Abstract
We describe novel plasmid DNA that encodes the full-length Japanese encephalitis virus (JEV) genomic cDNA and launches live-attenuated JEV vaccine in vitro and in vivo. The synthetic cDNA based on the sequence of JEV SA14-14-2 live-attenuated virus was placed under transcriptional control of the cytomegalovirus major immediate-early promoter. The stability and yields of the plasmid in E. coli were optimized by inserting three synthetic introns that disrupted JEV cDNA in the structural and nonstructural genes. Transfection of Vero cells with the resulting plasmid resulted in the replication of JEV vaccine virus with intron sequences removed from viral RNA. Furthermore, a single-dose vaccination of BALB/c mice with 0.5 – 5 μg of plasmid resulted in successful seroconversion and elicitation of JEV virus-neutralizing serum antibodies. The results demonstrate the possibility of using DNA vaccination to launch live-attenuated JEV vaccine and support further development of DNA-launched live-attenuated vaccine for prevention of JEV infections.
Keywords: Japanese encephalitis virus, JEV, JE, DNA vaccine, liveattenuated virus, iDNA
1. Introduction
Japanese encephalitis virus (JEV) is a flavivirus related to dengue, yellow fever and West Nile viruses and is the main cause of acute viral encephalitis in the Asia-Pacific region, primarily affecting children and young adults. JEV causes epidemics throughout Asia and is transmitted by the mosquito Culex tritaeniorhynchus (Heffelfinger et al., 2017; Mansfield et al., 2017; Wang et al., 2015). Four types of JEV vaccine have been licensed in different regions of the world (CDC, 2016; Wang et al., 2015; WHO, 2015). Over recent decades, killed virus vaccines were prepared in tissue culture or in mouse brain and have been used to immunize travelers and residents of enzootic countries. Concerns associated with cost, efficacy and safety of these vaccines have led to the development of other vaccines including live-attenuated vaccine SA14-14-2, chimeric vaccine YF-JEV, as well as purified inactivated, tissue culture-derived vaccine (Halstead and Thomas, 2011). Currently, attenuated strain SA14-14-2 derived from its wild-type parental strain SA14 is the most common strain used in vaccine development and production (Chen et al., 2015; Yu, 2010). However, despite available clinical and experimental JEV vaccines, improvements are needed for JEV vaccination due to limitations of currently available vaccines (Chen et al., 2015; Mansfield et al., 2017). Among early alternative approaches, plasmid DNA vaccines have been developed that expressed structural or non-structural JEV proteins in vivo. In a mouse model, DNA vaccines elicited detectable protection against challenge with a lethal dose of JEV (Putnak et al., 2003).
Previous results suggested that both live and inactivated JEV vaccines are safe and effective against JEV and can also elicit strong cross-immunity and protection in mice against all four serotypes of dengue, a related flavivirus (Li et al., 2016). However, there was also an indication of JEV vaccine-facilitated dengue virus infection-enhancement antibody in adults (Saito et al., 2016). Therefore, additional research is needed, and despite existing vaccines, improvements may be needed for JEV vaccination due to limitations of current vaccines.
DNA vaccines for JEV have been studied as alternative to traditional vaccines due to their potential to be safe and inexpensive formulations. Experimental DNA vaccines have been developed using plasmids that expressed JEV proteins (Putnak et al., 2003). Plasmids expressing the E protein induced JEV neutralizing antibodies, which are important indicators of protection (Konishi et al., 1999). Plasmid DNA vaccine encoding prM and E proteins appeared to provide more effective vaccination as compared with a construct expressing E protein alone (Konishi et al., 2003; Wu et al., 2006). However, similarly to other standard DNA vaccines, the immunogenicity of plasmid DNA encoding JEV proteins was relatively low as compared to inactivated vaccine (Bharati et al., 2005; Kaur et al., 2002). The immune response could be augmented by using advanced adjuvants and electroporation. DNA vaccine expressing prM-E proteins of JEV was found effective in mice following i.m. injection; however, when accompanied with electroporation, immune responses were improved in mouse and pig models (Sheng et al., 2016). The use of granulocyte-macrophage colony-stimulating factor to enhance immunogenicity of prM-E DNA based vaccine has been reported (Zhai et al., 2015).
Recently, DNA-launched live-attenuated vaccines have been described, which combine chemical and genetic stability of DNA vaccines with the efficacy of traditional live-attenuated vaccines (Pushko et al., 2016; Tretyakova et al., 2013). This platform is based on the infectious clone technology and represents plasmid DNA that encodes the full-length virus RNA and can initiate replication of viral RNA and launch live-attenuated virus in vitro or in vivo (Jiang et al., 2015; Pushko et al., 2014; Tretyakova et al., 2014a; Tretyakova et al., 2014b). DNA-launched live-attenuated vaccines were sometimes called iDNA® vaccines in order to distinguish them from the standard DNA vaccines (Pushko et al., 2016; Tretyakova et al., 2013; Tretyakova et al., 2014b). In the previous studies, the full-length JEV infectious clone has been reported and used to launch JEV from a plasmid in vitro. Transfection of the plasmid containing full-length JEV into mammalian cells resulted in the replication of JEV (Mishin et al., 2001; Yamshchikov et al., 2001). However, vaccination with the plasmid has not been evaluated in vivo. One potential reason for that was the difficulty of generating stable full-length JEV clone in E. coli. Hypothetically, JEV cDNA can contain cryptic bacterial promoters that drive synthesis of toxic proteins affecting genetic stability and DNA yields in E. coli (Rice et al., 1989; Tretyakova et al., 2014b; Yamshchikov et al., 2001). To improve stability of the plasmid in E. coli, the low-copy vector backbone has been used and two introns have been inserted into the full-length JEV cDNA clone. It is expected that the JEV RNA is transcribed from the plasmid in the nucleus, introns are removed from JEV RNA by RNA splicing machinery, and the full-length JEV RNA is secreted from the nucleus into cytoplasm to launch replication of live-attenuated virus (Yamshchikov et al., 2001).
In the current study, we report novel iDNA plasmid capable of launching live-attenuated JEV vaccine in vitro or in vivo. Plasmid was prepared by using the synthetic cDNA based on the SA14-14-2 strain. The stability and yields of the full-length plasmid in E. coli were achieved by inserting three synthetic introns in both the structural and nonstructural genes of JEV cDNA. The plasmid was initially confirmed for launching the JEV vaccine virus in vitro. Furthermore, this novel iDNA vaccine was evaluated in BALB/c mice for the ability to elicit immune response to JEV including virus-neutralizing serum antibody. Neutralizing antibody was detected after a single dose vaccination with either 500 ng or 5 μg of plasmid suggesting that the DNA-launched live-attenuated vaccine approach can be a feasible approach for the development of novel JEV vaccine.
