Abstract
Purpose
Lifestyle habits of primary care patients with recent, intentional weight loss are unclear and need to be better understood to aid in translational health promotion efforts. We aimed to characterize diet and exercise habits in primary care patients with recent, intentional weight loss, comparing those with greater (≥10%) vs. lesser (5 to <10%) weight loss.
Methods
This was a cross-sectional analysis of baseline data from a randomized trial comparing weight loss maintenance interventions. The study included primary care patients, 18–75 years old, with ≥5% intentional weight loss via lifestyle change in the past 2 years. Participants (74% female, 87% white) had mean age 53 (12) years, body mass index 30.4 (5.9) kg/m2, and recent weight loss of 11 (8)%. Dietary habits were measured by the Diet Habits Survey. Physical activity and sedentary behavior were measured by self-report and objectively by pedometer.
Results
On average, participants reported high fruits and vegetables intake (5 servings/day), and low intake of fried foods (1 serving/week), desserts (1 serving/week) and sugar-sweetened beverages (0 servings/week). Those with greater vs. lesser weight loss had higher intake of fruits and vegetables (p=0.037) and low fat foods or recipes (p=0.019). Average self-reported moderate-vigorous physical activity was 319 (281) minutes/week, with significant differences between greater (374 (328) minutes/week) vs. lesser (276 (230) minutes/week) weight loss groups (p=0.017). By pedometer, 30% had ≥7,500 steps/day; the proportion was higher in greater (43%) vs. lesser (19%) weight loss groups (p=0.005).
Conclusions
For weight loss, clinical patients typically employ simple strategies such as 5+ fruits and vegetables per day, fried foods and desserts ≤1 per week, elimination of sugary drinks, choosing low fat foods/recipes, and physical activity 45–60 min/day.
Keywords: physical activity, sedentary behavior, weight loss, diet, primary care
INTRODUCTION
More than one-third of US adults are obese,(11) a condition that increases the risk of cardiovascular disease, type 2 diabetes, some cancers, and premature death(15) and is estimated to incur an additional $149 million in U.S. healthcare spending annually.(19) Weight loss of as little as 5–10% can improve these health risks(1) and obesity-related medical costs.(24) Unfortunately, achieving weight loss remains challenging,(10, 12) rates of obesity remain high,(16) and population-level approaches to combat the obesity epidemic and its consequences remain an urgent public health need.
Research suggests certain lifestyle habits (i.e., diet and physical activity) are associated with lower weight in general populations. For example, higher consumption of fruits and vegetables and lower consumption of added sugars are associated with decreased weight gain over time.(2, 3, 22, 32) Higher levels of physical activity are also associated with healthier weight trajectories in population studies.(13, 20) Yet, many of these studies reflect observational cohorts that include healthy weight individuals who may be preventing initial weight gain with these strategies or selected populations of otherwise healthy research participants.
Less is known about whether these same habits are used by clinical populations with medical comorbidities who successfully achieve weight loss through lifestyle change. This is an important research gap because physicians and healthcare practitioners have been recognized as an effective channel for communicating lifestyle advice to patients.(14) The American College of Sports Medicine’s Exercise is Medicine (EIM) initiative seeks to make physical activity assessment and prescription a part of each medical encounter.(28) Yet, the paucity of research in clinical populations that have successfully made lifestyle changes is a barrier to translating lifestyle initiatives into clinical practice. For EIM and other translational lifestyle programs to be successful, there is a need to gather data on patients seen in clinical settings who have successfully adapted their lifestyle, lost weight, or otherwise improved health outcomes.
Our objective was to describe lifestyle habits of a clinical, primary care population that recently achieved clinically meaningful, intentional weight loss. Further, we investigated differences in lifestyle behaviors comparing those with greater (≥10%) vs. lesser (5% to <10%) recent weight loss.
METHODS
Subjects and Setting
The current study is a cross-sectional analysis of baseline data from the Maintaining Activity and Nutrition through Technology-Assisted Innovation in Primary Care (MAINTAIN-pc) randomized clinical trial and has been described in detail elsewhere.(7) Briefly, the purpose of MAINTAIN-pc is to evaluate the effects of an online weight loss maintenance intervention in primary care patients. All study participants receive an intervention delivered through a patient portal connected to an electronic health record, and half of the subjects were randomized to receive additional online coaching. To be eligible for the study, participants had to be aged 18–75 years old, to have intentionally lost at least 5% of their body weight in the past 2 years through lifestyle change, and to have (or be able to register for) an electronic patient portal account through the University of Pittsburgh Medical Center. Participants could have lost weight through a variety of methods, such as commercial weight loss programs, self-directed lifestyle changes, or research-based weight loss programs. Exclusion criteria included active preparation for bariatric surgery or pregnancy. MAINTAIN-pc enrolled 194 participants. Two enrolled subjects did not complete the study orientation or any subsequent visits and were thus not included in the current analysis, resulting in a final sample size of 192 participants. All research procedures were approved by the University of Pittsburgh Institutional Review Board. All participants provided written informed consent.
