Abstract
Significance
Varying amounts of peripheral defocus reported in previous studies are likely due whether peripheral defocus is measured while turning the eyes or the head. Contact lenses (CL) lag when viewing objects in peripheral gaze, so future studies ought to measure peripheral defocus while turning the head to measure defocus through the peripheral add power.
Purpose
Soft multifocal CL peripheral defocus studies report varying results. To determine whether soft multifocal CL lag when turning the eyes could affect the measurement of peripheral defocus, we measured how much CLs move when looking in different gazes.
Methods
The distance between limbus and CL edge was measured with a slit lamp reticle magnifier. Centration was measured as the distance between CL edge and limbus at the superior, inferior, nasal, and temporal location of the CL while in primary gaze. Decentration of the CL equals the difference of the distance between the CL edge and limbus while looking centrally and 20 degrees in each direction. All measurements were performed while subjects wore habitual and Proclear Multifocal CL.
Results
The average ± SD age of the 40 subjects was 27.8 ± 8.4 years, 65% were female, and SE refractive error was −4.43 ± 2.05 D. The soft multifocal CLs decentered 0.09 ± 0.03 mm temporal (p = 0.006). The soft multifocal CLs lagged 0.49 ± 0.28 mm while looking down (p < 0.001), 0.24 ± 0.36 mm while looking up (p = 0.008), 0.58 ± 0.20 mm while looking nasal (p < 0.001), and 0.35 ± 0.21 mm while looking temporal.
Conclusions
Soft multifocal CLs center temporally in primary gaze, and they lag significantly while looking in every direction, but a 0.50 mm or more when looking down or nasal, which could affect measurement of peripheral defocus when subjects turn their eyes instead of their head.
Keywords: myopia, contact lenses, multifocal, decentration, refractive error
Myopia is a very common visual condition that results from a mismatch between eye length (too long) and optical power. Myopia affects approximately one-third of the United States population.1 It is even more prevalent in East Asian countries, where over 80% of some samples are myopic.2, 3 There is no cure for myopia, and most research aims to slow its progression. Recent animal research suggests that visual signals from the fovea may not be essential for eye growth regulation, because the eye can still emmetropize after removing the myopic growth stimulus, even after the macula is ablated.4
Corneal reshaping contact lenses slow eye growth in myopic children while providing them with clear vision throughout the day.5–12 The putative cue for slowed eye growth is peripheral myopic defocus.4, 13 Center-distance multifocal contact lenses also slow eye growth,14–17 and, in theory, they also do so by creating peripheral myopic defocus. However, there is controversy regarding the amount of peripheral myopic defocus created by soft multifocal contact lenses.18–21
The inconsistency in study results may be explained by reports of the absolute peripheral defocus versus the relative peripheral defocus, various contact lens designs and add powers, variation of myopic refractive errors, a variety of retinal locations that were measured, and turning of eyes versus turning of head to examine peripheral defocus (Table 1).
Table 1.
Variable that may explain differences in results from various studies of peripheral defocus with soft multifocal contact lenses.
| Study | Mean ± SD spherical equivalent refractive error (D) |
Contact lens | Add power (D) | Retinal locations (degrees) | Turn eye or head |
|---|---|---|---|---|---|
| Lopes-Ferreira20 | −0.06 ± 0.54 | Proclear Multifocal D | +2.00 | 5–35° in 5° steps, nasal and temporal | Eye |
| Kang19 | −1.41 ± 0.60 (low myopes) −3.25 ± 0.80 (high myopes) | Proclear Multifocal D | +2.00 | 10°, 20°, 30°, 35° nasal and temporal | Eye |
| Berntsen18 | −3.62 ± 1.56 | Biofinity Multifocal D | +2.50 | 20°, 30°, 40° nasal and temporal | Head |
| Ticak21 | −2.84 ± 1.29 | Proclear Multifocal D | +2.00 | 10°, 20°, 30° nasal and temporal | Eye |
Using only 20 and 30 degrees in the nasal and temporal retinal locations, and extrapolating data from graphs when necessary, we can see that there is little agreement between the studies (Table 2).
Table 2.
