Abstract
OBJECTIVE
To review publications that address female reproductive health hazards in veterinary practice, summarize best practices to mitigate reproductive risks, and identify current knowledge gaps.
DESIGN
Systematized review.
SAMPLE
English-language articles describing chemical, biological, and physical hazards present in the veterinary workplace and associations with adverse reproductive outcomes or recommendations for minimizing risks to female reproductive health.
PROCEDURES
Searches of the CAB abstracts database were performed in July 2012 and in May 2015 with the following search terms: veterinarians AND occupational hazards and vets.id AND occupational hazards.sh. Searches of the PubMed database were conducted in November 2012 and in May 2015 with the following medical subject heading terms: occupational exposure AND veterinarians; anesthetics, inhalation/adverse effects AND veterinarians; risk factors AND pregnancy AND veterinarians; pregnancy outcome AND veterinarians; and animal technicians AND occupational exposure. Two additional PubMed searches were completed in January 2016 with the terms disinfectants/toxicity AND female AND fertility/drug effects and veterinarians/psychology AND stress, psychological. No date limits were applied to searches.
RESULTS
4 sources supporting demographic trends in veterinary medicine and 118 resources reporting potential hazards to female reproductive health were identified. Reported hazards included exposure to anesthetic gases, radiation, antineoplastic drugs, and reproductive hormones; physically demanding work; prolonged standing; and zoonoses.
CONCLUSIONS AND CLINICAL RELEVANCE
Demographic information suggested that an increasing number of women of reproductive age will be exposed to chemical, biological, and physical hazards in veterinary practice. Information on reproductive health hazards and minimizing risk, with emphasis on developing a safety-focused work culture for all personnel, should be discussed starting in veterinary and veterinary technical schools and integrated into employee training.
Most veterinary personnel engaged in clinical practice are generalists who, during a routine work day, may be exposed to ionizing radiation, anesthetic gases, zoonotic diseases, and trauma from fractious animals—both large and small. No other medical profession is required to assess and manage such a wide range of workplace exposures to chemical, biological, and physical hazards.1–8
Reproductive hazards are those hazards that may negatively impact fertility or pregnancy. The review reported here focused on pregnant women and women of childbearing age working in veterinary practice. Reproductive hazards common in the veterinary workplace can be categorized as chemical, biological, and physical hazards. Chemical hazards include contact with antineoplastic drugs, hormones, pesticides, and anesthetic gases; biological hazards include zoonotic and other infectious agents; and physical hazards include animal-related injuries, radiation exposure, demanding work conditions and physical work load, needle sticks, and psychosocial hazards from workplace stress, long work hours, and other factors that affect mental well-being.
The proportion of women in the veterinary profession in the United States has increased in recent years. More than 90% of veterinary technicians are, and historically have been, female.9 Of 105,000 US veterinarians actively practicing in 2015, 58% were women, and more than 80% of new graduates were women.10,11 This represents a dramatic shift from the demographic 50 years ago, when almost 90% of US veterinary students were male.12 As older male veterinarians retire from practice and are replaced by new female graduates, an increasing number of women of reproductive age will encounter workplace hazards that may pose undefined risks to fertility as well as to an embryo or fetus during pregnancy.
Comprehensive guidance to prevent or mitigate exposures to occupational reproductive health hazards for female veterinary personnel is greatly needed.13 In recognition of this, the NIOSH, in partnership with the National Occupational Research Agenda and other stakeholders, finalized a series of goals including raising awareness of reproductive hazards, formulating recommendations to mitigate them, and developing fact sheets and other outreach materials for veterinary personnel.13
The objectives of the study reported here were to conduct a systematized review of retrievable publications addressing hazards to female reproductive health in the veterinary workplace, to evaluate and summarize recommendations to minimize reproductive risks in veterinary practice, and to identify gaps in current knowledge related to these risks. This report is intended to provide a framework for education, research, and future development of materials in this area.
Materials and Methods
Searches of the CAB abstracts database were conducted in July 2012 and in May 2015. Two sets of search terms, veterinarians AND occupational hazards and vets.id AND occupational hazards.sh, were used without date limits, and both searches yielded the same results. Searches of PubMed without date limits were conducted in November 2012 and in May 2015, with the following MeSH search terms used: occupational exposure AND veterinarians; anesthetics, inhalation/adverse effects AND veterinarians; risk factors AND pregnancy AND veterinarians; pregnancy outcome AND veterinarians; and animal technicians AND occupational exposure. Two alternate MeSH search terms for the last string, veterinary nurse AND occupational exposure and risk factors AND pregnancy AND animal technicians, produced the same results. Two additional PubMed searches without date limits were completed in January 2016 to discover reproductive hazards related to disinfectants and hazards posed by psychosocial factors. These included MeSH search terms of disinfectants/toxicity AND female AND fertility/drug effects and veterinarians/psychology AND stress, psychological. Additional articles and recommendations were identified on US government and AVMA websites pertaining to reproductive health and by manually searching article reference lists.
The articles were divided among all 4 authors for review, and results were recorded on a shared spreadsheet. We determined relevance to veterinary occupational health and reproductive health and whether the article included best practices for prevention, control, and mitigation of reproductive hazards. References that were not written in English language were excluded. Articles that did not relate to occupational health or reproductive health or were not available were excluded. Excluded articles underwent a second evaluation by 2 reviewers (JMS and BLE).
Information recorded from the literature search included authorship information; title, journal, and year of publication; study type or design; resource type (eg, peer-reviewed journal article, non–peer-reviewed journal article, or meeting proceedings); reproductive hazard; reviewer comments; reviewer; and date. A spreadsheet template was used to organize relevant articles according to hazard (chemical, biological, physical, or general [for resources covering multiple hazards]) and strength of evidence. Strength of evidence was classified as primary, supportive, or anecdotal. Anecdotal publications were those that contained opinions or observations by experts but did not include objective safety data. Publications such as reviews, in which hazards and practices were described but lacked original data to support recommendations, were considered to have supportive evidence. Original studies that included statistically significant associations in reporting risk or contained quantitative or descriptive data to support recommendations were considered primary resources. Except for hazards such as zoonotic diseases with rare outcomes, reproductive risks reported here were supported by primary resources that reported statistically significant associations.
Results
Evaluation of 521 unique articles led to identification of 99 references that described chemical, biological, and physical hazards present in the veterinary workplace and their association with adverse reproductive outcomes, or contained recommendations for minimizing risk from exposure to reproductive hazards (Figure 1). These were categorized as primary (n = 57), supportive (41), or anecdotal (1). Thirty-four of 66 (52%) published papers pertaining specifically to veterinary occupational health focused predominantly on veterinarians, and 32 (48%) included all veterinary personnel, including veterinarians. In addition, 4 sources identifying demographic trends and 19 US government documents, US government websites, or AVMA websites containing information about reproductive health hazards and their mitigation were identified and included without categorization.
Figure 1.