Measures
All measures were collected during the baseline assessment for MAINTAIN-pc, prior to any study-related intervention. Demographic characteristics were measured using standardized questionnaires. Weight and height were measured during the study-specific baseline assessment. The inclusion criteria of qualifying, recent weight loss (≥ 5% in the past 2 years) was verified by abstracting the maximum weight in the past 2 years from the electronic health record and calculating percent weight change.
Dietary habits were assessed using the Connor Diet Habit Survey.(6) This 57-item questionnaire was developed for the rapid assessment of eating habits in the Family Heart Study and queries the usual intake of dietary food groups, salt, sweets and snacks, eating at restaurants, and types of recipes. This instrument has been found to be reliable and valid when compared to the criterion measure of dietary recall, and it has predictive validity as changes in the Diet Habit Survey have been related to changes in plasma cholesterol.(6) Similar to previous research,(2) we used specific questions chosen a priori from the survey to assess dietary habits that we hypothesized would be related to weight loss. These included intake of meats and cheese (oz per day), fruits and vegetables (servings per day), legumes (cups per week), fish (servings per week), and sugar-sweetened beverages. We assessed the type of milk consumed (skim, 1%, 2%, or whole) and estimated the weekly frequency of eating fried foods, desserts, at restaurants, and low-fat recipes. If the survey answers were given as ranges, the midpoint of the range was used to estimate individual dietary habits.
Physical activity and sedentary behavior were based on self-report using standardized instruments from the Behavioral Risk Factor Surveillance Survey (BRFSS) and the Sedentary Behavior Questionnaires (SBQ). Physical activity questions from the BRFSS assess usual participation in moderate and vigorous physical activity and have been found to be reliable and valid for classifying activity level in adults.(38) The SBQ measures time spent sitting in nine behaviors, separately for weekend and weekdays. It has been shown to have acceptable reliability and validity when compared to accelerometer-based inactivity and body mass index in a sample of over 400 overweight adults.(26) For the current study, a weighted average of total sitting time and television viewing time was calculated for the combined weekday and weekend estimates. Objective ambulatory physical activity was captured as steps per day using an Omron pedometer (HJ-720ITC). Participants were asked to wear the pedometer for 14 days during waking hours and return the monitor by mail. Pedometer data that had at least 500 steps/day was included, resulting in valid data for 166 participants, with an mean (SD) of 13.0 (1.9) wear days per participant. Steps per day were classified as sedentary (<5,000 steps per day), low active (5,000–7,499 steps per day), and active (≥ 7,500 steps per day) based on established cut points.(36)
Statistical Analyses
Participant characteristics and outcomes were described using means with standard deviations, medians with 25th and 75th percentiles, or counts with percentages. This was done overall and by categories of recent weight loss (greater: ≥10%; lesser: 5 to <10%). Participant characteristics and outcomes were compared across groups using independent t tests, Fisher’s exact tests, chi-square tests, or Wilcoxon tests, as appropriate. Post hoc tests, where appropriate, used Bonferroni adjustment for multiple comparisons.
RESULTS
Baseline characteristics of participants in the MAINTAIN-pc study are displayed in Table 1. Participants tended to be middle-aged (mean (SD) age was 53 (12) years), female (74%), and white (87%). About three quarters of participants had at least a college degree and 70% were employed full time. Smoking was infrequent and most reported no or minimal alcohol intake. Cardiovascular risk factors (high blood pressure and dyslipidemia) and musculoskeletal disorders affected about half of participants, while a smaller percentage had diabetes or cardiovascular disease. Though participants had lost an average of 11% of their body weight as qualifying recent weight loss for the study, the mean (SD) BMI was still in the obese category (30.4 (5.9) kg/m2) but had decreased from a maximum BMI of 34.4 (6.5) kg/m2 in the past 24 months.
Table 1.
