Abstract
Objective
Few studies have evaluated moderators of mindfulness-based relapse prevention (MBRP) for substance use disorders (SUD). We tested whether baseline patterns of scores for SUD symptom severity and depression and anxiety symptoms moderated the efficacy of MBRP.
Method
We used a latent class moderation approach with data from a randomized trial of MBRP compared to cognitive-behavioral relapse prevention (RP) and treatment-as-usual (TAU) (Bowen et al., 2014; N=286, mean age=38.44 (SD=10.92), 71.8% male, 48.4% non-white) and a randomized trial comparing MBRP to TAU (Bowen et al., 2009; N=168, mean age=40.45 (SD=0.28), 63.7% male, 44.6% non-white). Indicators for the latent class models were measures of SUD severity (Severity of Dependence Scale and Short Inventory of Problems), depression symptoms (Beck Depression Inventory), and anxiety symptoms (Beck Anxiety Inventory).
Results
In both trials, 3 latent classes provided the best fit: a “high/high” class characterized by high SUD severity and depression and anxiety symptoms, a “high/low” class characterized by high SUD severity and low depression and anxiety symptoms, and a “low/low” class characterized by low SUD severity and depression and anxiety symptoms. In both trials, we found significant latent class-by-treatment interaction effects: there were significant and large effects of MBRP on substance use outcomes in the high/high and high/low classes, but no MBRP effect in the low/low class.
Conclusion
MBRP may be an optimal treatment for preventing relapse among clients with severe levels of SUD symptoms and depression and anxiety symptoms, as well as clients with only severe SUD symptoms.
Keywords: Mindfulness-based relapse prevention, treatment moderators, substance use disorder, depressive symptoms, anxiety
Introduction
Substance use disorders (SUD) are associated with serious costs to societies and individuals across the world (Whiteford et al., 2014). Although effective treatments for SUDs exist, relapse to problematic substance use following treatment is still common (McLellan, 2000; McLellan, McKay, Forman, Cacciola, & Kemp, 2005). Continued efforts to develop and improve relapse prevention treatments are needed (Witkiewitz & Marlatt, 2004). Mindfulness-based relapse prevention (MBRP; Bowen, Chawla, & Marlatt, 2011) is a behavioral treatment for SUD that shows promise in enhancing long-term outcomes among individuals recovering from SUDs. Several randomized controlled trials have demonstrated that MBRP is efficacious in the treatment of SUDs (Bowen et al., 2009; Bowen et al., 2014; Brewer et al., 2009; Witkiewitz et al., 2014). Bowen et al. (2014) recently conducted the largest empirical study of MBRP to date. In this study, 286 participants were randomized to either MBRP, cognitive-behavioral relapse prevention, or treatment-as-usual. At the one-year follow-up, MBRP participants reported significantly lower rates of heavy drinking and fewer drug use days than participants assigned to the comparison treatments.
Although empirical evidence on overall efficacy of MBRP is growing, few studies have examined whether MBRP may be more effective for some types of clients versus others. Matching treatments to client characteristics has been of interest to researchers and clinicians in the addiction field for many decades (Project MATCH Research Group, 1997). More recently, interest in client-treatment matching has been renewed following President Obama’s announcement of the Precision Medicine Initiative (Collins & Varmus, 2015). Research on client characteristics that predict differential response to MBRP can facilitate precision medicine by aiding treatment providers in deciding which SUD clients may benefit the most from MBRP compared to other available treatments.
Extant research on mindfulness-based interventions for SUDs provides some guidance as to which clients may benefit most from MBRP. Witkiewitz and Bowen (2010) found that receiving MBRP attenuated the association between end-of-treatment depressive symptoms and subsequent self-reported craving 2-months following treatment, which in turn predicted less substance use 4-months post-treatment. Glasner et al. (2016) compared MBRP to a health education control intervention among adults with stimulant use disorders who were receiving contingency management. Among individuals with depressive and anxiety disorders, MBRP was more effective than the control condition in preventing stimulant use post-treatment. Other studies suggest that mindfulness-based interventions are effective in reducing negative affect and craving among individuals with SUDs and co-occurring psychiatric disorders (Garland et al., 2016; Zemestani & Ottaviani, 2016). Taken together, these empirical findings suggest MBRP may be a suitable treatment option among individuals with SUDs and co-occurring psychiatric symptoms such as anxiety and depression. Indeed, two review papers have proposed that mindfulness-based interventions may be particularly appropriate for individuals with co-occurring SUDs and depression (Brewer et al., 2010; Vujanovic et al., 2016).
Researchers have also examined client factors that moderate the efficacy of mindfulness-based interventions for other mental disorders. Arch and Ayers (2013) found that mindfulness-based stress reduction (MBSR) was more effective than cognitive behavioral therapy (CBT) in the treatment of anxiety disorders among individuals with moderate to high co-occurring depressive symptoms. Wolitzky-Taylor, Arch, Rosenfield, and Craske (2012) found that acceptance and commitment therapy (ACT) was more effective than CBT in treating anxiety disorders among those clients with co-occurring mood disorders. Finally, Williams et al. (2014) found that mindfulness-based cognitive therapy (MBCT) was more effective than cognitive psychological education (a dismantled version of MBCT that did not include meditation training) and treatment-as-usual in treating recurrent depression among clients with high severity of childhood trauma. Findings from these studies suggest that mindfulness-based interventions more generally may be particularly suitable for clients with relatively severe levels of co-occurring mental health symptoms in addition to their primary diagnosis.
Other studies on treatment moderators of mindfulness-based interventions suggest that severity of primary diagnosis may also play a role in moderating treatment effects. For example, in a meta-analysis of MBCT, Piet and Hougaard (2011) found that MBCT for recurrent depression demonstrated the largest treatment effects relative to comparison treatments among individuals with three or more depressive episodes. Arch and Ayers (2013) found some support for anxiety disorder severity as a moderator of MBSR relative to CBT, such that MBSR outperformed CBT at post-treatment among those with the highest levels of anxiety disorder severity. Finally, two studies examining dialectical behavior therapy (DBT) found that higher baseline severity predicted better responses in DBT than comparison treatments (Pistorello et al., 2012; Robinson & Safer, 2012).
Based on the current body of research on mindfulness-based interventions for SUDs and other disorders, co-occurring depression and anxiety symptoms and SUD severity stand out as potential key moderators of MBRP efficacy. Hence, in the current study the primary aim was to test whether baseline patterns of scores on measures of SUD symptom severity and depression and anxiety symptoms moderated the efficacy of MBRP relative to comparison treatments. We used data from two randomized trials of MBRP (Bowen et al., 2009; Bowen et al., 2014). Because we were interested in patterns of severity across SUD symptoms and depression and anxiety symptoms, we opted to use a subgroup analytic approach. That is, we used latent class analysis (Collins & Lanza, 2010), to empirically identify subgroups or classes of clients with distinct patterns of responses on measures of SUD severity and depression and anxiety symptoms. Subsequently, this categorical latent class variable was used as the moderator variable in moderation analyses. We hypothesized that MBRP would demonstrate the strongest treatment effects among a subgroup of clients characterized by a pattern of high levels of baseline SUD severity and high levels of depression and anxiety symptoms.