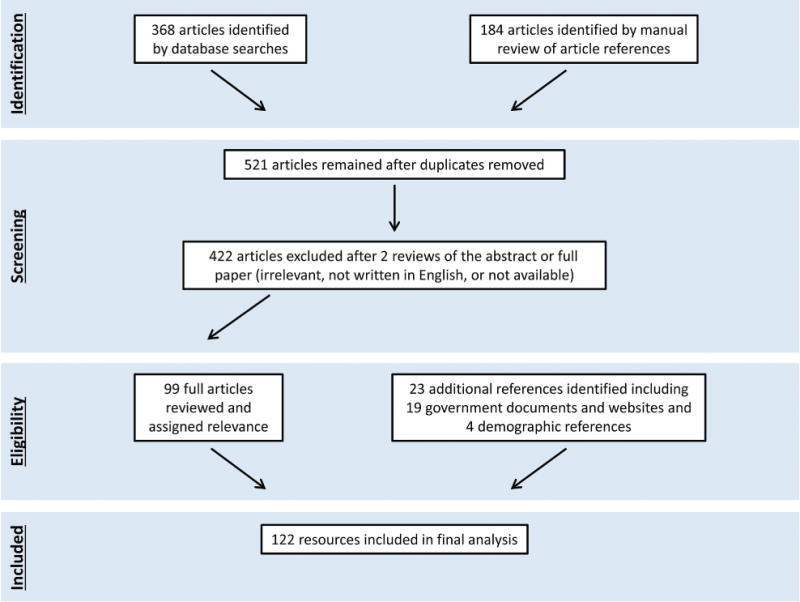
Diagram depicting resource selection process and outcome for a systematized review of hazards to female reproductive health in veterinary practice.
Chemical hazards
Chemical hazards in veterinary medical settings, including those from antineoplastic drugs and other pharmaceuticals, are often similar to those in human health care14 and have been identified and listed by the NIOSH.15 Safety data sheets for disinfectants and other chemicals are readily available both from the manufacturer and online. However, these documents do not always provide all necessary information for assessing health risks, and it is often necessary to consult other sources of information to fully assess health hazards from chemicals. The OSHA has published standards and the NIOSH has published guidelines addressing chemical hazards, including how these hazards should be communicated to workers who may be exposed occupationally.16–18 Similar to other health-care and industry settings, veterinary practices are subject to the OSHA Hazard Communication Standard18; information specific to veterinary medicine can be found on the AVMA website.19 Chemical exposures identified through the literature search that could present a risk to female reproductive health, and best practices to prevent or mitigate such exposures, were summarized (Table 1).6,15–17,20–45
Table 1.
Chemical hazards present in veterinary workplaces and recommendations for mitigation of risks to female reproductive health identified in the literature.
| Hazard | Reproductive risk | Best practices to mitigate risk |
|---|---|---|
| Anesthetic gases | Spontaneous abortions20 and preterm birth21 | Install scavenging and ventilation systems6,20–26
Properly inspect and maintain anesthesia machines, breathing circuits, and waste-gas scavenging systems6,22,25,26
Perform a comprehensive maintenance inspection annually Train all workers in hazard awareness, prevention, and control of exposures to waste anesthetic gases25 Inform female veterinary personnel of the risks27–29 |
| Carbon monoxide | Fetal anoxia leading to fetal death23 | Do not enter a poorly ventilated, artificially heated area where animals may be ill or dying, because of a potential for carbon monoxide exposure23 |
| Antineoplastic drugs and other hazardous pharmaceuticals | Reduced fertility, fetal loss, spontaneous abortion, preterm birth, and low birth weight30–32 | Read and follow recommendations in the following publications:
Other prevention practices for handling antineoplastic and other hazardous pharmaceuticals include the following:
Practice institution-wide prevention strategies,37 develop written chemotherapy safety protocols,33 and communicate risk and prevention strategies to employees32,33 |
| Ethylene oxide (gas sterilization) | Spontaneous abortion26 | Ethylene oxide gas sterilization procedures should be avoided in general veterinary practice because of the challenges involved with safe use26 If ethylene oxide is to be used, consult OSHA guidance documents39 and OSHA standards document 29 CFR 1910.1047,40 and observe the following:
|
| Insecticides and other pesticides | Birth defects41 and spontaneous abortion29 | Consult safety data sheets for the compounds42,43 Use appropriate protective measures to prevent or minimize exposure42 Avoid extralabel use42 Be aware that pesticide concentrates that require dilution pose a higher risk of exposure Avoid using materials that may absorb the compound and release it later43 Inform female veterinary personnel of possible reproductive effects of pesticide exposure29,44 Use extreme caution and biological monitoring to regulate occupational exposure to organophosphates41,43 |
| Prostaglandins and other reproductive hormones (eg, GnRH analog, human chorionic gonadotropin, estrogen, progester one, synthetic progestin, testosterone, and oxytocin) | Spontaneous abortion, fetal death (PGF2α and its analog), prolongation of pregnancy (synthetic progestin), disruption of menstrual cycle (GnRH analog, synthetic progestin), and increased or decreased uterine bleeding (synthetic progestin)23,45 |
Pregnant women should not handle or administer prostaglandin products23,45 Avoid direct skin contact by wearing impervious gloves during drug handling; wash hands immediately after removing gloves; adhere to manufacturers’ safety warnings45 When specific warnings and guidelines are not provided, follow NIOSH guidelines15–17 If contact with skin occurs, wash the affected area immediately and seek medical attention45 |
DHHS = US Department of Health and Human Services. GnRH = Gonadotropin-releasing hormone. PG = Prostaglandin.
Antineoplastic pharmaceuticals, primarily used to treat cancer in dogs and cats, are important reproductive hazards found in the veterinary setting.46 Many antineoplastic drugs have been reported to be carcinogenic, mutagenic, or teratogenic and have been associated with reduced fertility, spontaneous abortion, and fetal loss.30–32,46–49 Usage and exposure estimates have been reported for veterinary personnel in Canada46 and the Netherlands,50 where concerning exposures during preparation and administration of antineoplastic drugs were documented. No such antineoplastic pharmaceutical usage or exposure data for US veterinary personnel were identified in the literature search.
Reproductive hormones used in contemporary veterinary practice are especially hazardous to pregnant women. Prostaglandins, in particular, should be avoided during pregnancy; these and other reproductive hormones warrant meticulous care and training in their use.23
Beginning in the 1960s and 1970s, there was substantial concern about the effects of inhaled anesthetic gases on reproduction in health-care workers.51–56 In response, the NIOSH published recommendations for reducing exposure and risk.57 Importantly, most of the early epidemiological reports linking waste anesthetic gas exposure to adverse health events have since been critically reviewed and faulted for inappropriate design or improper statistical analysis.58–61 Thus, a direct cause-and-effect relationship between long-term exposure to waste anesthetic gas and adverse reproductive health events has not been firmly established. However, Boivin20 performed a meta-analysis of epidemiological studies and found that data obtained prior to the routine use of scavenging systems (exhaust systems to remove excess anesthetic gases) indicated an increased risk of spontaneous abortion, and Shirangi et al21 found an increased risk of preterm delivery in women exposed to unscavenged waste anesthetic gas for ≥ 1 h/wk, compared with that for an unexposed group. At the present time, owing to the almost universal adoption of scavenging systems, reproductive risk from occupational exposure to inhalation anesthetics in veterinary personnel appears to be minimal.27,58,59,61–65 Nevertheless, it remains prudent to recommend control measures that reduce occupational exposure.51,58–60,24,25,66
Awareness of potential health hazards from chemicals and pharmaceuticals, along with adoption of measures to reduce potential for exposure, are essential to prevent or reduce adverse health events.67 This can be accomplished through elimination or substitution of the chemical, changes to work practices, and use of personal protective equipment.46
Biological hazards
Exposure to biological hazards is inevitable when working closely with animals.68–72 A subset of these hazards may pose a particular risk for maternal and fetal health, including some zoonotic bacterial and viral pathogens and certain infectious agents that pose an increased risk of illness to immunocompromised individuals (including pregnant women); the most common of these were tabulated with recommendations for prevention (Table 2).23,26,68,70,72–84 The many zoonoses (eg, rabies virus, Salmonella spp, or herpesvirus B) that can adversely impact human health regardless of pregnancy status were not included in the summary.