2. Materials and Methods
2.1. Cell lines and viruses
African green monkey (Vero) and baby hamster kidney (BHK) cell lines were obtained from the American Type Culture Collection (ATCC, Manassas, VA) and were maintained in a humidified incubator at 37°C and 5% CO2 in αMEM medium supplemented with 10% fetal bovine serum (FBS) and gentamicin sulfate (10 μg/ml) (Thermo Scientific (Thermo), Carlsbad, CA).
2.2. Plasmids and preparation of iDNA
The full-length nucleotide sequence of cDNA for JEV live-attenuated vaccine strain SA14-14-2 (Genbank accession number AF315119) was prepared using synthetic biology methods (Wimmer et al., 2009). The resulting complete JEV cDNA sequence was cloned into kanamycin- resistant, high-copy pUC57 plasmid (Genscript, Piscataway, NJ) carrying standard ColE1/pMB1 origin of replication. CMV major immediate-early promoter was inserted upstream from the full-length SA14-14-2 cDNA. A ribozyme sequence derived from the hepatitis delta virus was inserted downstream from the JEV 3′ terminal sequence. In addition, three synthetic introns were inserted into the JEV sequence downstream of predicted bacterial promoters within the JEV genomic sequence with the purpose of preventing synthesis of potentially toxic proteins in E. coli. The E. coli promoters have been predicted by using BPROM software (SoftBerry, Mount Kisco, NY) to identify sites for intron insertions. Three chimeric introns 133, 82 and 118 bp in length were inserted into capsid, envelope, and NS1 genes of SA14-14-2 cDNA, respectively. Intron sequences were derived from mouse and human immunoglobulin precursor genes and synthesized with unique restriction sites to facilitate insertion into JEV cDNA. As a result, plasmid pMG8009 iDNA® was generated that encoded the SA14-14-2 full-length genomic RNA under transcriptional control of the CMV promoter (Fig. 1). The JEV iDNA was confirmed by DNA sequencing to be identical to Genbank AF315119 except the synthetic intron sequences in pMG8009.
Fig. 1.
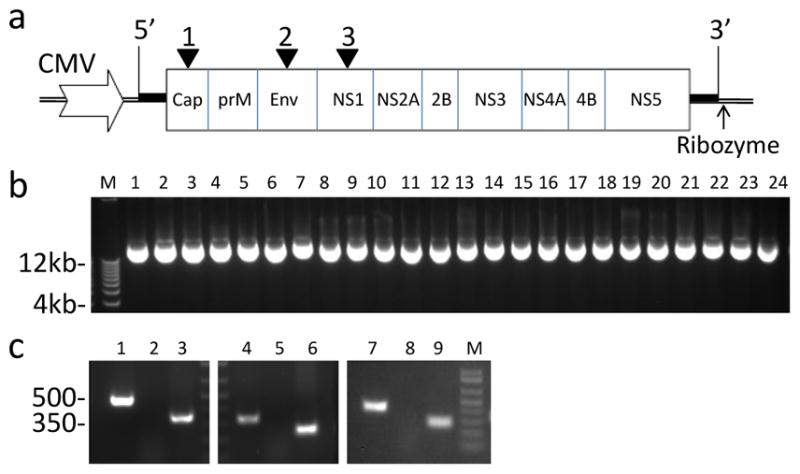
Preparation of pMG8009 JEV iDNA® vaccine containing synthetic cDNA of SA-14-14-2 JEV strain. (a) Diagram of iDNA construct. Locations of CMV promoter, JEV cDNA, genes, ribozyme and introns 1–3 (filled triangles) are shown not to scale. (b) pMG8009 plasmid stability study in E. coli, by 1% agarose gel electrophoresis. DNA was isolated from eight independent E. coli colonies after passages P1 (lanes 1–8), P5 (lanes 9–16), and P10 (lanes 17–24). To obtain P1 plasmids, pMG8009 was transformed into E. coli Stbl3 cells and grown on LB agar plate containing 50 μg/ml kanamycin. Eight independent colonies from the plate were grown in 2 ml LB cultures and DNA was isolated in 50 μl of sterile water. 1 μl of plasmid was loaded on 1% TAE agarose gel. Then, DNA preparation #1 was transformed into E. coli again and DNA isolations and transformations were repeated for ten times (P2–P10) as described above. M, molecular weight ladder (Thermo). (c) Confirmation of intron removal from viral RNA of pMG8009-derived JEV. PCR was done using pMG8009 as template (lanes 1, 4, 7), viral RNA (lanes 2, 5, 8), and cDNA (lanes 3, 6, 9). PCR was conducted using primers in the vicinity of introns 1 (lanes 1–3), 2 (lanes 4–6) and 3 (lanes 4–8); M, molecular weight ladder.
2.3. Plasmid growth and stability in E.coli
The pMG8009 plasmid was isolated from E.coli strain Stbl3™, genotype F-mcrB mrrhsdS20(rB−, mB−) recA13 supE44 ara-14 galK2 lacY1 proA2 rpsL20(StrR) xyl-5 λ-leumtl-1 (Thermo). The plasmid was confirmed by DNA sequencing, quantitated, and stored at −20°C. To confirm genetic stability of the plasmid in E.coli, plasmid was transformed into E.coli strain Stbl3, eight random colonies were inoculated into 2 ml of LB (Thermo) containing 25 μg/ml of kanamycin. E. coli cultures were grown at 37°C for 16 h, DNA was isolated and all eight DNA isolates were confirmed by 1% agarose gel electrophoresis and restriction enzyme digest. To detect potential deletion variants, a broad-range 1Kb Plus DNA ladder spanning 0.1–12 kb was used (Thermo). One DNA isolate was transformed again into E. coli and the process was repeated for the total of ten rounds of transformations and DNA isolations.
2.4. Plasmid transfections in vitro
Vero cells were transfected by electroporation with pMG8009 or control plasmid DNA at concentrations ranging from 10 ng to 1 μg. Transfection was carried out essentially as described previously for plasmid encoding the full-length RNA viruses (Tretyakova et al., 2013; Tretyakova et al., 2014b). Replication of JEV and expression of JEV antigens in the transfected Vero cells were determined by the infectious center assay (ICA), indirect immunofluorescence assay (IFA) and western blot.
Infectious center assay (ICA) was done using Vero cells transfected with pMG8009 or infected with the virus. Vero cells after transfection or infection with 10 ng, 100 ng,or 1 μg of iDNA were diluted 30-fold in complete αMEM containing 10% FBS, 1 ml aliquot of cell suspension was allowed to adhere for 4 h in 6-well plates, supernatant was removed, and cell monolayers were covered with 1% agarose overlay containing complete αMEM. Plates were incubated at 37°C in 5% CO2 for 3 days to form plaques, which were visualized using staining with neutral red.
