Abstract
A randomized controlled trial comparing the efficacy of pyrantel-oxantel (10 mg/kg) with mebendazole (500 mg) was performed on 1329 schoolchildren aged 6-9 years on Pemba Island in September-October 2000 to evaluate alternative single-dose drugs for regular treatment of intestinal nematode infections. Both mebendazole and pyrantel-oxantel were very effective in eliminating Ascaris lumbricoides infection, inducing cure rates of more than 96% and reducing the mean egg counts by more than 95%. Both drugs had a moderate efficacy against Trichuris trichiura infection, but pyrantel-oxantel had a higher cure rate (31.5% vs. 23.3%, P < O.Ol), though the reductions in egg counts did not differ significantly and were more than 80%. Pyrantel-oxantel and mebendazole had a similar, poor efficacy in curing hookworm infections and had a moderate effect in reducing the egg counts by 67% and 68%, respectively. Pyrantel-oxantel (10 mg/kg) offers a valuable alternative to mebendazole as a single-dose treatment for the control of intestinal nematode infections in children in endemic areas of sub-Saharan Africa, due to its comparable efficacy, its low cost and its suitability for use in young children.
Keywords: helminths, Ascaris lumbricoides, Trichuris trichiura, hookworm, control, chemotherapy, pyrantel-oxantel, mebendazole, Pemba Island
Introduction
Four single-dose anthelminthic drugs, albendazole, levamisole, mebendazole, and pyrantel are available for the treatment of soil-transmitted helminth (STH) infections in chemotherapy-based control programmes. These drugs are recommended by the WHO and are included in the List of Essential Drugs (WHO, 1995,1996).
A number of research studies have been carried out under the auspices of the WHO to reassess the efficacy of single-dose-anthelminthic drugs and to evaluate the effectiveness of drug combinations with a view to their use in large-scale chemotherapy-based helminth control programmes. A safety component to monitor serious adverse events or side effects has been added in some trials. These studies included the co-administration of praziquantel and albendazole (OLDS et al., 1999), the comparative evaluation of mebendazole and albendazole (ALBONICO et al., 1994) and the assessment of levamisole and the co-administration of levamisole and mebendazole (ALBONICO et al., in press).
Ivermectin and albendazole have been assessed for the treatment of strongyloidiasis and intestinal nematode infections WARTI et al.. 1996). and the administration of ivermectin alone or in combination with albendazole for the control of lymphatic filariasis is presently under evaluation (HORTON et al., 2000; ISMAIL et al., 2001).
Pyrantel has been extensively studied in the past and results demonstrated a good efficacy against Ascaris lumbricoides and the hookworms, but poor efficacy against Trichuris trichiura (DESOWITZ et al., 1976; HSIEH & CHEN, 1973; ISMAIL et al., 1991; LONG Qi et al., 1992). However oxantel, another pyrimidine derivative, has been reported to show high efficacy against T. trichiura, a species relatively resistant to other drugs (ZAMAN & SABAPATY, 1975; GARCIA, 1976; RIM etal., 1976; PELDAN & PITIUNEN, 1982) and the combination of pyrantel and oxantel to have good efficacy against the STHs (LIM, 1978; ZAHEDI et al., 1980; APONTE et al., 1982). However, no randomized placebo-controlled clinical trial has been recently carried out to evaluate the efficacy of the combination pyrantel-oxantel, a drug combination which is used more frequently in Latin America and South-East Asia, and to compare its efficacy with other anthelminthics given individually.
The availability of a single-dose pyrantel-oxantel treatment would increase the choice of anthelminthic drugs for public health planners and managers and facilitate implementation of strategies designed to cope with the possible emergence of anthelminthic drug resistance (SAVIOLI et al., 1997). The reassessment of the efficacy of the pyrantel-oxantel combination, in particular for the treatment of trichuriasis, was one of the recommendations from a recent meeting on controlling disease due to STHs which was organized by the WHO and the Ministry of Health of Indonesia in Bali in February 2000 (CROMPTON & NESHEIM, in press). The pyrantel-oxantel combination is currently used in large-scale helminth control programmes in Indonesia with good results (SASONGKO et al., in press).
