welsh RC. Temporal trends in patient and treatment delay among men and women presenting with ST-elevation myocardial infarction. American heart journal. 2011;161(1):91–7. doi: 10.1016/j.ahj.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 9.Radovanovic D, Nallamothu BK, Seifert B, Bertel O, Eberli F, Urban P, Pedrazzini G, Rickli H, Stauffer JC, Windecker S, Erne P Investigators AP. Temporal trends in treatment of ST-elevation myocardial infarction among men and women in Switzerland between 1997 and 2011. European heart journal Acute cardiovascular care. 2012;1(3):183–91. doi: 10.1177/2048872612454021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawesson SS, Alfredsson J, Fredrikson M, Swahn E. Time trends in STEMI--improved treatment and outcome but still a gender gap: a prospective observational cohort study from the SWEDEHEART register. BMJ open. 2012;2(2):e000726. doi: 10.1136/bmjopen-2011-000726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D'Onofrio G, Safdar B, Lichtman JH, Strait KM, Dreyer RP, Geda M, Spertus JA, Krumholz HM. Sex differences in reperfusion in young patients with ST-segment-elevation myocardial infarction: results from the VIRGO study. Circulation. 2015;131(15):1324–32. doi: 10.1161/CIRCULATIONAHA.114.012293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roswell RO, Kunkes J, Chen AY, Chiswell K, Iqbal S, Roe MT, Bangalore S. Impact of Sex and Contact-to-Device Time on Clinical Outcomes in Acute ST-Segment Elevation Myocardial Infarction-Findings From the National Cardiovascular Data Registry. J Am Heart Assoc. 2017;6(1) doi: 10.1161/JAHA.116.004521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dauerman HL, Bates ER, Kontos MC, Li S, Garvey JL, Henry TD, Manoukian SV, Roe MT. Nationwide Analysis of Patients With ST-Segment-Elevation Myocardial Infarction Transferred for Primary Percutaneous Intervention: Findings From the American Heart Association Mission: Lifeline Program. Circulation Cardiovascular interventions. 2015;8(5) doi: 10.1161/CIRCINTERVENTIONS.114.002450. [DOI] [PubMed] [Google Scholar]
- 14.Johnston N, Bornefalk-Hermansson A, Schenck-Gustafsson K, Held C, Goodman SG, Yan AT, Bierman AS. Do clinical factors explain persistent sex disparities in the use of acute reperfusion therapy in STEMI in Sweden and Canada? European heart journal Acute cardiovascular care. 2013;2(4):350–8. doi: 10.1177/2048872613496940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaw LJ, Bugiardini R, Merz CN. Women and ischemic heart disease: evolving knowledge. Journal of the American College of Cardiology. 2009;54(17):1561–75. doi: 10.1016/j.jacc.2009.04.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henry TD, Sharkey SW, Burke MN, Chavez IJ, Graham KJ, Henry CR, Lips DL, Madison JD, Menssen KM, Mooney MR, Newell MC, Pedersen WR, Poulose AK, Traverse JH, Unger BT, Wang YL, Larson DM. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116(7):721–8. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 17.Rokos IC, Larson DM, Henry TD, Koenig WJ, Eckstein M, French WJ, Granger CB, Roe MT. Rationale for establishing regional ST-elevation myocardial infarction receiving center (SRC) networks. American heart journal. 2006;152(4):661–7. doi: 10.1016/j.ahj.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 18.Henry TD, Unger BT, Sharkey SW, Lips DL, Pedersen WR, Madison JD, Mooney MR, Flygenring BP, Larson DM. Design of a standardized system for transfer of patients with ST-elevation myocardial infarction for percutaneous coronary intervention. American heart journal. 2005;150(3):373–84. doi: 10.1016/j.ahj.2005.01.059. [DOI] [PubMed] [Google Scholar]
- 19.Smith LG, Duval S, Tannenbaum MA, Johnson Brown S, Poulose AK, Iannone LA, Larson DM, Ghali MG, Henry TD. Are the results of a regional ST-elevation myocardial infarction system reproducible? The American journal of cardiology. 2012;109(11):1582–8. doi: 10.1016/j.amjcard.2012.01.382. [DOI] [PubMed] [Google Scholar]
- 20.Larson DM, Duval S, Sharkey SW, Garberich RF, Madison JD, Stokman PJ, Dirks TG, Westin RK, Harris JL, Henry TD. Safety and efficacy of a pharmaco-invasive reperfusion strategy in rural ST-elevation myocardial infarction patients with expected delays due to long-distance transfers. European heart journal. 2012;33(10):1232–40. doi: 10.1093/eurheartj/ehr403. [DOI] [PubMed] [Google Scholar]
- 21.Khera S, Kolte D, Gupta T, Subramanian KS, Khanna N, Aronow WS, Ahn C, Timmermans RJ, Cooper HA, Fonarow GC, Frishman WH, Panza JA, Bhatt DL. Temporal Trends and Sex Differences in Revascularization and Outcomes of ST-Segment Elevation Myocardial Infarction in Younger Adults in the United States. Journal of the American College of Cardiology. 2015;66(18):1961–72. doi: 10.1016/j.jacc.2015.08.865. [DOI] [PubMed] [Google Scholar]