Table 2.
Biological hazards present in veterinary workplaces and recommendations for mitigation of risks to female reproductive health identified in the literature.
| Hazard | Reproductive risk | Best practices to mitigate risk |
|---|---|---|
| Brucellosis (Brucella spp) | Preterm delivery and low birth weight70 | Use standard precautions72 Be aware of risk and attain prompt diagnosis70 Consult an infectious disease specialist if symptoms develop70 Report infection to animal and public health authorities72 |
| Leptospirosis (Leptospira interrogans) | Infection of the embryo or fetus with outcomes ranging from midgestational fetal death to birth of a healthy infant; maternal death can also occur73,74 | Use standard precautions72 Consult an infectious disease specialist if symptoms develop73 Contact local or state health departments for guidance following potential exposure72 Wear gloves when handling pet rats75 |
| Listeriosis (Listeria monocytogenes) | Preterm labor, fetal death, stillbirth, and Listeria septicemia and meningitis of the neonate26 | Wear gloves, facial protection, and protective clothing while working with aborted fetuses and tissues or fluids expelled by the dam23,72 Use extra caution when working with sheep, goats, and cattle during pregnancy26 |
| Lymphocytic choriomeningitis virus infection | Spontaneous abortion and severe birth defects (eg, chorioretinitis, hydrocephalus, and mental retardation)76 | Wear gloves and facial protection when handling rodents while pregnant72 Avoid sweeping or vacuuming rodent urine, droppings, and nesting materials72 Report infection to public health authorities72 |
| Gestational psittacosis (Chlamydophila psittaci) | Adverse pregnancy outcomes are very rare, but stillbirth has been reported77 | Wear gloves and N95 respirator when handling ill psittacine birds72 Consider all ill birds to be a potential source of infection68,72 Avoid sweeping or vacuuming bird urine, droppings, and nesting materials; use gloves, N95 respirator, goggles, and surgical cap when cleaning contaminated areas72,77 Report infection to public health authorities72 |
| Gestational chlamydiosis (Chlamydophila abortus) | Spontaneous abortion, severe chlamydiosis (coagulopathy, intense placentitis), and maternal death78 | Wear gloves, N95 respirator, and protective clothing while working with aborted sheep or goat fetuses or tissues and fluids expelled by the dam78,79 Pregnant women should avoid contact with aborting sheep and goats, if possible78 Report infection to public health authorities72 |
| Q Fever (Coxiella burnetii) | Spontaneous abortion, stillbirth, preterm birth, intrauterine growth retardation, and low birth weight80 | Consult an infectious disease specialist if symptoms develop80 Wear gloves, N95 respirator, and protective clothing when working with aborted sheep or goat fetuses or tissues and fluids expelled by the dam23,72 Use extra caution when working with sheep, goats, and cattle during pregnancy81 Report infection to public health authorities72 |
| Toxoplasmosis (Toxoplasma gondii) | Spontaneous abortion, preterm birth, stillbirth, fetal neurological damage, congenital chorioretinitis, hydrocephalus, encephalitis, and mental retardation23,26 | Avoid exposure to cat feces and litter while pregnant82 Consult a health-care provider when considering pregnancy or in early pregnancy about advisability of baseline antibody titer determination (authors’ recommendation on the basis of Weese et al82) Maintain a clinic practice of daily litter pan cleaning by nonpregnant staff members76 Use gloves when conducting feline fecal examinations and wash hands afterward83 |
| Infections from animal licks, bites, or scratches (eg, Pasturella multocida, Bartonella henselae, Capnocytophaga canimorsus) | Maternal pyrexia, premature labor, chorioamnionitis, and maternal and neonatal death76 | Counsel pregnant personnel likely to be exposed to animal flora84 Educate physicians to consider systemic infection with P multocida and other animal flora in symptomatic female veterinary personnel84 |
Emerging zoonotic diseases pose a risk to people who work at the human-animal interface. It is likely that reproductive health as well as fetal health may be acutely susceptible to adverse outcomes from emerging infectious diseases, particularly before the risk has been identified. Thus, when an emerging zoonotic disease is not yet well characterized, veterinary personnel are advised to strictly adhere to standard precautions.72,76
The proportion and magnitude of biological exposures that result in disease transmission to the veterinary workforce is poorly understood because of a lack of integrated surveillance systems for occupationally related infections. Ultimately, the advent of surveillance systems to consistently and uniformly record injuries and illnesses among veterinary personnel will better characterize the hazards so that attention and resources can be prioritized for most effective risk reduction.4,26,74,85 At present, best practices to mitigate these risks include environmental controls, written infection control policies that are consistently applied, staff training in the use of procedures and equipment to reduce risk, and use of appropriate personal protective equipment (eg, gloves, protective outerwear, and facial protection), with emphasis on groups that may be particularly vulnerable, such as pregnant women.72,82,86,87
Physical hazards
Physical hazards that can pose a risk to female reproductive health and recommended measures to prevent or mitigate injury were reviewed (Table 3).7,8,21,23,28,29,44,49,72,88–106 Prevention of physical workplace hazards in a veterinary setting is best accomplished through consistent application of safe workplace practices, such as routine use of personal dosimetry and lead apparel when performing radiography.28,92–95,97 During much of the first 7 weeks after conception, when the embryo is most susceptible to the effects of radiation, a woman may not be aware that she is pregnant. Therefore, any female veterinary personnel with the potential to be pregnant should use all available precautions when radiographic equipment is in use.23,88,96,107 Needle sticks and other traumatic physical injuries from animal bites, lifts, trips, slips, falls, and automobile accidents can be largely prevented by habitual safety practices.7,8,28,37,72,104,106 Most veterinary settings are small, and personnel are often cross-trained to perform multiple tasks, making workplace safety culture especially important in preventing accidents and injury.72
Table 3.
Physical hazards present in veterinary workplaces and recommendations for mitigation of risks to female reproductive health identified in the literature.
