Abstract
Serum uric acid (SUA), a causative agent for gout among others, is affected by both genetic and dietary factors, perhaps differentially by sex. We evaluated cross-sectional (SUAbase) and longitudinal (SUArate) associations of SUA with a genetic risk score (GRS), diet and sex. We then tested the interactive effect of GRS, diet and sex on SUA. Longitudinal data on 766 African-American urban adults participating in the Healthy Aging in Neighborhood of Diversity across the Lifespan study were used. In all, three GRS for SUA were created from known SUA-associated SNP (GRSbase (n 12 SNP), GRSrate (n 3 SNP) and GRStotal (n 15 SNP)). Dietary factors included added sugar, total alcohol, red meat, total fish, legumes, dairy products, caffeine and vitamin C. Mixed-effects linear regression models were conducted. SUAbase was higher among men compared with that among women, and increased with GRStotal tertiles. SUArate was positively associated with legume intake in women (γ = + 014; 95% CI +0.06, +0.22, P = 0.001) and inversely related to dairy product intake in both sexes combined (γ = −0.042; 95% CI −0.075, −0.009), P = 0.010). SUAbase was directly linked to alcohol consumption among women (γ = +0.154; 95% CI +0.046, +0.262, P = 0.005). GRSrate was linearly related to SUArate only among men. Legume consumption was also positively associated with SUArate within the GRStotal's lowest tertile. Among women, a synergistic interaction was observed between GRSrate and red meat intake in association with SUArate. Among men, a synergistic interaction between low vitamin C and genetic risk was found. In sum, sex–diet, sex–gene and gene–diet interactions were detected in determining SUA. Further similar studies are needed to replicate our findings.
Keywords: Serum uric acid, Diets, Genetic risk scores, African-Americans, Urban adults
Uric acid (UA), the final catabolic product of purine oxidation, is the causative agent of gout, characterised by urate crystal deposition in joints and elevated serum uric acid (SUA) or hyperuricaemia(1). Gout affects 6–8% of the elderly (>80 years) and approximately 3.9% of the entire US population(2). Moreover, hyperuricaemia independently predicts myocardial infarction and premature death(3). Two key physiological mechanisms determining hyperuricaemia are increased liver production of urate from dietary and endogenous substrates that raise purine levels, and reduced renal and gut excretion of UA(4). Thus, uncovering a genetic basis for both mechanisms might elucidate the aetiological factors behind gout. Recent genome-wide association studies (GWAS) have identified various genetic loci with the strongest influences on SUA such as ATP binding cassette subfamily G member 2 (ABCG2), sodium/phosphate cotransporter 4 (NPT4) (solute carrier family 17 (organic anion transporter), member 3), NPT1 (solute carrier family 17 (organic anion transporter), member 1 (SLC17A1)), solute carrier family 22 (organic anion/urate transporter), member 12 (URAT1) (solute carrier family 22 (organic anion/urate transporter), member 12 (SLC22A12)), organic anion uptake transporter 4 (OAT4) (solute carrier family 22 (organic anion/urate transporter), member 11) and GLUT9 (solute carrier family 2 (facilitated GLUT), member 9 (SLC2A9))(2) However, no study thus far has compiled all recently identified SNP into a genetic risk score (GRS) for SUA in a longitudinal study of African-American (AA) adults. Moreover, the sex-specific effect of this GRS is yet to be uncovered.
Although genetics has a strong influence on SUA, dietary factors including the Mediterranean Diet Score(5,6) and specific components may have equally important effects(2). On the basis of recent data(1,7–12), it is hypothesised that red meat and seafood consumption are linked to an increased risk for gout and/or hyperuricaemia(1,9), with similar adverse effects found for alcohol, particularly from beer and liquor(1,7,9,10,13,14), and fructose-containing foods including soft drinks(1,9,11,12) as well as intake of legumes in animal studies(15). In contrast, dairy products, particularly low-fat milk and yogurt(1,9,10,14) intake, caffeine intake(1,9,14) and vitamin C(1,9,14) intake are all hypothesised to be inversely related to gout and/or hyperuricaemia risk. This study evaluated the cross-sectional (SUAbase) and longitudinal (SUArate) associations of SUA with GRS, diet and sex. We then tested interactive effect of GRS, diet and sex on SUA.
Thus, using genetic data available on the AA urban adults participating in the Healthy Aging in Neighborhoods of Diversity Across the LifeSpan (HANDLS), this study had several key aims: first, the study generates and evaluates the effects of GRS for elevated SUA by relating it to both baseline SUA and over-time change in SUA among AA urban adults. Second, the study examines sex-specific association between this GRS and SUA, an association previously observed in individual SNP(16–18). Finally, the study evaluates the relationship between the eight previously described dietary factors and SUA at baseline and change over time, while examining sex–diet interactions and gene–diet interactions within sex groups.
Methods
Database
HANDLS is a prospective cohort study of a representative sample of AA and White men and women aged 30–64 years at baseline. Details of the study design have been described previously(23) (http://handls.nih.gov/). In brief, data were collected in two separate phases at baseline (2004–2009; visit 1), with Phase 1 assessing socio-demographic information (age, sex, education, poverty status, etc.), physiological and psychological chronic exposure, and including the first 24-h dietary recall, whereas Phase 2 consisting of in-depth examinations in Mobile Research Vehicles and including a second 24-h dietary recall, psychometric, anthropometric, body composition and laboratory parameter measurements(19). Visit 2 of HANDLS, initiated in 2009, followed a similar protocol, from which laboratory measurements, specifically SUA, were utilised in this study.
Procedures followed the ethical standards of the institution and approval was obtained from The MedStar Institutional Review Board, and written informed consent was obtained from all HANDLS participants.
Study sample
Data were derived from baseline visit 1 (2004–2009) and the first follow-up examination (visit 2; 2009–2013), and were appended in the long format to facilitate mixed-effects regression modelling analyses (N is the number of persons, N′ the number of observations and k the number of observations/person). Follow-up time (range: <1–approximately 8 years) had a mean of 4.64 (sd 0.93) years, with time = 0 for the baseline visit and time = elapsed years to the nearest day for follow-up visit. HANDLS initially recruited N1 3720 participants (sample 1, n1 2198 AA), with total observations at both visits being N1′ 6025 (n1′ 3616 AA). Among all HANDLS participants, SUA was available at either visits 1 or 2 for N2 3021 (N2′ 5315), of whom n2 1,792 were AA with n2′ 3199 observations (sample 2). Of AA in sample 2, participants with missing data on any of the two baseline 24-h dietary recalls were excluded, yielding a sample size of n3 1235 (n3′ 2206) (sample 3). Out of these participants, only those with complete genetic data (original sample, n 1024 AA) were selected (n4 766; n4′ 1375; visits/person, k 1.8) (sample 4). Thus, our final sample consisted of AA with complete genetic data, complete baseline dietary data with two 24-h recalls and SUA measured at either of the two visits. Sample 4 differed from the unselected participants of sample 1 AA, by having a lower proportion above poverty (49.5 v. 54.3%, P= 0.032), with no notable differences by sex or age (online Supplementary Fig. S1). The same pattern was noted when comparing AA with complete genetic data who were selected (n4 766, 49.5% above poverty) to those who were not (n 258/1024, 62.8% above poverty).
Serum uric acid
Using 1 ml of fasting blood serum, SUA was measured using a standard spectrophotometry method at both visits (Quest Diagnostics) (http://www.questdiagnostics.com/testcenter/TestDetail.action?ntc=905). SUA was measured at both visits in HANDLS, and expressed in mg/dl, whereby 1 mg/dl of SUA is equivalent to 0.01681237 μmol/l.
Dietary assessment
Dietary factors included in our analyses were measured at the baseline visit. Both baseline 24-h dietary recalls were obtained using the US Department of Agriculture Automated Multiple Pass Method, a computerised structured interview(20). Measurement aids were used and included measuring cups, spoons, a ruler and an illustrated Food Model Booklet. Both recalls were administered in-person by trained interviewers, 4–10 d apart. Trained nutrition professionals used Survey Net, matching foods consumed with eight-digit codes from the Food and Nutrient Database for Dietary Studies version 30(21), and MyPyramid Equivalents Database (MPED) for food groups (MPED 2: http://www.ars.usda.gov/SP2UserFiles/Place/80400530/pdf/mped/mped2_doc.pdf). Eight dietary factors were chosen as proxy or direct measures for dietary components previously linked SUA: (1) added sugars (teaspoon/d), (2) alcoholic beverages (drinks/d, with one drink defined as twelve fluid ounces of beer, five fluid ounces of wine, or one-and-a-half fluid ounces of 80-proof distilled spirits), (3) ounce equivalents/d of red meats, (4) ounce equivalents/d of fish (sum of fish high and low in n-3 fatty acids), and (5) cup equivalents/d of legumes, cup equivalents/d of dairy products (milk, cheese and yogurt), dietary vitamin C from foods (mg/d), and (8) caffeine (g/d); the later three were associated with reduced SUA(1,9).