Participant Characteristics Overall and by Percentage of Recent Weight Loss (n=192)
| Overall | 5 to <10% WL (n = 107) | ≥10% WL (n = 85) | p-value* | |
|---|---|---|---|---|
| Age, years | 53 (12) | 54 (13) | 53 (12) | 0.765 |
|
| ||||
| Male, n (%) | 50 (26%) | 26 (24%) | 24 (28%) | 0.537 |
|
| ||||
| Race | 0.858 | |||
| White | 167 (87%) | 94 (88%) | 73 (86%) | |
| Black | 19 (10%) | 10 (9%) | 9 (11%) | |
| Hispanic | 3 (2%) | 1 (1%) | 2 (2%) | |
| Asian | 3 (2%) | 2 (2%) | 1 (1%) | |
|
| ||||
| Education | 0.397 | |||
| High school | 9 (5%) | 4 (4%) | 5 (6%) | |
| Some college | 37 (19%) | 25 (24%) | 12 (14%) | |
| College | 61 (32%) | 33 (21%) | 40 (47%) | |
| Graduate degree | 85 (44%) | 25 (42%) | 63 (74%) | |
|
| ||||
| Employment | 0.239 | |||
| Full-time | 135 (70%) | 72 (67%) | 63 (74%) | |
| Unemployed | 6 (3%) | 4 (4%) | 5 (6%) | |
| Homemaker | 5 (3%) | 3 (3%) | 2 (2%) | |
| Student | 4 (2%) | 4 (3%) | 0 (0%) | |
| Retired | 38 (20%) | 20 (19%) | 18 (21%) | |
| Other | 4 (2%) | 4 (4%) | 0 (0%) | |
|
| ||||
| Smoker. n (%) | 5 (3%) | 3 (3%) | 2 (2%) | 1.000 |
|
| ||||
| Current Alcohol | 0.043 | |||
| Never | 64 (33%) | 31 (29%) | 33 (39%) | |
| ≤4 per month | 85 (44%) | 45 (42%) | 40 (47%) | |
| > 4 per month | 43 (22%) | 31 (29%) | 12 (14%) | |
|
| ||||
| Body mass index, kg/m2 | ||||
| Current | 30.4 (5.9) | 31.4 (6.0) | 29.1 (5.6) | 0.007 |
| Highest in past 24 mo. | 34.4 (6.5) | 33.8 (6.4) | 35.1 (6.7) | 0.179 |
|
| ||||
| Current Weight, lbs | 189 (42) | 196 (43) | 180 (39) | 0.009 |
|
| ||||
| Recent weight loss, % | −11% (8%) | −7% (2%) | −17% (9%) | <0.001 |
|
| ||||
| Comorbid Conditions | ||||
| High blood pressure | 96 (50%) | 54 (50%) | 43 (51%) | 0.884 |
| Dyslipidemia | 83 (43%) | 53 (50%) | 30 (35%) | 0.048 |
| Diabetes | 26 (14%) | 16 (15%) | 10 (12%) | 0.521 |
| Cardiovascular disease | 20 (10%) | 7 (7%) | 13 (15%) | 0.049 |
| Musculoskeletal disorder | 98 (51%) | 50 (46%) | 48 (57%) | 0.180 |
Data presented as mean (SD) or n (%)
p-value compares 5–<10% vs. ≥10% weight loss
Few differences were observed in participant characteristics when comparing greater to lesser recent weight loss categories (Table 1). In addition to the expected differences in amount of recent weight loss, current weight, and BMI, participants with greater weight loss were more likely to consume less alcohol (p = 0.043) and had a lower prevalence of dyslipidemia (p = 0.048), but they also had a higher prevalence of cardiovascular disease (p = 0.049).
Description of Dietary Habits Overall and by Amount of Recent Weight Loss
Dietary habits of study participants are listed in the first column of Table 2. The median meat and cheese consumption was 7 oz. per day and, for fruits and vegetables, it was 5 servings per day. Participants reported consuming about 1 cup of legumes and 1 serving of fish per week. Consumption of fried foods (1 serving per week) and desserts (1 serving per week) was infrequent. Most participants did not consume sugar-sweetened beverages per week, with only 17.7% of participants reporting any weekly consumption. More than half of participants consumed skim milk and participants reported eating low-fat foods or recipes 4 times per week. Participants ate at restaurants a median of 2 times per week.
Table 2.
