Abstract
Introduction
Childhood maltreatment is associated with later obesity, but the underlying mechanisms are unknown. The objective of this study was to estimate the extent to which depression mediates the associations between childhood maltreatment and BMI in adolescence through adulthood.
Methods
Data on a cohort of 13,362 adolescents in the National Longitudinal Study of Adolescent to Adult Health (Wave I [1994–1995] to Wave IV [2008–2009]) were analyzed in 2015–2016. Classes of maltreatment experienced prior to age 12 years were statistically identified using latent class analysis. Gender-stratified latent growth curve analysis was used to estimate total effects of maltreatment classes on latent BMI trajectory (aged 13–31 years) and indirect effects of maltreatment classes that occurred through latent depression trajectory (aged 12 – 31 years).
Results
Four latent maltreatment classes were identified: high abuse and neglect; physical abuse dominant; supervisory neglect dominant; and no/low maltreatment. In girls, compared with no/low maltreatment, supervisory neglect dominant (coefficient=0.3, 95% CI=0.0, 0.7) and physical abuse dominant (coefficient=0.6, 95% CI=0.1, 1.2) maltreatment were associated with faster gain in BMI. Change in depression over time fully mediated the association of BMI slope with physical abuse dominant maltreatment, but not with supervisory neglect dominant maltreatment. In boys, high abuse and neglect maltreatment was associated with marginally greater BMI at baseline (coefficient=0.7, 95% CI= −0.1, 1.5); this association was not mediated by depression.
Conclusions
Although maltreatment was associated with depression and BMI trajectories from adolescence to adulthood, depression only mediated associations with physical abuse dominant maltreatment in girls.
INTRODUCTION
Approximately 30% of the U.S. population experiences maltreatment during childhood.1,2 Childhood maltreatment is associated with faster gain in BMI from adolescence to adulthood3 and with elevated risk of incident visceral obesity,4 severe obesity,5,6 and cardiovascular disease.7 The pathways through which maltreatment during childhood may promote excessive weight gain are largely unexplored, but may include depression, as recently highlighted.8 Childhood maltreatment is associated with higher risk of early onset depressive symptoms,9 depression, and suicidality.10–14 In turn, in some types of depression, elevated appetite and psychomotor retardation15,16 can promote weight gain. However, the mediating role of depression has not been tested.
Furthermore, childhood maltreatment can take many forms, ranging from supervisory or emotional neglect to physical or sexual abuse. Depression may play a stronger role for maltreatment types that induce cognitive precursors to depression such as shame and guilt. For example, sexual abuse is predictive of adult obesity, theoretically by triggering overeating behaviors and altering neural systems,17 which are also linked to depression. Other types of childhood maltreatment are less studied, but may involve different behavioral pathways such as substance use or risky behaviors.18,19
This study addressed three corresponding gaps in understanding of pathways leading from childhood maltreatment to obesity. First, defining subtypes of maltreatment is critical for studying distinct pathways, but is complicated by the co-occurrence of multiple maltreatment types which may interact in their effects on mental and physical health.20 Second, boys and girls may respond differently to maltreatment; for example, to cope with stress, girls more often engage in emotional eating or binge eating, whereas boys are more likely to exhibit aggressive behavior.21,22 Third, different maltreatment pathways may incur health effects at different life stages. For example, disordered eating may impact early weight gain whereas depression may have delayed impacts on weight gain emerging in adolescence or adulthood.
Study objectives are to test the hypotheses that more severe types of maltreatment, such as sexual abuse, are (1) more strongly associated with depression and BMI trajectory and (2) more strongly mediated by depression earlier in adolescence, and that (3) these pathways are stronger in girls than boys. Latent class analysis (LCA) is used to account for comorbidity between maltreatment types. Gender-stratified latent growth curve (LGC) analysis is used to examine how depression trajectories contribute to associations between childhood maltreatment and BMI trajectories from adolescence to adulthood. LGCs model age-related differences within the critical periods of adolescence and young adulthood using an accelerated cohort design.23
METHODS
Study Population
Data were obtained from the National Longitudinal Study of Adolescent to Adult Health (Add Health).24 Initially a school-based study, the sample is representative of adolescents attending U.S. public, private, and parochial schools in grades seven to twelve in the 1994–1995 school year, with over-sampled groups (e.g., non-Hispanic blacks with a college-educated parent). The Wave I in-home participant and parental interview was conducted in 1994–1995 (aged 11–21 years, N=20,745; Appendix Figure 1). All participants were eligible for Wave II (1995–1996), excluding those who graduated in 1995 (N=14,738). All located Wave I respondents were eligible for Waves III (2001–2002, N=15,197) and IV (2008–2009, N=15,701).
Of the 18,923 participants in the probability sample, the following exclusions were applied in sequence: <2 non-pregnant BMI measurements (n=4,318 excluded), missing maltreatment data (n=59), Asian or other race (n=1,175), and age 11 years at Wave I (n=9). Inclusion of Asian or other race led to difficulties with model convergence, likely because of the small number and heterogeneity of participants in these categories. The age 11 years cohort was too small to be included in the accelerated cohort analysis. The analytic sample included 13,362 participants. Data were analyzed in 2015–2016. This study was determined exempt by the Oregon Health & Science University IRB.
Measures
Height and weight were measured by trained, non-medical field interviewers according to standard protocol in Waves II, III, and IV.25 BMI was calculated for each wave (kg/m2) and analyzed as a continuous variable.
