Abstract
Objective
We sought to prospectively investigate potential effects of alcohol by subtype on reported long-term weight change.
Methods
We examined change in alcohol intake (total, wine, light beer, regular beer, liquor) and simultaneous change in reported body weight within four-year periods from 1986 to 2010 from U.S. men in the Health Professionals Follow-Up Study. We adjusted for age, change in lifestyle and dietary covariates and cardiovascular risk factors.
Results
We observed 44,603 four-year periods from 14,971 men. Total alcohol, total beer, regular beer, and liquor, modeled as the increase in weight per increase in drink/day, were each directly associated with moderate weight gain over four-year periods, in pounds: total alcohol: 0.23 (0.10–0.35); total beer: 0.29 (0.08–0.51); regular beer: 0.61 (0.22–1.00); liquor: 0.28 (0.09–0.48). Results for wine and light beer were wine: 0.16 (−0.04–0.36); light beer: −0.38 (−1.07–0.08). Results were strongest for men <55 years old.
Conclusions
Increased alcohol consumption was associated with minor reported weight gain at levels unlikely to be clinically meaningful. Beverage specific differences are not substantial enough to make dietary recommendations for weight loss or maintenance by beverage type. The greatest risk of weight gain was among men that increased consumption to levels well above moderation.
Keywords: alcohol, body weight, weight change
Introduction
Studies consistently show that moderate alcohol intake is associated with lower risk of cardiovascular disease (CVD)(1, 2) and type 2 diabetes.(3−5) However, the relationship between alcohol intake and body weight is unclear. Typically, alcohol calories supplement rather than replace food calories.(6) Some evidence suggests alcohol intake may even lead to increased food intake(7) through enhancing food reward signals and impairing satiety.(8, 9)
A 2011 systematic review synthesizing evidence from cross-sectional studies, prospective studies, and randomized controlled trials (RCTs) found that evidence on total alcohol intake and body weight is inconclusive(10). A few studies suggested that moderate wine intake may be associated with weight maintenance, while liquor and beer intake may be associated with weight gain.(10) More recent studies continue to be largely inconclusive,(11−17) although most showed no association(16) or an inverse association(14, 15, 17) between wine and body weight. However, there are major limitations to this body of evidence; most of the studies were cross-sectional or retrospective instead of prospective, most did not have information on alcohol subtype, and the few RCTs were too short (≤12 weeks) to assess meaningful weight change. A recent two-year RCT instructing previously non-drinking diabetic patients to drink moderate amounts of red wine, white wine, or water during dinner observed more weight loss in the water groups.(5) However, everyone had type 2 diabetes, and they did not assess other alcoholic beverages. Subtype differences are important to understand for dietary recommendations, and may be due to either the variability in calorie content(18) or nutrient composition (e.g. differences in natural or added sugars, polyphenols, or other constituents).
No study has prospectively investigated the potential effects of alcohol by subtype on long-term weight change. The long-term, prospective, and repeated assessments of alcohol subtype and body weight is a unique advantage of the Health Professionals Follow-Up Study (HPFS) data. We prospectively investigate the relationship between change in alcohol intake and weight change over time among US men.
Methods
We include men from HPFS, an ongoing prospective cohort study of 51,529 middle-aged and older men in the US who were 40−75 years old at 1986 baseline. The Human Subjects’ Committee Review Board at Harvard T.H. Chan School of Public Health has approved the study protocol.
One unit of observation was one four-year period from one alcohol assessment to the next. Between 1986 and 2010, participants completed a validated(19) 131-item semi-quantitative food frequency questionnaire (FFQ) every four years. Thus, we had up to seven FFQs and six measurements of dietary change over six four-year periods. Every questionnaire asked average consumption of red wine, white wine, beer, and liquor intake. Beginning in 1994, regular beer and light beer were asked separately. The average Pearson Correlation coefficients comparing diet assessment from our FFQ with multiple seven-day food records ranged from 0.66 to 0.78 for individual alcohol items.(20)
Men reported height (inches) and reported weight (pounds [lbs]) at baseline and weight biennially thereafter during follow-up. In a validation study, the Pearson correlation coefficient comparing self-reported weight with technician-conducted weight among 123 men in HPFS was 0.97.(21) We calculated weight change every four years, at the same time that alcohol and diet were assessed, by subtracting weight from the beginning of each four-year period from weight at the end of the period. Thus, positive estimates represent an average weight gain and negative values represent an average weight loss associated with a one-drink increase over the four-year period.
Participants also completed biennial questionnaires asking about lifestyle habits, physician-diagnosed diseases, and clinical information. Our primary analyses adjusted for age, body mass index (BMI), smoking status, and calendar year at start of each four-year period, history of high cholesterol, history of high blood pressure, and four-year change in the following time-varying potential confounders: physical activity (MET hours/week), sitting or watching TV (hours/day), sleep (hours/night), and four-year change in the following dietary covariates that may be associated with both alcohol and weight change (servings/day): fried potatoes, fruits, vegetables, juice, whole grains, refined grains, fried foods, processed meat, non-processed meat, nuts, coffee, sweets, non-juice sugar sweetened beverages, diet beverages, whole-fat dairy products, low-fat dairy products, seafood, and trans fat. Beer, wine, and liquor were mutually adjusted for each other, as were regular beer and light beer. When total alcohol intake was the main exposure, the model was not adjusted for any alcohol subtypes. Total wine is the sum of red wine and white wine, total beer is the sum of regular beer and light beer beginning in 1994 (beer subtype was unspecified before 1994). Total alcohol is the sum of total wine, total beer, and total liquor. We used the Harvard University food composition database, which is derived from the US Department of Agriculture and other sources, to calculate nutrient values.