Serum uric acid–genetic risk score construction
Genotyping was performed in 1024 HANDLS AA participants using Illumina 1M SNP genotyping array (online Supplementary Appendix S1). A high-quality review paper of GWAS studies examining SNP at various gene loci in relation to phenotypes of SUA, gout or hyperuricaemia was used as a starting point for listing the SNP in the online Supplementary Table S1(22). This list was updated with four more recent GWAS studies(22–26). Despite the paucity of studies in AA adults, all SNP were included in the pool of potentially influential polymorphisms prospectively affecting SUA in our AA urban sample. Genotypes were imputed using the 1000 Genomes Project phase 1 multiethnic reference panel, with SNP extracted only from high-quality imputed genotypes. Of sixty-eight SNP, four were unavailable and rs72552713 was excluded because of poor imputation quality (imputation quality R2 0.0073). After performing linkage disequilibrium (LD)-based SNP pruning, using an LD threshold R2 of 0.8 in a 500 kb sliding window, forty-three independent markers were selected for further analysis. Using mixed-effects regression models adjusted for socio-demographic and lifestyle variables, dietary factors, ten principal components (PC) and the inverse Mills ratio, the forty-three SNP were screened for significant effects on SUA at baseline and rate of change in SUA at a type I error rate of 0.10 (online Supplementary Appendix S2 and Table S2). Only fifteen of the forty-three showed a significant association with baseline SUA (n 12) or rate of change in SUA (n 3). Those fifteen SNP were used to construct three GRS, one for total (GRStotal, n 15), one for baseline (GRSbase, n 12), and one for rate of change (GRSrate, n 3). Given the marked difference in interpretation of effects (base v. rate), only unweighted GRS were constructed and could range from 0 to 30 for GRStotal, 0 to 24 for GRSbase and 0 to 6 for GRSrate. The online Supplementary Table S1 describes those SNP, along with the selection process leading to the three GRS. The online Supplementary Table S2 shows the results of the mixed-effects regression models of the fifteen selected SNP. Notably, seven of the fifteen selected SNP were located on or near the SLC2A9 gene. The remaining eight SNP were located on ABCG2 (n 1), SLC22A12 (n 1), SLC17A1 (n 1), glucokinase (hexokinase 4) regulator (n 1), leucine rich repeat containing 16 A (n 1), neurexin 2 (n 1), nuclear factor of activated T-cells 5, tonicity-responsive (n 1) and hepatic leukaemia factor (n 1).
Covariates
Covariates included sex, age, education (<high school (HS) (grades 1–8), HS (grades 9–12), >HS (grade 13+)), poverty status (household incomes below or above 125% of the 2004 Federal poverty guidelines), smoking status (current smoker v. no use of cigarettes), illicit drug use (current v. no use of either marijuana, cocaine or opiates), BMI measured as weight/squared measured height (kg/m2) ten PC to control for population stratification (online Supplementary Table S1) and selected food groups determined using the MPED2 (http://www.ars.usda.gov/SP2UserFiles/Place/80400530/pdf/mped/mped2_doc.pdf), namely total fruits, total vegetables (cup equivalents/d), total grains (ounce equivalents/d), other meats (ounce equivalents/d) and discretionary solid fats and oils (g/d).
Statistical methods
Using Stata 13.0., sampling weights were included only in descriptive analyses, whereby means and proportions were compared across sex and GRS tertiles, using design-based F test. Moreover, Pfor trend values were estimated by entering GRS as an ordinal predictor in a bivariate regression model. Baseline and follow-up SUA were also plotted (box plots) and compared across GRS tertiles and sex(27). In the main part of the analysis, four sets of time-interval mixed-effects regression models with the outcome SUA measured at either visits 1 or 2 were conducted, which assumes missingness at random(28). (online Supplementary Appendix S2)
In a first model set, eight dietary components predicted baseline SUA (SUAbase) and annual rate of change in SUA (SUArate), overall and stratifying by sex. Type I error in analyses examining dietary factors was corrected for multiple testing using Bonferroni correction, assuming an initial type I error rate of 0.05 for main effects and 0.10 for interaction terms, yielding a corrected error rates of 0.05/8 = 0.006 and 0.10/8 = 0.013, respectively(29,30).
In a second model set, the GRS uppermost two tertiles were contrasted with the lowest in their association with SUAbase (cross-sectional, exposure main effect, GRSbase) and SUArate (longitudinal, exposure × Time, GRSrate); (model A). Cross-sectional and longitudinal effects were compared between sexes and tested for effect modification by including two-way and three-way interactions with sex in unstratified models. In model B, GRStotal tertiles substituted GRSbase and GRSrate.
In a third model set, eight dietary factors were also of primary interest, while effect modification was tested for GRStotal tertiles, by adding two-way and three-way interaction terms in the unstratified model.
Finally, stratifying the analysis by sex, gene–diet interactions were tested in a fourth model set, whereby each of eight dietary factors were separately interacted with continuous GRSbase to test their interactive effects on SUAbase. Similarly, three-way interactions between each dietary component, Time and continuous GRSrate were also examined in separate models. Predictive margins were estimated and plotted across Time, stratifying by exposure group, from selected mixed-effects regression models.
Selection bias due to the non-random selection of participants with complete data was corrected for, using a two-stage Heckman selection process, as was done in other previous studies(31,32).
Results
Table 1 describes baseline characteristics of the study sample by sex and by GRS tertile. While 55.2 % of the sample consisted of women, mean age overall was estimated at 47.4 years. Being below poverty was more likely in women, whereas being a current illicit drug user was more likely in men. Women also had a higher mean BMI than men. Men consumed higher amounts of all selected dietary factors than women, except for fish, caffeine and total vegetables (Table 1). Men had higher SUA at both baseline and follow-up compared with women, and there was a consistent positive association between GRStotal tertiles and SUA (baseline and follow-up). (online Supplementary Fig. S2 and S3)
Table 1. Baseline study characteristics by sex and genetic risk score (GRS) tertile (T), Healthy Aging in Neighborhoods of Diversity Across the Lifespan (Mean values with their standard errors).
| Sex | GRStotal tertile | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||||
| Total (n 766) | Men (n 343) | Women (n 423) | T1 | T2 | T3 | |||||||||