Method
Participants and Procedures
This study was a secondary data analysis using data from two randomized controlled trials of MBRP for SUDs. In both trials, MBRP was delivered as an aftercare treatment among individuals who had just completed inpatient or intensive outpatient treatment. In the first study (referred to as study 1; Bowen et al., 2014), participants were randomized to one of three conditions: mindfulness-based relapse prevention (MBRP), cognitive-behavioral relapse prevention (RP), or treatment-as-usual (TAU). Participants in study 1 were 286 individuals with SUDs, recruited from a two-site SUD treatment agency. Demographic and descriptive treatment-related information for study 1 participants is presented in Table 1. Inclusion criteria were: age 18 or older, fluency in English, medical clearance, ability to attend treatment sessions, agreement to random assignment, and prior completion of either intensive outpatient or inpatient care. Exclusion criteria were: current psychotic disorder, dementia, suicidality, imminent danger to others, or participation in prior MBRP trials. Of note, participants assigned to MBRP or RP did not attend standard aftercare groups during the study intervention period, but returned to these aftercare groups following completion of the assigned 8-week treatment. TAU participants continued attending standard aftercare groups, which included clients not enrolled in the study.
Table 1.
Descriptive Statistics for Study Variables in Study 1, n (%) or mean (standard deviation)
| TAU/RP (n= 183) |
MBRP only (n=103) |
Full Sample (n=286) |
|
|---|---|---|---|
|
|
|||
| Male | 125 (69.1%) | 76 (76.8%) | 201 (71.8%) |
| Female | 56 (30.9%) | 23 (23.2%) | 79 (28.2%) |
| Race/Ethnicity | |||
| Non-Hispanic White | 89 (48.9%) | 57 (56.4%) | 146 (51.6%) |
| Racial/Ethnic Minority | 93 (51.1%) | 44 (43.6%) | 137 (48.4%) |
| Age | 38.07 (10.89) | 39.11 (10.99) | 38.44 (10.92) |
| Prior Treatment Episodes | 1.50 (1.46) | 1.58 (1.52) | 1.53 (1.48) |
| Treatment Hours Completed | 11.68 (7.32) | 12.02 (6.63) | 11.81 (7.07) |
| Baseline SDS | 9.37 (4.16) | 9.52 (4.23) | 9.43 (4.18) |
| Baseline SIP | 10.39 (5.35) | 11.04 (5.42) | 10.63 (5.37) |
| Baseline BDI | 13.78 (9.92) | 12.17 (10.68) | 13.21 (10.21) |
| Baseline BAI | 11.09 (10.95) | 10.30 (12.30) | 10.81 (11.43) |
| 12-Month Drug Use Days | 5.34 (17.51) | 3.06 (15.08) | 4.52 (16.68) |
| 12-Month Heavy Drinking Days | 4.28 (13.64) | 1.44 (7.66) | 3.28 (11.94) |
Note. BDI = Beck Depression Inventory. BAI = Beck Anxiety Inventory. SIP = Short Inventory of Problems. SDS = Severity of Dependence Scale; MBRP = Mindfulness-Based Relapse Prevention; RP = Relapse Prevention; TAU = Treatment as Usual.
In the second study (referred to as study 2; Bowen et al., 2009), participants were randomized to either MBRP or TAU. Participants were 168 individuals with SUDs recruited from one SUD treatment agency. Demographic and descriptive treatment-related variables for study 2 participants are presented in Table 2. Inclusion criteria were: age 18 or older, fluency in English, completion of intensive outpatient or inpatient care, and medical clearance. Exclusion criteria were: need for more intensive treatment, significant withdrawal risk, imminent suicide risk, dementia, and psychosis.
Table 2.
Descriptive Statistics for Study Variables in Study 2, n (%) or mean (standard deviation)
| TAU (n=75) |
MBRP only (n=93) |
Full Sample (n=168) |
|
|---|---|---|---|
|
|
|||
| Gender | |||
| Male | 47 (62.7%) | 60 (64.5%) | 107 (63.7%) |
| Female | 28 (37.3%) | 33 (35.5%) | 61 (36.3%) |
| Race/Ethnicity | |||
| Non-Hispanic White | 41 (54.7%) | 59 (63.4%) | 93 (55.4%) |
| Racial/Ethnic Minority | 34 (45.3%) | 34 (36.6%) | 75 (44.6%) |
| Age | 39.97 (10.39) | 40.84 (10.23) | 40.45 (10.28) |
| Treatment Hours Completed | 9.75 (8.17) | 10.37 (4.83) | 10.09 (6.51) |
| Baseline SDS | 9.53 (4.62) | 9.53 (4.84) | 9.53 (4.53) |
| Baseline SIP | 11.67 (4.67) | 11.01 (5.43) | 11.30 (5.10) |
| Baseline BDI | 14.80 (12.94) | 13.08 (9.57) | 13.86 (11.27) |
| Baseline BAI | 10.84 (11.88) | 10.16 (10.81) | 10.47 (11.27) |
| During Treatment AODD Days | 2.57 (9.08) | 0.06 (0.30) | 1.12 (5.99) |
Note. BDI = Beck Depression Inventory. BAI = Beck Anxiety Inventory. SIP = Short Inventory of Problems. SDS = Severity of Dependence Scale; MBRP = Mindfulness-Based Relapse Prevention; TAU = Treatment as Usual. AODD = Alcohol or drug use days.
Measures
Substance use
In both study 1 and study 2, alcohol and drug use were measured with the Timeline Followback interview (Sobell & Sobell, 1992), a well-validated calendar-based method for assessing substance use. In the current study, we used the primary substance use outcome variables that were used in the main outcome papers for studies 1 and 2. In study 1 (Bowen at al., 2014), the two primary outcomes were number of drug use days and number of heavy drinking days (with heavy drinking defined as 4+/5+ standard drinks for women/men). These outcomes were assessed during the 90-day period prior to the 3-, 6- and 12-month post-treatment assessments. For the current study analyses, we focused on the final 12-month post-treatment substance use outcomes because it was the most distal, and because Bowen et al. (2014) found significant differences between MBRP and RP at this time point. In study 2 (Bowen et al., 2009), there was one primary outcome: number of alcohol or drug use days. This outcome was assessed during the 60-day period prior to the post-treatment, and at 2- and 4- months post-treatment. In the current study analyses, we chose to include only post-treatment outcomes, rather than follow-up outcomes, because the subgroup analyses ultimately led to subgroups with small samples sizes, and the combination of missing substance use follow-up data due to attrition and small cell sizes (i.e., number of individuals in a particular subgroup within a treatment group) led to model convergence issues in the moderation models with the follow-up outcomes as the dependent variables.