Mean peripheral defocus with soft multifocal contact lenses. If absolute data were available, they are included, otherwise relative data are included. Data reported as nasal and temporal visual field are adjusted to retinal location.19
| Author | Absolute or Relative | 30° temporal | 20° temporal | Central | 20° nasal | 30° nasal |
|---|---|---|---|---|---|---|
| Lopes-Ferreira20 | Absolute | −2.75 | −2.10 | −1.00 | −0.75 | −1.25 |
| Relative* | −1.70 | −1.21 | – | +0.23 | −0.29 | |
|
| ||||||
| Kang19 | Absolute | −0.90 | −1.60 | −0.40 | −0.10 | +0.20 |
| Relative | −0.40 | −0.60 | – | +0.20 | +0.50 | |
|
| ||||||
| Berntsen18 | Relative | −0.90 | −1.20 | – | −0.20 | −0.70 |
|
| ||||||
| Ticak21 | Relative | +0.50 | −0.15 | – | +0.50 | +0.60 |
Most studies measuring peripheral defocus at 20 and 30 degrees with a center-distance soft multifocal contact lens found more absolute and relative myopic blur in the periphery, at least in the temporal retina,18–20 although one found essentially no relative defocus temporally.21 Nasally, all studies found little relative or absolute blur in the nasal periphery, ranging from +0.60 to −1.25.18–21
One possible reason for the discrepancy between the peripheral defocus studies using soft multifocal contact lenses is lens lag when turning the eyes to look in extreme gazes, although there is no evidence in the literature of this effect. If the lens lags when subjects look in extreme gaze, the effects of peripheral defocus during primary gaze may be underestimated, because autorefractor measurements may be measured through the central distance or the intermediate portions of the multifocal contact lens instead of through the full near addition portion.
The purpose of this study is to measure soft multifocal contact lens decentration and lag to determine whether some of the discrepancy in peripheral defocus studies performed with soft multifocal contact lenses may be due to poor centration in primary gaze or lag of the lens when turning the eyes to peripheral targets.
METHODS
The study was approved by the Biomedical Institutional Review Board of The Ohio State University, and all subjects provided informed consent. Eligible subjects were 18 years and older and wore spherical soft contact lenses.
A total of 40 subjects participated in this study. While wearing the subjects’ habitual contact lens, the widest aperture size and lower lid position were measured while the subject fixated a single letter located on a visual acuity chart positioned at eye level, 4 m from the subject. A millimeter ruler, placed vertically in front of the eye was used to estimate the distance from the central lower lid to the central upper lid to the nearest 0.5 millimeter. Lower lid position was compared to the position of the limbus – subjectively defined as the middle border between the clear cornea and the opaque sclera – by setting the “zero” mark of the ruler at the lower lid margin, then quickly pulling down the lid to measure the location of the limbus from the zero mark to the nearest 0.5 mm. If the limbus was above the lower lid, it was recorded as a negative value.
Lens displacement upon blinking was measured to the nearest 0.1 mm using a reticle in the slit lamp ocular with magnification at 16×. Centration of the contact lens while the subject looked in primary gaze was determined by measuring the distance from the limbus to the contact lens edge at the inferior, superior, nasal, and temporal portions of the contact lens. Each measurement was repeated three times by the same examiner and averaged. To view the upper and lower distance from limbus to contact lens edge, the examiner raised the subjects’ upper lid and lowered the subjects’ lower lid and noted the distance from the limbus to the contact lens edge immediately after moving the lid. The reticle was oriented horizontally to measure the distance from limbus to contact lens edge at the nasal and temporal locations and vertically to measure the distance from limbus to contact lens edge at the superior and inferior locations.
The distance from the limbus to the contact lens edge was also measured while subjects viewed targets located 20 degrees superior, inferior, nasal, and temporal to primary gaze. While the subject looked in each direction of gaze, the distance from limbus to contact lens edge was only measured on the portion of the contact lens opposite to the subject’s direction of gaze. For example, the distance from limbus to contact lens edge was measured on the inferior portion of the contact lens edge while the subject looked at the superior target. The process was also repeated three times by the same examiner and averaged.
After removing the right contact lens, retinoscopy and non-cycloplegic manifest refraction with maximum-plus-to maximum-visual acuity were performed, followed by a binocular blur balance.
Simulated keratometry values were recorded for the right eye using one map with a “High Confidence” rating, measured by the Zeiss ATLAS Corneal Topography System model 993 (Carl Zeiss Meditec; Dublin, CA).
