Abstract
Background
This study reports dose-response estimates for the odds ratio (OR) and population attributable risk of acute alcohol use and road traffic injury (RTI).
Methods
Data were analyzed on 1,119 RTI patients arriving at 16 emergency departments (EDs) in Argentina, Brazil, Costa Rica, Dominican Republic, Guatemala, Guyana, Mexico, Nicaragua, Panama and Trinidad & Tobago. Case-crossover analysis, pair-matching the number of standard drinks consumed within the six hours prior to the RTI with two control periods (prior day/week) was performed using fractional polynomial analysis for dose-response.
Results
About 1 in 6 RTI patients in EDs were positive for self-reported alcohol 6 hours prior to the injury (country range 8.6%-24.1%). The likelihood of a RTI with any drinking prior (compared to not drinking) was 5 times higher (country range OR 2.50-15.00) and the more a person drinks the higher the risk. Every drink (12.8 g alcohol) increased the risk of an RTI by 13%, even one-two drinks were associated with a sizable increase in risk of an RTI and a dose-response was found. Differences in ORs for drivers (OR=3.51; 95%CI=2.25-5.45), passengers (OR=8.12; 95%CI=4.22-15.61) and pedestrians (OR=6.30; 95%CI=3.14-12.64) and attributable fractions were noted. Acute use of alcohol was attributable to 14% of all RTIs, varying from 7% for females to 19% for being injured as a passenger. Conclusions: The finding that the presence of alcohol increases risk among drivers and non-drivers alike may further help to drive interventions targeting passengers and pedestrians. Routine screening and brief interventions in all health services could also have a beneficial impact in decreasing rates of RTIs. Higher priority should be given to alcohol as a risk factor for RTIs, particularly in Latin America and the Caribbean.
Keywords: Alcohol, case-crossover, emergency department, risk, road traffic injury
Introduction
Globally, road traffic injuries (RTIs) claim more than 1.2 million lives annually (World Health Organization, 2015b). They are estimated to be the ninth leading cause of death across all age groups (leading cause of death among young people aged between 15 to 29 years), and are predicted to become the seventh leading cause of death by 2030, costing governments approximately 3% of their gross domestic product (GDP) (World Health Organization, 2015b). Data from the third Global Status Report on Road Safety show that low and middle-income countries present double the fatality rates of high-income countries and account for 90% of all road traffic deaths (World Health Organization, 2015b).
Current evidence from Latin America and the Caribbean (LAC) suggests that alcohol is an important component of the global burden of disease (GBD) in the region (Latin America and Caribbean – World Bank Region), with a great impact on non-communicable diseases and injuries (Institute for Health Metrics and Evaluation (IHME), 2015; Monteiro, 2007; Pan American Health Organization, 2015; World Health Organization, 2014). When examining where the impact of alcohol lies, a heavy burden is seen for injuries and, among these, for RTIs (motor vehicle crashes and deaths). Most of this burden is associated with alcohol use among males (2.12% of all disability-adjusted life years (DALY) than among females (0.47% of all DALY) (http://ihmeuw.org/3udw; http://ihmeuw.org/3udx). The World Health Organization estimated that 13% of all disability-adjusted life years (DALYS) for RTIs was attributable to alcohol (World Health Organization, 2014). It is well established that drinking alcohol increases the risk of a traffic crash (Cherpitel et al., 2015a; Krüger et al., 1995; Taylor et al., 2010). Evidence of this link is also available for some countries in the region (Pechansky et al., 2010), as well as data suggesting that alcohol-related road traffic deaths reduce the life expectancy (Andreuccetti et al., 2012; Borges et al., 2013; Chandran et al., 2013; Saldanha et al., 2014; Ye et al., 2013b) and increase years of life lost (Andreuccetti et al., 2013; Sousa et al., 2010).
While there is evidence from high-income countries on the important contribution of alcohol use in road traffic injuries and death (Beasley and Beirness, 2012; Berning et al., 2015; Houwing et al., 2011), local research on the relationship between alcohol and RTIs providing prevalence data, relative risk estimates, and alcohol attributable fractions for this association in LAC are scarce or simply lacking. Some countries, such as Brazil (Gjerde et al., 2015) have contributed with a large number of research studies (Pechansky et al., 2010) but for most countries the evidence is scattered and not comparable. Most importantly, there is a paucity of evidence on the presence of alcohol in RTIs among pedestrians and non-driver riders, who are important victims of RTIs(du Plessis et al., 2016; Forson et al., 2016; Maximus et al., 2016; Senserrick et al., 2014; Sethi et al., 2016; Waller et al., 1986).
Our goal is to report the risk of an RTI when drinking prior to the event and population attributable risk (PAR) for cases of RTI from 10 countries of Latin America and the Caribbean (Argentina, Brazil, Costa Rica, Dominican Republic, Guatemala, Guyana, Mexico, Nicaragua, Panama & Trinidad and Tobago) using a case-crossover design (Borges et al., 2006; Borges et al., 2013) with a new approach to estimate dose-response curves and attributable fractions (Cherpitel et al., 2015a; Cherpitel et al., 2015b) for this population. The case-crossover design is especially suited for studying the impact of a transient exposure (such as alcohol and drug use- i.e. substance use) on an acute outcome (such as an RTI) (Maclure, 1991; Mittleman et al., 1995), in which an individual is used as his own control and generates data that can be used in dose-response models that do not assume a specific form or shape of the dose response.
