Abstract
Background
Evidence regarding the effectiveness of arthroscopic debridement for a triangular fibrocartilage complex (TFCC) tear is uncertain. The purpose of this study was to conduct a systematic review of outcomes to evaluate the effectiveness of debridement for TFCC tears.
Methods
We searched all available literature in the PubMed, EMBASE.com, and MEDLINE (Ovid) databases for articles reporting on TFCC tear debridement. Data collection included arc of motion, grip strength, patient reported outcomes, and complications.
Results
A total of 1,723 unique studies were identified, of which 18 studies met our criteria. The mean pre- and post-arc of wrist extension/flexion motion were 120° and 146° (6 studies). The mean pre -and post-grip strength were 65% and 91% of the contralateral side (10 studies). Disabilities of the Arm, Shoulder, and Hand scores (6 studies) and pain visual analogue scales (VAS, 7 studies) improved from 39 to 18, and from 7 to 3 respectively. The mean pain-VAS after debridement was 1.9 in ulnar positive groups and 2.4 in ulnar neutral and negative groups. Eighty seven percent of patients returned to their original work.
Conclusion
Patients reported reduced pain, improved functional and patient-reported outcomes after debridement of TFCC tears. Most patients after debridement returned to previous work with few complications. Though some of these cases may require secondary procedures, simple debridement can be performed with suitable satisfactory outcomes for cases with any type of ulnar variance.
Keywords: Arthroscopy, debridement, systematic review, triangular fibrocartilage complex
Triangular fibrocartilage complex (TFCC) tears cause ulnar-sided wrist pain, a common condition that surgeons treat. Seventy percent of symptomatic patients and 38% of asymptomatic patients had TFCC injury in the age group 50–69 years.1 In addition to wrist pain, TFCC injuries result in decreased grip strength and impaired hand function.2 TFCC injuries are managed non-operatively initially. Immobilization, activity modification, and analgesics are used for a few weeks.3 Park et al. reported that 48 of the 84 patients with clinical diagnosis of TFCC injuries had complete pain relief with immobilization.4 Therefore, we believe that conservative treatment with immobilization is the first choice for patients with TFCC injuries. However, up to 43% patients still have pain after immobilization; therefore, the treatment of TFCC injuries such as TFCC debridement or TFCC repair can help improve their symptoms.
Arthroscopic debridement is a therapeutic procedure for stable distal-ulnar joint associated with TFCC tears that fail non-operative management.5–7 Arthroscopic or open repair is suitable to peripheral ulnar side tears that are in vascular zone of the TFCC. Open repair techniques were the first established and substantiated procedures.8 Arthroscopic repair with many arthroscopic techniques such as inside-out, outside-in, and all-inside techniques are effective for this type of tear.9–11 TFCC debridement is less invasive than other surgical treatments for a tear. Additionally, the postoperative care after debridement is much shorter than for a TFCC tear repair.12 After debridement for central or radial sided TFCC tear, up to 85% of patients reported pain relief, with a mean grip strength and mean arc of motion restored to 94% compared with that of unaffected side.13,14 Conversely, Nishizuka et al. reported that TFCC debridement for stable central tear did not significantly improve grip strength and patient reported outcomes (PROs) at 18 months.15 It was also reported that only 40% of patients with a degenerative TFCC tear associated with ulnar positive variance were satisfied.16
There are inconsistencies regarding the indications and effectiveness of arthroscopic debridement for TFCC tears. However, there are no prior attempts to evaluate the effectiveness of debridement rigorously. Additionally, although some patients need further treatments including ulnar shortening osteotomy (USO), robust evidence is lacking regarding factors of ulnar variance that influence outcomes after TFCC debridement. The purpose of this study was to conduct a systematic review of the outcomes on TFCC debridement to demonstrate the effectiveness of debridement for TFCC tears, and to investigate the influence of ulnar variance on outcomes and further surgeries. The evidence obtained from this study can guide surgeons in judging the effectiveness of using only simple TFCC debridement or performing debridement in association with other procedures such as USO initially.
METHODS
Literature Search and Criteria
We performed a literature review of articles related to TFCC debridement according the Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines.17 We used PubMed, Embase.com, and MEDLINE (Ovid) databases for our literature search. We used the key words “The triangular fibrocartilage complex”, “TFCC debridement”, "TFCC tear", and "ulnar impaction syndrome" for our search. Study selection was conducted in a stepwise manner, by title, abstract, and full-text review according to the predetermined inclusion and exclusion criteria (Table 1). We did not impose any limits on the language of articles. If outcomes of arthroscopic TFCC debridement were presented separately, we included those studies even though they presented outcomes of other procedures. Two reviewers performed the study selection (TS, and SM), and any discrepancies on article inclusion were resolved with discussion and further review. We also evaluated the outcome level of each selected article.
Table 1.
Predetermined Inclusion and Exclusion Criteria for Eligible studies
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
| |
| Human studies | Animal or cadaveric studies |
|
| |
| Primary data | Review, technique paper |
|
| |
| Studies that included patients treated with only arthroscopic debridement | Studies that included patients who had unstable DRUJ |
|
| |
| Studies that included patients with concomitant interosseous ligament injuries such as LT ligament tears | Studies that included patients who had distal radial fractures |
|
| |
| Studies that had only TFCC repair outcome. | |
| Open TFCC debridement | |
TFCC-Triangular Fibrocartilage Complex injuries; DRUJ-Distal Radio-ulna Joint; LT ligament-lunotriquetral ligament
Data Extraction and Analysis
Data extracted from the articles included in our review were as follows: publication year and location, patient demographic data, mean follow-up time, mean time off work, symptom of catching, ulnar side tenderness, history of trauma, worker’s compensation, Palmer classification, methods of diagnosis, ulnar variance, and secondary procedures required after TFCC debridement. We also extracted data on functional outcomes (range of motion, grip strength), PROs, Mayo Modified Wrist Score (MMWS), and return to previous work level. The PROs included the Disabilities of the Arm, Shoulder, and Hand (DASH) score, pain level, and patient satisfaction by asking if they were satisfied or not with the procedure. Pain level was demonstrated by pain visual analogue scale (VAS) such that 0 represented no pain and 10 represented severe pain or categorized as “severe”, “moderate”, “mild”, “incomplete pain relief”, or “none” in each study. Additionally, we analyzed the outcomes classified by type of TFCC tear. Palmer classification categorized TCC tear as two main classes, Class 1: Traumatic lesions and Class 2: Degenerative lesions.18 Class 1 is further divided into subtypes; 1A: central perforation, 1B: peripheral ulnar side tear, 1C: distal disruption, 1D: radial disruption. Although we excluded cases with DRUJ instability, we included all classes in our review. These data were extracted independently by two reviewers (TS and SM) based on a pre-decided format.