A Proclear Multifocal “D” contact lens with a +2.00D add was inserted in the right eye. The distance powers of all of the multifocal contact lenses worn ranged from −2.50 D to −3.00 D, and all contact lenses had an 8.4 mm base curve. The same slit lamp protocol for measuring lens movement and centration in primary and peripheral gaze was repeated.
For purposes of this paper, “centration” refers to the position of the contact lens in the horizontal meridian and the vertical meridian separately, while looking in primary gaze. If the distances between limbus and contact lens edge are not significantly different in either the horizontal or vertical meridians, then the lens is centered. If the distance from limbus to contact lens edge is significantly greater on one side than the other, then the lens is considered to be centered in the direction of the largest distance between the limbus and contact lens edge. For example, if the mean distance from contact lens edge to limbus is 1.3 mm at the bottom, 1.7 mm at the top, 1.4 mm temporally, and 1.6 mm nasally, and those distances are significantly different, the centration would be 0.2 mm superior and 0.1 mm nasal.
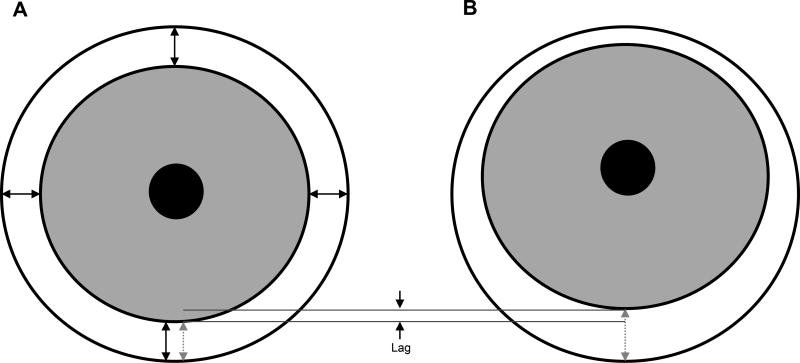
“Lag” refers to the difference in distance from contact lens edge to limbus in the same location (nasal, temporal, superior, or inferior) when looking in primary gaze compared to peripheral gaze. For example, the distance from the inferior contact lens edge to limbus may be 1.5 mm in primary gaze and the distance from the inferior contact lens edge to limbus may be 2.5 mm while looking in up gaze. The lag would then be +1.0 mm (peripheral gaze is greater than primary gaze). Figure 1 indicates the difference between centration and lag definitions.
Figure 1.
The black arrows in Figure 1 (A) illustrate centration; if all distances between limbus and contact lens edge are equal in primary gaze, the lens is centered perfectly. The lens is considered to be decentered in the direction of the largest distance between the lens edge and the limbus. For example, if the superior distance is greater than the inferior distance while in primary gaze, then the lens is decentered superiorly. The difference between the gray arrows indicated in Figures 1 (A) and (B) represents contact lens lag. For example, the gray arrow is longer in up gaze (B) than it is in primary gaze (A), and that difference is the amount of lag of the contact lens.
Statistics
Data were only collected on the right eye. Data were entered twice into a Microsoft Excel Database. Discrepancies between the datasets were verified from the source data, and a final, corrected dataset was maintained. SPSS version19 software was used for data analysis. A paired t-test was performed to determine whether the subjects’ contact lens significantly lagged while looking in each gaze. For example, we used a paired t-test to compare the distance between the limbus and contact lens edge when the subject is looking in primary gaze and when the subject is looking 20 degrees superior. A repeated measures ANOVA was performed to investigate the effect of myopia, flat keratometry reading, aperture size, age, gender, and ethnicity on contact lens lag in various gazes. We used Bonferroni correction to adjust for multiple comparisons when the repeated measures ANOVA indicated a significant effect. Pearson correlation coefficients were calculated to assess the relationship between centration and age, gender, ethnicity, and refractive error.
A post-hoc power calculation, assuming α = 0.05, exhibited 95% power to determine 0.25 mm contact lens lag when using the largest standard deviation (0.36), found for the lag of a multifocal contact lens when looking up.
