Abstract
Background
The rapid advancement in telecommunications on the African continent has opened up avenues for improving medical care to underserved populations. Although the greatest burden of neurological disorders is borne by Low-and-Middle Income Countries (LMICs) including sub-Saharan Africa (SSA), there is a profound paucity of neurologists to serve the population. Telemedicine presents a promising avenue for effective mobilization and utilization of the few neurologists in Africa.
Objective
To systematically review the published literature on the use of telemedicine for improved care and outcomes for patients with neurological disorders in SSA.
Methods
We searched PubMed and Cochrane library from January 1, 1980 to April 30, 2017 using the following keywords: “Telemedicine neurology Africa”, “Teleneurology Africa”, “Telestroke Africa”, “Telerehabilitation Africa”, “Telemedicine for epilepsy”, Telemedicine for Parkinson’s disease Africa”, “Telemedicine for dementia Africa”, “Telehealth neurology Africa”. Our inclusion criteria were randomized controlled trials, or case series that reported the utilization of telemedicine for care/education of individuals with neurological disorders in Sub-Saharan Africa.
Results
This search yielded 6 abstracts. By consensus between two investigators, 1 publication met the criteria for inclusion and further review. The one study identified utilized telemedicine for the purpose of improving education/knowledge of 16 doctors and 17 allied health professionals in Parkinson’s disease (PD) in Cameroon. The study noted feasibility and satisfaction of participants with telemedicine as well as improved knowledge base of participants after the educational course but noted access to healthcare by patients did not change. No studies have evaluated the use of telemedicine for care of patients with neurological disorders.
Conclusion
The indication is that teleneurology may be feasible in SSA and studies are needed to assess feasibility, acceptability, efficacy, cost-effectiveness of this promising discipline of neurology in these resource-limited settings. We propose the setting up of trans-continental, inter-regional, intra-regional, and national networks of neurologists to utilize teleneurology platforms to improve the reach of neurology care in SSA.
INTRODUCTION
The World Health Organization estimates 12 out of 100 deaths globally is the result of a neurological disorder. (1) Neurological disorders account for between 4.5–11% of illnesses depending on income status of nations. (1) The greatest burden of neurological disorders is borne by Low- and Middle Income Countries (LMICs) yet qualified health personnel are sorely lacking which undoubtedly contribute to sub-optimal care and poor outcomes. For instance, the neurologist-to-population ratio is 0.3/1,000,000 in Africa, where the few available neurologists are concentrated within cities. (2) These dare statistics coupled with non-existent neurology training programs in many LMICs requires novel approaches for using the scanty human resources available in these settings to address the ever widening gap between the growing burden of neurologic diseases and qualified neurologists.
One promising avenue for effective mobilization and utilization of the few neurologists available in LMICs is via the agency of telemedicine. Telemedicine is the use of telecommunication to provide medical information and services and it improves the efficiency or effectiveness of existing services. (3) Neurology telemedicine, also known as “teleneurology” has many potential benefits including increased practice outreach, decreased travel time and expenses for patients and doctors, expansion of educational opportunities and continuing medical education for physicians, individual and group education for patients about their neurologic diseases (4). The typical formats for delivery of telemedicine have included videoconferencing systems (real-time, synchronous) or store-and-forward systems (asynchronous). In the developed world setting, telemedicine has been utilized particularly for stroke as well as other disciplines of neurology and allied specialties such as dementia, (5) neuro-oncology, (6) neurocritical care, (7) migraine, (8) multiple sclerosis, (9) epilepsy, (10) Parkinson’s disease, (11) neurosurgery, (12) neuropathology, (13) psychiatry. (14).
What makes teleneurology a promising option for improving care of patients with neurological disorders in sub-Saharan Africa? Firstly, there has been an astronomical expansion in telecommunication infrastructure over the last two decades with internet services and mobile phone penetration reported to be about 75% among adults and about 35% ownership of Smartphones (15–17). Secondly, specialized care in neurology in most LMICs are restricted to a few Teaching or tertiary centers with limited access to care by the majority of the population who are resident in rural areas. Thirdly, in the developed world settings, teleneurology has been shown to be an effective model in bridging the rural-urban gap in access to specialized neurology services; a model which could be adopted, refined and culturally-tailored to suit the needs of SSA.
