Abstract
Objective
Methadone is associated with prolongation of the electrocardiographic QTc interval. QTc prolongation may be linked to cardiac dysrhythmia and sudden cardiac death. The rate of these events is unknown in methadone-maintained patients.
Methods
This retrospective cohort study of 749 patients with opioid use disorder receiving methadone maintenance therapy through a single safety-net hospital, queried the electronic health record for electrocardiogram results, demographics, methadone dose, and diagnostic codes consistent with cardiac conduction disorder (ICD-9 426) and cardiac dysrhythmia (ICD-9 427). Factors associated with QTc interval were explored; Cox-proportional hazards regression models were used to analyze time to an event that may predispose to sudden cardiac death.
Results
One hundred thirty four patients had an electrocardiogram while on methadone, 404 while off methadone, and 211 both while on and off methadone. Mean QTc interval while on methadone (436 msec, SD 36) was significantly greater than while off (423 msec, SD 33). Age and methadone dose were weakly associated with increased QTc interval (p<0.01 and p<0.0005, respectively, adjusted R2=0.05). There were 44 ICD-9 426 and 427 events over 7,064 patient years (6.3 events/1,000 patient years). Having a QTc greater than gender specific cut-off values was significantly associated with time to event (hazard ratio 3.32; 95% CI 1.25-8.81) but being on methadone was not.
Conclusions
Methadone is associated with QTc prolongation in a non-clinically significant dose-related manner. Cardiac events were rare and the sudden cardiac death rate was below that of the general population. Current recommendations for cardiac risk assessment in methadone maintained patients should be reconsidered.
Keywords: methadone, QTc interval, sudden cardiac death, electrocardiogram, event rate
Introduction
The incidence of heroin and prescription opioid misuse has increased dramatically over the past several years (Substance Abuse and Mental Health Services Administration, 2016). An estimated 3 million Americans have a current or previous diagnosis of an opioid use disorder (Substance Abuse and Mental Health Services Administration, 2016). Only 25% of these people engage in treatment, however (Substance Abuse and Mental Health Services Administration, 2016). Several recent state and federal initiatives have focused on improving access to medications for treating opioid use disorders. As awareness of and access to these highly effective medications grows, there has been concern about the safety of methadone specifically (Centers for Disease Control and Prevention, 2012).
A disproportionate number of opioid-related deaths have been linked to methadone (Centers for Disease Control and Prevention, 2012). Two separate federal panels concluded that the increase in methadone associated-deaths was not due to its use in treating opioid use disorders but rather to its less regulated use in the context of pain treatment (Center for Substance Abuse Treatment, 2004; Center for Substance Abuse Treatment, 2007). Nevertheless, the specter of methadone-induced sudden cardiac death has been raised for all persons exposed to methadone and in response, several medical societies have published clinical practice safety guidelines (Martin et al., 2011; Chou et al., 2014; American College of Medical Toxicology, 2016). While methadone is associated with prolongation of the electrocardiographic QTc interval, the clinical significance of this remains uncertain.
The electrocardiographic QT interval represents the depolarization and repolarization time of the cardiac ventricles. This interval can vary based on heart rate and thus is often expressed as the rate corrected QT interval, or QTc. Prolongation of the QTc interval may predispose the heart to irregular electrical activity and torsades des pointes, a potentially fatal dysrhythmia that can result in sudden cardiac death. This is most apparent in Long QT Syndrome, a genetically heterogeneous set of variations in cardiac ion channels that can impart a 5% annual incidence of sudden cardiac death (Goldenberg and Moss, 2008). Risk of sudden cardiac death in the setting of prolonged QTc interval has also been noted in patients with cardiovascular disease and abnormalities in serum electrolytes such as potassium, magnesium, and calcium. Several medications, including methadone, are known to increase the QTc interval with variable linkage to increased risk for torsades des pointes and sudden cardiac death (Woosley, Heise, and Romero, 2017). In the general population, however, there is little association between QTc interval and mortality in those without underlying heart disease (Goldberg et al., 1991; Elming et al., 1998; Montanez et al., 2004).
