Abstract
Objective
There have been suggestions that patients with subarachnoid hemorrhage (SAH) have a better outcome when treated in high-volume centers. Much of the published literature on the subject is limited by an inability to control for severity of SAH.
Methods
This is a nationwide retrospective cohort analysis using the Nationwide Inpatient Sample (NIS). The NIS Subarachnoid Severity Scale was used to adjust for severity of SAH in multivariate logistic regression modeling.
Results
The records of 47 911 414 hospital admissions from the 2006–2011 NIS samples were examined. There were 11 607 patients who met inclusion criteria for the study. Of these, 7787 (67.0%) were treated at a high-volume center compared with 3820 (32.9%) treated at a low-volume center. Patients treated at high-volume centers compared with low-volume centers were more likely to receive endovascular aneurysm control (58.5% vs 51.2%, P = .04), be transferred from another hospital (35.4% vs 19.7%, P < .01), be treated in a teaching facility (97.3% vs 72.9%, P < .01), and have a longer length of stay (14.9 days [interquartile range 10.3–21.7] vs 13.9 days [interquartile range, 8.9–20.1], P < .01). After adjustment for all baseline covariates, including severity of SAH, treatment in a high-volume center was associated with an odds ratio for death of 0.82 (95% confidence interval, 0.72–0.95; P < .01) and a higher odds of a good functional outcome (odds ratio, 1.16; 95% confidence interval, 1.04–1.28; P < .01).
Conclusion
After adjustment for severity of SAH, treatment in a high-volume center was associated with a lower risk of in-hospital mortality and a higher odds of a good functional outcome.
Keywords: Subarachnoid hemorrhage, Case volume, Outcomes, United States
1. Introduction
Subarachnoid hemorrhage (SAH) is a potentially devastating cerebrovascular insult which affects approximately 30 000 people in the United States each year [1]. The case mortality has decreased in recent years, potentially because of improved aneurysm control techniques and specialized neurocritical care centers [2,3]. Hospital size and case-volume have been examined as potential influences on outcomes for patients with SAH. Some authors have found improved survival for patients treated at high-volume centers [4–10], whereas others have not shown a benefit [11,12]. Many of these analyses have been limited by a lack of control for SAH grade, a fundamental covariate necessary to accurately compare care [4–10]. In analyses where SAH grade was included, the generalizability of these findings is limited because of the single-center nature of these publications [12].
Transfer to a high-volume center is recommended in patients with SAH by numerous societies [1,13]. Although there has been substantial literature published on the potential association of case-volume and improved outcomes for patients with SAH, the bulk of these analyses were completed without controlling for the severity of SAH. It was therefore the objective of this investigation to assess the association with hospital case-volume and outcomes of patients with SAH across the United States while adjusting for severity of hemorrhage.
2. Methods
Our study is reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology statement. A 09 deidentified data set was used for this retrospective cohort analysis, for which a waiver of consent was obtained from the University of British Columbia Institutional Review Board.
The 2 primary outcomes analyzed in this study were in-patient mortality and the Nationwide Inpatient Sample Subarachnoid Outcome Measure (NIS-SOM) [17]. The NIS-SOM was validated to correlate with the modified Rankin score (mRS) and thus reflects a good functional outcome vs not in patients with SAH. Further details on the derivation and validation of this score are available in the article by Washington et al [17].
2.1. Study population
The Nationwide Inpatient Sample (NIS) for the years 2006–2011 were used for this analysis. The NIS is produced by the Agency for Healthcare Research and Quality (AHRQ) and captures approximately 20% of all in-patient hospitalizations across the United States. Using a complex survey design, the NIS is powered to estimate 95% of all in-patient care delivered across the United States [14].