The present trial evaluated the efficacy of a single-dose of pyrantel-oxantel (10 mg/kg) as a tool for the control of intestinal nematode infections in children in an endemic area of sub-Saharan Africa. In this study, pyrantel-oxantel was compared with mebendazole (500 mg), which is the drug used for mass treatment of children and women of childbearing age in numerous helminth control programmes, worldwide (WHO,1996)
Materials and Methods
Study area and study population
The study was carried out on Pemba Island, the smaller of the 2 islands of Zanzibar, United Republic of Tanzania. Important features of the island have been described in detail elsewhere (ALBONICO et al., 1998). The study was conducted in September-October 2000 among children enrolled in the first grade (Standard 1; aged 6-7 years) and in the second grade (Standard 2; aged 8-9 years) of 7 public primary schools on Pemba Island. The schools were randomly selected from the 72 schools on the island. All children were included in the national helminth control programme and Standard 1 children had received 1 round of treatment with mebendazole 500 mg in March 2000. Standard 2 children had received 2 doses of mebendazole in 1999 and a third dose in March 2000. not have parental or guardian permission to participate; (ii) did not provide a stool sample; (iii) had significant co-morbidities (e.g. severe diarrhoea, severe anaemia, high fever); and (iv) had received anthelminthic treatment in the previous month.
Study design
The study was a randomized, placebo-controlled trial. Children enrolled in the study were randomly assigned to 1 of 3 treatment groups: (i) mebendazole 500 mg (Pharmamed, Zejtun, Malta); (ii) pyrantel-oxantel 10 mg/kg (Pfizer, Jakarta, Indonesia); and (iii) placebo. Pyrantel-oxantel was composed of pyrantel and oxantel in equal proportion, i.e. 150 mg of each drug in 1 tablet. Placebo pills resembled mebendazole in colour, size, taste, and shape. On the day prior to the scheduled treatment date, children eligible to participate in the trial were given a container in which to bring a fresh stool sample on the following day. On the day of treatment, their stools were collected, and their weight was measured and recorded. Randomization was blocked on weight and a computer-generated programme was used to create 3 randomized treatment lists, one for children weighing 15-20 kg receiving one tablet (150 mg) of pyrantel-oxantel, one for children weighing 21-30 kg receiving 2 tablets (300 mg) of pyrantel-oxantel, and one for children weighing 31-40 kg receiving 3 tablets (450 mg) of pyrantel-oxantel, according to the recommendations of the manufacturer. A single tablet of mebendazole and of placebo was given, irrespective of bodyweight. Treatments were placed in sealed, opaque envelopes and coded with a number. Children were identified solely by these numbers for the duration of the study.
Twenty-one days following treatment all children were revisited to collect a further stool sample. Any child who failed to bring a stool sample was followed up to 24 d. After both surveys stool samples were processed to assess egg counts within 6 h. All laboratory investigations were blinded, i.e. the technicians examining the slides were unaware of the treatment regimen of the patients.
Stools were analyzed using the Kate-Katz technique according to WHO guidelines (WHO. 1994) in order to assess prevalence &d intensity of helminth infection, indirectly measured as egg count.
Before enrolment in the study, parents or guardians of the children in the selected schools were met and a comprehensive explanation of the risk and benefits of the trial was given and verbal consent was sought. Parents and children were instructed to report to the teacher and refer to the nearest health centre any severe adverse effects occurring in the week after treatment.
After the completion of the study, children in the placebo group and children positive after the follow-up survey were treated with mebendazole 500 ma. The study- was approved by the Zanzibar Health Research Council. and bv the ethical committees of the WHO and of the London School of Hygiene and Tropical Medicine, UK.