|
|
|
|
|
|
|
|||||||||
| Mean | sem | Mean | sem | Mean | sem | P* | Mean | sem | Mean | sem | Mean | sem | Pfor trend† | |
| Age (years) | 47.4 | 0.6 | 48.4 | 0.8 | 46.6 | 0.8 | 0.14 | 45.7 | 1.1 | 48.2 | 0.7 | 48.8 | 1.2 | 0.043 |
| Marital status (%) | 0.23 | 0.81 | ||||||||||||
| Married | 27.5 | 30.2 | 25.1 | 23.9 | 29.7 | 29.1 | ||||||||
| Missing | 3.6 | 4.8 | 2.5 | 3.7 | 3.7 | 3.0 | ||||||||
| Education (%) | 0.53 | 0.25 | ||||||||||||
| <High school | 3.4 | 2.6 | 4.0 | 3.0 | 3.0 | 4.7 | ||||||||
| High school | 59.6 | 57.3 | 61.7 | 69.0 | 54.0 | 55.0 | ||||||||
| > High school | 37.0 | 40.1 | 34.3 | 28.0 | 43.0 | 40.3 | ||||||||
| Poverty:income ratio<125 %, (%) | 23.5 | 18.6 | 27.9 | 0.015 | 24.8 | 23.6 | 21.6 | 0.83 | ||||||
| Current smoking status (%) | 0.08 | 0.07 | ||||||||||||
| Yes | 48.0 | 56.2 | 40.9 | 55.2 | 39.0 | 52.6 | ||||||||
| Missing | 6.4 | 4.1 | 8.4 | 4.9 | 10.3 | 1.9 | ||||||||
| Current illicit drug use (%) | 0.009 | 0.09 | ||||||||||||
| Yes | 23.6 | 31.8 | 16.3 | 29.5 | 18.6 | 23.0 | ||||||||
| Missing | 4.9 | 2.2 | 7.4 | 1.8 | 8.8 | 3.1 | ||||||||
| BMI (kg/m2) | 29.4 | 0.5 | 27.3 | 0.5 | 31.2 | 0.8 | <0.001 | 28.5 | 0.8 | 30.0 | 0.8 | 29.6 | 1.1 | 0.36 |
| Key dietary intake factors | ||||||||||||||
| Added sugars (teaspoon/d) | 22.6 | 1.2 | 25.3 | 1.7 | 20.2 | 1.6 | 0.031 | 25.9 | 2.2 | 21.2 | 1.8 | 20.0 | 1.6 | 0.029 |
| Alcoholic beverages (drinks/d) | 0.70 | 0.1 | 1.13 | 0.2 | 0.32 | 0.06 | <0.001 | 0.4 | 0.1 | 0.9 | 0.2 | 0.8 | 0.2 | 0.08 |
| Red meat (oz equiv/d) | 1.70 | 0.15 | 2.25 | 0.25 | 1.22 | 0.17 | 0.001 | 2.1 | 0.3 | 1.5 | 0.2 | 1.5 | 0.2 | 0.09 |
| Fish (oz equiv/d) | 1.12 | 0.15 | 1.13 | 0.17 | 1.10 | 0.23 | 0.92 | 1.2 | 0.2 | 1.2 | 0.3 | 0.9 | 0.2 | 0.42 |
| Legumes (cup equiv/d) | 0.04 | 0.01 | 0.06 | 0.02 | 0.02 | 0.06 | 0.034 | 0.02 | 0.01 | 0.06 | 0.02 | 0.04 | 0.01 | 0.13 |
| Dairy products (cups equiv/d) | 0.96 | 0.07 | 1.15 | 0.10 | 0.79 | 0.08 | 0.008 | 1.03 | 0.13 | 0.95 | 0.09 | 0.85 | 0.13 | 0.33 |
| Vitamin C (mg/d) | 83.7 | 5.2 | 99.9 | 8.6 | 69.4 | 5.2 | 0.003 | 79.1 | 7.6 | 89.0 | 8.6 | 81.9 | 11.5 | 0.75 |
| Caffeine (mg/d) | 76.4 | 5.0 | 80.8 | 7.3 | 72.5 | 6.9 | 0.40 | 84.2 | 9.5 | 63.0 | 7.2 | 87.3 | 8.2 | 0.96 |
| Other dietary intake factors | ||||||||||||||
| Total grains (oz equiv/d) | 5.90 | 0.21 | 6.82 | 0.33 | 50.9 | 0.23 | <0.001 | 6.0 | 0.3 | 5.7 | 0.3 | 6.2 | 0.5 | 0.79 |
| Total fruits (cup equiv/d) | 0.77 | 0.05 | 0.93 | 0.08 | 0.62 | 0.06 | 0.003 | 0.7 | 0.1 | 0.8 | 0.1 | 0.9 | 0.1 | 0.40 |
| Total vegetables (cup equiv/d) | 1.39 | 0.10 | 1.54 | 0.19 | 1.25 | 0.07 | 0.15 | 1.3 | 0.1 | 1.5 | 0.2 | 1.3 | 0.1 | 0.62 |
| Other meats (oz equiv/d) | 4.76 | 0.22 | 5.92 | 0.37 | 3.73 | 0.21 | <0.001 | 5.0 | 0.4 | 4.3 | 0.3 | 5.0 | 0.4 | 0.83 |
| Discretionary oil (g/d) | 18.04 | 1.56 | 22.04 | 3.03 | 14.49 | 0.95 | 0.017 | 14.9 | 1.5 | 20.1 | 2.5 | 19.2 | 4.3 | 0.26 |
| Discretionary solid fat (g/d) | 47.45 | 1.96 | 58.26 | 2.84 | 37.87 | 2.37 | <0.001 | 51.7 | 3.6 | 45.6 | 2.9 | 44.3 | 3.5 | 0.13 |
P value for null hypothesis of no sex difference based on a design-based F test.
Pfor trend value was based on design-based F test for trend in exposures across tertiles of GRS.
Several key findings emerged from the mixed-effects regression models (Tables 2–5). After correction for multiple testing, overall, (Table 2; online Supplementary Fig. S4), higher rate of change in SUA was associated with lower dairy product intake (γ16 −0.042; 95% CI −0.075, −0.009, P = 0.010) When examining sex-specific associations, the association of legume intake with SUArate was stronger among women (γ +0.14; 95% CI +0.06, +0.22, P = 0.001), while alcohol intake was positively associated with SUAbase also among women (γ +0.154; 95% CI +0.046, +0.262, P = 0.005).
Table 2. Mixed-effects regression models of serum uric acid (SUA) by dietary components, stratified by sex* (Regression coefficients (γ) with their standard errors of the estimate (SEE)).
| SUA | Total: model 1† | Men: model 2† | Women: model 3† | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| n 766 | n′ 1341 | n 343 | n′ 583 | n 423 | n′ 758 | ||||
|
|
|
|
|
|
|
||||
| γ | SEE | P | γ | SEE | P | γ | SEE | P | |
| Fixed effects | |||||||||
| Added sugar (γ01 for π0i) | +0.002 | 0.004 | 0.69 | +0.003 | 0.005 | 0.55 | −0.003 | 0.006 | 0.65 |
| Added sugar × Time (γ11 for π1i) | +0.0005 | 0.0009 | 0.63 | −0.0002‡ | 0.001 | 0.90 | +0.0024‡ | 0.001 | 0.0834‡ |
| Alcohol (γ02 for π0i) | +0.082§ | 0.032 | 0.010§ | +0.05 | 0.04 | 0.22 | +0.154§‖ | 0.055 | 0.005§‖ |
| Alcohol × Time (γ12 for π1i) | −0.008 | 0.008 | 0.30 | −0.002 | 0.011 | 0.83 | −0.018 | 0.012 | 0.12 |
| Red meat (γ03 for π0i) | +0.046§ | 0.021 | 0.031§ | +0.035 | 0.025 | 0.15 | +0.090§ | 0.045 | 0.044§ |
| Red meat × Time (γ13 for π1i) | −0.002 | 0.005 | 0.70 | −0.003 | 0.006 | 0.55 | −0.001 | 0.010 | 0.94 |
| Fish (γ04 for π0i) | +0.025 | 0.025 | 0.31 | +0.011 | 0.040 | 0.78 | +0.028 | 0.032 | 0.39 |
| Fish × Time (γ14 for π1i) | −0.004 | 0.006 | 0.44 | −0.002 | 0.010 | 0.87 | −0.006 | 0.007 | 0.39 |
| Legumes (γ05 for π0i) | −0.28 | 0.18 | 0.12 | −0.33 | 0.37 | 0.38 | −0.29 | 0.21 | 0.17 |
| Legumes × Time (γ15 for π1i) | +0.09§ | 0.04 | 0.018§ | −0.073 | 0.087 | 0.40¶ | +0.14§‖ | 0.04 | 0.001§‖ |
| Dairy products (γ06 for π0i) | +0.09 | 0.07 | 0.24 | +0.07 | 0.11 | 0.50 | +0.15 | 0.11 | 0.17 |
| Dairy products × Time (γ16 for π1i) | −0.042§‖ | 0.017 | 0.010§‖ | −0.037 | 0.025 | 0.14 | −0.057§ | 0.024 | 0.015§ |
| Vitamin C (γ07 for π0i) | −0.001 | 0.001 | 0.12 | −0.003§ | 0.001 | 0.044§ | −0.001 | 0.001 | 0.71 |
| Vitamin C×Time (γ17 for π1i) | +0.0003 | 0.0002 | 0.16 | +0.0003 | 0.0003 | 0.34 | +0.0002 | 0.0003 | 0.49 |
| Caffeine (γ08 for π0i) | −0.0001 | 0.001 | 0.88 | −0.0002 | 0.0008 | 0.83 | −0.0002 | 0.0008 | 0.84 |
| Caffeine × Time (γ18 for π1i) | −0.0000 | 0.0001 | 0.92 | +0.0001 | 0.0002 | 0.70 | −0.0002 | 0.0002 | 0.40 |
n, number of participants in the analysis; n′, total number of visits included in the analysis; Agebase, baseline age at visit 1.
Random effects are not shown for simplicity.
Models were further adjusted for marital status, poverty status, education (years), baseline current smoking status, current illicit drug use and baseline BMI centred at 30 kg/m2, the ten principal components for population structure, other dietary factors namely total grains, total fruit, total vegetables, other meats, discretionary solid fat and discretionary oils, and the inverse Mills ratio. Agebase was centred at 50 years, sex was coded as 0 = women, 1 = men. All dietary factors were centred at their weighted means (see Table 1, total).
P < 0.10.
P < 005
Passed correction for multiple testing.
P<005 for interaction with sex to test effect modification by sex for each of the eight dietary factors on SUA at baseline and SUA change over time.