Statistical analysis
We used generalized linear regression models to investigate the association between four-year weight change (lbs, continuous) and simultaneous four-year change in alcohol intake (total, wine, beer, and liquor; servings/day, continuous) as described previously.(22) To investigate the dose-response relationship, we also categorized change in alcohol intake (decreased by ≥2, 1 to <2, or <1 drink/day, no change, increased by <1, 1 to <2, or ≥2 drinks/day). We used robust empirical-based variance to account for within-person correlated error. As most participants contributed multiple observations (one per four-year period), point estimates reflect mean weight change across all four-year periods.
At baseline, we excluded men who had a history of diabetes mellitus, CVD, cancer, renal failure, liver disease, ulcer disease, pulmonary disease, tuberculosis, multiple sclerosis, amyotrophic lateral sclerosis, and Parkinson’s disease. We also excluded men who were ≥65 years (loss of lean body mass increases with age), men who reported that their alcohol intake substantially “increased” or “decreased” within five years before because we could not account for the reasons for change, which could be related independently to weight change, and men who reported a weight loss of >15 lbs within five years before baseline. We censored men four years prior to diagnosis of cancer, renal failure, liver disease, ulcer disease, pulmonary disease, tuberculosis, multiple sclerosis, amyotrophic lateral sclerosis, and Parkinson’s disease, as they may result in substantial weight loss. We censored men at time of diagnosis of CVD or diabetes mellitus, gastric bypass surgery, and at age 65. We skipped four-year periods missing alcohol or weight information, those with implausible energy intake (<800 or >4200 kcals/day), or if a participant had BMI >30 at the beginning of the period. After exclusions, 14,971 men contributed 44,603 four-year periods of observation. Table S1 provides counts for these exclusions.
To minimize the influence of outliers, we winsorized change in all weight, alcohol, and dietary covariate values at the 0.5th and 99.5th percentiles. For missing data, we used missing indicators for categorical covariates and carried forward the last reported value for continuous covariates. This is equivalent to assuming that covariate value did not change during the four-year period. For alcohol and weight, missing values were carried forward a maximum of one time; any four-year change period requiring a second consecutive missing value was skipped. When investigating light and regular beer, we only included information from 1994 onward, when they were first asked separately; we did not carry forward information from questionnaires prior to 1994 for these analyses.
To test whether subtypes were associated with significantly different weight gain, we conducted three 2-way Wald tests comparing the coefficients for beer, wine, and liquor in our main analysis.
To explore effect modification by age, BMI, and alcohol intake at the start of the four-year period, we stratified on BMI (<25, 25 to <27.5, and 27.5 to <30 kg/m2), age (<55, 55 to <60, and 60 to <65 years), and baseline total alcohol intake (<1, >1 to 2, and >2 to 4 drinks/day), with separate models for each covariate category. We reported p-values for multiplicative interaction terms between the categorical stratification variable and continuous alcohol change variable to assess interaction.
The main analyses did not adjust for change in total energy; in contrast to most dietary components, alcohol is likely not consumed in replacement of other components.(6−9) However, we included an alternate model additionally adjusted for change in total energy. We also conducted sensitivity analyses to test the robustness of associations observed in our primary analyses: 1) omitting observations missing exposure, outcome, or covariate values in the beginning or end of the period (as opposed to using observations with missing values as described above); 2) adjusting for 1986 baseline BMI instead of BMI at the start of each period; 3) without adjusting for dietary covariates; 4) additionally adjusting for weight and total alcohol intake at the start of each four-year period; 5) various different exclusion criteria. We used SAS version 9.2 (SAS Institute) and 0.05 two-tailed alpha level for all analyses.
Results
The 14,971 men included in our analysis contributed an average of 3.0 four-year observation periods over follow-up. Table 1 shows average four-year changes in lifestyle and dietary factors according to simultaneous change in total alcohol intake. Men gained an average of 2.0 lbs during each period. Most time-varying covariates did not differ according to change in alcohol intake, although change in alcohol intake corresponded directly with change in hours/week of TV watching (r <0.001). During four-year periods with increased alcohol intake, total calorie intake increased beyond calories from increased alcohol. The range for total alcohol change after truncating extreme values was −3.5 to 2.4 servings/day from 1986 to 1990 and −3.2 to 2.9 servings/day from 2006 to 2010. Table S2 shows mean covariate values, rather than change in values, at 1986 baseline according to change in alcohol intake from 1986 to 1990.
Table 1.