Materials and Methods
Sample
The methods for this case-crossover study are similar to those used previously in emergency department (ED) studies from the World Health Organization (World Health Organization, 2009), Collaborative Study on Alcohol and Injury (Borges et al., 2006) and the Pan American Health Organization (Pan American Health Organization, 2013) study in EDs (Borges et al., 2013) that reported on the risk of alcohol use and injury. In all studies, probability samples of patients aged 18 years and older who arrived at the ED within 6 hours of the injury event were obtained by approaching consecutive arrivals to each ED, with equal representation of each shift for each day of the week. Further details on the general methodology, questionnaire development and training for the WHO study and the associated PAHO study can be found elsewhere (Borges et al., 2013; Cherpitel et al., 2006; World Health Organization, 2009). For this study, only patients from LAC attending the ED, who reported their cause of injury as a result of a road traffic crash (“Hit by vehicle”, “Collision as driver” or “Collision as passenger”) were included. The following study sites contributed with cases: Argentina (2001), Brazil (2001), Costa Rica (2012-2013), Dominican Republic (2010), Guatemala (2011), Guyana (2011), Mexico (2002), Nicaragua (2010), Panama (2010), Trinidad and Tobago (2015). Ethical approval was obtained from institutional review boards in each participating country, and the WHO and PAHO Ethics Review Committee.
Alcohol use
The interview included questions on whether the participant reported drinking during the 6 hours before the RTI, the same 6-hour period in the previous week (all sites), and the same time of day on the day prior to injury (all sites except Argentina and Brazil). For alcohol use during the 6 hours prior to the RTI, patients were asked: ‘In the 6 hours before and up to you having the RTI, did you have any alcohol to drink, even one drink?’ (yes/no). Information on alcohol use at the same time in the previous week was elicited as follows: ‘In this next section, I am going to ask you about what you were doing exactly 1 week ago. Think about the time you had your RTI (today) and remember the same time a week ago. Last week at the same time, did you have any alcohol to drink in the 6 hours leading up to this time?’ (yes/no). Parallel questions were asked for the day prior to the injury. If patients reported drinking prior to the RTI or in the prior week or the prior day, they were asked the beverage-specific number and size of containers consumed in the relevant six-hour period prior to the RTI. The volume of alcohol consumed during the 6-hour period was analyzed by converting the number and size of drinks of wine, beer, spirits, and local beverages to pure ethanol, and summing across beverage types, using a standard drink size of 16 ml (12.8 grams) as a common volume measure across beverages.
Data analysis
Patients who reported drinking at any time within the 6 hours prior to RTI were considered exposed cases. The multiple pair-matching approach compared the reported use of alcohol of each patient during the 6 hours prior to the RTI with their respective use of alcohol during the same time-period on the same day in the previous week and the same time of day on the day prior to injury (when available for the site). Conditional logistic regression was used to calculate matched-pair odds ratios (ORs) and 95% confidence intervals (CI) (Rothman et al., 2008). Three models were calculated: one with alcohol prior as a dichotomous exposure, and two with alcohol volume as continuous: linear and polynomial. Variations in the magnitude of the OR across levels of fixed characteristics (study site, sex, age, type of road traffic injury) were examined using the X2 test of homogeneity (Rothman et al., 2008). The analysis of dose-response relationship between the amount of drinking 6 hours prior and the RTI using fractional polynomial and calculations of alcohol attributable fractions, or population attributable risk (PAR), is explained in full detail in two prior works from our group (Cherpitel et al., 2015a; 2015b). Briefly, this approach circumvents the more traditional use of preset cut-points that are somehow arbitrary (for example, 1-10 drinks; 11-20 drinks, etc.). While the use of preset cut-points does not assume any pre- specified dose-response shape (exponential, quadratic, etc.), it presupposes that there may be abrupt changes in the OR of RTI from 1-10 drinks to 11-20. As an alternative to categorical step-functions, fractional polynomials have recently been used to estimate the alcohol and injury dose-response relationship in a systematic review and meta-analysis of articles reporting acute alcohol dose-response data (Taylor et al., 2010). Models were fitted using the STATA version 13.1 (Stata Corp LP, 2013) fracpoly command. Royston et al. (1999) provides details of model fitting as well as estimation of analytic 95% CIs. PAR was calculated based on the OR estimates, evaluating the fractional polynomial function at the observed mean volume for a given range of drinks, by the prevalence of drinking six hours prior in that range: PARi = Prevalencei x (1-1/ORi) (Steenland and Armstrong, 2006). The total PAR was computed as the summation of all PARi. The Specific Volume Alcohol Attributable Fraction (SVAAF) or PAR, is interpretable as the proportion of RTIs that is attributable to alcohol drinking at a particular drinking level, with 95% CIs for this proportion.
Results
Table 1 presents the number of patients arriving at each ED by country and the percentage that arrived because of an RTI. In total, almost 1 in every 5 injury patients was treated for an RTI, ranging from a low 9.6% in Mexico to a high 43.9% in the Dominican Republic. Of those patients arriving because of a RTI, 17.3% reported alcohol use 6 hours prior to the crash, ranging from a low 8.6% in Costa Rica to a high 24.1% in Argentina. For the total sample of patients with a RTI (data not shown), about 27% were females, 73% reported working at least 30 hours a week, had a mean age of 29 years and had a mean of 10 years of formal education. The distribution of type of motor vehicle injury was: 25.1% were hit by a vehicle (range 14.6%-35.4%), 47% had a collision as a driver (range 31.8%-56.7%), and 27.9% reported a collision as a passenger (range 20.9%-47.6%).