Methadone is a synthetic opioid agonist that is known to prolong the QTc interval (Martin et al., 2011). Whether this prolongation imparts increased risk for sudden cardiac death remains controversial (Bart, 2011). Previous reports have linked methadone to QTc prolongation but few have examined prospective cohorts where pre- versus post- methadone QTc interval comparisons can be made (Martell et al., 2005; Peles et al., 2013). Martell et al. found a dose-response relationship between methadone and QTc at 6 months but not at 12 months (Martell et al. 2005). No prospective studies have tracked QTc measurement and the incidence of cardiac events during methadone maintenance treatment. Most cross-sectional and retrospective cohort studies have evaluated mean QTc interval in methadone patients with no control group for comparison (Fonseca et al., 2009; Mayet et al., 2011). Some cross-sectional studies have found a dose-response relationship between methadone and QTc interval (Krantz et al., 2003; Anchersen et al., 2009), while others have not (Isbister et al., 2017). Further, very few studies have considered incidence of dysrhythmia or cardiac events in methadone patients with or without QTc prolongation (Krantz et al., 2003; Anchersen et al., 2009; Mayet et al., 2011).
The purpose of this retrospective cohort study was twofold: (1) to evaluate the prevalence of and factors associated with QTc interval prolongation in a methadone exposed population, and (2) to evaluate the risk of developing sudden cardiac death or a dysrhythmia that may predispose to sudden cardiac death in a methadone exposed population. Because our cohort of methadone patients includes those whose electrocardiogram was obtained while on methadone, while off methadone, or both on and off methadone, we have the internal cohort controls that most other studies lack.
Methods
This retrospective cohort study was performed at a single urban safety-net hospital's methadone maintenance treatment program. The Human Subjects Research Committee of the Hennepin County Medical Center provided expedited approval of this chart review study. The medical record numbers of all methadone treatment admissions between 1994 and 2010 were cross-referenced with the health system electronic health record and electrocardiogram (ECG) database for the presence of an ECG. All methadone treatment admissions receiving at least one dose of methadone were included (n=1,168 admissions representing 778 unique individuals). Patients with no history of an ECG (n=29) were excluded from the analysis. If a patient had more than one ECG while taking methadone, the ECG closest to their date of admission to methadone treatment was selected. If a patient had no ECG while on methadone, the ECG in closest proximity to (i.e., before or following) their methadone treatment was selected. For patients who had ECGs both while on and off methadone, a similar convention was used for selecting ECGs. The methadone treatment program does not engage in ECG screening of its patient population. Therefore, all ECGs were obtained elsewhere in the health system during the course of routine or emergency care and at the providers' discretion.
The QTc interval was obtained from Tracemaster (Philips Medical Systems, Oxnard, CA) ECG analysis software. Tracemaster provides computerized interpretations of ECGs and provides a uniform interpretation of the QTc interval following a validated algorithm. Each electrocardiogram was reviewed by a staff cardiologist before its entry into the electronic health record. Electrocardiograms showing atrial fibrillation (n=5) were excluded due to beat-to-beat variability that makes QTc interval interpretation unreliable.
Patient demographic and methadone dose information on the day of ECG acquisition was taken from an electronic medication dispensing system (Methasoft, Netalytics, Greer, SC). Information about the setting of ECG acquisition (i.e., inpatient, outpatient, or emergency department), and presence of an International Classification of Disease, Ninth Revision (ICD-9) diagnosis of a cardiac conduction disorder (ICD-9 426) or cardiac dysrhythmias (ICD-9 427) was obtained from the electronic medical record (Epic, Verona, WI). To track time to possible cardiac diagnoses, the electronic health record was queried through November 17, 2011.
Statistical Analysis
Characteristics of those with an ECG while on methadone were compared to those with an ECG while off methadone using Chi-square tests for categorical measures and two-sample t-tests for continuous measures. In the subset of patients who had an ECG both while off and while on methadone, a paired t-test was used to evaluate the difference in QTc interval off methadone versus on methadone. Stepwise linear regression was used to evaluate the relationship between QTc (the dependent variable) and these candidate predictors: age at time of ECG, methadone dose, gender, race, and setting where the ECG was obtained (inpatient, outpatient, or emergency department). Forward and backward steps required a p value less than 0.15 to be retained in the model.