For IFA, 0.3 ml aliquots of pMG8009 DNA-transfected Vero cells were seeded in 8-well chamber slides in complete αMEM. At 48 h posttransfection, cells were rinsed with PBS, dried and fixed with cold acetone, then IFA was carried out using JEV (Nakayama strain) specific mouse antiserum VR-1259AF (ATCC), followed by the secondary fluorescein-labeled antibody to mouse IgG (H+L) (KPL, Gaithersburg, MD) as described previously (Pushko et al., 2001; Tretyakova et al., 2014b). Mounting medium containing propidium iodide counterstain (Vector Labs, Burlingame, CA) was used to visualize nuclei of the cells.
SDS-PAGE and western blot were used to detect JEV antigens in Vero cells transfected with iDNA. Transfected Vero cells were harvested on day 9 post-transfection, solubilized in the SDS-PAGE sample buffer containing 2-Mercaptoethanol, and proteins were separated by 4–12% SDS-PAGE. Proteins were transferred to nitrocellulose membranes and probed with VR-1259AF JEV-specific antiserum followed by alkaline phosphatase conjugated secondary antibody and stained using 1-component BCIP/NBT phosphatase substrate (KPL, Gaithersburg, MD).
2.5. Plaque assay and viral RNA isolation
The virus presence in the growth medium was confirmed by standard plaque assay in BHK cells. For virus growth curves, samples were taken for 9 days at 24 h time intervals. On day 9 day, the supernatant containing the virus was harvested, clarified by centrifugation at 3000 x g for 10 min, sterile filtered using 0.2 μm filter and frozen at −80°C. For plaque assay titers, average and standard deviation values were determined for each time point. Each experiment was conducted at least two times to ensure reproducibility.
Viral RNA was isolated from harvested JEV by using Trizol LS method (Thermo). The cDNA was prepared using RevertAid first strand cDNA synthesis kit (Thermo). PCR was carried out with JEV-specific primers adjacent to the introns and Q5 high-fidelity DNA polymerase (New England Biolabs, Ipswich, MA). The resulting PCR fragments were cloned into pCR-Blunt II-TOPO (Thermo) and sequenced.
2.6. Immunizations and serology
The iDNA plasmid was isolated from E.coli and formulated in phosphate-buffered saline (PBS) to a final concentration of 0.5 mg/ml. Animal studies were conducted in accordance with the regulations in the Guide for the Care and Use of Laboratory Animals under animal protocol approved by the Institutional Animal Care and Use Committee (IACUC) (Noble Life Sciences, Woodbine, MD). Four-week-old female BALB/c mice (5–10 mice/group) were anesthetized with isoflurane and vaccinated intramuscularly (i.m.) with a dose of 5 μg or 500 ng of pMG8009 iDNA vaccine in 20 μl into the tibialis anterior muscle. After injection of iDNA, animals were electroporated using BTX830 as described elsewhere (Tretyakova et al., 2013) or by using the TriGrid electroporation (Ichor Medical Systems, Inc., San Diego, CA) as previously described (Luxembourg et al., 2006). As a control, the plasmid expressing secreted embryonic alkaline phosphatase (SEAP) gene was injected-electroporated similarly. After vaccinations, animals were observed daily for clinical signs of infection. Sera were collected on days 3 and 4 for viremia detection, and at day 21 and 28 for antibody response evaluation. For viremia detection, sera were tested individually in direct plaque assay. Additionally, in order to amplify the virus in the serum, each serum was incubated with Vero cells for 10 days before harvesting. At the time of harvest, Vero cells were observed for cytopathic effects (CPE), while harvested media were tested by plaque assay.
To determine antibody responses, plaque reduction neutralization test (PRNT), western blot, and IFA were performed. For PRNT, an equal volume (0.1 ml) of virus suspension containing 500 PFU/ml and serial twofold dilutions of heat-inactivated serum were incubated 1 h at 37°C, and the serum-virus mixture was plated onto BHK cell monolayers in 12-well plates. An agarose overlay in complete αMEM was added and plates were incubated at 37°C for 3 days prior to neutral red staining and plaque count determination. The endpoint PRNT50 titers were expressed as the highest dilution of serum that reduces plaque count by 50% as compared to the wells without serum.
For determination of antibody response by IFA, Vero cell monolayers were initially infected with 102 PFU/well of JEV vaccine virus in chamber slides for 24 h in complete αMEM. Then, infected Vero cells were fixed with cold acetone and used as immobilized antigen essentially as described above. The JEV-infected Vero cell monolayers were probed with sera from vaccinated experimental mice to detect JEV-specific antibodies in the sera. As controls, pre-bleed sera, as well as sera from unvaccinated mice were used.
3. Results
3.1. Plasmid design and preparation of DNA-launched JEV vaccine
JEV pMG8009 iDNA plasmid vaccine was designed with the goal to transcribe the full-length genomic RNA of live-attenuated JEV vaccine in the eukaryotic cells. The genomic RNA of flaviviruses is infectious and is capable of launching replication of live virus (Tretyakova et al., 2014b; Yun et al., 2003). The synthetic JEV cDNA was assembled in the pUC57-Kan plasmid from chemically synthesized fragments based on the nucleotide sequence of JEV SA14-14-2 virus. The CMV major immediate-early promoter was inserted upstream from JEV cDNA. Because the authentic 5′ terminus of RNA is important for flavivirus replication (Khromykh et al., 2001), the distance between the CMV promoter and the 5′ of JEV cDNA has been optimized to ensure transcription of the functional 5′ terminus of the JEV genomic RNA. Ribozyme after 3′ untranslated region (UTR) was placed to ensure authentic JEV 3′ end (Fig.1a). As a result, the plasmid encoded the full-length, infectious genomic RNA of JEV strain SA14-14-2 live-attenuated vaccine virus operationally linked to the CMV promoter in the pUC57-Kan plasmid backbone (Fig. 1a). It has been reported previously that the full-length JEV and other flavivirus cDNA is unstable in E. coli due to potentially toxic translation products, and insertion of two introns into JEV capsid and E genes to disrupt potentially toxic open reading frames has improved genetic stability of JEV cDNA clone in the pBR322 plasmid (Yamshchikov et al., 2001). Therefore, we initially inserted two introns into JEV capsid and E genes. However, the resulting plasmid was unstable in E. coli in the context of high-copy, kanamycin resistant pUC57-Kan plasmid backbone. The pUC family of plasmids has mutations, which increase plasmid copy number to approximately 500 copies per cell (Wu and Liu, 2010), which potentially can amplify effects of toxic translation products. Several putative bacterial promoters within NS1 have been identified in silico, and an additional synthetic intron was introduced into the JEV NS1 gene. This resulted in the plasmid pMG8009 14.8 kb in length and containing the full-length cDNA with three introns in the capsid, E, and NS1 genes of JEV cDNA (Fig. 1a). Locations of the CMV promoter, intron and ribozyme sequences in the pMG8009 are summarized in Table 1.
Table 1.