The objective of this systematic review is to assess the feasibility, acceptability, and efficacy of tele-medicine for care of patients with neurological disorders in SSA.
METHODS
We searched PubMed and Cochrane Library from January 1, 1980 to April 30, 2017 using the following keywords: “Telemedicine neurology Africa”, “Teleneurology Africa”, “Telestroke Africa”, “Telerehabilitation Africa”, “Telemedicine for epilepsy”, Telemedicine for Parkinson’s disease Africa”, “Telemedicine for dementia Africa”, “Telehealth neurology Africa”. We employed a systematic search methodology and study selection process. Our inclusion criteria were randomized controlled trials, or case series that reported the utilization of telemedicine for care/education of individuals with neurological disorders in Sub-Saharan Africa.
Exclusion criteria
Literature reviews, meta-analysis, commentaries, concept papers on Telemedicine for neurology in sub-Saharan Africa. The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement was followed for the systematic review. The articles included in this study underwent independent appraisal, data abstraction by 2 investigators (S.A. and D.A.) and F.S.S. served as arbiter for consensus.
RESULTS
The search identified 6 abstracts with one study meeting the criteria for inclusion for review. One study used telemedicine for education on Parkinson’s disease education doctors and allied health professionals. The aim of the study by Cubo et al. was to access the feasibility, satisfaction, pre-post course medical knowledge improvements and patient’s access of a tele-education program for healthcare providers in Cameroon. The participants included 16 doctors and 17 allied health professionals who were exposed to remotely administered courses on Parkinson’s disease by 18 experts. Twenty lectures over the period of 12 months were administered by movement disorder experts via live, synchronous video conferences with teaching materials provided to participants. Videoconference completion rates were 80%, participation rates ranged between 20% to 70% and satisfaction level at least above average was reported in 70%. The authors noted a significant improvement in medical knowledge however that post-course patient access was not significantly changed. The authors concluded that telemedicine for education of health professionals is feasible in Africa but access of patients with Parkinson’s disease for improved care of trained health professional needed improvement and testing. (18)
DISCUSSION
This systematic review identified one study in SSA that utilized telemedicine for the purposes of educating health professional to improve their knowledge base in Parkinson’s disease. SSA is bracing itself for an upsurge in neurodegenerative diseases mainly dementia from Alzheimer’s disease, vascular cognitive impairment and Parkinson’s disease (PD) due to increasing age of its population. The hundreds of thousands patients with PD on the continent and indeed with many other neurological disorders have no access to neurologists. Hence the greater proportion of patients with PD are undiagnosed, untreated or under-treated by primary healthcare workers with insufficient knowledge to coordinate the multi-faceted aspects of PD care. Thus a viable strategy is task-shifting by empowering primary and allied health workers with the requisite knowledge to successfully oversee the management of PD patients. The study by Cubo et al. demonstrated the feasibility of tele-educational programs as a prototype for knowledge transfer on neurological disorders. (18)
Although we identified no studies reporting on acceptability and efficacy of telemedicine for neurology in SSA and indeed in many LMICs, there were some encouraging results on use of telemedicine in other fields of medicine on the continent. Telemedicine has been successfully deployed in dermatology (19–25), ophthalmology (26,27), HIV prevention and care (28), clinical psychology and psychiatry (29,30), neurosurgery (31), radiology (32–35), and non-commuicable diseases including hypertension (36–38). Overall, the most successful telemedicine endeavors in SSA have relied on international collaborative efforts between centers in Africa and counterparts in North America or Europe. For instance, the Réseau en Afrique Francophone pour la Télémédecine (RAFT network), is an ensemble of 10 French speaking countries in Africa and two European countries (France and Switzerland) established to offer continuing medical education of healthcare professionals and teleconsultations to help improve quality and efficiency of health systems in these SSA countries. (39). Also, the Telehealth in Africa project was developed by the European Collaborative Group involving intergovernmental organizations, non-governmental organizations and the private sector with networks between European reference Hospitals in Milan (Italy), Toulouse (France) and African hospitals in Abidjan (Ivory Coast) and Midrand (South Africa) with the aim of improving medical care for in these LMICs. (40).
