Abstract
Objective
Short sleep duration has been linked with a wide array of poor mental and physical health outcomes. Such risks, however, may be moderated by demographic factors such as gender and race/ethnicity. In a diverse community sample, the current study examined the relationship between gender, race/ethnicity and objectively measured sleep duration, controlling for select potential confounds.
Methods
Participants were 300 community adults (50% female), aged 21 to 70 years, and included 60% non-Hispanic Whites, 15% non-Hispanic Blacks, 19% Hispanic/Latino, and 6% Other. As part of a larger study, participants wore an actigraphy device over two nights to assess sleep duration (averaged across both nights). Gender and race/ethnicity were used as grouping variables in a two-way analysis of covariance (ANCOVA) predicting objectively assessed total sleep time, with age, income and employment status as covariates.
Results
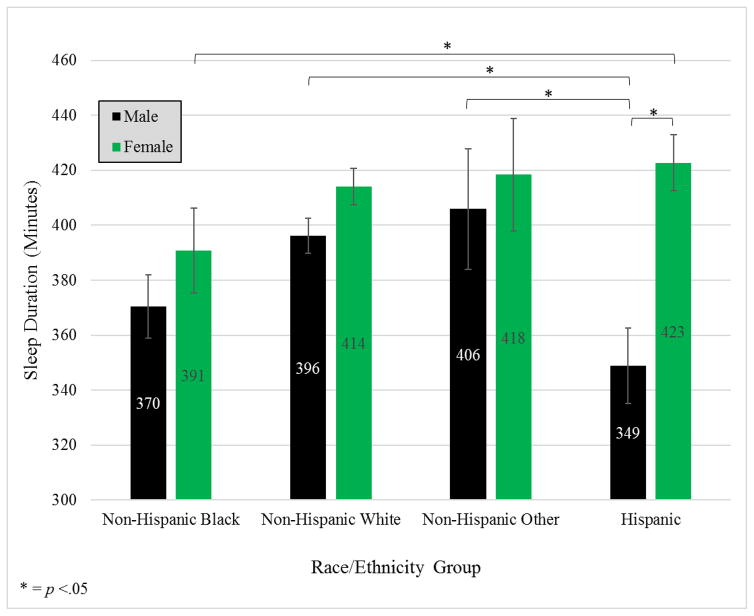
On average, males slept 34 min less than females (p=0.002). After controlling for socioeconomic factors, there was a gender by race/ethnicity interaction (p=0.030). Within males, Hispanics slept 45 min less than non-Hispanic Whites (p=.002) and 57 min less than non-Hispanic Others (p=.008). Males also slept significantly less than females within the non-Hispanic White (difference=−22.9; p=.016) and the Hispanic (difference=−77.1; p<.001) groups.
Conclusions
Extending previous research, the current study provides additional evidence for differences in objective sleep duration based on gender and race/ethnicity in daily life. These data suggest that risk associated with sleep duration is patterned in important ways across gender and race/ethnicity; such information can be used to tailor prevention efforts.
Keywords: Sleep duration, health disparity, race, gender
Previous studies (1–4) have shown significant differences in sleep duration by gender, but less information is known about potential race/ethnicity differences (3) and few studies have examined interactions between gender and race/ethnicity (3). More studies examining gender and race/ethnicity disparities in sleep duration are needed, because it is plausible sleep behaviors are an important mechanism in other health disparities such as hypertension (5), cardiovascular disease (6), diabetes (7), obesity (8), and all-cause mortality (9, 10). Increased stressors experienced by racial/ethnic minority individuals, such as lower socioeconomic status and discrimination may lead to disparities in sleep duration (11).
Racial/ethnic differences in sleep duration are unclear. That is, studies have shown Non-Hispanic Blacks (1, 3, 12, 13), Hispanics (1, 13, 14) and Asians (1, 13, 14) have shorter sleep duration than Non-Hispanic Whites in some cases, and longer sleep duration in other cases (1, 4). Notably, these prior studies have been limited by being largely ethnically homogenous or comparing a limited range of race/ethnicities (3, 15), or relying primarily on self-report (e.g., 1, 16) or laboratory-based polysomnography (12) for sleep assessment. Additionally, these studies often categorized sleep duration (e.g., into <5, 6, 7, 8, >9 hrs), which limited power (17).