Table 5. Sex-specific interactions between genetic risk score (GRS) tertiles (GRSbase and GRSrisk) and dietary factors in their association with serum uric acid (SUA): mixed-effect regression models* (Regression coefficients (γ) with their standard errors of the estimate (SEE)).
| SUA | Men† | Women† | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| n 343 | n′ 583 | n′ 423 | n′ 758 | |||||||
|
|
|
|
|
|||||||
| γ | SEE | P | γ | SEE | P | |||||
| Added sugar | ||||||||||
| Model 1.A | ||||||||||
| Added sugar (γ01 for π0i) | +0.013 | 0.016 | 0.41 | +0.023 | 0.016 | 0.14 | ||||
| GRSbase (γ09 for π0i) | +0.093‡ | 0.039 | 0.018‡ | +0.126‡ | 0.032 | <0.001‡ | ||||
| Added sugar × GRSbase (γ019 for π0i) | −0.001 | 0.01 | 0.57 | −0.002§ | 0.001 | 0.098§ | ||||
| Model 1.B | ||||||||||
| Added sugar × Time (γ11 for π1i) | −0.000 | 0.001 | 0.91 | −00026§ | 0.0014 | 007§ | ||||
| GRSrate × Time (γ19 for π1i) | +0.044‡ | 0.019 | 0.018‡ | −0019 | 0.016 | 0.24 | ||||
| Added sugar × GRSrate × Time (γ119 for π1i) | +0.001 | 0.001 | 0.31 | +0.002 | 0.001 | 0.16 | ||||
| Alcohol | ||||||||||
| Model 2.A | ||||||||||
| Alcohol (γ02 for π0i) | −0.004 | 0.011 | 0.73 | −0.07 | 0.26 | 0.79 | ||||
| GRSbase (γ09 for π0i) | +0.073‡ | 0.024 | 0.003‡ | +0.077‡ | 0.019 | <0.001‡ | ||||
| Alcohol × GRSbase (γ01 for π0i) | +0.001 | 0.009 | 0.90 | +0.016 | 0.019 | 0.41 | ||||
| Model 2.B | ||||||||||
| Alcohol × Time (γ12 for π1i) | +0.004 | 0.011 | 0.73 | −0.018 | 0.014 | 0.13 | ||||
| GRSrate × Time (γ19 for π1i) | +0.048‡ | 0.019 | 0.010‡ | +0.016 | 0.016 | 0.30 | ||||
| Alcohol × GRSrate × Time (γ129 for π1i) | −0.012 | 0.011 | 0.31 | +0.001 | 0.011 | 0.90 | ||||
| Red meat | ||||||||||
| Model 3.A | ||||||||||
| Red meat (γ03 for π0i) | +0.13‡ | 0.06 | 0.026‡ | +0.38‡ | 0.13 | 0.003‡ | ||||
| GRSbase (γ09 for π0i) | +0.095‡ | 0.025 | <0.001‡ | +0.118‡ | 0.023 | <0.001‡ | ||||
| Red meat × GRSbase (γ039 for π0i) | −0.010§ | 0.06 | 0.09§ | −0.026‡ | 0.010 | 0.014‡ | ||||
| Model 3.B | ||||||||||
| Red meat × Time (γ13 for π1i) | −0.001 | 0.008 | 0.86 | −0.003 | 0.010 | 0.80 | ||||
| GRSrate × Time (γ19 for π1i) | +0.044‡ | 0.018 | 0.014‡ | +0.023 | 0.016 | 0.15 | ||||
| Red meat × GRSrate × Time (γ139 for π1i) | +0.001 | 0.007 | 0.93 | +0.025‡‖ | 0.010 | 0.012‡‖ | ||||
| Fish | ||||||||||
| Model 4.A | ||||||||||
| Fish (γ04 for π0i) | −0.018 | 0.154 | 0.91 | −0.002 | 0.087 | 0.98 | ||||
| GRSbase (γ09 for π0i) | +0.072‡ | 0.024 | 0.003‡ | +0.077‡ | 0.020 | <0.001‡ | ||||
| Fish × GRSbase (γ149 for π0i) | +0.003 | 0.014 | 0.82 | +0.004 | 0.007 | 0.57 | ||||
| Model 4.B | ||||||||||
| Fish × Time (γ14 for π1i) | −0.003 | 0.010 | 0.76 | −0.006 | 0.007 | 0.39 | ||||
| GRSrate × Time (γ19 for π1i) | +0.048‡ | 0.019 | 0.010‡ | +0.017 | 0.016 | 0.29 | ||||
| Fish × GRSrate × Time (γ149 for π1i) | −0.006 | 0.008 | 0.46 | +0.001 | 0.008 | 0.90 | ||||
| Legumes | ||||||||||
| Model 5.A | ||||||||||
| Legumes (γ05 for π0i) | +2.146 | 2.315 | 0.35 | +1.222 | 1.311 | 0.35 | ||||
| GRSbase (γ09 for π0i) | +0.082‡ | 0.023 | <0.001‡ | +0.088‡ | 0.019 | <0.001‡ | ||||
| Legumes × GRSbase (γ059 for π0i) | −0.219 | 0.202 | 0.28 | −0.102 | 0.083 | 0.22 | ||||
| Model 5.B | ||||||||||
| Legumes × Time (γ15 for π1i) | −0.056 | 0.091 | 0.54 | +0.258‡ | 0.077 | 0.001‡ | ||||
| GRSrate × Time (γ19 for π1i) | +0.048‡ | 0.019 | 0.013‡ | +0.007 | 0.016 | 0.66 | ||||
| Legumes × GRSrate × Time (γ159 for π1i) | −0.073 | 0.153 | 0.63 | +0.219§ | 0.121§ | 0.072§ | ||||
| Dairy products | ||||||||||
| Model 6.A | ||||||||||
| Dairy products (γ06 for π0i) | −0.42 | 0.32 | 0.20 | +0.314 | 0.290 | 0.28 | ||||
| GRSbase (γ09 for π0i) | +0.035 | 0.033 | 0.29 | +0.093‡ | 0.025 | <0.001‡ | ||||
| Dairy products × GRSbase (γ069 for π0i) | +0.041 | 0.026 | 0.12 | −0.015 | 0.026 | 0.55 | ||||
| Model 6.B | ||||||||||
| Dairy products × Time (γ19 for π1i) | −0.054‡ | 0.027 | 0.043‡ | −0.053‡ | 0.024 | 0.027‡ | ||||
| GRSrate × Time (γ19 for π1i) | +0.043‡ | 0.018 | 0.018‡ | +0.019 | 0.016 | 0.23 | ||||
| Dairy products × GRSrate × Time (γ169 for π1i) | +0.005 | 0.018 | 0.77 | +0.014 | 0.019 | 0.45 | ||||
| Vitamin C | ||||||||||
| Model 7.A | ||||||||||
| Vitamin C (γ07 for π0i) | −0.0121‡ | 0.004 | 0.001‡ | +0.002 | 0.003 | 0.51 | ||||
| GRSbase (γ09 for π0i) | +0.0134 | 0.031 | 0.66 | +0.097‡ | 0.0263 | <0.001‡ | ||||
| Vitamin C × GRSbase (γ079 for π0i) | +0.001‡‖ | 0.000 | 0.006‡‖ | −0.0001 | 0.0002 | 0.47 | ||||
| Model 7.B | ||||||||||
| Vitamin C × Time (γ19 for π1i) | +0.0002 | 0.0003 | 0.79 | −0.0002 | 0.0003 | 0.58 | ||||
| GRSrate × Time (γ19 for π1i) | +0.043‡ | 0.018 | 0.018‡ | +0.017 | 0.016 | 0.26 | ||||
| Vitamin C × GRSrate × Time (γ179 for π1i) | −0.0005‡ | 0.0002 | 0.026‡ | +0.0003 | 0.0002 | 0.19 | ||||
| Caffeine | ||||||||||
| Model 8.A | ||||||||||
| Caffeine (γ08 for π0i) | +0.002 | 0.002 | 0.51 | +0.0048§ | 0.028 | 0.083§ | ||||
| GRSbase (γ09 for π0i) | +0.089‡ | 0.029 | 0.002‡ | +0.111‡ | 0.023 | <0.001‡ | ||||
| Caffeine × GRSbase γ089 for π0i) | −0.0001 | 0.0002 | 0.46 | −0.0004§ | 0.0002 | 0.055§ | ||||
| Model 8.B | ||||||||||
| Caffeine × Time γ19 for π1i) | +0.0001 | 0.0002 | 0.71 | −0.0001 | 0.0002 | 0.48 | ||||
| GRSrate × Time γ19 for π1i) | +0.046‡ | 0.019 | 0.013‡ | +0.020 | 0.016 | 0.21 | ||||
| Caffeine × GRSrate × Time γ189 for π1i) | −0.0001 | 0.0002 | 0.79 | +0.0003§ | 0.0002 | 0.055§ | ||||
n, number of participants in the analysis; n′, total number of visits included in the analysis; Agebase, baseline age at visit 1.
Random effects are not shown for simplicity.
Each of the models' intercepts and slopes were further adjusted for Agebase, marital status, poverty status, education (years), baseline current smoking status, current illicit drug use and baseline BMI centred at 30 kg/m2, the ten principal components for population structure, and all the remaining dietary factors, that is, seven of the eight key dietary factors in addition to total grains, total fruit, total vegetables, other meats, discretionary solid fat and discretionary oils, and the inverse Mills ratio. Agebase was centred at 50 years, and all dietary factors were centred at their weighted means (see Table 1, total). GRSbase was centred at 11.5 and GRSrate was centred at 1.6.
P<0.05.
P<0.10.
Passed correction for multiple testing.