Time to event analysis defined an event as either of ICD-9 diagnosis codes 426 (conduction disorders) or 427 (cardiac dysrhythmias). Each patient's event-time clock started with the date of their first ECG in the dataset and ended (i.e., censoring) at the date of event or when our data collection period ended (November 17, 2011), whichever occurred first. Person time at risk was calculated and incident rates defined per 1,000 person years. Because not all ICD-9 426 and 427 diagnoses predispose to risk for sudden cardiac death, a subset of those diagnoses that could plausibly lead to SCD were analyzed (ICD-9 426.82, 427.1, 427.41, 427.41, 427.5, 427.89) using a Cox proportional-hazards regression model that included the patient's most recent QTc as a binary predictor defined by whether the person exceeded the gender-specific upper limit of normal QTc interval (>450 msec for men and >470 msec for women) and an indicator of whether the ECG was obtained while on or off methadone. For people who did not have an event, the QTc measurement from the date closest to the censoring date was included in the model.
All analyses were performed using SAS (version 9.4, SAS Institute Inc., Cary, NC). A two-sided p-value < 0.05 was considered statistically significant.
Results
Patient characteristics and relationship to QTc interval
Characteristics of patients with an ECG only while on methadone (ON, n=134) compared to those with an ECG only while off methadone (OFF, n=404) are presented in Table 1. The mean methadone dose ON was 77 mg (SD 41). The mean length of time on methadone at time of ECG acquisition was 2.2 years (SD 2.9). The mean length of time either before starting or after stopping methadone at time of ECG acquisition in the OFF group was 2.9 years (SD 3.2). Patients ON were older at the time of ECG than those OFF, mean age in years 45.2 (SD 12.2) versus 41.5 (10.8) (p < 0.001). The ethnic distribution differed between the groups (p < 0.0001), with more Asians in the ON group. The setting where the ECG was acquired also differed between the groups with the ON group having more ECGs obtained in an inpatient setting, but this did not reach statistical significance. Finally, the mean QTc interval in the ON group (436 msec, SD 36) was significantly greater than the QTc interval in the OFF group (423 msec, SD 33), p < 0.001. Four patients (3%) ON had a QTc interval ≥ 500 msec compared to 6 (1.5%) OFF.
Table 1. Baseline Characteristics.
| Characteristic | ECG on Methadone (n=134) | ECG off Methadone (n=404) | P |
|---|---|---|---|
| Age at time of ECG, years (SD) | 45.2 (12.2) | 41.5 (10.8) | <0.001 |
| Male (%) | 69 (51.5) | 212 (52.5) | NS |
| Race (%) | <0.0001 | ||
| Caucasian | 67 (50.0) | 205 (50.7) | |
| African American | 33 (24.6) | 145 (35.9) | |
| Asian | 23 (17.1) | 13 (3.2) | |
| Other | 11 (8.2) | 41 (10.2) | |
| ECG Setting (%) | NS | ||
| Emergency department | 97 (72.4) | 278 (69.0) | |
| Inpatient | 16 (11.9) | 31 (7.7) | |
| Outpatient | 21 (15.7) | 95 (23.3) | |
| QTc, msec (SD) | 436 (36) | 423 (33) | <0.001 |
| QTc ≥ 500 msec (%) | 4 (3.0) | 6 (1.5) | NS |
| Dose, mg (range) (SD)* | 77 (1-285) (41) | -- |
Dose data missing in 12 patients
We next examined the subset of patients that had ECGs both on (bON) and off (bOFF) methadone (n=211). The mean length of time on methadone at time of ECG acquisition was 1.2 years (SD 1.6). The mean length of time either before or after stopping methadone at time of ECG acquisition in the bOFF group was 2.6 years (SD 3.0). Among these patients, the mean length of time between the two ECGs was 1.1 years (SD 3.8). Characteristics of patients with ECGs bON and bOFF are presented in Table 2. The mean dose of methadone bON was 74.5 mg (SD 26.5). Neither age nor setting differed between bON and bOFF ECGs. The mean QTc interval bON was 440 msec (SD 35) versus 429 msec (SD 34) bOFF, p < 0.0005. Of the 211 patients who had an ECG both on and off of methadone, 7 had a QTc interval ≥ 500 msec only while on, 4 had a QTc interval ≥ 500 msec only while off, and 3 had a QTc interval ≥ 500 msec both on and off.