Statistical Analysis
Patient demographic data and TFCC related information were weighted based on the number of patients in the study. Mean functional outcomes, PROs, and return to work level were also weighted similarly. We added the range and standard deviations (SDs) of the weighted mean for functional outcomes. Range of motion was reported as degree or percentage compared with the contralateral unaffected side. We performed meta-analysis using R (www.r-project.org) and made funnel plots to assess publication bias. (See Supplemental Digital Content 1, Appendix 1, which shows the Funnel plot for studies included in figure 2, INSERT LINK.) (See Supplemental Digital Content 2, Appendix 2, which shows the Funnel plot for studies included in figure 3, INSERT LINK.) These continuous data were shown as the weighted mean difference or the standardized mean difference. Statistical heterogeneity was quantified using the I2 statistic.
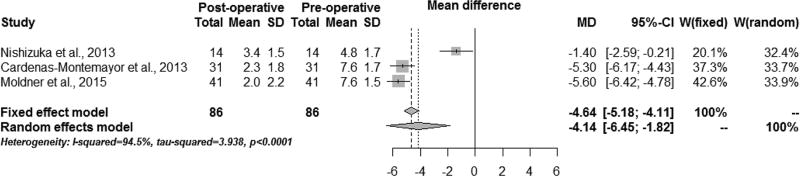
Figure 2. Comparison of the pain-VAS (pre- VS. post-operation).
VAS-visual analogue scale (0–10 scale); SD-standard deviation; MD-mean difference; CI-confidence interval; W-weight
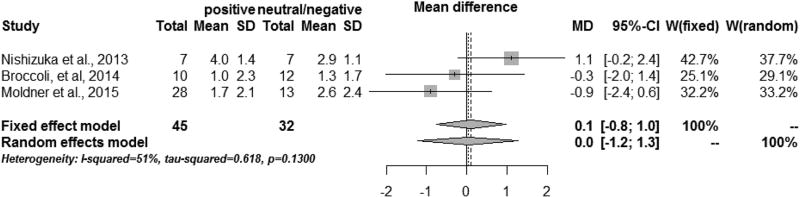
Figure 3. Comparison of the pain-VAS (ulnar positive VS. neutral/negative).
VAS-visual analogue scale (0–10 scale); SD-standard deviation; MD-mean difference; CI-confidence interval; W-weight
RESULTS
Study retrieval and characteristics
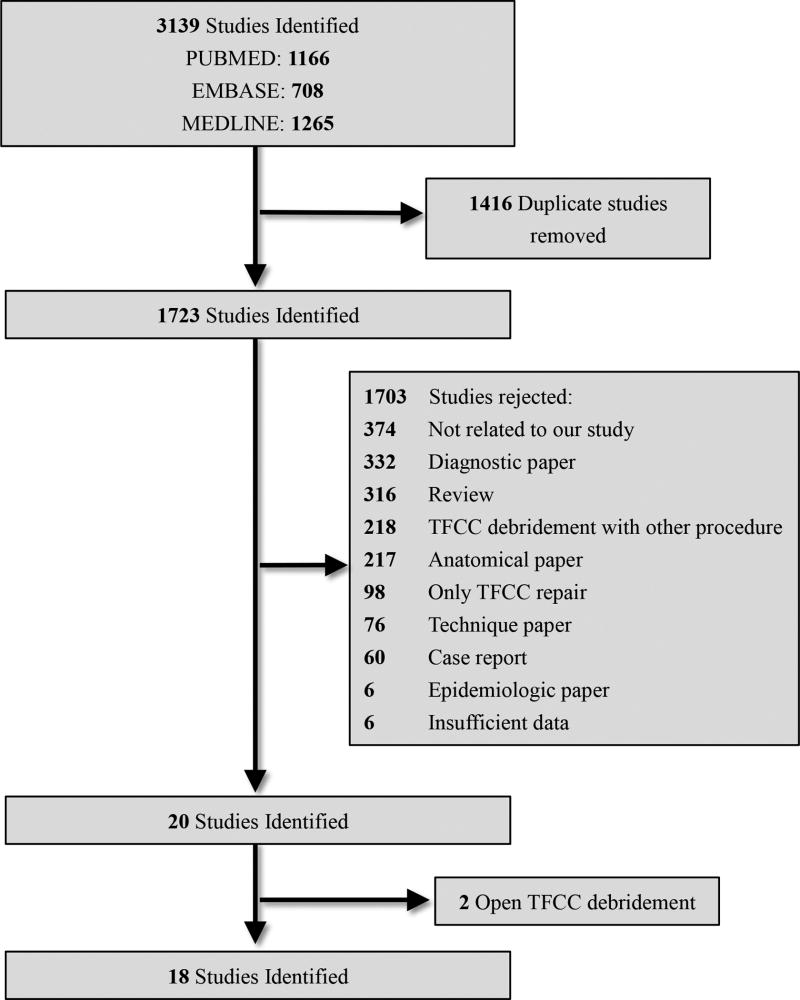
A flow diagram of our database search tree is presented in Figure 1. A total of 1,723 unique studies were identified through the initial search of PUBMED, Embase.com, and MEDLINE (Ovid) databases. Upon further review, 18 articles met our inclusion and exclusion criteria. All of the studies were retrospective with study characteristics shown in Table 2; this review had no study with level-1 evidence.
Figure 1.
Flow diagram of database search for Triangular Fibro Cartilage Complex debridement
Table 2.
Study and Patient Characteristics
| Number | |
|---|---|
|
| |
| Period of study reported (y) | |
|
| |
| 1990–1999 | 5 |
|
| |
| 2000–2009 | 6 |
|
| |
| 2010–2015 | 7 |
|
| |
| Study location | |
|
| |
| North America | 6 |
|
| |
| Europe | 8 |
|
| |
| Asia | 4 |
|
| |
| Patients demographics | |
|
| |
| Mean age (y) | 34 (reported in all studies) |
|
| |
| Mean symptom duration (m) | 8 (reported in 12 of 18 studies) |
|
| |
| Mean follow-up period (m) | 30 (reported in 15 of 18 studies) |
|
| |
| Mean time off work (m) | 4 (reported in 9 of 18 studies) |
|
| |
| TFCC demographics | |
|
| |
| Dominant hand injured (%) | 68 (reported in 10 of 18 studies) |
|
| |
| Symptom of catching (%) | 63 (reported in 6 of 18 studies) |
|
| |
| Ulnar side tenderness (%) | 63 (reported in 7 of 18 studies) |
|
| |
| History of trauma (%) | 84 (reported in 12 of 18 studies) |
|
| |
| Worker’s compensation (%) | 24 (reported in 3 of 18 studies) |
| Palmer classification (%) | (reported in 12 of 18 studies) |
| 1A | 38 |
| 1B | 28 |
| 1C | 4 |
| 1D | 11 |
| II | 19 |
|
| |
| Method for diagnosis (%) | (reported in 16 of 18 studies) |
|
| |
| Arthrography | 28 |
|
| |
| MRI | 35 |
|
| |
| Intra-operative findings | 37 |
y-year; m-months; MRI- magnetic resonance imaging
Patient and TFCC characteristics
Mean follow-up period was 30 months (15 studies) with a range of 17 to 39 months. (Table 2) All patients in this review had stable DRUJs and received conservative treatment including rest with cast, anti-inflammatory agents, or physiotherapy for at least 6 weeks before they underwent TFCC debridement. Arthrography (28%) was used to confirm the diagnosis and type of TFCC tear in suspected cases after physical examination.5,6,16,19,20 Several studies included in this review used magnetic resonance imaging (MRI, 35%) to diagnose TFCC tear before performing arthroscopies.13,15,21–24 However, the exact reason for MRI use was not reported in those studies.