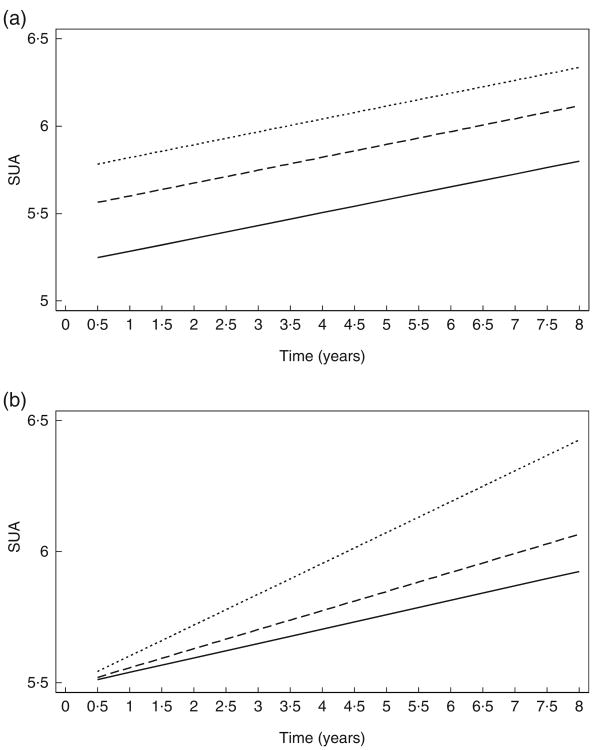
Table 3 tests associations between GRSbase tertiles and baseline SUA and between GRSrate tertiles and rate of change in SUA, overall and stratified by sex (model A). Both the middle and uppermost tertiles of GRSbase were associated with higher SUA compared with the lowest tertile, with a significantly stronger association of the highest tertile v. lowest among women and the middle tertile v. lowest among men. Only the uppermost tertile of GRSrate was linked to faster rate of increase in SUArate compared with the lowest tertile. This effect was significantly stronger among men and non-significant in women. The predictive margins of SUA across time by tertiles of GRSbase and GRSrate are presented in Fig. 1(a) and (b). Mixed-effects regression models with GRStotal tertiles (model B) indicated that higher GRStotal was associated with higher SUAbase overall though no association was detected with SUArate.
Table 3. Mixed-effects regression models of serum uric acid (SUA) by genetic risk score (GRS) tertiles (GRSbase and GRSrate: model A; GRStotal: model B), stratified by sex* (Regression coefficients (γ) with their standard errors of the estimate (SEE)).
| SUA | Total† | Men† | Women† | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| n 766 | n′ 1341 | n 343 | n′ 583 | n 423 | n′ 758 | ||||
|
|
|
|
|
|
|
||||
| γ | SEE | P | γ | SEE | P | γ | SEE | P | |
| Model A: GRS base and rate | |||||||||
| Fixed effects | |||||||||
| GRS21base (γ021 for π0i) | +0.32 | 0.11 | 0.004 | +0.36 | 0.18 | 0.043‡ | +0.30 | 0.14 | 0.029 |
| GRS21rate × Time (γ121 for π1i) | +0.02 | 0.020 | 0.47 | +0.03 | 0.041 | 0.42 | +0.02 | 0.03 | 0.56 |
| GRS31base (γ031 for π0i) | +0.54 | 0.12 | <0.001 | +0.44 | 0.18 | 0.013‡ | +0.60 | 0.15 | <0.001 |
| GRS31rate × Time (γ131 for π1i) | +0.06 | 0.03 | 0.037 | +0.11 | 0.05 | 0.021‡ | +0.004 | 0.039 | 0.90 |
| Model B: GRS total | |||||||||
| Fixed effects | |||||||||
| GRS21total (γ021 for π0i) | +0.31 | 0.11 | 0.007 | +0.40 | 0.18 | 0.022 | +0.23 | 0.15 | 0.12 |
| GRS21total × Time (γ121 for π1i) | +0.01 | 0.03 | 0.73 | +0.02 | 0.05 | 0.61 | +0.02 | 0.03 | 0.56 |
| GRS31total (γ031 for π0i) | +0.50 | 0.12 | <0.001 | 0.44 | 0.19 | 0.020 | +0.56 | 0.16 | 0.001 |
| GRS31total × Time (γ131 for π1i) | +0.04 | 0.03 | 0.20 | 0.01 | 0.05 | 0.81 | +0.03 | 0.04 | 0.36 |
n, number of participants in the analysis; n′, total number of visits included in the analysis; Agebase, baseline age at visit 1; GRS21, High Serum Uric Acid Risk Score dummy for tertile 2 v. tertile 1; GRS31, High Serum Uric Acid Risk Score dummy for tertile 3 v. tertile 1.
Random effects are not shown for simplicity.
Models were further adjusted for marital status, poverty status, education (years), baseline current smoking status, current illicit drug use and baseline BMI centred at 30 kg/m2, the ten principal components for population structure, other dietary factors namely total grains, total fruit, total vegetables, other meats, discretionary solid fat and discretionary oils, and the inverse Mills ratio. Agebase was centred at 50 years, sex was coded as 0 = women, 1 = men. All dietary factors were centred at their weighted means (see Table 1, total). Tertiles of GRSbase had the following distribution: T1 (N 258, mean 7.80, sd 1.95, range 2–10); T2 (N 279, mean 11.76, sd 0.94, range 10–13); T3 (N 229, mean 15.18, sd 1.28, range 13–19). Tertiles of GRSrate had the following distribution: T1 (N 325, mean 0.68, sd 0.46, range 0–1); T2 (N 291, mean 1.85, sd 0.34, range 1–2); T3 (N 150, mean 2.88, sd 0.61, range 2–5). See Table 4 for ranges and mean values and standard deviations of GRStotal within its tertiles.
P<005 for interaction with sex to test effect modification by sex for each of the two dummy variables (i.e. GRS21 and GRS31) on SUA at baseline and SUA change over time.
Fig. 1.
Predictive margins of serum uric acid (SUA) by time and tertiles (T) of genetic risk scores (GRS), (a) GRSbase and (b) GRSrate, from mixed-effects regression model, total population. Predictive margins obtained from mixed-effects regression model with SUA as the outcome, random effects added to slope and intercept, and both slopes and intercept adjusted for multiple factors including age, sex, poverty status, marital status, education, smoking and drug use, several dietary factors, BMI, ten principal components for population structure and an inverse Mills ratio. The figure simulates the trajectory of a population with comparable characteristics (covariates set at their observed values in the sample) when exposed alternatively to T1, T2 and T3 of GRSbase and GRSrate, respectively (see Table 3, model 1). (a): –––, GRSbase, T1; ------, GRSbase, T2; …………, GRSbase, T3; (b): –––, GRSrate, T1; -----, GRSrate, T2; …………, GRSrate, T3. Tertiles of GRSbase had the following distribution: T1 (n 258, mean 7.80, sd 1.95, range 2–10); T2 (n 279, mean 11.76, sd 0.94, range 10–13); T3 (n 229, mean 15.18, sd 1.28, range 13–19). Tertiles of GRSrate had the following distribution: T1 (n 325, mean 0.68, sd 0.46, range 0–1); T2 (n 291, mean 1.85, sd 0.34, range 1–2); T3 (n 150, mean 2.88, sd 0.61, range 2–5).
In Table 4, after correction for multiple testing, the association between legume consumption and SUArate was restricted to the lowest tertile of GRStotal; (γ15 +0.491; 95% CI +0.246, +0.736, P< 0.001), indicating an antagonistic GRStotal × legume interaction.
Table 4. Mixed-effects regression models of serum uric acid (SUA) by dietary components, stratified by genetic risk score(GRS) tertile (GRStotal)* (Mean values and standard deviations; regression coefficients (γ) with their standard errors of the estimate (SEE)).