Table 2. Baseline Characteristics of Patients with ECG bON and bOFF Methadone.
| Characteristic N = 211 | ECG on Methadone | ECG off Methadone | P |
|---|---|---|---|
| Age at time of ECG, years (SD) | 47.6 (9.7) | 46.5 (10.0) | NS |
| Male (%) | 57.4 | 57.4 | -- |
| Race (%) | -- | ||
| Caucasian | 46.5 | -- | |
| African American | 37.4 | -- | |
| Asian | 5.2 | -- | |
| Other | 10.9 | -- | |
| ECG Setting (%) | NS | ||
| Emergency department | 64.0 | 66.4 | |
| Inpatient | 22.3 | 24.2 | |
| Outpatient | 13.7 | 9.5 | |
| QTc, msec (SD) | 440 (35) | 429 (34) | <0.001 |
| QTc ≥ 500 msec (%) | 10 (4.8) | 4 (1.9) | NS |
| Dose, mg (range) (SD)* | 74.5 (15-140) (26.5) | -- | -- |
Dose data missing in 15 patients
All patients with an ECG while on methadone were combined (i.e., ON and bON groups) in a regression analysis with dependent variable QTc interval. In selecting predictors of QTc interval, neither gender nor setting of ECG made it into the final model, which is presented in Table 3. Both age and methadone dose were associated with QTc interval, p<0.01 and p<0.0005, respectively. Only 5% of the variance in QTc interval was associated with methadone dose and age, however (see Figure).
Table 3. Linear Regression Model.
| Coefficient | 95% CI | P | |
|---|---|---|---|
| QTc, msec (intercept) | 401 | 381-421 | -- |
| Age at ECG | 0.47 | 0.11-0.83 | < 0.01 |
| Methadone dose | 0.21 | 0.09-0.33 | < 0.0005 |
| Adj-R2 | 0.05 |
Figure. Regression of methadone dose on QTc interval (N=318*).
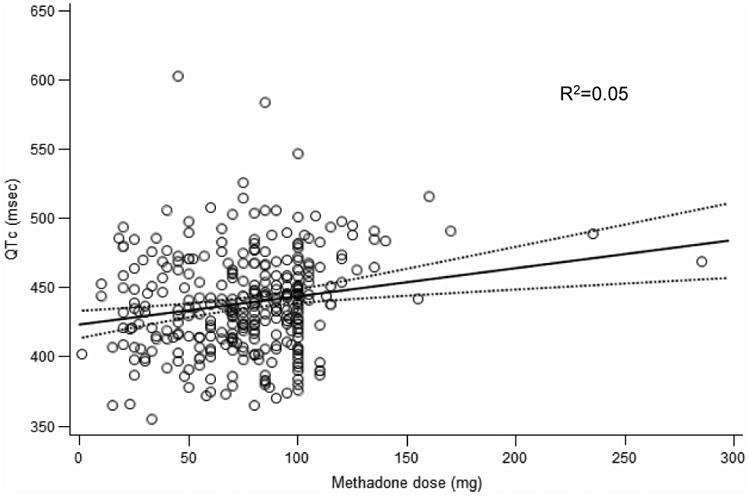
Dashed lines are mean predicted 95% confidence limits; * Dose data missing on 27 patients
QTc interval and risk of event
There were 44 ICD-9 diagnosis codes 426 or 427 events over 7,064 person-years (6.3 events per 1,000 person-years). A table of all 44 ICD-9 diagnosis codes is presented in the supplementary materials. Only 18 of these events could plausibly lead to SCD, an event rate of 2.5 per 1,000 person-years. The hazard ratio for one of these events, comparing QTc over versus under the gender-specific threshold, was 3.32 (95% CI 1.25-8.81), p < 0.05 but methadone at time of ECG was not significantly associated with this type of event (hazard ratio 0.67, 95% CI 0.25-1.82). Cardiac arrest (ICD-9 427.5) occurred in three male patients, two while taking methadone (both died from the event) and one while off methadone (this man survived the event to die of an overdose six years later). All three events were considered sudden cardiac death (with one successful resuscitation), for an event rate of 0.42 per 1,000 person-years. None of the patients had known structural cardiac disease prior to the event; although one initially found in pulseless electrical activity had chronic obstructive pulmonary disease and one (who survived) had hyperkalemia and was taking tricyclic antidepressants at the time of the event. Two of these patients had an ECG within 2 months of the event and the QTc intervals were ON (methadone 260 mg daily) 460 msec and OFF 404 msec.
