Abstract
Objective
People dealing with serious mental illness frequently report turning to religion to help cope with the disorder. However, little is known about how religion impacts commitment to psychotherapy programs for people with schizophrenia and their caregivers.
Method
In a sample of 64 families enrolled in a culturally-informed family treatment for schizophrenia that targets religiosity, we hypothesized that patients and caregivers who utilize high levels of adaptive religious coping and low levels of maladaptive religious coping, would be less likely to drop out of treatment than their counterparts.
Results
In line with hypotheses, results demonstrated that greater maladaptive religious coping was associated with fewer family therapy sessions attended. Contrary to expectations, greater adaptive religious coping was also associated with attending fewer family therapy sessions.
Conclusion
Results suggest that any type of religious coping may be associated with higher levels of attrition from family therapy. Perhaps spiritual/religious people are already getting support and guidance from their beliefs and practices that aid them in coping with mental illness. Results may also suggest that there is a “religiosity gap” in which religious individuals perceive a disconnect between their beliefs and the beliefs of their mental health providers. It is important to point out that in this study, of those who dropped out prematurely, nearly all did so before the religiosity segment of treatment even began. Modifying how family treatments are introduced early on in therapy to ensure they appear congruent with the beliefs and values of religious families may help to reduce attrition.
Keywords: schizophrenia, religiosity, religious coping, attrition, premature dropout
Prior research suggests that using religion as a coping resource when facing stressful life events (e.g., mental illness in the family) is quite common, particularly among some ethnic minority groups such as Blacks and Hispanics/Latinos1 (Chatters, Taylor, Jackson, & Lincoln, 2008; Dessio et al., 2004; Esterberg & Compton, 2006; Weisman, Gomes, & López, 2003). In addition, religiosity has demonstrated a strong relationship with schizophrenia symptomatology and course of illness. For example, greater religiosity has been found to be associated with greater symptom remission and less substance use in patients with schizophrenia and other psychotic disorders (Borras et al., 2007). Esterberg and Compton (2006) found that religious and/or spiritual beliefs about schizophrenia played an important role in their sample of Black patients and suggest that these beliefs may influence how family members cope with and make decisions about how to seek help for the illness. Weisman, Gomes, and López (2003) similarly found that nearly 40% of less acculturated Hispanics/Latinos with a relative with schizophrenia used their religion as a way to cope with the stressors of the illness. Thus, religiosity may also be related to treatment beliefs and behaviors such as the decision to prematurely drop out of family treatments. Previous studies have demonstrated that family treatments are effective in reducing patient symptom severity, hospitalizations, and relapse rates (e.g., Pitschel-Walz, Leucht, Bäuml, Kissling, & Engel, 2001; AUTHORS, 2014). However, as few as 0.7% to 8.0% of families coping with severe mental illness receive any family therapy at all (Dixon et al., 1999). To date, the majority of attrition studies have focused on fixed, demographic variables. For example, younger age, male gender, lower level of education or income, and ethnic minority status have been found to be associated with higher attrition rates (O’Brien, Fahmy, & Singh, 2009; Salmoiraghi & Sambhi, 2010; Swift & Greenberg, 2012; Wierzbicki & Pekarik, 1993). Attrition rates are noted to be high in family treatments ranging from 40 to 60% (Wierzbicki & Pekarik, 1993). The majority of studies indicate that the largest percentage of dropouts occur earlier as opposed to later in treatment programs, typically within the first few sessions (e.g., Harris, 1998; Swift & Greenberg, 2012). To the best of our knowledge, no studies to date have specifically examined sociocultural factors which may predict attrition from family treatments for schizophrenia. Surprisingly, religiosity has yet to be examined as a potential predictor of attrition. While religiosity is typically an integral part of Black and Hispanic/Latino families (Weisman, 1997; Weisman & López, 1996), it is a common coping resource for many families, which is why it may be a particularly strong predictor of treatment-related decisions.
Previous findings demonstrate that maladaptive uses of religious coping such as passively relying on prayer or holding punishing God appraisals, negatively impact physical and mental health behaviors and outcomes. For example, Blacks with strong religious beliefs who put their fate entirely in “the hands of God” are less likely to abstain from smoking (Hooper, Baker, Rodriguez de Ybarra, McNutt, & Ahluwalia, 2012) and are also less likely to engage in preventive health behaviors such as getting breast cancer screenings (e.g., Kinney, Emery, Dudley, & Croyle, 2002). Relatedly, in a sample of chronic pain patients, Edwards, Moric, Husfeldt, Buvanendran, and Ivankovich (2005) found Black and Hispanic/Latino patients relied more heavily on a “passive” coping strategy of prayer when compared with White patients. Interestingly, the authors found that passive forms of coping were related to greater pain, distress, and disability (Edwards et al., 2005). Thus, it seems that more passive or inactive means of coping with illness (e.g., relying solely on prayer or faith that God will take care of all problems) may lead individuals to take a “back seat” approach to their healthcare and simply wait to see what their fate will be (e.g., “I let God solve my problems for me.”). Furthermore, endorsing maladaptive religious beliefs such as punishing God appraisals (e.g., viewing an event as a punishment from God) has been found to be associated with greater psychological distress, poorer psychological wellbeing (Phillips & Stein, 2007), and faster disease progression in individuals with HIV (Ironson et al., 2011). For example, Lee, Roberts, and Gibbons (2013) found that in a sample of college students coping with the death of a loved one, negative religious coping (e.g., endorsing beliefs such as, “Wondered whether God had abandoned me.”) was associated with increased negative emotions and prolonged recovery from grief. Holding these types of beliefs also seems to coincide with a more passive religious coping style in which God has already predetermined one’s fate and since the individual feels that they have little control or say in the situation, they adopt an inactive stance (e.g., “What’s the point?” or “I will focus on the world-to-come rather than the problems of this world.”). Furthermore, holding beliefs of punishment from or abandonment by God can also lead to feelings of discontent and resentment with one’s religion (e.g., “I felt angry with or distant from God.” or “I questioned my religious beliefs and faith.”). Based on the literature reviewed above, maladaptive forms of religious coping and holding negative religious appraisals may make individuals feel as if they have little control in a situation at hand. Therefore, these individuals may be more likely to adopt an inactive stance towards mental health care (e.g., “What’s the point in trying if my fate has been decided for me?”) and drop out of treatment.
On the other hand, previous studies also suggest that adaptive religious beliefs (e.g., viewing a negative event as a life lesson from God which ultimately serves to strengthen the person) may provide a foundation for meaning making in coping with mental illness and may also create an opportunity for spiritual growth (Tabak & Weisman de Mamani, 2014). Furthermore, positive religious appraisals can instill a sense of hope and optimism and help individuals make sense of life events (Weisman, 2005). For example, religious reappraisals that aid individuals in benefit-finding related to life experiences (e.g., “Found the lesson from God in the event.”) or feeling as if they have the collaboration of God in attempting to solve life problems (e.g., “Took control over what I could and gave the rest to God.”), have been found to be associated with a greater sense of personal control and better quality of life (e.g., Pargament et al., 1988). Individuals who rely on their religious belief systems as a resource to help them through a difficult time (versus solving their problems for them) may be empowered by tenets such as, “God helps those that help themselves” to seek out ways in which they can improve their situation. Instead of submitting to a difficult situation and taking on a “woe is me” attitude, these individuals may be more likely to adopt a “can do” attitude as they go forth with the assistance and support of their religion (e.g., “In dealing with the problem, I was guided by God.”). Thus, it seems likely that adaptive religious beliefs and appraisals may positively influence retention rates in treatment since these individuals may be more likely to actively seek out ways in which they can improve their family’s situation and may be more committed to being a unified front against mental illness.