Substance use disorder symptom severity
In both study 1 and study 2, SUD symptom severity at baseline was measured with the Severity of Dependence Scale (SDS; Gossop et al., 1995) a 5-item self-report measure with total scores ranging from 0 to 15, and with the Short Inventory of Problems (Blanchard et al., 2003), a 15-item self-report measure of substance-related consequences with total scores ranging from 0 to 15. Internal consistency reliabilities were in the high range: SDS (study 1 = 0.86, study 2 = 0.87) and SIP (study 1 = 0.96, study 2 = 0.95).
Depression and anxiety symptoms
In both studies 1 and 2, depression symptoms at baseline were measured with the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996), a 21-item self-report measure of depressive symptoms and anxiety symptoms were measured with the Beck Anxiety Inventory (BAI; Beck & Steer, 1993), a 21-item self-report measure of anxiety symptoms. Total scores on the BDI and BAI range from 0 to 63. Internal consistency reliabilities were in the high range and identical across studies: BDI (study 1 = 0.92, study 2 = 0.92) and BAI (study 1 = 0.94, study 2 = 0.94).
Interventions
In both study 1 and study 2, the MBRP intervention was delivered as outlined in the MBRP Clinician’s Guide (Bowen, Chawla, & Marlatt, 2011). The intervention involved eight weekly 2-hour group-based sessions, and each group was led by two therapists. Core components included guided in-session meditation practices, open discussion about personal experiences during meditation practices, discussion of various core themes of each session (e.g., triggering situations, self-care and compassion), and discussion of applications of mindfulness to daily living and prevention of substance use. Additionally, participants were provided audio-recordings of mindfulness meditations to practice at home.
In both studies 1 and 2, the TAU program was based on 12-step programs such as Alcoholics Anonymous and Narcotics Anonymous. In addition, the TAU program involved process-oriented groups that focused on topics such as communication and stress management. TAU groups met 1 to 2 times per week for 1.5-hour sessions.
RP was a treatment condition in study 1 only. The RP intervention was based on an established cognitive-behavioral relapse prevention program (Monti, Kadden, Cooney, & Abrams, 2002), and similarly involved eight weekly 2-hour group-based sessions. In addition to matching MBRP in time, the RP intervention was designed to match MBRP in format, size, location, and the amount of assigned homework. Core topics of the RP intervention included self-efficacy, coping skills training, goal setting, problem solving, and social support.
Statistical Analyses
Mplus Version 7.4 (Muthén & Muthén, 2012) was used to conduct analyses. All analyses were conducted separately for studies 1 and 2. We used a latent class moderation approach (Lanza & Rhoades, 2013), rather than the traditional variable-centered approach of conducting separate moderated regression analyses for each moderator. That is, we used latent class analysis (Collins & Lanza, 2010) to empirically identify latent classes of individuals with distinct patterns of scores across the four continuous moderator variables of interest: the two measures of SUD symptom severity (total scores on the SDS and the SIP), the measure of depression symptoms (total score on BDI-II), and the measure of anxiety symptoms (total scores on the BAI). Subsequently, we used the classify-analyze approach (Lanza & Rhoades, 2013) in which the latent class variable was used as the moderator variable in moderated regression analyses. Latent class moderation can be particularly useful when multiple moderator variables are considered at once and when there may be meaningful and distinct patterns of responses across these several moderator variables (Collins & Lanza, 2010). Moreover, we selected the latent class moderation approach because it provided a novel approach to assessing the roles of SUD severity and depression and anxiety symptoms, when considered simultaneously, in moderating MBRP effects. Considering the high rates of comorbidity of SUD with depression and anxiety (Conway, Compton, Stinson, & Grant, 2006; Grant, 1995), and the poor treatment outcomes common in comorbid clients (Dodge, Sindelar, & Sinha, 2005; Hasin et al., 2002; McKay et al., 2016; Simpson, Joe, & Broome, 2004) clinicians may consider severities of both SUD and depression and anxiety symptoms together when making treatment decisions regarding a particular client.
The first step in our analyses was to identify latent classes or subgroups of individuals based on their patterns of scores on baseline measures of SUD symptoms severity and depression and anxiety symptoms We first conducted latent class analyses in study 1, and then conducted the same analyses in study 2 to determine whether the same latent classes could be identified. For each latent class model, there were four continuous indicators of latent class: SDS scores, SIP scores, BDI scores, and BAI scores. To determine the optimal class solution (i.e., number of classes), we considered several factors: 1) values on model fit indices, including Akaike’s Information Criterion (AIC), Bayesian Information Criterion (BIC), and sample size adjusted BIC (aBIC), with lower values indicating better fit; 2) the Lo-Mendell-Rubin Adjusted Likelihood Ratio Test (Lo et al. 2001), which compares whether a k class solution fits better than a k − 1 class solution; 3) entropy values, with higher values indicating better classification precision, and; 4) the parsimony and theoretical relevance of the class solution. For each latent class model, we examined the conditional response means to interpret each identified class. The conditional response means provide the estimate mean value for each indicator given expected classification in a particular latent class.
The next major step in our analyses was to conduct regression models to examine the main effects of treatment and latent class on outcomes, and then to examine the interaction effect between treatment and latent class. For all regression models in this study, including main effect and interaction models, we used negative binomial regression because there was an over-dispersion of data in the substance use outcome variables due to a high frequency of zero values. For study 1, the treatment variable was dummy-coded as 1 = MBRP and 0 = RP/TAU. RP and TAU were collapsed into one category because there were no differences between TAU and RP in the primary outcomes at month 12 with MBRP outperforming both TAU and RP on the primary outcomes at month 12 (Bowen et al., 2014). For study 2, the treatment variable was dummy-coded as 1 = MBRP, 0 = TAU. In both study 1 and study 2, each individual was assigned class membership based on the posterior class probabilities. A series of dummy-coded class variables (e.g., 1 = classified to class x, 0 = not classified to class x) were then created to represent latent classes in regression models.
For the main effect models and the interaction models, we controlled for the same set of covariates that were included in the main outcome analyses for study 1 (Bowen et al., 2014) and study 2 (Bowen et al., 2009). For study 1, these covariates included: age, number of prior treatment episodes, treatment hours completed, and treatment site (two treatment sites, coded 0,1). For study 2, these covariates included: race/ethnicity (1 = white, 0 = non-white) and treatment hours completed. In study 1 and study 2, the treatment hours covariate was total treatment hours at the treatment center, including study intervention hours and any additional care the participant received at the treatment center.