Gender might moderate race/ethnicity differences in sleep, but the relationship is complex and has received limited attention (3, 16). One study using objective measurement of sleep duration (18) found Hispanic males sleep significantly longer than Hispanic females, but did not examine other race/ethnicities. Another study (3) examined interactions between race/ethnicity (non-Hispanic only) and gender demonstrated significant differences among groups such that White women slept the longest, followed by White men, Black women, and Black men, even after adjusting for socioeconomic, employment, household, and lifestyle factors. More research is needed to more fully understand the interactions between gender and race/ethnicity.
Differences in sleep duration could be an important component of race/ethnic disparities in chronic diseases (e.g., cardiovascular disease). As such, the current study examined relationships between gender, race/ethnicity and sleep duration using actigraphy in a diverse community sample. Importantly, the use of actigraphy provides objective sleep data while maintaining ecological validity (3, 4, 12, 18). Based on previous research, it was hypothesized that Hispanics and Non-Hispanic Blacks would have shorter sleep durations than the other racial groups and that within Hispanics and Non-Hispanic Blacks, men would have even lower sleep durations.
Methods
Participants
A community-based sample of 300 adults between 21 to 70 years was enrolled. The sample recruitment was stratified by age within gender (150 men) and race/ethnicity in order to examine age-related effects. The mean age at enrollment was 42.44 years (SD=12.76) with men significantly younger than women. The sample included 60% non-Hispanic Whites, 15% non-Hispanic Blacks, 19% Hispanic/Latino of which 75% self-identified as being of Mexican descent, and 6% who identified as Asian or “Other”. A majority of participants were married (60%), owned a home (63%), and were employed outside the home (79%). Participants represented a broad range of educational backgrounds with more than 86% reporting some college. Similarly, the sample reflected significant income diversity with 12% reporting a household income less than $20,000, 10% above $150,000, and the modal annual household income reported to be $75,000 to $100,000. Detailed demographics are reported elsewhere (19).
Procedures
All study examinations were conducted at a single site. Following arrival and consent, participants completed a psychosocial survey. Prior to leaving, participants were given an actigraph and cellular phone for the 2-day/1-night, ambulatory/ecological momentary assessment (EMA) study. Participants completed EMA-based sleep diaries upon awakening each morning. Institutional review board approval was obtained for the study.
Measures
Actigraph Spectrum devices (Philips-Respironics, Inc), are wristwatch-like devices. Actigraph records were hand-scored with EMA-based sleep diaries by two independent trained scorers, with discrepancies resolved by a third reviewer. Participants wore the actigraph over two nights (Thursday and Friday) to provide data for one weekday and one weekend night. Total sleep time (TST; i.e., sleep duration), calculated by subtracting sleep onset latency, wake after sleep onset, and morning wakefulness from total time in bed. Actiware (Philips-Respironics, Inc.) settings of medium activity threshold and 10 immobile minutes were used to detect wakefulness. Actigraphy has been well-validated and shown to correlate highly with polysomnography (20). In addition, sleep quality was assessed during the EMA-based sleep diary each morning with a single question (“Overall, how would you rate your sleep quality last night?”) rated on a 5-point Likert scale ranging from “very poor” (0) to “very good” (4).
Analytic Approach
A portion of the sample had unusable data for either the first (13.7%) or second (9.0%) night of data collection due to technical difficulties/adherence issues. Following Tabachnick and Fidel’s advice (21) to impute data missing >5%, an Expectation Maximization data imputation procedure was used and then sleep data was averaged across days. Next, two-way analysis of covariance (ANCOVA) were performed with gender (male vs. female) and race/ethnicity (non-Hispanic White vs. non-Hispanic Black vs. Hispanic/Latino vs. Other) as grouping variables, actigraphy-assessed total sleep time as the dependent variable, controlling for traditional risk factors of age, socioeconomic and employment status. The same procedure was used to analyze sleep quality.