Table 1. Road traffic injury in Latin-American & Caribbean ED's (10 countries; 16 ED's).
| Country | Total sample | Type of RTI among RTI cases | |||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Sample | Road traffic injuries | % Road traffic injuries | % Self-report alcohol use before inj | % Hit by vehicle | % Collision as driver | % Collision as passenger | |
|
|
|
||||||
| Argentina | 452 | 104 | 23.0 | 24.1 | 20.2 | 56.7 | 23.1 |
| Brazil | 496 | 82 | 16.5 | 12.7 | 35.4 | 42.7 | 22.0 |
| Costa Rica | 1013 | 211 | 20.8 | 8.6 | 20.4 | 56.4 | 23.2 |
| Dominican Republic | 501 | 220 | 43.9 | 18.8 | 23.2 | 55.9 | 20.9 |
| Guatemala | 513 | 120 | 23.4 | 21.1 | 35.0 | 38.3 | 26.7 |
| Guyana | 485 | 86 | 17.7 | 20.6 | 33.7 | 32.6 | 33.7 |
| Mexico | 456 | 44 | 9.6 | 17.1 | 25.0 | 31.8 | 43.2 |
| Nicaragua | 518 | 110 | 21.2 | 21.0 | 30.0 | 40.0 | 30.0 |
| Panama | 490 | 103 | 21.0 | 20.4 | 14.6 | 37.9 | 47.6 |
| Trinidad and Tobago | 252 | 39 | 15.5 | 18.7 | 18.0 | 48.7 | 33.3 |
|
| |||||||
| TOTAL | 5176 | 1119 | 21.6 | 17.3 | 25.1 | 47.0 | 27.9 |
ED - Emergency Department; RTI - Road traffic injury
Table 2 presents the ORs estimates for dichotomous exposure (alcohol yes/no) by selected key variables, together with homogeneity tests. The use of alcohol six hours prior to the RTI increased the risk by 5.07 times for the total sample. Examination of changes in these ORs by country suggested that while they varied from a low 2.50 (in Costa Rica) to a high 15.00 (in Argentina), these ORs are homogenous (by the homogeneity test), that is, these country specific ORs are conceptually the same and the variation across countries is just random. Demographic variables (sex and age) did not modify the effect; the type of motor vehicle injury had a borderline significance, suggesting the need for inspecting the dose-response curves more closely. “Collision as driver” had the lowest OR, followed by “hit by vehicle” and “collision as passenger.”
Table 2. Matched pair analysis of any alcohol use before road traffic injury and the day/week prior in Latin-American & Caribbean ED's (n=1,119)*.
| Valid N | OR | 95% CI | Homogeneity test | |||
|---|---|---|---|---|---|---|
|
| ||||||
| X2 | d.f | p | ||||
|
|
|
|||||
| TOTAL | 1089 | 5.07 | (3.68-6.98) | - | - | - |
| Country | ||||||
| Argentina | 101 | 15.00 | (1.98-113.56) | 9.49 | 9 | 0.394 |
| Brazil | 79 | 3.50 | (1.15-10.63) | |||
| Costa Rica | 209 | 2.50 | (1.07-5.83) | |||
| Dominican Republic | 214 | 3.55 | (1.91-6.59) | |||
| Guatemala | 119 | 12.03 | (4.20-34.44) | |||
| Guyana | 84 | 4.80 | (1.52-15.13) | |||
| Mexico | 44 | 3.14 | (0.76-13.00) | |||
| Nicaragua | 105 | 8.58 | (1.85-39.71) | |||
| Panama | 95 | 6.05 | (2.43-15.09) | |||
| Trinidad and Tobago | 39 | 9.29 | (2.02-42.68) | |||
| Sex | ||||||
| Female | 292 | 4.78 | (2.00-11.42) | 0.04 | 1 | 0.841 |
| Male | 791 | 5.26 | (3.72-7.45) | |||
| Age category | ||||||
| Age 31+ | 477 | 5.60 | (3.31-9.49) | 0.23 | 1 | 0.631 |
| Age 18-30 | 600 | 4.76 | (3.18-7.14) | |||
| Type of road traffic injury | ||||||
| Hit by vehicle | 271 | 6.30 | (3.14-12.64) | 5.00 | 2 | 0.082 |
| Collision as driver | 512 | 3.51 | (2.25-5.45) | |||
| Collision as passenger | 306 | 8.12 | (4.22-15.61) | |||
Patients with missing information on any alcohol use the injury day and the control period (Argentina and Brazil) or in both control periods (all other) were not used in the analysis.