Statistical analysis
Data were entered and analyzed using the Epi Info database package (CDC, Atlanta, GA, USA). Cure rates (CR) were calculated as the percentage of children with egg counts > 0 before treatment who become negative after treatment. The percentage reduction in prevalence was calculated as [(N+/n) -(N21+/n)] / (N+/n). where N+ is the number of positive children at baseline, N21+ is the number of positive children 21 d after treatment, and n is the total number of children with samples from both day 0 and day 21. Daily variation of egg excretion in each individual meant that some children who were egg-positive before treatment became negative at the follow-up, irrespective of treatment, and that some children who were negative in the first survey were found positive at the second survey. Cure rates could be biased by the daily variation of egg excretion because they included only children who were positive at baseline and who became negative at the follow-up. Both CRs and the percentage reduction in prevalence were calculated and presented in the Tables. Proportions were compared using standard x2 tests. Geometric mean egg counts were estimated as exp [(loge c + 1)/n] - 1, where c was the count (eggs per gram) for a particular individual and n the total number of samples. Geometric means were compared using analyses of variance (ANOVA) tests if Bartlett’s test of heterogeneity indicated homogeneity of variances, and by the Kruskal-Wallis test if Bartlett’s test was significant at the 5% level. The egg reduction rate (ERR) induced by treatment was estimated as 100 [1 − exp (-D)]%, where D was the mean difference for a particular treatment.
Results
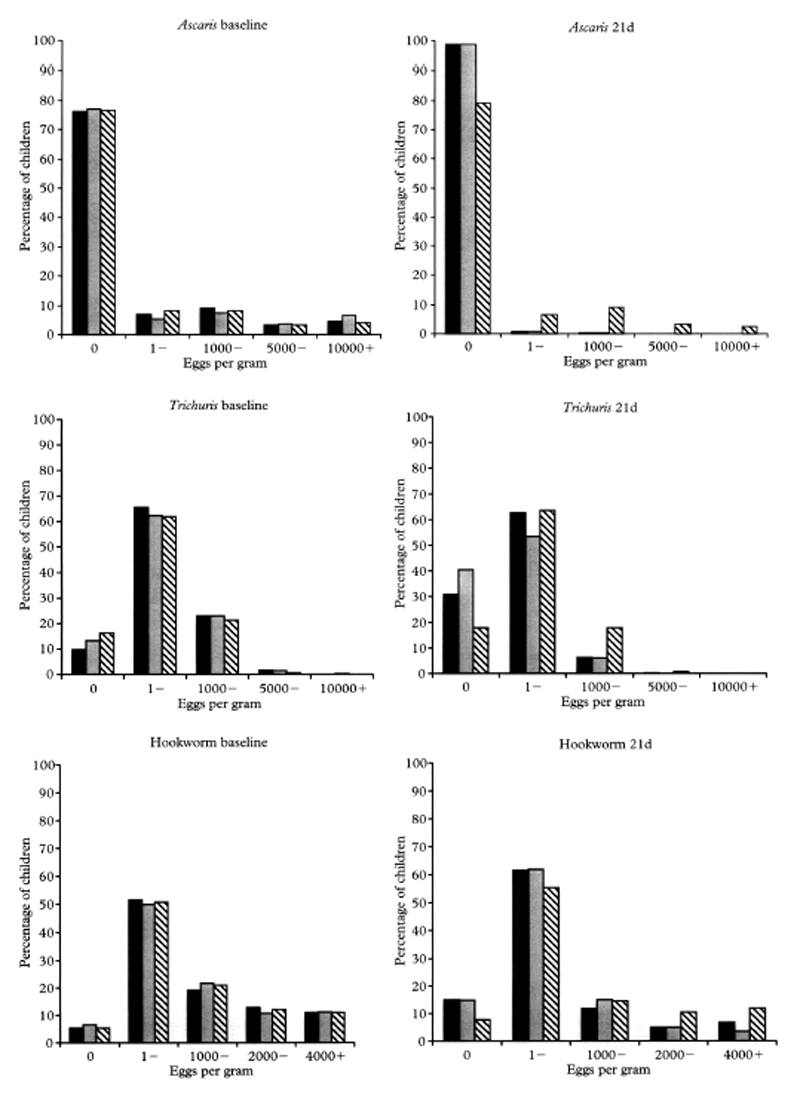
In September 2000, 1435 children brought a stool sample for the first examination. Of these, a second stool sample was collected from 1329 (92.6%) children between 20 and 23 d after treatment, with 95% of the samples collected 21 d after treatment. A second stool sample was not collected from 38 (8.5%) children treated with mebendazole, from 38 (8.6%) children treated with pyrantel-oxantel, or from 30 (6.8%) children treated with placebo. The children enrolled at both surveys were between 8 and 13 years of age (mean = 9.4) and 44.6% were boys (P< 0.05). Sex, age, prevalence of helminth infections, and geometric mean egg counts (before treatment) of the children who provided a post-treatment stool sample were compared with children who did not provide