Patients ≥18 years of age with a primary diagnosis of SAH (International Classification of Diseases, Ninth Revision, code 430) were included in the analysis. Only patients that had definitive treatment of their aneurysm were included in the analysis. This was done to isolate a patient population that was deemed salvageable and to remove patients who presented with fatal bleeds. Treatment of aneurysm was defined as the presence of procedure codes for open aneurysm clipping (39.51) or endovascular coiling (39.72, 39.75, 39.76, 39.79). Patients were then segregated into 2 cohorts of hospital types, high-volume (≥20 cases per year) and low-volume centers (<20 cases per year), similar to previous literature and the Joint Commission standards for Advanced Stroke Center Certification [6,15]. A flow diagram for cohort selection is displayed in Figure.
Figure.
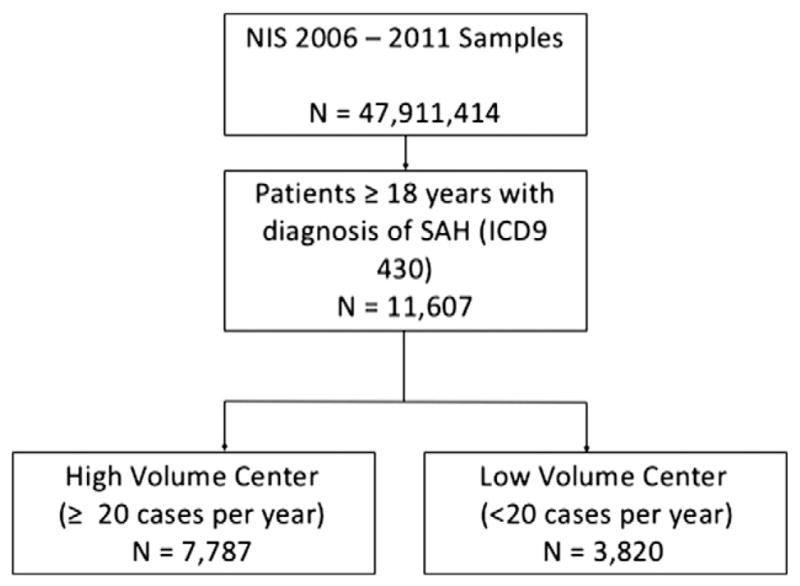
Patient cohort selection diagram.
Patient-level variables obtained from the NIS included age, sex, in-hospital mortality, length of stay, insurance coverage (yes vs no), and patient transfer status (transferred from another hospital vs not). Hospital characteristics acquired included size (small, medium, or large as defined by the AHRQ [14]), location (rural vs urban), teaching status (yes vs no), and region of country (Northeast, Midwest, South, West). We also collected the 29 Elixhauser comorbidity indices for each patient [16].
To control for severity of SAH, we used the Nationwide Inpatient Sample Subarachnoid Severity Score (NIS-SSS) as developed by Washington et al [17]. This validated score correlates with the Hunt and Hess grading scale and is equivalent statistically to the Hunt and Hess score for predicting 6-month outcomes based on the mRS. The variables included in the NIS-SSS are coma (International Classification of Diseases, Ninth Revision, codes 780.01 and 780.03), stupor (780.02, 780.09), paresis/plegia (438.2–438.53, 781.4), aphasia (438.1–438.89), cranial nerve deficits (378.5–378.56, 379.4–379.43), cerebrospinal fluid shunting (02.31–02.39), and mechanical ventilation (96.04, 96.7–96.72).
2.2. Transfer of patients
Patients presenting to peripheral hospitals with SAH may be selectively referred to a higher level of care. If the patient has a high-grade SAH and survival is not expected, the patient may not be transferred. This is an example of selection bias, and it could possibly confound the results of our analysis. To account for this possible bias, we will repeat the analysis excluding all patients at high-volume centers that were transferred in from another institution.