Dietary Habits in Primary Care Patients with Recent Intentional Weight Loss by Amount of Recent Weight Loss
| Overall | 5 to <10% Weight Loss (n = 107 ) | ≥10% Weight Loss (n = 85) | p-value | |
|---|---|---|---|---|
| Cheeses and meats, oz per day | 7 [5, 7] | 7 [5, 7] | 7 [5, 7] | 0.407 |
|
| ||||
| Fruits and vegetables, servings per day | 5 [3, 6] | 5 [3, 6] | 5 [4, 7] | 0.037 |
|
| ||||
| Legumes, cups per week | 1 [0, 2] | 1 [0, 2]] | 1 [0, 2] | 0.941 |
|
| ||||
| Fish, servings per week | 1 [1, 2] | 1 [1, 2] | 1 [1, 2] | 0.336 |
|
| ||||
| Sugar-sweetened beverages, oz. per week | 0 [0, 0] | 0 [0, 0] | 0 [0, 0] | 0.274 |
|
| ||||
| Type of Milk | ||||
| Skim | 113 (59%) | 56 (52%) | 57 (67%) | 0.169 |
| 1% | 29 (15%) | 20 (19%) | 9 (11%) | |
| 2% | 24 (17.7%) | 20 (19%) | 14 (17%) | |
| Whole | 16 (8%) | 11 (10%) | 5 (6%) | |
|
| ||||
| Fried foods, servings per week | 1 [0, 3] | 1 [0, 3] | 0 [0, 1] | 0.181 |
|
| ||||
| Desserts, servings per week | 1 [1, 4] | 1 [1, 4] | 1 [1, 4] | 0.492 |
|
| ||||
| Eating at restaurants, times per week | 2 [1, 4] | 2 [1, 4] | 1 [1, 4] | 0.150 |
|
| ||||
| Low-fat foods or recipes, times per week | 4 [2, 6] | 2 [0, 6] | 4 [2, 6] | 0.019 |
Data are reported as median [25th percentile, 75th percentile] or mean ± SD
When comparing greater vs. lesser recent weight loss subgroups of participants, there were statistically important differences in some habits and behaviors (Table 2). Though the median was the same across weight loss categories, participants with greater recent weight loss ate more fruits and vegetables (75th percentile was 7 vs. 6 servings per day, p=0.037) suggesting the overall distribution was shifted toward higher amounts of daily fruits and vegetables intake in the greater weight loss group. Those in the greater weight loss group were also more likely to eat low-fat foods or recipes (median was 4 vs. 2 times per week, p=0.019). Other habits were statistically similar.
Description of Physical Activity Habits Overall and by Amount of Recent Weight Loss
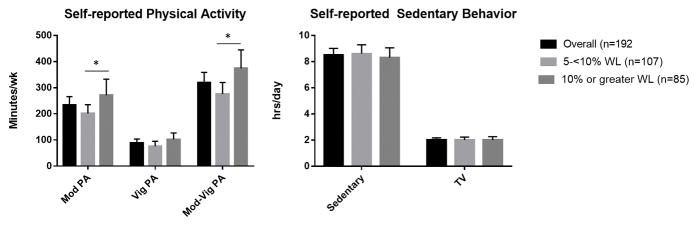
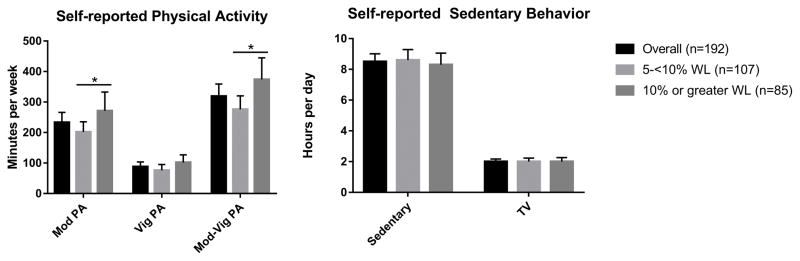
Participants reported high levels of moderate intensity physical activity with a mean (SD) of 233 (233) minutes/week and vigorous intensity physical activity with a mean (SD) of 88 (108) minutes/week, totaling an average (SD) of 319 (281) minutes/week of moderate-vigorous intensity physical activity which equates to 5.3 hr/wk (Figure 1). When separated into weight loss categories, individuals with greater vs. lesser recent weight loss had higher moderate intensity physical activity with mean (SD) (271 (287) vs. 202 (173) minutes/week (p=0.039) and higher moderate-vigorous intensity physical activity with mean (SD) 374 (328) vs. 276 (230) minutes/week, (p=0.017). Mean (SD) self-reported sedentary behavior was 8.5 (3.6) hrs/day and television viewing 2.0 (1.2); these sedentary behaviors were similar across weight loss groups.
Figure 1. Self-reported Physical Activity and Sedentary Behavior in Primary Care Patients with Recent Weight Loss (n = 192) Overall and by Percentage of Recent Weight Loss.
Mod PA = moderate intensity physical activity; Vig PA = vigorous intensity physical activity; Mod-Vig PA = moderate-vigorous intensity physical activity; TV = television; WL = weight loss. * p<0.05 when comparing 5–<10% weight loss to 10% or greater weight loss categories.