Dichotomous experience of five types of childhood maltreatment was ascertained from data collected in Waves III and IV (Appendix Table 1). Participants reported the number of times (1, 2–3, 4–5, >5) they experienced physical abuse and sexual abuse (Wave III, IV), supervisory neglect and physical neglect (Wave III), and emotional neglect (Wave IV). In Wave III, the time frame was prior to beginning sixth grade; in Wave IV, maltreatment that occurred prior to age 12 years was based on the earliest age at which each type of maltreatment occurred. Physical abuse and sexual abuse (reported in both waves) were defined as reporting that maltreatment type in one or both waves. Detail about the validity, concordance, and selection of the maltreatment measures is described in Appendix A.
Depression was ascertained at each wave using a modified version of the validated Center for Epidemiological Studies Depression Inventory,26–28 which included nine statements about how the participant had felt over the previous 30 days (0 [never] to 3 [nearly every day]; Appendix Table 2). Summed depression scores for each wave (range, 0 to 27) were analyzed as continuous variables.
Characteristics related to experiencing childhood maltreatment, depression, or higher BMI were included as control variables. Time-invariant covariates included participant race (non-Hispanic white, non-Hispanic black, non-Hispanic Asian, or Hispanic), highest parental education level (less than high school [HS] graduate, HS graduate, some college or technical school, college graduate), and household income, were all reported in Wave I. Time-varying covariates included smoking in Waves II, III, and IV (yes/no), participant income in Waves III and IV, and the participant’s educational attainment in Wave IV (less than HS degree, HS graduate, some college or technical school, college graduate).
Statistical Analysis
Data management and descriptive analyses were conducted using Stata, version 13. LCA and LGC analyses were performed in Mplus, version 7.2. Mplus accounts for missing data within the analytic sample of 13,362 using full information maximum likelihood estimation. AddHealth sample weights adjusted for non-participation in Waves II, III, or IV.24 All analyses were adjusted for complex survey design using the Stata survey function or the Mplus complex analysis command.
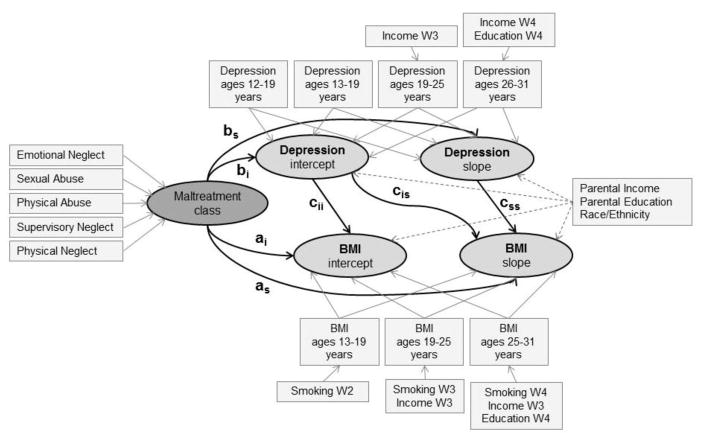
In step one, LCA was used to identify latent maltreatment classes that underlie reported dichotomous experience of five types of childhood maltreatment (supervisory neglect, physical neglect, physical abuse, sexual abuse, emotional neglect; Figure 1). LCA statistically identifies classes of maltreatment comorbidity while avoiding the statistical challenges present in traditional regression techniques due to high collinearity between maltreatment types.29–31
Figure 1.
Structural equation model of pathway from latent childhood maltreatment classes, latent depression trajectory, and BMI trajectory, with covariates.
Notes: Data from National Longitudinal Study of Adolescent Health.
W2, W3, W4: Wave 2, Wave 3, Wave 4
a, b, and c indicate coefficients for the corresponding pathway
Models with three, four, and five class solutions were fit using maximum likelihood estimation with robust SEs to account for non-normality and non-independence of observations in complex survey weighted data. The final model was selected on the basis of model fit (Bayesian Information Criterion and entropy) and interpretability of the classes. Participants were assigned to the maltreatment class for which they had the highest probability of membership.32
In step two, LGC modeling was used to examine trajectories of (1) BMI and (2) depression from adolescence to adulthood (Figure 1). Models were stratified by gender because of evidence suggesting gender differences in the relationship between maltreatment and BMI21,22; and because associations between maltreatment and depression trajectory differed significantly between males and females. Appendix B provides details about the LGC analysis, including multiple groups analysis and the accelerated cohort design.
Examination of latent trajectories across study wave, each containing a broad age range (12–19 years at Wave I), can mask age-related differences within the critical periods of adolescence and young adulthood. Therefore, this study used an accelerated cohort design to examine BMI and depression with increasing age; each age group is treated as one of eight age cohorts (aged 12 years cohort, aged 13 years cohort, etc.).
First, for each gender, three separate models of the direct relationships between (1) maltreatment (referent: no/low maltreatment) and BMI trajectory (aged 13–31 years), (2) maltreatment and depression trajectory (aged 12–31 years), and (3) depression trajectory and BMI trajectory were fit (Figure 1). For each relationship, crude and adjusted associations were determined. Linear BMI and depression trajectories are defined by their latent intercept (i, baseline) and slope (s, change over time).
