Abstract
Background
Menu labeling may help people select foods and beverages with lower calories and is a potential population-based strategy to reduce obesity and diet-related chronic diseases in the United States.
Objectives
The aim of this cross-sectional study was to examine the prevalence of menu labeling use among adults and its association with sociodemographic, behavioral, and policy factors.
Methods
2012 Behavioral Risk Factor Surveillance System data from 17 states that included 100,141 adults who noticed menu labeling at fast food/chain restaurants (“When calorie information is available in the restaurant, how often does this information help you decide what to order?”) were used. Menu labeling use was categorized: frequent (always/most of the time), moderate (half the time/sometimes), and never. Multinomial logistic regression was used to examine associations of sociodemographic, behavioral, and policy factors with menu labeling use.
Results
Overall, of adults who noticed menu labeling, 25.6% reported frequent use of menu labeling, 31.6% reported moderate use, and 42.7% reported that they never use menu labeling. Compared to never users, frequent users were significantly more likely to be younger, female, non-white, more educated, high-income, overweight or obese, physically active, former- or never-smokers, with no or lower (<1 time/day) sugar-sweetened beverage intake, and living in states where menu labeling legislation was enacted or proposed.
Conclusions
Menu labeling is one method that consumers can use to help reduce their calorie consumption from restaurants. These findings can be used to develop targeted interventions to increase menu labeling use among subpopulations with lower use.
Keywords: Menu labeling, States, Sociodemographics, Behaviors, BRFSS, Adults
INTRODUCTION
Menu labeling provides the calorie content and/or other nutrition information for foods and beverages on menus and menu boards at restaurants at the point of purchase. Menu labeling may help people select foods and beverages with lower calories1 and is a potential population-based strategy to reduce obesity and diet-related chronic diseases in the United States.2,3 The Nutrition Labeling and Education Act of 1990, which requires nutrition labeling on most packaged foods, did not require nutrition labeling for restaurant foods.4 In the years that followed, some state and local jurisdictions created their own menu labeling requirements for restaurants.5,6 In 2010, a federal law was passed requiring restaurants with 20 or more establishments nationally to post nutrition information on menus.7 Restaurants were required to comply with the law by December 1, 2016.8
People’s knowledge and attitudes have been shown to influence behaviors associated with weight management.9,10 Menu labeling use may be associated with other healthy behaviors such as low consumption of sugar-sweetened beverages (SSB).11 Moreover, environmental factors such as enacted state and local menu labeling legislation could influence menu labeling use. Most menu labeling research has focused on awareness12,13 and use14 of calorie information and has been restricted to a single jurisdiction (e.g., New York City, King County, Washington). Although few previous studies11,15 examined the possible associations between menu labeling use and certain sociodemographic and behavioral factors adjusting for confounders, one study used data from 2009 before the federal law was passed using sociodemographic variables and reading calorie information when available15 and the other study using 2011 Behavioral Risk Factor Surveillance System (BRFSS) included food consumption variables, body mass index, self-perception of general health, and sociodemographic variables, but did not include race/ethnicity as a covariate because the sample consisted of adults from only 3 states (Wisconsin, Hawaii, and Minnesota), limiting subgroup analyses by race/ethnicity.11 A recent surveillance study using 2012 BRFSS data focused on the state-specific prevalence of menu labeling use and bivariate relationship between menu labeling use with age, sex, and race/ethnicity without adjusting for other sociodemographic and behavioral factors.16 However, none of these studies included policy factors such as the status of state or local menu labeling legislation. Having information on associations between policy factors and menu labeling use at the population level is important because it contributes to the evidence base and could be used to understand how menu labeling law influence usage. Furthermore, to date, menu labeling studies have dichotomized menu labeling usage categories (users vs. non-users), limiting ways to differentiate frequent, moderate, and non-users. Therefore, the purpose of this study was to examine the associations among 3 levels of menu labeling usage in (frequent, moderate, and none) with sociodemographic, behavioral, and policy factors in US adults.
METHODS
Data Source and Study Sample
The Behavioral Risk Factor Surveillance System (BRFSS) is an annual, state-based, random-digit-dialed telephone survey of noninstitutionalized, civilian, US adults. It uses a multistage cluster sampling design and applies raking17 weights to adjust for nonresponse, noncoverage, and unequal selection of population, in order to generate demographic distributions that correspond to the state population. Detailed information on validity of measures and survey data can be found elsewhere.18,19 Every year, states select optional modules for inclusion in their surveys. In 2012, one menu labeling question was included in the Sugar-Sweetened Beverage and Menu Labeling Optional Module and used by 18 states (California, Delaware, Georgia, Hawaii, Iowa, Kansas, Maryland, Minnesota, Mississippi, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New York, Oklahoma, South Dakota, and Tennessee). However, California was excluded from this analysis because of a high proportion of missing data for the menu labeling question (58%), leaving data from 17 states for use in the analytic sample. This study was deemed exempt by CDC Institutional Review Board under federal regulation 45 46.101 (b) CFR.20
The analysis was restricted to adults who ate at fast food and chain restaurants and who noticed menu labeling. Of the initial study population of 118,013 adults from 17 states, 10,548 (8.9%) adults were ineligible for this study because they did not eat at fast food or chain restaurants (6.4%), never noticed or never looked for calorie information (2.2%), or usually could not find calorie information (0.3%), resulting in an eligible sample of 107,465 adults (Figure 1). Another 7,324 (6.2%) adults were excluded because of missing outcome data for the menu labeling question, leaving an analytic sample of 100,141 adults. Compared to the analytic sample, the excluded adults had a higher proportion of adults aged 18‒29 years (20.5% vs 34.8%) and men (48.0% vs 53%) and had a lower proportion of whites (68.5% vs 54.9%). Furthermore, 10,635 adults were excluded from the multinomial logistic regression model sample because of missing covariates (Figure 1). Compared to those included in the multinomial regression model (n=89,506), those excluded for missing covariate data from the analytic sample had a significantly higher proportion of adults aged 18–29 years (19.9% vs 26.4%) and women (50.4% vs 65.8%) and a lower proportion of whites (69.1% vs 61.2%).