Functional outcomes
The mean pre-operative extension/flexion arc was 120° ± 3° with a range of 118°–122°13,15 and the mean pre-operative pronosupination arc was 140° ± 14° with a range of 132°–152°.13,15 (Table 3) The pre-operative radioulnar deviation was 43° (ones study).13 The mean post-operative extension/flexion arc was 146° ± 18° with a range of 117°–163°,7,12,13,15,22,25 the mean post-operative pronosupination arc was 161° ± 11° with a range of 152°–178°7,12,13,15,22, and the mean post-operative radioulnar deviation arc was 53° ± 5° with a range of 46°–58°.7,12,13,19,22 These radioulnar deviation data are inclusive of all studies that presented post-operative arc of motion. Mean post-operative extension/flexion arc and pronosupination arc from the studies that reported both pre- and post-operative arc of motion data were 136° ± 6° with a range of 132°–140° and 162° ± 13° with a range of 152°–171°, respectively. The mean pre- and post-operative grip strengths were 66% ± 3% with a range of 64%–69% and 91% ± 6% with a range of 74%–97% of the contralateral side, respectively.7,12–15,19,22,26–28
Table 3.
Summary of Functional Outcomes
| Range of Motion (Degree or %*) | Grip Strength (%*) | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-Operative | Post-Operative | Pre- Operative |
Post- Operative |
|||||
| Study | Extension- Flexion |
Pronation- Supination |
Radial- Ulnar Deviation |
Extension- Flexion |
Pronation- Supination |
Radial- Ulnar Deviation |
||
| Cooney, 1993 | N/A | N/A | N/A | 117 | N/A | 46 | 69 | N/A |
| Husby et al., 2001 | N/A | N/A | N/A | 94% | 100% | 96% | N/A | 95 |
| Blackwell et al., 2001 | N/A | N/A | N/A | 83.5% | 96% | 82% | N/A | 91 |
| Miwa et al., 2004 | N/A | N/A | N/A | 90% | 88% | 88% | N/A | 88 |
| Darlis et al., 2005 | 118 | 132 | 43 | 132 | 153 | 48 | 64 | 83 |
| Infanger et al., 2009 | N/A | N/A | N/A | 163 | 152 | 58 | N/A | 93 |
| Garcia-Lopez et al., 2012 | N/A | N/A | N/A | 92% | 97% | N/A | N/A | N/A |
| Nishizuka et al., 2013 | 122 | 152 | N/A | 140 | 171 | N/A | 69 | 74 |
| Cardenas-Montemayor et al., 2013 | N/A | N/A | N/A | 147 (99%) | 178 (99%) | 50 (95%) | N/A | 97 |
| Broccoli, et al., 2014 | N/A | N/A | N/A | 92.3% | N/A | N/A | N/A | 78.6 |
| Moldner et al., 2015 | N/A | N/A | N/A | 122 (96%) | 164 (100%) | 48 (100%) | N/A | 96 |
| Mean ± SD | 120± 3 | 140 ± 14 | 43 | 146 ± 18 (136 ± 6§) (92%) | 161 ± 11 (162± 13§) (96%) | 53 ± 5 (92%) | 66 ± 3 | 91 ± 6 |
“%” means a percentage, normalized to measurements taken on the unaffected side; N/A-not available; SD- standard deviation;
Mean data were calculated from the data that showed pre-operative arc of motion.
Patient-reported outcome
The mean pre- and post-operative DASH scores were 39 and 18, respectively (6 studies).7,12,21,22,28,29 (Table 4) Post TFCC debridement, DASH scores reduced by half indicating less pain and less disability. Seventy one percent of patients (307 of 432) reported “none or slight” pain, 40% of patients (57 of 142) reported “mild or moderate” pain, 1 % of patients (2 of 142) reported “severe” pain. Categories of pain evaluation were not consistent across the inclusive studies in our review. A few studies used all categories, such as, “severe”, “mild or moderate”, “none or slight pain”, however some studies only presented pain outcome with few categories such as “severe” and “none or slight pain”.
Table 4.