Second, individual models were combined into gender-stratified mediation models.33 Models controlled for exposure-mediator and mediator-outcome confounding by including time-constant characteristics as predictors of depression (mediator) and BMI (outcome) trajectories and time-varying predictors of depression and BMI at specific time points (Figure 1). Direct effects for each relationship were obtained from the adjusted mediation model. Indirect effects were calculated as the product of the coefficients from the exposure–mediator and mediator–outcome relationships.34 CIs for the indirect effects were estimated using a Monte Carlo approach.35
RESULTS
Participants were, on average, approximately aged 15 years at Wave I (Appendix Table 3). Girls and boys had similar demographic characteristics, though boys tended to earn more income and girls tended to have higher education by Wave IV. Girls and boys had similar BMI across waves. Depression was higher in girls in all Waves, but decreased over time in boys and girls.
Overall maltreatment prevalence was 55% in girls and boys. Supervisory neglect was the most common (Girls, 38.0%; Boys, 43.2%) and sexual abuse was the least common (Girls, 8.0%; Boys, 5.1%; Appendix Table 3). Boys and girls were pooled in the LCA because the maltreatment classes were similar by gender (Table 1). The four-class model provided the optimal model fit and interpretability (entropy 0.69; Appendix Table 4). The no/low maltreatment class experienced, on average, <1 type of maltreatment. The supervisory neglect dominant class was characterized by supervisory neglect, the physical abuse dominant class had high prevalence of physical abuse and emotional neglect, and the high abuse and neglect class had elevated prevalence of all types of maltreatment except for emotional neglect.
Table 1.
Latent Childhood Maltreatment Classesa
| Characteristic | No/Low maltreatment (n=7,849) | Supervisory neglect dominant (n=3,178) | Physical abuse dominant (n=1,551) | High abuse and neglect (n=784) |
|---|---|---|---|---|
| Class prevalence (row %) | ||||
| Females | 59.8 | 23.1 | 12.5 | 4.6 |
| Males | 57.9 | 24.6 | 10.5 | 7.0 |
| Class probabilities of maltreatment types (column %) | ||||
| Supervisory neglect | 0.0 | 100 | 53.6 | 97.0 |
| Physical neglect | 2.0 | 11.5 | 5.0 | 100 |
| Physical abuse | 10.2 | 23.9 | 94.9 | 96.8 |
| Sexual abuse | 1.5 | 1.2 | 23.0 | 48.3 |
| Emotional neglect | 11.2 | 12.2 | 91.1 | 33.9 |
| Average number of maltreatment types | 0.2 | 1.4 | 2.5 | 3.6 |
National Longitudinal Study for Adolescent and Adult Health (n=13,362). Latent class analysis of five dichotomous maltreatment types. Four-class solution selected over three- and five-class solutions (Appendix Table 3) on the basis on Bayes Information Criteria (BIC) =54087.422 and Entropy =0.690.
Associations with depression (Figure 1, paths b and c) from adjusted individual models were similar to analogous associations in the mediation model; crude associations are reported in Appendix Table 5. In adjusted individual models, compared with no/low maltreatment, supervisory neglect dominant, physical abuse dominant, and high abuse and neglect maltreatment were associated with 0.7, 1.5, and 2.4 points greater baseline depression (intercept; age 12), respectively, in girls, and 0.5, 1.1, and 1.5 points greater baseline depression, respectively, in boys (Table 2, Model 1). Maltreatment was not associated with change in depression over time (slope). Associations between depression and BMI trajectories were largely weak and non-significant (Table 2, Model 2). In one exception, in females, depression slope was associated with faster BMI gain; although not statistically significant, mediation results are sensitive to the strength and direction of association in each pathway.
Table 2.
Associations Between Maltreatment Classa and Depression Trajectory, and Depression and BMI Trajectoryb
| Independent variable | Females | Males |
|---|---|---|
| Model 1 | Dependent variable: Depression intercept | |
|
|
||
| No/Low maltreatment | (ref) | (ref) |
| Supervisory neglect dominant | 0.7 (0.3, 1.0) | 0.5 (0.2, 0.8) |
| Physical abuse dominant | 1.5 (1.0, 2.0) | 1.1 (0.7, 1.6) |
| High abuse and neglect | 2.4 (1.5, 3.2) | 1.5 (1.0, 2.0) |
|
|
||
| Dependent variable: Depression slope | ||
|
|
||
| No/Low maltreatment | (ref) | (ref) |
| Supervisory neglect dominant | −0.2 (−0.4, 0.1) | −0.0 (−0.3, 0.2) |
| Physical abuse dominant | 0.1 (−0.3, 0.6) | 0.1 (−0.2, 0.5) |
| High abuse and neglect | −0.2 (−1.0, 0.5) | 0.0 (−0.5, 0.5) |
|
|
||
| Model 2 | Dependent variable: BMI intercept | |
|
|
||
| Depression intercept | 0.1 (−0.0, 0.2) | −0.1 (−0.2, 0.1) |
|
|
||
| Dependent variable: BMI slope | ||
|
|
||
| Depression intercept | 0.1 (−0.0, 0.2) | 0.0 (−0.1, 0.1) |
| Depression slope | 1.6 (−2.9, 6.0) | −0.7 (−1.5, 0.2) |
Note: Boldface indicates statistical significance (p<0.05).
Maltreatment classes derived using latent class analysis (Table 1).