a second –stool sample (Table 1). The mean age did not differ between the -2 groups, ‘whereas a higher percentage of the enrolled children lost at follow-up were boys (55.7% vs. 44.6%; P= 0.03) and this difference was particularly evident in the mebendazole-treated group (P= 0.04). Prevalences and egg counts were not different in the 2 groups for T. trichiura or hookworms, but for A. lumbricoides children treated with mebendazole who did not return a second stool sample had higher prevalence (P = 0.0 1) and higher egg counts (P = 0.007). Analysis of the efficacy trial was done on the 1329 children who returned a stool sample at baseline and also at the follow-up survey. The groups of children receiving mebendazole, pyrantel-oxantel and placebo were homogeneous for sex, age, and for prevalence and intensity of helminth infections (Table 1). The Figure shows the distribution of egg counts at baseline and at 21 d after treatment for A. lumbricoides, T. trichiura and hookworm infections, respectively. Prevalences and mean egg counts before treatment and CRs and ERRS 21 d after treatment in the 3 treatment groups are reported in Table 2.
Table 1. Baseline characteristics of children who provided a post-treatment stool sample at follow up compared to those children who were lost at follow up.
| Number of children | Age (year) (mean ± SD) |
Sex (% boys) |
Ascaris
|
Trichuris
|
Hookworm |
||||
|---|---|---|---|---|---|---|---|---|---|
| Prevalencea | Egg countb | Prevalencea | Egg countb | Prevalencea | Egg countb | ||||
| Mebendazole | |||||||||
| Sample | 448 | 9·5 ± 1·9 | 46·4 | 23·9 | 5 | 90·2 | 257 | 94·6 | 588 |
| Lost at follow-up | 38 | 9·8 ± 2·1 | 63·2 | 42·1 | 29 | 94·7 | 329 | 92·1 | 745 |
| P | NS | 0·04 | 0·01 | 0·007 | NS | NS | NS | NS | |
| Pyrantel-oxantel | |||||||||
| Sample | 440 | 9·5 ±1·8 | 47·5 | 22·8 | 5 | 86·8 | 213 | 93·4 | 571 |
| Lost at follow-up | 38 | 9·4±1·9 | 52·6 | 23·7 | 5 | 86·8 | 252 | 94·7 | 777 |
| P | NS | NS | NS | NS | NS | NS | NS | NS | |
| Placebo | |||||||||
| Sample | 441 | 9·4 ± 1·5 | 39·9 | 23·4 | 5 | 83·7 | 163 | 94·6 | 573 |
| Lost at follow-up | 30 | 9·2 ± 1·4 | 50·0 | 23·3 | 4 | 90·0 | 200 | 93·3 | 571 |
| P | NS | NS | NS | NS | NS | NS | NS | NS | |
| Total | |||||||||
| Sample | 1329 | 9·4 ± 1·3 | 44·6 | 23·4 | 5 | 86·9 | 208 | 94·2 | 577 |
| Lost at follow-up | 106 | 9·5 ± 1·4 | 55·7 | 30·2 | 9 | 90·6 | 260 | 93·4 | 701 |
| P | NS | 0·03 | NS | NS | NS | NS | NS | NS | |
NS, Not Significant.