Summary of Patient-Reported Outcomes
| DASH | pain | Pain-VAS | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Author | Pre- operative |
Post- operative |
Pre- operative (%*) |
Post- operative (%*) |
Pre- operative |
Post- operative |
Patient's satisfaction (%*) |
|
| |||||||
| Osterman, 1990 | N/A | N/A | Constant: 5 | Worse: 5 | N/A | N/A | 88 |
| Present: 7 | No change: 10 | ||||||
| Intermittent: 86 | Intermittent: 12 | ||||||
| None: 2 | None: 73 | ||||||
|
| |||||||
| Cooney, 1993 | N/A | N/A | N/A | No change: 33 | N/A | N/A | N/A |
|
| |||||||
| De Smet et al, 1996 | N/A | N/A | N/A | N/A | N/A | N/A | 46 |
|
| |||||||
| Minami et al, 1996 | N/A | N/A | Severe: 13 | Severe: 6 | N/A | N/A | 81 |
| Moderate: 31 | Moderate: 12 | ||||||
| Mild: 56 | Slight: 50 | ||||||
| None: 31 | |||||||
|
| |||||||
| Husby et al., 2001 | N/A | N/A | N/A | No change: 14 | N/A | 2.9 | 94 |
| Mild: 23 | |||||||
| Slight: 40 | |||||||
| None: 23 | |||||||
|
| |||||||
| Blackwell et al., 2001 | N/A | N/A | N/A | Mild or None: 79 | N/A | N/A | 75 |
|
| |||||||
| Miwa et al., 2004 | N/A | N/A | N/A | Severe: 9 | N/A | N/A | 97 |
| Mild: 45.5 | |||||||
| Slight or None: 45.5 | |||||||
|
| |||||||
| Darlis et al., 2005 | N/A | N/A | N/A | No change: 15 | Rest: 6.0 | Rest: 2.7 | N/A |
| Pain relief: 85 | Normal activity: 7.8 | Normal activity: 3.8 | |||||
| Heavy work: 8.5 | Heavy work: 5.2 | ||||||
|
| |||||||
| McAdams et al, 2009 | 43.2 ± 17.3 | 0 | N/A | N/A | N/A | N/A | N/A |
|
| |||||||
| Infanger et al., 2009 | N/A | 12 | N/A | 1A | N/A | N/A | N/A |
| Severe: 0 | |||||||
| Moderate: 7 | |||||||
| Mild: 12 | |||||||
| None: 81 | |||||||
| 1B | |||||||
| Severe: 0 | |||||||
| Moderate: 22 | |||||||
| Mild: 22 | |||||||
| None: 56 | |||||||
| 1C | |||||||
| Severe: 0 | |||||||
| Moderate: 0 | |||||||
| Mild: 25 | |||||||
| None: 75 | |||||||
| 1D | |||||||
| Severe 0 | |||||||
| Moderate: 17 | |||||||
| Mild: 17 | |||||||
| None: 66 | |||||||
|
| |||||||
| Tan et al, 2012 | N/A | N/A | N/A | Servere: 0 | N/A | N/A | N/A |
| Moderate: 25 | |||||||
| Mild occasional: 33 | |||||||
| None: 42 | |||||||
|
| |||||||
| Garcia-Lopez et al., 2012 | N/A | N/A | N/A | No change: 4.9 | N/A | N/A | N/A |
| Incomplete pain relief: 14.8 | |||||||
| None: 80.3 | |||||||
|
| |||||||
| Nishizuka et al., 2013 | N/A | N/A | N/A | N/A | 4.8 | 3.4 | N/A |
|
| |||||||
| Cardenas-Montemayor et al., 2013 | N/A | 17.0 | N/A | N/A | 7.6 | 2.3 | N/A |
|
| |||||||
| De Smet et al, 2014 | 42 | 25 | N/A | N/A | N/A | 4.6 | N/A |
|
| |||||||
| Broccoli, et al., 2014 | N/A | 30.2 | N/A | N/A | N/A | 1.2 | N/A |
|
| |||||||
| Moldner et al., 2015 | N/A | 18 | N/A | N/A | 7.6 | 2.0 | N/A |
|
| |||||||
| Mean | 39 | 18 | 7 | 3 | 84 | ||
“%” means a percentage of all patients in each study; VAS-visual analogue scale (0–10 scale); N/A-not available; DASH-the Disabilities of the Arm, Shoulder, and Hand
The mean pre-operative and post-operative VAS of pain were 7 points and 3 points, respectively. Overall, 84% of patients were satisfied with their treatment and subsequent quality of life (6 studies).5,6,14,16,26,27 We also compared the pain-VAS between pre- and post-operative times among 3 studies using meta-analysis (Figure 2)7,12,15. The pain VAS decreased significantly after debridement [Mean difference (MD): – 4.14, 95% confidence interval (CI): −6.45 to −1.82 (random effects model), I2= 94.5%, and Tau 2 =3.938].
Clinical results
Clinical results were categorized according to MMWS, 13,20,23,26 Minami’s criteria, 14,16 Modified Green O’Brien (MGO) criteria,27 or DASH score.22 (Table 5) Eighty seven percent (222/255) of patients were in “good to excellent”, nine percent of patients were in “fair” (22/255), and four percent of patients were in “poor” categories. In this calculation, “very good” was accounted as “excellent” category.
Table 5.
Summary of Clinical Outcome
| Author | Clinical Outcome (%*) |
|---|---|
|
| |
| Osterman, 1990 | Failure: 5/42 (11.9) |
|
| |
| Minami et al, 1996 | Minami’s criteria |
| Excellent: 13/16 (81.2) | |
| Fair: 2/16 (12.5) | |
| Poor: 1/16 (6.3) | |
|
| |
| Westkaemper et al, 1998 | MMWS |
| Excellent: 13/28 (46.4) | |
| Good: 8/28 (28.6) | |
| Fair: 2/28 (7.1) | |
| Poor: 5/28 (17.9) | |
|
| |
| Husby et al., 2001 | MMWS |
| Excellent: 13/32 (40.6) | |
| Good: 14/32 (43.8) | |
| Fair: 4/32 (12.5) | |
| Poor: 1/32 (3.1) | |
|
| |
| Blackwell et al., 2001 | MGO criteria |
| Good to Excellent: 19/27 (70.4) | |
| Fair: 6/27 (22.2) | |
| Poor: 2/27 (7.4) | |
|
| |
| Miwa et al., 2004 | Minami’s criteria |
| Excellent: 16/29 (55.2) | |
| Good: 10/29 (34.5) | |
| Fair: 2/29 (6.9) | |
| Poor: 1/29 (3.4) | |
|
| |
| Darlis et al., 2005 | MMWS |
| Excellent: 10/20 (50.0) | |
| Good: 7/20 (35.0) | |
| Fair: 3/20 (15.0) | |
| Poor: 0/20 (0) | |
|
| |
| Infanger et al., 2009 | DASH |
| Very good: 60/79 (75.9) | |
| Good: 19/79 (24.0) | |
| poor: 0/79 (0) | |
|
| |
| Tan et al, 2012 | MMWS |
| Excellent: 12/24 (50.0) | |
| Good: 8/24 (33.3) | |
| Fair: 3/24 (12.5) | |
| Poor: 1/24 (4.2) | |
|
| |
| Mean | Good to Excellent: 222/255 (87) |
| Fair: 22/255 (9) | |
| Poor: 11/255 (4) | |
“%” means a percentage of all patients in each study; DASH-the Disabilities of the Arm, Shoulder, and Hand; MMWS-Mayo Modified Wrist Score
Return to work level
The mean time off work post TFCC debridement was 4 months in nine studies.5,16,21–24,26,27,29 (Table 6) A mean of 87% patients returned to their previous work after TFCC debridement (13 studies).5,12–14,16,19,21–24,26,27,29 The rate of return to original work was low (mean weighted value based on the number of patients: 19%) in the studies with a high rate of worker’s compensation (mean weighted value: 94%).24,27 On the other hand, the rate of return to work was high (mean weighted value: 97%) in the studies with low worker’s compensation rate (mean weighted value: 12%).14,23
Table 6.