National Longitudinal Study for Adolescent and Adult Health (n=13,362). Associations estimated from gender-stratified, individual latent growth curve models: Model 1 models maltreatment class predicting depression trajectory, Model 2 models depression trajectory predicting BMI trajectory. Adjusted for race/ethnicity, parental education, parental income at Wave I; and time-varying smoking, participant income, and participant education.
In females, no maltreatment classes were associated with BMI at baseline in individual models or in the mediation model (direct effects; Table 3). Supervisory neglect dominant and physical abuse dominant maltreatment were associated with faster BMI increases (0.3 [marginal] and 0.7 kg/m2 faster over 10 years, respectively), compared with no/low maltreatment (Table 3, individual models). The association of physical abuse dominant maltreatment with faster BMI gain was mediated through depression slope. The association between physical abuse dominant maltreatment and BMI slope was attenuated in the mediation model (coefficient=0.2; Table 3, direct effects); mediated effects included 0.07 indirect effects occurring through depression intercept and 0.36 indirect effects through depression slope. Although the relationship between maltreatment and depression slope was weak and not significant, mediation by depression slope may have occurred through physical abuse dominant maltreatment effects on depression intercept, which was correlated with depression slope, which in turn was strongly (but not significantly) associated with BMI slope (Table 3). The relationship between supervisory neglect dominant maltreatment and faster BMI gain was not mediated by depression.
Table 3.
Individual Association and Mediation Model for Childhood Maltreatment and BMI Trajectorya
| Independent variable | Individual association modelb | Direct effects | Indirect effects
|
|
|---|---|---|---|---|
| Through depression intercept | Through depression slope | |||
| Females (n=6,993) | ||||
| Estimated effects on BMI intercept | ||||
| No/Low maltreatment | (ref) | (ref) | (ref) | NA |
| Supervisory neglect dominant | 0.1 (−0.3, 0.6) | 0.1 (−0.4, 0.6) | 0.04 (−0.02, 0.13) | NA |
| Physical abuse dominant | 0.1 (−0.4, 0.6) | 0.0 (−0.5, 0.5) | 0.10 (−0.04, 0.26) | NA |
| High abuse and neglect | 0.4 (−0.4, 1.1) | 0.2 (−0.6, 1.0) | 0.16 (−0.07, 0.40) | NA |
| Estimated effects on BMI slope | ||||
| No/Low maltreatment | (ref) | (ref) | (ref) | (ref) |
| Supervisory neglect dominant | 0.3 (0.0, 0.7) | 0.5 (−0.6, 1.6) | 0.03 (−0.04, 0.10) | −0.23 (−1.98, 0.79) |
| Physical abuse dominant | 0.6 (0.1, 1.2) | 0.2 (−1.3, 1.7) | 0.07 (−0.08, 0.24) | 0.36 (−1.42, 2.98) |
| High abuse and neglect | −0.1 (−0.9, 0.7) | 0.1 (−2.1, 2.3) | 0.11 (−0.13, 0.36) | −0.33 (−4.63, 2.03) |
| Males (n=6,369) | ||||
| Estimated effects on BMI intercept | ||||
| No/Low maltreatment | (ref) | (ref) | (ref) | NA |
| Supervisory neglect dominant | 0.2 (− 0.3, 0.6) | 0.2 (−0.2, 0.7) | −0.03 (−0.11, 0.03) | NA |
| Physical abuse dominant | −0.5 (−1.1, 0.2) | −0.4 (− 1.1, 0.3) | −0.00 (− 0.23, 0.06) | NA |
| High abuse and neglect | 0.7 (− 0.1, 1.5) | 0.8 (0.0, 1.6) | −0.09 (− 0.29, 0.08) | NA |
| Estimated effects on BMI slope | ||||
| No/Low maltreatment | (ref) | (ref) | (ref) | (ref) |
| Supervisory neglect dominant | −0.2 (− 0.5, 0.2) | −0.2 (− 0.6, 0.3) | −0.01 (−0.06, 0.05) | 0.02 (−0.30, 0.45) |
| Physical abuse dominant | 0.2 (−0.2, 0.6) | 0.3 (−0.3, 0.8) | −0.00 (−0.14, 0.10) | −0.09 (− 0.47, 0.22) |
| High abuse and neglect | 0.0 (−0.7, 0.6) | 0.1 (− 0.7, 0.8) | −0.03 (−0.18, 0.13) | −0.04 (−0.50, 0.44) |
Note: Boldface indicates statistical significance (p<0.05).
National Longitudinal Study for Adolescent and Adult Health. Associations estimated from gender-stratified latent growth curve models. Adjusted for race/ethnicity, parental education, parental income at Wave I; and time-varying smoking, participant income, and participant education. All estimates except individual association model obtained from mediation model. CIs for indirect and total effects were not calculated due to the numerical integration used in the model.
Individual association model includes maltreatment class predicting BMI intercept and slope (without depression trajectory), adjusting for covariates listed in (a).
NA, Not Applicable
In males, high abuse and neglect maltreatment was marginally associated with higher BMI intercept in males, but this relationship was not mediated by depression. The association decomposed into 0.8 of the association through pathways other than depression intercept (direct effect) and −0.09 through depression intercept (indirect effect; Table 3). Otherwise, maltreatment was not associated with BMI intercept or slope in males.
DISCUSSION
This study investigated depression as a potential mechanism by which discrete classes of childhood maltreatment may impact BMI trajectory from adolescence to adulthood. Although maltreatment was associated with both depression and, to a lesser extent, BMI trajectories from adolescence to adulthood, only the relationship between physical abuse dominant maltreatment and faster BMI gain was mediated by depression only among girls.