OR - Odds Ratio; CI - Confidence Interval; d.f. - degrees of freedom
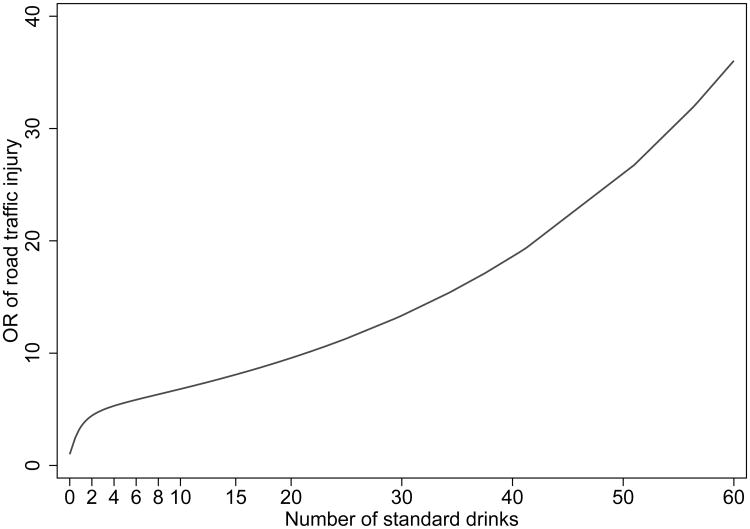
Table 3 presents the dose-response estimates for alcohol use and all RTIs for up to 60 drinks. The number of drinkers at each consumption level ranged from 8 to 45 and the prevalence at each consumption level ranged from 0.70% up to 4.02%. First, even one-two drinks increased the likelihood of a RTI, with an OR=3.87; 95% CI=(2.77-5.41) and the ORs for up to 60 drinks was 26.50 (6.93-101.33). In some instances the confidence intervals were wide, reflecting the fact that even with such large sample size, there are few discordant pairs for specific levels of drinking. The corresponding graph of these ORs (Figure 1) suggests a monotonic increase in risk of RTI with more alcohol consumption. Table 3 also presents the corresponding Specific Volume Alcohol Attributable Fraction (SVAAF) or PAR associated with these drinking levels. It is noteworthy that while the lower categories of drinking have comparatively lower ORs, these categories have a large number of RTI cases and a similar or sometimes higher prevalence of exposure and PARs that are comparable with those of higher number of drinks. The highest PAR is of the category “2.1-4 drinks.” Across levels of drinking, the summation of PARs implies that the elimination of alcohol would reduce RTIs by about 14%.
Table 3. Alcohol Odds Ratios and Attributable Fraction estimates by levels of alcohol consumed six hours before road traffic injury and the day/week prior in Latin-American & Caribbean ED's (n=1,074).
| Alcohol intake before injury1,6 | Odds Ratios3 | Attributable Fraction4 | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Range | n | Prevalence2 | OR | 95% CI | AF | 95% CI |
|
|
|
|
||||
| No drinking | 882 | - | 1 | - | - | - |
| ≤2 | 37 | 3.38 | 3.87 | (2.77-5.41) | 2.50 | (1.42-3.58) |
| 2.1-4 | 45 | 4.02 | 4.96 | (3.43-7.17) | 3.21 | (2.03-4.38) |
| 4.1-6 | 26 | 2.36 | 5.53 | (3.82-8.00) | 1.94 | (1.03-2.83) |
| 6.1-8 | 16 | 1.41 | 6.00 | (4.16-8.66) | 1.18 | (0.49-1.86) |
| 8.1-10 | 8 | 0.70 | 6.54 | (4.51-9.49) | 0.59 | (0.11-1.07) |
| 10.1-15 | 16 | 1.48 | 7.30 | (4.91-10.84) | 1.28 | (0.56-1.99) |
| 15.1-30 | 27 | 2.49 | 9.52 | (5.63-16.09) | 2.23 | (1.29-3.16) |
| 30.1-60 | 17 | 1.59 | 26.50 | (6.93-101.33) | 1.53 | (0.77-2.28) |
| TOTAL5 | 1074 | 17.43 | - | - | 14.45 | - |
Number of standard drinks
Prevalence rates do not match exactly with sample frequencies, since some studies were weighted.
Odds ratios are fractional polynomial estimates based on the mean volume of each volume category (e.g. 1.36 drinks for the (0,2] range).
Specific Volume Alcohol Attributable Fraction (SVAAF) = Pi*(1-1/RRi) in which Pi is the prevalence of drinking at a given volume among total injured patients (cases) and RRi the odds ratios of injury for a given volume compared to no drinking.
The total includes the sum of the prevalence and SVAAF across dose levels
Measures were capped to 60 drinks
Matched OR from linear model with capped volume = 1.13; 95% CI = (1.09-1.18)
CI - Confidence Interval
Figure 1.
Odds ratios of road traffic injury by alcohol volume consumed before injury. Best fit polynomial model with powers -2, 1. Volume capped to 60 drinks (10 measures).
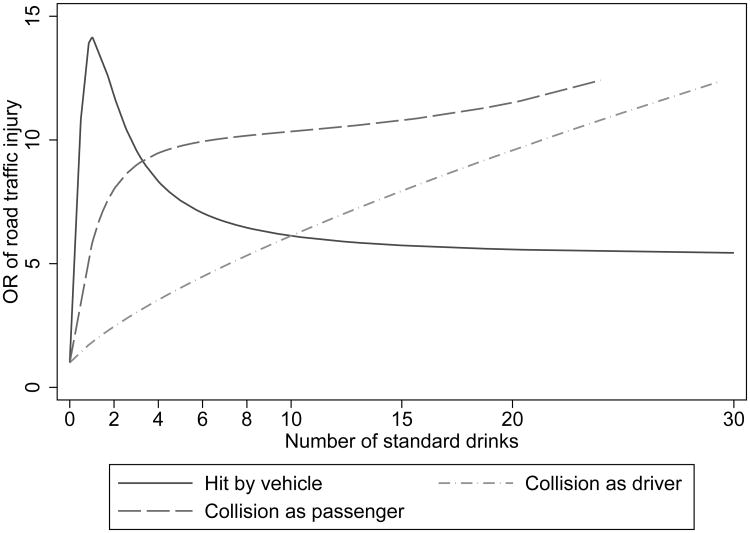
We examined the dose-response curves by sex, age and type of RTI. Curves were similar for sex and age groups (not shown) but varied by type of RTI (Figure 2), with a very sharp increase in risk at low levels of consumption for “hit by vehicle,” followed by high slopes for “collision as passenger” and a plateau after 8 drinks for “hit by a vehicle.” While ORs were homogeneous across different groups, large variations were observed of PAR for these categories: males: 17.33%; females: 7.15%;18-30 years old:15.36%; 31 and over:13.48%; hit by vehicle:14.93%; collisions as driver:11.12%; collision as passenger:19.35%.