Location of CMV promoter, introns and ribozyme in the pMG8009 JEV iDNA.
| Sequence Element | Length, nt | Location* | GenBank# |
|---|---|---|---|
| CMV Promoter/Enhancer | 380/204 | Upstream from 5′ JEV Cdna | X90639 |
| Intron 1 | 133 | Capsid (415–547) | U47119.2 |
| Intron 2 | 82 | Envelope (2347–2428) | U05272.1 |
| Intron 3 | 118 | NS1 (3350–3467) | NG_001019.6 |
| Rybozyme | 98 | Downstream from 3′ JEV cDNA | DQ322635.1 |
Locations of the sequence elements in relation to JEV cDNA are indicated including synthetic introns. Coordinates of the genes including introns are shown in parentheses. The GenBank accession numbers of the source sequence elements are also shown.
3.2 Characterization of pMG8009 in E.coli
The pMG8009 was evaluated in E. coli for growth and DNA yields. Plasmid was transformed into chemically competent E. coli Stbl3 cells to generate passage 1 (P1) progeny colonies and DNA yields were examined from eight random colonies (Fig. 1b, lanes 1–8). Plasmids migrated on 1% agarose gel at apparent size approximately 12 kb or higher as expected for supercoiled plasmids of 14.8 kb size. No plasmids with considerable deletions were detected (Fig. 1b). The observed minor variations in DNA yields and apparent size could be explained by small differences in the bacterial growth and DNA isolation. One DNA preparation was transformed into E. coli again and DNA isolations and transformations were repeated for five times to generate passage 5 (P5) progeny, followed by DNA isolations from eight independent E. coli colonies (Fig. 1b, lanes 9–16). Similarly, passage 10 (P10) colonies were examined for DNA yield and size (Fig. 1b, lanes 17–24). The pMG8009 plasmid yields and sizes were comparable between the DNA isolates in passages P1, P5 and P10 suggesting genetic uniformity and stability of pMG8009. The pMG8009 yields from E. coli were approximately 5–10 mg per 1 L of culture. The pMG8009 iDNA plasmid was isolated from E.coli Stbl3 cells resulting in a sterile, endotoxin-free DNA with 95% supercoiled fraction and an A260/A280 ratio of ~1.8.
3.3. Replication of JEV vaccine virus from iDNA in vitro
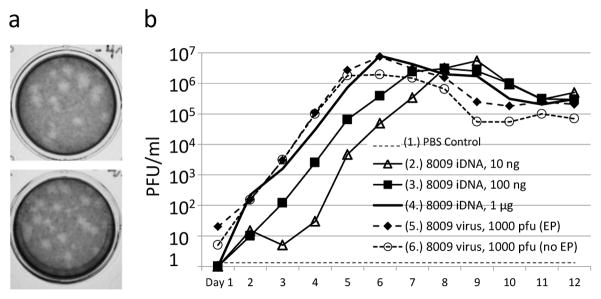
In order to test if transfection of pMG8009 iDNA can launch replication of live JEV vaccine virus in vitro, Vero cells were transfected with 10 ng, 100ng, and 1 μg of pMG8009 by electroporation. The transfected Vero cells were analyzed for expression of JEV vaccine virus by ICA, IFA, western blot, while medium from transfected cells was tested by direct plaque assay. For ICA, a suspension of electroporated Vero cells was seeded into 6-well plates and overlaid with 1% agarose in complete αMEM. At 72 h, plaques were detected, indicating presence of replicating virus in the infectious centers, IC (Fig. 2a). Specific infectivity of pMG8009 iDNA was calculated at ~103 to 105 IC per 1 μg of DNA depending on experimental conditions including quantity of DNA used in electroporation. Expression of JEV antigens in transfected cells was further examined by SDS-PAGE and western blot. The antigen bands were detected in iDNA-transfected Vero cells (Fig. 2b, lane 1). Western blot confirmed the presence of JEV antigens that were consistent with the predicted processing of prM, E and NS1 polypeptides. As expected, no bands were detected in the uninfected Vero cells (Fig. 2b, lane 2). Furthermore, expression of JEV antigens in transfected cells was confirmed at 24 h posttransfection by IFA using mouse anti-JEV antiserum (Fig. 2c). Foci of JEV positive cells were detected (Fig. 2c, panel 1), while no positive cells or foci were detected in the untransfected Vero control (Fig. 2c, panel 2). As expected for a flavivirus, expression of JEV antigen was found in the cytoplasm of pMG8009 iDNA-transfected cells (Fig. 2c, panels 1 and 3).
Fig. 2.
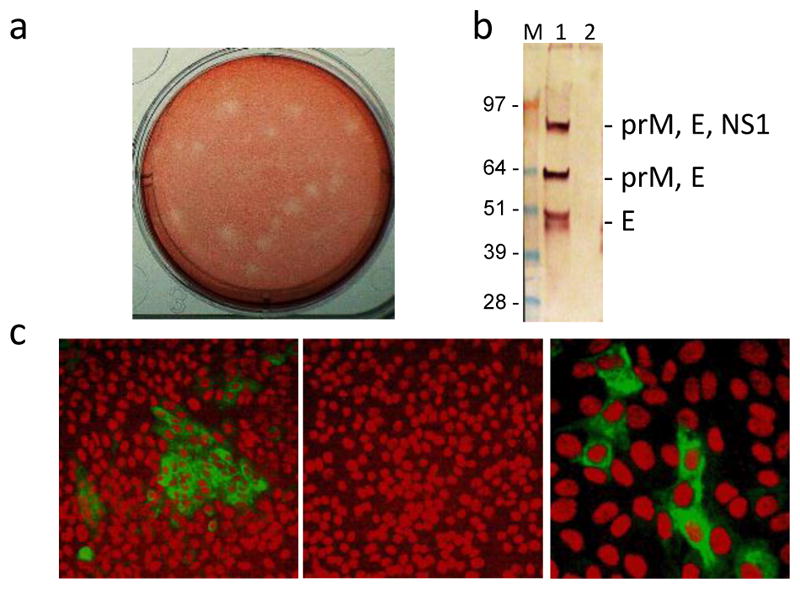
Expression of JEV virus in Vero cells transfected with pMG8009 iDNA plasmid. (a) JEV plaques by the infectious center assay (ICA) in Vero cells transfected by electroporation with 1 μg of pMG8009 iDNA plasmid. Representative ICA image shows ~26 ICs and corresponds to approximately 780 IC/μg of iDNA. (b) Western blot using mouse anti-JEV (ATCC VR-1259AF) antibody. Lane M shows SeeBlue Plus 2 protein molecular weight marker (Thermo). Lane 1 shows JEV antigens in pMG8009-transfected Vero cell. Lane 2, untransfected Vero cells. Location of predicted prM, E and NS1 translation products are indicated. (c) Indirect IFA using anti-JEV mouse ATCC VR-1259AF and fluorescein labeled anti-mouse IgG. Panels 1 and 2 show pMG8009-transfected Vero cells and untransfected Vero cells at 160x magnification), respectively. Panel 3 shows pMG8009-transfected Vero cells at 400x magnification. Nuclei of Vero cells are stained in red using propidium iodide counterstain.