| Hazard | Reproductive risk | Best practices to mitigate risk |
|---|---|---|
| Radiography | Risks depend on stage of embryonic or fetal development and level of radiation exposure. Outcomes range from death of the embryo to congenital malformations and mental retardation88 | Occupational exposure limit for ionizing radiation to the fetus is 5 mSv (0.5 rem) cumulative during pregnancy, with a 0.5 mSv limit for each month of pregnancy89 Keep radiation exposure as low as reasonably achievable or as low as reasonably practicable90–93 Avoid radiographic evaluation unless it is justified90 Perform yearly safety verification of gloves and aprons, and check the tube device for leakage93 Increase distance of the individual performing radiography from the radiation source, reduce the duration and amount of exposure, and use protective barriers between the individual and the source23 Perform radiography only in controlled areas90; wear radioprotective clothing (eg, lead aprons, thyroid shields, glasses, and gloves) and use personal dosimetry badges worn on the trunk under the lead gown23,28,90,94,95; gloves and thyroid shields should have a minimum lead equivalent of 0.5 mm90 Prohibit manual restraint of animals by pregnant women during radiography90 Use tube stands or a pole with a cassette holder, rather than holding with hands, for radiography of large animals90–92 Emphasize the importance of adequate radiation protection and knowledge in schools of veterinary medicine and professional associations96 Include written policies in a practice infection control plan requiring staff members to notify hospital leadership of pregnancy as soon as the staff member becomes aware of it97 Fully inform female veterinary personnel of the risks from ionizing radiation29,44 Work with employers to reduce exposures during pregnancy and lactation23,49,90 |
| Standing at work | Preterm delivery98–100 and low birth weight101 | Pregnant personnel should not stand > 6 h/d98 Limit standing and walking at work, especially standing in 1 position, to 4 to 5 hours during the second and third trimesters99,101 |
| Long working hours | Preterm delivery21,98 | Limit work to < 42–45 h/wk21,98 |
| Physically demanding work, including lifting | Preterm delivery, maternal hypertension,100 and low birth weight102 | Reduce or eliminate physically demanding work from job duties of pregnant personnel100,103 Consult MacDonald et al (2013)102 for specific guidelines for occupational lifting during pregnancy; guidelines are given for infrequent lifting, repetitive short-duration lifting, and repetitive long-duration lifting in multiple body positions at < 20 wk of gestation and ≥ 20 wk of gestation. Reductions in recommended weight limits may need to be made for veterinary personnel, considering the unpredictability of sudden animal movement or pushing and pulling of animals during lifting that may influence recommended weight limits102 Minimize or eliminate demanding levels of physical work for women with previous complications of pregnancy that are likely to recur, such as low birth weight of infants and premature labor23 |
| Shift and night work | Preterm delivery100 | Limit shift or night work100 |
| Needle sticks | Spontaneous abortion104 | Establish a needle-stick prevention program7,8 Provide information and training on needle-stick prevention and establish written infection control policies that include needle-stick prevention72,105 Practice standard precautions when using anthelmintic, euthanasia, and anesthetic agents104 Avoid recapping needles or use a 1-handed scooping technique to recap37,72,106 Perform worksite analyses for tasks causing needle sticks106 |
Several studies21,98–100,102 identified an association between long work hours, prolonged standing at work, or physically demanding work including manual lifting, and preterm delivery or low birth weight for gestational age. Measures to mitigate certain physical hazards become more important as a pregnancy progresses, including adoption of recommended weight limits for lifting and adjusting work practices to address concerns associated with fatigue, prolonged standing or walking, and working long hours.21,23,98–103 The importance of physical work limits during pregnancy should be discussed starting in veterinary and veterinary technical schools and carried through to employee health practices in clinical settings.103 Organizational policies regarding reproductive hazards and pregnancy should be documented and clearly communicated to female employees.29,44,105
The association between serious life events and workplace stress on preterm delivery and low birth weight has been established.108–111 Specific to veterinary medicine, the literature review identified articles pertaining to stress and work-related exhaustion in the veterinary workplace98,103,112,113 and substantial and deeply concerning psychological work stress and suicidal ideation among veterinarians.114–116 Given what is known about the detrimental effects of stress on gestation, it is clear that more research in this area, focused on the veterinary community, is needed.
Available guidance resources
Guidance documents regarding veterinary workplace safety and health are available from varied sources, including the NIOSH, OSHA, and AVMA. The NIOSH provides health and safety recommendations to protect workers in workplace settings, including resources specific to workplace hazards and reproductive health117,118; the organization’s website also directly addresses veterinary safety and health.119
In the United States, the OSHA is the federal agency charged with enforcing laws regarding workplace safety and health. Exposures that occur in human as well as animal medical facilities are addressed in a variety of OSHA publications.120 Although some of the information reflects employer legal obligations, much of the guidance is intended as advisory, so that medical facility managers can optimize prevention practices. The AVMA is a member organization representing > 88,000 veterinarians.121 The AVMA’s website122 and the JAVMA frequently publish articles addressing veterinary workplace hazards and prevention guidance.
Discussion
Most veterinarians presently in practice are women, and most veterinary technician and veterinary assistant positions are, and historically have been, filled by women. The present review was performed to summarize the available information on veterinary workplace exposures that can negatively impact a woman’s reproductive health, to raise awareness of established risks, and to explore knowledge gaps related to this subject. In addition, the review identified current best practices that veterinary personnel can institute to mitigate risks associated with workplace reproductive hazards.
Exposure to anesthetic gases and ionizing radiation are reproductive hazards that are generally well recognized and addressed in most veterinary workplaces.46 Other hazards are perhaps less well understood. For example, our literature review revealed associations between long work hours, physically demanding work, or standing at work for > 4 to 6 hours at a time and preterm delivery.21,98–100,102 Historically, the veterinary profession has been a demanding, physically difficult profession often requiring long work hours. Culturally, workplace dispensations for pregnancy (or other conditions requiring special consideration) have not been the norm. Changes in workplace culture regarding perceptions of work ethic could be the most difficult adjustment that must occur to accommodate increasing numbers of women in the veterinary workplace.
We attempted to identify all publications that addressed chemical, biological, and physical hazards in veterinary practice that may impact female reproductive health. This is a broad topic, and it is possible that relevant literature was missed. We also attempted to capture all exposures relevant to veterinary personnel in the literature search; however, it is likely that some exposures that occur in other health-care disciplines and have implications for veterinary personnel were overlooked. Another potential limitation was that the review was focused on general hazard mitigation, as it was performed by public health and occupational health professionals without specialized knowledge in reproductive health.
A number of recent publications on this topic originated from sources in countries other than the United States, reflecting international recognition of the need for occupational health research and guidance for female veterinary personnel. Literature included in the review identified risks to reproductive health and recommendations to mitigate exposures. However, specific information about the extent or scope of risk, such as usage or exposure estimates for a particular hazard, was frequently lacking. Of the 66 published articles pertaining specifically to veterinary occupational health that were identified in the literature search, only 32 (48%) included veterinary technicians and other veterinary staff, a population with arguably as much exposure (or even more exposure) to most hazards as veterinarians. A better understanding of where, how, to whom, and to what extent reproductive health hazards occur in the veterinary workplace would allow for targeted interventions.46 Additional research is needed to evaluate associations between psychosocial or workplace stress, physically demanding work, zoonotic diseases, and adverse reproductive outcomes in veterinary clinical practice. In particular, there is an opportunity to apply to veterinary medicine what is known in other fields about mitigating psychosocial and workplace stress and other physical reproductive health hazards such as lifting, working long hours, and prolonged standing. Similarly, best practices for preparation and administration of antineoplastic pharmaceuticals are well established in human health care and can be used in private veterinary practice; however, data are needed on veterinary usage and exposure in the United States, and efforts should be made to increase awareness among veterinary personnel of the risks and recommendations to mitigate them. In the same way, female veterinarians, technicians, and staff represent a uniquely exposed workforce which, if followed over time, would provide health and safety information applicable to other fields involving animal care.
Although additional research is needed to more clearly define workplace hazards for female veterinary personnel, current knowledge is sufficient to justify instituting interventions to reduce reproductive risks and minimize adverse reproductive outcomes. Best practices for mitigating risk should be introduced and discussed during veterinary and veterinary technician training and integrated into employee training. Early introduction to and familiarity with reproductive health hazards and practical information about mitigating risk, with emphasis on developing a safety-focused work culture for all veterinary personnel, are critical for making the changes necessary to meet current and future veterinary occupational health challenges.
Acknowledgments
No third-party funding or support was received in connection with this study or the writing or publication of the manuscript. The authors declare that there were no conflicts of interest.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC or the Agency for Toxic Substances and Disease Registry.
The authors thank André J. Nault, from the Veterinary Medical Library at the University of Minnesota College of Veterinary Medicine, for assistance with literature searches.