Figure 1.
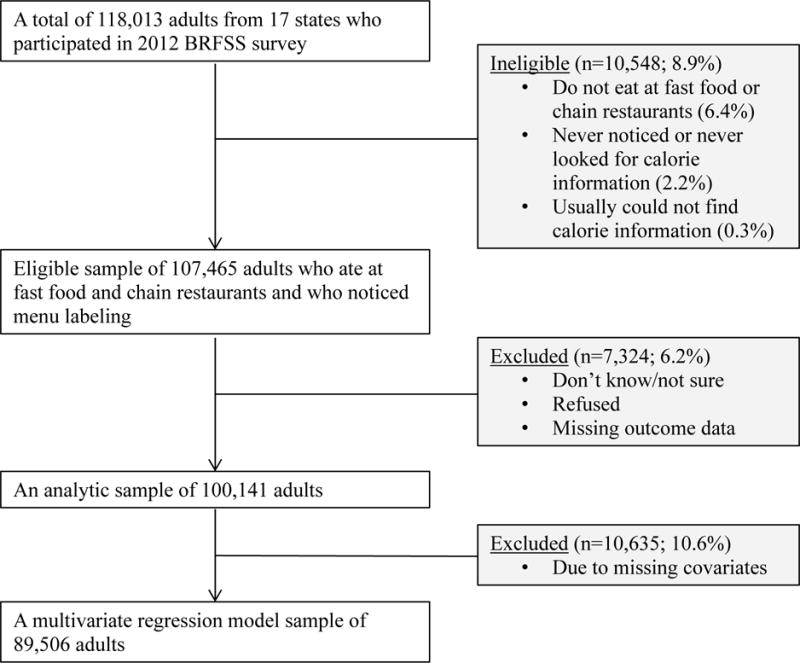
Analytic and model sample flow chart of eligible adults on menu labeling usage question in 2012 BRFSS survey
Outcome Variable
The outcome measure was menu labeling use among adults who ate at fast food and chain restaurants and who noticed menu labeling. Menu labeling use was assessed by the following question: “The next question is about eating out at fast food and chain restaurants. When calorie information is available in the restaurant, how often does this information help you decide what to order?” Response options were “always,” “most of the time,” “about half the time,” “sometimes,” and “never.” Menu labeling use was categorized into three groups: frequent (always/most of the time), moderate (about half the time/sometimes), and never.
Sociodemographic, Behavioral, and Policy Variables
Exposure variables included sociodemographic, behavioral, and policy variables. Sociodemographic variables included age (18–29, 30–39, 40–49, 50–59, 60–69, and ≥70 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic other [Asian, Hawaiian/Pacific Islander, American Indian/Alaskan Native, and multiracial]), education level (≤high school, some college, and college graduate), marital status (married or not married), and annual household income (<$25,000, $25,000–$49,999, $50,000–$74,999, ≥$75,000, and don’t know/refused/missing). Because a relatively large proportion (12.2%) of adults had missing/don’t know/refused responses for annual household income, an additional category for these respondents was created to reduce missing data bias.
Based on a review of the literature showing associations of menu labeling use with behavioral factors, the following behavioral variables were selected: weight status, leisure time physical activity, smoking status, and SSB consumption.11 Weight status was classified into three categories based on participants’ body mass index (BMI) using self-reported height and weight data: underweight/normal weight (BMI <25.0 kg/m2); overweight (BMI 25.0–29.9 kg/m2); and obese (BMI ≥30.0 kg/m2).21 The weight status categories of underweight and normal weight were combined as a single category because <2% of participants were classified as underweight. Leisure time physical activity was defined as doing physical activity or exercise during the past 30 days other than their regular job (yes or no). Smoking status consisted of three categories (current, former, and never). SSB consumption during the past 30 days was calculated by summarizing daily intake of regular soda and fruit drinks (excluding 100% fruit juice) and then categorizing totals into three levels (0, >0 to <1, and ≥1 times/day).