Results
The average total sleep time across all groups was 396.6 min (SE = 5.1 min). See Figure 1 for means by group. After controlling for age, household income, and employment status, there was a main effect for gender (women slept 34 min longer than men; p = .002; part. η2 = .034) and race/ethnicity (p = .028; part. η2 = .033; see Table 1 for unadjusted and adjusted models). There was a significant gender by race/ethnicity interaction (p = .030; part. η2 = .033). Simple effects ANCOVAs follow. There were significant differences between males (p = .01; part. η2 = .071), but not females (p = .38; part. η2 = .021) across race/ethnicity. Among males, Hispanics slept significantly less than non-Hispanic Whites (Δ = −44.6; p = .002; part. η2 = .087) and non-Hispanic Others (Δ = −56.7; p = .008; part. η2 = .247), and there was a trend to sleep less than non-Hispanic Blacks (Δ = −24.6; p = .05; part. η2 = .079). There were significant gender differences within non-Hispanic White and Hispanic individuals: non-Hispanic White (Δ = −22.9; p = .02; part. η2 = .032) and Hispanic (Δ = −77.1; p < .001; part. η2 = .312) males slept significantly less than females. Descriptive statistics of percent of the sample falling into hourly (e.g., <5, 5–6, 6–7) total sleep time categories are provided by race/ethnicity and gender in Table 2. Race/ethnicity and gender were not significantly associated with sleep quality.
Figure 1.
Estimated marginal means and standard errors of sleep duration by race/ethnicity and gender. Note. Values are estimated marginal means and standard errors controlling for age (M = 42.4), employment status (employed vs. not) and household income median split. Brackets represent significant simple effects tests after a significant interaction. Main effects were not denoted.
Table 1.
Analysis of Covariance of Sleep Duration as a Function of Gender, Race/Ethnicity, with Age, Household Income, and Employment Status as Covariates
| Unadjusted | Fully Adjusted* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Source | df | SS | MS | F | p | η2 | df | SS | MS | F | p | η2 |
| Age | 1 | 23047.24 | 23047.24 | 4.43 | .036 | .016 | ||||||
| Household Income | 1 | 8985.02 | 8985.02 | 1.73 | .190 | .006 | ||||||
| Employment Status | 1 | 33.77 | 33.77 | .01 | .936 | <.001 | ||||||
| Gender | 1 | 68471.43 | 68471.43 | 13.03 | <.001 | .046 | 1 | 49920.88 | 49920.88 | 9.59 | .002 | .034 |
| Race/Ethnicity | 3 | 50664.98 | 16888.33 | 3.21 | .023 | .034 | 3 | 48145.70 | 16048.57 | 3.08 | .028 | .033 |
| Gender X Race/Ethnicity | 3 | 41068.69 | 13689.56 | 2.61 | .052 | .028 | 3 | 47371.70 | 15790.57 | 3.03 | .030 | .033 |
| Error | 272 | 1429580.31 | 5255.81 | 269 | 1400459.53 | 5206.17 | ||||||
| Total | 280 | 45957111.50 | 280 | 45957111.50 | ||||||||
Note:
Adjusted for Age, Employment Status (Full-Time or Part-Time/Unemployed), and Household Income (<$75k or >$75k)
Table 2.