ABBREVIATIONS
- NIOSH
National Institute for Occupational Safety and Health
- OSHA
Occupational Safety and Health Administration
References
- 1.Jeyaretnam J, Jones H. Physical, chemical and biological hazards in veterinary practice. Aust Vet J. 2000;78:751–758. doi: 10.1111/j.1751-0813.2000.tb10446.x. [DOI] [PubMed] [Google Scholar]
- 2.Nienhaus A, Skudlik C, Seidler A. Work-related accidents and occupational diseases in veterinarians and their staff. Int Arch Occup Environ Health. 2005;78:230–238. doi: 10.1007/s00420-004-0583-5. [DOI] [PubMed] [Google Scholar]
- 3.Wiggins P, Schenker MB, Green R, et al. Prevalence of hazardous exposures in veterinary practice. Am J Ind Med. 1989;16:55–66. doi: 10.1002/ajim.4700160107. [DOI] [PubMed] [Google Scholar]
- 4.Fowler HN, Holzbauer SM, Smith KE, et al. Survey of occupational hazards in Minnesota veterinary practices in 2012. J Am Vet Med Assoc. 2016;248:207–218. doi: 10.2460/javma.248.2.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC. Veterinary safety and health. Available at: www.cdc.gov/niosh/topics/veterinary/chemical.html. Accessed May 4, 2016.
- 6.Langley RL, Pryor WH, O’Brien KF. Health hazards among veterinarians: a survey and review of the literature. J Agromed. 1995;2:23–52. [Google Scholar]
- 7.Poole AG, Shane SM, Kearney MT, et al. Survey of occupational hazards in large animal practices. J Am Vet Med Assoc. 1999;215:1433–1435. [PubMed] [Google Scholar]
- 8.Poole AG, Shane SM, Kearney MT, et al. Survey of occupational hazards in companion animal practices. J Am Vet Med Assoc. 1998;212:1386–1388. [PubMed] [Google Scholar]
- 9.National Association of Veterinary Technicians in America. NAVTA news, NAVTA survey. 2012 Sep-Oct; Available at: c.ymcdn.com/sites/www.navta.net/resource/resmgr/NAVTA_SeptOct12_Survey.pdf. Accessed May 4, 2016.
- 10.AVMA, Association of American Veterinary Medical Colleges. 2016 AVMA & AAVMC Report on the market for veterinary education. 2016 Apr; Available at: www.avma.org/PracticeManagement/BusinessIssues/Documents/2016-econ-rpt2-mkt-vet-education.pdf. Accessed May 4, 2016.
- 11.AVMA. Market research statistics: US veterinarians. 2015 Available at: www.avma.org/KB/Resources/Statistics/Pages/Market-research-statistics-US-veterinarians.aspx. Accessed May 4, 2016.
- 12.Burns K. At veterinary colleges, male students are in the minority. J Am Vet Med Assoc. 2010;236:376–377. 384. [Google Scholar]
- 13.CDC National Institute for Occupational Safety and Health. National occupational research agenda, national healthcare and social assistance agenda for occupational safety and health research and practice in the US health-care and social assistance (HCSA) sector. 2013 Feb; Available at www.cdc.gov/niosh/nora/comment/agendas/hlthcaresocassist/pdfs/HlthcareSocAssistFeb2013pdf. Accessed Jun 30, 2016.
- 14.Meggs WJ. Chemical hazards faced by animal handlers. Occup Med. 1999;14:213–224. [PubMed] [Google Scholar]
- 15.CDC National Institute for Occupational Safety and Health. NIOSH list of antineoplastic and other hazardous drugs in healthcare settings, 2014. Cincinnati: CDC; 2014. (DHHS (NIOSH) publication No. 2014-138). Available at: www.cdc.gov/niosh/docs/2014-138/pdfs/2014-138.pdf Accessed Apr 21, 2016. [Google Scholar]
- 16.CDC National Institute of Occupational Safety and Health. Preventing occupational exposures to antineoplastic and other hazardous drugs in health care settings. Cincinnati: CDC; 2004. (DHHS (NIOSH) publication No. 2004-165). Available at: www.cdc.gov/niosh/docs/2004-165/pdfs/2004-165.pdf. Accessed Apr 21, 2016. [Google Scholar]
- 17.CDC National Institute of Occupational Safety and Health. Workplace solutions Safe handling of hazardous drugs for veterinary healthcare workers. Cincinnati: CDC; 2010. (DHHS(NIOSH) publication No. 2010-150). Available at: www.cdc.gov/niosh/docs/wp-solutions/2010-150/pdfs/2010-150.pdf. Accessed Apr 21, 2016. [Google Scholar]
- 18.US Department of Labor Occupational Safety and Health Administration website. Hazard communication. Available at: www.osha.gov/dsg/hazcom/. Accessed Apr 21, 2016.
- 19.AVMA. Workplace hazard communications. Available at: www.avma.org/KB/Resources/Reference/Pages/Workplace-Hazard-Communications.aspx. Accessed Apr 21, 2016.
- 20.Boivin JF. Risk of spontaneous abortion in women occupationally exposed to anaesthetic gases: a meta-analysis. Occup Environ Med. 1997;54:541–548. doi: 10.1136/oem.54.8.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shirangi A, Fritschi L, Holman CD. Associations of unscavenged anesthetic gases and long working hours with preterm delivery in female veterinarians. Obstet Gynecol. 2009;113:1008–1017. doi: 10.1097/AOG.0b013e31819fe996. [DOI] [PubMed] [Google Scholar]
- 22.Korczynski RE. Anesthetic gas exposure in veterinary clinics. Appl Occup Environ Hyg. 1999;14:384–390. doi: 10.1080/104732299302783. [DOI] [PubMed] [Google Scholar]
- 23.Gold CB, Beran GW. Occupational hazards to pregnant veterinarians. Iowa State Univ Vet. 1983;45:55–60. [Google Scholar]
- 24.Smith JA. Anesthetic pollution and waste anesthetic gas scavenging. Semin Vet Med Surg (Small Anim) 1993;8:90–103. [PubMed] [Google Scholar]
- 25.CDC National Institute of Occupational Safety and Health. Waste anesthetic gases: occupational hazards in hospitals. Cincinnati: CDC; 2007. (DHHS(NIOSH) publication No. 2007-151). Available at: www.cdc.gov/niosh/docs/2007-151/pdfs/2007-151.pdf. Accessed Apr 21, 2016. [Google Scholar]
- 26.Moore RM, Jr, Davis YM, Kaczmarek RG. An overview of occupational hazards among veterinarians, with particular reference to pregnant women. Am Ind Hyg Assoc J. 1993;54:113–120. doi: 10.1080/15298669391354423. [DOI] [PubMed] [Google Scholar]
- 27.Johnson JA, Buchan RM, Reif JS. Effect of waste anesthetic gas and vapor exposure on reproductive outcome in veterinary personnel. Am Ind Hyg Assoc J. 1987;48:62–66. doi: 10.1080/15298668791384373. [DOI] [PubMed] [Google Scholar]
- 28.Fritschi L, Shirangi A, Robertson ID, et al. Trends in exposure of veterinarians to physical and chemical hazards and use of protection practices. Int Arch Occup Environ Health. 2008;81:371–378. doi: 10.1007/s00420-007-0221-0. [DOI] [PubMed] [Google Scholar]