Summary of Return to Work’s Level
| Author | Time off work (m) | Return to Work (%*) |
Worker’s compensation (%*) |
|---|---|---|---|
|
| |||
| Osterman, 1990 | 3.2 | Original work: 60 | N/A |
| Sports related: 1.5 | |||
|
| |||
| Cooney, 1993 | N/A | Work: 66.6 | N/A |
|
| |||
| Minami et al, 1996 | Sports related: 1.5 | Original work: 81 | N/A |
|
| |||
| Husby et al., 2001 | 1.3 | Full time work: 89 | N/A |
|
| |||
| Blackwell et al., 2001 | 5 | Original work: 88 | 65 |
| (WC/non-WC: 5.6/3.8) | Minor restriction: 25 | ||
|
| |||
| Miwa et al., 2004 | N/A | Original work: 100 | 19 |
|
| |||
| Darlis et al., 2005 | N/A | Original work: 55 | N/A |
| Lighter work: 25 | |||
|
| |||
| McAdams et al, 2009 | 3.7 | Original work: 100 | N/A |
|
| |||
| Infanger et al., 2009 | 3.5 | Original work: 100 | N/A |
|
| |||
| Tan et al, 2012 | 2.6 | Original work: 97 | 6 |
|
| |||
| Garcia-Lopez et al., 2012 | 5.3 | Original work: 87.7 | N/A |
| 1A: 5.1 | Original work (WC): 12.3 | ||
| 1B: 5.1 | Restricted job: 8.6 | ||
| 1C: 6.1 | didn't return: 3.6 | ||
| 1D: 4.5 | |||
| 2A: 8.2 | |||
| 2C: 5.6 | |||
|
| |||
| Cardenas-Montemayor et al., 2013 | N/A | Original work: 78 | N/A |
| Restricted job: 19 | |||
| Able to work but unemployed: 3 | |||
|
| |||
| De Smet et al, 2014 | 5.8 | Original work: 80 | N/A |
|
| |||
| Mean | 4 | Original work: 87 | 24 |
“%” means a percentage of all patients in each study; m-months; N/A-not available; WC-worker’s compensation
Outcomes categorized by Ulnar Variance
Patients with ulnar positive variance reported worse outcomes of satisfaction and MMWS than those of patients with ulnar neutral and negative variance, with 55% and 73% for satisfaction and, 89 and 91 for MMWS scores, respectively (Table 7). 6–8,16,17,25,26 We also assessed a relationship between ulnar variance and type of pathology based on Palmer classification, and further surgeries after TFCC debridement in each study. The Darrach procedure, Sauvé-Kapandji procedure, and ulnar shortening osteotomy were performed as further surgeries in 6 studies (n=26/173). Patients with ulnar positive variance required more subsequent surgeries than cases with ulnar neutral or negative variance [40% (23/58) vs. 3% (1/32)]. We performed a meta-analysis of 3 studies to compare the pain-VAS between the ulnar positive group and ulnar neutral and ulnar negative groups after TFCC debridement (Figure 3).7,15,28 The mean pain-VAS of the ulnar positive group and that of ulnar neutral and negative groups were 1.9 and 2.4, respectively. There were no statistically significant differences between them (MD: 0.0, 95% CI: −1.2 to 1.3 (random effects model), I2 = 51%, and Tau 2 =0.618).
Table 7.
Summary Outcomes Categorized by Ulnar Variance
| Ulnar variance | |||||
|---|---|---|---|---|---|
|
| |||||
| Author | Classification (%) | Mean (mm) |
Outcomes (%) | Palmer classification |
Further surgery (%) |
|
| |||||
| Osterman, 1990 | Positive: 15/52 (29) | N/A | Failure rate | 1A: 46% | Darrach procedure: 1/52 (2) |
| Neutral: 20/52 (39) | Positive: 2/12 (17) | 1B: 20% | USO: 1/52 (2) | ||
| Negative: 17/52 (32) | Neutral: 2/16 (13) | 1D: 34% | |||
| Negative: 1/13 (8) | |||||
|
| |||||
| De Smet et al, 1996 | Positive: 5/13 (38) | N/A | Satisfaction | Sauvé-Kapandji procedure | |
| Neutral: 7/13 (54) | Positive: 3/4 (75) | Positive: 2/5 (40) | |||
| Negative: 1/13 (8) | Neutral: 2/7 (29) | Neutral: 1/7 (14) | |||
| Negative: 1/1 (100) | |||||
|
| |||||
| Minami et al, 1996 | Positive: 5/16 (31) | N/A | Satisfaction | USO | |
| Neutral: 9/16 (56) | Positive: 2/5 (40) | Positive: 2/5 (40) | |||
| Negative: 2/16 (13) | Neutral: 9/9 (100) | ||||
| Negative: 2/2 (100) | |||||
|
| |||||
| Husby et al., 2001 | Positive: 7/35 (20) | N/A | MMWS | 1A: 74% | N/A |
| Neutral: 22/35 (63) | Positive: 90 | 1D: 17% | |||
| Negative: 6/35 (17) | 2C: 6% | ||||
| 2D: 3% | |||||
|
| |||||
| Darlis et al., 2005 | Positive: 1/20 (5) | N/A | N/A | 1A: 70% | USO |
| neutral: 16/20 (80) | 1D: 10% | Positive: 1/1 (100) | |||
| negative: 3/20 (15) | II: 20% | ||||
|
| |||||
| Nishizuka et al., 2013 | Positive: 7/14 (50) | 0.7 | Pain | N/A | |
| Neutral + Negative: 7/14 (50) | Positive: 4.0 | ||||
| Neutral + Negative: 2.8 | |||||
|
| |||||
| Broccoli, et al., 2014 | Positive: 10/22 (45) | N/A | Pain | Palmar 2A, 2C, 2D or 2E | USO |
| Neutral + Negative: 12/22 (55) | Positive: 1.0 | Positive: 9/10 (90) | |||
| Neutral + Negative: 1.3 | Neutral + Negative: 0/12 | ||||
| DASH | |||||
| Positive: 32.3 | |||||
| Neutral + Negative: 28.5 | |||||
| MMWS | |||||
| Positive: 75.0 | |||||
| Neutral + Negative: 78.8 | |||||
|
| |||||
| Moldner et al., 2015 | Positive 37/50(74) | 0.5 (stress view: 1.3) | Pain | 2C: 100% | USO: 9/50 |
| Neutral + negative 13/50(26) | Positive: 1.7 | Positive: 9/37 (24) | |||
| Neutral + Negative: 2.6 | Neutral + Negative: 0/13 | ||||
| DASH | (Mean ulnar variance: 2.4mm) | ||||
| Positive: 17 | |||||
| Neutral + Negative: 20 | |||||
| MMWS | |||||
| Positive: 88 | |||||
| Neutral + Negative: 91 | |||||
USO-Ulnar shortening osteotomy; DO-Debridement only group; UPV-Ulnar positive variance group; DASH-the Disabilities of the Arm, Shoulder, and Hand; MMWS-Mayo Modified Wrist Score
Outcomes categorized by Palmer classification
Six articles reported outcomes including DASH score or pain level categorized by Palmer classification.7,12,14,21,22,28(Table 8) The mean DASH score in class 1A and 1D was lower to that in other class. (class 1A: 0, class 1B: 15, class1D: 0, class 2: 22) Additionally, in class 1A, rate of both excellent clinical outcome (70%) and pain-free rate (81%) were highest after TFCC debridement. No study reported DASH scores in class 1C.