In general, telemedicine for neurology holds great promise for patient care in resource-limited LMICs in SSA but there is a paucity of clinical studies on the continent. Teleneurology as a discipline is in its nascent stages in most developing regions as this review highlights. In the other medical disciplines where a measure of success has been achieved using telemedicine, mHealth approaches in particular have been employed. The advancement of teleneurology is challenged by a myriad of factors such as dependency on funding, unclear healthcare system responsibilities, lack of neurologists and allied health professional to provide drive and leadership, unreliable infrastructure and lack of evidence on cost-effectiveness challenge their implementation. However, m-health have demonstrated positive health-related outcomes in other settings and their success is based on the accessibility, acceptance and low-cost of the technology, effective adaptation to local contexts, strong stakeholder collaboration, and government involvement. Telemedicine for neurology can potentially be scaled-up after high-quality evidence has accrued from well designed and powered feasibility, efficacy and effectiveness studies in SSA and indeed in other LMICs regions around the globe to establish this promising discipline. We propose the setting up of a Teleneurology network for SSA (figure 1) comprising of transcontinental networks (collaborative networks between neurology centers in North America and Europe with institutions in SSA) as a first tier. The first tier will be pivotal for teleneurology education of residents in neurology training and for tele-consultations between neurologists in SSA and colleagues abroad. Tier 2 would comprise of inter-regional networks within the United Nation sub-regions of Africa, tier 3 would consist of intra-regional networks and tier 4 made of national networks of academic institutions/tertiary medical centers with neurologist serving peripheral hospitals by way of teleconsultations and medical education. Within this network patients with neurological disorders could be triaged for medical review by neurologists and neurology residents in LMICs who can in turn seek advise from colleagues in-country, within a sub-region or from partners in High-Income Countries.
Figure 1.
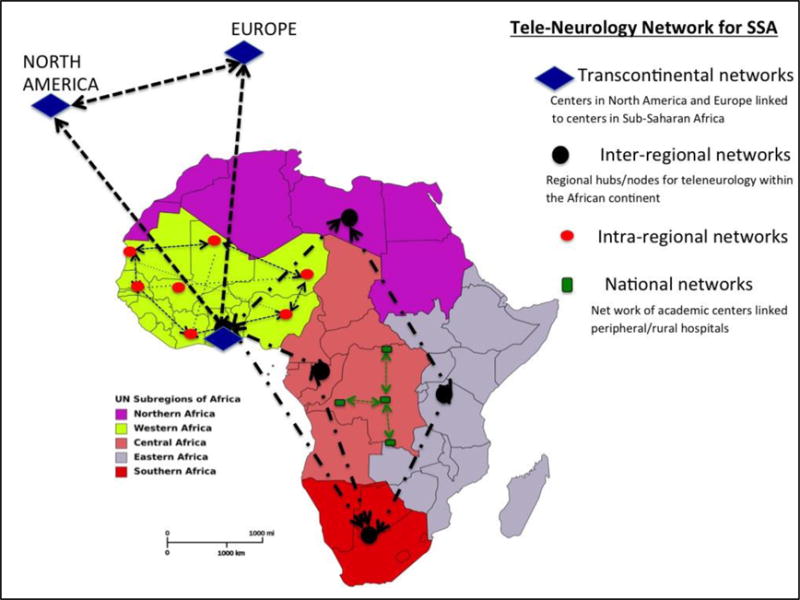
Proposed Teleneurology Networks for Sub-Saharan Africa.