Contact Lenses
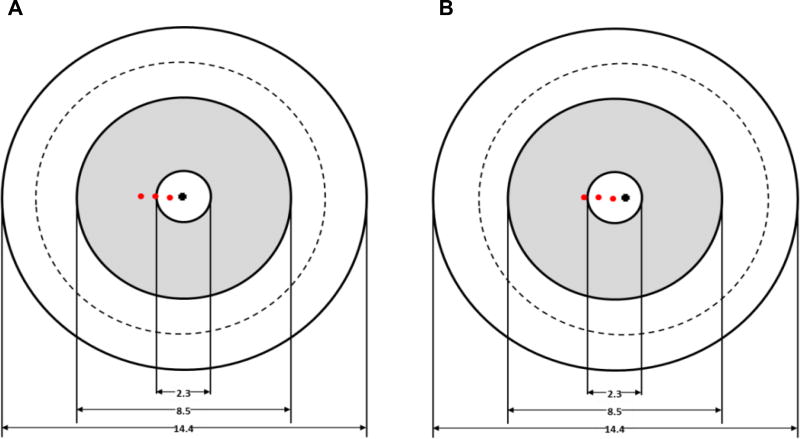
The multifocal contact lens used during this study was the Proclear Multifocal “D” with a +2.00 D add power (CooperVision, Fairport, NY). The lens is made of omafilcon A, has 62% water content, an 8.4 mm base curve, and the overall diameter is 14.4 mm. A small range of sphere powers was chosen for this study (−2.50 D to −3.00 D) in order to control for the effect of different contact lens powers on lag. The −2.50 D to −3.00 D power is also similar to the spherical equivalent refractive error of subjects enrolled in many myopia control studies, so it is representative of the contact lens power of many subjects at the beginning of a study. Both undercorrected and overcorrected myopes were able to see the near target clearly. The Proclear Multifocal “D” lens features a spherical central zone surrounded by an aspheric annular zone, which is followed by another spherical peripheral annular zone. According to the Proclear Multifocal Fitting Guide, it contains a 2.3 mm wide distance center portion, then the power progressively becomes less negative until it reaches the stated add power at a radius of 4.25 mm, similar to the Biofinity Multifocal contact lens.22
RESULTS
Of the forty subjects recruited for this study, two-thirds were female, a large majority was Caucasian, and they ranged in age from 21 to 46 years. Nearly one-third (32.5%) had −5.00 D or more spherical equivalent myopia, based on non-cycloplegic manifest refraction. The widest aperture size of the right eye ranged from 7 mm to 10 mm. The distance between limbus and lower lid ranged from −1.0 mm (limbus above lid margin) to +1.5 mm (limbus below lid margin). Demographic and ocular information are presented in Table 3.
Table 3.
Demographic and ocular (right eye) information of the 40 subjects enrolled in the study. For lower lid position, a positive number indicates the limbus was below the lid margin.
| Demographic and ocular information | 40 Subjects |
|---|---|
| Mean ± SD age (years) | 27.8 ± 8.4 |
| Gender (%female) | 65 |
| Ethnicity (%) | |
| American Indian or Alaskan Native | 0 |
| Asian or Pacific Islander | 12.5 |
| Black, not of Hispanic origin | 0 |
| Hispanic | 0 |
| White, not of Hispanic origin | 85 |
| Other or unknown | 2.5 |
| Baseline Refractive Error (D) | |
| M | −4.43 ± 2.05 |
| J0 | +0.02 ± 0.15 |
| J45 | 0.00 ± 0.06 |
| Simulated Keratometry (D) | |
| Steep meridian | 44.34 ± 1.65 |
| Flat meridian | 43.75 ± 1.52 |
| Widest aperture (mm) | 8.83 ± 1.11 |
| Lower lid position (mm) | +0.44 ± 0.69 |
The 95% limits of agreement of the difference between three measurements by one examiner of the distance between the limbus and contact lens edge is ±0.09 mm while the subject fixates in primary gaze and ±0.08 mm while the subject fixates in peripheral gaze.