The policy variable was obtained using the Center for Science in the Public Interest and National Conference of State Legislatures database to determine the status of state menu labeling legislation as of January 1, 2012 (enacted/proposed or none).5,6 Six states had enacted status, 24 states (including the District of Columbia) had proposed legislation (i.e., introduced the legislation in 2003–2009 but had not yet passed the legislation), and 20 states had neither enacted nor proposed legislation. Among the 17 states included in our analysis, nine states had enacted or proposed menu labeling legislation (enacted: New Jersey; proposed: Delaware, Hawaii, Iowa, Maryland, New Hampshire, New York, Oklahoma, and Tennessee), and eight states had no legislation (Georgia, Kansas, Minnesota, Mississippi, Montana, Nebraska, Nevada, and South Dakota). Proposed menu labeling legislation was grouped with enacted because only one state had enacted legislation and because we hypothesized that states with proposed menu labeling legislation might have greater availability of menu labeling in anticipation of the enactment and consumers might have greater awareness if covered in the media in proposed states. For example, some states with proposed legislation already had locally enacted menu labeling legislation (e.g., Montgomery County, Maryland, and New York City).
Statistical Analysis
Chi-square tests were used to examine the bivariate relationships between menu labeling use and sociodemographic, behavioral, and policy variables in the analytic sample, with a p value of <0.05 defining statistical significance. A multinomial logistic regression model22 was used to estimate adjusted odds ratios (AORs) and 95% confidence intervals (CIs) for associations between menu labeling use and sociodemographic, behavioral, and policy variables (n=89,506), and the reference group was those who never used menu labeling. Sensitivity analysis was conducted treating policy variable categorized as enacted, proposed, and none. All statistical analyses were performed in SAS (Version 9.3, 2011; SAS Institute, Cary, North Carolina) using the sample weights and accounting for the complex sample design to yield estimates for civilian noninstitutionalized adults.
RESULTS
Among adults from 17 states who ate at fast food and chain restaurants and noticed menu labeling, 25.6% reported frequent use of menu labeling, 31.6% reported moderate use, and 42.7% reported that they never used menu labeling. Menu labeling use varied by all sociodemographic, behavioral, and policy factors studied (χ2 tests, p <0.05 for all variables). For example, the percentage of frequent users was highest among adults aged 30‒49 years, women, non-Hispanic others, college graduates, married adults, and those with higher household income (≥$75,000). Additionally, underweight/normal weight adults, physically active adults, never smokers, non-SSB consumers, and adults living in states with menu labeling legislations enacted or proposed had the highest percentage of frequent menu labeling users (Table 1).
Table 1.
Sociodemographic, behavioral, and policy characteristics of respondents and their associations with menu labeling use among adults in 17 statesa, Behavioral Risk Factor Surveillance System, 2012
| Characteristic | All respondents | Menu labeling useb | ||
|---|---|---|---|---|
| Frequent | Moderate | Never | ||
| n (%)c | % (SE) | % (SE) | % (SE) | |
| Total sample (N=100,141) | 100,141 (100.0) | 25.6 (0.3) | 31.6 (0.3) | 42.7d (0.3) |
|
| ||||
| Sociodemographic factors | ||||
|
| ||||
| Age, y (n=99,383) | ||||
| 18–29 | 9,918 (20.5) | 23.2 (0.8) | 32.8 (0.8) | 44.0 (1.0) |
| 30–39 | 11,711 (17.0) | 27.1 (0.8) | 33.7 (0.8) | 39.2 (0.9) |
| 40–49 | 15,073 (18.3) | 27.3 (0.7) | 31.8 (0.8) | 40.9 (0.8) |
| 50–59 | 21,241 (18.6) | 26.6 (0.6) | 31.7 (0.6) | 41.7 (0.7) |
| 60–69 | 20,593 (13.8) | 26.7 (0.7) | 29.6 (0.7) | 43.7 (0.8) |
| ≥70 | 20,847 (11.7) | 22.3 (0.6) | 28.6 (0.7) | 49.1 (0.8) |
| Sex (n=100,141) | ||||
| Men | 40,772 (48.0) | 18.8 (0.4) | 28.1 (0.5) | 53.1d (0.5) |
| Women | 59,369 (52.0) | 31.9 (0.4) | 34.9 (0.4) | 33.2d (0.4) |
| Race/ethnicity (n=96,400) | ||||
| White, non-Hispanic | 78,828 (68.5) | 25.3 (0.3) | 30.9 (0.4) | 43.8d (0.4) |
| Black, non-Hispanic | 7,744 (14.8) | 27.7 (1.0) | 31.2 (1.1) | 41.1d (1.1) |
| Hispanic | 3,943 (10.0) | 24.2 (1.2) | 33.9 (1.5) | 41.8d (1.4) |
| Other, non-Hispanic | 5,885 (6.6) | 28.3 (1.8) | 36.8 (2.2) | 45.0d (1.6) |