| GRStotal (T1) | GRStotal (T2) | GRStotal (T3) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| GRStotal score | |||||||||
| Mean | 9.19 | 13.51 | 16.88 | ||||||
| sd | 2.05 | 1.09 | 1.37 | ||||||
| Range | 3–12 | 12–15 | 15–22 | ||||||
|
| |||||||||
| SUA | Model 1† | Model 2† | Model 3† | ||||||
|
|
|
|
|||||||
| n 256 | n′ 453 | n 297 | n′ 514 | n 213 | n′ 374 | ||||
|
|
|
|
|
|
|
||||
| γ | SEE | P | γ | SEE | P | γ | SEE | P | |
|
| |||||||||
| Fixed effects | |||||||||
| Added sugar (γ01 for π0i) | +0.005 | 0.063 | 0.94 | +0.004 | 0.006 | 0.55 | +0.004 | 0.008 | 0.65 |
| Added sugar × Time (γ11 for π1i) | +0.002 | 0.001 | 0.15 | +0.001 | 0.002 | 0.59 | −0.002 | 0.002 | 0.21 |
| Alcohol (γ02 for π0i) | +0.005 | 0.063 | 0.94 | +0.161‡ | 0 061 | 0.009‡ | +0.091§ | 0.047 | 0.05§ |
| Alcohol × Time (γ12 for π1i) | −0.005 | 0.013 | 0.71 | −0.012 | 0 02 | 0.48 | −0.015 | 0.012 | 0.19 |
| Red meat (γ03 for π0i) | +0.078‡ | 0.031 | 0.011‡ | +0.01 | 0.05 | 0.84 | −0.055 | 0.042 | 0.19‖ |
| Red meat × Time (γ13 for π1i) | −0.005 | 0.006 | 0.37 | +0.02 | 0.01 | 0.22‖ | +0.005 | 0.010 | 0.58 |
| Fish (γ04 for π0i) | +0.001 | 0.04 | 0.98 | +0.11‡ | 0.05 | 0.021‡ | −0.010 | 0.045 | 0.82 |
| Fish × Time (γ14 for π1i) | −0.000 | 0.008 | 0.99 | −0.005 | 0.012 | 0.66 | −0.012 | 0.010 | 0.25 |
| Legumes (γ05 for π0i) | −0.759 | 0.660 | 0.25 | −0.211 | 0.409 | 0.61 | −0.49‡ | 0.23 | 0.034‡ |
| Legumes × Time (γ15 for π1i) | +0.491‡¶ | 0.125 | <0.001‡¶ | −0.038 | 0.102 | 0.71‖ | +0.083 | 0.050 | 0.10‖ |
| Dairy products (γ06 for π0i) | −0.049 | 0.13 | 0.70 | +0.160 | 0.124 | 0.20 | +0.102 | 0.139 | 0.46 |
| Dairy products × Time (γ16 for π1i) | −0.013 | 0.024 | 0.61 | −0.057§ | 0.030 | 0.053§ | −0.036 | 0.033 | 0.26 |
| Vitamin C (γ07 for π0i) | +0.000 | 0.002 | 0.91 | −0.001 | 0.001 | 0.66 | −0.005‡ | 0.002 | 0.008‡ |
| Vitamin C × Time (γ17 for π1i) | +0.000 | 0.000 | 0.50 | +0.000 | 0.000 | 0.30 | +0.000 | 0.000 | 0.31 |
| Caffeine (γ08 for π0i) | +0.001 | 0.001 | 0.17 | −0.002§ | 0.001 | 0.065§ | −0.001 | 0.001 | 0.34 |
| Caffeine × Time (γ18 for π1i) | −0.000 | 0.000 | 0.47 | +0.000 | 0.000 | 0.97 | +0.000 | 0.000 | 0.30 |
T1, lowest tertile; T2, middle tertile; T3, highest tertile; n, number of participants in the analysis; n′, total number of visits included in the analysis; Agebase, baseline age at visit 1; GRStotal, High Serum Uric Acid Risk Score, total.
Random effects are not shown for simplicity.
Each of the model's intercepts and slopes were further adjusted for marital status, poverty status, education (years), baseline current smoking status, current illicit drug use and baseline BMI centred at 30kg/m2, the ten principal components for population structure, other dietary factors namely total grains, total fruit, total vegetables, other meats, discretionary solid fat and discretionary oils, and the inverse Mills ratio. Agebase was centred at 50 years, sex was coded as 0 = women, 1 = men, and all dietary factors were centred at their weighted means (see Table 1, total).
P<0.05.
P<0.10.
P<005 for interaction with GRStotal tertiles to test effect modification by GRStotal tertiles for each of the eight dietary factors on SUA at baseline and SUA change over time.
Passed correction for multiple testing.
In Table 5, among women, we detected a synergistic interaction between GRSrate and red meat consumption in relation to SUArate (γ139 +0.025 (standard error of the estimate (SEE) 0.010), P= 0.012). Specifically, GRSrate among women was associated with non-significant increase in SUA over time among non-consumers of red meat, which was accelerated with red meat consumption. Among men, lower vitamin C intake was associated with higher SUAbase, particularly at higher GRSbase (γ079 +0.001 (SEE 0.000), P = 0.006) indicating also a synergistic effect between having high genetic and high dietary risk in terms of lower vitamin C intake.
Discussion
To our knowledge, this is the first study to evaluate SUAbase and SUArate associations with GRS in a large sample of AA urban adults, while examining sex-specific genetic and dietary associations with SUA and gene-diet interactions. Among key findings, SUAbase was higher among men and increased with GRStotal tertiles. SUArate was positively associated with legume intake among women (γ +0.14; 95% CI +0.06, +0.22, P= 0.001) and inversely related to dairy product intake in both sexes combined (γ = −0.042; 95% CI −0.075, −0.009, P= 0.010). SUAbase was directly linked to alcohol consumption among women (γ +0.154; 95% CI +0.046, +0.262, P=0.005). GRSrate was linearly related to SUArate only among men. Legume consumption's positive association with SUArate was restricted to GRStotal's lowest tertile. Among women, a synergistic interaction was observed between GRSrate and red meat intake in association with SUArate. Among men, a synergistic interaction between low vitamin C and genetic risk was also found.
Doring et al. indicated that the most significant SNP's associated with SUA were within the SLC2A9 gene, introns 4 and 6 (P < 1.2 × 10−8). This gene encodes two GLUT9 isoforms of the class II facilitative glucose transport family(16). The long isoform GLUT9a (SLC2A9_L, GLUT9, 540 amino acids) is strongly expressed among humans in the basolateral side of the proximal renal tubular cells, and is responsible for the transport of UA back into the bloodstream(33), whereas the shorter isoform GLUT9b (SLC2A9_S, GLUT9ΔN, 511 amino acids) is expressed only in the apical membrane of polarised renal tubular cells, and gain of function mutations would be expected to increase the reuptake of excreted UA causing hyperuricaemia(34). Although RNA expression analysis has confirmed that the short isoform of SLC2A9 was significantly and positively associated with SUA, to our knowledge SNP associated with SLC2A9b have yet to predict amino acid changes in GLUT9b which would predict a gain of function. Conversely, loss of function mutations in SLC2A9b have been reported to be causative of renal hypouricaemia in human subjects(16,35,36). However, none of the SLC2A9 SNP are predicted to be deleterious in in silico functional annotation. Experimental studies are required to assess the biological consequences of these variants. Fructose is also a substrate for liver GLUT9a (the longer isoform), as well as GLUT5 and GLUT11(16). Following its transport into hepatocytes, fructose is phosphorylated by fructokinase, generating ADP that is rapidly transformed into UA(16). Therefore, the net effect of increasing fructose intake would be facilitative of liver purine breakdown into UA, thus increasing SUA(24).
In a large GWAS by Kolz et al., the rs734553 minor allele in SLC2A9 had a stronger effect on reducing SUA in women, while the effect was stronger in men for the minor allele of rs2231142 in ABCG2 which elevates SUA(17). The percentage variance explained by SLC2A9 variants in SUA differs between sexes with genotypes explaining 1.2% in men and 6% in women and expression levels explaining 3.5% in men and 15% in women(16). Another confirmatory study genotyped four previously identified SNP in the SLC2A9 gene (rs6855911, rs7442295, rs6449213 and rs12510549) and found significant associations with SUA in the expected direction. However, this association was significantly stronger among women and among individuals with higher BMI(18). Our study indicated that the uppermost tertile of GRSbase was more strongly associated with SUAbase in women compared with men, though the reverse was true for the middle tertile. However, GRSrate was positively linked to SUArate only in men, while comparing the uppermost tertile to the lowest. As most other studies were cross-sectional and considering the uppermost tertile v. lowest contrast as the most important finding, our results replicated those prior studies, particularly that GRSbase consisted mostly of SLC2A9 gene SNP(16–18).
The association between diet and SUA were also explored in previous studies, though failing to test sex-related differences. Given the consistently higher levels of SUA in men compared with that in women, it is important to include sex as an effect modifier when examining other risk factors for SUA levels. Large prospective cohort studies showed that higher meat and seafood intakes were associated with higher gout risk and higher SUA concentrations(1,8). However, no association was detected for other purine-rich foods including peas, lentils, beans, spinach, mushrooms and cauliflower(1), highlighting the importance of amount, bioavailability and types of purines in foods(1). We found that among women, there was a synergistic interaction between GRSrate and red meat intake in association with faster increase in SUArate. Thus, even though GRSrate by itself was not associated with SUArate among AA women (unlike among AA men), red meat consumption in this group may accelerate the genetic risk's effect on SUA's rate of increase. In other words, there is a super-additive effect of increasing meat consumption and increasing genetic risk on the rate of change in SUA among women. The biological mechanism behind this finding is worth further exploration. Furthermore, randomised controlled trials of red meat consumption in relation SUArate should be conducted among AA women while stratifying by genetic risk, to replicate those findings.
The positive association between legume consumption with SUArate was restricted to the lowest tertile of GRStotal, indicating an antagonistic interaction, and was significantly stronger in women. Thus, legume consumption may affect the rate at which SUA increases over time in women and among individuals with lower genetic risk for elevated SUA. This finding is novel and worth further exploration in larger AA adult samples, particularly that the positive association between legume intake and SUA was only found in animal studies(15).