2.3. Statistical analysis
Analyses were performed using SAS v9.4 (Cary, NC) while using complex survey weights provided by the NIS. All analyses incorporated appropriate survey procedures in SAS to accurately compute national projections. Univariate analysis was by χ2 and independent t tests where appropriate. An α level of .05 was used in all cases. In accordance with the AHRQ data use agreement, cells containing less than 10 patients were reported as such to prevent identification of individual patients [18]. Missing data for variables in the final cohort were excluded from individual patient analyses; however, missing data represented less than 1% of data. The only variable with significant missing data was transfer status of patients, with approximately 30% of data missing.
Multivariate logistic regression was used to model the risk of in-hospital mortality and the NIS-SOM. Variables included in the model were age, NIS-SSS, sex, hospital case volume, endovascular control of aneurysm, hospital bed size, hospital region, hospital teaching status, hospital location, and the 29 Elixhauser comorbidity indices. Two models were created for each outcome; the first model included all patients, whereas the second model for each outcome excluded transferred patients.
3. Results
The records of 47 911 414 hospital admissions from the 2006–2011 NIS samples were examined. There were 11 607 patients who met inclusion criteria for the study. Of these, 7787 (67.0%) were treated at a high-volume center compared with 3820 (32.9%) treated at a low-volume center (Table 1). There were 3489 (30.1%) patients who were transferred from another institution in the cohort.
Table 1.
Results of univariate analysis between high-volume and low-volume centers
| High-volume center (n = 7787) | Low-volume center (n = 3820) | P value | |
|---|---|---|---|
| Age in years, mean (SD) | 54.4 (13.7) | 54.5 (13.6) | .76 |
| Length of stay in days, median (IQR) | 14.9 (10.3–21.7) | 13.9 (8.9–20.1) | <.01 |
| Total hospital mortality, n (%) | 864 (11.0) | 542 (14.2) | <.01 |
| Female sex, n (%) | 5339 (68.6) | 2612 (68.5) | .94 |
| Endovascular control of aneurysm, n (%) | 4543 (58.5) | 1952 (51.2) | .04 |
| Patient transferred into hospital, n (%) | 2738 (35.4) | 751 (19.7) | <.01 |
| Insurance coverage, n (%) | 6489 (87.5) | 3124 (81.3) | .24 |
| NIS-SSS, median (IQR) | 2.3 (1–14.9) | 1.8 (1–12.5) | .41 |
| Teaching hospital, n (%) | 7548 (97.3) | 2653 (72.9) | <.01 |
| Urban hospital, n (%) | 7689 (99.1) | 3598 (98.5) | .76 |
| Hospital size, n (%) | |||
| Small | 372 (4.4) | 120 (2.9) | |
| Medium | 764 (10.0) | 623 (17.0) | |
| Large | 6627 (85.5) | 2917 (80.1) | .16 |
| Hospital region, n (%) | |||
| Northeast | 1381 (18.4) | 460 (12.7) | |
| Midwest | 1607 (20.8) | 1010 (26.7) | |
| South | 2577 (32.7) | 1458 (37.6) | |
| West | 2222 (28.1) | 892 (23.0) | .47 |
Patients treated at high-volume centers compared with low-volume centers were more likely to receive endovascular aneurysm control (58.5% vs 51.2%, P = .04), be transferred from another hospital (35.4% vs 19.7%, P < .01), be treated in a teaching facility (97.3% vs 72.9%, P < .01), and have a longer length of stay (14.9 days [interquartile range {IQR}, 10.3–21.7] vs 13.9 days [IQR, 8.9–20.1], P < .01). The unadjusted in-hospital mortality was lower in high-volume centers (11.0% vs 14.2%, P < .01). There was no difference in the severity of SAH between high- and low-volume centers (NIS-SSS median, 2.3 [IQR, 1–14.9] vs 1.8 [IQR, 1–12.5], P = .41).