Figure 2.
Odds ratios of road traffic injury by alcohol volume consumed before injury, by type. X axis trimmed to 30 drinks.
Discussion
To summarize, 1 in every 5 injury patients in EDs in LAC presented with a RTI, and 1 in every 6 RTI patients were positive for alcohol 6 hours prior to the event. The likelihood of an RTI after any drinking was 5 times higher (compared to not drinking) and the more a person drank the higher the risk. For each drink there was a 13% increased risk, and alcohol use prior to RTI was responsible for 14% of all RTIs, varying from 7% for females to 19% for being injured as a passenger. Differences in ORs and attributable fractions for drivers, passengers and pedestrians were noted. Our finding of a PAR of 14.4% for RTI is consistent with prior studies from non-LAC samples (Cherpitel et al., 2015b; Kuendig et al., 2008; World Health Organization, 2014).
The high OR (5.07) result for any drinking from our sample of LAC patients may be due to the high frequency of heavy episodic drinking characterizing the LAC region (Pan American Health Organization, 2015), even at low levels of overall per capita consumption. Unfortunately, our sample size per study site is too small for studying variations in ORs by study site by age/sex or drinking level, but prior studies from Cherpitel et al. (2015a) on possible effects of a country-level drinking pattern determined by the World Health Organization (WHO) country's detrimental drinking pattern (Rehm et al., 2001) shows that countries with the most detrimental drinking patterns may have increased alcohol attributable fractions for injuries compared to countries with a lower detrimental drinking pattern. The finding that at low and middle levels of drinking there is extensive PAR, brings attention to population measures for all drinkers and not only those with alcohol use disorders, as stated before (Poikolainen et al., 2007).
One of the few studies to separate RTI by type reported an OR of 5.2 and PAR of 24% for motor vehicle injury after drinking, but a high OR of 9.5 and high PAR of 39% for pedestrians (Miller and Spicer, 2012). Our study documents for the first time in the LAC region that while an important part of RTIs are due to drivers using alcohol, passengers and pedestrians involved in road traffic crash also contribute significantly to the burden of RTI. They comprise more than 50% of the cases, have considerable OR of an injury if drinking, and have even higher PAR than the drivers.
Prior efforts to estimate the role of alcohol in RTI in the LAC region exist (Christophersen et al., 2016), but translating data to the need for intervention to both policy makers and the population at large has proven to be difficult (Pechansky et al., 2016; Pechansky and Chandran, 2012). The recently approved Decade of Action for Road Safety calls on Member States to take the necessary steps to make their roads safer (World Health Organization, 2010a), and the 2030 Agenda on Sustainable Development Goals, set a goal of reducing road traffic deaths and injuries by 50% by 2020 (World Health Organization, 2015a). In order to accomplish these goals, measures to decrease modifiable risk factors, such as alcohol use before driving, are essential. Comparable data across a large number of LAC countries and the findings of this study showing that the presence of alcohol increases risk among drivers and non-drivers alike, may further help to drive interventions targeting passengers and pedestrians. Data now exist to show that public health measures centered exclusively on drink-drivers are inadequate since they may miss about half of the cases of alcohol-involved RTI in the LAC region.
The differences in the risk curves by type of RTI that we reported should be investigated further. While we know experimentally the influence of alcohol on motor coordination of drivers, we know very little on how alcohol affects time reaction, judgment and impulsive behavior among pedestrians or passengers. Further studies on the different risk curves reported here by type of RTI are however important, as we cannot rule out that our limited sample size for each type of RTI produced unstable estimates that may have driven these curves apart. Delving into the coalescence of other risk factors that put passengers and pedestrians at high risk of RTI is beyond the scope of the current report, but a common and potentially preventable risk is the consumption of alcohol.