Discussion
Our results confirm previous findings and extend them by addressing the clinical significance of the relationship between methadone and the QTc interval. As with other reports, we found a significant relationship between the QTc interval and methadone. While the relationship was dose-dependent, the clinical significance of this relationship is questionable for those taking generally therapeutic doses of methadone (e.g., 80-120 mg). For example, if we use the regression coefficient in our study to project QTc change per milligram of methadone, a person with a baseline QTc of 420 msec would need to be on a methadone dose greater than 140 mg or 225 mg daily to exceed the upper limits of QTc threshold for a man or woman, respectively.
With over 7,000 person-years tracked, the event rate for ICD-9 diagnoses that could plausibly lead to SCD was only 2.5 per 1,000 person-years. We were very liberal in our inclusion of ICD-9 codes that could lead to SCD (e.g., we included sinus bradycardia, a known effect of all opioids), so the event rate for more worrisome codes such as ventricular tachycardia is even lower. The event rate for sudden cardiac death in this study was 0.42 per 1,000 person years, which is higher than the estimated rate of 0.14 per 1,000 person years reported by Butler et al. (Butler et al., 2011). To place our finding in context, however, the age-adjusted event rate for sudden cardiac death in the US general population is 1.75 per 1,000 person-years (Centers for Disease Control and Prevention, 2002). Because the QTc interval most proximal to the SCD event was normal in two patients and 460 msec in the other, it remains unclear how current recommendations for cardiac risk monitoring in methadone populations would have prevented these events. In fact, the American Heart Association, the American College of Cardiology Foundation, the Heart Rhythm Society, and the National Heart, Lung, and Blood Institute advise against using the QTc interval to risk-stratify for SCD (Goldberger et al., 2008; Fishman et al., 2010). A Cochrane review of QTc interval screening in methadone maintained patients was unable to find adequate evidence of benefit from screening in the prevention of cardiac morbidity or mortality (Pani et al., 2013).
Our study has a number of strengths. Our inclusion of ECGs obtained from methadone patients during a time when they were not taking methadone allows us to have comparator ECGs from within the population, which serve as a control for factors such as smoking prevalence, other substance use, and comorbid illness that may differ between drug users and the general population. That we have a subset of individuals for whom we have an ECG both while on and while off methadone further strengthens our findings. Unlike prior studies with small sample sizes, our sample size allowed us to assess the effect on the QTc interval of covariates such as age, gender, methadone dose, and context in which the ECG was obtained. Our inclusion of patients who had an ECG taken in the context of acute care (i.e., emergency and inpatient settings) may have biased our sample towards those suspected to have increased cardiac risk. We found few clinically important associations between methadone, QTc, and cardiac events despite this bias, which may strengthen our findings when placed in the context of current guideline recommendations for universal cardiac risk assessment screening (i.e., including otherwise healthy individuals) in methadone settings.