The results of multivariate logistic regression modeling the outcome of in-hospital mortality are displayed in Table 2. After adjustment for all covariates in the model, including severity of SAH and method of aneurysm control, treatment in a high-volume center was associated with an odds ratio (OR) for death of 0.82 (95% confidence interval [CI], 0.72–0.95; P < .01). To eliminate referral bias, patients who were transferred to a higher level of care were excluded in a prespecified analysis. After only including patients who were not transferred, we observed an OR for death of 0.86 (95% CI, 0.74–1.01; P = .06) for treatment in a high-volume center. In both models, the use of endovascular control was not associated with a difference in mortality (model 1: OR, 1.09; 95% CI, 0.96–1.23; P = .20 and model 2: OR, 1.10; 95% CI, 0.96–1.28; P = .18).
Table 2.
Results of multivariate logistic regression modeling outcome of in-hospital mortality
| OR | 95% CI | P | |
|---|---|---|---|
| Model 1: in-hospital mortality, all patients | |||
| Age, per 5-y increase | 1.16 | 1.13–1.19 | <.01 |
| High-volume center | 0.82 | 0.72–0.95 | <.01 |
| NIS-SSS | 1.021 | 1.020–1.023 | <.01 |
| Endovascular aneurysm control | 1.09 | 0.96–1.23 | .20 |
| Female sex | 1.02 | 0.89–1.16 | .83 |
| Teaching hospital | 0.71 | 0.59–0.87 | <.01 |
| Urban hospital | 0.82 | 0.48–1.40 | .46 |
| Northeast hospital | – | – | |
| Midwest hospital | 0.95 | 0.77–1.18 | .65 |
| South hospital | 1.22 | 1.01–1.48 | .04 |
| West hospital | 1.16 | 0.94–1.41 | .16 |
| Small hospital | – | – | |
| Medium hospital | 1.34 | 0.92–1.94 | .13 |
| Large hospital | 1.23 | 0.88–1.72 | .22 |
| Model 2: in-hospital mortality, excluding transferred patients | |||
| Age, per 5-y increase | 1.15 | 1.11–1.18 | <.01 |
| High-volume center | 0.86 | 0.74–1.01 | .06 |
| NIS-SSS | 1.021 | 1.019–1.023 | <.01 |
| Endovascular aneurysm control | 1.10 | 0.96–1.28 | .18 |
| Female sex | 1.12 | 0.95–1.31 | .17 |
| Teaching HOSPITAL | 0.70 | 0.56–0.86 | <.01 |
| Urban Hospital | 0.99 | 0.54–1.82 | .97 |
| Northeast hospital | |||
| Midwest hospital | 1.02 | 0.79–1.32 | .90 |
| South hospital | 1.27 | 1.01–1.59 | .04 |
| West hospital | 1.27 | 1.00–1.61 | .05 |
| Small hospital | |||
| Medium hospital | 1.63 | 1.05–2.54 | .03 |
| Large hospital | 1.47 | 0.98–2.20 | .06 |
For hospital region, Northeast is the reference; and for hospital size, small hospitals are the reference. Model 1 includes all patients in the cohort, whereas model 2 excludes those patients transferred in from another institution.
The results of multivariate analysis predicting the outcome of NIS-SOM are displayed in Table 3. For all patients in the cohort, treatment at a high-volume center was associated with a higher odds of a good outcome (model 3: OR, 1.16; 95% CI, 1.04–1.28; P < .01). When transferred patients were excluded, the observed increased odds of a favorable outcome at discharge were preserved (model 4: OR, 1.13; 95% CI, 1.01–1.27; P = .04). In both models examining discharge functional status, aneurysm treatment with an endovascular approach compared with an open approach was associated with improved odds of a good outcome (model 3: OR, 1.39; 95% CI, 1.27–1.52; P < .01 and model 4: OR, 1.45; 95% CI, 1.30–1.61; P < .01).
Table 3.