Average 4-year changes (Δ) in lifestyle and dietary factors according to simultaneous 4-year changes in total alcohol intake1, among HPFS men without obesity, 1986–2010. (n=14,971 men contributing 44,603 4-year periods)
| Change in Total Alcohol Intake | ||||
|---|---|---|---|---|
| Increased intake |
No change | Decreased intake |
Total | |
| # 4-year periods | 4,977 | 34,860 | 4,766 | 44,603 |
|
| ||||
| Alcohol (Δservings/day) | ||||
| Total Alcohol | 1.16 | 0.00 | −1.23 | 0.00 |
| Beer | 0.32 | −0.01 | −0.43 | −0.01 |
| Wine | 0.45 | 0.01 | −0.37 | 0.02 |
| Liquor | 0.35 | 0.00 | −0.38 | 0.00 |
| Smoking Status (%)3 | ||||
| Never | 47 | 60 | 42 | 57 |
| Past | 45 | 33 | 48 | 36 |
| Current | 8 | 7 | 10 | 7 |
| BMI (Δkg/m2) | 0.36 | 0.31 | 0.24 | 0.31 |
| Weight (Δpounds) | 2.37 | 2.05 | 1.55 | 2.03 |
| Physical Activity (ΔMET-hr/wk)2 | ||||
| Total | 5.92 | 5.28 | 6.42 | 5.47 |
| Vigorous | 2.01 | 0.42 | 2.26 | 0.79 |
| TV watching (Δhours/week) | 0.25 | −0.13 | −0.52 | −0.13 |
| Dietary Covariates (ΔServings/Day) | ||||
| Total fruit without juice | 0.10 | 0.07 | 0.08 | 0.07 |
| Total vegetables | 0.37 | 0.18 | 0.17 | 0.20 |
| Whole-fat dairy | −0.04 | −0.07 | −0.11 | −0.07 |
| Low-fat dairy | −0.10 | −0.06 | 0.00 | −0.06 |
| Seafood | 0.00 | 0.00 | −0.02 | −0.01 |
| Whole grains | −0.03 | −0.03 | −0.01 | −0.03 |
| Refined grains | 0.06 | −0.03 | −0.06 | −0.02 |
| Nuts | 0.06 | 0.02 | 0.01 | 0.03 |
| Coffee | 0.03 | −0.05 | −0.14 | −0.05 |
| Sugary soft drinks | 0.00 | −0.02 | −0.03 | −0.02 |
| Low-calorie soft drinks | −0.02 | 0.00 | 0.01 | 0.00 |
| Juice | 0.01 | −0.01 | −0.03 | −0.01 |
| Sweets | 0.03 | −0.02 | −0.02 | −0.01 |
| Processed meats | 0.01 | −0.02 | −0.04 | −0.01 |
| Non-processed meats | 0.01 | −0.02 | −0.04 | −0.02 |
| Fried food away from home | −0.02 | −0.02 | −0.03 | −0.02 |
| Trans fat (Δg/day)) | −0.14 | −0.03 | 0.08 | −0.03 |
| Calories (Δkcal/day) | 213.86 | −5.79 | −187.81 | −0.73 |
A "decrease" is defined as a decrease in ≥0.5 drinks per day; an "increase" is defined as an increase in ≥0.5 drinks per day.
The apparent increase in physical activity over time is an artifact of physical activity assessment becoming more comprehensive over time. 1986 values include walking, stairs, jogging, running, biking, swimming, tennis, racquet sports, and rowing. Outdoor work was added in 1988. Weightlifting was added in 1990. Aerobic exercise was added in 2010.
Smoking status based on report from the beginning of the four-year period.
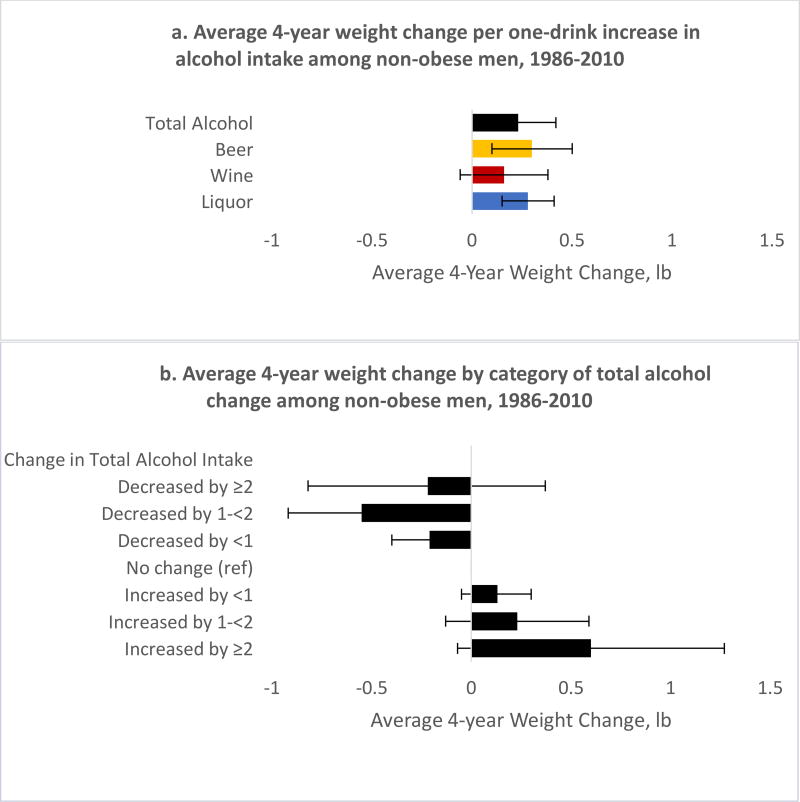
Table 2 (and Figure 1) shows age-adjusted and multivariable-adjusted results for the association between four-year change in alcohol intake (total, beer, wine, liquor) and simultaneous weight change. Based on multivariable-adjusted models, one-drink increases of total alcohol, total beer, liquor, or regular beer were each directly associated with the following moderate but significant mean weight gain over four-year periods (mean weight change [lbs], 95% CI): total alcohol (0.23, 0.10−0.35); total beer (0.29, 0.08−0.51); regular beer (0.61, 0.22−1.00); liquor (0.28, 0.09−0.48) (Table 2a and Figure 1a). Wine was not associated with weight change (0.16, −0.04, 0.36). Weight change did not significantly differ by alcohol subtype (beer vs. wine: p=0.38, beer vs. liquor: p=0.92, wine vs. liquor: p=0.40). There was a roughly linear dose-response relationship. Compared to those who did not change their alcohol intake, those who increased intake by ≥2 drinks/day gained an average of 0.62 lbs; those who increased by 1 to <2 drinks/day gained an average of 0.20 lbs; those who increased by <1 drinks/day gained an average of 0.13 lbs; those who decreased by <1 drink/day lost an average of 0.21 lbs; those who decreased by 1 to ≤2 lost an average of 0.55 lbs. Those who decreased intake by ≥2 drinks/day did not change weight, on average (Table 2b and Figure 2b).