The growth medium from JEV-infected or iDNA-transfected Vero cells was examined for the presence of replicating virus by plaque assay (Fig. 3). We evaluated the escalating quantities of pMG8009 iDNA for the ability to launch live JEV in vitro. Vero cells were transfected with pMG8009 plasmid with doses ranging from 10 ng to 1 μg. As positive control, Vero cells (either mock-electroporated or non-treated) were infected with 103 PFU of the iDNA-derived virus. Negative controls were mock-electroporated with PBS. As expected, no replicating virus was detected in the mock-electroporated, control Vero cells. Plaques were detected in the cells of Vero cells infected with 103 PFU of JEV (Fig 3a, upper panel) or transfected with various amounts (10–1000 ng) of iDNA plasmid or (Fig. 3a, lower panel; Fig. 3b). These experiments showed that iDNA plasmid was capable of launched replication of live vaccine virus and that insertion of introns did not affect the ability of pMG8009 to initiate synthesis of live JEV vaccine virus. To investigate if introns were removed by RNA splicing, viral RNA was isolated from the iDNA-launched virus, and the cDNA was prepared by using reverse transcription. Then, three PCR fragments encompassing three introns (Fig. 1a) were generated (Fig. 1c) and sequenced. The PCR fragments generated from viral cDNA were smaller in size (Fig. 1c, lanes 3, 6, 9) as compared to PCR fragments generated by using the same primers and pMG8009 plasmid as a template (Fig. 1c, lanes 1, 4, 7), which was consistent with removal of introns by RNA splicing as confirmed by cDNA sequencing. As expected, no PCR fragments were generated by using isolated viral RNA as a template (Fig. 1c, lanes 2, 5, 8).
Fig. 3.
Detection of JEV virus in the medium from Vero cells transfected with pMG8009 iDNA plasmid. (a) Plaque assay in BHK cells. Upper panel, plaque assay of growth medium from virus-infected Vero cells (no electroporation), sample taken on day 7 post-infection with 1000 PFU (sample #6 on Fig. 3b). Lower panel, plaque assay of growth medium from pMG8009-transfected Vero cells (after electroporation), sample taken on day 7 post-transfection with 10 ng of DNA (sample #2 on Fig. 3b). (b) Growth curves of JEV virus in the medium of Vero cells transfected with pMG8009 iDNA (samples 2, 3, 4) or infected with pMG8009-derived virus (samples 5 and 6). Samples 5 and 6 show infection with 103 PFU of pMG8009-derived vaccine virus of electroporated and non-electroporated Vero cells, respectively.
Growth curves of viruses from the transfected/infected cells are shown on Fig. 3b. The peak virus titers were comparable at all DNA doses tested. In the culture media from cells transfected with 1 μg of pMG8009, the peak titers reached 106–107 PFU/ml on day 6 post-transfection, similar to the cells infected with 1000 PFU of JEV. This experiment suggests the equivalency of 1 μg of DNA to 1000 PFU of virus in terms of virus replication kinetics by using described experimental conditions. However, the DNA dose dependence was detectable as a delayed onset of replication when 10 ng or 100 ng of DNA was used. We observed approximately 48–72 h delay for peak titers when Vero cells were transfected with 10 ng or 100 ng of pMG8009. As shown on Fig. 3b, transfection of only 10 ng of DNA resulted in the replication of JEV virus, with peak virus titers reaching approximately 106 – 107 PFU/ml on day 9, with peak titer similar to that from transfections with higher quantities of DNA (Fig. 3b).
These results suggest that the minimal dose of iDNA to launch JEV vaccine virus in Vero cells is below 10 ng (Fig. 3b), which is consistent with our previous findings with iDNA plasmids encoding YF flavivirus (Tretyakova et al., 2014b) and VEEV and CHIKV alphaviruses (Tretyakova et al., 2014a; Tretyakova et al., 2013).
3.4. Immunogenicity of pMG8009 JEV iDNA vaccine in BALB/c mice
To determine if pMG8009 iDNA plasmid can be used for vaccination in vivo, BALB/c mice were vaccinated by injection-electroporation with pMG8009 plasmid. Current JEV vaccines are based on induction of neutralizing antibodies, and a neutralization titer of 1:10 is considered protective (Plotkin, 2010). Therefore, we focused on detecting serum antibody response including neutralizing antibodies. Mice were vaccinated with a single i.m. injection of either 500 ng or 5 μg of iDNA followed by electroporation. As a control, mice were vaccinated using unrelated DNA expressing SEAP reporter gene. After vaccinations, all mice remained healthy with no detectable pathology at the site of injection or adverse effects due to vaccinations. No viremia was detected on days 3 and 4 in the vaccinated mice by direct plaque assay. Virus in the serum was also undetectable by incubating each serum with Vero cells for 10 days followed by CPE analysis and plaque assays in an attempt to amplify virus in the serum (Table 2). This result indicates no significant presence of replicating vaccine virus on days 3 and 4 after iDNA injection. In order to detect serum antibodies in vaccinated mice, we used IFA and PRNT methods. For IFA, Vero cells were initially infected with 100 PFU per well of JEV vaccine virus in chamber slides, fixed, and then probed with immunized mouse sera at 1:10 dilution (Fig. 4). By IFA, all experimental mice vaccinated with 5 μg of pMG8009 have seroconverted as shown on Fig. 4 and Table 1. Seroconversion was also detected by IFA in all mice vaccinated with 500 ng of pMG8009 (Table 2). Finally, neutralizing antibodies were detected by PRNT in the serum of pMG8009 vaccinated mice (Table 2). In the 5 μg vaccination group, most mice had PRNT50 titer of 10, which is similar to a protective titer against JEV as described previously (Plotkin, 2010), while one mouse had the titer 40 and one mouse had undetectable titer. In the 500 ng vaccination group, all mice had PRNT50 titers in the range from 10 to 40, which were comparable to the titers from mice vaccinated with 5 μg of pMG8009. These pilot data warrant further studies of using iDNA vaccination to protect against JEV infections.
Table 2.
Viremia and serum antibodies in mice vaccinated with pMG8009 iDNA vaccine.
| Dose | Viremia, PFU/ml* | Serum Antibody** | ||
|---|---|---|---|---|
|
| ||||
| Plaque assay | Amplification | IFA | PRNT50 | |
| 500 ng | <50 (0%) | <50 (0%) | + (100%) | 1:10 (40%) |
| 1:20 (40%) | ||||
| 1:40 (20%) | ||||
| 5 μg | <50 (0%) | <50 (0%) | + (100%) | <1:10 (20%) |
| 1:10 (60%) | ||||
| 1:40 (20%) | ||||
For viremia, serum was taken on days 3 and 4. Percentage of viremic mice is shown in parentheses. Tests for viremia included direct plaque assay and by amplification in Vero cells followed by plaque assay and CPE observation.