The study findings partially support the hypotheses that depression mediates effects of more severe types of childhood maltreatment, and that depression pathways are stronger in girls than in boys. The four identified latent classes of maltreatment corresponded to severity and number of maltreatment types, which consistent with prior research in clinical and local populations,10–12 were associated with adolescent depression in a dose–dependent manner. Physical abuse dominant maltreatment was one of the more severe maltreatment classes and was characterized by physical abuse and emotional neglect, which are associated with dysregulated eating behaviors in previous research.39 Thus, physical abuse dominant is one type of maltreatment that may operate on BMI through depression, potentially via increases in emotional eating or psychomotor retardation15,16 among girls. However, depression may manifest differently in boys, such as through substance abuse, thus not leading to higher weight or weight gain.
A more severe type of maltreatment—high abuse and neglect — was strongly associated with depression in girls and boys; but was unrelated to BMI in girls and only marginally associated with higher baseline BMI in boys. The relationship between high abuse and neglect and BMI among boys, however, was not mediated by depression. The high frequency and severity of the high abuse and neglect class may induce pathways other than depression impacting BMI or different types of depression that do not affect energy balance.
Depression also did not mediate associations between supervisory neglect dominant maltreatment and BMI in girls. The high prevalence of this maltreatment class and mild nature of the supervisory neglect questionnaire item (“left home alone”; Appendix Table 1) suggest that this class may not reflect meaningful neglect. Rather, its marginal association with BMI gain may reflect more general aspects of the family environment, such as low family functioning. Fuller characterization of child neglect in the absence of physical or sexual abuse is needed to understand the processes underlying associations between this measure of child neglect and later health outcomes observed in prior research.40,41
Study findings did not support the hypothesis that associations between childhood maltreatment and later obesity are more strongly mediated by depression earlier in adolescence. For example, physical abuse dominant maltreatment was associated with marginally faster increase in BMI, but not BMI at baseline; this association was mediated by depression change from adolescence to adulthood. This finding is similar to a prior AddHealth study,4 in which abuse was associated with BMI increase in girls. With regard to depression, some studies conclude little sensitivity to age depression ascertainment,10 whereas others, primarily in high risk or clinical populations, suggest stronger associations with depression in adolescents than adults.55 Delayed effects could manifest through behavioral mechanisms that emerge or change during and after adolescence, such as depression, dysregulated eating, or sedentary behavior.
Depression mediated associations between physical abuse dominant maltreatment and modestly faster BMI gain (0.7 kg/m2 faster gain in BMI over 10 years) in girls. These findings suggest that depression treatment in childhood or adolescence may ameliorate a small degree of the effects of one type of childhood maltreatment, which was experienced by 12% of girls, on the development of obesity. However, further exploration of distinct, sex-specific psychological and behavioral trajectories that follow different types of maltreatment is needed.
In particular, these findings suggest critical gaps in understanding about psychological and behavioral responses to childhood maltreatment that occur throughout childhood and adolescence, when occurrence of maltreatment is often revealed.42–44 First, depression subtypes have different behavioral effects—for example, decreased or increased appetite,43 therefore the impact of childhood maltreatment on depression subtypes and subsequent obesity warrants further attention. Second, understanding of the extent to which depression or BMI trajectories can be altered by social support and family-based intervention is needed. Third, the roles of other mediators such as anxiety disorders, eating behaviors, and hormonal profiles, such as cortisol, are additional promising topics for future studies.
Limitations
The primary limitation of this study was its reliance on a retrospective measure of childhood maltreatment; more severe maltreatment may be under-reported, whereas less severe forms, such as supervisory neglect, may be over-reported. However, discordance in reports separated by 6 years was low, the AddHealth maltreatment measure is valid,36,45–47 and false-positive reports of childhood maltreatment are likely rare.48 Furthermore, retrospective reporting provides information about maltreatment on a prospective cohort, while avoiding ethical issues stemming from mandatory reporting of maltreatment reported by minors.
Other limitations include lack of information on pubertal onset, which may have impacted BMI trajectories. Although this study controlled for observed confounders of exposure–mediator, mediator–outcome, and exposure–outcome associations, residual confounding may remain.49 Investigation of effects of childhood maltreatment on depression and BMI earlier in childhood and reciprocal relationships between depression and BMI trajectories is needed.50 Similarly, exploration of interactions between maltreatment and depression in association with BMI (exposure–mediator interaction) is an important next step.51 Lastly, race/ethnic differences in associations between childhood maltreatment and BMI trajectory and body composition should be investigated.
These limitations are balanced by numerous strengths, including the use of a longitudinal design, a nationally representative sample, and classification of maltreatment that accounts for comorbidity of multiple types of abuse and neglect.
CONCLUSIONS
A recent call for “trauma-informed obesity prevention” recommends development of secondary prevention strategies that mitigate the adverse health consequences of childhood maltreatment.8 This study investigated depression as a potential secondary prevention focus. Although childhood maltreatment was consistently associated with depression in adolescence, less improvement in depression mediated the relationship between only one type of maltreatment—physical abuse dominant—and faster BMI gain in girls. Investigation of additional potential mitigation strategies is needed.