For each interaction model in study 1 and study 2, in addition to the covariates mentioned above, we included the dummy-coded latent class moderator variables, the treatment variable, and interaction terms (treatment × each latent class dummy variable). To investigate the nature of any statistically significant two-way interactions, we analyzed the effect of treatment within each latent class. For these follow-up simple slope analyses, we also controlled for the abovementioned set of covariates in study 1 and study 2. To further probe the significant interaction effects, we also report the following descriptive statistics by treatment group: 1) percentage who abstained from heavy drinking or drug use, and 2) mean score for the outcomes. These statistics were examined to provide further clarity about differences in treatment outcomes by treatment condition within each latent class.
We provide the effect size of treatment in terms of incidence rate ratios (IRRs). IRR can be interpreted as the rate of increase (when the IRR is above 1.0) or the rate of decrease (when the IRR is below 1.0) in heavy drinking or drug use days for a 1-unit increase in the predictor (with other predictors in the model held constant). To facilitate interpretation of IRRs, we provide IRR values that correspond with Cohen’s d effect size cut-offs (Borenstein, Hedges, Higgins, & Rothstein, 2009): an IRR of approximately 1.44 (for IRRs above 1) or 0.69 (for IRRs below 1) corresponds with a Cohen’s d effect size of 0.2 (small effect); an IRR of approximately 2.48 or 0.40 corresponds with a Cohen’s d effect size of 0.5 (medium effect); and an IRR of approximately 4.27 or 0.23 corresponds with a Cohen’s d effect size of 0.8 (large effect). Finally, for all statistical models, we used all available data and parameters were estimated with full information maximum likelihood (Witkiewitz et al., 2014).
Results
Latent Class Models
Study 1
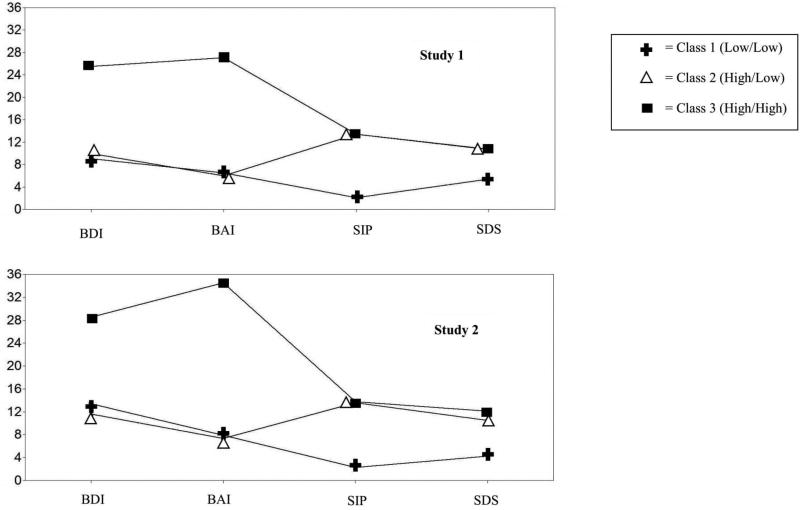
Based on the model fit statistics and the LRT tests across the latent class models (see Table 3), we chose a 3-class solution in study 1. Entropy of 0.892 indicated excellent classification precision. The pattern of conditional response means (see Figure 1) were used to characterize the three classes that were identified as providing the best fit to the data based on BIC and LRT. Using the conditional response means, we labeled class 1 as the “low/low” class,, which was characterized by low scores across the SUD severity and depression and anxiety symptom indicators.. We labeled class 2 as the “high/low” class, which was characterized by high scores on SUD severity indicators and low scores on and depression and anxiety symptom indicators. Finally, we labeled class 3 as the “high/high” class, which was characterized by high scores across SUD severity and depression and anxiety symptom indicators.. The latent class prevalences (proportion of individuals expected to be classified within each class) were: low/low class (0.24), high/low class (0.54), and high/high class (0.22).
Table 3.
Fit Statistics for Class Solutions 1 through 5 for Latent Class Analyses in Studies 1 and 2
| Study 1 | |||||
|
| |||||
| Number of Classes | |||||
|
| |||||
| Fit Statistics | 1 | 2 | 3 | 4 | 5 |
| AIC | 7666.84 | 7355.85 | 7202.01 | 7122.49 | 7091.98 |
| BIC | 7696.06 | 7403.33 | 7267.75 | 7206.49 | 7194.25 |
| Adjusted BIC | 7670.69 | 7362.11 | 7210.68 | 7133.56 | 7105.46 |
| Lo-Mendell-Rubin test | — | 310.02 p <0.001 | 158.24 p < 0.001 | 86.46 p = 0.07 | 39.12 p = 0.57 |
| Entropy | — | 0.952 | 0.892 | 0.901 | 0.907 |
|
| |||||
| Study 2 | |||||
|
| |||||
| AIC | 4530.57 | 4364.38 | 4284.84 | 4209.35 | 4189.85 |
| BIC | 4555.56 | 4404.99 | 4341.07 | 4281.20 | 4277.33 |
| Adjusted BIC | 4530.23 | 4363.83 | 4284.08 | 4208.37 | 4188.67 |
| Lo-Mendell-Rubin test | — | 169.57 p<0.001 | 86.18 p<0.001 | 66.62 p=0.10 | 28.38 p=0.32 |
| Entropy | — | 0.949 | 0.931 | 0.944 | 0.947 |
Note. Akaike's Information Criterion (AIC), the Bayesian Information Criterion (BIC), sample size adjusted BIC (adjusted BIC). Lower values of AIC BIC and Adjusted BIC indicate a better fitting model.
Figure 1.
Conditional response means for the 3-class solution in study 1 and study 2. BDI = Beck Depression Inventory. BAI = Beck Anxiety Inventory. SIP = Short Inventory of Problems. SDS = Severity of Dependence Scale. Total scores for each measure can fall in the following ranges: BDI and BAI (0 to 63), SIP and SDS (0 to 15).
Study 2
Our next step was to test whether we could replicate the results from the latent class analyses in study 2. Based on the model fit statistics and the LRT tests (see Table 3), we also chose a 3-class solution in study 2. A very similar pattern of conditional response means was found across the 3 classes (see Figure 1). Accordingly, we labeled the 3 classes in study 2 in the same manner as the classes were labeled in study 1. The latent class prevalences in study 2 were: low/low class (0.29), high/low class (0.69), and high/high class (0.11).
Main Effects of Latent Class
Study 1
After controlling for site, treatment hours, age, number of prior treatment episodes, and treatment condition, expected membership in the high/low class (with the low/low class as the reference class) predicted higher 12-month drug use days (DUD) (B(SE) = 1.6 (0.60), p = 0.01), but did not significantly predict 12-month heavy drinking days (HDD) (B(SE) = 1.04 (0.72), p = 0.15). After controlling for site, treatment hours, age, number of prior treatment episodes, and treatment condition, expected membership in the high/high class (with the low/low class as the reference class) predicted higher DUD (B(SE) = 1.57 (0.76), p = 0.04), but did not significantly predict 12-month HDD (B(SE) = 1.06 (0.72), p = 0.14).