| Education level (n=99,956) | ||||
| ≤High school | 36,564 (41.7) | 19.9 (0.5) | 30.5 (0.5) | 49.6 (0.6) |
| Some college | 28,444 (30.6) | 26.5 (0.6) | 31.5 (0.6) | 42.0 (0.6) |
| College graduate | 34,948 (27.7) | 33.3 (0.5) | 33.4 (0.5) | 33.3 (0.5) |
| Marital status (n=99,753) | ||||
| Married | 56,908 (55.8) | 26.7 (0.4) | 32.6 (0.4) | 40.8 (0.4) |
| Not marriede | 42,845 (44.2) | 24.3 (0.5) | 30.5 (0.5) | 45.2 (0.6) |
| Annual household income (n=100,141) | ||||
| <$25,000 | 24,263 (24.4) | 21.4 (0.6) | 32.0 (0.7) | 46.5 (0.7) |
| $25,000–$49,999 | 23,826 (21.7) | 23.6 (0.6) | 30.4 (0.7) | 46.0 (0.7) |
| $50,000–$74,999 | 14,659 (13.6) | 25.4 (0.7) | 31.7 (0.8) | 42.8 (0.8) |
| ≥$75,000 | 25,054 (26.3) | 32.4 (0.6) | 32.3 (0.6) | 35.4 (0.6) |
| Don’t Know/Refused/Missing | 12,339 (13.4) | 23.3 (0.9) | 31.5 (1.0) | 45.2 (1.1) |
|
| ||||
| Behavioral factors | ||||
|
| ||||
| Weight statusf (n=95,470) | ||||
| Underweight/normal weight | 33,097 (35.5) | 26.9 (0.6) | 29.7 (0.6) | 43.3 (0.6) |
| Overweight | 34,877 (36.2) | 25.2 (0.5) | 30.5 (0.5) | 44.3 (0.6) |
| Obese | 27,496 (28.2) | 24.2 (0.6) | 34.5 (0.6) | 41.4 (0.6) |
| Leisure time physical activity during the past 30 days (n=100,035) | ||||
| Yes | 75,994 (76.6) | 27.9 (0.4) | 32.2 (0.4) | 39.9 (0.4) |
| No | 24,041 (23.4) | 18.3 (0.6) | 29.6 (0.7) | 52.1 (0.7) |
| Smoking status (n=99,716) | ||||
| Current | 16,327 (18.0) | 17.7 (0.6) | 26.2 (0.7) | 56.1 (0.8) |
| Former | 29,013 (24.7) | 26.0 (0.5) | 29.1 (0.6) | 44.9 (0.6) |
| Never | 54,376 (56.8) | 28.1 (0.4) | 34.5 (0.5) | 37.4 (0.5) |
| SSB consumptiong (n=98,550) | ||||
| None | 32,743 (27.1) | 34.8 (0.6) | 28.5 (0.6) | 36.7 (0.6) |
| >0 to <1 time/day | 43,353 (44.7) | 25.8 (0.5) | 34.9 (0.5) | 39.3 (0.5) |
| ≥1 time/day | 22,454 (28.2) | 16.8 (0.5) | 29.7 (0.6) | 53.5 (0.7) |
|
| ||||
| Policy factor | ||||
|
| ||||
| Menu labeling legislationh(n= 100,141) | ||||
| Enacted or proposed | 36,817 (62.7) | 27.3 (0.4) | 31.6 (0.5) | 41.1 (0.5) |
| None | 63,324 (37.3) | 22.8 (0.3) | 31.7 (0.4) | 45.5 (0.4) |
17 states included were Delaware, Georgia, Hawaii, Iowa, Kansas, Maryland, Minnesota, Mississippi, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New York, Oklahoma, South Dakota, and Tennessee.
χ2 tests were used for each variable to examine differences across categories, and all p-values were <0.0001. Frequent category included “Always” and “Most of the time” and moderate category included “About half of the time” and “Sometimes”.
Unweighted sample size and weighted percentage are presented. Weighted percentage may not add up to 100% because of rounding.
Never user prevalence for total, sex, and race/ethnicity were previously reported.16
Not married included “Never married”, “Divorced”, “Widowed” and “Separated”.
Weight status categories were defined using calculated BMI (kg/m2): underweight/normal weight, BMI<25; overweight, BMI 25‒<30; Obese, BMI ≥30.
SSBs included regular soda and fruit drinks (excluding 100% fruit juice). Weekly or monthly SSB intake during the past 30 days was converted to daily SSB intake.
Menu labeling legislation status as of January 1, 2012. States with enacted or proposed legislation included Delaware, Hawaii, Iowa, Maryland, New Hampshire, New Jersey, New York, Oklahoma, Tennessee, and states with no legislation included Georgia, Kansas, Minnesota, Mississippi, Montana, Nebraska, Nevada, South Dakota.
Several subgroups of sociodemographic, behavioral, and policy variables were significantly associated with frequent use of menu labeling. Sex and SSB consumption had the strongest associations – women and non-daily SSB consumers had 184% and 154% increased odds of being frequent users compared with men and daily SSB consumers, respectively (Table 2). The findings showed small effects in odds of being a frequent user in the following population subgroups; age groups younger than 70 y (AOR ranges= 1.29−1.58), Hispanic (AOR=1.28), non-Hispanic Black (AOR=1.37), non-Hispanic other (AOR=1.32), some college (AOR=1.3), college graduate (AOR=1.65), annual household income ≥$75,000 (AOR=1.22). Additionally, overweight (AOR=1.16) or obese (AOR=1.23) adults, physically active (AOR=1.77), former (AOR=1.53) or never (AOR=1.67) smokers, and those living in states with menu labeling legislations enacted or proposed (AOR=1.26) groups had increased odds of being a frequent user (Table 2).
Table 2.