In the context of a newly developed, culturally informed family treatment for schizophrenia ([BLIND]; AUTHORS, 2014), the current study examined patient and primary caregiver religiosity in an attempt to predict premature family dropout. As religion/spirituality is a topic covered in the [BLIND] treatment, results from the current study may allow us to better predict those at high risk for attrition and identify a sociocultural variable that could be targeted and modified early in treatment. Results may help decrease the risk of premature dropout and ensure that families are staying in treatments for schizophrenia long enough to obtain benefit.
The Current Study
This study aimed to examine religiosity and its relationship with attrition in an ethnically diverse sample of families (patients and their primary caregivers) coping with schizophrenia. Based on the literature reviewed above, the current study tested the following hypotheses in patients and caregivers: 1) Greater adaptive religious coping (i.e., greater overall religiosity, greater use of spiritually-based coping, greater endorsement of good deeds, greater use of interpersonal religious support) would be associated with a greater number of family therapy sessions attended. 2) Greater maladaptive forms of religious coping (i.e., demonstrating discontent with God and/or religious faith, pleading with God, greater use of religious avoidance) would be associated with a lower number of family therapy sessions attended. 3) On an exploratory basis, we attempted to pinpoint the session(s) in which the majority of families dropped out of [BLIND] TREATMENT.
Method
Sample
The current study is part of a larger treatment study examining the efficacy of a culturally informed family treatment for schizophrenia ([BLIND]) when compared to a psychoeducational (PSY-ED) comparison condition (AUTHORS, 2014). AUTHORS (2014) found that [BLIND] outperformed PSY-ED in reducing patient psychiatric symptom severity with a medium effect size. AUTHORS (2016) further found that the treatment reduced caregiver burden relative to PSY-ED with a large effect. AUTHORS (in press) further tested a multi-family version of [BLIND] and found that patients who participated in the [BLIND] group had significantly lower psychiatric symptoms at termination compared to their own baseline and compared to patients assigned to a waitlist control condition. With the efficacy of [BLIND] already established, the current study focused on evaluating the role of religion in predicting attrition in [BLIND], an intervention that directly targets religion as a core treatment component.
Patients with schizophrenia and their family members were recruited for the study at the University of [BLIND] Department of Psychology (see AUTHORS, 2014). Our print advertisements stated, “Have you or one of your relatives been diagnosed with schizophrenia or schizoaffective disorder? If so, you may be eligible to participate in a research study. During the study you will take part in an interview (regarding symptoms, how you cope with the illness, and cultural information) and, if interested, you may also be eligible for a free family therapy for schizophrenia/schizoaffective disorder. Interviews/therapy are available in English and Spanish. You will be compensated $25 for your interview time.” All participants that inquired about treatment details during their phone screen or assessment were provided with information about the five [BLIND] modules. After the baseline assessment (approximately 3 hours), families were randomly assigned to the [BLIND] or PSY-ED family therapy treatment conditions. The current study’s sample is only comprised of the families randomized to the [BLIND] treatment condition because PSY-ED is only 3 sessions and does not focus on religion ([BLIND] is described in detail below). Several family members could participate in the study together. However, to ensure independence of data, the current study only used data from patients and primary caregivers. Primary caregiver status was defined as the relative who reported spending the most time with the patient. Professional or paid caregivers were not eligible to participate in the current study. Sixty-four [BLIND] families comprised the current study sample. The sample of patients was 63.0% male with a mean age of 38.06 (SD = 14.15). Patients self-identified their ethnicity as White (17.3%), Black (32.7%), Hispanic/Latino (44.2%), or Other (5.8%). Two patients had missing data for ethnicity. Patients reported their highest level of education as advanced degree (1.9%), college degree (15.1%), some college (28.3%), high school (22.6%), some high school (18.9%), grade 8 (5.7%), or below grade 8 (7.5%). Primary caregivers in this sample were 62.5% female with a mean age of 49.69 (SD = 15.90). Caregivers self-identified their ethnicity as White (18.8%), Black (29.7%), Hispanic/Latino (48.4%), or Other (3.1%). Caregivers reported their highest level of education as advanced degree (9.4%), college degree (25%), some college (17.2%), high school (31.3%), some high school (10.9%), grade 8 (4.7%), or below grade 8 (1.6%). Caregivers reported their relationship to the patient as mother (35.9%), father (7.8%), significant other (21.9%), sister (1.6%), brother (6.3%), daughter (3.1%), son (4.7%), friend (10.9%), uncle (1.6%), niece (1.6%), grandmother (1.6%), or cousin (3.1%). The majority (40.8%) of primary caregivers reported spending 100+ hours per week with the patient or living together full-time. Though participants did not systematically indicate their specific country of origin, several Hispanic/Latino participants revealed this information during the interview. Most Hispanic participants reported being from Cuba, followed by Puerto Rico, Nicaragua, and Venezuela. Of the Hispanic/Latino participants, 33.5% of families elected to receive their treatment in Spanish.
[BLIND] TREATMENT NAME
[BLIND] is a fully manualized family treatment with 5 modules. Each topic is discussed for 3 weeks for a total of 15 weekly sessions lasting 60–75 minutes per session (see AUTHORS, 2005; AUTHORS, 2006). All materials are available in English or Spanish. [BLIND] incorporates therapeutic elements informed by cross-cultural research and includes two novel modules on religion/spirituality and family collectivism (AUTHORS, 2014). [BLIND] also takes into consideration the beliefs, behaviors, and practices of the family presenting to treatment and aims to incorporate these constructs into treatment. In other words, [BLIND] is tailored to account for a family’s established cultural values and does not aim to sway the family in a particular direction (e.g., toward a specific organized religion). [BLIND] attempts to access and foster adaptive beliefs, behaviors, and cultural practices of families’ backgrounds while also attempting to modify maladaptive beliefs and behaviors. An additional goal of the [BLIND] treatment is to foster spiritual beliefs and perceptions of family collectivism.
Family Collectivism (module one)
The primary objective of this module is to enhance the families’ perspective that they are a part of a unified team working towards the same goal. Handouts, activities, and homework assignments are used to generate discussions about how family members view their personal identity in the family unit, their values and contributions, what they like about their family, and what part(s) of the family dynamic they would like to see change. Through these discussions, the therapist works to unify the family, emphasize commonalities, and deemphasize differences (AUTHORS, 2014). Emphasis is also placed on how the family can work together as a unit to improve family functioning, reduce family problems, and best care for the patient.
Psychoeducation (module two)
This module is primarily drawn from a previously developed intervention (Falloon, Boyd, & McGill, 1984) that was adapted by others (Miklowitz, 2008; Miklowitz & Goldstein, 1997; Mueser & Glynn, 1999). The objective of this segment is to educate patients and their family members on the common symptoms of schizophrenia, prodromal symptoms that may be indicative of an impending relapse, and information on the diathesis-stress model of schizophrenia including genetic vulnerability and environmental factors that can exacerbate the illness. Families also learn about the impact that the family environment can have on the patient’s course of illness.
Religion/Spirituality (module three)
The objective of the third module is to aid family members in tapping into spiritual or existential beliefs they have which may serve as an adaptive coping skill or resource in dealing with the illness. Open-ended questions help guide the discussion about participants’ history of their spiritual beliefs, practices, and values, beliefs about God or other supreme being, and their perspective on the meaning of life. Participants are also asked to discuss the meaning of spiritual concepts such as forgiveness, empathy, gratitude, generosity, compassion, and other values that the family finds important. Family members are encouraged to discuss spiritual practices that they currently use or would like to use such as prayer, meditation, yoga, volunteering in the community, or attending religious services. Family members are encouraged to identify how becoming involved in (or reconnecting with) these activities might be beneficial to them and then attempt to engage in the activities more often. It is important to note that therapists do not push or encourage any particular set of religious beliefs but instead, attempt to discuss the aforementioned concepts in the context of the family’s existing religious or spiritual beliefs. If families or certain family members do not subscribe to a particular religion or do not wish to discuss their religious beliefs, the therapist provides a parallel set of handouts that target existential and philosophical beliefs. Many of the concepts and values previously mentioned in the religious handouts (e.g., forgiveness, gratitude, compassion) are also addressed in the existential handouts and are relevant to treatment regardless of participant spiritual or religious beliefs. During this module, the therapist attempts to foster adaptive spiritual beliefs while attempting to reframe any maladaptive uses of religion such as passive use of religious practices (i.e., “I only need to pray about it and God will take care of everything.”) or unhelpful beliefs (i.e., “Mental illness is a punishment from God.”).