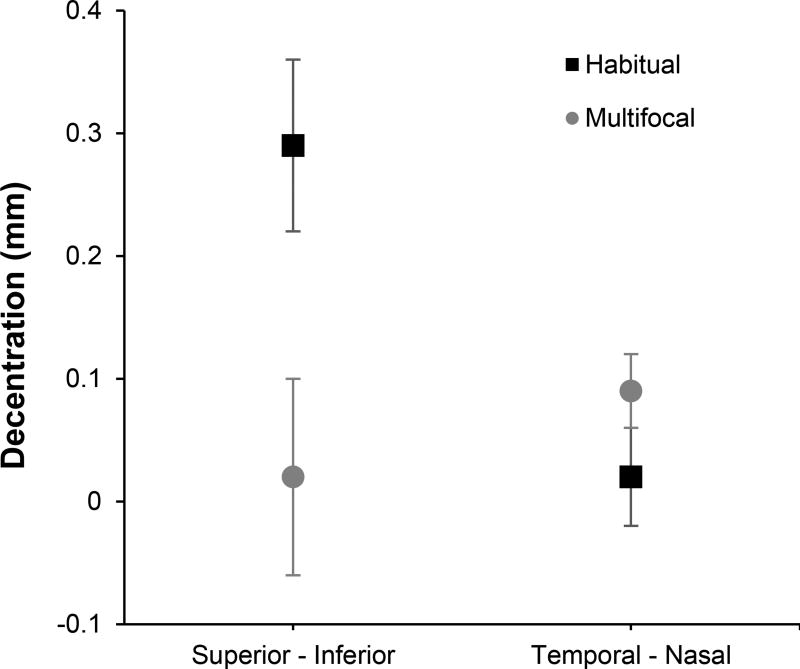
Centration (Primary Gaze)
For the subjects’ habitual contact lens, there was a significant difference in distance from limbus to contact lens edge in the vertical meridian (p < 0.001), but not the horizontal meridian (p=0.60), which indicated overall superior decentration by 0.15 mm. For the multifocal lenses, there was a significant difference in the horizontal meridian (p = 0.006) but not the vertical meridian (p=0.76), which indicated overall temporal decentration by 0.05 mm (Table 4).
Table 4.
The mean ± SD difference between the limbus and contact lens edge at the superior and inferior locations (superior minus inferior) or the temporal and nasal locations (temporal minus nasal) while the subject fixates in primary gaze. Positive numbers indicate greater distance in the superior and temporal locations. Overall, the habitual spherical lenses centered superiorly and the multifocal contact lenses centered slightly temporarily (paired t-test).
| Lens type | Location | Difference (mm) | p-value |
|---|---|---|---|
| Habitual spherical contact lenses | Superior - Inferior | +0.29 ± 0.07 | < 0.001 |
| Habitual spherical contact lenses | Temporal - Nasal | +0.02 ± 0.04 | 0.60 |
| Multifocal contact lenses | Superior - Inferior | +0.02 ± 0.08 | 0.76 |
| Multifocal contact lenses | Temporal - Nasal | +0.09 ± 0.03 | 0.006 |
Overall, the multifocal contact lenses had better centration than the habitual spherical contact lenses in primary gaze (Figure 2).
Figure 2.
Centration of the habitual and soft multifocal contact lenses in primary gaze.
Contact Lens Lag (Peripheral Gaze)
When the subject looked down or nasal, both the habitual spherical and multifocal contact lenses lagged approximately 0.5 mm (p < 0.001). In comparison, they lagged less than 0.25 mm in superior gaze (Table 5).
Table 5.
Lag of the contact lens, which is the difference in distance from the limbus to contact lens edge between when the subject fixates in various gazes and the same lens location while the subject fixates in primary gaze of habitual and multifocal contact lenses. For example, decentration = distance from limbus to contact lens edge of the inferior contact lens while looking superiorly – distance from limbus to contact lens edge of the inferior contact lens while looking in primary gaze.
| Average decentration ± SD | Habitual | p-value | Multifocal | p-value |
|---|---|---|---|---|
| Inferior - primary | 0.52 ± 0.29 | < 0.001 | 0.49 ± 0.28 | < 0.001 |
| Superior - primary | 0.19 ± 0.34 | = 0.01 | 0.24 ± 0.36 | = 0.008 |
| Nasal - primary | 0.56 ± 0.23 | < 0.001 | 0.58 ± 0.20 | < 0.001 |
| Temporal - primary | 0.43 ± 0.24 | < 0.001 | 0.35 ± 0.21 | < 0.001 |
Factors that May Affect Centration or Contact Lens Lag
Neither the centration nor the lag of the contact lens in the vertical meridian was associated with the subjects’ age, gender, ethnicity (Asian versus non-Asian), or amount of myopia (5.00 D or more spherical component versus less than 5.00 D), except spherical lenses tended to center more inferior for high myopes than for low myopes (Table 6).
Table 6.