Study 2
For study 2, the number of participants with expected classification to the high/high class was very small (11% of sample or approximately 18 individuals). Accordingly, for the interaction models, the high/high class and high/low class were collapsed into one group and a binary moderator variable (0 = low/low class, 1= high/high class or high/low class) was used in the models. Thus, for the main effect of class for study 2, we report the main effect of this binary variable. After controlling for race, treatment hours completed, and treatment condition, expected membership in the high/high class or the high/low class (with the low/low class as the reference group) did not significantly predict post-treatment alcohol or drug use days (AODD) (B(SE) = −1.05 (1.14), p = 0.356).
Main Effects of Treatment in the Full Samples
Study 1
As seen in Table 5, in the full sample for study 1, treatment condition did not significantly predict 12-month HDD, and treatment condition had a significant main effect on 12-month DUD, such that MBRP participants reported 82% fewer DUD than RP/TAU participants (Incidence Rate Ratio (IRR)= 0.18).
Table 5.
Effects of Treatment among Full Sample and among Latent Classes in Study 1
| 12-Month Heavy Drinking Days (HDD) as Outcome | |||
|
| |||
| Effect of Treatment (Coded 0 = RP or TAU, 1 = MBRP) | n (%) with zero HDD | Mean (SD) | |
|
| |||
| Full Sample | B (SE) = −1.13 (0.69) | MBRP only: 71 (89.9%) | MBRP only: 1.44 (7.65) |
| p=0.10 | RP/TAU: 110 (75.3%) | RP/TAU: 4.28 (13.64) | |
| IRR = 0.32 | TAU only: 57 (75.0%) | TAU only: 4.64 (14.93) | |
| RP only: 53 (75.7%) | RP only: 3.89 (12.17) | ||
| Low/low class | B (SE) = 1.11 (1.15) | MBRP only: 18 (94.7%) | MBRP only: 1.32 (5.7) |
| p=0.33 | RP/TAU: 31 (79.5%) | RP/TAU: 0.54 (1.45) | |
| IRR = 3.03 | TAU only: 17 (77.3%) | TAU only: 0.45 (1.29) | |
| RP only: 14 (82.4%) | RP only: 0.65 (1.65) | ||
| High/high class | B (SE) = −3.14 (0.92)** | MBRP only: 14 (87.5%) | MBRP only: 0.38 (1.26) |
| p=0.002 | RP/TAU: 25 (75.8%) | RP/TAU: 8.67 (21.90) | |
| IRR = 0.04 | TAU only: 13 (72.2%) | TAU only: 8.78 (24.26) | |
| RP only: 12 (80.0%) | RP only: 8.53 (19.53) | ||
| High/lowClass | B (SE) = −3.27 (0.71*) | MBRP only: 39 (88.6%) | MBRP only: 1.89 (9.56) |
| p=0.04 | RP/TAU: 54 (73.0%) | RP/TAU: 4.30 (11.92) | |
| IRR = 0.04 | TAU only: 27 (75.0%) | TAU only: 5.14 (13.07) | |
| RP only: 27 (71.1%) | RP only: 3.50 (10.82) | ||
|
| |||
| 12-Month Drug Use Days (DUD) as Outcome | |||
|
| |||
| Effect of Treatment (Coded 0 = RP or TAU, 1 = MBRP) | n (%) with zero HDD | Mean (SD) | |
|
| |||
| Full Sample | B (SE) = −1.72 (0.49)** | MBRP only: 74 (89.2%) | MBRP only: 3.06 (15.08) |
| p=0.001 | RP/TAU: 119 (81.0%) | RP/TAU: 5.34 (17.51) | |
| IRR = 0.18 | TAU only: 63 (82.9%) | TAU only: 4.63 (16.03) | |
| RP only: 56 (78.9%) | RP only: 6.10 (19.05) | ||
| Low/low class | B (SE) = −0.42 (0.84) | MBRP only: 18 (90.0%) | MBRP only: 2.85 (12.51) |
| p=0.62 | RP/TAU: 34 (87.2%) | RP/TAU: 5.19 (19.10) | |
| IRR = 0.66 | TAU only: 20 (90.9%) | TAU only: 1.32 (5.55) | |
| RP only: 14 (82.4%) | RP only: 10.18 (27.90) | ||
| High/high class | B (SE) = −2.79 (1.03)** | MBRP only: 15 (88.2%) | MBRP only: 0.35 (1.22) |
| p=0.007, | RP/TAU: 26 (78.8) | RP/TAU: 4.58 (13.32) | |
| IRR = 0.06 | TAU only: 14 (77.8%) | TAU only: 5.33 (17.61) | |
| RP only: 12 (80.0%) | RP only: 3.67 (9.51) | ||
| High/low Class | B (SE) = −1.72 (0.59)** | MBRP only: 40 (88.9%) | MBRP only: 4.24 (18.74) |
| p=0.003, | RP/TAU: 59 (78.7%) | RP/TAU: 5.76 (18.13) | |
| IRR = 0.18 | TAU only: 29 (80.6%) | TAU only: 6.31 (19.27) | |
| RP only: 30 (76.9%) | RP only: 5.26 (17.23) | ||
Note.
= p < .05;
= p < .01.
MBRP = Mindfulness-Based Relapse Prevention; RP = Relapse Prevention; TAU = Treatment as Usual; B = unstandardized regression coefficient; SE = standard error. IRR = Incidence Rate Ratio. IRR can be interpreted as the rate of increase (when the IRR is above 1.0) or the rate of decrease (when the IRR below 1.0) in heavy drinking or drug use days for a 1-unit increase in the predictor (with other predictors in the model held constant). All negative binomial regression models conducted among the full sample and within latent classes controlled for the following covariates: site, age, treatment hours completed, and prior treatment episodes.
Study 2
As seen in Table 6, in the full sample for study 2 treatment condition had a significant main effect on post-treatment AODD, such that MBRP participants had 96% fewer post-treatment AODD than TAU participants (IRR = 0.04).
Table 6.
Effects of Treatment among Full Sample and among Latent Classes in Study 2
| Post-Treatment Alcohol or Drug Use Days (AODD) as Outcome | |||
|---|---|---|---|
|
| |||
| Effect of Treatment (Coded 0 = TAU, 1 = MBRP) |
n (%) with zero AODD | Mean (SD) | |
| Full Sample | B (SE) = −3.32 (0.66)** | MBRP only: 73 (94.8%) | MBRP only: 0.10 (0.30) |
| p<0.001 | TAU only: 47 (83.9%) | TAU only: 2.57 (9.08) | |
| IRR = 0.04 | |||
| Low/low class | B (SE) = 2.32 (1.42) | MBRP only: 14 (87.5%) | MBRP only: 0.19 (0.54) |
| p=0.103 | TAU only: 8 (88.9%) | TAU only: 0.22 (0.67) | |
| IRR = 9.97 | |||
| High/high Class and High/low class combined | B (SE) = −4.33 (0.85)** | MBRP only: 59 (96.7%) | MBRP only: 0.03 (0.18) |
| p<0.001 | TAU only: 39 (83.0%) | TAU only: 3.02 (9.86) | |
| IRR = 0.01 | |||
Note.