Communication Training (module 4)
The last two modules of [BLIND] are also largely drawn from previously developed interventions which have demonstrated strong empirical support in families coping with schizophrenia and bipolar disorder (Falloon et al., 1984; Miklowitz & Goldstein, 1997). In the communication-training module, family members learn a specific set of skills designed to help families express themselves and support each other more effectively. This module discusses the techniques of active listening, expressing positive and negative feelings, and making requests for behavioral change.
Problem-Solving (module five)
In the final module of treatment, family members are taught a systematic way to enhance their problem-solving skills and apply them to the challenges associated with coping with schizophrenia. Through use of a step-by-step handout, family members work together to identify a problem, brainstorm all possible solutions, evaluate each solution, choose the optimal solution(s), and then create a strategy and plan for implementing the chosen solution. This module creates an opportunity for family members to collaborate and strategize together to create a plan that is acceptable to all family members. We provide case examples in the following papers that illustrate how this culturally informed treatment functions: AUTHORS (2014) and AUTHORS (2006).
Attrition
The number of therapy sessions (0–15) that families attended was documented. Families who missed sessions or no-showed were rescheduled for the following week or soon after, based on the family’s availability. In other words, a missed session did not equate to missing any modules as families were scheduled to pick up where they had left off. If a family did not return multiple calls for a period of 1 month, they were considered a dropout and not contacted further. Treatment completion was defined as attending all 15 [BLIND] therapy sessions. Families that left treatment any time after the baseline assessment/randomization to [BLIND] but before the fifteenth and final therapy session were considered non-completers. Of the 64 [BLIND] families, 26 families completed treatment (40.6%) and 38 families dropped out prematurely (59.4%). The average number of sessions attended was 4.53 (SD = 5.88).
Translation of Materials
All study materials including consent forms, assessment measures, and therapy materials were provided in English or Spanish. Materials were translated from English to Spanish utilizing an editorial board approach. The editorial board was comprised of individuals from diverse Hispanic/Latino backgrounds including Cuba, Colombia, Nicaragua, Costa Rica, Mexico, and Puerto Rico. This translation method is considered to be more effective than translation-back translation as the review board takes into account within-group language variations (Geisinger, 1994). Study materials were first translated into Spanish by a native Spanish speaker. Each member of the editorial review board then independently reviewed the Spanish versions and compared them to the English versions. The review board convened and discussed any discrepancies with the goal of having materials written in the most generic and universally understood wording. It was also important that the wording in the Spanish versions of the documents continued to accurately reflect the original English meaning of the constructs. The editorial review board continued to meet and compare the Spanish and English versions until a consensus was reached on all remaining discrepancies.
Informed Consent
All participants provided written informed consent through forms approved by the University of [BLIND] Institutional Review Board. Due to participant variability in reading fluency, assessments were conducted by bilingual research associates and all measures were administered in a verbal interview format in which the assessor recorded participant responses.
Eligibility for the Current Study
Patients for the current study were required to meet DSM lifetime criteria for a schizophrenia or schizoaffective diagnosis. A semi-structured interview, the Structured Clinical Interview for DSM-IV-TR, Patient Edition (SCID-I/P, Version 2.0), Psychotic Symptoms module (First, Spitzer, Gibbon, & Williams, 2002), was used for diagnosis confirmation and was administered by graduate level research assistants. The SCID-I/P has previously demonstrated high inter-rater reliability for both symptoms and diagnoses (Ventura, Liberman, Green, Shaner, & Mintz, 1998). In order to determine inter-rater reliability, the Principal Investigator (NAME) and all other interviewers for the current study, watched six videotapes of SCID-I/P interviews and provided their independent determinations of patient diagnoses. Inter-rater agreement for the current study using Cohen’s Kappa was 1.0. While the majority of individuals with schizophrenia who participated in our study continued to experience some symptoms of psychosis, we excluded a handful of individuals who were severely psychotic and therefore, unable to tolerate lengthy assessments, hour-long therapy sessions, and/or would have difficulty understanding the material being covered in therapy. The criteria that was used to indicate this was based on scores of “6” (severe) or “7” (extremely severe) on any of the 4 BPRS core psychosis items: unusual thought content, suspiciousness, hallucinations, and conceptual disorganization. Participants who received these scores were referred out for more comprehensive care. Additional exclusion criteria included being suicidal at the time of the assessment, having a suicide attempt within the last year, an involuntary hospitalization within the past 3 months, or having ever been incarcerated for violent crimes.
Measures
Religious/Moral Values
Patient and caregiver religiosity was assessed using the Moral-Religious Emphasis subscale of the FES (Moos & Moos, 1981). This subscale is designed to assess the degree to which family members actively discuss and emphasize ethical and religious matters (Moos & Moos, 1976). This subscale consists of nine T/F items which were summed and calculated such that higher scores were indicative of greater religious and moral emphasis. Sample item: “Family members attend church, synagogue, or Sunday School fairly often.” Internal reliability for the subscale is reported to have a Cronbach’s alpha of .78 (Moos & Moos, 1981). In the current study, Cronbach’s alpha was .77 for patients and .59 for caregivers.
Religious Coping
Adaptive and maladaptive religious coping were measured with the Religious Coping Activities Scale (RCAS; Pargament et al., 1990). The RCAS is comprised of 29 statements in which participants rate the extent to which the item is or is not related to their religious coping. Responses choices are: “not at all,” “somewhat,” “quite a bit,” or “a great deal.” The RCAS contains 6 subscales in which higher scores are indicative of greater use of that type of religious coping activity: 1) the Spiritual Based Coping subscale (12 items e.g., “Used my faith to help me decide how to cope with the situation.”), 2) the Good Deeds subscale (6 items e.g., “Tried to be less sinful.”), 3) the Discontent subscale (3 items e.g., “Felt angry with or distant from God.”), 4) the Interpersonal Religious Support subscale (2 items e.g., “Received support from other members of the church.”), 5) the Plead subscale (3 items e.g., “Bargained with God to make things better.”), and 6) the Religious Avoidance subscale (3 items e.g., “Prayed or read the Bible to keep my mind off my problems.”). The Spiritual Based Coping, Good Deeds, and Interpersonal Religious Support subscales were indicative of adaptive religious coping whereas the Discontent, Plead, and Religious Avoidance subscales represented maladaptive religious coping (Pargament et al., 1990; Pargament, Smith, Koenig, & Perez, 1998; Thompson & Vardaman, 1997). Internal reliability for the subscales is reported to range from adequate to excellent by the scale’s developers (Pargament et al., 1990). Internal reliability for the current study was calculated using Cronbach’s alpha (Patients adaptive coping subscales = .96; Patients maladaptive coping subscales = .73; Patients individual subscales: Spiritual Based Coping = .96, Good Deeds = .87, Discontent = .48, Interpersonal Religious Support = .86, Plead = .78, Religious Avoidance = .75; Caregivers adaptive coping subscales = .95; Caregivers maladaptive coping subscales = .76; Caregivers individual subscales: Spiritual Based Coping = .95, Good Deeds = .85, Discontent = .66, Interpersonal Religious Support = .82, Plead = .74, Religious Avoidance = .82).