Results of multivariate logistic regression modeling outcome of a good discharge mRS based on the NIS-SOM
| OR | 95% CI | P | |
|---|---|---|---|
| Model 3: NIS-SOM, all patients | |||
| Age, per 5-yincrease | 0.77 | 0.76–0.79 | <.01 |
| High-volume center | 1.16 | 1.04–1.28 | <.01 |
| NIS-SSS | 0.93 | 0.926–0.937 | <.01 |
| Endovascular aneurysm control | 1.39 | 1.27–1.52 | <.01 |
| Female sex | 0.87 | 0.79–0.96 | .01 |
| Teaching hospital | 1.47 | 1.25–1.71 | <.01 |
| Urban hospital | 0.91 | 0.61–1.35 | .63 |
| Northeast hospital | – | – | |
| Midwest hospital | 1.36 | 1.18–1.58 | <.01 |
| South hospital | 1.75 | 1.53–2.00 | <.01 |
| West hospital | 2.06 | 1.78–2.38 | <.01 |
| Small hospital | – | – | |
| Medium hospital | 1.08 | 0.84 | .56 |
| Large hospital | 1.25 | 1.00–1.55 | .05 |
| Model 4: NIS-SOM, excluding transferred patients | |||
| Age, per 5-y increase | 0.77 | 0.76–0.80 | <.01 |
| High-volume center | 1.13 | 1.01–1.27 | .04 |
| NIS-SSS | 0.94 | 0.93–0.95 | <.01 |
| Endovascular aneurysm control | 1.45 | 1.30–1.61 | <.01 |
| Female sex | 0.85 | 0.76–0.96 | <.01 |
| Teaching hospital | 1.48 | 1.25–1.76 | <.01 |
| Urban hospital | 0.87 | 0.58–1.32 | .52 |
| Northeast hospital | – | – | |
| Midwest hospital | 1.31 | 1.09–1.57 | <.01 |
| South hospital | 1.65 | 1.40–1.93 | <.01 |
| West hospital | 1.95 | 1.64–2.32 | <.01 |
| Small hospital | – | – | |
| Medium hospital | 0.94 | 0.70–1.26 | .67 |
| Large hospital | 1.10 | 0.85–1.43 | .45 |
For hospital region, Northeast is the reference; and for hospital size, small hospitals are the reference. Model 3 includes all patients in the cohort, whereas model 4 excludes those patients transferred in from another institution.
4. Discussion
Approximately two thirds of all patients who suffer an aneurysmal SAH and have definitive control of the aneurysm receive treatment in hospitals which meet the Joint Commission requirements for high-volume centers. About 30% of these patients were transferred from another institution. Treatment in a high-volume center was associated with lower rates of in-hospital mortality and a better odds of a good functional outcome even after adjustment for baseline covariates and severity of SAH. After excluding transferred patients, treatment in high-volume centers was still associated with a higher risk of a good functional outcome; however, the CI for in-hospital mortality became nonsignificant.
Potential explanations for the improved hospital survival and functional outcomes of patients treated at high-volume centers have been explored previously. Large referral centers may have specialized neurocritical care units which have been shown to improve outcomes in a variety of neurologic disease [3,19,20]. These centers may also be equipped with interventional neuroradiology departments which offer advanced aneurysm treatment modalities and vasospasm management. Cross et al [4] in 2003 found that only 37% of patients with SAH were treated at centers with endovascular capabilities. It is probable that this percentage has increased since 2003 with the widespread utilization of endovascular therapies for SAH and other conditions.
The recent analysis of Chang et al [12] demonstrating similar outcomes for patients with SAH treated in specialized neurocritical care units regardless of case volume is important to consider. Improved outcomes observed in high-volume centers may reflect the expertise present at these centers more so than an absolute case volume cutoff. An ideal combination of case volume and expertise may maximize the benefit to patients. Determining this optimal mix would allow for more effective hospital planning and treatment algorithms for these patients.
Our finding of a higher percentage of patients at high-volume centers being transferred from another hospital warrants close examination. The transfer of patients to higher levels of care may select for salvageable patients and artificially increase the case mortality at smaller hospitals. If a patient presented with a devastating SAH with a very poor prognosis, instead of transferring to a more specialized center, the patient may have been transitioned toward comfort care. We attempted to control for this by repeating a subgroup analysis including only patients who were not transferred. Future studies are warranted to examine the effects of transportation of SAH patients and to better elucidate the outcomes of these patients.