- 29.Shirangi A, Fritschi L, Holman CD. Maternal occupational exposures and risk of spontaneous abortion in veterinary practice. Occup Environ Med. 2008;65:719–725. doi: 10.1136/oem.2007.035246. [DOI] [PubMed] [Google Scholar]
- 30.Fransman W, Roeleveld N, Peelen S, et al. Nurses with dermal exposure to antineoplastic drugs: reproductive outcomes. Epidemiology. 2007;18:112–119. doi: 10.1097/01.ede.0000246827.44093.c1. [DOI] [PubMed] [Google Scholar]
- 31.Stücker I, Caillard JF, Collin R, et al. Risk of spontaneous abortion among nurses handling antineoplastic drugs. Scand J Work Environ Health. 1990;16:102–107. doi: 10.5271/sjweh.1811. [DOI] [PubMed] [Google Scholar]
- 32.Dranitsaris G, Johnston M, Poirier S, et al. Are health care providers who work with cancer drugs at an increased risk for toxic events? A systematic review and meta-analysis of the literature. J Oncol Pharm Pract. 2005;11:69–78. doi: 10.1191/1078155205jp155oa. [DOI] [PubMed] [Google Scholar]
- 33.Henry C. Safe handling of antineoplastic agents: a survey of protocols from 24 veterinary referral institutions. Vet Cancer Soc Newslett. 1993;17:1,4–6. [Google Scholar]
- 34.Lucroy M. Review of safe cytotoxic drug preparation practices. Vet Cancer Soc Newslett. 2000;24:3,6–8. [Google Scholar]
- 35.Lucroy M. Chemotherapy safety in veterinary practice: hazardous drug preparation. Compend Contin Educ Pract Vet. 2001;23:860–867. [Google Scholar]
- 36.Takada S. Principles of chemotherapy safety procedures. Clin Tech Small Anim Pract. 2003;18:73–74. doi: 10.1053/svms.2003.36618. [DOI] [PubMed] [Google Scholar]
- 37.Epp T, Waldner C. Occupational health hazards in veterinary medicine: physical, psychological, and chemical hazards. Can Vet J. 2012;53:151–157. [PMC free article] [PubMed] [Google Scholar]
- 38.Shirangi A, Bower C, Holman CD, et al. A study of handling cytotoxic drugs and risk of birth defects in offspring of female veterinarians. Int J Environ Res Public Health. 2014;11:6216–6230. doi: 10.3390/ijerph110606216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.CDC National Institute of Occupational Safety and Health. Small business guide for ethylene oxide. Washington DC: OSHA; 2009. (OSHA 3359-04). 2009. Available at: www.osha.gov/Publications/ethylene-oxide-final.html. Accessed Apr 21, 2016. [Google Scholar]
- 40.Ethylene oxide standard. 29 CFR 1940, 1047
- 41.Elsheikha HM, Saied NA, El-Dahtory F. Risks to vets from pesticides: study into organophosphates. Vet Times. 2009;39:28–29. [Google Scholar]
- 42.Bukowski J. Real and potential occupational health risks associated with insecticide use. Compend Contin Educ Pract Vet. 1990;12:1617–1626. [Google Scholar]
- 43.McKillen M. Health and safety management in veterinary practices 4. Risk assessments for selected hazards: risk control by means of personal protective equipment (PPE) Ir Vet J. 1999;52:168. [Google Scholar]
- 44.Shirangi A, Fritschi L, Holman CD, et al. Birth defects in offspring of female veterinarians. J Occup Environ Med. 2009;51:525–533. doi: 10.1097/JOM.0b013e3181a01af3. [DOI] [PubMed] [Google Scholar]
- 45.Vanderwall D. Safe handling of reproductive hormones routinely used in equine practice. Clin Theriogenology. 2012;4:39–48. [Google Scholar]
- 46.Hall AL, Davies HW, Demers PA, et al. Occupational exposures to antineoplastic drugs and ionizing radiation in Canadian veterinary settings: findings from a national surveillance project. Can J Public Health. 2013;104:e460–e465. doi: 10.17269/cjph.104.4167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Selevan SG, Lindbohm ML, Hornung RW, et al. A study of occupational exposure to antineoplastic drugs and fetal loss in nurses. N Engl J Med. 1985;313:1173–1178. doi: 10.1056/NEJM198511073131901. [DOI] [PubMed] [Google Scholar]
- 48.Valanis B, Vollmer WM, Steele P. Occupational exposure to antineoplastic agents: self-reported miscarriages and stillbirths among nurses and pharmacists. J Occup Environ Med. 1999;41:632–638. doi: 10.1097/00043764-199908000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Lawson CC, Rocheleau CM, Whelan EA, et al. Occupational exposures among nurses and risk of spontaneous abortion. Am J Obstet Gynecol. 2012;206:e321–e328. doi: 10.1016/j.ajog.2011.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meijster T, Fransman W, Veldhof R, et al. Exposure to antineoplastic drugs outside the hospital environment. Ann Occup Hyg. 2006;50:657–664. doi: 10.1093/annhyg/mel023. [DOI] [PubMed] [Google Scholar]
- 51.Barr FM. Waste anaesthetic gas exposure in veterinary surgeries: a need for scavenging systems. N Z Vet J. 1987;35:68–71. doi: 10.1080/00480169.1987.35386. [DOI] [PubMed] [Google Scholar]
- 52.Cohen EN, Bellville JW, Brown BW., Jr Anesthesia, pregnancy, and miscarriage: a study of operating room nurses and anesthetists. Anesthesiology. 1971;35:343–347. doi: 10.1097/00000542-197110000-00005. [DOI] [PubMed] [Google Scholar]
- 53.Corbett TH, Cornell RG, Endres JL, et al. Birth defects among children of nurse-anesthetists. Anesthesiology. 1974;41:341–344. [PubMed] [Google Scholar]
- 54.Hoerauf K, Lierz M, Wiesner G, et al. Genetic damage in operating room personnel exposed to isoflurane and nitrous oxide. Occup Environ Med. 1999;56:433–437. doi: 10.1136/oem.56.7.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ward GS, Byland RR. Concentrations of methoxyflurane and nitrous oxide in veterinary operating rooms. Am J Vet Res. 1982;43:360–362. [PubMed] [Google Scholar]
- 56.Occupational disease among operating room personnel: a national study. Report of an ad hoc committee on the effect of trace anesthetics on the health of operating room personnel, American Society of Anesthesiologists. Anesthesiology. 1974;41:321–340. [PubMed] [Google Scholar]
- 57.CDC National Institute of Occupational Safety and Health. Criteria for a recommended standard: occupational exposure to waste anesthetic gases and vapors. Cincinnati: CDC; 1977. (DHHS(NIOSH) publication No. 77-140). Available at: www.cdc.gov/niosh/docs/1970/77-140.html. Accessed Apr 21, 2016. [Google Scholar]