Supplementary Material
Acknowledgments
This research uses data from National Longitudinal Study of Adolescent to Adult Health (Add Health), a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is given to Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining Data Files from Add Health should contact Add Health, The University of North Carolina at Chapel Hill, Carolina Population Center, 206 W. Franklin Street, Chapel Hill, NC 27516-2524 (addhealth_contracts@unc.edu). No direct support was received from grant P01-HD31921 for this analysis.
The project described was supported by the Office of Research in Women’s Health and the National Institute of Child Health and Human Development, Oregon Building Interdisciplinary Research Careers in Women’s Health Award Number K12HD043488 (JBH) and National Institute of Digestive Disorders and Nutrition K01DK102857 (JBH). RMS conceived of the study, performed statistical analysis, and drafted the manuscripts. NFD assisted with statistical analysis and interpretation of statistical findings and critically reviewed the manuscript. KWB assisted with the interpretation of study findings and critically reviewed the manuscript. ET and SA performed supplementary data analyses and critically reviewed the manuscript. JBH assisted with and supervised all aspects of the study and critically reviewed the manuscript. All authors approved the final version of the manuscript. No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tjaden P, Thoennes N. Prevalence, incidence, and consequences of violence against women: Findings from the national violence against women survey. Violence Against Women. 2000;6(2):142–161. https://doi.org/10.1177/10778010022181769. [Google Scholar]
- 2.Finkelhor D, Turner HA, Shattuck A, et al. Prevalence of childhood exposure to violence, crime, and abuse: Results from the National Survey of Children’s Exposure to Violence. JAMA Pediatr. 2015;169(8):746. doi: 10.1001/jamapediatrics.2015.0676. https://doi.org/10.1001/jamapediatrics.2015.0676. [DOI] [PubMed] [Google Scholar]
- 3.Shin SH, Miller DP. A longitudinal examination of childhood maltreatment and adolescent obesity: Results from the National Longitudinal Study of Adolescent Health (AddHealth) Study. Child Abuse Negl. 2012;36(2):84–94. doi: 10.1016/j.chiabu.2011.08.007. https://doi.org/10.1016/j.chiabu.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Power C, Pinto Pereira SM, Li L. Childhood Maltreatment and BMI Trajectories to Mid-Adult Life: Follow-Up to Age 50y in a British Birth Cohort. PLoS One. 2015;10(3):e0119985. doi: 10.1371/journal.pone.0119985. https://doi.org/10.1371/journal.pone.0119985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry. 2013;(19):544–554. doi: 10.1038/mp.2013.54. https://doi.org/10.1038/mp.2013.54. [DOI] [PubMed]
- 6.Richardson AS, Dietz WH, Gordon-Larsen P. The association between childhood sexual and physical abuse with incident adult severe obesity across 13 years of the National Longitudinal Study of Adolescent Health. Pediatr Obes. 2014;9(5):351–361. doi: 10.1111/j.2047-6310.2013.00196.x. https://doi.org/10.1111/j.2047-6310.2013.00196.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong M, Giles WH, Felitti VJ, et al. Insights into causal pathways for ischemic heart disease: Adverse childhood experiences study. Circulation. 2004;110(13):1761–1766. doi: 10.1161/01.CIR.0000143074.54995.7F. https://doi.org/10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- 8.Mason SM, Bryn Austin S, Bakalar JL, et al. Child Maltreatment’s Heavy Toll: The Need for Trauma-Informed Obesity Prevention. Am J Prev Med. 2016;50(5):646–649. doi: 10.1016/j.amepre.2015.11.004. https://doi.org/10.1016/j.amepre.2015.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernet CZ, Stein MB. Relationship of childhood maltreatment to the onset and course of major depression in adulthood. Depress Anxiety. 1999;9(4):169–174. https://doi.org/10.1002/(SICI)1520-6394(1999)9:4<169::AID-DA4>3.0.CO;2-2. [PubMed] [Google Scholar]
- 10.Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. Am J Psychiatry. 2012;169(2):141–151. doi: 10.1176/appi.ajp.2011.11020335. https://doi.org/10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- 11.Gibb BE, Alloy LB, Abramson LY, et al. History of childhood maltreatment, negative cognitive styles, and episodes of depression in adulthood. Cognit Ther Res. 2001;25(4):425–446. https://doi.org/10.1023/A:1005586519986. [Google Scholar]
- 12.Toth SL, Manly JT, Cicchetti D. Child maltreatment and vulnerability to depression. Dev Psychopathol. 1992;4(1):97–112. https://doi.org/10.1017/S0954579400005587. [Google Scholar]
- 13.Cowell RA, Cicchetti D, Rogosch FA, Toth SL. Childhood maltreatment and its effect on neurocognitive functioning: Timing and chronicity matter. Dev Psychopathol. 2015;27(2):521–533. doi: 10.1017/S0954579415000139. https://doi.org/10.1017/S0954579415000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dunn EC, McLaughlin KA, Slopen N, Rosand J, Smoller JW. Development and timing of child maltreatment and symptoms of depression and suicidal ideation in young adulthood: results from the national longitudinal study of adolescent health. Depress Anxiety. 2013;30(10):955–964. doi: 10.1002/da.22102. https://doi.org/10.1002/da.22102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Konttinen H, Männistö S, Sarlio-Lähteenkorva S, Silventoinen K, Haukkala A. Emotional eating, depressive symptoms and self-reported food consumption. A population-based study. Appetite. 2010;54(3):473–479. doi: 10.1016/j.appet.2010.01.014. https://doi.org/10.1016/j.appet.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 16.Lewinsohn PM, Petit JW, Joiner TE, Seeley JR. The symptomatic expression of major depressive disorder in adolescents and young adults. J Abnorm Psychol. 2003;112(2):244–252. doi: 10.1037/0021-843x.112.2.244. https://doi.org/10.1037/0021-843X.112.2.244. [DOI] [PubMed] [Google Scholar]