For antibody, serum was taken on days 21 and 28. In IFA, “+” indicates positive reaction. In PRNT50, dilution of serum that produced 50% reduction of plaques is indicated. Percentage of seropositive mice is shown in parentheses.
Fig. 4.
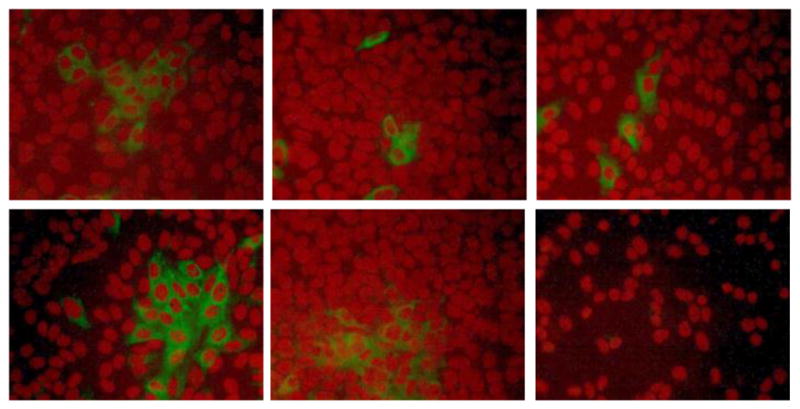
Immunogenicity of pMG8009 JEV vaccine in BALB/c mice, by IFA. Mice were vaccinated on day 0 with 5 μg pf pMG8009 plasmid intramuscularly using electroporation. To detect antibodies mice were bled on day 21. Serum from vaccinated mice was used to probe JEV-infected Vero cells in IFA in chamber slides at 1:10 dilution. After incubation with mouse sera, Vero cells were treated with fluorescein-labeled antibodies to mouse IgG (H+L) to visualize cells expressing JEV antigens in green. Slides were covered with mounting medium containing propidium iodide nuclear counterstain and observed under microscope using 160x magnification. Nuclei of Vero cells are stained in red.
4. Discussion
JEV is a zoonotic disease transmitted to humans by mosquitoes. The virus also grows and can be amplified in pigs (Mansfield et al., 2017). Endemic JEV transmission has been reported in humans in 24 countries in the South-East Asia and Western Pacific, exposing more than 3 billion people to risks of JEV infection (WHO, 2015). There is no specific treatment for the disease and current therapeutic approaches are focused on support for the patient to overcome the infection. However, prophylactic vaccines are manufactured in several countries. There are 4 main types of JEV vaccines including inactivated mouse brain-derived vaccines, inactivated Vero cell-derived vaccines, live-attenuated vaccines, and live recombinant vaccines (WHO, 2015). Over the past years, the live-attenuated SA14-14-2 vaccine manufactured in China has become the most widely used vaccine in endemic countries. Cell-culture based inactivated vaccines and the live recombinant vaccine based on the yellow fever vaccine strain have also been approved and WHO-prequalified. In the U.S., vaccination is recommended for travelers who plan to spend a month or more in endemic areas during JEV transmission season. Inactivated Vero cell culture-derived IXIARO vaccine is the only vaccine approved in the U.S., based on the inactivated SA14-14-2 virus strain (CDC, 2016; Firbas and Jilma, 2015), which is given as two doses spaced 28 days apart. Veterinary vaccination against JEV has also been conducted, with live-attenuated and inactivated vaccines available for swine (Lutticken et al., 2007).
Here we configured recent iDNA® technology of DNA-launched live-attenuated vaccines to prepare novel experimental DNA-based vaccine for JEV. In the pMG8009, the full-length synthetic cDNA of SA-14-14-2 JEV vaccine strain was introduced downstream from the CMV promoter, which resulted in the transcription of the infectious genomic viral RNA and launching the vaccine virus in eukaryotic cells. The advantages of DNA-launched iDNA vaccines include the genetic and physical stability, ease of production, and high purity of the DNA vaccines, as well as high efficacy of live-attenuated vaccines (Pushko et al., 2016). Traditional cell substrates used for vaccine production are often contaminated with latent viruses that can be identified by next generation (NGS) sequencing and other methods (Onions et al., 2011). In contrast, endotoxin-free DNA can be isolated from E. coli without latent viruses or impurities associated with cell culture production. However, preparation of the plasmids encoding the full-length flavivirus cDNA has been notoriously difficult due to the toxicity and instability in E. coli (Rice et al., 1989; Sumiyoshi et al., 1992; Tretyakova et al., 2014b; Tsetsarkin et al., 2016; Yamshchikov et al., 2001). The challenge of preparing the full-length JEV cDNA clone in the high copy E.coli plasmid was addressed in the current study by insertion of three distinct synthetic intron sequences in the structural and nonstructural JEV genes. In the previous study, two introns have been inserted into the JEV structural genes, which facilitated preparation of the full-length clone (Yamshchikov et al., 2001). We found that inclusion of the third intron in the nonstructural NS1 gene in addition to two introns in the structural genes considerably improved infectious clone preparation in the pUC backbone with kanamycin antibiotic resistance. Furthermore, in the proof-of-concept study in vivo, we demonstrated that a single dose of 500 ng or 5 μg of pMG8009 plasmid induced immune response to JEV in BALB/c mice including JEV neutralizing antibodies. The comparable virus neutralization titers in the sera of mice vaccinated with either 500 ng or 5 μg of iDNA suggest the possibility of further iDNA vaccine dose reduction. We hypothesize that live-attenuated virus is launched in vivo similarly to our observations in vitro, in which transfection of Vero cells with escalating amounts of DNA reached comparable virus titers (Fig. 3b). However, we were unable to detect live vaccine virus in mice in our viremia experiments. One explanation could be relatively low viremia levels, which can represent a safety advantage for a vaccine designed to launch expression of live virus. Another explanation is that viremia may have not reached detectable levels in the serum samples on day 3 and 4. Additional studies are needed including confirmation of vaccine virus launch in vivo, improvement of immunogenicity, determination of the minimal immunogenic dose of iDNA, as well as evaluation of the protective efficacy of DNA-launched pMG8009 JEV vaccine against pathogenic JEV challenge. Previously, DNA-launched experimental vaccines were also prepared for yellow fever virus, another member of the flavivirus family (Jiang et al., 2015; Tretyakova et al., 2014b), West Nile flavivirus (Hall et al., 2003; Yamshchikov, 2015; Yamshchikov et al., 2015), as well as vaccines for alphaviruses (Tretyakova et al., 2014a; Tretyakova et al., 2013). We have also shown by the NGS that iDNA-derived vaccine strain of Chikungunya virus (CHIKV) has higher homogeneity as compared to the traditional, cell culture-derived CHIKV virus (Hidajat et al., 2016). Similarly, JEV vaccine launched from iDNA is expected to represent a more homogenous population of viruses, which may represent a safety advantage in comparison with classic SA-14-14-2 virus. In conclusion, JEV iDNA vaccine shows successful application of synthetic biology methods (Wimmer et al., 2009) for converting classic live-attenuated vaccines into a DNA vaccine format with potential safety advantages. In addition, JEV infectious clone can serve as a reverse genetics system for JEV, as well as a vector platform to prepare chimeric JEV-based vaccines for other viruses including flaviviruses such as Zika, Dengue and West Nile viruses as was previously shown for chimeric yellow fever-based vaccines (Guy et al., 2010). Thus, with iDNA technology, DNA vaccine platform can be configured not only for expression of subunit vaccines but also for expression of live vaccines (Pushko et al., 2016). Taken together, the results of the current pilot study warrant further studies of DNA-launched live-attenuated vaccine approach for the development of safe and effective vaccines for JEV and potentially, other flaviviruses.