- 58.McGregor DG. Occupational exposure to trace concentrations of waste anesthetic gases. Mayo Clin Proc. 2000;75:273–277. doi: 10.4065/75.3.273. [DOI] [PubMed] [Google Scholar]
- 59.Meyer RE. Anesthesia hazards to animal workers. Occup Med. 1999;14:225–234. [PubMed] [Google Scholar]
- 60.Short CE, Harvey RC. Anesthetic waste gases in veterinary medicine: analysis of the problem and suggested guidelines for reducing personnel exposures. Cornell Vet. 1983;73:363–374. [PubMed] [Google Scholar]
- 61.Tannenbaum TN, Goldberg RJ. Exposure to anesthetic gases and reproductive outcome. A review of the epidemiologic literature. J Occup Med. 1985;27:659–668. [PubMed] [Google Scholar]
- 62.Allweiler SI, Kogan LR. Inhalation anesthetics and the reproductive risk associated with occupational exposure among women working in veterinary anesthesia. Vet Anaesth Analg. 2013;40:285–289. doi: 10.1111/vaa.12014. [DOI] [PubMed] [Google Scholar]
- 63.Lindbohm ML, Taskinen H. Spontaneous abortions among veterinarians. Scand J Work Environ Health. 2000;26:501–506. doi: 10.5271/sjweh.574. [DOI] [PubMed] [Google Scholar]
- 64.Shuhaiber S, Einarson A, Radde IC, et al. A prospective-controlled study of pregnant veterinary staff exposed to inhaled anesthetics and x-rays. Int J Occup Med Environ Health. 2002;15:363–373. [PubMed] [Google Scholar]
- 65.Steele LL, Wilkins JR., III Occupational exposures and risks of spontaneous abortion among female veterinarians. Int J Occup Environ Health. 1996;2:26–36. doi: 10.1179/oeh.1996.2.1.26. [DOI] [PubMed] [Google Scholar]
- 66.Manley SV, McDonell WN. Recommendations for reduction of anesthetic gas pollution. J Am Vet Med Assoc. 1980;176:519–524. [PubMed] [Google Scholar]
- 67.Wilkins JR, III, Steele LL. Occupational factors and reproductive outcomes among a cohort of female veterinarians. J Am Vet Med Assoc. 1998;213:61–67. [PubMed] [Google Scholar]
- 68.Longley L. Exotic patients: biosecurity aspects worth considering. Vet Times. 2010;40:14–15. [Google Scholar]
- 69.Jones M, Jeal H, Schofield S, et al. Rat-specific IgG and IgG(4) antibodies associated with inhibition of IgE-allergen complex binding in laboratory animal workers. Occup Environ Med. 2014;71:619–623. doi: 10.1136/oemed-2014-102119. [DOI] [PubMed] [Google Scholar]
- 70.Gulsun S, Aslan S, Satici O, et al. Brucellosis in pregnancy. Trop Doct. 2011;41:82–84. doi: 10.1258/td.2011.100386. [DOI] [PubMed] [Google Scholar]
- 71.Carcopino X, Raoult D, Bretelle F, et al. Q fever during pregnancy: a cause of poor fetal and maternal outcome. Ann N Y Acad Sci. 2009;1166:79–89. doi: 10.1111/j.1749-6632.2009.04519.x. [DOI] [PubMed] [Google Scholar]
- 72.Williams CJ, Scheftel JM, Elchos BL, et al. Compendium of veterinary standard precautions for zoonotic disease prevention in veterinary personnel. J Am Vet Med Assoc. 2015;247:1252–1277. doi: 10.2460/javma.247.11.1252. [DOI] [PubMed] [Google Scholar]
- 73.Guerra MA. Leptospirosis. J Am Vet Med Assoc. 2009;234:472–478. doi: 10.2460/javma.234.4.472. [DOI] [PubMed] [Google Scholar]
- 74.Puliyath G, Singh S. Leptospirosis in pregnancy. Eur J Clin Microbiol Infect Dis. 2012;31:2491–2496. doi: 10.1007/s10096-012-1625-7. [DOI] [PubMed] [Google Scholar]
- 75.Baer R, Turnberg W, Yu D, et al. Leptospirosis in a small animal veterinarian: reminder to follow standardized infection control procedures. Zoonoses Public Health. 2010;57:281–284. doi: 10.1111/j.1863-2378.2009.01240.x. [DOI] [PubMed] [Google Scholar]
- 76.Hankenson C. The 3 R’s for laboratory animal zoonoses. Contemp Top Lab Anim Sci. 2003;42:66–68. 70. [PubMed] [Google Scholar]
- 77.Stewardson AJ, Grayson ML. Psittacosis. Infect Dis Clin North Am. 2010;24:7–25. doi: 10.1016/j.idc.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 78.Iowa State University, Center for Food Security and Public Health. Chlamydiosis. Available at: www.cfsph.iastate.edu/Factsheets/pdfs/chlamydiosis.pdf. Accessed Jun 6, 2016.
- 79.LeJeune J, Kersting A. Zoonoses: an occupational hazard for livestock workers and a public health concern for rural communities. J Agric Saf Health. 2010;16:161–179. doi: 10.13031/2013.32041. [DOI] [PubMed] [Google Scholar]
- 80.Anderson A, Bijlmer H, Fournier PE, et al. Diagnosis and management of Q fever–United States, 2013: recommendations from CDC and the Q Fever Working Group. MMWR Recomm Rep. 2013;62:1–30. [PubMed] [Google Scholar]
- 81.Nielsen SY, Molbak K, Nybo Andersen AM, et al. Prevalence of Coxiella burnetii in women exposed to livestock animals, Denmark, 1996 to 2002. Euro Surveill. 2013;18:20528. doi: 10.2807/1560-7917.es2013.18.28.20528. [DOI] [PubMed] [Google Scholar]
- 82.Weese JS, Peregrine AS, Armstrong J. Occupational health and safety in small animal veterinary practice: part II—parasitic zoonotic diseases. Can Vet J. 2002;43:799–802. [PMC free article] [PubMed] [Google Scholar]
- 83.Shuhaiber S, Koren G, Boskovic R, et al. Seroprevalence of Toxoplasma gondii infection among veterinary staff in Ontario, Canada (2002): implications for teratogenic risk. BMC Infect Dis. 2003;3:8. doi: 10.1186/1471-2334-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Waghorn DJ, Robson M. Occupational risk of Pasteurella multocida septicaemia and premature labour in a pregnant vet. BJOG. 2003;110:780–781. [PubMed] [Google Scholar]
- 85.Sharpe D. Implementing a medical surveillance program for animal care staff. Lab Anim (NY) 2009;38:275–278. doi: 10.1038/laban0809-275. [DOI] [PubMed] [Google Scholar]
- 86.Cheek R. What can you get from your pet? Vet Tech. 2009;30:32–38. [Google Scholar]
- 87.McGrath J. Beware the unseen bugs. Ir Vet J. 2009;62:794–795. [Google Scholar]
- 88.Widmer WS, Shaw SM, Thrall DE. Effects of low-level exposure to ionizing radiation: current concepts and concerns for veterinary workers. Vet Radiol Ultrasound. 1996;37:227–239. [Google Scholar]
- 89.US Nuclear Regulatory Commission website. (10 CFR § 20.1208).Dose equivalent to an embryo/fetus. Available at: www.nrc.gov/reading-rm/doc-collections/cfr/part020/part020/1208.html Accessed Jan 2, 2017.