Table 2.
4-year weight change (lb) according to change in alcohol intake among HPFS men without obesity, 1986–2010 (n=14,971 men contributing 44,603 4-year periods)
| 2a. Average weight change, lb (95% CI) for every one-drink continuous change in alcohol consumption | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Age-Adjusted Model1 |
p- value |
Multivariable- Adjusted Model2 |
p-value | Multivariable2 + Total Energy Adjusted Model |
p-value | |
|
|
||||||
| Total Alcohol | 0.20 (0.08, 0.32) | 0.001 | 0.23 (0.10, 0.35) | <0.001 | 0.19 (0.06, 0.32) | 0.004 |
| Beer | 0.30 (0.09, 0.52) | 0.006 | 0.29 (0.08, 0.51) | 0.008 | 0.25 (0.03, 0.47) | 0.03 |
| Wine | 0.09 (−0.11, 0.29) | 0.40 | 0.16 (−0.04, 0.36) | 0.11 | 0.13 (−0.07, 0.33) | 0.21 |
| Liquor | 0.28 (0.08, 0.48) | 0.007 | 0.28 (0.09, 0.48) | 0.005 | 0.26 (0.05, 0.46) | 0.01 |
| 2b. Average weight change, lb (95% CI) by category of total alcohol change | ||||
|---|---|---|---|---|
|
| ||||
| Age-Adjusted Model1 |
Multivariable- Adjusted Model2 |
Multivariable2 + Total Energy Adjusted Model |
||
|
|
||||
| Total Alcohol | # 4-year periods | |||
| Decreased by ≥2 drinks/day | 745 | 0.03 (−0.57, 0.64) | −0.24 (−0.84, 0.36) | −0.15 (−0.76, 0.46) |
| Decreased by 1–<2 drinks/day | 1,585 | −0.52 (−0.90, −0.15) | −0.55 (−0.93, −0.18) | −0.51 (−0.88, −0.13) |
| Decreased by <1 drink/day | 7,102 | −0.22 (−0.40, −0.03) | −0.21 (−0.39, −0.03) | −0.20 (−0.38, −0.01) |
| No change3 | 25,365 | 0.00 (ref) | 0.00 (ref) | 0.00 (ref) |
| Increased by <1 drink/day | 7,461 | 0.13 (−0.05, 0.30) | 0.13 (−0.05, 0.31) | 0.11 (−0.07, 0.29) |
| Increased by 1–<2 drinks/day | 1,702 | 0.27 (−0.09, 0.63) | 0.20 (−0.15, 0.56) | 0.16 (−0.21, 0.52) |
| Increased by ≥2 drinks/day | 643 | 0.62 (−0.04, 1.28) | 0.62 (−0.04, 1.27) | 0.52 (−0.14, 1.19) |
Age-adjusted models are adjusted for age (years) at start of each 4-year period
Multivariable-adjusted models are adjusted for age (years) at start of each 4-year period, year (at start of 4-year period), history of high cholesterol (ever, never), history of high blood pressure (ever, never), 4-year change in the following time-varying covariates: smoking status (current, past, never), total physical activity (MET hours per week), vigorous physical activity (MET hours per week), watching TV (hours per week), sleep (hours per night), and 4-year change in the following dietary covariates (servings/day): fried potatoes, fruits, vegetables, juice, whole grains, refined grains, fried foods, processed meat, non-processed meat, nuts, coffee, sweets, sugar sweetened beverages (other than juice), diet beverages, whole-fat dairy products, low-fat dairy products, seafood, and trans fat. Beer, wine, and liquor were also mutually adjusted for each other. When total alcohol intake was the main exposure models were not adjusted for any alcohol subtypes.
No change was defined as changing by less than 1 drink per week (0.14 drinks per day).
Figure 1.
Figure 2.