The strengths of this study lie in its large size and ability to capture the treatment of SAH patients across the entire United States. The NIS is powered to estimate approximately 95% of all US in-patient care by applying complex weights to a 20% sample of all admissions [14]. Previous analyses using the NIS to address this topic by Leake et al [6] were hindered by the inability to control for SAH grade. Using the NIS-SSS in our modeling allowed a more robust comparison of hospital volume and outcomes in SAH. The utilization of the NIS-SOM adds a second well-validated outcome measure to this analysis which goes beyond base mortality and reflects functional outcomes. A 6-month functional outcome would be more informative; however, those data are unfortunately not available in the NIS.
The results of this analysis must be interpreted in the context of its study design. Utilization of large administrative databases contains inherent risk for misclassification and selection bias. Another key limitation of our study is the inability to capture vasospasm incidence and its management. Ideally, more granular information regarding this dreaded complication of SAH would allow for more accurate comparison of case severity between center volumes.
5. Conclusion
Approximately two thirds of all patients with SAH that receive definitive aneurysmal therapy in the United States are treated in high-volume centers. After adjustment for severity of SAH, treatment in a high-volume center was associated with a lower risk of in-hospital mortality and poor functional outcome.
Footnotes
Conflict of interest: No authors have any conflicts of interest to disclose.
References
- 1.Bederson JB, Connolly ES, Batjer HH, Dacey RG, Dion JE, Diringer MN, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke J Cereb Circ. 2009;40:994–1025. doi: 10.1161/STROKEAHA.108.191395. http://dx.doi.org/10.1161/STROKEAHA.108.191395. [DOI] [PubMed] [Google Scholar]
- 2.Rincon F, Rossenwasser RH, Dumont A. The epidemiology of admissions of nontraumatic subarachnoid hemorrhage in the United States. Neurosurgery. 2013;73:217–22. doi: 10.1227/01.neu.0000430290.93304.33. http://dx.doi.org/10.1227/01.neu.0000430290.93304.33 [discussion 212–3] [DOI] [PubMed] [Google Scholar]
- 3.Suarez JI, Zaidat OO, Suri MF, Feen ES, Lynch G, Hickman J, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med. 2004;32:2311–7. doi: 10.1097/01.ccm.0000146132.29042.4c. [DOI] [PubMed] [Google Scholar]
- 4.Cross DT, Tirschwell DL, Clark MA, Tuden D, Derdeyn CP, Moran CJ, et al. Mortality rates after subarachnoid hemorrhage: variations according to hospital case volume in 18 states. J Neurosurg. 2003;99:810–7. doi: 10.3171/jns.2003.99.5.0810. http://dx.doi.org/10.3171/jns.2003.99.5.0810. [DOI] [PubMed] [Google Scholar]
- 5.Prabhakaran S, Fonarow GC, Smith EE, Liang L, Xian Y, Neely M, et al. Hospital case volume is associated with mortality in patients hospitalized with subarachnoid hemorrhage. Neurosurgery. 2014;75:500–8. doi: 10.1227/NEU.0000000000000475. http://dx.doi.org/10.1227/NEU.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 6.Leake CB, Brinjikji W, Kallmes DF, Cloft HJ. Increasing treatment of ruptured cerebral aneurysms at high-volume centers in the United States. J Neurosurg. 2011;115:1179–83. doi: 10.3171/2011.7.JNS11590. http://dx.doi.org/10.3171/2011.7.JNS11590. [DOI] [PubMed] [Google Scholar]