This study has several limitations. It is a retrospective cohort study, so we cannot assess change in QTc interval in a strictly pre- versus post-methadone manner. Information was not available on several factors relevant to QTc interval, such as serum levels of potassium, calcium, magnesium, use of other medications that may prolong the QTc, history of underlying heart disease, or urine drug test results. Our review of the electronic medical record for ICD-9 events was limited to a single safety-net health system and if events occurring in another health system were not later documented in our medical record, we may have underestimated the event rate. As the largest provider of emergency services in the region, it is likely that most acute cardiac events would be captured with our electronic health record. Additionally, we are not able to report overall mortality for the cohort. While we have tracked ICD-9 426 and 427 diagnostic codes, it is possible that some patients may have died from an undiagnosed cardiac event.
Conclusion
In conclusion, this retrospective cohort study of patients with opioid use disorder on methadone maintenance confirms the association between methadone and QTc interval prolongation but does not support a clinically meaningful dose dependence of this association. Cardiac events that could be associated with QTc prolongation occurred at a low rate and actual sudden cardiac death events were below those of the general population. It is unlikely that existing recommendations related to cardiac screening for methadone patients are warranted or can be effective in reducing methadone-associated cardiac morbidity and mortality.
Supplementary Material
Acknowledgments
The authors would like to thank Mr. Scott Lenz and Dr. JoAn Laes who helped with data acquisition. This work was supported in part by a National Institutes of Health–National Institute on Drug Abuse career development award K23 DA024663 (GB).
Funding: This work was supported by a National Institutes of Health–National Institute on Drug Abuse career development award K23 DA024663 (GB)
References
- American College of Medical Toxicology. ACMT Position Statement: The Use of Methadone as an Analgesic. J Med Toxicol. 2016;12:213–15. doi: 10.1007/s13181-015-0532-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anchersen K, Clausen T, Gossop M, et al. Prevalence and clinical relevance of corrected QT interval prolongation during methadone and buprenorphine treatment: a mortality assessment study. Addiction. 2009;104:993–99. doi: 10.1111/j.1360-0443.2009.02549.x. [DOI] [PubMed] [Google Scholar]
- Bart G. CSAT's QT interval screening in methadone report: outrageous fortune or sea of troubles? J Addict Dis. 2011;30:313–17. doi: 10.1080/10550887.2011.610707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler B, Rubin G, Lawrance A, et al. Estimating the risk of fatal arrhythmia in patients in methadone maintenance treatment for heroin addiction. Drug Alcohol Rev. 2011;30:173–80. doi: 10.1111/j.1465-3362.2010.00213.x. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration. Rockville, MD: Department of Health and Human Services; 2016. 2015 National Survey on Drug Use and Health: Detailed Tables. [Google Scholar]
- Center for Substance Abuse Treatment. Substance Abuse and Mental Health Services Administration. Rockville, MD: Department of Health and Human Services; 2004. Methadone-Associated Mortality: Report of a National Assessment. [Google Scholar]
- Center for Substance Abuse Treatment. Substance Abuse and Mental Health Services Administration. Rockville, MD: Department of Health and Human Services; 2007. Methadone mortality - a reassessment. [Google Scholar]
- Centers for Disease, Control, and Prevention. 2002. State-Specific Mortality from Sudden Cardiac Death — United States, 1999. MMRW. 2002;51:123–26. [PubMed] [Google Scholar]
- Centers for Disease, Control, and Prevention. Vital signs: Risk for overdose from methadone used for pain relief, United States, 1999-2010. MMRW. 2012;61:493–97. [PubMed] [Google Scholar]