P-values for the individual Pearson correlation coefficients assessing the relation between spherical and bifocal contact lens centration (primary gaze) in the vertical meridian and age, gender, ethnicity (Asian versus non-Asian), and myopia (median split).
| Lens | Gaze | Age | Gender | Ethnicity | Myopia |
|---|---|---|---|---|---|
| Spherical | Primary | 0.39 | 0.68 | 0.45 | < 0.0001 |
| Spherical | Various | 0.82 | 0.28 | 0.75 | 0.62 |
| Bifocal | Primary | 0.42 | 0.55 | 0.61 | 0.43 |
| Bifocal | Various | 0.55 | 0.66 | 0.52 | 0.63 |
DISCUSSION
Corneal reshaping5–12 and soft multifocal contact lenses14–17 are thought to slow myopic eye growth by providing peripheral myopic defocus.21, 23, 24 Both animal25, 26 and human16 studies provide evidence of the effect of peripheral defocus on axial elongation of the eye. However, investigations of peripheral defocus created by soft multifocal contact lenses show little myopic blur on the nasal retina and variable results in the temporal retina.18–21 Our investigation indicates that contact lenses tend to lag in peripheral gaze, which may underestimate the peripheral defocus associated with soft multifocal contact lens wear. Investigators should have subjects turn their heads to peripheral targets, maintaining primary gaze, and therefore reduce the effects of contact lenses that lagged on peripheral defocus.
Spherical contact lenses tended to center superiorly when subjects were looking in primary gaze in this study. This finding is perhaps due to the lid interaction pushing the lens up. The upper lid was held by the examiner to take the superior measurement, but the lower lid was not touched, which could push and decenter the lens up. It is also possible that subjects looked slightly inferiorly to avoid the bright light of the slit lamp, which shifted the lens superiorly.
While looking in different gazes, the average distance from limbus to contact lens edge was significantly greater than primary gaze, which means that both spherical and soft multifocal contact lenses lag when looking in peripheral gaze. They do not lag equally in each gaze, possibly due to ocular asymmetry and/ or lid interaction. Spherical and soft multifocal contact lenses both tend to lag approximately 0.50 mm or more inferiorly and nasally, about 0.4 mm temporally, and less than 0.25 mm superiorly.
Figure 3 indicates where autorefraction would be performed on the lens when the subject looks at 10°, 20°, and 30° in primary (Figure 3a) and temporal gaze (Figure 3b). The contact lens parameters were obtained from the Proclear Multifocal fitting guide. The locations of the red dots were estimated using the tangent of each angle and the estimated distance from the entrance pupil of the eye to the cornea of 3.0 mm. Those distances from the center of the lens were calculated to be 0.5 mm at 10 degrees, 1.1 mm at 20 degrees, and 1.7 mm at 30 degrees in primary gaze.
Figure 3.
Estimation of where the center of the autorefractor entrance pupil would sample when measuring peripheral defocus at 10°, 20°, and 30° in primary (A) and temporal gaze (B).
When the subject turns the eyes 20° nasal, the lens lags 0.50 mm temporal, and the 20° autorefractor reading is still centered in the distance portion of the contact lens, so little peripheral defocus would be measured. Although the entrance pupil of the Grand Seiko autorefractor is 2 mm in diameter, it does not measure as much of the peripheral add power when the eyes are turned. Therefore, any peripheral refractive error measurements performed through multifocal contact lenses should be made with eyes in primary gaze by turning the subject’s head instead of moving the eyes.
This study was limited by the examiner’s knowledge of which contact lenses, habitual or soft multifocal, the subjects wore. This limitation could have been eliminated by randomizing the order the subject wore the lenses and masking the examiner. A less subjective measurement of contact lens lag could have also been made by using a video camera and semi-automated software to measure distances. This study was also performed on young adults, as opposed to children who are most likely to undergo soft multifocal contact lens myopia control, but the eyes and lids are fully developed by 10 years of age, so very little difference would be expected from a study of younger subjects. Furthermore, only one of the three center-distance design multifocal contact lenses available at the time was used. We used the same lens that was used in the study by Ticak21, which is very similar in design to another of the three and would be expected to provide similar results.