- 22.Mossong J, Grapsa E, Tanser F, Barnighausen T, Newell ML. Modelling HIV incidence and survival from age-specific seroprevalence after antiretroviral treatment scale-up in rural South Africa. Aids. 2013;27(15):2471–9. doi: 10.1097/01.aids.0000432475.14992.da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jollis JG, Roettig ML, Aluko AO, Anstrom KJ, Applegate RJ, Babb JD, Berger PB, Bohle DJ, Fletcher SM, Garvey JL, Hathaway WR, Hoekstra JW, Kelly RV, Maddox WT, Jr, Shiber JR, Valeri FS, Watling BA, Wilson BH, Granger CB Reperfusion of Acute Myocardial Infarction in North Carolina Emergency Departments I. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. Jama. 2007;298(20):2371–80. doi: 10.1001/jama.298.20.joc70124. [DOI] [PubMed] [Google Scholar]
- 24.Yu J, Mehran R, Grinfeld L, Xu K, Nikolsky E, Brodie BR, Witzenbichler B, Kornowski R, Dangas GD, Lansky AJ, Stone GW. Sex-based differences in bleeding and long term adverse events after percutaneous coronary intervention for acute myocardial infarction: three year results from the HORIZONS-AMI trial. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2015;85(3):359–68. doi: 10.1002/ccd.25630. [DOI] [PubMed] [Google Scholar]
- 25.Lambert L, Brown K, Segal E, Brophy J, Rodes-Cabau J, Bogaty P. Association between timeliness of reperfusion therapy and clinical outcomes in ST-elevation myocardial infarction. Jama. 2010;303(21):2148–55. doi: 10.1001/jama.2010.712. [DOI] [PubMed] [Google Scholar]
- 26.Rathore SS, Curtis JP, Chen J, Wang Y, Nallamothu BK, Epstein AJ, Krumholz HM National Cardiovascular Data R. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. Bmj. 2009;338:b1807. doi: 10.1136/bmj.b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pancholy SB, Shantha GP, Patel T, Cheskin LJ. Sex differences in short-term and long-term all-cause mortality among patients with ST-segment elevation myocardial infarction treated by primary percutaneous intervention: a meta-analysis. JAMA internal medicine. 2014;174(11):1822–30. doi: 10.1001/jamainternmed.2014.4762. [DOI] [PubMed] [Google Scholar]
- 28.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB American Heart Association Statistics C, Stroke Statistics S. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 29.Agrawal S, Van Eyk J, Sobhani K, Wei J, Bairey Merz CN. Sex, Myocardial Infarction, and the Failure of Risk Scores in Women. Journal of women's health. 2015;24(11):859–61. doi: 10.1089/jwh.2015.5412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wenger NK. Disparities in ST-elevation myocardial infarction management for the young goose and young gander: clinical, organizational, and educational challenges. Circulation. 2015;131(15):1310–2. doi: 10.1161/CIRCULATIONAHA.115.015855. [DOI] [PubMed] [Google Scholar]
- 31.Wei J, Henry TD. Gender equity in STEMI: not so simple! Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2015;85(3):369–70. doi: 10.1002/ccd.25800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, Lindley KJ, Vaccarino V, Wang TY, Watson KE, Wenger NK American Heart Association Cardiovascular Disease in W, Special Populations Committee of the Council on Clinical Cardiology CoE, Prevention CoC, Stroke N, Council on Quality of C, Outcomes R. Acute Myocardial Infarction in Women: A Scientific Statement From the American Heart Association. Circulation. 2016;133(9):916–47. doi: 10.1161/CIR.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 33.Crea F, Battipaglia I, Andreotti F. Sex differences in mechanisms, presentation and management of ischaemic heart disease. Atherosclerosis. 2015;241(1):157–68. doi: 10.1016/j.atherosclerosis.2015.04.802. [DOI] [PubMed] [Google Scholar]
- 34.Lindahl B, Baron T, Erlinge D, Hadziosmanovic N, Nordenskjold AM, Gard A, Jernberg T. Medical Therapy for Secondary Prevention and Long-Term Outcome in Patients with Myocardial Infarction with Non-Obstructive Coronary Artery (MINOCA) Disease. Circulation. 2017 doi: 10.1161/CIRCULATIONAHA.116.026336. [DOI] [PubMed] [Google Scholar]
- 35.Ishii M, Kaikita K, Sato K, Yamanaga K, Miyazaki T, Akasaka T, Tabata N, Arima Y, Sueta D, Sakamoto K, Yamamoto E, Tsujita K, Yamamuro M, Kojima S, Soejima H, Hokimoto S, Matsui K, Ogawa H. Impact of aspirin on the prognosis in patients with coronary spasm without significant atherosclerotic stenosis. Int J Cardiol. 2016;220:328–32. doi: 10.1016/j.ijcard.2016.06.157. [DOI] [PubMed] [Google Scholar]
- 36.Niccoli G, Scalone G, Crea F. Acute myocardial infarction with no obstructive coronary atherosclerosis: mechanisms and management. European heart journal. 2015;36(8):475–81. doi: 10.1093/eurheartj/ehu469. [DOI] [PubMed] [Google Scholar]