Patient Symptom Severity
Severity of patient psychotic symptoms was measured through use of the Brief Psychiatric Rating Scale (BPRS; Lukoff, Nuechterlein, & Ventura, 1986; Overall & Gorham, 1962). The BPRS is a 24-item, semi-structured interview which assesses the following eight areas: unusual thought content, hallucinations, conceptual disorganization, depression, suicidality, self-neglect, bizarre behavior, and hostility. The 24 items are assessed using a 7-point anchor rating with 1 indicative of a “not present” symptom to 7 indicating an “extremely severe” level of the symptom. Total BPRS scores were obtained by summing scores on all 24 items with higher total scores indicating greater symptom severity. The BPRS is reported to have good reliability and has been reported as having intraclass coefficients ranging from .74–1.00 on scale items (Weisman, Rosales, Kymalainen, & Armesto, 2005). The Principal Investigator (NAME) completed a UCLA BPRS training and quality assurance program and has demonstrated reliability with the program’s creator, Dr. Joseph Ventura. Dr. NAME trained all graduate student interviewers. Interviewers then coded six training videotapes selected by Dr. Joseph Ventura. Intraclass correlations between interviewers and consensus ratings of Dr. Ventura ranged from .79 to .98 for total BPRS scores.
Proposed Analytic Plan
Preliminary Analyses
Statistical analyses were conducted using SPSS statistics software, Version 22. All variables were assessed for outliers and normality and were transformed, if necessary. Non-normality was identified when univariate values of 2.0 or greater were present for skewness and values of 7.0 or greater were present for kurtosis (Curran, West, & Finch, 1996). In line with prior research and in order to identify any potential covariates, the relationships among variables previously found to be associated with attrition (age, gender, education, ethnicity, patient symptom severity) were examined. Significant covariates were statistically controlled for in the primary analyses.
Primary Analyses
Multiple Linear Regression
A series of hierarchical multiple linear regression analyses were conducted. The number of therapy sessions that the family attended (0 to 15) was the dependent variable which was regressed upon the independent variables. Primary study variables were examined to determine if they predicted the number of family therapy sessions attended over and above the covariates. All primary study variables that were determined to be significant predictors of the number of family therapy sessions attended were then entered into another linear regression analysis together to determine if the linear combination of the primary study variables predicted the number of family therapy sessions attended over and above the linear combination of covariates.
Survival Analysis
On an exploratory basis, we applied survival analysis techniques to determine which session(s) the majority of families dropped out of [BLIND]. The Life Tables cumulative survival graph allowed us to determine which session(s) families dropped out most frequently. The number and proportion of families that dropped out of these sessions, the proportion of the sample that remained in treatment (“survived”), probability density, and hazard rates are provided for the highest-risk sessions. A series of Kaplan-Meier analyses were also conducted to determine if there were significant differences in the number of therapy sessions attended between high and low levels of the significant covariates and predictor variables from our regression analyses. Each variable was dichotomized into “low” and “high” levels based on histograms and median scores. If Log Rank (Mantel-Cox) test results were significant, a graph of the cumulative probability of survival, mean estimates of the number of therapy sessions attended, standard errors (S.E.), the median number of sessions attended, and confidence intervals were provided for each group.
RESULTS
Preliminary Analyses
Missing data
All study variables had missing data. However, the data did not appear to be affected by systematic response biases and Little’s Missing Completely at Random (MCAR) test supports this assertion, X2 (778) = 804.977, p = .244. Thus, listwise deletion was used.
Normality of study variables
The skew and kurtosis of all study variables had values within a conservative −1 to +1 range and no transformations were required. Table 1 (patients) and Table 2 (caregivers) on page 32 contain descriptive statistics for all continuous variables (n, mean, standard deviation, possible range, observed range, skew, kurtosis).
Table 1.
Descriptive Statistics for Continuous Variables (Patients)
| Variable* | n | Mean | Standard Deviation | Skewness | Kurtosis | Possible Range | Observed Range |
|---|---|---|---|---|---|---|---|
| FES Religion | 49 | 6.00 | 2.30 | −1.124 | .852 | 0–9 | 0–9 |
| RCAS Spiritual | 52 | 34.08 | 11.69 | −.423 | −.975 | 12–48 | 12–48 |
| RCAS Good Deeds | 53 | 15.48 | 5.51 | .046 | −1.026 | 6–24 | 6–24 |
| RCAS Discontent | 52 | 5.38 | 2.03 | .546 | −.714 | 3–12 | 3–12 |
| RCAS Interpersonal | 52 | 4.27 | 2.25 | .552 | −1.215 | 2–8 | 2–8 |
| RCAS Plead | 52 | 7.71 | 3.18 | .046 | −1.398 | 3–12 | 3–12 |
| RCAS Relig Avoid | 52 | 7.19 | 2.93 | .347 | −1.065 | 3–12 | 3–12 |
| Patient age | 53 | 38.06 | 14.15 | .429 | −.625 | 18–100+ | 18–75 |
| BPRS | 52 | 54.56 | 13.94 | −.255 | .322 | 24–168 | 24–87 |
Table 2.
Descriptive Statistics for Continuous Variables (Caregivers)
| Variable* | n | Mean | Standard Deviation | Skewness | Kurtosis | Possible Range | Observed Range |
|---|---|---|---|---|---|---|---|
| FES Religion | 63 | 6.00 | 1.89 | −.605 | −.598 | 0–9 | 2–9 |
| RCAS Spiritual | 64 | 35.08 | 10.62 | −.382 | −1.204 | 12–48 | 12–48 |
| RCAS Good Deeds | 64 | 15.42 | 5.38 | −.089 | −1.090 | 6–24 | 6–24 |
| RCAS Discontent | 64 | 4.84 | 2.13 | 1.143 | .640 | 3–12 | 3–11 |
| RCAS Interpersonal | 64 | 4.25 | 2.03 | .422 | −1.108 | 2–8 | 2–8 |
| RCAS Plead | 64 | 7.27 | 2.91 | .098 | −1.088 | 3–12 | 3–12 |
| RCAS Relig Avoid | 64 | 6.52 | 3.14 | .357 | −1.332 | 3–12 | 3–12 |
| Caregiver age | 64 | 49.69 | 15.90 | −.069 | −.441 | 18–100+ | 16–86 |
Covariates
The identification of potential covariates was conducted through use of Pearson correlations for continuous variables (see table 3 on page 32 for correlation matrix), independent sample t-tests for dichotomous variables (patient and caregiver gender), and one-way ANOVAs with post-hoc Bonferroni comparisons for categorical covariates (patient and caregiver ethnicity and education). Older caregiver age was associated with a greater number of family therapy sessions attended (r= .429, p < .001). Greater patient psychiatric symptom severity (BPRS total scores) was associated with fewer family therapy sessions attended (r= −.292, p = .036). Significant differences in the number of family therapy sessions based on patient ethnicity were observed (F(3,48)= 6.055, p = .001) such that families with Black patients had a lower average number of therapy sessions attended (M=1.18, SD = 3.63) when compared to families with White patients (M=10.78, SD=6.42; p = .002) or Hispanic/Latino patients (M=7.61, SD= 7.0; p = .010). No other between-group ethnicity comparisons were significant. Similar differences in the number of family therapy sessions were observed based on caregiver ethnicity (F(3,60)= 11.907, p < .001) such that families with Black caregivers had a lower average number of therapy sessions attended (M= .316, SD = .671) when compared to families with White caregivers (M=10.83, SD=6.56; p < .001) or Hispanic/Latino caregivers (M=7.50, SD= 6.73; p < .001). No other between-group ethnicity comparisons were significant. Significant differences were also noted for caregiver level of education (F(2,61)= 26.715, p < .001) such that families with caregivers who attended some college to advanced degree had a higher average number of therapy sessions attended (M= 11.40, SD = .614) when compared to families with caregivers who completed high school (M=1.550, SD= 3.66; p < .001) or with caregivers with some high school education or lower (M=2.46, SD= 4.46; p < .001). Significant differences in the number of sessions attended were not observed for other variables (patient gender t(52) = 1.248, p = .218; caregiver gender t(62) = −1.473, p = .146; patient education F(6,46)= 1.681, p=.147). Therefore, caregiver age, patient symptom severity, patient and caregiver ethnicity, and caregiver education were controlled for in the primary analyses.