The angle of observation is closer to perpendicular when viewing lag of the lens 20 degrees in peripheral gaze than when viewing centration of the lens in primary gaze, so the distance between the limbus and contact lens edge would appear approximately 6.4% larger in peripheral gaze. A lag of approximately 0.50 mm while looking in peripheral gaze may actually be only 0.47 mm (6.4% smaller). This difference is small enough compared to the overall effect to be considered negligent.
Future studies may consider direct comparison of turning the eyes and turning the head to measure peripheral defocus to determine the true effect of contact lens lag while looking in peripheral gaze.
CONCLUSIONS
Contact lenses lag up to approximately 0.50 mm when looking in various gazes. When turning the eyes to measure peripheral defocus while wearing a contact lens, the autorefractor may measure primarily through the central distance portion of the contact lens or the lowest add power of the near addition. That may explain some of the variability in soft multifocal contact lens peripheral defocus study results. Future studies ought to employ head turn instead of eye turn when measuring peripheral defocus with soft multifocal contact lenses in order to measure peripheral defocus through the add power of a multifocal contact lens.
Acknowledgments
Supported by T35 EY007151; Jeffrey J. Walline receives research materials from Bausch + Lomb. Nevin W.
Footnotes
El-Nimri has no conflicts to disclose.
This manuscript was presented as a poster titled “Centration of Contact Lens in Peripheral Gaze” in 2012 at the American Academy of Optometry.
Contributor Information
Nevin W. El-Nimri, University of California, Berkeley, School of Optometry; Berkeley, California.
Jeffrey J. Walline, The Ohio State University College of Optometry; Columbus, Ohio.
References
- 1.Vitale S, Sperduto RD, Ferris FL, 3rd, et al. Increased Prevalence of Myopia in the United States between 1971–1972 and 1999–2004. Arch Ophthalmol. 2009;127:1632–9. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 2.Seet B, Wong TY, Tan DT, et al. Myopia in Singapore: Taking a Public Health Approach. Br J Ophthalmol. 2001;85:521–6. doi: 10.1136/bjo.85.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jung SK, Lee JH, Kakizaki H, et al. Prevalence of Myopia and Its Association with Body Stature and Educational Level in 19-Year-Old Male Conscripts in Seoul, South Korea. Invest Ophthalmol Vis Sci. 2012;53:5579–83. doi: 10.1167/iovs.12-10106. [DOI] [PubMed] [Google Scholar]
- 4.Smith EL, 3rd, Ramamirtham R, Qiao-Grider Y, et al. Effects of Foveal Ablation on Emmetropization and Form-Deprivation Myopia. Invest Ophthalmol Vis Sci. 2007;48:3914–22. doi: 10.1167/iovs.06-1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Charm J, Cho P. High Myopia-Partial Reduction Ortho-K: A 2-Year Randomized Study. Optom Vis Sci. 2013;90:530–9. doi: 10.1097/OPX.0b013e318293657d. [DOI] [PubMed] [Google Scholar]
- 6.Chen C, Cheung SW, Cho P. Myopia Control Using Toric Orthokeratology (to-See Study) Invest Ophthalmol Vis Sci. 2013;54:6510–7. doi: 10.1167/iovs.13-12527. [DOI] [PubMed] [Google Scholar]
- 7.Cho P, Cheung SW. Retardation of Myopia in Orthokeratology (Romio) Study: A 2-Year Randomized Clinical Trial. Invest Ophthalmol Vis Sci. 2012;53:7077–85. doi: 10.1167/iovs.12-10565. [DOI] [PubMed] [Google Scholar]
- 8.Cho P, Cheung SW, Edwards M. The Longitudinal Orthokeratology Research in Children (Loric) in Hong Kong: A Pilot Study on Refractive Changes and Myopic Control. Curr Eye Res. 2005;30:71–80. doi: 10.1080/02713680590907256. [DOI] [PubMed] [Google Scholar]
- 9.Hiraoka T, Kakita T, Okamoto F, et al. Long-Term Effect of Overnight Orthokeratology on Axial Length Elongation in Childhood Myopia: A 5-Year Follow-up Study. Invest Ophthalmol Vis Sci. 2012;53:3913–9. doi: 10.1167/iovs.11-8453. [DOI] [PubMed] [Google Scholar]