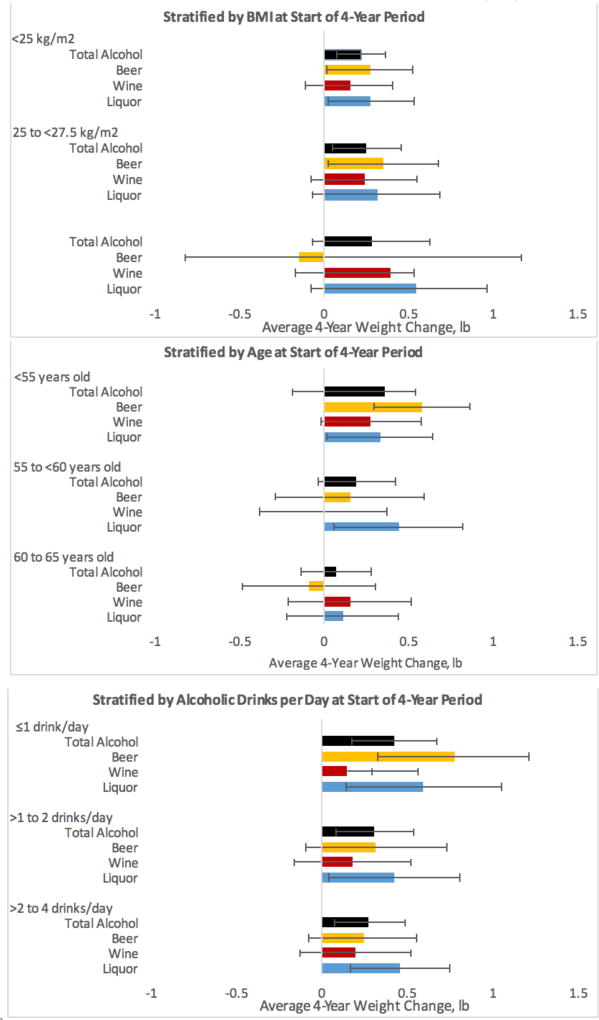
Average 4-year weight change by per one-drink increase in alcohol intake among non-obese men, 1986−2010, stratified on characteristics at start of 4-year period
Table 3 (and Figure 2) shows results stratified by BMI, age, and alcohol intake at the start of the four-year period. BMI did not modify any of the associations. The significant interaction between change in total alcohol and age (pinteraction=0.01) appeared to be driven primarily by change in beer; change in beer intake was associated with less weight gain among older men (pinteraction=0.002). There was also a significant interaction between category of alcohol intake at the start of the four-year period and liquor; however, the mean weight change across these categories was not meaningfully different.
Table 3.
4-year weight change (lb) for every 1 drink per day change in alcohol intake among HPFS men without obesity2, 1986–2010 (n=14,971 men contributing 44,603 4-year periods)
| Weight Change, lb (95% CI) |
P-value | Weight Change, lb (95% CI) |
P-value | Weight Change, lb (95% CI) |
P-value | P- interaction |
|
|---|---|---|---|---|---|---|---|
|
|
|||||||
| BMI at start of 4-year period | |||||||
| BMI <25 kg/m2 | BMI 25 to <27.5 kg/m2 | BMI 27.5 to <30 kg/m2 | |||||
| # 4-year periods | 21,961 | 15,733 | 6,909 | ||||
| Total Alcohol | 0.21 (0.06, 0.36) | 0.006 | 0.24 (0.04, 0.44) | 0.02 | 0.31 (−0.04, 0.65) | 0.08 | 0.47 |
| Beer | 0.27 (0.01, 0.52) | 0.04 | 0.31 (−0.07, 0.68) | 0.11 | 0.54 (−0.08, 1.17) | 0.09 | 0.39 |
| Wine | 0.15 (−0.11, 0.40) | 0.26 | 0.31 (−0.02, 0.63) | 0.06 | −0.03 (−0.69, 0.63) | 0.93 | 0.82 |
| Liquor | 0.26 (0.00, 0.52) | 0.05 | 0.26 (−0.06, 0.58) | 0.11 | 0.35 (−0.21, 0.92) | 0.22 | 0.63 |
| Age at start of 4-year period | |||||||
| <55 years old | 55 to <60 years old | 60 to 65 years old | |||||
| # 4-year periods | 22,360 | 10,651 | 11,592 | ||||
| Total Alcohol | 0.37 (0.19, 0.54) | <0.001 | 0.21 (−0.02, 0.43) | 0.08 | 0.06 (−0.16, 0.27) | 0.61 | 0.01 |
| Beer | 0.57 (0.28, 0.85) | <0.001 | 0.14 (−0.30, 0.58) | 0.53 | −0.09 (−0.48, 0.30) | 0.64 | 0.002 |
| Wine | 0.28 (−0.02, 0.57) | 0.07 | 0.03 (−0.34, 0.40) | 0.88 | 0.13 (−0.23, 0.49) | 0.47 | 0.29 |
| Liquor | 0.32 (0.01, 0.64) | 0.04 | 0.44 (0.06, 0.83) | 0.02 | 0.10 (−0.24, 0.44) | 0.56 | 0.27 |
| Total alcohol intake (drinks/day) at start of 4-year period | |||||||
| ≤1 drinks/day | >1 to 2 drinks/day | >2 to 4 drinks/day | |||||
| # 4-year periods | 29,329 | 8,749 | 5,360 | ||||
| Total Alcohol | 0.43 (0.18, 0.68) | 0.001 | 0.29 (0.07, 0.51) | 0.01 | 0.29 (0.09, 0.49) | 0.005 | 0.04 |
| Beer | 0.78 (0.34, 1.23) | 0.001 | 0.32 (−0.10, 0.73) | 0.14 | 0.24 (−0.08, 0.56) | 0.15 | 0.06 |
| Wine | 0.12 (−0.30, 0.54) | 0.57 | 0.18 (−0.16, 0.52) | 0.31 | 0.22 (−0.12, 0.56) | 0.20 | 0.90 |
| Liquor | 0.60 (0.14, 1.06) | 0.01 | 0.38 (0.01, 0.76) | 0.04 | 0.47 (0.16, 0.78) | 0.003 | 0.04 |
Multivariable-adjusted models are adjusted for age (years) at start of each 4-year period, year (at start of 4-year period), history of high cholesterol (ever, never), history of high blood pressure (ever, never), 4-year change in the following time-varying covariates: smoking status (current, past, never), total physical activity (MET hours per week), vigorous physical activity (MET hours per week), watching TV (hours per week), sleep (hours per night), and 4-year change in the following dietary covariates (servings/day): fried potatoes, fruits, vegetables, juice, whole grains, refined grains, fried foods, processed meat, non-processed meat, nuts, coffee, sweets, sugar sweetened beverages (other than juice), diet beverages, whole-fat dairy products, low-fat dairy products, seafood, and trans fat. Beer, wine, and liquor were also mutually adjusted for each other. When total alcohol intake was the main exposure models were not adjusted for any alcohol subtypes. Models were not adjusted for the stratification variable.