Mean (SD) steps were 6,318 (3,188) per day and, using steps per days, 42% were classified as sedentary, 32% were classified as low active, and 26% were classified as active. When categorized by greater vs. lesser recent weight loss, those with greater weight loss had higher mean steps per day (1,723 greater steps per day, p=0.005). When classified into activity levels based on steps, the overall distribution differed in those with greater vs. lesser weight loss (p=0.005) and post hoc testing revealed that those with greater vs. lesser weight loss were more likely to be classified as active (43% vs. 14%, p=0.003) and less likely to be classified as insufficiently active (22% vs. 40%, p=0.048)(Figure 2).
Figure 2. Objectively-measured Physical Activity Category in Primary Care Patients with Recent Weight Loss (n = 166) Overall and by Amount of Recent Weight Loss.
Sedentary indicates <5,000 steps per day; Low Active indicates 5,000–7,499 steps per day; Active indicates ≥7,500 steps per day.
*p<0.05 comparing greater to lesser weight loss groups
**p<0.01 comparing greater to lesser weight loss groups
DISCUSSION
We have described some typical dietary and physical activity habits in a clinical population of primary care patients who had recently achieved clinically meaningful and intentional weight loss through a variety of methods. On average, study participants reported consuming the recommended 5 servings of fruits and vegetables per day, limiting their intake of desserts and fried foods (once per week), and avoiding sugar-sweetened beverages. Participants with greater recent weight loss reported eating more fruits and vegetables and more low-fat foods and recipes vs. those with lesser recent weight loss. Those with greater weight loss were also more physically active.
Our data provide evidence in a contemporary cohort of primary care patients that common dietary recommendations from the United States Department of Agriculture,(37) American Dietetic Association,(29) and the American Heart Association(21) prioritizing a diet rich in produce,(21, 37) low in fat (limited fried foods and frequent low fat choices),(21, 29) and low in added sugars (desserts and sugar-sweetened beverages)(2, 21) are part of a lifestyle strategy that has resulted in successful weight loss. Our findings are comparable to those from a 4-year lifestyle intervention study in post-menopausal women that found decreased sugar-sweetened beverages and desserts, decreased fried foods, and increased fruits and vegetables (similarly measured by the Dietary Habits Survey) were associated with lower weight.(2) One somewhat surprising result was that participants in this study reported eating at restaurants twice a week and this number was similar across weight loss categories, suggesting that occasional eating at restaurants and weight loss can coexist.
Intake of fruits and non-starchy vegetables has also been inversely associated with weight gain in large cohort studies,(3) though a recent meta-analysis of randomized intervention trials concluded that increasing fruits and vegetables alone was not an effective strategy for weight loss.(18) However, the authors also noted that most of the studies included in the meta-analysis were short in duration (e.g., 8 weeks),(18) and it is possible that increasing fruits and vegetables represents a ‘small change strategy’ that is more conducive to long-term vs. short-term weight loss or maintenance.(2)
The data suggesting an association between added sugar (especially sugar-sweetened beverages) and weight gain are more consistent. A meta-analysis of the effects of sugar-sweetened beverage consumption on weight change found clearly positive associations between consumption and weight gain in adults and children in longitudinal cohort studies.(22) The same meta-analysis found that randomized trials reducing sugar-sweetened beverages prevented weight gain in children, while trials increasing sugar-sweetened beverages led to weight gain in adults.(22) Similar results were observed in a meta-analysis evaluating added sugars (sugar-sweetened beverages and other foods such as desserts), but this study adds a finding in adults where recommendations to decrease added sugars were associated with weight loss and vice versa.(32)
Though a low fat diet is widely recommended due to the high energy density of fat,(21, 29) controversy exists as to whether a low fat diet is preferred for weight loss. Two recent meta-analyses of clinical trials comparing dietary interventions concluded that a low fat diet resulted in less weight loss compared to a low carbohydrate diet.(27, 34) Yet, low carbohydrate diets have been criticized for less favorable changes to cardiovascular risk factors such as higher low density lipoprotein cholesterol.(23) An important distinction is that, in the current study, adherence to an overall low fat diet was not evaluated. Rather, among primary care patients with recent weight loss, those who had recently lost more vs. less weight were more likely to consume low fat foods and recipes – on average 4 times per week. It is possible that the low-fat choice among individuals with greater weight loss may reflect the higher prevalence of cardiovascular disease in this group, which could potentially also influence motivation for weight loss.