- 17.Nelson EC, Heath AC, Madden PAF, et al. Association Between Self-reported Childhood Sexual Abuse and Adverse Psychosocial Outcomes. Arch Gen Psychiatry. 2002;59(2):139. doi: 10.1001/archpsyc.59.2.139. https://doi.org/10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- 18.Snyder SM, Merritt DH. The Effect of Childhood Supervisory Neglect on Emerging Adults’ Drinking. Subst Use Misuse. 2016;51(1):1–14. doi: 10.3109/10826084.2015.1073321. https://doi.org/10.3109/10826084.2015.1073321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Snyder SM, Merritt DH. The Influence of Supervisory Neglect on Subtypes of Emerging Adult Substance Use After Controlling for Familial Factors, Relationship Status, and Individual Traits. Subst Abus. 2015;36(4):507–514. doi: 10.1080/08897077.2014.997911. https://doi.org/10.1080/08897077.2014.997911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herrenkohl RC, Herrenkohl TI. Assessing a child’s experience of multiple maltreatment types: Some unfinished business. J Fam Violence. 2009;24(7):485–496. doi: 10.1007/s10896-009-9247-2. https://doi.org/10.1007/s10896-009-9247-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mamun AA, Lawlor DA, O’Callaghan MJ, Bor W, Williams GM, Najman JM. Does childhood sexual abuse predict young adult’s BMI? A birth cohort study. Obesity (Silver Spring) 2007;15(8):2103–2110. doi: 10.1038/oby.2007.250. https://doi.org/10.1038/oby.2007.250. [DOI] [PubMed] [Google Scholar]
- 22.Gunstad J, Paul RH, Spitznagel MB, et al. Exposure to early life trauma is associated with adult obesity. Psychiatry Res. 2006;142(1):31–37. doi: 10.1016/j.psychres.2005.11.007. https://doi.org/10.1016/j.psychres.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 23.Galbraith S, Bowden J, Mander A. Accelerated longitudinal designs: An overview of modelling, power, costs and handling missing data. Stat Methods Med Res. 2017;26(1):374–398. doi: 10.1177/0962280214547150. https://doi.org/10.1177/0962280214547150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris K, Halpern C, Whitsel E, et al. The National Longitudinal Study of Adolescent to Adult Health: research design. Add Health: The National Longitudinal Study of Adolescent to Adult Health. www.cpc.unc.edu/projects/addhealth/design. Published 2009.
- 25.Hussey JM, Nguyen QC, Whitsel EA, et al. The reliability of in-home measures of height and weight in large cohort studies: Evidence from Add Health. Demogr Res. 2015;32:1081–1098. doi: 10.4054/DemRes.2015.32.39. https://doi.org/10.4054/DemRes.2015.32.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977;1(3):385–401. https://doi.org/10.1177/014662167700100306. [Google Scholar]
- 27.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two Shorter Forms of the CES-D Depression Symptoms Index. J Aging Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. https://doi.org/10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 28.Cole JC, Rabin AS, Smith TL, Kaufman AS. Development and validation of a Rasch-derived CES-D short form. Psychol Assess. 2004;16(4):360–372. doi: 10.1037/1040-3590.16.4.360. https://doi.org/10.1037/1040-3590.16.4.360. [DOI] [PubMed] [Google Scholar]
- 29.Armour C, Elklit A, Christoffersen MN. A Latent Class Analysis of Childhood Maltreatment: Identifying Abuse Typologies. J Loss Trauma. 2014;19(1):23–39. https://doi.org/10.1080/15325024.2012.734205. [Google Scholar]
- 30.Nooner KB, Litrownik AJ, Thompson R, et al. Youth self-report of physical and sexual abuse: a latent class analysis. Child Abuse Negl. 2010;34(3):146–154. doi: 10.1016/j.chiabu.2008.10.007. https://doi.org/10.1016/j.chiabu.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Berzenski SR, Yates TM. Classes and Consequences of Multiple Maltreatment: A Person-Centered Analysis. Child Maltreat. 2011;16(4):250–261. doi: 10.1177/1077559511428353. https://doi.org/10.1177/1077559511428353. [DOI] [PubMed] [Google Scholar]
- 32.Clark S, Muthen B. [Accessed June 15, 2017];Relating Latent Class Analysis Results to Variables not Included in the Analysis. https://www.statmodel.com/download/relatinglca.pdf.
- 33.Hayes AF, Preacher KJ. Statistical mediation analysis with a multicategorical independent variable. Br J Math Stat Psychol. 2014;67(3):451–470. doi: 10.1111/bmsp.12028. https://doi.org/10.1111/bmsp.12028. [DOI] [PubMed] [Google Scholar]
- 34.Sobel ME. Direct and Indirect Effects in Linear Structural Equation Models. Sociol Methods Res. 1987;16(1):155–176. https://doi.org/10.1177/0049124187016001006. [Google Scholar]
- 35.Selig J, Preacher KJ. Monte Carlo method for assessing mediation: An interactive tool for creating confidence intervals for indirect effects. 2008 www.quantpsy.org.