- 90.Baker M. An introduction to radiation protection in veterinary radiography. Vet Nurse. 2014;5:496–501. [Google Scholar]
- 91.Tyson R, Smiley DC, Pleasant RS, et al. Estimated operator exposure for hand holding portable x-ray units during imaging of the equine distal extremity. Vet Radiol Ultrasound. 2011;52:121–124. doi: 10.1111/j.1740-8261.2010.01754.x. [DOI] [PubMed] [Google Scholar]
- 92.Barbee D. Invited guest editorial in response to: estimated operator exposure for hand holding portable x-ray units during imaging of the equine distal extremity (lett) Vet Radiol Ultrasound. 2011;52:213–214. doi: 10.1111/j.1740-8261.2010.01796.x. author reply, 214. [DOI] [PubMed] [Google Scholar]
- 93.Martinez NE, Kraft SL, Gibbons DS, et al. Occupational per-patient radiation dose from a conservative protocol for veterinary (18) F-fluorodeoxyglucose positron emission tomography. Vet Radiol Ultrasound. 2012;53:591–597. doi: 10.1111/j.1740-8261.2012.01958.x. [DOI] [PubMed] [Google Scholar]
- 94.Shirangi A, Fritschi L, Holman CD. Prevalence of occupational exposures and protective practices in Australian female veterinarians. Aust Vet J. 2007;85:32–38. doi: 10.1111/j.1751-0813.2006.00077.x. [DOI] [PubMed] [Google Scholar]
- 95.Thomas HL, Trout DR, Dobson H, et al. Radiation exposure to personnel during examination of limbs of horses with a portable hand-held fluoroscopic unit. J Am Vet Med Assoc. 1999;215:372–379. [PubMed] [Google Scholar]
- 96.Moritz SA, Hueston WD, Wilkins JR., III Patterns of ionizing radiation exposure among women veterinarians. J Am Vet Med Assoc. 1989;195:737–739. [PubMed] [Google Scholar]
- 97.Crimmins WF. Practices should take precautions to protect pregnant workers. J Am Vet Med Assoc. 2001;218:1251–1252. [PubMed] [Google Scholar]
- 98.Saurel-Cubizolles MJ, Zeitlin J, Lelong N, et al. Employment, working conditions, and preterm birth: results from the Europop case-control survey. J Epidemiol Community Health. 2004;58:395–401. doi: 10.1136/jech.2003.008029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Henriksen TB, Hedegaard M, Secher NJ, et al. Standing at work and preterm delivery. Br J Obstet Gynaecol. 1995;102:198–206. doi: 10.1111/j.1471-0528.1995.tb09094.x. [DOI] [PubMed] [Google Scholar]
- 100.Mozurkewich EL, Luke B, Avni M, et al. Working conditions and adverse pregnancy outcome: a meta-analysis. Obstet Gynecol. 2000;95:623–635. doi: 10.1016/s0029-7844(99)00598-0. [DOI] [PubMed] [Google Scholar]
- 101.Henriksen TB, Hedegaard M, Secher NJ. Standing and walking at work and birthweight. Acta Obstet Gynecol Scand. 1995;74:509–516. doi: 10.3109/00016349509024380. [DOI] [PubMed] [Google Scholar]
- 102.MacDonald LA, Waters TR, Napolitano PG, et al. Clinical guidelines for occupational lifting in pregnancy: evidence summary and provisional recommendations. Am J Obstet Gynecol. 2013;209:80–88. doi: 10.1016/j.ajog.2013.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Reijula K, Rasanen K, Hamalainen M, et al. Work environment and occupational health of Finnish veterinarians. Am J Ind Med. 2003;44:46–57. doi: 10.1002/ajim.10228. [DOI] [PubMed] [Google Scholar]
- 104.Wilkins JR, III, Bowman ME. Needlestick injuries among female veterinarians: frequency, syringe contents and side-effects. Occup Med (Lond) 1997;47:451–457. doi: 10.1093/occmed/47.8.451. [DOI] [PubMed] [Google Scholar]
- 105.Wright JG, Jung S, Holman RC, et al. Infection control practices and zoonotic disease risks among veterinarians in the United States. J Am Vet Med Assoc. 2008;232:1863–1872. doi: 10.2460/javma.232.12.1863. [DOI] [PubMed] [Google Scholar]
- 106.Hafer AL, Langley RL, Morrow WM, et al. Occupational hazards reported by swine veterinarians in the United States. J Swine Health Prod. 1996;4:128–141. [Google Scholar]
- 107.Schenker MB, Samuels SJ, Green RS, et al. Adverse reproductive outcomes among female veterinarians. Am J Epidemiol. 1990;132:96–106. doi: 10.1093/oxfordjournals.aje.a115648. [DOI] [PubMed] [Google Scholar]
- 108.Hedegaard M, Henriksen TB, Secher NJ, et al. Do stressful life events affect duration of gestation and risk of preterm delivery? Epidemiology. 1996;7:339–345. doi: 10.1097/00001648-199607000-00001. [DOI] [PubMed] [Google Scholar]
- 109.Hansen D, Lou HC, Olsen J. Serious life events and congenital malformations: a national study with complete follow-up. Lancet. 2000;356:875–880. doi: 10.1016/S0140-6736(00)02676-3. [DOI] [PubMed] [Google Scholar]
- 110.Khashan AS, McNamee R, Abel KM, et al. Rates of preterm birth following antenatal maternal exposure to severe life events: a population-based cohort study. Hum Reprod. 2009;24:429–437. doi: 10.1093/humrep/den418. [DOI] [PubMed] [Google Scholar]
- 111.Larsen AD. The effect of maternal exposure to psychosocial job strain on pregnancy outcomes and child development. Dan Med J. 2015;62:B5015. [PubMed] [Google Scholar]
- 112.Hansez I, Schins F, Rollin F. Occupational stress, work-home interference and burnout among Belgian veterinary practitioners. Ir Vet J. 2008;61:233–241. doi: 10.1186/2046-0481-61-4-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fenster L, Schaefer C, Mathur A, et al. Psychologic stress in the workplace and spontaneous abortion. Am J Epidemiol. 1995;142:1176–1183. doi: 10.1093/oxfordjournals.aje.a117576. [DOI] [PubMed] [Google Scholar]
- 114.Jeyaretnam J, Jones H, Phillips M. Disease and injury among veterinarians. Aust Vet J. 2000;78:625–629. doi: 10.1111/j.1751-0813.2000.tb11939.x. [DOI] [PubMed] [Google Scholar]
- 115.Nett RJ, Witte TK, Holzbauer SM, et al. Risk factors for suicide, attitudes toward mental illness, and practice-related stressors among US veterinarians. J Am Vet Med Assoc. 2015;247:945–955. doi: 10.2460/javma.247.8.945. [DOI] [PubMed] [Google Scholar]
- 116.Scotney RL, McLaughlin D, Keates HL. A systematic review of the effects of euthanasia and occupational stress in personnel working with animals in animal shelters, veterinary clinics, and biomedical research facilities. J Am Vet Med Assoc. 2015;247:1121–1130. doi: 10.2460/javma.247.10.1121. [DOI] [PubMed] [Google Scholar]
- 117.CDC National Institute of Occupational Safety and Health. website Reproductive health and the workplace. Available at: www.cdc.gov/niosh/topics/repro/default.html. Accessed May 4, 2016.
- 118.CDC National Institute of Occupational Safety and Health. The effects of workplace hazards on female reproductive health. Cincinnati: CDC; 1999. (DHHS(NIOSH) publication No. 99-104). Available at: www.osha.gov/dsg/hazcom/. Accessed Apr 21, 2016. [Google Scholar]
- 119.CDC National Institute of Occupational Safety and Health. Veterinary safety and health. Available at: www.cdc.gov/niosh/topics/veterinary/hazard.html. Accessed Apr 21, 2016.
- 120.US Department of Labor Occupational Safety and Health Administration website. Available at: www.osha.gov. Accessed May 4, 2016.
- 121.AVMA. About AVMA. Available at: www.avma.org/About/Pages/default.aspx. Accessed Jan 2, 2017.
- 122.AVMA. Available at: www.avma.org/Pages/home.aspx. Accessed Jan 2, 2017.