Limitations
This study is limited to analysis of data from a representative sample of patients with RTI who attended specific EDs during a large time frame (2001-2015). Data from each country are most representative of the time period of data collection and current proportion of alcohol use, proportion of RTI and potentially the SVAAF/ PAR would have been impacted by socioeconomic/transportation and infrastructure development, alcohol policy and cultural changes in each country during the total time period. Cases cannot be assumed to be representative of other individuals suffering a RTI who did not seek medical attention and may be of lesser severity. In the LAC region, motorcycle crashes account for a sizable proportion of the motor vehicle injuries as a driver, and they have been reported with high prevalence of alcohol and cannabis (Longo et al., 2000), but we lack this information. All analyses reported here are based on the patient's reported alcohol consumption across different times, which may not be evenly accurate, thereby producing an overestimate of the association between alcohol and RTI for case-crossover studies. Findings using control periods other than drinking during the previous week have been mixed, suggesting either higher estimates (Borges et al., 2004; Gmel and Daeppen, 2007), lower estimates (Borges et al., 2013), or no differential report (Ye et al., 2013a). While our approach of multiple matching aimed to reduce such bias, if present at all, this is a topic for further research. Biological measures of blood alcohol content (BAC) at time of injury are desirable, and the WHO-PAHO studies include such, but there are no biological measures available for the control periods. Despite the fact that case–crossover studies are well suited to control for between-person confounders, they do not remove the possibility that within-person confounders (such as use of safe-belt) may exist. Other variables, such as street illumination and presence of pedestrians' bridges or sidewalks, may also have played a role in RTI, but are beyond the scope of this research. Importantly, new research should include substances other than alcohol and estimate ORs for combinations of drugs and alcohol on RTI (Gjerde et al., 2015; Strand et al., 2016). This is the largest case-crossover study reported to date but our sample size was still insufficient to perform analyses by gender or age groups or by study site, and the dose-response estimates are unstable, especially for the higher consumption categories.
Conclusion
Despite these limitations, this is one of the largest studies ever reported on acute alcohol use and RTI with data coming from a large sample of patients from several countries of LAC. Alcohol was found among 1 in every 6 RTI cases (drivers, passengers, and pedestrians alike) and reducing consumption even at low and middle levels (<=4 drinks) can have a sizable impact on risk and population burden. Measures to reduce alcohol consumption among drivers, passengers and pedestrians involved in RTI, within the scope of global and local strategies to reduce alcohol consumption (World Health Organization, 2010b) is a step that shouldn't be postponed in LAC.
Acknowledgments
The paper is based, in part on data collected by the following collaborators participating in the World Health Organization and implemented by the WHO Collaborative Study Group on Alcohol and Injuries under the direction of V. Poznyak and M. Peden (WHO, Switzerland): G. Borges (Mexico); M. Cremonte (Argentina); N. Figlie and R. Larajeira (Brazil). A list of other staff contributing to the project can be found in the Main Report of the Collaborative Study on Alcohol and Injuries, WHO, Geneva. The paper is also based on work performed by collaborators participating in the Pan American Health Organization Collaborative Study on Alcohol and Injuries, directed by M. Monteiro (PAHO, USA) in coordination with C. J. Cherpitel (USA) and G. Borges (Mexico). It was implemented at country level by the following lead investigators: V. Aparicio and A. de Bradshaw (Panama); V. Lopez (Guatemala); M. Paltoo (Guyana); E. Perez (Dominican Republic); D. Weil (Nicaragua). We also acknowledge Julio Bejarano (Costa Rica) and Sandra Reid (Trinidad & Tobago). The authors alone are responsible for views expressed in this paper, which do not necessarily represent those of the other investigators participating in the WHO or PAHO collaborative studies on alcohol and injuries, nor the views or policy of the World Health Organization or the Pan American Health Organization.
Funding: Supported in part by the Pan American Health Organization, the government of Valencia, Spain and World Health Organization. Supported in part by a grant from the U.S. National Institute on Alcohol Abuse and Alcoholism (NIAAA) (R01 5 AA013750). Supported in part by Instituto Nacional de Psiquiatria Ramon de la Fuente Muñiz.
Footnotes
Conflict of Interest: None declared
References
- Andreuccetti G, Carvalho HB, Korcha R, Ye Y, Bond J, Cherpitel CJ. A review of emergency room studies on alcohol and injuries conducted in Latin America and the Caribbean region. Drug Alcohol Rev. 2012;31:737–746. doi: 10.1111/j.1465-3362.2012.00419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreuccetti G, Gawryszewski V, Diehl A, Monteiro M, Cherpitel CJ. In: Alcohol's causal role in interpersonal violence and road traffic injuries in the Americas, in Prevention of alcohol-related injuries in the Americas: from evidence to policy action. Cherpitel CJ, Borges G, Giesbrecht N, Monteiro M, Stockwell T, editors. Pan American Health Organization; Washington DC: 2013. pp. 27–35. [Google Scholar]