Table 3.
Correlation Matrix for Potential Covariates
| Variable* | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. # Sessions | 1 | |||
| 2. IPage | −.175 | 1 | ||
| 3. CGage | .429** | .067 | 1 | |
| 4. BPRS | −.292* | .078 | .043 | 1 |
# Sessions=the number of family therapy sessions attended; IPage= identified patient age; CGage= caregiver age; BPRS = patient total BPRS scores
Primary Analyses
Hierarchical Multiple Linear Regression
Study hypotheses related to maladaptive religious coping were supported in that higher patient Plead scores on the Religious Coping Activities Scale (RCAS) were predictive of a lower number of family therapy sessions attended. Results were in the opposite direction of study hypotheses related to adaptive religious coping as higher scores on the following variables were predictive of a lower number of family therapy sessions attended: Patient Family Environment Scale (FES) Religiosity, Patient RCAS Interpersonal Religious Support, Caregiver RCAS Good Deeds, and Caregiver RCAS Interpersonal Religious Support. Contrary to study hypotheses, the remainder of primary study variables examined were not significant predictors of the number of family therapy sessions attended.
An additional model was run in which number of family therapy sessions attended was regressed upon covariates and primary study variables identified as significant predictors of number of family therapy sessions attended. Study hypotheses related to maladaptive religious coping were supported as higher patient RCAS Plead scores remained predictive of fewer family therapy sessions attended. Results were in the opposite direction of study hypotheses related to adaptive religious coping as higher Caregiver RCAS Interpersonal Religious Support scores continued to be predictive of fewer family therapy sessions attended. The remaining primary study variables were not significant predictors of number of family therapy sessions attended (Patient FES Religiosity; Patient RCAS Interpersonal Religious Support; Caregiver RCAS Good Deeds). Please see Table 4 (pg. 32) for a summary table of these findings and Table 5 for all statistical figures (pg. 33).2
Table 4.
Summary of Multiple Linear Regression Analyses
| Covariates controlled for in Primary Analyses | Non-Significant Predictors* | Significant Predictors of Number of Family Therapy Sessions Attended** | Study Hypotheses Supported? | Significant Predictors in Combined Model (covariates + primary study variables) | Study Hypotheses Supported? |
|---|---|---|---|---|---|
|
Patient Variables
|
Patient Variables
|
Maladaptive coping hypothesis supported Results in opposite direction of adaptive coping hypothesis |
Covariates of caregiver education, patient symptom severity, Patient RCAS Plead, Caregiver RCAS Interpersonal Religious Support | Maladaptive coping hypothesis supported Results in opposite direction of adaptive coping hypothesis |
FES = Family Environment Scale; RCAS = Religious Coping Activities Scale; RCAS subscale 1= Spiritual-Based Coping; RCAS subscale 2= Good Deeds; RCAS subscale 3= Discontent; RCAS subscale 4= Interpersonal Religious Support; RCAS subscale 5= Plead; RCAS subscale 6 = Religious Avoidance
Note: Higher scores on all significant predictor variables were predictive of fewer family therapy sessions attended
Table 5.
Hierarchical Linear Regression Results
| Patient RCAS Plead and covariates | ||||
| Model: F(6,41)= 8.711, p < .001, R2= .560, R2ADJUSTED= .496 | ||||
| Variable | β | t | p | Partial r |
| Patient RCAS Plead | −.277 | t(41)= −2.419 | .020 | −.353 |
| Caregiver education | .485 | t(41) = 4.050 | < .001 | .535 |
| Patient symptom severity | −.258 | t(41) = −2.267 | .029 | −.334 |
| Patient FES Religiosity and covariates | ||||
| Model: F(6,38)= 7.913, p < .001, R2= .555, R2ADJUSTED= .485 | ||||
| Variable | β | t | p | Partial r |
| Patient FES Religiosity | −.283 | t(38)= −2.556 | .015 | −.383 |
| Caregiver education | .485 | t(38) = 3.956 | < .001 | .540 |
| Patient symptom severity | −.249 | t(38) = −2.133 | .039 | −.327 |
| Patient RCAS Interpersonal Religious Support and covariates | ||||
| Model: F(6,41)= 8.222, p < .001, R2= .546, R2ADJUSTED= .480 | ||||
| Variable | β | t | p | Partial r |
| Patient RCAS Interpersonal Religious Support | −.238 | t(41)= −2.093 | .043 | −.311 |
| Caregiver education | .499 | t(41) = 4.121 | < .001 | .541 |
| Caregiver RCAS Good Deeds and covariates | ||||
| Model: F(6,43)= 9.182, p < .001, R2= .562, R2ADJUSTED= .500 | ||||
| Variable | β | t | p | Partial r |
| Caregiver RCAS Good Deeds | −.266 | t(43)= −2.448 | .019 | −.350 |
| Caregiver education | .480 | t(43) = 4.073 | < .001 | .528 |
| Patient symptom severity | −.227 | t(43) = −2.060 | .046 | −.300 |
| Caregiver RCAS Interpersonal Religious Support and covariates | ||||
| Model: F(6,43)= 8.913, p < .001, R2= .554, R2ADJUSTED= .492 | ||||
| Variable | β | t | p | Partial r |
| Caregiver RCAS Interpersonal Support | −.247 | t(43)= −2.277 | .028 | −.328 |
| Caregiver education | .522 | t(43) = 4.520 | < .001 | .568 |
| Results for significant predictors and covariates (full model) | ||||
| Model: F(5,39)= 7.170, p < .001, R2= .479, R2ADJUSTED= .412 | ||||
| Variable | β | t | p | Partial r |
| Patient RCAS Plead | −.452 | t(34)= −4.378 | < .001 | −.600 |
| Caregiver RCAS Interpersonal Support | −.410 | t(34)= −3.224 | .003 | −.484 |
| Caregiver education | .253 | t(34) = 2.458 | .019 | .388 |
| Patient symptom severity | −.193 | t(34) = −2.067 | .046 | −.334 |
Survival Analysis
Results of the Life Tables function indicated that the majority of families who left treatment prematurely dropped out after randomization (session 0) and before session 1. Sessions 1 through 3 experienced the next highest losses of families to premature dropout. However, the likelihood of premature dropout decreased with each session. Results also demonstrated that no families left treatment from session 10 onwards with the proportion of those lost to premature dropout remaining the same for sessions 10 through 15. In other words, if families were able to remain in treatment until session 10 (which coincides with the end of the religiosity segment), their risk of dropout was essentially nonexistent. Please see Graph 1 for life tables graph (pg. 33) and Table 6 (pg. 34) for the number of families that dropped out per session as well as proportion terminated, proportion surviving, probability density, and hazard rates.
Graph 1.
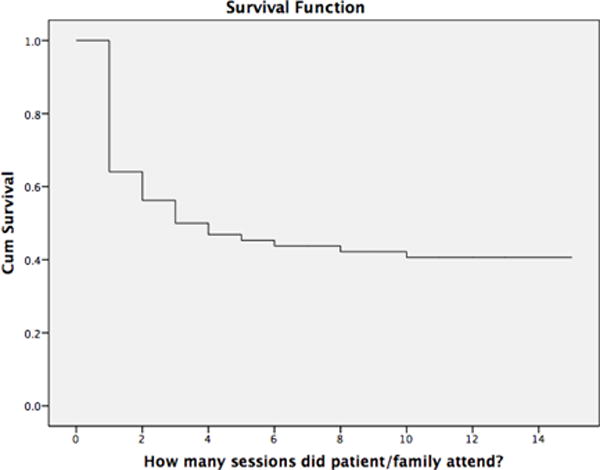
Cumulative Proportion of Completer Families (TREATMENT NAME)
Table 6.