Fructose intake, as discussed earlier, exerts a direct effect on SUA, through liver ATP utilisation for phosphorylation and production of ADP. In addition, SLC2A9 transports both fructose and UA with maximal transport of fructose occurring in the absence of UA. In fact, oral fructose administration in hyperuricaemic patients further increased SUA(1,37). Using national data (National Health and Nutrition Examination Survey III (NHANES III)) on 14761 adults, soft drink consumption was shown to increase SUA in a dose-response way from +0.08 mg/dl higher SUA (for <0.5 servings v. no intake), to 0.42 mg/dl higher SUA (for ≥4 servings/d v. no intake), Pfor trend = 0.003. Findings were similar for sugar-sweetened soft drinks in relation to the odds of hyperuricaemia(11), and were replicated only in men in another analysis using NHANES 2001–2002(12). At least one study found a non-additive interaction between SLC2A9 genotype and sugar-sweetened beverage consumption in determining the risk for gout, when analysing genotype-specific groups(38). Our study did not detect an association between added sugars and SUAbase/rate, possibly due to differences between our study and previous ones in terms of racial/ethnic composition. However, larger studies of AA adult populations are needed to replicate those findings.
Based on a recent meta-analysis of 42 924 adults, alcohol consumption had a linear dose–response relationship with gout. Compared with no/little alcohol drinking, light (≤1 drink/d), moderate (>1–<3 drinks/d) and heavy drinking (≥3 drinks/d) had a risk ratio of 1.16 (95% CI 1.07, 1.25), 1.58 (95% CI 1.50, 1.66) and 2.64 (95% CI 2.26, 3.09), respectively(39). Studies also indicated that the association between alcohol and SUA pertained mostly to beer and liquor/spirits(7). Similar to fructose, alcohol increases liver UA production through ATP degradation, leading to accumulation of ADP and AMP. Alcohol intake additionally leads to dehydration and metabolic acidosis, resulting in a decreased urate excretion(1). A study among Japanese adults confirmed an association between SUA and an LDL-receptor-related protein (LRP2) polymorphism rs2544390 (C/T). The study found this association to be stronger among males drinking five times or more per week, with a significant gene–diet interaction, indicating synergism(40). In contrast, an antagonistic interaction on gout outcomes was found in another study that combined Maori and Pacific Islanders, in which alcohol consumption was associated with higher risk for gout only in the rs2544390 CC genotype group(41). Another study showed alcohol consumption and ABCG2 Q141K was independently and jointly associated with the risk for chronic tophaceous gout(42). Our findings indicated sex-specific associations between alcohol and SUA (stronger cross-sectional positive effect in women), without detecting any gene–diet interactions. This suggests that among women, reducing alcohol consumption may potentially reduce SUA, irrespective of genetic risk for elevated SUA.
Vitamin C may also reduce SUA based on a cross-sectional study(43) and a meta-analysis of randomised controlled trials that administered a median dose of 500mg/d(44). Biological mechanisms involved include a uricosuric effect of vitamin C at the URAT1 and a sodium-dependent anion co-transporter solute carrier family 5, member 8 (SLCA5A8)/A12; an enhanced fractional kidney clearance of UA; and a reduced oxidative damage of body cells which reduces SUA(14). In our study, among men, low vitamin C was shown to increase SUAbase only at higher GRSbase levels, indicating a synergistic interaction. This suggests that among AA men, increasing intake of vitamin C may potentially reduce SUAbase, particularly when genetic risk is elevated. However, randomised controlled trials among AA men and stratified by genetic risk are needed to confirm this observation.
Several studies have shown a relationship between dairy product consumption and SUA/gout(10,14). The evidence thus far points to a protective effect of milk and low-fat yogurt against gout occurrence and hyperuricaemia(8). There is also evidence that a vegan diet lacking dairy products is more hyperuricaemic than a vegetarian or fish eating type of diet, with the differences most pronounced among men(45). Several mechanisms were suggested including the effects of orotic acid in milk which promotes renal urate excretion, the uricosuric effect of milk casein and lactalbumin, and a putative biological effect of vitamin D on SUA which has yet to be confirmed(14). Besides specific dietary components, a higher Mediterranean diet score was linked to lower SUA(5,6), particularly among women(5). We found that SUArate was inversely related to dairy product intake in the overall AA sample (Dairy product × Time effect: γ −0.042 (SEE 0.017), P= 0.010). However, there were no gene–diet or sex–diet interactions for this dietary component.
Among its strengths, this study systematically examined SNP previously shown to be associated with higher SUA and evaluated SUA's sex-specific association with a composite GRS, while testing gene–diet interactions. Our study is among the few to include AA. Despite its strengths, some limitations include a statistical power-limiting small sample size, which precluded further adjustment for incomplete potential con-founders such as lipid profiles, ferritin, C-reactive protein and depressive symptoms. In fact, further analyses suggested that the power to detect the effect that was detected in our models was more adequate for the total population than for sex-stratified models. Another limitation is the lack of adequately measured baseline covariates that could potentially act as confounders, including baseline physical activity. Moreover, most of our selected SNP came from studies conducted among subjects of European ancestry as well as other ethnic groups because of the paucity of studies among AA. Availability of genetic data in our HANDLS study among Whites would have strengthened our findings if replicated. Moreover, although GRS weighting by effect size was possible, we opted not to weight our gene scores due to the multiplicity of racial and ethnic groups in previous studies and for ease of interpretation. Finally, because of the low level of correlation between dietary factors that were related to SUA (r < 0.20), a valid index for elevated SUA or faster increase in SUA could not be computed.
In sum, sex-diet, sex–gene and gene–diet interactions were detected in determining SUA. Dietary factors which interacted with genetic risk to alter SUAbase/rate included legumes (overall), red meat (among women) and vitamin C (among men). Legumes and alcohol intakes were shown to potentially alter SUA's trajectory only in women. Finally, the GRSrate altered the rate of change in SUA only among men. Further studies on similar AA adult populations and incorporating larger samples of men and women are needed to replicate our findings.
Supplementary Material
Acknowledgments
The authors would like to thank Gregory A. Dore and Ola S. Rostant for their internal review of the manuscript.
This work was fully supported by the Intramural Research Program of the NIH, National Institute on Aging.
Abbreviations
- AA
African-American
- GRS
genetic risk score
- HANDLS
Healthy Aging in Neighborhoods of Diversity Across the Lifespan
- SLC2A9
solute carrier family 2 (facilitated GLUT), member 9
- SUA
serum uric acid
- UA
uric acid
Footnotes
M. A. B.: had full access to the data used in this paper, performed data management and all statistical analyses and had primary responsibility for the final content; J.-A. C. and M. T. F.-K.: participated in the literature review; M. A. B., J.-A. C., M. T. F.-K., S. M. T., M. K. E. and A. B. Z.: wrote and revised the manuscript; M. A. B., J.-A. C., M. T. F.-K. and A. B. Z.: participated in the plan of analysis; M. T. F.-K., M. K. E. and A. B. Z.: participated in data acquisition; S. M. T.: participated in data management and statistical analysis. All authors read and approved the final version of the manuscript.
None of the authors has any conflicts of interest to declare.