- Beasley EE, Beirness DJ. Alcohol and Drug Use Among Drivers Following the Introduction of Immediate Roadside Prohibitions in British Columbia: Findings from the 2012 Roadside Survey. Final Report 2012 [Google Scholar]
- Berning A, Compton R, Wochinger K. Traffic Safety Facts Research Note. HTSA; Washington, DC: 2015. Results of the 2013–2014 National Roadside Survey of alcohol and drug use by drivers. Report No. DOT HS 812 118. [Google Scholar]
- Borges G, Cherpitel CJ, Mondragón L, Poznyak V, Peden M, Gutierrez I. Episodic alcohol use and risk of nonfatal injury. Am J Epidemiol. 2004;159:565–571. doi: 10.1093/aje/kwh073. [DOI] [PubMed] [Google Scholar]
- Borges G, Cherpitel CJ, Orozco R, Bond J, Ye Y, MacDonald S, Rehm J, Poznyak V. Multicentre study of acute alcohol use and non-fatal injuries: data from the WHO collaborative study on alcohol and injuries. Bull World Health Organ. 2006;84:453–460. doi: 10.2471/blt.05.027466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Orozco R, Monteiro M, Cherpitel CJ, Then EP, Lopez VA, Bassier-Paltoo M, Weil DA, Bradshaw AM. Risk of injury after alcohol consumption from case–crossover studies in five countries from the Americas. Addiction. 2013;108:97–103. doi: 10.1111/j.1360-0443.2012.04018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandran A, Kahn G, Sousa T, Pechansky F, Bishai DM, Hyder AA. Impact of road traffic deaths on expected years of life lost and reduction in life expectancy in Brazil. Demography. 2013;50:229–236. doi: 10.1007/s13524-012-0135-7. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Bond J, Ye Y, Borges G, Room R, Poznyak V, Hao W. Multi-level analysis of causal attribution of injury to alcohol and modifying effects: Data from two international emergency room projects. Drug Alcohol Depend. 2006;82:258–268. doi: 10.1016/j.drugalcdep.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Bond J, Borges G, Monteiro M. Relative risk of injury from acute alcohol consumption: modeling the dose–response relationship in emergency department data from 18 countries. Addiction. 2015a;110:279–288. doi: 10.1111/add.12755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Bond J, Borges G, Monteiro M, Chou P, Hao W. Alcohol Attributable Fraction for Injury Morbidity from the Dose-Response Relationship of Acute Alcohol Consumption: Emergency Department Data from 18 Countries. Addiction. 2015b;110:1724–1732. doi: 10.1111/add.13031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christophersen AS, Mørland J, Stewart K, Gjerde H. International trends in alcohol and drug use among motor vehicle drivers. Forensic Sci Rev. 2016;28:37–66. [PubMed] [Google Scholar]
- du Plessis M, Hlaise KK, Blumenthal R. Ethanol-related death in Ga-Rankuwa road-users, South Africa: A five-year analysis. J Forensic Leg Med. 2016;44:5–9. doi: 10.1016/j.jflm.2016.08.006. [DOI] [PubMed] [Google Scholar]
- Forson PK, Gardner A, Oduro G, Bonney J, Biney EA, Oppong C, Momade E, Maio RF. Frequency of alcohol use among injured adult patients presenting to a Ghanaian emergency department. Ann Emerg Med. 2016;68:492–500. doi: 10.1016/j.annemergmed.2016.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjerde H, Strand MC, Mørland J. Driving under the influence of non-alcohol drugs—an update. Part I: Epidemiological studies. Forensic Sci Rev. 2015;27:89–113. [PubMed] [Google Scholar]
- Gmel GA, Daeppen JB. Recall bias for seven-day recall measurement of alcohol consumption among emergency department patients: implications for case-crossover designs. J Stud Alcohol Drugs. 2007;68:303–310. doi: 10.15288/jsad.2007.68.303. [DOI] [PubMed] [Google Scholar]
- Houwing S, Hagenzieker M, Mathijssen R, Bernhoft I, Hels T, Janstrup K, Van der Linden T, Legrand S, Verstraete A. Prevalence of alcohol and other psychoactive substances in drivers in general traffic.Part I: General results. DRUID. 2011:1–173. [Google Scholar]
- Institute for Health Metrics and Evaluation (IHME) GBD Compare. [Accessed June 16, 2016];2015 Available at: http://vizhub healthdata org/gbd-compare.
- Krüger HP, Kazenwadel J, Vollrath M. Grand Rapids effects revisited: Accidents, alcohol and risk. ICADTS. 1995;1:S222–S230. [Google Scholar]
- Kuendig H, Hasselberg M, Laflamme L, Daeppen JB, Gmel GA. Acute alcohol consumption and injury: risk associations and attributable fractions for different injury mechanisms. J Stud Alcohol Drugs. 2008;69:218–226. doi: 10.15288/jsad.2008.69.218. [DOI] [PubMed] [Google Scholar]
- Longo MC, Hunter CE, Lokan RJ, White JM, White MA. The prevalence of alcohol, cannabinoids, benzodiazepines and stimulants amongst injured drivers and their role in driver culpability: part ii: the relationship between drug prevalence and drug concentration, and driver culpability. Accid Anal Prev. 2000;32:623–632. doi: 10.1016/s0001-4575(99)00110-4. [DOI] [PubMed] [Google Scholar]
- Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133:144–153. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- Maximus S, Figueroa C, Pham J, Kuncir E, Barrios C. DUI Histories in Intoxicated Injured Bicyclists. J Trauma Acute Care Surg. 2016;81:638–643. doi: 10.1097/TA.0000000000001168. [DOI] [PubMed] [Google Scholar]
- Miller TR, Spicer RS. Hospital-Admitted Injury Attributable to Alcohol. Alcohol Clin Exp Res. 2012;36:104–112. doi: 10.1111/j.1530-0277.2011.01593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittleman MA, Maclure M, Robins JM. Control sampling strategies for case-crossover studies: an assessment of relative efficiency. Am J Epidemiol. 1995;142:91–98. doi: 10.1093/oxfordjournals.aje.a117550. [DOI] [PubMed] [Google Scholar]
- Monteiro M. Alcohol and public health in the Americas: a case for action. Pan American Health Organization; Washington, DC: 2007. [Google Scholar]