Higher levels of physical activity have been associated with decreased weight gain and maintenance of healthy weight in large observational studies such as the Coronary Artery Risk Development in young Adults Study (CARDIA)(13) and the Women’s Health Study.(20) In clinical trials, physical activity results in modest weight loss (1–3 kgs) either in isolation or in addition to caloric restriction as part of a lifestyle intervention.(8, 30, 31) The American College of Sports Medicine recommends between 150–250 minutes per week of moderate intensity physical activity for weight loss and ≥250 minutes per week for weight loss maintenance.(9) The Institute of Medicine suggests that 60 minutes of physical activity per day (420 minutes per week) are needed to prevent overweight and obesity.(35) Primary care patients with recent weight loss enrolled in the current study, on average, reported participated in about 45 minutes per day (319 minutes per week) of moderate-vigorous physical activity; those with greater weight loss participated in 53 minutes per day (376 minutes per week). Of interest, the high levels of physical activity participation and its direct association with greater weight loss at enrollment into MAINTAIN-pc was similar to that reported by enrolling participants of the National Weight Control Registry (with ≥ 30 lbs. weight loss maintained it for at least 1 year).(4, 5) Thus, despite the modest contribution of physical activity to weight loss, consistent findings that high levels of physical activity are present in successful weight losers and with consideration for the numerous other health benefits of physical activity, 45–60 minutes per day of physical activity could be recommended to primary care patients as potentially important for promoting weight loss.
Though the levels of self-reported physical activity were high in our sample, on average above the recommended threshold of ≥150 minutes per week, (9) objectively-measured steps suggested that ~70% were below the threshold corresponding to meeting recommendations. (36) This could reflect over-reporting or the inability of a pedometer to capture non-ambulatory physical activity (e.g., swimming, bicycling).(25) However, the observed association between higher physical activity category and greater weight category was consistent regardless of measurement method, adding strength to the overall finding. Also, despite the limitations, self-report and perhaps increasingly step counts are the primary methods of assessing physical activity in the clinic, making our results helpful for translation.
Our study has strengths including the unique primary care population who lost weight through a variety of real-world methods and presented with comorbidities that would typically be encountered in medical practice (but perhaps not in clinical research). These data therefore contribute to the overarching goal of designing weight loss interventions that are readily translated to clinical settings. This contrasts with the much larger National Weight Control Registry, which includes thousands of participants of similar age to our sample but who had maintained an average weight loss of over 30% at the time of enrollment.(33) Though weight loss maintenance of the magnitude observed in the National Weight Control Registry is desirable, the more modest weight loss included in MAINTAIN-pc (particularly those with 5 to <10% weight loss) is important to study because such smaller weight losses are associated with health benefits(17) and may be more achievable on the population level. Other strengths include that weight loss and steps per day were objectively assessed. Lastly, the dietary assessment instrument allowed us to evaluate habits which may lend more easily to recommendations from healthcare providers to patients.
A limitation of this cross-sectional analysis is the limited ability to infer causation between dietary and physical activity habits and weight loss due to concurrent measurement. Also, although we compared participants with greater and lesser weight loss at the time of enrollment, the sampling strategy of MAINTAIN-pc did not include a comparison group of individuals unsuccessful at weight loss which could have strengthened conclusions. Further, while all study participants recently lost weight and expressed an interest in continuing to lose weight or maintain weight loss, it is possible that their currently reported eating patterns differ from those used during weight loss. Some dietary habits (e.g., whole grains, nuts) could not be considered because they are not easily delineated from the dietary instrument used. Lastly, generalizability of our findings might be limited based on the largely white, highly educated sample.
Our findings add valuable data for translating best practices for lifestyle counselling to clinical encounters. Barriers to lifestyle counselling during medical visits are numerous and include an inconsistent literature regarding effective weight loss strategies – especially in clinical patient populations, lack of time, insufficient training in effective lifestyle counselling, and low confidence in patients’ abilities to enact lifestyle advice.(14) Overcoming these barriers to capitalize on the unique opportunity for lifestyle counselling during clinical encounters ideally incorporates simple recommendations for both physicians and patients but also must be based on relevant data such as that presented herein. Despite the ever growing number of studies that both support and refute dietary recommendations, our findings are consistent with conventional wisdom for weight loss strategies, based on more fruits and vegetables, less added sugar, and inclusion of low fat choices. Most people who are successful at losing weight perform high levels of physical activity. Whether these habits are the most effective or simply the most palatable and sustainable is not clear, but in either case they are a good place to start for clinical populations needing to lose weight. Future studies comparing primary care patients that are both successful and unsuccessful at weight loss and testing the delivery of these specific lifestyle messages in clinical settings will inform translating best practices for lifestyle counselling.
Acknowledgments
MAINTAIN-pc was funded by a grant from the Agency for Health Research and Quality (R18HS021162-02) and was supported by the National Institutes of Health through Grant Number UL1TR000005 (University of Pittsburgh CTSI, providing research registry support). Preliminary analyses from this manuscript were presented as abstracts at the American Heart Association Lifestyle|Epidemiology conference in March, 2017.