= p < .05;
= p < .01.
MBRP = Mindfulness-Based Relapse Prevention. TAU = Treatment as Usual. B =unstandardized regression coefficient; SE = standard error. IRR = Incidence Rate Ratio. IRR can be interpreted as the rate of increase (when the IRR is above 1.0) or the rate of decrease (when the IRR below 1.0) in heavy drinking or drug use days for a 1-unit increase in the predictor (with other predictors in the model held constant). All negative binomial regression models conducted among the full sample and within latent classes controlled for the following covariates: treatment hours completed and race (coded 1= non-Hispanic white, 0 = non-white).
Interaction of Latent Class and Treatment Condition in the Prediction of Substance Use Outcomes1
Study 1
As seen in Table 4, there was a significant interaction between the high/high class (with the low/low class as the reference class) and treatment condition in the prediction of 12-month HDD and DUD. To probe the nature of the interaction, we examined the main effect of treatment within latent class. Table 5 presents the main effects of treatment in the full sample and within each latent class, as well as the number and percentage of participants abstinent from heavy drinking and drug use and the mean outcome scores for each treatment condition within the full sample and within each latent class. As seen in Table 5, among individuals with expected classification to the high/high class, there was a significant main effect of treatment on 12-month HDD and DUD, such that MBRP participants had 96% fewer 12-month HDD (IRR = 0.04) and 94% fewer DUD (IRR = .06) than RP/TAU participants. However, among individuals in the low/low class, there was not a significant difference in 12-month HDD between MBRP and RP/TAU participants.
Table 4.
Summary of Results Across Interaction Models with Latent Class × Treatment Condition Predicting Outcomes in Studies 1 and 2
| Study 1 | ||
| Predictor | 12-Month Heavy Drinking Days B (SE) | 12-Month Drug Use Days B (SE) |
|
| ||
| Low/low class as reference class | ||
| Treatment (0 = TAU or RP, 1 = MBRP) × high/high class | −3.53 (1.49)*; p=0.02 | −2.93 (1.48)*; p=0.04 |
| Treatment (0 = TAU or RP, 1 = MBRP) × high/low class | −3.19 (1.44)*; p =0.03 | −0.67 (1.11); p = 0.55 |
| High/low class as reference class | ||
| Treatment (0 = TAU or RP, 1 = MBRP) × high/high class | −0.34 (1.16); p = 0.77 | −2.26 (1.24); p=0.07 |
|
| ||
| Study 2 | ||
| Predictor | Post-Treatment Alcohol or Drug Days B (SE) | |
|
| ||
| Treatment (0 = TAU, 1 = MBRP) × latent class (0 = low/low class, 1 = high/high class or high/low class) | −5.33 (1.38)**; p <0.001 | |
Note.
= p < .05;
= p < .01.
B = unstandardized regression coefficient; SE = standard error. For Study 1, interaction models included the following other covariates: the dummy-coded latent class variables, the treatment variable, site, treatment hours completed, age, and prior treatment episodes. For Study 2, interaction models included the following other covariates: the dummy-coded latent class variables, the treatment variable, treatment hours completed, and race (coded 1= non-Hispanic white, 0 = non-white). MBRP = Mindfulness-Based Relapse Prevention; TAU = Treatment as Usual.
As seen in Table 4, there was also a significant interaction between the high/low class (with the low/low class as the reference class) in the prediction of 12-month HDD. As seen in Table 5, among individuals with expected classification to the high/low class, there was a significant main effect of treatment on 12-month HDD, such that MBRP participants reported 96% fewer HDD than RP/TAU participants (IRR = 0.04). However, as noted above, among individuals in the low/low class there was no main effect of treatment on 12-month HDD.
Study 2
As noted above, for study 2, the number of participants in the high/high class was very small (11% of sample or approximately 18 individuals). In turn, for the interaction models, the high/high class and high/low class were collapsed into one group and a binary latent class moderator variable (0 = low/low class, 1= high/high class or high/low class) was used. As seen in Table 4, there was a significant interaction between latent class and treatment in the prediction of post-treatment AODD. Table 5 presents the main effects of treatment in the full sample and within each latent class, as well as the number and percentage of participants abstinent from alcohol or drug use and the mean outcome score for each treatment condition within the full sample and within each latent class. As seen in Table 6, among individuals with expected classification to the high/high class or the high/low class, there was a significant main effect of treatment, such that MBRP participants reported 99% fewer AODD than TAU participants (IRR = 0.01). However, among individuals with expected classification in the low/low class, there was no main effect of treatment.
Discussion
The current study used data from two randomized controlled trials of mindfulness-based relapse prevention (MBRP; Bowen et al., 2009; Bowen et al., 2014) to test whether baseline patterns of substance use disorder (SUD) symptom severity and depression and anxiety symptoms moderated the efficacy of MBRP as an aftercare intervention for individuals with SUD. We used a latent class moderation approach (Lanza & Rhoades, 2013). In both MBRP trials, a 3-class solution fit the data best: a high/high class characterized by high scores on SUD severity and depression and anxiety symptoms, a high/low class characterized by high scores on SUD severity and low scores on depression and anxiety symptoms, and a low/low class characterized by low scores on SUD severity and depression and anxiety symptoms. In the larger MBRP trial (n = 286; Bowen et al., 2014) we found a significant interaction between the high/high class (with the low/low class as the reference class) and treatment condition in the prediction of both 12-month heavy drinking days (HDD) and drug use days (DUD). Among those in the high/high class, MBRP participants had significantly fewer 12-month HDD and DUD than those who received cognitive behavioral relapse prevention (RP) or treatment as usual (TAU), and both of these effects were in the large range. However, among those in the low/low class, there were no significant effect of treatment condition on either 12-month HDD or DUD. Furthermore, we found a significant interaction between the high/low class (with the low/low class as the reference class) in the prediction of 12-month HDD. Among those in the high/low class, those who received MBRP had significantly fewer 12-month HDD than those who received RP or TAU, and this effect was in the large range. In the smaller trial (n = 168; Bowen et al., 2009) we found a significant interaction effect between latent class and treatment condition in the prediction of post-treatment alcohol or drug use days (AODD). Among those in the high/high or high/low class, those who received MBRP had significantly fewer post-treatment AODD than those who received TAU, and this effect was in the large range. However, among those in the low/low class, there was no significant effect of treatment condition.