Survival Analysis data by Session
| Session | # of dropout families | Proportion terminated | Proportion surviving | Probability Density | Hazard Rate |
|---|---|---|---|---|---|
| 0 | 23 | .36 | .64 | .359 | .44 |
| 1 | 5 | .12 | .88 | .078 | .13 |
| 2 | 4 | .11 | .89 | .063 | .12 |
| 3 | 2 | .06 | .94 | .031 | .06 |
| 10–15 | 0 | 0 | .41 | .000 | .000 |
Results of the Kaplan-Meier analysis for Patient RCAS Plead indicated significant between-group differences such that families with patients who had low plead scores attended a greater number of therapy sessions when compared to families in which patients had high scores. Please see page 34 for graph and Log Rank (Mantel-Cox) test results. Results of the Kaplan-Meier analysis for Caregiver RCAS Good Deeds also indicated significant between-group differences in which families with caregivers who had low good deeds scores attended a greater number of therapy sessions when compared to families in which caregivers had high scores. Please see page 34 for graph and Log Rank (Mantel-Cox) test results. Results for the following variables did not demonstrate significant between-group differences: Patient psychiatric symptom severity, Patient FES Religiosity, Patient RCAS Interpersonal Religious Support, and Caregiver RCAS Interpersonal Religious Support.
DISCUSSION
The primary objective of the current study was to assess whether religiosity predicted premature dropout from a culturally informed family intervention for schizophrenia. We hypothesized that for patients and caregivers, higher levels of adaptive religious coping would be associated with a greater number of family therapy sessions attended. We also hypothesized that higher levels of maladaptive religious coping would be associated with fewer sessions attended. Surprisingly, and contrary to expectations, within our sample, greater religiosity was associated with attending fewer family therapy sessions. In the current study, this pattern was observed across adaptive and maladaptive religious coping, across analyses, and for patients and caregivers alike.
Many ethnic minorities such as Hispanics/Latinos and Blacks believe that mental illness is “an issue of faith” (Avent, Cashwell, & Brown-Jeffy, 2013; Campbell & Long, 2014). Unfortunately, individuals who attempt to treat their mental illness solely with faith and prayer but continue to experience distressing symptoms may be met with unhelpful statements/beliefs which contribute to feelings of shame and guilt (e.g., “You didn’t pray hard enough.” or “You don’t have enough faith;” Campbell & Long, 2014). Thus, for many, the stigma and shame associated with having a mental health problem may represent major barriers to seeking or sticking with professional, secular care (Avent et al., 2013; Hamid & Furnham, 2013). Families in the current study were able to overcome the aforementioned barriers and seek professional mental healthcare. However, families with religious caregivers and/or patients attended fewer therapy sessions when compared to their less religious counterparts. Interestingly, even though religion/spirituality is an important culturally informed module of the [BLIND] treatment, families with religious caregivers or patients were still at an increased likelihood of premature dropout. In other words, religious families attended fewer sessions, despite religion/spirituality being one of the topics covered.
Study results may be explained by the “religiosity gap” theory. This theory posits that religious individuals may expect or assume that there will be fundamental differences in belief systems between them and their mental health professionals or, that their therapist may attempt to dissuade them from their faith (Crosby & Bossley, 2012). Thus, it is possible that within our sample, religious families did not feel comfortable discussing their faith or religious beliefs with therapists from the current study. Instead of censoring themselves, feeling uncomfortable, or feigning agreement with the views presented regarding the etiology and treatment of schizophrenia, they may have preferred to look for a treatment that was congruent with their beliefs (Crosby & Bossley, 2012). Results from our survival analyses support this assertion as most families who left treatment did so within the first three sessions. Interestingly, results also demonstrated that once [BLIND] families made it to session 10 and had completed the religion/spirituality module, the likelihood of leaving treatment prematurely dropped to zero. This pattern seems to suggest that once therapists were able to demonstrate their openness, acceptance, and willingness to explore a family’s belief system, the family was then willing to complete the full course of treatment. Although the majority of families did not provide an exact reason as to why they dropped out of treatment, one caregiver explicitly reported that due to church involvement, the patient had been cured of the illness and treatment was no longer needed. Study results may suggest that regardless of whether their coping strategies are adaptive or not, religious individuals may already be receiving support, guidance, and other resources from their spiritual institutions which could impact their willingness to remain in treatment elsewhere. Relatedly, religious families may have been less likely to believe in the efficacy of secular mental health treatments. While it is very likely that some [BLIND] families had reasons for leaving treatment prematurely that were unrelated to their religious beliefs, it is also possible that some families held beliefs they felt were incongruent with our treatment and simply did not share them with us.
In the current study, results also demonstrated that higher levels of caregiver education and less severe patient psychiatric symptom severity were strong predictors of a decreased likelihood of attrition. These results are consistent with prior research and further underscore the need to address why certain populations are more likely to drop out of treatment prematurely. Patients with greater symptom severity may have greater difficulty staying organized and keeping track of their schedule. Similarly, the robust relationship between caregiver education and attrition may convey information about family members’ day-to-day lives and how this might influence treatment-related decisions. Since education level and SES are closely tied, individuals with lower levels of education may face unique challenges (e.g., long and inflexible work schedules/multiple jobs, financial hardships, childcare and transportation issues) which must be addressed before these families can truly be invested and remain in treatment. Among families that provided a reason for dropout, financial difficulties and work schedule conflicts were the most commonly reported reasons for premature dropout.
Future Directions
The marketing and advertising of interventions and studies could be an effective communication and educational tool to begin to reduce the religiosity gap even before families enter treatment. By using advertisements that convey that individuals from diverse cultural and/or religious backgrounds are welcome to participate and that their existing beliefs will be incorporated into treatment by skilled, culturally sensitive therapists, we may be able to change how families perceive treatment. Instead of assuming that there will be a cultural mismatch, families may approach with intrigue and excitement. It is important to communicate that religious beliefs and/or services and mental health care are not mutually exclusive and mental health interventions will not attempt to dissuade participants from existing religious beliefs. These ideas should be emphasized and repeated throughout the course of treatment. In the future, it will also be useful to examine how retention rates would be impacted by modifying the order of how materials are presented in religiously based treatments (such as [BLIND]) that also contain secular modules. For example, by putting the religion/spirituality module earlier in the sequence, families may feel that the treatment is more compatible with their values, which may enhance rapport and reduce the likelihood of premature dropout. It will also be important in future research to evaluate whether collaborations with religious institutions and leaders could help to improve engagement and retention rates in psychotherapy programs. Future studies should continue to explore religiosity and other important sociocultural variables and their relationships with treatment-related beliefs, behaviors, and decisions to prematurely terminate treatment (e.g., beliefs about the efficacy of secular mental health treatment, in relation to religiosity and treatment attrition). In addition, cultural and religious beliefs should continue to be explored in ethnic minority groups. Despite [BLIND] being specifically designed to address a family’s unique cultural and religious/spiritual beliefs, no [BLIND] families with Black caregivers completed the treatment. As such, it may be particularly important to explore cultural views and norms in Black families to obtain a better understanding of their typically high dropout rates.
Limitations and Conclusions
The current study had a modest sample size which may have prevented us from identifying some significant relationships that might be detected with larger samples. It is also important to note that there may have been key differences in families who were willing to come in for treatment versus those who did not attend. In addition, although families with religious individuals were found to attend fewer sessions, it is possible that some religious families left treatment prematurely for reasons unrelated to their religious beliefs. Research designed to more comprehensively and systematically pinpoint why participants drop out of treatment could enhance future research. In conclusion, results from the current study indicate that religious clients are at greater risk of dropping out of family based treatments for schizophrenia. Study results may suggest that greater collaboration between religious institutions and mental health care providers is warranted. Additionally, it will be important to convey to clients that faith and mental health care do not have to be mutually exclusive entities.