Men with obesity are not included in any other part of this analysis
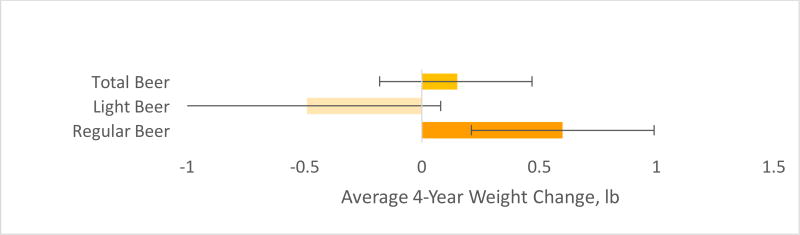
Table 4 (and Figure 3) shows age-adjusted and multivariable-adjusted results for the association between four-year change in regular and light beer and simultaneous weight change. A one-drink increases in regular beer was directly associated with a 0.61 (0.22−1.00) lb weight gain. We did not see an association for light beer.
Table 4.
4-year weight change (lb) for every simultaneous 1 drink per day change in alcohol intake among HPFS men without obesity, 1994–2010 (n=7,371 men contributing 17,485 4-year periods)
| Weight Change, lb (95% CI) |
p-value | Weight Change, lb (95% CI) |
p-value | Weight Change, lb (95% CI) |
p-value | |
|---|---|---|---|---|---|---|
|
|
||||||
| Age-Adjusted Model1 | Multivariable-Adjusted Model2 | Multivariable + total energy | ||||
| Total Beer | 0.08 (−0.24, 0.40) | 0.61 | 0.15 (−0.17, 0.47) | 0.36 | 0.13 (−0.19, 0.46) | 0.43 |
| Light Beer | −0.83 (−1.39, −0.27) | 0.004 | −0.50 (−1.07, 0.08) | 0.09 | −0.51 (−1.08, 0.07) | 0.09 |
| Regular Beer | 0.66 (0.28, 1.04) | 0.001 | 0.61 (0.22, 1.00) | 0.002 | 0.60 (0.20, 1.00) | 0.004 |
Age-adjusted models are adjusted for age (years) at start of each 4-year period
Multivariable-adjusted models are adjusted for age (years) at start of each 4-year period, year (at start of 4-year period), history of high cholesterol (ever, never), history of high blood pressure (ever, never), 4-year change in the following time-varying covariates: smoking status (current, past, never), total physical activity (MET hours per week), vigorous physical activity (MET hours per week), watching TV (hours per week), sleep (hours per night), and 4-year change in the following dietary covariates (servings/day): fried potatoes, fruits, vegetables, juice, whole grains, refined grains, fried foods, processed meat, non-processed meat, nuts, coffee, sweets, sugar sweetened beverages (other than juice), diet beverages, whole-fat dairy products, low-fat dairy products, seafood, and trans fat, wine (drinks/day), liquor (drinks/day). Light beer and regular beer were mutually adjusted for each other.
Figure 3.
Average 4-year weight change (lb) per one-drink increase in beer intake among non-obese men, 1994−2010
Results from alternate version of our multivariate models are virtually identical to our original model (Table S3). Increased light beer was associated with weight gain when men were <55 years old, but null for older age groups(pinteraction=0.01). Increased regular beer was associated with significant weight gain for men <55 years old, and weight loss for men 60−65 years old (Table S4). Associations were not substantially different among men with obesity, although liquor appeared to be more strongly associated with weight gain (Table S5). We also conducted several sensitivity analyses to see if our findings were robust to various baseline exclusions (not excluding men ≥65 years old, men who reported a significant change in alcohol intake 5 years before baseline, and men who reported ≥15 pound weight loss before baseline; Table S6). Our results were robust to these sensitivity analyses.
Discussion
We prospectively assessed alcohol intake every four years from 1986 to 2010, and found that four-year increases in total alcohol, total beer, regular beer, and liquor intake were each associated with minimal reported four-year weight gain (i.e. all less than 0.3 lbs per 1 drink per day increase over 4 years). These associations did not significantly differ by alcohol subtype. Although not statistically different, liquor appeared to be associated with more weight gain, whilechanges in wine and light beer were not significantly associated with weight change. We observed a steady dose-response relationship between changes in alcohol and weight change.
We found that change in beer has a stronger effect on reported weight among younger men. However, we suspect that the relationship between beer and adiposity is roughly constant across ages. As men age, they tend to lose muscle mass more quickly(23). It is likely that an older man who maintained his weight actually gained a comparable amount of adiposity as a younger man who gained weight. The dose-response relationship did not hold for men who decreased by ≥2 drinks/day; it is possible that this was due to small sample size or men who drastically decreased alcohol intake may be compensating with increased food intake and other behavioral changes. Studies of alcohol subtype and body weight are limited, but our results are consistent overall. Most studies also found that beer and liquor intake were associated with greater weight gain than wine.(5, 10, 11, 16, 17). However, all existing studies investigating alcohol subtype and weight gain are either cross-sectional(10, 14) retrospective(10, 11), prospective with only one alcohol measurement(10, 16, 17), or from short RCTs5 or in diabetic population only(5).