Taken together, findings from the current study suggest that MBRP may be particularly effective for more severe clients, specifically those with co-occurring high SUD symptom severity and high levels of depression and anxiety symptoms, as well as clients with high SUD symptom severity only. Additionally, our findings indicate that among clients with relatively less severe SUD symptoms and depression and anxiety symptoms, there may be no significant differences in treatment effects among MBRP, RP, and TAU. Our findings are in line with prior empirical findings showing that MBRP may be a suitable treatment for SUD clients with co-occurring psychiatric symptoms, such as anxiety and depression (Glasner et al., 2016; Witkiewitz & Bowen, 2010). Moreover, our findings support a growing body of evidence showing that mindfulness-based interventions more generally (e.g., mindfulness-based cognitive therapy, mindfulness-based stress reduction, acceptance and commitment therapy, dialectical behavior therapy) appear to be particularly effective for more vulnerable or severe clients, including clients with co-occurring disorders (Arch & Ayers, 2013; Wolitzky-Taylor et al., 2012), clients with high severity of childhood trauma (Williams et al., 2014), and clients with greater severity for their primary diagnosis being treated (Arch & Ayers, 2013; Piet & Hougaard, 2011; Pistorello et al., 2012; Robinson & Safer, 2012).
This line of research would benefit from future research examining how and why MBRP may be particularly effective in preventing substance relapse among individuals with more severe SUD, depressive, and anxiety symptoms. Future work could evaluate formal mindfulness meditation practice and use of informal mindfulness-based skills as mechanisms of change among more severe individuals (Witkiewitz et al., 2014). Of note, in this study we did not find evidence for a subgroup of clients characterized by severe depression and anxiety symptoms and low severity of SUD symptoms. This finding is not surprising given that SUD clients with clinically significant depression and anxiety symptoms are much more likely to have more severe, rather than less severe SUD symptoms (Dodge, Sindelar, & Sinha, 2005; Hasin et al., 2002; McKay et al., 2016; Simpson, Joe, & Broome, 2004).
A strength of the current study is the identification of similar latent class structures and treatment moderation effects by latent class across two independent samples of individuals receiving MBRP. However, in the smaller MBRP study (Bowen et al., 2009), we were limited to examining only substance use outcomes measured at the end-of-treatment assessment, which therefore included only within-treatment substance use behavior. Additionally, in the smaller MBRP study, due to small class sizes, we had to collapse the high/high class and the high/low class into one group. Hence, although the current study results from the smaller MBRP trial are consistent with results from the larger MBRP trial (Bowen et al., 2014), there were some differences in methodology for conducting interaction analyses in each study, thus not allowing an exact replication of the moderation effects across the two trials. Other limitations of this study are also noteworthy. Although latent class analysis is a useful approach for identifying subgroups, it is an inherently probabilistic approach, and it is possible that some participants were misclassified, thus skewing the results. The sizes of the latent classes in this study were also relatively small, and it is possible that this led to unreliable parameter estimates. It is also possible that we are not accurately “carving nature at its joints,” and that while the subgroup analyses were statistically useful, the subgroupings may not correspond to the types of complex clients seen in clinical practice, and many real-world clients may not “fit” into these subgroups. Reliance on retrospective self-report to measure days of substance use is another limitation of this study. We only examined substance use as an outcome, excluding other important outcomes such as psychosocial functioning and quality of life. Thus, it is not known whether MBRP differentially affects these other outcomes based on patterns of severity. Some of the identified latent classes, particularly the low/low and high/high class in each study sample, had relatively small sample sizes. It is possible that the small sample sizes of the classes could have affected the results. For example, in the case of the low/low class in each study sample, the relatively small sample size could have limited power to detect significant effects. Furthermore, the relatively small sample size of the high/high class in each study sample may limit the generalizability of our findings regarding the effect of MBRP among individuals with high depression and anxiety symptoms. However, we were able to detect large-sized treatment effects among this subgroup with high depression and anxiety, suggesting that the effects may be substantive. Future work with a larger sample of individuals with SUDs and co-occurring high depression and anxiety symptoms is warranted to elucidate the effect of MBRP among this specific population of individuals. A final limitation is including only anxiety and depressive symptoms as indicators of psychiatric symptoms. Other psychiatric symptoms (e.g., presence of other co-occurring disorders such as PTSD or personality disorders) may also play a role in predicting differential benefit from MBRP.
The current study demonstrated that MBRP may be beneficial for the more severe aftercare SUD clients. Specifically, our findings indicate that MBRP appears to be a good match for types of clients characterized by both severe levels of SUD symptoms and co-occurring depression and anxiety symptoms, as well as types of clients characterized by only severe SUD symptoms. Our study also suggests that the Severity of Dependence Scale (Gossop et al., 1995), the Short Inventory of Problems (Blanchard et al., 2003), the Beck Depression Inventory (Beck et al., 1996), and the Beck Anxiety Inventory (Beck & Steer, 1993) may be useful measurement instruments for identifying subgroups of clients that may respond best to MBRP. All of these measures have shown good psychometric properties and their brief, self-report format allows easy administration in clinical practice. Future work may provide further empirical support for using these measures in clinical practice to identify clients who are a good match for MBRP. Future research can also evaluate mechanisms of behaviors change (e.g., engagement in mindfulness practice and use of mindfulness skills in daily life) that may explain these treatment moderation effects, thereby providing further empirical guidance about key processes that mobilize and maintain change among severe SUD clients receiving MBRP.
Public Health Significance.
This study provides clarity about which aftercare clients with substance use disorders may benefit the most from receiving mindfulness-based relapse prevention (MBRP). Specifically, our findings suggest that MBRP may be most beneficial for clients characterized by severe levels of SUD symptoms and high co-occurring levels of depression and anxiety symptoms, as well as clients characterized by only severe SUD symptoms.
Acknowledgments
This research was supported by a training fellowship to Corey Roos (1T32 AA0018108-01A1; Barbara S. McCrady, principal investigator)
Footnotes
Sensitivity analyses were conducted in studies 1 and 2 to evaluate whether the pattern of interaction effects would remain the same if additional covariates were controlled for and if we adjusted for clustering within therapy groups. For these sensitivity analyses, the same set of covariates were included in moderation analyses for studies 1 and 2. These covariates included demographic variables [age, gender (0 = male, 1 = female), race (0 = White, 1 = Racial/Ethnic Minority), unemployment (0 = employed, 1 = unemployed), marital status (0 = not married/single, 1 = married), education status (0 = did not complete any college, 1 = completed some college) and treatment-related variables (treatment hours, prior treatment episodes, polysubstance use (0 = reported only one substance of choice, 1 = reported more than one substance of choice)]. Additionally, we adjusted for clustering within groups using the sandwich estimator in Mplus. Including the aforementioned set of covariates and adjusting for clustering in each study did not change the pattern of findings in the current moderation analyses.