Adjusted associations between menu labeling usage and sociodemographic, behavioral, and policy factors among adults in 17 statesa, Behavioral Risk Factor Surveillance System, 2012 (n=89,506)
| Multinomial Logistic Regression Analysisb Menu labeling usec | ||
|---|---|---|
| Frequent | Moderate | |
| AOR (95% CI) | AOR (95% CI) | |
| Sociodemographic factors | ||
|
| ||
| Age, y | ||
| 18–29 | 1.54 (1.33, 1.79)d | 1.41 (1.23, 1.60) |
| 30–39 | 1.58 (1.37, 1.82) | 1.36 (1.20, 1.54) |
| 40–49 | 1.41 (1.24, 1.61) | 1.20 (1.06, 1.36) |
| 50–59 | 1.34 (1.19, 1.51) | 1.23 (1.10, 1.37) |
| 60–69 | 1.29 (1.14, 1.46) | 1.11 (0.99, 1.25) |
| ≥70 | Reference | Reference |
| Sex | ||
| Men | Reference | Reference |
| Women | 2.84 (2.62, 3.08) | 2.09 (1.95, 2.24) |
| Race/ethnicity | ||
| White, non-Hispanic | Reference | Reference |
| Black, non-Hispanic | 1.37 (1.20, 1.57) | 1.06 (0.94, 1.20) |
| Hispanic | 1.28 (1.08, 1.52) | 1.24 (1.06, 1.45) |
| Other, non-Hispanic | 1.32 (1.06, 1.65) | 1.39 (1.16, 1.66) |
| Education level | ||
| ≤High school | Reference | Reference |
| Some college | 1.30 (1.15, 1.46) | 1.18 (1.06, 1.31) |
| College graduate | 1.65 (1.47, 1.85) | 1.38 (1.25, 1.53) |
| Marital status | ||
| Married | 0.94 (0.86, 1.03) | 0.87 (0.81, 0.95) |
| Not marriede | Reference | Reference |
| Annual household income | ||
| <$25,000 | Reference | Reference |
| $25,000–$49,999 | 0.94 (0.83, 1.06) | 0.88 (0.79, 0.97) |
| $50,000–$74,999 | 0.95 (0.83, 1.01) | 0.91 (0.81, 1.03) |
| ≥$75,000 | 1.22 (1.07, 1.39) | 1.02 (0.90, 1.14) |
| Don”t Know/Refused/Missing | 0.85 (0.72, 1.00) | 0.84 (0.73, 0.96) |
|
| ||
| Behavioral factors | ||
|
| ||
| Weight statusf | ||
| Underweight/normal | Reference | Reference |
| Overweight | 1.16 (1.06, 1.27) | 1.19 (1.09, 1.30) |
| Obese | 1.23 (1.11, 1.36) | 1.47 (1.35, 1.61) |
| Leisure time physical activity during the past 30 days | ||
| Yes | 1.77 (1.60, 1.96) | 1.39 (1.27, 1.51) |
| No | Reference | Reference |
| Smoking status | ||
| Current | Reference | Reference |
| Former | 1.53 (1.35, 1.73) | 1.28 (1.15, 1.43) |
| Never | 1.67 (1.49, 1.87) | 1.57 (1.42, 1.73) |
| SSB consumptiong | ||
| None | 2.54 (2.27, 2.85) | 1.31 (1.19, 1.45) |
| >0 to <1 time/day | 1.68 (1.51, 1.87) | 1.45 (1.33, 1.57) |
| ≥1 time/day | Reference | Reference |
|
| ||
| Policy factor | ||
|
| ||
| Menu labeling legislationh | ||
| Enacted or proposed | 1.26 (1.18, 1.35) | 1.08 (1.01, 1.15) |
| None | Reference | Reference |
17 states included were Delaware, Georgia, Hawaii, Iowa, Kansas, Maryland, Minnesota, Mississippi, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New York, Oklahoma, South Dakota, and Tennessee.
The multinomial logistic regression included all variables in one model. The reference group was never users of menu labeling.
Frequent category included “Always” and “Most of the time” and moderate category included “About half of the time” and “Sometimes”.
Bolded values do not include 1 in 95% CI.
Not married included “Never married”, “Divorced”, “Widowed” and “Separated”.
Weight status categories were defined using calculated BMI (kg/m2): underweight/normal weight, BMI<25; overweight, BMI 25‒<30; Obese, BMI ≥30.
SSBs include regular soda and fruit drink (excluding 100% fruit juice). Weekly or monthly SSB intake during the past 30 days was converted to daily SSB intake.
Menu labeling legislation status as of January 1, 2012. States with enacted or proposed legislation included Delaware, Hawaii, Iowa, Maryland, New Hampshire, New Jersey, New York, Oklahoma, Tennessee, and states with no legislation included Georgia, Kansas, Minnesota, Mississippi, Montana, Nebraska, Nevada, South Dakota.
Furthermore, patterns for moderate users were similar to those of frequent users, with the following exceptions in age, race/ethnicity, marital status, and annual household income. Unlike patterns for frequent users, the odds of being moderate menu labeling users were not significantly higher for the 60- to 69-year-old age group, non-Hispanic blacks, and those in the highest-income category. Further, married adults had 13% reduced odds than unmarried adults to be moderate users (Table 2).
Sensitivity analysis showed similar results as mentioned earlier. The odds of being a frequent user were 26% higher for those living in states with menu labeling legislations enacted (95% CI: 1.11, 1.43) and proposed (95% CI: 1.17, 1.36) compared to non-users. The odds of being a moderate user was 10% higher for those living in states with proposed menu labeling legislations (95% CI 1.03, 1.18) but no differences for enacted (AOR=0.97 (95% CI: 0.85, 1.10)) compared to non-users (data not shown).