Percentage positive.
Eggs per gram expressed as geometric mean.
Table 2. Analysis of the efficacy of mebendazole, pyrantel–oxantel, and placcbo against soil-transmitted helminths in 1329 schoolchildren on Pemba Island, September–October 2000.
| Number of children | Day 0 |
Day 21 |
Cure rate | Percentage reduction in prevalence | P (day 0/21) | ERR (95% CI)c | P (day 0/21) | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Prevalencea | Egg countb | Prevalencea | Egg countb | |||||||
| Ascaris | ||||||||||
| Mebendazole | 448 | 23·9 | 5 | 1·1 | 0·1 | 98·0 | 95·4 | 0·001 | 96·1 (94·3–97·9) | 0·001 |
| Pyrantel–oxantel | 440 | 22·8 | 5 | 1·4 | 0·1 | 96·3 | 93·9 | 0·001 | 95·1 (92·3–97·9) | 0·001 |
| Placebo | 441 | 23·4 | 5 | 21·1 | 4 | 27·9 | 9·8 | NS | 18·1 (−2·7–34·8) | NS |
| Trichuris | ||||||||||
| Mebendazole | 448 | 90·2 | 257 | 69·2 | 41 | 25·2 | 23·3 | 0·001 | 83·6 (79·1–87·2) | 0·001 |
| Pyrantel–oxantel | 440 | 86·8 | 213 | 59·5 | 27 | 38·2d | 31·5d | 0·001 | 86·9 (82·2–90·3) | 0·001 |
| Placebo | 441 | 83·7 | 163 | 82·1 | 129 | 11·7 | 1·9 | NS | 21·2 (−0·6–38·2) | NS |
| Hookworm | ||||||||||
| Mebendazole | 448 | 94·6 | 588 | 85·0 | 193 | 13·2 | 10·1 | 0·001 | 67·0 (58·5–73·8) | 0·001 |
| Pyrantel–oxantel | 440 | 93·4 | 571 | 85·2 | 182 | 12·7 | 8·8 | 0·001 | 68·0 (59·2–74·8) | 0·001 |
| Placebo | 441 | 94·6 | 573 | 92·3 | 466 | 6·2 | 2·4 | NS | 18·6 (−0·4–34·0) | NS |
Percentage positive.
Eggs per gram expressed as geometric mean.
Egg reduction rate 95% confidence interval.
Different from mebendazole, P < 0·01.
The CRs, the reductions in prevalence, and the ERRS of the children treated with mebendazole and with pyrantel-oxantel were all significant (P < 0.001), and were significantly different from placebo at follow-up (P < 0.001).
Both mebendazole and pyrantel-oxantel were very effective in eliminating A. lumbricoides infection, producing CRs of more than 96% and reducing the mean egg counts by more than 95% (Table 2). As shown in the Figure all heavy and moderate infections and most of the light infections were cleared after treatment with either-drug. Both drugs had a moderate efficacy against T. trichiura infection, but pyrantel-oxantel had a higher CR (P < 0.0 l), though the reduction in egg count did not differ significantly and was more than 80% for both drugs (Table 2). The Figure shows a comparable reduction of heavy and moderate infections, while light infections were cured more effectively by pyrantel-oxantel. Both mebendazole and pyrantel-oxantel had poor efficacy in curing hookworm infections, though pyrantel-oxantel was more effective in reducing heavy infections (Figure). Both drugs likewise had moderate effects in reducing egg counts, by 67% and 68%, respectively (Table 2). No adverse events were reported after any of the treatments.
Figure. Distribution of A. lumbricoides, T. trichiura and hookworms egg count before and 21 d after treatment with mebendazole, pyrantel oxantel and placebo.