It is unclear whether the minor weight gain associated with increased alcohol consumption is due to alcohol or increased food intake(7). Clinical studies suggest that alcohol may impair satiety and activate food reward signaling. We also observe that when men increase alcohol, they increase their total calories beyond calories from alcohol.
Lastly, our finding that moderate alcohol increase is associated with minor – and unlikely clinically meaningful(24) – weight gain is consistent with a recent analysis that found that moderate alcohol attenuated the association between the genetic risk score (GRS) and BMI, suggesting that moderate alcohol may mitigate a genetic predisposition to having obesity(25).
HPFS data allowed us to conduct the most comprehensive study of alcohol and weight change to date. Almost all other studies investigating this relationship have major limitations, described above. We have a large study population, regular assessment of exposure and outcome, and long follow-up. Multiple within-person assessments allow us to indirectly adjust for within-person variation and reporting error. The prospective design minimizes recall bias, especially relative to cross-sectional and retrospective studies. In our validated FFQ(26). alcohol reports are highly correlated with food records(27). Ours is one of the only studies with long-term information on alcohol subtype, and the only study to date able to distinguish between light beer and regular beer. We were able to adjust for many potential clinical, lifestyle, and dietary confounders. The relative demographic homogeneity of our population is a potential advantage; it helps reduce residual confounding by unmeasured lifestyle characteristics associated with alcohol intake patterns.
There are also potential limitations. As in all prospective studies, despite adjusting for many confounding variables, there remains potential for unmeasured and residual confounding. It is unlikely that results of a randomized trial long enough to test the effects of drinking on weight with precision will be available anytime in the near future. Our population was ethnically and socioeconomically homogenous (>90% Caucasian and all health professionals), which reduces confounding but also potentially limits generalizability to other ethnicities and demographics. Social norms may have encouraged heavy drinkers to differentially underreport intake. All dietary assessment methods have measurement error. Additionally, the FFQ does not distinguish between “mixed drinks” and “shots”; thus, it is uncertain whether the association between liquor and weight gain is from only liquor or the mixer as well. However, adjusting for juice and sugary beverages likely partially accounted for this. While adult weight change typically represents change in adiposity, and while we exclude men more than 65 years old, weight change may also be capturing loss of muscle mass. Results could also be partially attributable to reverse causation; if men who gained weight at the beginning of the four-year period reduced alcohol intake later in an effort to lose weight, this could attenuate a positive association between alcohol intake and weight gain.
Conclusions
Our findings suggest that increased alcohol consumption is associated with minor weight gain that is unlikely to be clinically meaningful. This supports that light to moderate consumption of alcohol can be part of a healthy diet. However, major increases in alcohol beyond 2 drinks/day (the maximum recommended moderate alcohol intake level for men) are inadvisable as there appears to be a dose-dependent relationship between alcohol change and weight change. It is also crucial to consider the other health and safety consequences related to excess alcohol consumption.
Supplementary Material
Study Importance Questions.
What is already known?
Alcohol is associated with lower risk of cardiovascular disease and type 2 diabetes
Typically, alcohol calories supplement rather than replace food calories, and may even lead to increased food intake
What does this study add?
The relationship between alcohol intake and body weight is unclear; No study has prospectively investigated the potential effects of alcohol by subtype on long-term weight change.
We are able to address this using long-term, prospective, repeated assessments of alcohol subtype and body weight
Acknowledgments
We would like to thank all HPFS participants for their important contributions to this research.
Funding: UM1 CA167552, R01 HL35464
Funding sources played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Researchers are independent of funders.
Footnotes
Disclosure: There are no potential conflicts of interst.