DISCUSSION
A previous surveillance report found 57.3% of adults were restaurant menu labeling users.16 In this study using the same dataset, we further specified that among the same population, 25.6% were frequent users and 31.6% were moderate users. The findings showed a somewhat higher prevalence of menu labeling use than previous studies in single jurisdictions14,23 and multiple jusrisdictions.11,15 A 2010 study among 1,083 customers from King County, Washington, showed that while 60% of customers reported seeing menu labeling, only about 25% reported using it.14 Another study with 8,489 adult customers from New York City in 2009 showed that only 15% of customers reported using calorie information after 9 months of full enforcement of menu labeling, though the researchers did not specify whether or not customers noticed or saw menu labeling.23 Wethington and colleagues conducted a study of 4,363 adults surveyed in 2009, which was weighted to match the distribution of the US population, that found 36% of adults reported reading calorie information, and of those, 95% reported using this information at least sometimes when making their food selection.15 Differences in the prevalence of menu labeling use between our study and the previous research may be partially due to differences in samples, mode of surveys, geographic areas, survey years, or how menu labeling use was defined. For example, the wording of menu labeling usage in the survey could result in difference in menu labeling prevalence. Thus, for surveillance purposes, using the same question over time could benefit the validity of the measurement.
Similar to previous studies, the findings showed that women were more likely than men to use menu labeling,11,14,24 as were those with higher education24,25 and higher income14,24,25 than their counterparts. Women had 2.8 times higher odds for being frequent menu labeling users than men in our study. Previous studies showed that women perceived menu labeling to be more useful26 and were more likely to select lower calorie foods than men.21 Disparities of menu labeling use by education and income are similar to other diet-related health behaviors such as being less likely to drink SSB and more likely to consume fruits and vegetables.25 Although previous studies showed inconsistent associations between menu labeling use and age,11,15 race/ethnicity,14,15 and weight status,11,21,27 this study found that younger adults (<70 years), non-white adults, and adults who were overweight or obese were more likely to be frequent menu labeling users than their counterparts. For instance, this study found that the odds of being frequent menu labeling users were 50% higher among young adults aged 18–24 years than older adults aged ≥70 years. Younger adults may have more opportunities to be exposed to menu labeling than older adults because they frequently eat at fast food restaurants with menu labeling.28,29 The reasons for the differences in menu labeling use across race/ethnicity are unclear. However, non-Hispanic blacks and Hispanics are more likely than non-Hispanic whites to report that posting calorie information would encourage their selection of a lower-calorie food.26
In terms of behavioral variables that were included in the analysis, adults who were overweight or obese were more likely to be frequent and moderate users of menu labeling than underweight/normal weight adults. It is possible that overweight and obese adults may frequently use menu labeling as a tool to select lower calorie meals at restaurants for weight management. Additionally, similar to previous findings, adults who were physically active and who are not daily SSB drinkers were more likely to use menu labeling.11 Given the findings that show menu labeling usage among those who already engage in healthy behaviors, targeted interventions to increase menu labeling usage among people who are not participating in such healthy behaviors would be needed.
The study showed that the odds of being a frequent user of menu labeling were 1.26 times higher among adults living in states with enacted/proposed state menu labeling legislation than those living in states with no menu labeling legislation. This association might be explained in part by a greater availability and awareness of menu labeling in states with enacted/proposed menu labeling legislation. For enacted states, a previous study reported 98% menu labeling availability in eligible restaurants at 4 months post-enforcement of menu labeling implementation.30 For proposed states, menu labeling could be available in anticipation of the enactment and consumers might have greater awareness of menu labeling if covered in the media because media coverage influences awareness of pending legislation.31
Although availability and awareness do not guarantee use of menu labeling, they may increase its likelihood. However, the magnitude of menu labeling availability in the states was unknown. Furthermore, even among adults living in states with enacted/proposed menu labeling legislation, 41% of respondents reported never using menu labeling when they noticed it. The reasons for this finding could be attributed to the influence of other factors such as marketing, menu design, and nutrition knowledge.32 For example, knowledge of how to interpret calorie information could encourage restaurant consumers to use the information. U.S. Food and Drug Administration regulations call for restaurants to display the information that “2,000 calories a day is used for general nutrition advice, but calorie needs vary”33 along with menu labeling. Such information provides a context for comparison of meal or food calories in relation to estimated daily energy requirements for the general public,34 which might lead to making healthier food and beverage choices. A recent systematic review and meta-analysis found that while menu labeling with calories alone did not have the intended effect of decreasing calories consumed, the addition of contextual or interpretive nutrition information on menus helped consumers consume fewer calories by 81 kcal.35 To that effect, menu labeling could be a strategy that requires other complementary strategies, such as behavioral economics, store pricing, and nutrition guidelines, to work effectively. Policy may be an essential factor that would lead to the increase of ML usage. These findings could be informative in developing targeted interventions to increase menu labeling use among low users.