Figure 1.
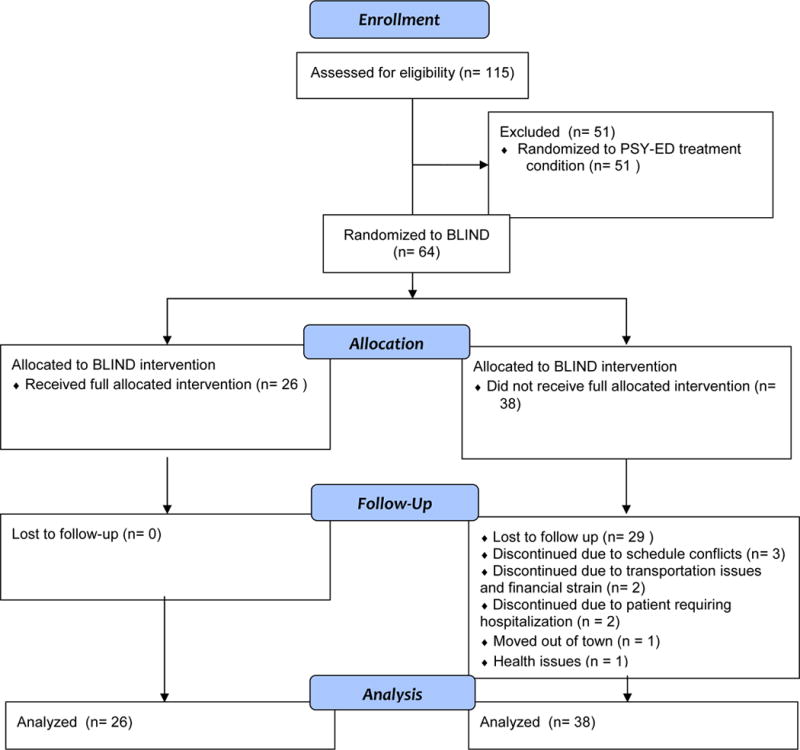
CONSORT Flow Diagram
Graph 2.
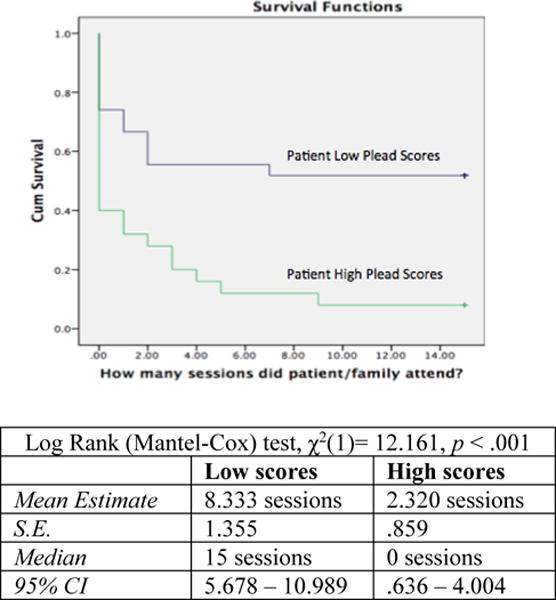
Cumulative Probability of Survival Based on High vs. Low Patient RCAS Plead Scores
Graph 3.
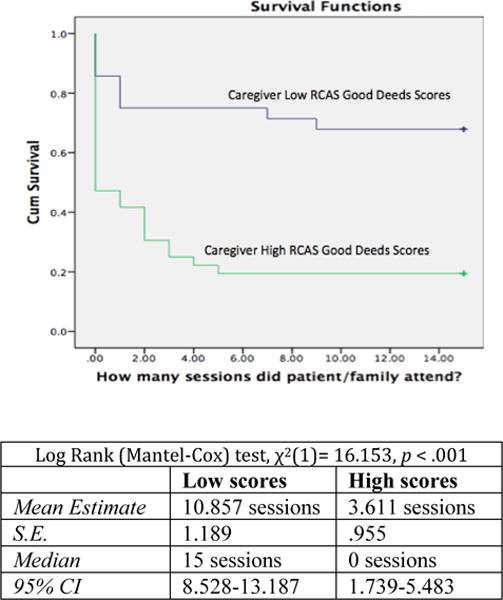
Cumulative Probability of Survival Based on High vs. Low Caregiver RCAS Good Deeds Scores
Public Health Significance Statement.
Results demonstrate that religious individuals (caregivers and patients) attended fewer family therapy sessions for schizophrenia. Findings suggest that changes to how family treatments are marketed and presented may be warranted so religious families do not feel that psychological treatments and religious beliefs are mutually exclusive.
Footnotes
Throughout this paper, we utilize the broad terms White, Black, and Hispanic/Latino. While we recognize that some readers may prefer different terminology, we aimed to use the most inclusive terms recommended by APA (e.g., Blacks to refer to African Americans and Caribbean Blacks). Several of the studies cited in this paper examined specific subgroups (e.g., Mexican Americans). We refer readers to these papers if they are interested in learning more about a specific group.
In the current study, we analyzed the relationships between potential covariates (patient and caregiver age, gender, ethnicity, education, patient symptom severity) to assess whether any of these mediated or moderated the relationship between religion and attrition/sessions attended. With respect to mediation, neither education nor patient symptom severity were associated with both religion and attrition (a necessary prerequisite for mediation). Therefore, full mediation models were not assessed. In addition, there were no significant interactions between the other covariates and religiosity in predicting attrition/sessions attended. Thus, moderation was not supported either.