Supplementary material: For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114517000411
References
- 1.Choi H, Mount D, Reginato A. Pathogenesis of gout. Ann Intern Med. 2005;143:499–516. doi: 10.7326/0003-4819-143-7-200510040-00009. [DOI] [PubMed] [Google Scholar]
- 2.George RL, Keenan RT. Genetics of hyperuricemia and gout: implications for the present and future. Curr Rheumatol Rep. 2013;15:309. doi: 10.1007/s11926-012-0309-8. [DOI] [PubMed] [Google Scholar]
- 3.Fang J, Alderman M. Serum uric acid and cardiovascular mortality the NHANES I epidemiologic follow-up study, 1971–1992. National Health and Nutrition Examination Survey. JAMA. 2000;283:2404–2410. doi: 10.1001/jama.283.18.2404. [DOI] [PubMed] [Google Scholar]
- 4.Merriman TR. An update on the genetic architecture of hyperuricemia and gout. Arthritis Res Ther. 2015;17:98. doi: 10.1186/s13075-015-0609-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kontogianni MD, Chrysohoou C, Panagiotakos DB, et al. Adherence to the Mediterranean diet and serum uric acid: the ATTICA study. Scand J Rheumatol. 2012;41:442–449. doi: 10.3109/03009742.2012.679964. [DOI] [PubMed] [Google Scholar]
- 6.Chrysohoou C, Skoumas J, Pitsavos C, et al. Long-term adherence to the Mediterranean diet reduces the prevalence of hyperuricaemia in elderly individuals, without known cardiovascular disease: the Ikaria study. Maturitas. 2011;70:58–64. doi: 10.1016/j.maturitas.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Choi HK, Atkinson K, Karlson EW, et al. Alcohol intake and risk of incident gout in men: a prospective study. Lancet. 2004;363:1277–1281. doi: 10.1016/S0140-6736(04)16000-5. [DOI] [PubMed] [Google Scholar]
- 8.Choi HK, Atkinson K, Karlson EW, et al. Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med. 2004;350:1093–1103. doi: 10.1056/NEJMoa035700. [DOI] [PubMed] [Google Scholar]
- 9.Torralba KD, De Jesus E, Rachabattula S. The interplay between diet, urate transporters and the risk for gout and hyperuricemia: current and future directions. Int J Rheum Dis. 2012;15:499–506. doi: 10.1111/1756-185X.12010. [DOI] [PubMed] [Google Scholar]
- 10.Poletto J, Harima HA, Ferreira SR, et al. Hyperuricemia and associated factors: a cross-sectional study of Japanese-Brazilians. Cad Saude Publica. 2011;27:369–378. doi: 10.1590/s0102-311x2011000200018. [DOI] [PubMed] [Google Scholar]
- 11.Choi JW, Ford ES, Gao X, et al. Sugar-sweetened soft drinks, diet soft drinks, and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2008;59:109–116. doi: 10.1002/art.23245. [DOI] [PubMed] [Google Scholar]
- 12.Gao X, Qi L, Qiao N, et al. Intake of added sugar and sugar-sweetened drink and serum uric acid concentration in US men and women. Hypertension. 2007;50:306–312. doi: 10.1161/HYPERTENSIONAHA.107.091041. [DOI] [PubMed] [Google Scholar]
- 13.Gaffo AL, Roseman JM, Jacobs DR, et al. Serum urate and its relationship with alcoholic beverage intake in men and women: findings from the Coronary Artery Risk Development in Young Adults (CARDIA) cohort. Ann Rheum Dis. 2010;69:1965–1970. doi: 10.1136/ard.2010.129429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Towiwat P, Li ZG. The association of vitamin C, alcohol, coffee, tea, milk and yogurt with uric acid and gout. Int J Rheum Dis. 2015;18:495–501. doi: 10.1111/1756-185X.12622. [DOI] [PubMed] [Google Scholar]
- 15.Rotimi SO, Olayiwola I, Ademuyiwa O, et al. Inability of legumes to reverse diabetic-induced nephropathy in rats despite improvement in blood glucose and antioxidant status. J Med Food. 2010;13:163–169. doi: 10.1089/jmf.2008.0293. [DOI] [PubMed] [Google Scholar]
- 16.Doring A. SLC2A9 influences uric acid concentrations with pronounced sex-specific effects. Nat Genet. 2008;40:430–436. doi: 10.1038/ng.107. [DOI] [PubMed] [Google Scholar]
- 17.Kolz M. Meta-analysis of 28,141 individuals identifies common variants within five new loci that influence uric acid concentrations. PLoS Genet. 2009;5:e1000504. doi: 10.1371/journal.pgen.1000504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brandstatter A. Sex-specific association of the putative fructose transporter SLC2A9 variants with uric acid levels is modified by BMI. Diabetes Care. 2008;31:1662–1667. doi: 10.2337/dc08-0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evans MK, Lepkowski JM, Powe NR, et al. Healthy Aging in Neighborhoods of Diversity Across the Life Span (HANDLS): overcoming barriers to implementing a longitudinal, epidemiologic, urban study of health, race, and socioeconomic status. Ethn Dis. 2010;20:267–275. [PMC free article] [PubMed] [Google Scholar]
- 20.Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88:324–332. doi: 10.1093/ajcn/88.2.324. [DOI] [PubMed] [Google Scholar]
- 21.US Department of Agriculture Agricultural Research Service & Food Surveys Research Group. USDA Food and Nutrient Database for Dietary Studies, 3.0. [accessed February 2017];2016 http://www.ars.usda.gov/Services/docs.htm?docid=12089.
- 22.Reginato AM, Mount DB, Yang I, et al. The genetics of hyperuricaemia and gout. Nat Rev Rheumatol. 2012;8:610–621. doi: 10.1038/nrrheum.2012.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Voruganti VS, Laston S, Haack K, et al. Serum uric acid concentrations and SLC2A9 genetic variation in Hispanic children: the Viva La Familia Study. Am J Clin Nutr. 2015;101:725–732. doi: 10.3945/ajcn.114.095364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang B, Mo Z, Wu C, et al. A genome-wide association study identifies common variants influencing serum uric acid concentrations in a Chinese population. BMC Med Genomics. 2014;7:10. doi: 10.1186/1755-8794-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li C, Yu Q, Han L, et al. The hURAT1 rs559946 polymorphism and the incidence of gout in Han Chinese men. Scand J Rheumatol. 2014;43:35–42. doi: 10.3109/03009742.2013.808375. [DOI] [PubMed] [Google Scholar]
- 26.Kottgen A. Genome-wide association analyses identify 18 new loci associated with serum urate concentrations. Nat Genet. 2013;45:145–154. doi: 10.1038/ng.2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lohr SL. Sampling: Design and Analysis. Boston, MA: Duxbury-Press; 1999. [Google Scholar]
- 28.Ibrahim JG, Molenberghs G. Missing data methods in longitudinal studies: a review. Test (Madr) 2009;18:1–43. doi: 10.1007/s11749-009-0138-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Selvin S. Statistical Analysis of Epidemiologic Data. 3rd. New York: Oxford University Press; 2004. [Google Scholar]
- 30.Hochberg Y, Tamhane AC. Multiple Comparison Procedures. New York: Wiley; 1987. [Google Scholar]
- 31.Beydoun MA, Beydoun HA, Kitner-Triolo MH, et al. Thyroid hormones are associated with cognitive function: moderation by sex, race, and depressive symptoms. J Clin Endocrinol Metab. 2013;98:3470–3481. doi: 10.1210/jc.2013-1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beydoun MA, Beydoun HA, Rostant OS, et al. Thyroid hormones are associated with longitudinal cognitive change in an urban adult population. Neurobiol Aging. 2015;36:3056–3066. doi: 10.1016/j.neurobiolaging.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Witkowska K, Smith KM, Yao SY, et al. Human SLC2A9a and SLC2A9b isoforms mediate electrogenic transport of urate with different characteristics in the presence of hexoses. Am J Physiol Renal Physiol. 2012;303:F527–F539. doi: 10.1152/ajprenal.00134.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Augustin R, Carayannopoulos MO, Dowd LO, et al. Identification and characterization of human glucose transporter-like protein-9 (GLUT9): alternative splicing alters trafficking. J Biol Chem. 2004;279:16229–16236. doi: 10.1074/jbc.M312226200. [DOI] [PubMed] [Google Scholar]
- 35.Anzai N, Kanai Y, Endou H. New insights into renal transport of urate. Curr Opin Rheumatol. 2007;19:151–157. doi: 10.1097/BOR.0b013e328032781a. [DOI] [PubMed] [Google Scholar]
- 36.Matsuo H, Chiba T, Nagamori S, et al. Mutations in glucose transporter 9 gene SLC2A9 cause renal hypouricemia. Am J Hum Genet. 2008;83:744–751. doi: 10.1016/j.ajhg.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Emmerson BT. Effect of oral fructose on urate production. Ann Rheum Dis. 1974;33:276–280. doi: 10.1136/ard.33.3.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Batt C, Phipps-Green AJ, Black MA, et al. Sugar-sweetened beverage consumption: a risk factor for prevalent gout with SLC2A9 genotype-specific effects on serum urate and risk of gout. Ann Rheum Dis. 2014;73:2101–2106. doi: 10.1136/annrheumdis-2013-203600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang M, Jiang X, Wu W, et al. A meta-analysis of alcohol consumption and the risk of gout. Clin Rheumatol. 2013;32:1641–1648. doi: 10.1007/s10067-013-2319-y. [DOI] [PubMed] [Google Scholar]
- 40.Hamajima N, Naito M, Okada R, et al. Significant interaction between LRP2 rs2544390 in intron 1 and alcohol drinking for serum uric acid levels among a Japanese population. Gene. 2012;503:131–136. doi: 10.1016/j.gene.2012.04.064. [DOI] [PubMed] [Google Scholar]
- 41.Rasheed H, Phipps-Green A, Topless R, et al. Association of the lipoprotein receptor-related protein 2 gene with gout and non-additive interaction with alcohol consumption. Arthritis Res Ther. 2013;15:R177. doi: 10.1186/ar4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tu HP, Ko AM, Chiang SL, et al. Joint effects of alcohol consumption and ABCG2 Q141K on chronic tophaceous gout risk. J Rheumatol. 2014;41:749–758. doi: 10.3899/jrheum.130870. [DOI] [PubMed] [Google Scholar]
- 43.Ryu KA, Kang HH, Kim SY, et al. Comparison of nutrient intake and diet quality between hyperuricemia subjects and controls in Korea. Clin Nutr Res. 2014;3:56–63. doi: 10.7762/cnr.2014.3.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Juraschek SP, Miller ER, 3rd, Gelber AC. Effect of oral vitamin C supplementation on serum uric acid: a meta-analysis of randomized controlled trials. Arthritis Care Res (Hoboken) 2011;63:1295–1306. doi: 10.1002/acr.20519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schmidt JA, Crowe FL, Appleby PN, et al. Serum uric acid concentrations in meat eaters, fish eaters, vegetarians and vegans: a cross-sectional analysis in the EPIC-Oxford cohort. PLOS ONE. 2013;8:e56339. doi: 10.1371/journal.pone.0056339. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.