CONCLUSIONS
Teleneurology via mHealth approaches in Africa represent an innovative and promising approach to delivering health services in improving the reach of neurology services to deprived populations. In this fast-growing technological field, research opportunities include assessing implications of scaling-up mHealth projects, evaluating cost-effectiveness and impacts on the overall health system.
Acknowledgments
Source of funding: National Institute of Health-National Institute of Neurological Disorders & Stroke; R21 NS094033.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None to declare
References
- 1.WHO. Global burden of neurological disorders: estimates and projections. http://www.who.int/mentalhealth/neurology/chapter2neurodisorderspublichchallenges.pdf accessed 3/07/2017.
- 2.WHO. Neurology Atlas. 2004 http://www.who.int/mentalhealth/neurology/neurogyatlaslr.pdf accessed 3/07/2017.
- 3.American Association of Telemedicine. What is telemedicine and telehealth? Available at http://www.americantelemed.org/files/public/abouttelemedicine/whatistelemedicine.pdf Accessed 30/06/2017.
- 4.Wechsler L, Tsao JW, Levine SR, Swain-Eng RJ, Adams RJ, Demaerschalk BM, et al. Teleneurology applications. Report of the telemedicine working group of the American Academy of Neurology. Neurology. 2013;80:670–676. doi: 10.1212/WNL.0b013e3182823361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loh PK. Telemedicine and Alzheimer’s disease from studio-based videoconferencing to mobile handheld cell phones. J Brain Dis. 2009;1:39–43. doi: 10.4137/jcnsd.s2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qaddoumi I, Mansour A, Musharbash A, et al. Impact of telemedicine on pediatric neuro-oncology in a developing country: the Jordanian-Canadian experience. Pediatr Blood Cancer. 2007;48:39–43. doi: 10.1002/pbc.21085. [DOI] [PubMed] [Google Scholar]
- 7.Terry JB. Evolution of neuronetworks. Neuroepidemiology. 2000;19:20–29. doi: 10.1159/000026234. [DOI] [PubMed] [Google Scholar]
- 8.Cottrell C, Drew J, Gibson J, Holroyd K, O’Donnell F. Feasibility assessment of telephone-administered behavioral treatment for adolescent migraine. Headache. 2007;47:1293–1302. doi: 10.1111/j.1526-4610.2007.00804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kane RL, Bever CT, Ehrmantraut M, Forte A, Culpepper WJ, Wallin MT. Teleneurology in patients with multiple sclerosis: EDSS rating derived remotely and from hands-on examination. J Telemed Telecare. 2008;14:190–194. doi: 10.1258/jtt.2008.070904. [DOI] [PubMed] [Google Scholar]
- 10.Rasmusson KA, Hartshorn JC. A comparison of epilepsy patients in a traditional ambulatory clinic and a telemedicine clinic. Epilepsia. 2005;5:767–770. doi: 10.1111/j.1528-1167.2005.44804.x. [DOI] [PubMed] [Google Scholar]
- 11.Samii A, Ryan-Dykes P, Tsukuda RA, Zink C, Franks R, Nichol WP. Telemedicine for delivery of health care in Parkinson’s disease. J Telemed Telecare. 2006;12:16–18. doi: 10.1258/135763306775321371. [DOI] [PubMed] [Google Scholar]
- 12.Mendez I, Hill R, Clarke D, Kolyvas G, Walling S. Robotic long-distance telementoring in neurosurgery. Neurosurgery. 2005;56:434–440. doi: 10.1227/01.neu.0000153928.51881.27. [DOI] [PubMed] [Google Scholar]
- 13.Hutarew G, Schlicker HU, Idriceanu C, Strasser F, Dietze O. Four years experience with teleneuropathology. J Telemed Telecare. 2006;12:387–391. doi: 10.1258/135763306779378735. [DOI] [PubMed] [Google Scholar]
- 14.Paing WW, Weller RA, Welsh B, Foster T, Birnkrant JM, Weller EB. Telemedicine in children and adolescents. Curr Psychiatry Rep. 2009;11:114–119. doi: 10.1007/s11920-009-0018-9. [DOI] [PubMed] [Google Scholar]
- 15.Powell AC. Gallup/bbg survey: ‘Massive’ increase in mobile phone, internet use in nigeria. 2012 Accessed at http://uscpublicdiplomacy.Org/index.Php/newswire/cpdblogdetail/gallupbbgsurveymassiveincreaseinmobilephoneinternetuseinnigeria/ on february 9, 2014.