Table 8.
Summary Outcomes Categorized by Palmer classification
| Author | Post-operative outcomes categorized by Palmer classification | ||||
|---|---|---|---|---|---|
|
| |||||
| 1A | 1B | 1C | 1D | 2 | |
|
| |||||
| Miwa et al., 2004 | Clinical outcome | Clinical outcome | Clinical outcome | Clinical outcome | No case |
| Excellent 70% | Excellent 50% | Excellent 50% | Excellent 40% | ||
| good 20% | good 50% | good 38% | good 40% | ||
| fair 10% | fair 0% | fair 13% | fair 0% | ||
| poor 0% | poor 0% | poor 0% | poor 20% | ||
|
| |||||
| McAdams et al, 2009 | DASH 0 | DASH 0 | No case | DASH 0 | No case |
|
| |||||
| Infanger et al., 2009 | Pain level | Pain level | Pain level | Pain level | No case |
| severe 0% | severe 0% | severe 0% | severe 0% | ||
| moderate 7% | moderate 22% | moderate 0% | moderate 17% | ||
| mild 12% | mild 22% | mild 25% | mild 17% | ||
| none 81% | none 56% | none 75% | none 66% | ||
|
| |||||
| Cardenas-Montemayor et al., 2013 | No case | DASH 17 Pain-VAS 2.3 | No case | No case | No case |
|
| |||||
| Broccoli, et al., 2014 | No case | No case | No case | No case | DASH 30.2 Pain-VAS 1.2 |
|
| |||||
| Moldner et al., 2015 | No case | No case | No case | No case | DASH 18 Pain-VAS 2.0 |
VAS-visual analogue scale (0–10 scale); DASH-the Disabilities of the Arm, Shoulder, and Hand
Complications
Five studies reported no complications after TFCC debridement,7,13,14,21,22 whereas four studies reported complications.16,23,24,27 (table 9) Overall, 2% (11/456) of all the patients had complications in studies that mentioned complications. One percent (4/456) of patients had dorsal ulnar sensory symptoms.16,23 Deep infection and portal problem was reported in 0.2% (1/456) and 1% (6/456) of all the studies, respectively.24,27.
Table. 9.
Summary of Complications
| Author | Complication (affected / total) |
|---|---|
| Minami et al, 1996 | Dorsal ulnar sensory symptoms (2/16) |
| Blackwell et al., 2001 | Deep infection (1/35) |
| Tan et al, 2012 | Dorsal ulnar sensory symptoms (2/68) |
| Garcia-Lopez et al., 2012 | Portal problem (burns, painful scar) (6/162) |
DISCUSSION
Patients reported reduced pain and improved PROs with TFCC debridement in our review. Debridement also achieved good postoperative arc of motion and a mean of 91% of the grip strength compared to the unaffected side among the 550 patients evaluated in our review.
Overall time to return to work in our review was about 4 months, and 87% of patients returned to original work. Patients who did not return to original work performed heavy manual labor or repeated assembly line work,5,16 and wrist pain was the primary reason for unemployment in those patients.27 Our study also found that the group with a low rate of worker’s compensation resulted in a high rate of return to original work, whereas the group with high rate of worker’s compensation resulted in a low rate of return to original work.14,23,24,27 Blackwell et al. reported that patients without workers’ compensation (WC) were reinstated faster, and that pain relief, wrist score, and most objective measures of hand function of these patients were better than those of WC patients.27 These outcomes may result in submaximal effort by some WC patients during their functional rehabilitation.
Our review showed a positive correlation between positive ulnar variance and degenerative lesions, especially degenerative central perforation similar to earlier studies.30,31 The ratio of patients with positive ulnar variance that included only degenerative wear was higher than the ratios in other studies.7,28 However, ulnar impaction syndrome can also develop in wrists with ulnar neutral or negative variance32, and USO has been recommended in wrists with ulnar neutral and negative variance recently.33 Because a posture of forearm pronation or grip can make dynamic increases in ulnar variance34, and wrists with ulnar neutral or negative variance may become ulnar positive variance owing to this dynamic increase. An inverse relationship between ulnar variance and triangular fibrocartilage complex thickness can be also one of the reasons.35 In our review, further surgery was required in 31% of patients with ulnar positive variance and 1% of patients with neutral or negative variance. However, not every patient with ulnar positive variance needs further surgery. Moldner et al. demonstrated that the parameters measured preoperatively, such as ulnar variance and pain level, do not predict the need for initial USO.7 However, in our review the overall pain level improved postoperatively and was not significantly different between the ulnar positive group and the ulnar negative or neutral group. This demonstrates that TFCC debridement can improve wrist pain regardless of ulnar variance. Resection of unstable TFCC flap or synovectomy via debridement may relieve pain. Palmer and Werner have demonstrated that about 20 % of forearm axial load is transferred from the carpus to the ulna through the TFCC in the neutral ulnar variant wrist and that the axial load decreases to about 6% by resection of the TFCC.36 This change also may improve ulnar sided wrist pain. Considering these results, simultaneous USO with TFCC debridement may not be desirable even for ulnar positive variance cases.
In patients with central TFCC perforation (class 1A) included our review, the mean DASH was 0 (indicating no disability), 81% patients had no pain after treatment, and 70% of patients achieved excellent clinical outcomes in Minami’s criteria. These outcomes were superior to outcomes in other TFCC injury types; therefore, TFCC debridement is ideal for a central TFCC perforation.
Arthroscopic repair is often used to treat ulnar side tears. Postoperative pain VAS was 2.3 in the TFCC repair group, and 3.4 in the TFCC debridement group. Grip strength improved better with TFCC repair than TFCC debridement. Other study also showed that TFCC repair could improve DASH scores from 51 to 0 for patients with ulnar side TFCC tear. Miwa et al. reported that 91% of patients who had TFCC repair for ulnar side tear got an excellent or good result in Minami’s criteria. These outcomes supported that arthroscopic repair is a suitable treatment for ulnar side tears.