Descriptive Percentage of Sample by Total Sleep Time Hours Category, Gender, and Race/Ethnicity
| Men (N = 136) | Women (N = 143) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <5h | 5–6h | 6–7h | 7–8h | 8–9h | >9h | <5h | 5–6h | 6–7h | 7–8h | 8–9h | >9h | |
|
|
|
|||||||||||
| NH Black | 1.8 | 2.2 | 2.2 | 1.8 | 0.4 | 0.4 | 0.4 | 1.1 | 1.1 | 1.8 | 0 | 0 |
| NH White | 2.9 | 5.4 | 12.2 | 8.2 | 2.2 | 0 | 1.8 | 5.0 | 7.9 | 10.8 | 3.9 | 1.4 |
| NH Other | 0 | 0.4 | 1.4 | 1.1 | 0 | 0 | 0.4 | 0 | 0.7 | 1.8 | 0 | 0.4 |
| Hispanic | 1.1 | 3.6 | 1.1 | 0.7 | 0 | 0 | 0 | 2.2 | 3.2 | 6.1 | 1.1 | 0.4 |
| Total | 5.7 | 11.5 | 16.8 | 11.8 | 2.5 | 0.4 | 2.5 | 8.2 | 12.9 | 20.4 | 5.0 | 2.2 |
Note: NH = Non-Hispanic
Discussion
In this diverse community sample, and consistent with previous findings (1–4), males slept significantly less than females. Novel findings were that this effect was largely driven by gender differences between non-Hispanic Whites and Hispanics. Additionally, non-Hispanic Whites and Other males slept longer than Hispanic males. Finally, non-Hispanic White and Hispanic males slept significantly less than their female counterparts. These results suggest sleep may be an important area in which to examine health disparities, but the relationship between race/ethnicity, gender, and total sleep time is complex. It appears clear, however, that Hispanic males (and, to a lesser extent, non-Hispanic males) have a significantly shorter sleep duration than other groups. In contrast with previous studies (for a review, see 22), we did not find any statistically significant differences between Black and non-Hispanic White individuals although their sleep duration differed by about 20 minutes on average. This difference may be attributable to previous studies using longer (and thus more stable) assessment periods (12), subjective measures (1, 13), or a Black sample with lower SES than the current study.
Previous findings on race/ethnicity and sleep quality have largely demonstrated that Black and Hispanic individuals tend to have worse perceived sleep quality than Non-Hispanic White individuals. In contrast, race/ethnicity and gender were not related to sleep quality in the present study. This is likely due, in part, to the combination of an imprecise measurement method (i.e., single question) and too little statistical power. Other studies that have found a significant relationship between race/ethnicity and sleep quality typically employ greater sample sizes (e.g., >4000; 23, 24, 25) or used multidimensional measures that can detect greater variance (e.g., Pittsburgh Sleep Quality Index; 12). It is also possible that non-significant findings related to sleep quality have not been published (i.e., the file drawer effect).
A variety of pathways have been examined as potential drivers of health disparities (26). Racial/ethnic disparities are potentially related to stress caused by lower socioeconomic status and daily experiences of discrimination (11), whereas sex health disparities are potentially related to fluctuating hormone levels (27) and different coping styles (28). It was beyond the scope of this brief report to investigate these pathways given limited sample size, but this is an important area for future research.
Other than sample size/small cell sizes, another notable limitation of the current study included measuring objective sleep over only two days, which may not be reflective of average habitual sleep duration. Further, the current study only examined sleep duration, which does not fully reflect the complexities of sleep (e.g., architecture, continuity, subjective distress).
Future studies should objectively assess sleep over longer periods of time and complement actigraphy with other comprehensive measures of sleep (e.g., clinical interview, validated survey measures). Future studies should also examine discrimination, hormone levels and coping styles as potential mediators of sleep health disparities as well as sleep health disparities as potential mediators or moderators of other health disparities (e.g., Type II diabetes, obesity, cardiovascular risk and disease). Finally, studies should extend this area by examining if interventions for sleep difficulties can help mitigate differences.
Conclusions
This study extends previous research by using a diverse community sample with naturalistic objective assessment of sleep duration as a continuous variable. The current study provides insight that may prove helpful in understanding disparities in objective sleep duration based on gender and race/ethnicity. Racial/ethnic and gender interactions persisted, even after controlling for traditional risk factors of age, socioeconomic and employment status. The risk associated with sleep duration was patterned across gender and race/ethnicity; in particular, race/ethnic disparities in TST appear to be more pronounced among males (and reduced or even absent in females). For those interested in the risks associated with sleep duration, particularly in the context of health disparities, this information may help inform both research and prevention efforts.
Acknowledgments
Special thanks to Earl Crew, Brett Messman, and Jennifer Warmann. Research supported by a grant from the National Heart, Lung, and Blood Institute of the National Institutes of Health (RHL109340A).