- 10.Kakita T, Hiraoka T, Oshika T. Influence of Overnight Orthokeratology on Axial Elongation in Childhood Myopia. Invest Ophthalmol Vis Sci. 2011;52:2170–4. doi: 10.1167/iovs.10-5485. [DOI] [PubMed] [Google Scholar]
- 11.Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, et al. Myopia Control with Orthokeratology Contact Lenses in Spain (Mcos): Refractive and Biometric Changes. Invest Ophthalmol Vis Sci. 2012;53:5060–5. doi: 10.1167/iovs.11-8005. [DOI] [PubMed] [Google Scholar]
- 12.Walline JJ, Jones LA, Sinnott LT. Corneal Reshaping and Myopia Progression. Br J Ophthalmol. 2009;93:1181–5. doi: 10.1136/bjo.2008.151365. [DOI] [PubMed] [Google Scholar]
- 13.Diether S, Schaeffel F. Local Changes in Eye Growth Induced by Imposed Local Refractive Error Despite Active Accommodation. Vision Res. 1997;37:659–68. doi: 10.1016/s0042-6989(96)00224-6. [DOI] [PubMed] [Google Scholar]
- 14.Anstice NS, Phillips JR. Effect of Dual-Focus Soft Contact Lens Wear on Axial Myopia Progression in Children. Ophthalmology. 2011;118:1152–61. doi: 10.1016/j.ophtha.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 15.Lam CS, Tang WC, Tse DY, et al. Defocus Incorporated Soft Contact (Disc) Lens Slows Myopia Progression in Hong Kong Chinese Schoolchildren: A 2-Year Randomised Clinical Trial. Br J Ophthalmol. 2014;98:40–5. doi: 10.1136/bjophthalmol-2013-303914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sankaridurg P, Holden B, Smith E, 3rd, et al. Decrease in Rate of Myopia Progression with a Contact Lens Designed to Reduce Relative Peripheral Hyperopia: One-Year Results. Invest Ophthalmol Vis Sci. 2011;52:9362–7. doi: 10.1167/iovs.11-7260. [DOI] [PubMed] [Google Scholar]
- 17.Walline JJ, Greiner KL, McVey ME, et al. Multifocal Contact Lens Myopia Control. Optom Vis Sci. 2013;90:1207–14. doi: 10.1097/OPX.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 18.Berntsen DA, Kramer CE. Peripheral Defocus with Spherical and Multifocal Soft Contact Lenses. Optom Vis Sci. 2013;90:1215–24. doi: 10.1097/OPX.0000000000000066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang P, Fan Y, Oh K, et al. The Effect of Multifocal Soft Contact Lenses on Peripheral Refraction. Optom Vis Sci. 2013;90:658–66. doi: 10.1097/OPX.0b013e3182990878. [DOI] [PubMed] [Google Scholar]
- 20.Lopes-Ferreira D, Ribeiro C, Maia R, et al. Peripheral Myopization Using a Dominant Design Multifocal Contact Lens. J Optom. 2011;4:14–21. [Google Scholar]
- 21.Ticak A, Walline JJ. Peripheral Optics with Bifocal Soft and Corneal Reshaping Contact Lenses. Optom Vis Sci. 2013;90:3–8. doi: 10.1097/OPX.0b013e3182781868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Plainis S, Atchison DA, Charman WN. Power Profiles of Multifocal Contact Lenses and Their Interpretation. Optom Vis Sci. 2013;90:1066–77. doi: 10.1097/OPX.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 23.Charman WN, Mountford J, Atchison DA, et al. Peripheral Refraction in Orthokeratology Patients. Optom Vis Sci. 2006;83:641–8. doi: 10.1097/01.opx.0000232840.66716.af. [DOI] [PubMed] [Google Scholar]
- 24.Queirós A, González-Méijome JM, Jorge J, et al. Peripheral Refraction in Myopic Patients after Orthokeratology. Optom Vis Sci. 2010;87:323–9. doi: 10.1097/OPX.0b013e3181d951f7. [DOI] [PubMed] [Google Scholar]
- 25.Smith EL, 3rd, Hung LF, Huang J. Relative Peripheral Hyperopic Defocus Alters Central Refractive Development in Infant Monkeys. Vision Res. 2009;49:2386–92. doi: 10.1016/j.visres.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith EL, 3rd, Hung LF, Huang J, et al. Effects of Local Myopic Defocus on Refractive Development in Monkeys. Optom Vis Sci. 2013;90:1176–86. doi: 10.1097/OPX.0000000000000038. [DOI] [PMC free article] [PubMed] [Google Scholar]