- Pan American Health Organization. Prevention of alcohol-related injuries in the Americas: from evidence to policy action. Pan American Health Organization; Washington, DC: 2013. [Google Scholar]
- Pan American Health Organization. Regional Status Report on Alcohol and Health in the Americas. Pan American Health Organization; Washington, DC: 2015. [Google Scholar]
- Pechansky F, Chandran A. Why don't northern American solutions to drinking and driving work in southern America? Addiction. 2012;107:1201–1206. doi: 10.1111/j.1360-0443.2011.03731.x. [DOI] [PubMed] [Google Scholar]
- Pechansky F, Chandran A, Sousa T. Bridging a historical gap: can changes in perceptions of law enforcement and social deterrence accelerate the prevention of drunk driving in low and middle-income countries? Rev Bras Psiquiatr. 2016;38:161–166. doi: 10.1590/1516-4446-2015-1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pechansky F, De Boni RB, Duarte P. Use of alcohol and other drugs on Brazilian roads and other studies. 1. Digitalcom; Porto Alegre: 2010. [Google Scholar]
- Poikolainen K, Paljärvi T, Mäkelä P. Alcohol and the preventive paradox: serious harms and drinking patterns. Addiction. 2007;102:571–578. doi: 10.1111/j.1360-0443.2006.01740.x. [DOI] [PubMed] [Google Scholar]
- Rehm J, Monteiro M, Room R, Gmel GA, Jernigan D, Frick U, Graham K. Steps towards constructing a global comparative risk analysis for alcohol consumption: determining indicators and empirical weights for patterns of drinking, deciding about theoretical minimum, and dealing with different consequences. Eur Addict Res. 2001;7:138–147. doi: 10.1159/000050731. [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Lash L. Modern Epidemiology. 3rd. Lippincott William & Wilkins; Philadelphia: 2008. [Google Scholar]
- Royston P, Ambler G, Sauerbrei W. The use of fractional polynomials to model continuous risk variables in epidemiology. Int J Epidemiol. 1999;28:964–974. doi: 10.1093/ije/28.5.964. [DOI] [PubMed] [Google Scholar]
- Saldanha RF, Pechansky F, Benzano D, Barros CA, Boni RB. Differences between attendance in emergency care of male and female victims of traffic accidents in Porto alegre, Rio Grande do Sul state, Brazil. Cien Saude Colet. 2014;19:3925–3930. doi: 10.1590/1413-81232014199.12892013. [DOI] [PubMed] [Google Scholar]
- Senserrick T, Boufous S, De Rome L, Ivers R, Stevenson M. Detailed analysis of pedestrian casualty collisions in Victoria, Australia. Traffic Inj Prev. 2014;15:S197–S205. doi: 10.1080/15389588.2014.935356. [DOI] [PubMed] [Google Scholar]
- Sethi M, Heyer J, Wall S, DiMaggio C, Shinseki M, Slaughter D, Frangos S. Alcohol use by urban bicyclists is associated with more severe injury, greater hospital resource use, and higher mortality. Alcohol. 2016;53:1–7. doi: 10.1016/j.alcohol.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa TRV, Correa E, Stampe MZ, Junior SDSP, De Boni R. In: Cost of traffic accidents with victims associated with alcohol use in Porto Alegre, in Use of alcohol and other drugs on Brazilian roads and other studies. Pechansky F, De Boni RB, Duarte P, editors. Digitalcom; Porto Alegre: 2010. [Google Scholar]
- Stata Corp LP. Stata Statistical Software [Release 13.1] College Statio, TX: 2013. [Google Scholar]
- Steenland K, Armstrong B. An overview of methods for calculating the burden of disease due to specific risk factors. Epidemiology. 2006;17:512–519. doi: 10.1097/01.ede.0000229155.05644.43. [DOI] [PubMed] [Google Scholar]
- Strand MC, Gjerde H, Mørland J. Driving under the influence of non-alcohol drugs-An update. Part II: Experimental studies. Forensic Sci Rev. 2016;28:79–101. [PubMed] [Google Scholar]
- Taylor B, Irving H, Kanteres F, Room R, Borges G, Cherpitel CJ, Greenfield T, Rehm J. The more you drink, the harder you fall: a systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend. 2010;110:108–116. doi: 10.1016/j.drugalcdep.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller P, Stewart J, Hansen A, Stutts J, Popkin C, Rodgman E. The potentiating effects of alcohol on driver injury. JAMA. 1986;256:1461–1466. [PubMed] [Google Scholar]
- World Health Organization. Alcohol and Injuries: Emergency Department Studies in an International Perspective. World Health Organization; Geneva: 2009. [Google Scholar]
- World Health Organization. Global Plan for the Decade of Action for Road Safety 2011-2020. World Health Organization; Geneva: 2010a. [Google Scholar]
- World Health Organization. Global strategy to reduce the harmful use of alcohol. World Health Organization; Geneva: 2010b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Global status report on alcohol and health 2014. World Health Organization; Geneva: 2014. [Google Scholar]
- World Health Organization. Brasilia Declaration: Second Global High-level Conference on Road Safety: Time for Results Brasilia. World Health Organization; Geneva: 2015a. Nov 18-19, 2015. [Google Scholar]
- World Health Organization. Global status report on road safety 2015. World Health Organization; Geneva: 2015b. [Google Scholar]
- Ye Y, Bond J, Cherpitel CJ, Borges G, Monteiro M, Vallance K. Evaluating recall bias in a case-crossover design estimating risk of injury related to alcohol: Data from six countries. Drug Alcohol Rev. 2013a;32:512–518. doi: 10.1111/dar.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Y, Cherpitel CJ, MacDonald S. Alcohol-related injuries in the Americas: variation by cause and country, in Prevention of Alcohol-Related Injuries in the Americas: From evidence to policy action. Pan American Health Organization; Washington, DC: 2013b. pp. 61–68. [Google Scholar]