Highlights.
Novel iDNA plasmid was developed to improve vaccination against JEV flavivirus
The iDNA platform combines advantages of DNA immunization and live attenuated vaccine
Only 10 ng of JEV iDNA plasmid initiated replication of live JEV vaccine virus in vitro
BALB/c mice vaccinated with a single dose of JEV iDNA plasmid have seroconverted
Virus-specific neutralizing response was elicited in vaccinated mice
Acknowledgments
We thank Igor Lukashevich (University of Louisville), Drew Hannaman, Marcos Valenzuela and May Pidding (Ichor Medical Systems) for reading the manuscript and discussions. Research reported in this publication was supported in part by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number R44AI094863. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bharati K, Appaiahgari MB, Vrati S. Effect of cytokine-encoding plasmid delivery on immune response to Japanese encephalitis virus DNA vaccine in mice. Microbiol Immunol. 2005;49:349–353. doi: 10.1111/j.1348-0421.2005.tb03739.x. [DOI] [PubMed] [Google Scholar]
- CDC. Japanese Encephalitis Vaccine. 2016. [Google Scholar]
- Chen HL, Chang JK, Tang RB. Current recommendations for the Japanese encephalitis vaccine. J Chin Med Assoc. 2015;78:271–275. doi: 10.1016/j.jcma.2014.12.009. [DOI] [PubMed] [Google Scholar]
- Firbas C, Jilma B. Product review on the JE vaccine IXIARO. Hum Vaccin Immunother. 2015;11:411–420. doi: 10.4161/21645515.2014.983412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy B, Guirakhoo F, Barban V, Higgs S, Monath TP, Lang J. Preclinical and clinical development of YFV 17D-based chimeric vaccines against dengue, West Nile and Japanese encephalitis viruses. Vaccine. 2010;28:632–649. doi: 10.1016/j.vaccine.2009.09.098. [DOI] [PubMed] [Google Scholar]
- Hall RA, Nisbet DJ, Pham KB, Pyke AT, Smith GA, Khromykh AA. DNA vaccine coding for the full-length infectious Kunjin virus RNA protects mice against the New York strain of West Nile virus. Proc Natl Acad Sci U S A. 2003;100:10460–10464. doi: 10.1073/pnas.1834270100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halstead SB, Thomas SJ. New Japanese encephalitis vaccines: alternatives to production in mouse brain. Expert Rev Vaccines. 2011;10:355–364. doi: 10.1586/erv.11.7. [DOI] [PubMed] [Google Scholar]
- Heffelfinger JD, Li X, Batmunkh N, Grabovac V, Diorditsa S, Liyanage JB, Pattamadilok S, Bahl S, Vannice KS, Hyde TB, Chu SY, Fox KK, Hills SL, Marfin AA. Japanese Encephalitis Surveillance and Immunization - Asia and Western Pacific Regions, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:579–583. doi: 10.15585/mmwr.mm6622a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hidajat R, Nickols B, Forrester N, Tretyakova I, Weaver S, Pushko P. Next generation sequencing of DNA-launched Chikungunya vaccine virus. Virology. 2016;490:83–90. doi: 10.1016/j.virol.2016.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang X, Dalebout TJ, Lukashevich IS, Bredenbeek PJ, Franco D. Molecular and immunological characterization of a DNA-launched yellow fever virus 17D infectious clone. J Gen Virol. 2015;96:804–814. doi: 10.1099/jgv.0.000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur R, Sachdeva G, Vrati S. Plasmid DNA immunization against Japanese encephalitis virus: immunogenicity of membrane-anchored and secretory envelope protein. J Infect Dis. 2002;185:1–12. doi: 10.1086/338015. [DOI] [PubMed] [Google Scholar]
- Khromykh AA, Meka H, Guyatt KJ, Westaway EG. Essential role of cyclization sequences in flavivirus RNA replication. J Virol. 2001;75:6719–6728. doi: 10.1128/JVI.75.14.6719-6728.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konishi E, Ajiro N, Nukuzuma C, Mason PW, Kurane I. Comparison of protective efficacies of plasmid DNAs encoding Japanese encephalitis virus proteins that induce neutralizing antibody or cytotoxic T lymphocytes in mice. Vaccine. 2003;21:3675–3683. doi: 10.1016/s0264-410x(03)00382-7. [DOI] [PubMed] [Google Scholar]
- Konishi E, Yamaoka M, Khin Sane W, Kurane I, Takada K, Mason PW. The anamnestic neutralizing antibody response is critical for protection of mice from challenge following vaccination with a plasmid encoding the Japanese encephalitis virus premembrane and envelope genes. J Virol. 1999;73:5527–5534. doi: 10.1128/jvi.73.7.5527-5534.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Gao N, Fan D, Chen H, Sheng Z, Fu S, Liang G, An J. Cross-protection induced by Japanese encephalitis vaccines against different genotypes of Dengue viruses in mice. Sci Rep. 2016;6:19953. doi: 10.1038/srep19953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutticken D, Segers RP, Visser N. Veterinary vaccines for public health and prevention of viral and bacterial zoonotic diseases. Rev Sci Tech. 2007;26:165–177. [PubMed] [Google Scholar]
- Luxembourg A, Hannaman D, Ellefsen B, Nakamura G, Bernard R. Enhancement of immune responses to an HBV DNA vaccine by electroporation. Vaccine. 2006;24:4490–4493. doi: 10.1016/j.vaccine.2005.08.014. [DOI] [PubMed] [Google Scholar]
- Mansfield KL, Hernandez-Triana LM, Banyard AC, Fooks AR, Johnson N. Japanese encephalitis virus infection, diagnosis and control in domestic animals. Vet Microbiol. 2017;201:85–92. doi: 10.1016/j.vetmic.2017.01.014. [DOI] [PubMed] [Google Scholar]
- Mishin VP, Cominelli F, Yamshchikov VF. A ‘minimal’ approach in design of flavivirus infectious DNA. Virus Res. 2001;81:113–123. doi: 10.1016/S0168-1702(01)00371-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onions D, Cote C, Love B, Toms B, Koduri S, Armstrong A, Chang A, Kolman J. Ensuring the safety of vaccine cell substrates by massively parallel sequencing of the transcriptome. Vaccine. 2011;29:7117–7121. doi: 10.1016/j.vaccine.2011.05.071. [DOI] [PubMed] [Google Scholar]