To our knowledge, this was the first study to include state menu labeling policy as a predictor for menu labeling use in addition to sociodemographic and behavioral factors. However, this study has several limitations. First, because the BRFSS relies on self-reported information, the results were subject to potential reporting bias. Second, the analytic sample consisted of adults in 17 states that participated in BRFSS Sugar-Sweetened Beverage and Menu Labeling Optional Module, potentially limiting the generalizability of findings to all US adults. We do not know if the states that did not participate in the Module differ from the 17 states that did participate. Third, both the analytic and model samples excluded higher proportions of young adults and whites who are typically less likely to use menu labeling, thus resulting in an overestimate of menu labeling usage. However, the model sample contained a lower proportion of women, thus bias may have been minimized because women typically are more likely to use menu labeling. Lastly, certain factors that may be related to menu labeling use (i.e., frequency of visiting fast food or chain restaurants, why menu labeling information was not noticed, coverage of the topic or legislation in media, and availability of menu labeling) is unknown. This could affect consumers’ use of menu labeling information.
CONCLUSIONS
In conclusion, overall, more than half of surveyed adults who noticed menu labeling reported using menu labeling. Menu labeling is one method that consumers can use in restaurants to help them select food and beverage options with lower calories. With the implementation of federal policy to post calorie information on menus and menu boards in restaurants with 20 or more establishments,7 the study results can be used to develop targeted interventions to increase the use of menu labeling to make healthy food and beverage choices. Future research to understand disparities in menu labeling use among certain subgroups and the reasons that consumers use menu labeling information could help in the development of these interventions.
Contributor Information
Seung Hee Lee-Kwan, Epidemic Intelligence Service Officer, Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion, CDC. 4770 Buford Hwy, MS F-79, Atlanta, GA 30341, Phone number: 770-488-6020.
Liping Pan, Epidemiologist, Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion, CDC. 4770 Buford Hwy, MS F-79, Atlanta, GA 30341, 770-488-8001.
Leah M. Maynard, Epidemiologist, Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion, CDC. 4770 Buford Hwy, MS F-77, Atlanta, GA 30341, 770-488-5393.
Lisa C. McGuire, Epidemiology and Surveillance Team Lead, Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion, CDC. 4770 Buford Hwy, MS F-77, Atlanta, GA 30341, Phone number: 770-488-1478.
Sohyun Park, Epidemiologist, Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion, CDC. 4770 Buford Hwy, MS F-79, Atlanta, GA 30341, Phone number: 770-488-5163.
References
- 1.Block JP, Roberto CA. Potential benefits of calorie labeling in restaurants. JAMA. 2014;312:887–8. doi: 10.1001/jama.2014.9239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuo T, Jarosz CJ, Simon P, Fielding JE. Menu labeling as a potential strategy for combating the obesity epidemic: a health impact assessment. Am J Public Health. 2009;99:1680–6. doi: 10.2105/AJPH.2008.153023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krieger J, Saelens BE. Impact of menu labeling on consumer behavior: A 2008–2012 update. A research review. http://healthyeatingresearch.org/wp-content/uploads/2013/12/HER-RR-Menu-Labeling-FINAL-6-2013.pdf. Published June 2013. Accessed September 5, 2014.
- 4.Nutrition Labeling and Education Act of 1990, Pub L No. 101–535 104 Stat 2353 (1990).
- 5.Center for Science in the Public Interest. State and local menu labeling policies. http://www.cspinet.org/new/pdf/ml_map.pdf. Published April, 2011. Accessed May 15, 2014.
- 6.National Conference of State Legislatures. Trans fat and menu labeling legislation. www.ncsl.org/research/health/trans-fat-and-menu-labeling-legislation.aspx. Published January 2013. Accessed May 15, 2014.
- 7.Department of Health and Human Services & Food and Drug Administration. Food Labeling; Nutrition Labeling of Standard Menu Items in Restaurants and Similar Retail Food Establishments. Federal Regulations. 2011;76:19191–19236. [Google Scholar]
- 8.Food Labeling. Nutrition labeling of standard menu items in restaurants and similar retail food establishments; Extension of compliance date. 80 Fed Reg. 2015 Jul 10;:39675. (21 CFR pts. 11 and 101). http://www.gpo.gov/fdsys/pkg/FR-2015-07-10/pdf/2015-16865.pdf. Accessed October 15, 2015. [PubMed]
- 9.Schifter DE, Ajzen I. Intention, perceived control, and weight loss: An application of the theory of planned behavior. J Pers Soc Psychol. 1985;49:843–51. doi: 10.1037//0022-3514.49.3.843. [DOI] [PubMed] [Google Scholar]
- 10.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–72. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 11.Bowers KM, Suzuki S. Menu-Labeling Usage and Its Association with Diet and Exercise: 2011 BRFSS Sugar Sweetened Beverage and Menu Labeling Module. Prev Chronic Dis. 2014;11:130231. doi: 10.5888/pcd11.130231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krieger JW, Chan NL, Saelens BE, Ta ML, Solet D, Fleming DW. Menu Labeling Regulations and Calories Purchased at Chain Restaurants. Am J Prev Med. 2013;44:595–604. doi: 10.1016/j.amepre.2013.01.031. [DOI] [PubMed] [Google Scholar]
- 13.Dumanovsky T, Huang CY, Bassett MT, Silver LD. Consumer Awareness of Fast-Food Calorie Information in New York City After Implementation of a Menu Labeling Regulation. Am J Public Health. 2010;100:2520–5. doi: 10.2105/AJPH.2010.191908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen R, Smyser M, Chan N, Ta M, Saelens BE, Krieger J. Changes in Awareness and Use of Calorie Information After Mandatory Menu Labeling in Restaurants in King County, Washington. Am J Public Health. 2015;105:546–53. doi: 10.2105/AJPH.2014.302262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wethington H, Maynard LM, Haltiwanger C, Blanck HM. Use of calorie information at fast-food and chain restaurants among US Adults, 2009. J Public Health. 2014;36:490–6. doi: 10.1093/pubmed/fdt109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee-Kwan S, Pan L, Maynard L, Kumar G, Park S. Restaurant menu labeling use among adults – 17 states, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(27):581–4. [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Weighting BRFSS Data – BRFSS. 2013 http://www.cdc.gov/brfss/annual_data/2013/pdf/Weighting_Data.pdf. Accessed October 28, 2015.