Footnotes
CONFLICTS OF INTEREST
Dr. Barone Gibbs received grant funding to her institution from Humanscale to study the health effects of using a sit-stand desk. Drs. Conroy, Hess, and McTigue received royalties paid to the University of Pittsburgh Division of General Internal Medicine from Canary Health for assisting in the development of an online lifestyle program. The other authors report no conflicts of interest. Results of this study do not constitute endorsement of the American College of Sports Medicine.
References
- 1.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. WMJ. 1998;97(9):20–1. 4–5, 7–37. [PubMed] [Google Scholar]
- 2.Barone Gibbs B, Kinzel LS, Pettee Gabriel K, Chang YF, Kuller LH. Short- and long-term eating habit modification predicts weight change in overweight, postmenopausal women: results from the WOMAN study. J Acad Nutr Diet. 2012;112(9):1347–55. 55 e1–2. doi: 10.1016/j.jand.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bertoia ML, Mukamal KJ, Cahill LE, Hou T, Ludwig DS, Mozaffarian D, et al. Changes in Intake of Fruits and Vegetables and Weight Change in United States Men and Women Followed for Up to 24 Years: Analysis from Three Prospective Cohort Studies. PLoS Med. 2015;12(9):e1001878. doi: 10.1371/journal.pmed.1001878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Catenacci VA, Odgen L, Phelan S, Thomas JG, Hill J, Wing RR, et al. Dietary habits and weight maintenance success in high versus low exercisers in the National Weight Control Registry. J Phys Act Health. 2014;11(8):1540–8. doi: 10.1123/jpah.2012-0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Catenacci VA, Ogden LG, Stuht J, Phelan S, Wing RR, Hill JO, et al. Physical activity patterns in the National Weight Control Registry. Obesity (Silver Spring) 2008;16(1):153–61. doi: 10.1038/oby.2007.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Connor SL, Gustafson JR, Sexton G, Becker N, Artaud-Wild S, Connor WE. The Diet Habit Survey: a new method of dietary assessment that relates to plasma cholesterol changes. J Am Diet Assoc. 1992;92(1):41–7. Epub 1992/01/01. [PubMed] [Google Scholar]
- 7.Conroy MB, Bryce CL, McTigue KM, Tudorascu D, Gibbs BB, Comer D, et al. Promoting weight maintenance with electronic health record tools in a primary care setting: Baseline results from the MAINTAIN-pc trial. Contemporary Clinical Trials. 2017;54:60–7. doi: 10.1016/j.cct.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 8.DeLany JP, Kelley DE, Hames KC, Jakicic JM, Goodpaster BH. Effect of physical activity on weight loss, energy expenditure, and energy intake during diet induced weight loss. Obesity (Silver Spring) 2014;22(2):363–70. doi: 10.1002/oby.20525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK, et al. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–71. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 10.Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 11.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–91. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fothergill E, Guo J, Howard L, Kerns JC, Knuth ND, Brychta R, et al. Persistent metabolic adaptation 6 years after “The Biggest Loser” competition. Obesity (Silver Spring) 2016;24(8):1612–9. doi: 10.1002/oby.21538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hankinson AL, Daviglus ML, Bouchard C, Carnethon M, Lewis CE, Schreiner PJ, et al. Maintaining a high physical activity level over 20 years and weight gain. JAMA. 2010;304(23):2603–10. doi: 10.1001/jama.2010.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hivert MF, Arena R, Forman DE, Kris-Etherton PM, McBride PE, Pate RR, et al. Medical Training to Achieve Competency in Lifestyle Counseling: An Essential Foundation for Prevention and Treatment of Cardiovascular Diseases and Other Chronic Medical Conditions: A Scientific Statement From the American Heart Association. Circulation. 2016 doi: 10.1161/CIR.0000000000000442. [DOI] [PubMed] [Google Scholar]
- 15.Hruby A, Manson JE, Qi L, Malik VS, Rimm EB, Sun Q, et al. Determinants and Consequences of Obesity. Am J Public Health. 2016;106(9):1656–62. doi: 10.2105/AJPH.2016.303326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imes CC, Burke LE. The Obesity Epidemic: The United States as a Cautionary Tale for the Rest of the World. Curr Epidemiol Rep. 2014;1(2):82–8. doi: 10.1007/s40471-014-0012-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, et al. Executive summary: Guidelines (2013) for the management of overweight and obesity in adults. Obesity. 2014;22(S2):S5–S39. [Google Scholar]