Footnotes
Conflicts of Interest
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Basner M, Spaeth AM, Dinges DF. Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep. Sleep. 2014;37(12):1889–906. doi: 10.5665/sleep.4238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jean-Louis G, Kripke DF, Ancoli-Israel S, Klauber MR, Sepulveda RS. Sleep duration, illumination, and activity patterns in a population sample: effects of gender and ethnicity. Biological Psychiatry. 2000;47(10):921–7. doi: 10.1016/s0006-3223(99)00169-9. [DOI] [PubMed] [Google Scholar]
- 3.Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively measured sleep characteristics among early-middle-aged adults: The CARDIA study. American Journal of Epidemiology. 2006;164(1):5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 4.Chen X, Wang R, Zee P, Lutsey PL, Javaheri S, Alcántara C, et al. Racial/Ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA) Sleep. 2015;38(6):877–88. doi: 10.5665/sleep.4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Q, Xi B, Liu M, Zhang Y, Fu M. Short sleep duration is associated with hypertension risk among adults: a systematic review and meta-analysis. Hypertension Research. 2012;35(10):1012–8. doi: 10.1038/hr.2012.91. [DOI] [PubMed] [Google Scholar]
- 6.Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European heart journal. 2011;32(12):1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 7.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2010;33(2):414–20. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cappuccio FP, Taggart FM, Kandala N-B, Currie A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. Journal of sleep research. 2009;18(2):148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 11.Thoits PA. Stress and health major findings and policy implications. Journal of Health and Social Behavior. 2010;51(1 suppl):S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- 12.Mezick EJ, Matthews KA, Hall M, Strollo PJ, Jr, Buysse DJ, Kamarck TW, et al. Influence of race and socioeconomic status on sleep: Pittsburgh Sleep SCORE project. Psychosomatic Medicine. 2008;70(4):410–6. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37(3):601–11. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americana: A meta-analysis. Sleep Medicine. 2011;12(3):209–14. doi: 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Medicine. 2010;11(5):470–8. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy people 2020. Washington, DC: [Google Scholar]
- 18.Cespedes EM, Hu FB, Redline S, Rosner B, Alcantara C, Cai J, et al. Comparison of self-reported sleep duration with actigraphy: Results from the Hispanic Community Health Study/Study of Latinos Sueño Ancillary Study. American Journal of Epidemiology. 2016;183(6):561–73. doi: 10.1093/aje/kwv251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uchino BN, Ruiz JM, Smith TW, Smyth JM, Taylor DJ, Allison M, et al. Ethnic/racial differences in the association between social support and levels of C-reactive proteins in the North Texas Heart Study. Psychophysiology. 2016;53(1):64–70. doi: 10.1111/psyp.12499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sadeh A. The role and validity of actigraphy in sleep medicine: An update. Sleep Medicine Reviews. 2011;15(4):259–67. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Tabachnick BG, Fidell LS. Using Multivariate Statistics. Pearson/Allyn & Bacon; 2007. [Google Scholar]
- 22.Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, Jean-Louis G. Sleep in America: Role of racial/ethnic differences. Sleep Medicine Reviews. 2013;17(4):255–62. doi: 10.1016/j.smrv.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10(1):475. doi: 10.1186/1471-2458-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grandner MA, Petrov MER, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. Journal of Clinical Sleep Medicine. 2013;9(9):897–905. doi: 10.5664/jcsm.2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baldwin CM, Ervin A-M, Mays MZ, Robbins J, Shafazand S, Walsleben J, et al. Sleep disturbances, quality of life, and ethnicity: the Sleep Heart Health Study. Journal of Clinical Sleep Medicine. 2010;6(2):176. [PMC free article] [PubMed] [Google Scholar]
- 26.Adler NE, Rehkopf DH. US disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–52. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 27.Seeman MV. Psychopathology in women and men: focus on female hormones. Am J Psychiatry. 1997;154(12):1641–7. doi: 10.1176/ajp.154.12.1641. [DOI] [PubMed] [Google Scholar]
- 28.Nolen-Hoeksema S. Emotion regulation and psychopathology: The role of gender. Annual Review of Clinical Psychology. 2012;8:161–87. doi: 10.1146/annurev-clinpsy-032511-143109. [DOI] [PubMed] [Google Scholar]