- Chou R, Cruciani RA, Fiellin DA, Compton P, et al. Methadone Safety: A Clinical Practice Guideline From the American Pain Society and College on Problems of Drug Dependence, in Collaboration With the Heart Rhythm Society. The Journal of Pain. 2014;15:321–37. doi: 10.1016/j.jpain.2014.01.494. [DOI] [PubMed] [Google Scholar]
- Elming HE, Holm L, Jun C, et al. The prognostic value of the QT interval and QT interval dispersion in all-cause and cardiac mortality and morbidity in a population of Danish citizens. EurHeart J. 1998;19:1391–400. doi: 10.1053/euhj.1998.1094. [DOI] [PubMed] [Google Scholar]
- Fishman GI, Chugh SS, Dimarco JP, et al. Sudden cardiac death prediction and prevention: report from a National Heart, Lung, and Blood Institute and Heart Rhythm Society Workshop. Circulation. 2010;122:2335–48. doi: 10.1161/CIRCULATIONAHA.110.976092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonseca FJ, Marti-Almor A, Pastor M, et al. Prevalence of long QTc interval in methadone maintenance patients. Drug Alcohol Depend. 2009;99:327–32. doi: 10.1016/j.drugalcdep.2008.06.018. [DOI] [PubMed] [Google Scholar]
- Goldberg RJ, Bengtson J, Chen ZY, et al. Duration of the QT interval and total and cardiovascular mortality in healthy persons (The Framingham Heart Study experience) Am J Cardiol. 1991;67:55–58. doi: 10.1016/0002-9149(91)90099-7. [DOI] [PubMed] [Google Scholar]
- Goldberger JJ, Cain ME, Hohnloser SH, et al. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death: a scientific statement from the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and Prevention. Circulation. 2008;118:1497–518. [PubMed] [Google Scholar]
- Goldenberg I, Moss AJ. Long QT syndrome. J Am Coll Cardiol. 2008;51:2291–300. doi: 10.1016/j.jacc.2008.02.068. [DOI] [PubMed] [Google Scholar]
- Isbister GK, Brown AL, Alexander AG, et al. QT interval prolongation in opioid agonist treatment: analysis of continuous 12-lead electrocardiogram recordings. Br J Clin Pharmacol. 2017 May 9; doi: 10.1111/bcp.13326. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krantz MJ, Kutinsky IB, Robertson AD, et al. Dose-related effects of methadone on QT prolongation in a series of patients with torsade de pointes. Pharmacotherapy. 2003;23:802–5. doi: 10.1592/phco.23.6.802.32186. [DOI] [PubMed] [Google Scholar]
- Martell BA, Arnsten JH, Krantz MJ, et al. Impact of methadone treatment on cardiac repolarization and conduction in opioid users. Am J Cardiol. 2005;95:915–18. doi: 10.1016/j.amjcard.2004.11.055. [DOI] [PubMed] [Google Scholar]
- Martin JA, Campbell A, Killip T, et al. QT interval screening in methadone maintenance treatment: report of a SAMHSA expert panel. J Addict Dis. 2011;30:283–306. doi: 10.1080/10550887.2011.610710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayet S, Gossop M, Lintzeris N, et al. Methadone maintenance, QTc and torsade de pointes: who needs an electrocardiogram and what is the prevalence of QTc prolongation? Drug Alcohol Rev. 2011;30:388–96. doi: 10.1111/j.1465-3362.2010.00237.x. [DOI] [PubMed] [Google Scholar]
- Montanez A, Ruskin JN, Hebert PR, et al. Prolonged QTc interval and risks of total and cardiovascular mortality and sudden death in the general population: a review and qualitative overview of the prospective cohort studies. Arch Intern Med. 2004;164:943–48. doi: 10.1001/archinte.164.9.943. [DOI] [PubMed] [Google Scholar]
- Pani PP, Trogu E, Maremmani I, et al. QTc interval screening for cardiac risk in methadone treatment of opioid dependence. Cochrane Database of Systematic Reviews. 2013 doi: 10.1002/14651858.CD008939.pub2. Art No: CD008939. [DOI] [PubMed] [Google Scholar]
- Peles E, Linzy S, Kreek MJ, et al. Prospective study of QTc changes among former opiate addicts since admission to methadone maintenance treatment: benzodiazepine risk. J Addict Med. 2013;7:428–34. doi: 10.1097/ADM.0b013e3182a8a4f2. [DOI] [PubMed] [Google Scholar]
- Woosley RL, Heise CW, Romero KA. AZCERT, Inc.; [Accessed May 25, 2017]. QTdrugs List. www.CredibleMeds.org. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