- 16.Okoro EO, Sholagberu HO, Kolo PM. Mobile phone ownership among nigerians with diabetes. Afr Health Sci. 10:183–186. [PMC free article] [PubMed] [Google Scholar]
- 17.Jidenma N. The real mobile revolution: Africa’s smartphone future. Cnn marketplace africa. 2013 Last accessed at http://www.Cnn.Com/2013/11/07/opinion/real-mobile-revolution-africa-smartphone/ on february 8, 2014.
- 18.Cubo E, Doumbe J, Njiengwe E, Onana P, Garona R, Alcalde J, et al. A Parkinson’s disease tele-education program for health care providers in Cameroon. J Neurol Sci. 2015;357(1–2):285–7. doi: 10.1016/j.jns.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 19.Delaigue S, Bonnardot L, Olson D, Morand JJ. Overview of teledermatology in low-resource settings. Med Sante Trop. 2015;25(4):365–72. doi: 10.1684/mst.2015.0504. [DOI] [PubMed] [Google Scholar]
- 20.Lipoff JB, Cobos G, Kaddu S, Kovarik CL. The Africa Teledermatology Project: A retrospective review of 1229 consultations from sub-Saharan Africa. J Am Acad Dermatol. 2015;72(6):1084–5. doi: 10.1016/j.jaad.2015.02.1119. [DOI] [PubMed] [Google Scholar]
- 21.Azfar RS, Lee RA, Castelo-Soccio L, Greeberg MS, Bilker WB, Gelfand JM, et al. Reliability and validity of mobile teledermatology in human immunodeficiency virus-positive patients in Botswana: a pilot study. JAMA Dermatol. 2014;150(6):601–7. doi: 10.1001/jamadermatol.2013.7321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Osei-Tutu A, Shih T, Rosen A, Amanquah N, Chowdhury M, Nijhawan R, et al. Mobile teledermatology in Ghana: sending and answering consults via mobile platform. M Acad Dermatol. 2013;69(2):e90–1. doi: 10.1016/j.jaad.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Weinberg J, Kaddu S, Gabler G, Kovarik C. The African teledermatology project: providing access to dermatologic care and education in sub-Saharan Africa. Pan Afr Med J. 2009;3:16. [PMC free article] [PubMed] [Google Scholar]
- 24.Schmid-Grendelmeier P, Masenga EJ, Haeffner A, Burg G. Teledermatology as a new tool in sub-Saharan Africa: an experience from Tanzania. J Am Acad Dermatology. 2000;42(5 Pt 1):833–5. doi: 10.1067/mjd.2000.104796. [DOI] [PubMed] [Google Scholar]
- 25.Tesfalul M, Littman-Quinn R, Antwi C, Ndlovu S, Motsepe D, Phuthego M, et al. Evaluating the potential impact of a mobile telemedicine system on coordination of specialty care for patients with complicated oral lesions in Botswana. J Am Med Inform Assoc. 2016;23(e1):e142–5. doi: 10.1093/jamia/ocv140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matimba A, Woodward R, Tambo E, Ramsay M, Gwanzura L, Guramatunhu S. Tele-ophthalmology: opportunities for improving diabetes eye care in resource- and specialist-limited sub-Saharan African countries. J Telemed Telecare. 2016;22(5):311–6. doi: 10.1177/1357633X15604083. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy C, Van Heerden A, Cook C, Murdoch I. Utilization and practical aspects of tele-ophthalmology between South Africa and the UK. J Telemed Telecare. 2001;7(Suppl 1):20–2. doi: 10.1177/1357633X010070S108. [DOI] [PubMed] [Google Scholar]
- 28.Forrest JI, Wiens M, Kanters S, Nsanzimana S, Lester RT, Mills EJ. Mobile health applications for HIV prevention and care in Africa. Curr Opin HIV AIDS. 2015;10(6):464–71. doi: 10.1097/COH.0000000000000198. [DOI] [PubMed] [Google Scholar]