References
- Arch JJ, Ayers CR. Which treatment worked better for whom? Moderators of group cognitive behavioral therapy versus adapted mindfulness based stress reduction for anxiety disorders. Behaviour Research and Therapy. 2013;51(8):434–442. doi: 10.1016/j.brat.2013.04.004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck depression inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory Manual. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Blanchard KA, Morgenstern J, Morgan TJ, Lobouvie EW, Bux DA. Assessing consequences of substance use: psychometric properties of the inventory of drug use consequences. Psychology of Addictive Behaviors. 2003;17(4):328–331. doi: 10.1037/0893-164X.17.4.328. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins J, Rothstein HR. Introduction to meta-analysis. Chichester, West Sussex, UK: Wiley; 2009. Converting among effect sizes. [Google Scholar]
- Bowen S, Chawla N, Marlatt GA. Mindfulness-based relapse prevention for addictive behaviors: A clinician's guide. Guilford Press; 2010. [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Marlatt A. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Substance Abuse. 2009;30(4):295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, Larimer ME. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders. JAMA Psychiatry. 2014;71(5):547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Bowen S, Smith JT, Marlatt GA, Potenza MN. Mindfulness-based treatments for co-occurring depression and substance use disorders: what can we learn from the brain? Addiction. 2010;105(10):1698–1706. doi: 10.1111/j.1360-0443.2009.02890.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C, Rounsaville BJ. Mindfulness training and stress reactivity in substance abuse: Results from a randomized, controlled stage I pilot study. Substance Abuse. 2009;30(4):306–317. doi: 10.1080/08897070903250241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins FS, Varmus H. A new initiative on precision medicine. New England Journal of Medicine. 2015;372(9):793–795. doi: 10.1056/NEJMp1500523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. Vol. 718. John Wiley & Sons; 2010. [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the national epidemiologic survey on alcohol and related conditions. The Journal of Clinical Psychiatry. 2006;67(2):247–257. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- Dodge R, Sindelar J, Sinha R. The role of depression symptoms in predicting drug abstinence in outpatient substance abuse treatment. Journal of Substance Abuse Treatment. 2005;28(2):189–196. doi: 10.1016/j.jsat.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Garland EL, Roberts-Lewis A, Tronnier CD, Graves R, Kelley K. Mindfulness-Oriented Recovery Enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: Proximal outcomes from a pragmatic randomized trial. Behaviour Research and Therapy. 2016;77:7–16. doi: 10.1016/j.brat.2015.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasner S, Mooney LJ, Ang A, Garneau HC, Hartwell E, Brecht ML, Rawson RA. Mindfulness-Based Relapse Prevention for Stimulant Dependent Adults: A Pilot Randomized Clinical Trial. Mindfulness. 2016:1–10. doi: 10.1007/s12671-016-0586-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Darke S, Griffiths P, Hando J, Powis B, Hall W, Strang J. The Severity of Dependence Scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction. 1995;90(5):607–614. doi: 10.1046/j.1360-0443.1995.9056072.x. [DOI] [PubMed] [Google Scholar]
- Grant BF. Comorbidity between DSM-IV drug use disorders and major depression: Results of a national survey of adults. Journal of Substance Abuse. 1995;7(4):481–497. doi: 10.1016/0899-3289(95)90017-9. [DOI] [PubMed] [Google Scholar]
- Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Archives of General Psychiatry. 2002;59(4):375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- Lanza ST, Rhoades BL. Latent class analysis: An alternative perspective on subgroup analysis in prevention and treatment. Prevention Science. 2013;14(2):157–168. doi: 10.1007/s11121-011-0201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- McKay JR, Pettinati HM, Morrison R, Feeley M, Mulvaney FD, Gallop R. Relation of depression diagnoses to 2-year outcomes in cocaine-dependent patients in a randomized continuing care study. Psychology of Addictive Behaviors. 2002;16(3):225–235. [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness. JAMA. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR, Forman R, Cacciola J, Kemp J. Reconsidering the evaluation of addiction treatment: from retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100(4):447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- Monti PM, Kadden RM, Cooney NL, Abrams DB. Treating alcohol dependence: A coping skills training guide. Guilford Press; 2002. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clinical Psychology Review. 2011;31(6):1032–1040. doi: 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Pistorello J, Fruzzetti AE, MacLane C, Gallop R, Iverson KM. Dialectical behavior therapy (DBT) applied to college students: a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2012;80(6):982–994. doi: 10.1037/a0029096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Robinson AH, Safer DL. Moderators of dialectical behavior therapy for binge eating disorder: results from a randomized controlled trial. International Journal of Eating Disorders. 2012;45(4):597–602. doi: 10.1002/eat.20932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Broome KM. A national 5-year follow-up of treatment outcomes for cocaine dependence. Archives Of General Psychiatry. 2002;59(6):538–544. doi: 10.1001/archpsyc.59.6.538. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Measuring alcohol consumption. New York: Humana Press; 1992. Timeline follow-back; pp. 41–72. [Google Scholar]
- Vujanovic AA, Meyer TD, Heads AM, Stotts AL, Villarreal YR, Schmitz JM. Cognitive-behavioral therapies for depression and substance use disorders: an overview of traditional, third-wave, and transdiagnostic approaches. The American Journal of Drug and Alcohol Abuse. 2016:1–14. doi: 10.1080/00952990.2016.1199697. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Burstein R. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Crane C, Barnhofer T, Brennan K, Duggan DS, Fennell MJ, Shah D. Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: a randomized dismantling trial. Journal of Consulting and Clinical Psychology. 2014;82(2):275–286. doi: 10.1037/a0035036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology. 2010;78(3):362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Harrop EN, Douglas H, Enkema M, Sedgwick C. Mindfulness-based treatment to prevent addictive behavior relapse: theoretical models and hypothesized mechanisms of change. Substance Use & Misuse. 2014;49(5):513–524. doi: 10.3109/10826084.2014.891845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. American Psychologist. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Falk DE, Kranzler HR, Litten RZ, Hallgren KA, O'malley SS, Anton RF. Methods to analyze treatment effects in the presence of missing data for a continuous heavy drinking outcome measure when participants drop out from treatment in alcohol clinical trials. Alcoholism: Clinical and Experimental Research. 2014;38(11):2826–2834. doi: 10.1111/acer.12543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Warner K, Sully B, Barricks A, Stauffer C, Thompson BL, Luoma JB. Randomized trial comparing mindfulness-based relapse prevention with relapse prevention for women offenders at a residential addiction treatment center. Substance Use & Misuse. 2014;49(5):536–546. doi: 10.3109/10826084.2013.856922. [DOI] [PubMed] [Google Scholar]
- Wolitzky-Taylor KB, Arch JJ, Rosenfield D, Craske MG. Moderators and non-specific predictors of treatment outcome for anxiety disorders: A comparison of cognitive behavioral therapy to acceptance and commitment therapy. Journal of Consulting and Clinical Psychology. 2012;80(5):786–799. doi: 10.1037/a0029418. [DOI] [PubMed] [Google Scholar]