- 18.Kaiser KA, Brown AW, Bohan Brown MM, Shikany JM, Mattes RD, Allison DB. Increased fruit and vegetable intake has no discernible effect on weight loss: a systematic review and meta-analysis. Am J Clin Nutr. 2014;100(2):567–76. doi: 10.3945/ajcn.114.090548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim DD, Basu A. Estimating the Medical Care Costs of Obesity in the United States: Systematic Review, Meta-Analysis, and Empirical Analysis. Value Health. 2016;19(5):602–13. doi: 10.1016/j.jval.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 20.Lee IM, Djousse L, Sesso HD, Wang L, Buring JE. Physical activity and weight gain prevention. JAMA. 2010;303(12):1173–9. doi: 10.1001/jama.2010.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. Epub 2010/01/22. CIRCULATIONAHA.109.192703 [pii] [DOI] [PubMed] [Google Scholar]
- 22.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98(4):1084–102. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mansoor N, Vinknes KJ, Veierod MB, Retterstol K. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomised controlled trials. Br J Nutr. 2016;115(3):466–79. doi: 10.1017/S0007114515004699. [DOI] [PubMed] [Google Scholar]
- 24.Oster G, Thompson D, Edelsberg J, Bird AP, Colditz GA. Lifetime health and economic benefits of weight loss among obese persons. Am J Public Health. 1999;89(10):1536–42. doi: 10.2105/ajph.89.10.1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. International Journal of Behavioral Nutrition and Physical Activity. 2008;5(1):56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosenberg DE, Norman GJ, Wagner N, Patrick K, Calfas KJ, Sallis JF. Reliability and validity of the Sedentary Behavior Questionnaire (SBQ) for adults. J Phys Act Health. 2010;7(6):697–705. doi: 10.1123/jpah.7.6.697. Epub 2010/11/23. [DOI] [PubMed] [Google Scholar]
- 27.Sackner-Bernstein J, Kanter D, Kaul S. Dietary Intervention for Overweight and Obese Adults: Comparison of Low-Carbohydrate and Low-Fat Diets. A Meta-Analysis. PLoS One. 2015;10(10):e0139817. doi: 10.1371/journal.pone.0139817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sallis R. Exercise is medicine: a call to action for physicians to assess and prescribe exercise. The Physician and sportsmedicine. 2015;43(1):22–6. doi: 10.1080/00913847.2015.1001938. Epub 2015/02/17. [DOI] [PubMed] [Google Scholar]
- 29.Seagle HM, Strain GW, Makris A, Reeves RS American Dietetic A. Position of the American Dietetic Association: weight management. J Am Diet Assoc. 2009;109(2):330–46. doi: 10.1016/j.jada.2008.11.041. [DOI] [PubMed] [Google Scholar]
- 30.Shaw K, Gennat H, O’Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006;(4):CD003817. doi: 10.1002/14651858.CD003817.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56(4):441–7. doi: 10.1016/j.pcad.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2013;346:e7492. doi: 10.1136/bmj.e7492. [DOI] [PubMed] [Google Scholar]
- 33.Thomas JG, Bond DS, Phelan S, Hill JO, Wing RR. Weight-loss maintenance for 10 years in the National Weight Control Registry. Am J Prev Med. 2014;46(1):17–23. doi: 10.1016/j.amepre.2013.08.019. Epub 2013/12/21. [DOI] [PubMed] [Google Scholar]
- 34.Tobias DK, Chen M, Manson JE, Ludwig DS, Willett W, Hu FB. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3(12):968–79. doi: 10.1016/S2213-8587(15)00367-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trumbo P, Schlicker S, Yates AA, Poos M Food, Nutrition Board of the Institute of Medicine TNA. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc. 2002;102(11):1621–30. doi: 10.1016/s0002-8223(02)90346-9. [DOI] [PubMed] [Google Scholar]
- 36.Tudor-Locke C, Craig CL, Thyfault JP, Spence JC. A step-defined sedentary lifestyle index: <5000 steps/day. Appl Physiol Nutr Metab. 2013;38(2):100–14. doi: 10.1139/apnm-2012-0235. [DOI] [PubMed] [Google Scholar]
- 37.United States. Department of Health and Human Services., United States. Department of Agriculture., United States. Dietary Guidelines Advisory Committee. Dietary guidelines for Americans, 2010. 7. xi. Washington, D.C: G.P.O; 2010. p. 95. [Google Scholar]
- 38.Yore MM, Ham SA, Ainsworth BE, Kruger J, Reis JP, Kohl HW, 3rd, et al. Reliability and validity of the instrument used in BRFSS to assess physical activity. Med Sci Sports Exerc. 2007;39(8):1267–74. doi: 10.1249/mss.0b013e3180618bbe. [DOI] [PubMed] [Google Scholar]