- 29.Adjorlolo S. Can teleneuropsychology help meet the neuropsychology needs of Western Africans? The case of Ghana. Appl Neuropsychol Adult. 2015;22(5):388–98. doi: 10.1080/23279095.2014.949718. [DOI] [PubMed] [Google Scholar]
- 30.Chipps J, Ramlall S, Mars M. Practice guidelines for videoconference-based telepsychiatry in South Africa. Afr J Psychiatry (Johannesbg) 2012;15(4):271–82. doi: 10.4314/ajpsy.v15i4.35. [DOI] [PubMed] [Google Scholar]
- 31.Jithoo R, Govender PV, Corr P, Nathoo N. Telemedicine and neurosurgery: experience of a regional unit based in South Africa. J Telemed Telecare. 2003;9(2):63–6. doi: 10.1258/135763303321327894. [DOI] [PubMed] [Google Scholar]
- 32.Zennaro F, Oliveira Gomes JA, Casalino A, Lonardi M, Starc M, Paoletti P, et al. Digital radiology to improve the quality of care in countries with limited resources: a feasibility study from Angola. PLoS One. 2013;8(9):e73939. doi: 10.1371/journal.pone.0073939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwartz AB, Siddiqui G, Barbieri JS, Akhtar AL, Kim W, Littman-Quinn R, et al. The accuracy of mobile teleradiology in the evaluation of chest X-rays. J Telemed Telecare. 2014;20(8):460–3. doi: 10.1177/1357633X14555639. [DOI] [PubMed] [Google Scholar]
- 34.Halton J, Kosack C, Spijker S, Joekes E, Andronikou S, Chetcuti K, et al. Teleradiology usage and user satisfaction with the telemedicine system operated by medecins san frontiers. Front Public Health. 2014;28:202. doi: 10.3389/fpubh.2014.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sangare M, Tanner L, Voss S, Laureys F, Hollow D, Toure M. A national teleradiology programme in Mali: implementation and results. J Telemed Telecare. 2015;21(3):131–8. doi: 10.1177/1357633X15569966. [DOI] [PubMed] [Google Scholar]
- 36.Yepes M, Maurer J, Viswanathan B, Gedeon J, Bovet P. Potential reach of mhealth versus traditional mass media for prevention of chronic diseases: evidence from a national representative survey in a middle-income country in Africa. J Med Internet Res. 2016;18(5):e114. doi: 10.2196/jmir.5592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bobrow K, Farmer AJ, Springer D, Shanyinde M, Yu LM, Brennan T, et al. Mobile phone text messages to support treatment adherence in adults with high blood pressure (SMS-Text Adherence Support [STAR]): A single-blind, randomized trial. Circulation. 2016;133(6):595–600. doi: 10.1161/CIRCULATIONAHA.115.017530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kingue S, Angandii P, Menanga AP, Ashuntantang G, Sobngwi E, Dossou-Yovo RA, et al. Efficiency of an intervention package for arterial hypertension comprising telemanagement in a Cameroonian rural setting: The TELEMED-CAM study. Pan Afr Med J. 2013;15:153. doi: 10.11604/pamj.2013.15.153.2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bediang G, Perrin C, Ruiz de Casteneda R, Kamga Y, Sawadogo A, Bagayoko CO, Geissbuhler A. The RAFT Telemedicine Network: lessons learnt and perspectives from a decade of educational and clinical services in Low-and Middle-Income Countries. Front Public Health. 2014;2:180. doi: 10.3389/fpubh.2014.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rovetta A, Falcone F, Sala R, Garavaldi ME. Telehealth in Africa. Stud Health Technol Inform. 1997;39:277–85. [PubMed] [Google Scholar]