- 7.Boogaarts HD, van Amerongen MJ, de Vries J, Westert GP, Verbeek ALM, Grotenhuis JA, et al. Caseload as a factor for outcome in aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Neurosurg. 2014;120:605–11. doi: 10.3171/2013.9.JNS13640. http://dx.doi.org/10.3171/2013.9.JNS13640. [DOI] [PubMed] [Google Scholar]
- 8.Berman MF, Solomon RA, Mayer SA, Johnston SC, Yung PP. Impact of hospital-related factors on outcome after treatment of cerebral aneurysms. Stroke J Cereb Circ. 2003;34:2200–7. doi: 10.1161/01.STR.0000086528.32334.06. http://dx.doi.org/10.1161/01.STR.0000086528.32334.06. [DOI] [PubMed] [Google Scholar]
- 9.Johnston SC. Effect of endovascular services and hospital volume on cerebral aneurysm treatment outcomes. Stroke J Cereb Circ. 2000;31:111–7. doi: 10.1161/01.str.31.1.111. [DOI] [PubMed] [Google Scholar]
- 10.McNeill L, English SW, Borg N, Matta BF, Menon DK. Effects of institutional caseload of subarachnoid hemorrhage on mortality: a secondary analysis of administrative data. Stroke J Cereb Circ. 2013;44:647–52. doi: 10.1161/STROKEAHA.112.681254. http://dx.doi.org/10.1161/STROKEAHA.112.681254. [DOI] [PubMed] [Google Scholar]
- 11.Hattori N, Katayama Y, Abe T Japan Neurosurgical Society. Case volume does not correlate with outcome after cerebral aneurysm clipping: a nationwide study in Japan. Neurol Med Chir (Tokyo) 2007;47:95–100. doi: 10.2176/nmc.47.95. [discussion 100–1] [DOI] [PubMed] [Google Scholar]
- 12.Chang TR, Kowalski RG, Carhuapoma JR, Tamargo RJ, Naval NS. Impact of case volume on aneurysmal subarachnoid hemorrhage outcomes. J Crit Care. 2015;30:469–72. doi: 10.1016/j.jcrc.2015.01.007. http://dx.doi.org/10.1016/j.jcrc.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 13.Diringer MN, Bleck TP, Claude Hemphill J, Menon D, Shutter L, Vespa P, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit Care. 2011;15:211–40. doi: 10.1007/s12028-011-9605-9. http://dx.doi.org/10.1007/s12028-011-9605-9. [DOI] [PubMed] [Google Scholar]
- 14.Washington CW, Derdeyn CP, Dacey RG, Dhar R, Zipfel GJ. Analysis of subarachnoid hemorrhage using the Nationwide Inpatient Sample: the NIS-SAH Severity Score and Outcome Measure. J Neurosurg. 2014;121:482–9. doi: 10.3171/2014.4.JNS131100. http://dx.doi.org/10.3171/2014.4.JNS131100. [DOI] [PubMed] [Google Scholar]
- 15.HCUP. INTRODUCTION TO THE HCUP NATIONWIDE INPATIENT SAMPLE (NIS) n.d. [Google Scholar]
- 16.Joint Commission Advanced Stroke Center Standards for Case Volume. n.d. [Google Scholar]
- 17.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. http://dx.doi.org/10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 18.HCUP. HCUP AHRQ Data Use Agreement for the Nationwide Inpatient Sample. n.d. [Google Scholar]
- 19.Varelas PN, Conti MM, Spanaki MV, Potts E, Bradford D, Sunstrom C, et al. The impact of a neurointensivist-led team on a semiclosed neurosciences intensive care unit. Crit Care Med. 2004;32:2191–8. doi: 10.1097/01.ccm.0000146131.03578.21. [DOI] [PubMed] [Google Scholar]
- 20.Varelas PN, Schultz L, Conti M, Spanaki M, Genarrelli T, Hacein-Bey L. The impact of a neuro-intensivist on patients with stroke admitted to a neurosciences intensive care unit. Neurocrit Care. 2008;9:293–9. doi: 10.1007/s12028-008-9050-6. http://dx.doi.org/10.1007/s12028-008-9050-6. [DOI] [PubMed] [Google Scholar]