Discussion
This trial was the first randomized, placebo controlled study comparing the efficacy of single dose pyrantel-oxantel (10 mg/kg) with mebendazole (500 mg). In addition, the study was carried out in sub-Saharan Africa, where intestinal helminths are common and where pyrantel-oxantel has rarely, if ever, been used for control of intestinal nematode infections. This trial has confirmed the findings of previous studies that both mebendazole (ABADI, 1985; ISMAIL et al., 1991; ALBONICO et al., 1994) and pyrantel-oxantel (RIM et al., 1975; DISSANAIKE, 1978; LIM, 1978) are highly effective single-dose treatments for A. lumbricoides infection, with mean egg counts after treatment being reduced by more than 95%.
Pyrantel-oxantel achieved a CR of only 38% for T. trichiura infection, considerably lower than the majority of results obtained in previous trials using the same dosage of 10 mg/kg (RIM et al., 1975; CHO, 1976 LIM. 1978). Only a few previous studies have reported a similarly low CR (DISSANAIKE, 1978; SINNIAH & SINNIAH, 1981). This may be explained bv the lower mean egg counts pretreatment which were reported in studies in which CRs of between 70% and 90% were achieved, and/or by different drug sensitivities of T. trichiura strains. It is noteworthy that all previous studies were carried out in Asia and that, for T. trichiura, sensitivity to ivermectin has been shown to be highly dependent on geographical location (MARTI et al., 1996). Cure rates with mebendazole were lower than those obtained with pyrantel-oxantel, though higher than CRs reported in a previous study from Pemba Island (ALBONICO et al., 1994). A lower mean egg count pretreatment may account for the higher CR reported in the present study, as it has been shown that light infections are more likely to be cured with benzimidazoles than heavy infections (PENE et al., 1981; ROSSIGNOL & MAISSONNEUVE, 1983). Both drugs were similarly effective in reducing mean egg counts by more than 80%; pyrantel-oxantel showed a better, though not significantly greater effect. The 87% reduction of T. trichiura mean egg count seen after pyrantel-oxantel treatment is consistent with previous studies (RIM et al., 1976; DISSANAIKE, 1978; LIM, 1978). This comparable effect on intensity supports the suggestion that the higher CRs reported in the earlier studies is explained by lower pretreatment intensities. Previous direct comparisons with mebendazole suggested that pyrantel-oxantel was more effective against T. trichiura infection, although in those studies both the drugs were given in multiple doses. Thus, mebendazole given at 100 mg twice a day for 3 d was compared with pyrantel-oxantel given at 10 mg/kg daily for 3 d (SINNIAH & SINNIAH, 1981), or with pyrantel-oxantel given at 15-20 mg/kg daily for 2 (LEE & LIM, 1978) or for 3 consecutive days (DISSANAIKE, 1978).
Cure rates for hookworm infections were poor and ERRS were only moderate for both drugs. Pyrantel-oxantel has generally been reported to have a higher efficacy than this against hookworms (RIM et al.. 1975: CHO, i976; LIM, r978), though low/moderate efficacy has been reported by some other authors (DISSANAIKE, 1978; SINNIAH & SINNIAH, 1981). The present data on mebendazole efficacy against hookworm infection are similar to those of another comparable study recently carried out on Pemba Island (ALBONICO et al., in press), though both CR and ERR were significantly lower than those reported in an efficacy trial carried out before the beginning of periodic chemotherapy in this population (ALBONICO et al.. 1994). The possibility that this apparent reduction in mebendazole efficacy & due to emerging benzimidazole drug resistance means that the validation of pyrantel-oxantel as another broad spectrum, effective drug given as a single-dose may prove valuable in the development of strategies to delay the occurrence of anthelminthic drug- resistance (RAVIOLI et al.. 1997). It would be advisable to repeat this efficacy trial in an area with high worm burden-and with less drug exposure, and to evaluate also the effect of both pyrantel-oxantel and mebendazole given in combination.