In our review, few patients had complications such as ulnar sensory symptoms or pain scars with arthroscopic TFCC debridement.16,23,24,27 Conversely, Rajgopal et al. reported that more than 20% of patients had delayed union or nonunion and that 45% required hardware removal because of plate irritation.37 Chan et al. also noted a high risk of plate irritation (51%).38 These high complication rates of USO can support our recommendation that USO can be used only for recalcitrant cases after arthroscopic debridement.
Our review has some limitations owing to the quality of evidence in available literature. The first limitation is that many studies reported only post-operative data for outcomes. Therefore, we could not perform statistical analysis for these outcomes and we could not conduct a meta-analysis with enough number of papers. Our meta-analyses related to pain included only three papers. Therefore, we could not perform further analyses in sub-groups although heterogeneity was high in figure 2. Additionally, funnel plots showed the possibility of publication bias. (See Supplemental Digital Content 1, INSERT LINK.) (See Supplemental Digital Content 2, INSERT LINK.) All three studies in our meta-analysis showed the same direction and the meta-analysis revealed that TFCC debridement can improve pain. However, we have to be careful that the high heterogeneity and publication bias made the impact of this outcome weak. The second limitation is that the literature in our review included cases with concomitant interosseous ligament injuries such as lunotriquetral (LT) ligament tears. Studies have not presented the results of patients with ligament injuries separately; therefore, we could not exclude those studies. However, only 6% patients in our review had LT ligament tears, owing to which, the effect of these cases on our overall results is minimal. The mean follow up period in our review was 30 months, with the longest follow up period being 39 months.24 Accordingly, we could not assess a long-term effect of TFCC debridement. All studies included in this review were uncontrolled case series. Therefore, our conclusions may be prone to publication bias that favors positive results. The readers do have to consider this bias in interpreting our study outcomes.
In this literature review, patients reported reduced pain, improved functional outcomes, and PROs after debridement of TFCC tears. However, a causal relationship cannot be determined due to the lack of nonoperative controls in the included studies. Though some of these cases may require a secondary procedure, simple debridement without USO can be performed for cases with any type of ulnar variance. TFCC debridement also enabled most patients return to original work and was performed safely with few complications.
Supplementary Material
Supplemental Digital Content 1, Appendix 1 shows the Funnel plot for studies included in figure 2, INSERT LINK.
Supplemental Digital Content 2, Appendix 2 shows the Funnel plot for studies included in figure 3, INSERT LINK.
Acknowledgments
Author’s role
Taichi Saito: study design, data extraction, data analysis, manuscript preparation
Sunitha Malay: study design, data extraction, manuscript preparation
Kevin C. Chung: study design, manuscript review
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number 2 K24-AR053120-06. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
We like to thank Lin Zhong and Ting-Ting Chung, research analysts, for her help with the data analysis.
References
- 1.Chan JJ, Teunis T, Ring D. Prevalence of Triangular Fibrocartilage Complex Abnormalities Regardless of Symptoms Rise With Age: Systematic Review and Pooled Analysis. Clinical Orthopaedics and Related Research. 2014;472:3987–3994. doi: 10.1007/s11999-014-3825-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atzei A, Luchetti R, Braidotti F. Arthroscopic foveal repair of the triangular fibrocartilage complex. J Wrist Surg. 2015;4:22–30. doi: 10.1055/s-0035-1544226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sachar K. Ulnar-Sided Wrist Pain: Evaluation and Treatment of Triangular Fibrocartilage Complex Tears, Ulnocarpal Impaction Syndrome, and Lunotriquetral Ligament Tears. The Journal of Hand Surgery. 2008;33:1669–1679. doi: 10.1016/j.jhsa.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 4.Park MJ, Jagadish A, Yao J. The Rate of Triangular Fibrocartilage Injuries Requiring Surgical Intervention. Orthopedics. 2010 doi: 10.3928/01477447-20100924-03. [DOI] [PubMed] [Google Scholar]
- 5.Osterman AL. Arthroscopic debridement of triangular fibrocartilage complex tears. Arthroscopy. 1990;6:120–124. doi: 10.1016/0749-8063(90)90012-3. [DOI] [PubMed] [Google Scholar]
- 6.De Smet L, De Ferm A, Steenwerckx A, Dauwe D, Zachee B, Fabry G. Arthroscopic treatment of triangular fibrocartilage complex lesions of the wrist. Acta Orthop Belg. 1996;62:8–13. [PubMed] [Google Scholar]
- 7.Moldner M, Unglaub F, Hahn P, Muller LP, Bruckner T, Spies CK. Functionality after arthroscopic debridement of central triangular fibrocartilage tears with central perforations. J Hand Surg. Am. 2015;40:252–258. e252. doi: 10.1016/j.jhsa.2014.10.056. [DOI] [PubMed] [Google Scholar]
- 8.Cooney WP, Linscheid RL, Dobyns JH. Triangular fibrocartilage tears. The Journal of Hand Surgery. 1994;19:143–154. doi: 10.1016/0363-5023(94)90238-0. [DOI] [PubMed] [Google Scholar]
- 9.Trumble TE, Gilbert M, Vedder N. Arthroscopic repair of the triangular fibrocartilage complex. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 1996;12:588–597. doi: 10.1016/s0749-8063(96)90199-1. [DOI] [PubMed] [Google Scholar]
- 10.Haugstvedt JR, Husby T. Results of repair of peripheral tears in the triangular fibrocartilage complex using an arthroscopic suture technique. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery. 1999;33:439–447. doi: 10.1080/02844319950159172. [DOI] [PubMed] [Google Scholar]
- 11.Bohringer G, Schadel-Hopfner M, Petermann J, Gotzen L. A method for all-inside arthroscopic repair of Palmer 1B triangular fibrocartilage complex tears. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2002;18:211–213. doi: 10.1053/jars.2002.30445. [DOI] [PubMed] [Google Scholar]