References
- Avent JR, Cashwell CS, Brown-Jeffy S. African American pastors on mental health, coping, and help seeking. Counseling and Values. 2013;60:32–47. [Google Scholar]
- Borras L, Mohr S, Brandt PY, Gillieron C, Eytan A, Huguelet P. Religious beliefs in schizophrenia. Schizophrenia Bulletin. 2007;33:1238–1246. doi: 10.1093/schbul/sbl070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell RD, Long LA. Cultural as a social determinant of mental and behavioral health: A look at culturally shaped beliefs and their impact on help-seeking behaviors and service use patterns of black Americans with depression. Best Practices in Mental Health. 2014;10:48–62. [Google Scholar]
- Chatters L, Taylor R, Jackson J, Lincoln K. Religious coping among African-Americans, Caribbean Blacks and Non-Hispanic Whites. Journal of Community Psychology. 2008;36:371–386. doi: 10.1002/jcop.20202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosby JW, Bossley N. The religiosity gap: preferences for seeking help from religious advisors. Mental Health, Religion & Culture. 2012;15:141–159. [Google Scholar]
- Curran P, West S, Finch J. The robustness of test statistics to nonnormality and specification error in confirmatory analysis. Psychological Methods. 1996;1:16–29. [Google Scholar]
- Dessio W, Wade C, Chao M, Kronenberg F, Cushman LE, Kalmuss D. Religion, spirituality, and healthcare choices of African-American women: Results of a national survey. Ethnicity and Disease. 2004;14:189–197. [PubMed] [Google Scholar]
- Dixon L, Lyles A, Scott J, Lehman A, Postrado L, Goldman H, McGlynn E. Services to families of adults with schizophrenia: From treatment recommendations to dissemination. Psychiatric Services. 1999;50:233–238. doi: 10.1176/ps.50.2.233. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Moric M, Husfeldt B, Buvanendran A, Ivankovich O. Ethnic similarities and differences in the chronic pain experience: A comparison of African American, Hispanic, and White patients. Pain Medicine. 2005;6:88–98. doi: 10.1111/j.1526-4637.2005.05007.x. [DOI] [PubMed] [Google Scholar]
- Esterberg ML, Compton MT. Causes of schizophrenia reported by family members of urban African American hospitalized patients with schizophrenia. Comprehensive Psychiatry. 2006;47:221–226. doi: 10.1016/j.comppsych.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Falloon IRH, Boyd JL, McGill CW. Family care of schizophrenia: A problem solving approach to the treatment of mental illness. New York, NY: Guilford Press; 1984. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition (SCID- I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Geisinger KF. Cross-cultural normative assessment: Translation and adaptation issues influencing the normative interpretation of assessment instruments. Psychological Assessment. 1994;6:304–312. [Google Scholar]
- Goldstein MJ, Miklowitz DJ. The effectiveness of psychoeducational family therapy in the treatment of schizophrenic disorders. Journal of Marriage and Family Therapy. 1995;21:361–376. [Google Scholar]
- Hamid A, Furnham A. Factors affecting attitudes towards seeking professional help for mental illness: a UK Arab perspective. Mental Health, Religion & Culture. 2013;16:741–758. [Google Scholar]
- Harris PM. Attrition revisited. American Journal of Evaluation. 1998;19:293–305. [Google Scholar]
- Hooper MW, Baker EA, Rodriguez de Ybarra D, McNutt M, Ahluwalia JS. Acculturation Ppedicts 7-Day smoking cessation among treatment-seeking African-Americans in a group intervention. Annals of Behavioral Medicine. 2012;43:74–83. doi: 10.1007/s12160-011-9304-y. [DOI] [PubMed] [Google Scholar]
- Ironson G, Stuetzle R, Ironson D, Balbin E, Kremer H, George A, Schneiderman N, Fletcher MA. View of God as benevolent and forgiving or as harsh and punishing predicts disease progression. Journal of Behavioral Medicine (Special Issue on Spirituality and Health) 2011;34(6):414–425. doi: 10.1007/s10865-011-9314-z. [DOI] [PubMed] [Google Scholar]
- Kinney AY, Emery G, Dudley WN, Croyle RT. Screening behaviors among African American women at high risk for breast cancer: Do beliefs about God matter? Oncology Nursing Forum. 2002;29:835–843. doi: 10.1188/02.ONF.835-843. [DOI] [PubMed] [Google Scholar]
- Lee SA, Roberts LB, Gibbons JA. When religion makes grief worse: Negative religious coping as associated with maladaptive emotional responding patterns. Mental Health, Religion, and Culture. 2013;16:291–305. [Google Scholar]
- Lukoff D, Nuechterlein KH, Ventura J. Appendix A: Manual for expanded brief psychiatric rating scale (BPRS) Schizophrenia Bulletin. 1986;12:594–602. [Google Scholar]
- Miklowitz DJ. Bipolar disorder: A family-focused treatment approach. 2nd. New York, NY: Guilford Press; 2008. [Google Scholar]
- Miklowitz DJ, Goldstein MJ. Bipolar disorder: A family-focused treatment approach. New York, NY: Guilford Press; 1997. [Google Scholar]
- Moos RH, Moos B. Manual for the family environment scale. Palo Alto, CA: Consulting Psychologists Press; 1981. [Google Scholar]
- Moos RH, Moos BS. A typology of family social environments. Family Process. 1976;15:357–371. doi: 10.1111/j.1545-5300.1976.00357.x. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Glynn SM. Behavioral family therapy for psychiatric disorders. 2nd. Oakland, CA: New Harbinger; 1999. [Google Scholar]
- O’Brien A, Fahmy R, Singh SP. Disengagement from mental health services: A literature review. Social Psychiatry and Psychiatric Epidemiology. 2009;44:558–568. doi: 10.1007/s00127-008-0476-0. [DOI] [PubMed] [Google Scholar]
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychological Reports. 1962;10:799–812. [Google Scholar]
- Pargament KI, Kennell J, Hathaway W, Grevengoad N, Newman J, Jones W. Religion and problem-solving: Three styles of coping. Journal of Clinical Psychology. 1988;56:193–207. [Google Scholar]
- Pargament KI, Ensing DS, Falgout K, Olsen H, Reilly B, Van Haitsma K, Warren R. God help me: (I): Religious coping efforts as predictors of the outcomes to significant negative life events. American Journal of Community Psychology. 1990;18:793–824. [Google Scholar]
- Pargament KI, Smith B, Koenig HG, Perez L. Patterns of positive and negative religious coping with major life stressors. Journal for the Scientific Study of Religion. 1998;37:710–724. [Google Scholar]
- Phillips RE, Stein CH. God’s will, God’s punishment or God’s limitations? Religious coping strategies reported by young adults living with serious mental illness. Journal of Clinical Psychology. 2007;63:529–540. doi: 10.1002/jclp.20364. [DOI] [PubMed] [Google Scholar]
- Pitschel-Walz G, Leucht S, Bäuml J, Kissling W, Engel RR. The effect of family interventions on relapse and rehospitalization in schizophrenia- A meta analysis. Schizophrenia Bulletin. 2001;27:73–92. doi: 10.1093/oxfordjournals.schbul.a006861. [DOI] [PubMed] [Google Scholar]
- Salmoiraghi A, Sambhi R. Early termination of cognitive-behavioral interventions: Literature review. The Psychiatrist. 2010;34:529–532. [Google Scholar]
- Swift JK, Greenberg RP. Premature siscontinuation in adult psychotherapy: A meta-analysis. Journal of Consulting and Clinical Psychology. 2012;80:547–559. doi: 10.1037/a0028226. [DOI] [PubMed] [Google Scholar]
- Tabak NT, Weisman de Mamani A. Religion’s effect on mental health in schizophrenia: Examining the roles of meaning-making and seeking social support. Clinical Schizophrenia and Related Psychoses. 2014;8:91–100. doi: 10.3371/CSRP.TUWE.021513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson MP, Vardaman PJ. The role of religion in coping with the loss of a family member to homicide. Journal for the Scientific Study of Religion. 1997;36:44–51. [Google Scholar]
- Ventura J, Liberman RP, Green MF, Shaner A, Mintz J. Training and quality assurance with the structured clinical interview for DSM-IV (SCID-I/P) Psychiatry Research. 1998;79:163–173. doi: 10.1016/s0165-1781(98)00038-9. [DOI] [PubMed] [Google Scholar]
- Weisman A. Integrating culturally based approaches with existing interventions for Hispanic/Latino families coping with schizophrenia. Psychotherapy: Theory, Research, Practice, Training. 2005;42:178–197. [Google Scholar]
- Weisman AG. Understanding cross-cultural prognostic variability for schizophrenia. Cultural Diversity and Mental Health. 1997;3:23–35. [PubMed] [Google Scholar]
- Weisman AG, López SR. Family values, religiosity and emotional reactions to schizophrenia in Mexican and Anglo-Americans cultures. Family Process. 1996;35:227–237. doi: 10.1111/j.1545-5300.1996.00227.x. [DOI] [PubMed] [Google Scholar]
- Weisman AG, Gomes L, López SR. Shifting blame away from ill relatives: Latino families’ reactions to schizophrenia. The Journal of Nervous and Mental Disease. 2003;191:574–581. doi: 10.1097/01.nmd.0000087183.90174.a8. [DOI] [PubMed] [Google Scholar]
- Weisman A, Rosales G, Kymalainen J, Armesto J. Ethnicity, family cohesion, religiosity and general emotional distress in patients with schizophrenia and their relatives. Journal of Nervous and Mental Disease. 2005;193:359–368. doi: 10.1097/01.nmd.0000165087.20440.d1. [DOI] [PubMed] [Google Scholar]
- Wierzbicki M, Pekarik G. A meta-analysis of psychotherapy dropout. Professional Psychology: Research and Practice. 1993;24:190–195. [Google Scholar]