- Plotkin SA. Correlates of protection induced by vaccination. Clin Vaccine Immunol. 2010;17:1055–1065. doi: 10.1128/CVI.00131-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pushko P, Bredenbeek PP, Lukashevich IS. Experimental DNA-launched live-attenuated vaccines against infections caused by Flavi-and alphaviruses. In: Lukashevich IS, Shirwan H, editors. Novel Technologies for Vaccine Development. Springer; Vienna: 2014. pp. 153–177. [Google Scholar]
- Pushko P, Geisbert J, Parker M, Jahrling P, Smith J. Individual and bivalent vaccines based on alphavirus replicons protect guinea pigs against infection with Lassa and Ebola viruses. J Virol. 2001;75:11677–11685. doi: 10.1128/JVI.75.23.11677-11685.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pushko P, Lukashevich IS, Weaver SC, Tretyakova I. DNA-launched live-attenuated vaccines for biodefense applications. Expert Rev Vaccines. 2016;15:1223–1234. doi: 10.1080/14760584.2016.1175943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnak R, Porter K, Schmaljohn C. DNA vaccines for flaviviruses. Adv Virus Res. 2003;61:445–468. doi: 10.1016/s0065-3527(03)61012-2. [DOI] [PubMed] [Google Scholar]
- Rice CM, Grakoui A, Galler R, Chambers TJ. Transcription of infectious yellow fever RNA from full-length cDNA templates produced by in vitro ligation. New Biol. 1989;1:285–296. [PubMed] [Google Scholar]
- Saito Y, Moi ML, Takeshita N, Lim CK, Shiba H, Hosono K, Saijo M, Kurane I, Takasaki T. Japanese encephalitis vaccine-facilitated dengue virus infection-enhancement antibody in adults. BMC Infect Dis. 2016;16:578. doi: 10.1186/s12879-016-1873-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheng Z, Gao N, Cui X, Fan D, Chen H, Wu N, Wei J, An J. Electroporation enhances protective immune response of a DNA vaccine against Japanese encephalitis in mice and pigs. Vaccine. 2016;34:5751–5757. doi: 10.1016/j.vaccine.2016.10.001. [DOI] [PubMed] [Google Scholar]
- Sumiyoshi H, Hoke CH, Trent DW. Infectious Japanese encephalitis virus RNA can be synthesized from in vitro-ligated cDNA templates. J Virol. 1992;66:5425–5431. doi: 10.1128/jvi.66.9.5425-5431.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tretyakova I, Hearn J, Wang E, Weaver S, Pushko P. DNA vaccine initiates replication of live attenuated chikungunya virus in vitro and elicits protective immune response in mice. J Infect Dis. 2014a;209:1882–1890. doi: 10.1093/infdis/jiu114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tretyakova I, Lukashevich IS, Glass P, Wang E, Weaver S, Pushko P. Novel vaccine against Venezuelan equine encephalitis combines advantages of DNA immunization and a live attenuated vaccine. Vaccine. 2013;31:1019–1025. doi: 10.1016/j.vaccine.2012.12.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tretyakova I, Nickols B, Hidajat R, Jokinen J, Lukashevich IS, Pushko P. Plasmid DNA initiates replication of yellow fever vaccine in vitro and elicits virus-specific immune response in mice. Virology. 2014b;468–470:28–35. doi: 10.1016/j.virol.2014.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsetsarkin KA, Kenney H, Chen R, Liu G, Manukyan H, Whitehead SS, Laassri M, Chumakov K, Pletnev AG. A Full-Length Infectious cDNA Clone of Zika Virus from the 2015 Epidemic in Brazil as a Genetic Platform for Studies of Virus-Host Interactions and Vaccine Development. MBio. 2016:7. doi: 10.1128/mBio.01114-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang SY, Cheng XH, Li JX, Li XY, Zhu FC, Liu P. Comparing the immunogenicity and safety of 3 Japanese encephalitis vaccines in Asia-Pacific area: A systematic review and meta-analysis. Hum Vaccin Immunother. 2015;11:1418–1425. doi: 10.1080/21645515.2015.1011996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Japanese encephalitis. 2015 Fact sheet No 386. [Google Scholar]
- Wimmer E, Mueller S, Tumpey TM, Taubenberger JK. Synthetic viruses: a new opportunity to understand and prevent viral disease. Nat Biotechnol. 2009;27:1163–1172. doi: 10.1038/nbt.1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu CJ, Li TL, Huang HW, Tao MH, Chan YL. Development of an effective Japanese encephalitis virus-specific DNA vaccine. Microbes Infect. 2006;8:2578–2586. doi: 10.1016/j.micinf.2006.06.010. [DOI] [PubMed] [Google Scholar]
- Wu YC, Liu ST. A sequence that affects the copy number and stability of pSW200 and ColE1. J Bacteriol. 2010;192:3654–3660. doi: 10.1128/JB.00095-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamshchikov V. Development of a human live attenuated West Nile infectious DNA vaccine: conceptual design of the vaccine candidate. Virology. 2015;484:59–68. doi: 10.1016/j.virol.2015.04.027. [DOI] [PubMed] [Google Scholar]
- Yamshchikov V, Manuvakhova M, Rodriguez E. Development of a human live attenuated West Nile infectious DNA vaccine: Suitability of attenuating mutations found in SA14-14-2 for WN vaccine design. Virology. 2015;487:198–206. doi: 10.1016/j.virol.2015.10.015. [DOI] [PubMed] [Google Scholar]
- Yamshchikov V, Mishin V, Cominelli F. A new strategy in design of +RNA virus infectious clones enabling their stable propagation in E. coli. Virology. 2001;281:272–280. doi: 10.1006/viro.2000.0793. [DOI] [PubMed] [Google Scholar]
- Yu Y. Phenotypic and genotypic characteristics of Japanese encephalitis attenuated live vaccine virus SA14-14-2 and their stabilities. Vaccine. 2010;28:3635–3641. doi: 10.1016/j.vaccine.2010.02.105. [DOI] [PubMed] [Google Scholar]
- Yun SI, Kim SY, Rice CM, Lee YM. Development and application of a reverse genetics system for Japanese encephalitis virus. J Virol. 2003;77:6450–6465. doi: 10.1128/JVI.77.11.6450-6465.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Y, Zhou Y, Li X, Feng G. Immune-enhancing effect of nano-DNA vaccine encoding a gene of the prME protein of Japanese encephalitis virus and BALB/c mouse granulocyte-macrophage colony-stimulating factor. Mol Med Rep. 2015;12:199–209. doi: 10.3892/mmr.2015.3419. [DOI] [PMC free article] [PubMed] [Google Scholar]