- 18.Fahimi M, Link M, Mokdad A, Schwartz DA, Levy P. Tracking Chronic Disease and Risk Behavior Prevalence as Survey Participation Declines: Statistics From the Behavioral Risk Factor Surveillance System and Other National Surveys. Prev Chronic Dis. 2008;5(3):A80. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2483564. Accessed May 11, 2014. [PMC free article] [PubMed] [Google Scholar]
- 19.Pierannunzi C, Hu SS, Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med Res Methodol. 2014;13:49. doi: 10.1186/1471-2288-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services. Protection of human subjects. 45 CFR §46. http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.html. Published January 2009. Revised January 15, 2010. Accessed June 8, 2015.
- 21.National Heart Lung and Blood Institute. (NIH Publication 1998; No. 98-4083).Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. http://www.nhlbi.nih.gov/files/docs/guidelines/ob_gdlns.pdf. Accessed November 10, 2015. [PubMed]
- 22.Multinomial Logistic Regression. UCLA: Statistical Consulting Group. http://www.ats.ucla.edu/stat/sas/dae/mlogit.htm. Accessed February 19, 2015.
- 23.Dumanovsky T, Huang CY, Nonas CA, Matte TD, Bassett MT, Silver LD. Changes in energy content of lunchtime purchases from fast food restaurants after introduction of calorie labelling: cross sectional customer surveys. BMJ. 2011;343:d4464. doi: 10.1136/bmj.d4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Breck A, Cantor J, Martinez O, Elbel B. Who reports noticing and using calorie information posted on fast food restaurant menus? Appetite. 2014;81:30–6. doi: 10.1016/j.appet.2014.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Green JE, Brown AG, Ohri-Vachaspati P. Sociodemographic disparities among fast-food restaurant customers who notice and use calorie menu labels. J Acad Nutr Diet. 2015;115(7):1093–101. doi: 10.1016/j.jand.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 26.Bleich SN, Pollack KM. The publics’ understanding of daily caloric recommendations and their perceptions of calorie posting in chain restaurants. BMC Public Health. 2010;10:121. doi: 10.1186/1471-2458-10-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harnack LJ, French SA, Oakes JM, Story MT, Jeffery RW, Rydell SA. Effects of calorie labeling and value size pricing on fast food meal choices: Results from an experimental trial. Int J Behav Nutr Phys Act. 2008;5:63. doi: 10.1186/1479-5868-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bowman SA, Vinyard BT. Fast food consumption of US adults: impact on energy and nutrient intakes and overweight status. J Am Coll Nutr. 2004;23:163–8. doi: 10.1080/07315724.2004.10719357. [DOI] [PubMed] [Google Scholar]
- 29.Paeratakul S, Ferdinand DP, Champagne CM, Ryan DH, Bray GA. Fast-food consumption among US adults and children: dietary and nutrient intake profile. J Am Diet Assoc. 2003;103:1332–8. doi: 10.1016/s0002-8223(03)01086-1. [DOI] [PubMed] [Google Scholar]
- 30.Saelens BE, Chan NL, Krieger J, Nelson Y, Boles M, Colburn TA, Glanz K, Ta ML, Bruemmer B. Nutrition-Labeling Regulation Impacts on Restaurant Environments. Am J Prev Med. 2012;43:505–11. doi: 10.1016/j.amepre.2012.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barabas J, Jerit J. Estimating the Causal Effects of Media Coverage on Policy-Specific Knowledge. Am J Polit Sci. 2009;53:73–89. [Google Scholar]
- 32.Auchincloss A, Young C, Davis AL, Wasson S, Chilton M, Karamanian V. Barriers and facilitators of consumer use of nutrition labels at sit-down restaurant chains. Public Health Nutr. 2013;16:2138–45. doi: 10.1017/S1368980013000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Food US, Administration Drug. How many calories? Look at the menu! http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm423082.htm. Published November 2014. Accessed December 2, 2014.
- 34.Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. Am J Public Health. 2010;100:312–8. doi: 10.2105/AJPH.2009.160226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sinclair SE, Cooper M, Mansfield ED. The influence of menu labeling on calories selected or consumed: A systematic review and meta-analysis. J Acad Nutr Diet. 2014;114:1375–88. doi: 10.1016/j.jand.2014.05.014. [DOI] [PubMed] [Google Scholar]