- 36.Hussey JM, Chang JJ, Kotch JB. Child maltreatment in the United States: prevalence, risk factors, and adolescent health consequences. Pediatrics. 2006;118(3):933–942. doi: 10.1542/peds.2005-2452. https://doi.org/10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- 37.Straus MA. Prevalence of Violence Against Dating Partners by Male and Female University Students Worldwide. Violence Against Women. 2004;10(7):790–811. https://doi.org/10.1177/1077801204265552. [Google Scholar]
- 38.Higgins DJ. The importance of degree versus type of maltreatment: a cluster analysis of child abuse types. J Psychol. 2004;138(4):303–324. doi: 10.3200/JRLP.138.4.303-324. https://doi.org/10.3200/JRLP.138.4.303-324. [DOI] [PubMed] [Google Scholar]
- 39.Van der Kolk BA, Fisler RE. Childhood abuse and neglect and loss of self-regulation. Bull Menninger Clin. 1994;58(2):145–168. [PubMed] [Google Scholar]
- 40.Slack KS, Holl JL, McDaniel M, Yoo J, Bolger K. Understanding the Risks of Child Neglect: An Exploration of Poverty and Parenting Characteristics. Child Maltreat. 2004;9(4):395–408. doi: 10.1177/1077559504269193. https://doi.org/10.1177/1077559504269193. [DOI] [PubMed] [Google Scholar]
- 41.Knutson JF, Taber SM, Murray AJ, Valles NL, Koeppl G. The Role of Care Neglect and Supervisory Neglect in Childhood Obesity in a Disadvantaged Sample. J Pediatr Psychol. 2010;35(5):523–532. doi: 10.1093/jpepsy/jsp115. https://doi.org/10.1093/jpepsy/jsp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sobin C, Sackeim HA. Psychomotor symptoms of depression. Am J Psychiatry. 1997;154(1):4–17. doi: 10.1176/ajp.154.1.4. https://doi.org/10.1176/ajp.154.1.4. [DOI] [PubMed] [Google Scholar]
- 43.Casper RC, Redmond DE, Katz MM, et al. Somatic Symptoms in Primary Affective Disorder. Arch Gen Psychiatry. 1985;42(11):1098. doi: 10.1001/archpsyc.1985.01790340082012. https://doi.org/10.1001/archpsyc.1985.01790340082012. [DOI] [PubMed] [Google Scholar]
- 44.Keller MC, Neale MC, Kendler KS. Association of Different Adverse Life Events With Distinct Patterns of Depressive Symptoms. Am J Psychiatry. 2007;164(10):1521–1529. doi: 10.1176/appi.ajp.2007.06091564. https://doi.org/10.1176/appi.ajp.2007.06091564. [DOI] [PubMed] [Google Scholar]
- 45.Fang X, Corso PS. Child Maltreatment, Youth Violence, and Intimate Partner Violence: Developmental Relationships. Am J Prev Med. 2007;33(4):281–290. doi: 10.1016/j.amepre.2007.06.003. https://doi.org/10.1016/j.amepre.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 46.Yun I, Ball JD, Lim H. Disentangling the relationship between child maltreatment and violent delinquency: using a nationally representative sample. J Interpers Violence. 2011;26(1):88–110. doi: 10.1177/0886260510362886. https://doi.org/10.1177/0886260510362886. [DOI] [PubMed] [Google Scholar]
- 47.Ouyang L, Fang X, Mercy J, Perou R, Grosse SD. Attention-deficit/hyperactivity disorder symptoms and child maltreatment: a population-based study. J Pediatr. 2008;153(6):851–856. doi: 10.1016/j.jpeds.2008.06.002. https://doi.org/10.1016/j.jpeds.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 48.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. J Child Psychol Psychiatry Allied Discip. 2004;45(2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. https://doi.org/10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 49.Vanderweele TJ. Invited commentary: Structural equation models and epidemiologic analysis. Am J Epidemiol. 2012;176(7):608–612. doi: 10.1093/aje/kws213. https://doi.org/10.1093/aje/kws213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. https://doi.org/10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 51.Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: Theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–150. doi: 10.1037/a0031034. https://doi.org/10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. J Child Psychol Psychiatry Allied Discip. 2004;45(2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. https://doi.org/10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 53.Osofsky JD. Prevalence of children’s exposure to domestic violence and child maltreatment: Implications for prevention and intervention. Clin Child Fam Psychol Rev. 2003;6(3):161–170. doi: 10.1023/a:1024958332093. https://doi.org/10.1023/A:1024958332093. [DOI] [PubMed] [Google Scholar]
- 54.Schneiderman JU, Negriff S, Peckins M, Mennen FE, Trickett PK. Body mass index trajectory throughout adolescence: a comparison of maltreated adolescences by maltreatment type to a community sample. Pediatr Obes. 2014;10(4):296–304. doi: 10.1111/ijpo.258. https://doi.org/10.1111/ijpo.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Infurna MR, Reichi C, Parzer P, Schimmenti A, Bifulco A, Kaess M. Associations between depression and specific childhood experiences of abuse and neglect: A meta-analysis. J Affect Disord. 2016;190:47–55. doi: 10.1016/j.jad.2015.09.006. https://doi.org/10.1016/j.jad.2015.09.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.