- Mary Kathryn Downer: ideation, statistical programming and data analysis, manuscript writing, submission
- Monica Bertoia: statistical program review and assistance, data analysis, manuscript editing
- Ken Mukamal: ideation, expert substantive and methodological advice, manuscript editing
- Eric Rimm: ideation, expert substantive and methodological advice, manuscript editing
- Meir Stampfer: ideation, expert substantive and methodological advice, manuscript editing
References
- 1.Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rimm E. Alcohol and cardiovascular disease. Curr Atheroscler Rep. 2000;2(6):529–35. doi: 10.1007/s11883-000-0054-8. [DOI] [PubMed] [Google Scholar]
- 3.Baliunas DO, Taylor BJ, Irving H, Roerecke M, Patra J, Mohapatra S, et al. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2009;32(11):2123–32. doi: 10.2337/dc09-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stampfer MJ, Colditz GA, Willett WC, Manson JE, Arky RA, Hennekens CH, et al. A prospective study of moderate alcohol drinking and risk of diabetes in women. Am J Epidemiol. 1988;128(3):549–58. doi: 10.1093/oxfordjournals.aje.a115002. [DOI] [PubMed] [Google Scholar]
- 5.Golan R, Shelef I, Shemesh E, Henkin Y, Schwarzfuchs D, Gepner Y, et al. Effects of initiating moderate wine intake on abdominal adipose tissue in adults with type 2 diabetes: a 2-year randomized controlled trial. Public Health Nutr. 2016:1–7. doi: 10.1017/S1368980016002597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colditz GA, Giovannucci E, Rimm EB, Stampfer MJ, Rosner B, Speizer FE, et al. Alcohol intake in relation to diet and obesity in women and men. Am J Clin Nutr. 1991;54(1):49–55. doi: 10.1093/ajcn/54.1.49. [DOI] [PubMed] [Google Scholar]
- 7.Breslow RA, Chen CM, Graubard BI, Jacobovits T, Kant AK. Diets of drinkers on drinking and nondrinking days: NHANES 2003–2008. Am J Clin Nutr. 2013;97(5):1068–75. doi: 10.3945/ajcn.112.050161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeomans MR. Effects of alcohol on food and energy intake in human subjects: evidence for passive and active over-consumption of energy. Br J Nutr. 2004;92(Suppl 1):S31–4. doi: 10.1079/bjn20041139. [DOI] [PubMed] [Google Scholar]
- 9.Schrieks IC, Stafleu A, Griffioen-Roose S, de Graaf C, Witkamp RF, Boerrigter-Rijneveld R, et al. Moderate alcohol consumption stimulates food intake and food reward of savoury foods. Appetite. 2015;89:77–83. doi: 10.1016/j.appet.2015.01.021. [DOI] [PubMed] [Google Scholar]
- 10.Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutr Rev. 2011;69(8):419–31. doi: 10.1111/j.1753-4887.2011.00403.x. [DOI] [PubMed] [Google Scholar]
- 11.Bergmann MM, Schutze M, Steffen A, Boeing H, Halkjaer J, Tjonneland A, et al. The association of lifetime alcohol use with measures of abdominal and general adiposity in a large-scale European cohort. Eur J Clin Nutr. 2011;65(10):1079–87. doi: 10.1038/ejcn.2011.70. [DOI] [PubMed] [Google Scholar]
- 12.Chakraborty S. Analysis of NHANES 1999–2002 data reveals noteworthy association of alcohol consumption with obesity. Ann Gastroenterol. 2014;27(3):250–7. [PMC free article] [PubMed] [Google Scholar]
- 13.Lourenco S, Oliveira A, Lopes C. The effect of current and lifetime alcohol consumption on overall and central obesity. Eur J Clin Nutr. 2012;66(7):813–8. doi: 10.1038/ejcn.2012.20. [DOI] [PubMed] [Google Scholar]
- 14.Dumesnil C, Dauchet L, Ruidavets JB, Bingham A, Arveiler D, Ferrieres J, et al. Alcohol consumption patterns and body weight. Ann Nutr Metab. 2013;62(2):91–7. doi: 10.1159/000342839. [DOI] [PubMed] [Google Scholar]
- 15.MacInnis RJ, Hodge AM, Dixon HG, Peeters A, Johnson LE, English DR, et al. Predictors of increased body weight and waist circumference for middle-aged adults. Public Health Nutr. 2014;17(5):1087–97. doi: 10.1017/S1368980013001031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sayon-Orea C, Bes-Rastrollo M, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Martinez-Gonzalez MA. Type of alcoholic beverage and incidence of overweight/obesity in a Mediterranean cohort: the SUN project. Nutrition. 2011;27(7–8):802–8. doi: 10.1016/j.nut.2010.08.023. [DOI] [PubMed] [Google Scholar]
- 17.Thomson CA, Wertheim BC, Hingle M, Wang L, Neuhouser ML, Gong Z, et al. Alcohol consumption and body weight change in postmenopausal women: results from the Women's Health Initiative. Int J Obes (Lond) 2012;36(9):1158–64. doi: 10.1038/ijo.2012.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agriculture UDo. USDA National Nutrient Database for Standard Reference, Release 28, 2015. Nutrient Data Laboratory Home Page. 2015 [Google Scholar]
- 19.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992;135(10):1114–26. doi: 10.1093/oxfordjournals.aje.a116211. discussion 27–36. [DOI] [PubMed] [Google Scholar]
- 20.Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, et al. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr. 1999;69(2):243–9. doi: 10.1093/ajcn/69.2.243. [DOI] [PubMed] [Google Scholar]
- 21.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1(6):466–73. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deschenes MR. Effects of aging on muscle fibre type and size. Sports Med. 2004;34(12):809–24. doi: 10.2165/00007256-200434120-00002. [DOI] [PubMed] [Google Scholar]
- 24.Adams KF, Leitzmann MF, Ballard-Barbash R, Albanes D, Harris TB, Hollenbeck A, et al. Body mass and weight change in adults in relation to mortality risk. Am J Epidemiol. 2014;179(2):135–44. doi: 10.1093/aje/kwt254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ding MEC, Huang T, Jensen MK, et al. Diet Quality and Genetic Association with Body Mass Index (BMI) PLoS Med (under review) 2017 [Google Scholar]
- 26.Chiva-Blanch G, Arranz S, Lamuela-Raventos RM, Estruch R. Effects of wine, alcohol and polyphenols on cardiovascular disease risk factors: evidences from human studies. Alcohol Alcohol. 2013;48(3):270–7. doi: 10.1093/alcalc/agt007. [DOI] [PubMed] [Google Scholar]
- 27.Pan A, Malik VS, Hao T, Willett WC, Mozaffarian D, Hu FB. Changes in water and beverage intake and long-term weight changes: results from three prospective cohort studies. Int J Obes (Lond) 2013;37(10):1378–85. doi: 10.1038/ijo.2012.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.