- 12.Cardenas-Montemayor E, Hartl JF, Wolf MB, et al. Subjective and objective results of arthroscopic debridement of ulnar-sided TFCC (Palmer type 1B) lesions with stable distal radio-ulnar joint. Arch Orthop Trauma Surg. 2013;133:287–293. doi: 10.1007/s00402-012-1643-z. [DOI] [PubMed] [Google Scholar]
- 13.Darlis NA, Weiser RW, Sotereanos DG. Arthroscopic triangular fibrocartilage complex debridement using radiofrequency probes. J Hand Surg. Br. 2005;30:638–642. doi: 10.1016/j.jhsb.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 14.Miwa H, Hashizume H, Fujiwara K, Nishida K, Inoue H. Arthroscopic surgery for traumatic triangular fibrocartilage complex injury. J Orthop Sci. 2004;9:354–359. doi: 10.1007/s00776-004-0796-1. [DOI] [PubMed] [Google Scholar]
- 15.Nishizuka T, Tatebe M, Hirata H, Shinohara T, Yamamoto M, Iwatsuki K. Simple debridement has little useful value on the clinical course of recalcitrant ulnar wrist pain. Bone Joint J. 2013;95-B:1687–1696. doi: 10.1302/0301-620X.95B12.31918. [DOI] [PubMed] [Google Scholar]
- 16.Minami A, Ishikawa J, Suenaga N, Kasashima T. Clinical results of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg. Am. 1996;21:406–411. doi: 10.1016/s0363-5023(96)80353-4. [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 18.Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg. Am. 1989;14:594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 19.Cooney WP. Evaluation of chronic wrist pain by arthrography, arthroscopy, and arthrotomy. J Hand Surg. Am. 1993;18:815–822. doi: 10.1016/0363-5023(93)90047-7. [DOI] [PubMed] [Google Scholar]
- 20.Westkaemper JG, Mitsionis G, Giannakopoulos PN, Sotereanos DG. Wrist arthroscopy for the treatment of ligament and triangular fibrocartilage complex injuries. Arthroscopy. 1998;14:479–483. doi: 10.1016/s0749-8063(98)70075-1. [DOI] [PubMed] [Google Scholar]
- 21.McAdams TR, Swan J, Yao J. Arthroscopic treatment of triangular fibrocartilage wrist injuries in the athlete. Am J Sports Med. 2009;37:291–297. doi: 10.1177/0363546508325921. [DOI] [PubMed] [Google Scholar]
- 22.Infanger M, Grimm D. Meniscus and discus lesions of triangular fibrocartilage complex (TFCC): treatment by laser-assisted wrist arthroscopy. J Plast Reconstr Aesthet Surg. 2009;62:466–471. doi: 10.1016/j.bjps.2007.02.035. [DOI] [PubMed] [Google Scholar]
- 23.Tan SW, Ng SW, Tan SH, Teoh LC. Arthroscopic debridement of intercarpal ligament and triangular fibrocartilage complex tears. Singapore Med J. 2012;53:188–191. [PubMed] [Google Scholar]
- 24.Garcia-Lopez I, Delgado PJ, Abad JM, De Lucas FG. Thermal energy for the arthroscopic treatment of tears of the triangular fibrocartilage of the wrist. Acta Orthopaedica Belgica. 2012;78:719–723. [PubMed] [Google Scholar]
- 25.Cooney WP, Linscheid RL, Dobyns JH. Triangular fibrocartilage tears. J Hand Surg. Am. 1994;19:143–154. doi: 10.1016/0363-5023(94)90238-0. [DOI] [PubMed] [Google Scholar]
- 26.Husby T, Haugstvedt JR. Long-term results after arthroscopic resection of lesions of the triangular fibrocartilage complex. Scand J Plast Reconstr Surg Hand Surg. 2001;35:79–83. doi: 10.1080/02844310151032655. [DOI] [PubMed] [Google Scholar]
- 27.Blackwell RE, Jemison DM, Foy BD. The holmium:yttrium-aluminum-garnet laser in wrist arthroscopy: a five-year experience in the treatment of central triangular fibrocartilage complex tears by partial excision. J Hand Surg. Am. 2001;26:77–84. doi: 10.1053/jhsu.2001.20157. [DOI] [PubMed] [Google Scholar]
- 28.Broccoli G, Vaske B, Muller L, Kahmann R, Isenberg J. Limits to arthroscopic treatment of degenerative triangular fibrocartilage complex lesions depending on the ulnar variance. Handchir Mikrochir Plast Chir. 2014;46:151–162. doi: 10.1055/s-0034-1371851. [DOI] [PubMed] [Google Scholar]
- 29.De Smet L, Van Nuffel M, Koorneef P, Degreef I. Arthroscopic debridement with and without distal ulnar resection in the treatment of triangular fibrocartilage complex tears. Acta Orthop Belg. 2014;80:112–115. [PubMed] [Google Scholar]
- 30.Unglaub F, Wolf MB, Thome MA, Germann G, Sauerbier M, Reiter A. Correlation of ulnar length and apoptotic cell death in degenerative lesions of the triangular fibrocartilage. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2008;24:299–304. doi: 10.1016/j.arthro.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 31.Unglaub F, Thomas SB, Kroeber MW, et al. Apoptotic Pathways in Degenerative Disk Lesions in the Wrist. Arthroscopy-the Journal of Arthroscopic and Related Surgery. 2009;25:1380–1386. doi: 10.1016/j.arthro.2009.04.071. [DOI] [PubMed] [Google Scholar]
- 32.Tomaino MM. Results of the wafer procedure for ulnar impaction syndrome in the ulnar negative and neutral wrist. J Hand Surg. Br. 1999;24:671–675. doi: 10.1054/jhsb.1999.0268. [DOI] [PubMed] [Google Scholar]
- 33.Tatebe M, Nakamura R, Horii E, Nakao E. Results of ulnar shortening osteotomy for ulnocarpal impaction syndrome in wrists with neutral or negative ulnar variance. J Hand Surg. Br. 2005;30:129–132. doi: 10.1016/j.jhsb.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 34.Friedman SL, Palmer AK, Short WH, Levinsohn EM, Halperin LS. The change in ulnar variance with grip. J Hand Surg. Am. 1993;18:713–716. doi: 10.1016/0363-5023(93)90325-w. [DOI] [PubMed] [Google Scholar]
- 35.Palmer AK, Glisson RR, Werner FW. Relationship between ulnar variance and triangular fibrocartilage complex thickness. J Hand Surg. Am. 1984;9:681–682. doi: 10.1016/s0363-5023(84)80013-1. [DOI] [PubMed] [Google Scholar]
- 36.Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984:26–35. [PubMed] [Google Scholar]
- 37.Rajgopal R, Roth J, King G, Faber K, Grewal R. Outcomes and complications of ulnar shortening osteotomy: an institutional review. Hand. 2015;10:535–540. doi: 10.1007/s11552-014-9727-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chan SK, Singh T, Pinder R, Tan S, Craigen MA. Ulnar Shortening Osteotomy: Are Complications Under Reported? Journal of Hand and Microsurgery. 2015;7:276–282. doi: 10.1007/s12593-015-0201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1, Appendix 1 shows the Funnel plot for studies included in figure 2, INSERT LINK.
Supplemental Digital Content 2, Appendix 2 shows the Funnel plot for studies included in figure 3, INSERT LINK.