The results of this trial have significant implications for the use of targeted chemotherapy at the community and at school level for the control of STHs. Pyrantel-oxantel has been shown to have comparable efficacy to mebendazole (500 mg) in treating STHs, and to have a better efficacy in curing T. trichiura infections. Pyrantel-oxantel is available in Indonesia for targeted treatment of schoolchildren at a cost of only few US cents per tablet (A. Sasongko, personal communication) and competes with the very low cost of mebendazole as a generic product (ALBONICO et al., 1994). A possible disadvantage of pyrantel-oxantel *is that patients need to be weighed, though the producing company does give alternative indications to treat based on weight and/or age. Furthermore, pyrantel-oxantel is not contraindicated in young children, and prescribing information indicates administration of 1 tablet of 150 mg to children between 6 months and 2 years. Pyrantel-oxantel is also available as a suspension containing 20 mg of each base drug (pyrantel pamoate and oxantel pamoate) per mL.
Further research is needed to better refine the spectrum of efficacy of pyrantel-oxantel against ST& in sub-Saharan Africa. For example, implementation of studies in areas of low endemic&, evaluation of the efficacy of pyrantel-oxantel at the -higher dosages (15-20 ma/kg) shown in Asia to be more effective (CABRER.& al., 1980), and assessment of combined treatment with pyrantel-oxantel and other single-dose anthelminthics, are some suggestions for work needed for scaling-up the use of pyrantel-oxantel in large-scale helminth control programmes.
Acknowledgements
Special thanks to Professor Peter Smith for his precious advice on statistical analysis, and to Victoria Wright for her contribution to the field activities, as well as the revision of the manuscript. We are grateful to the staff of the Parasitology Department of the Public Health Laboratory Ivo de Carneri on Pemba Island whose dedication and enthusiasm made this study possible. We acknowledge the donation of placebo and mebendazole by Pharmamed (Malta), and of pyrantel-oxantel by Pfizer (Indonesia). This study was generously supported by the Parasitic and Vector Control, Division of Communicable Diseases, World Health Organization.
References
- Abadi K. Single dose mebendazole therapy for soil transmitted nematodes. American Journal of Tropical Medicine and Hygiene. 1985;34:129–133. doi: 10.4269/ajtmh.1985.34.129. [DOI] [PubMed] [Google Scholar]
- Albonico M, Smith I’G, Hall A, Chwaya HM, Alawi IS, Savioli L. A randomized controlled trial comparing mebendazole and albendazole against Ascaris, Trichuris and hookworm infections. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1994;88:585–589. doi: 10.1016/0035-9203(94)90174-0. [DOI] [PubMed] [Google Scholar]
- Albonico M, Stoltzfus RJ, Tielsch JM, Chwaya HM, Ercole E, Cancrini G. Epidemiological evidence of a differential effect of hookworm species, Ancylostoma duodenale and Necator americanus, on iron status of children. International Journal of Epidemiology. 1998;27:530–537. doi: 10.1093/ije/27.3.530. [DOI] [PubMed] [Google Scholar]
- Albonico M, Bickle Q, Ramsan M, Montresor A, Savioli L, Taylor M. Efficacy of mebendazole and levamisole alone or in combination against intestinal nematode infections following repeated targeted mebendazole treatment in Zanzibar. Bulletin of the World Health Organization. (in press) [PMC free article] [PubMed] [Google Scholar]
- Aponte A, Alvarez N, Perez de Suarez E, Blanco de Davila D, Gomez de Rodriguez G, Romer H. Massive trichocephaliasis and other helminthiasis in children and its treatment with pyrantel pamoate/oxantel. Revista de la Sociedad Venezuelana de Gastroenterologia. 1982;36:162–176. [PubMed] [Google Scholar]
- Cabrera BD, Valdez EV, Go TG. Clinical trials of broad spectrum anthelmintics against soil-transmitted helminthiasis. Southeast Asian Journal of Tropical Medicine and Public Health. 1980;11:502–506. [PubMed] [Google Scholar]
- Cho SY. Anthelmintic efficacy of combined preparation of pyrantel pamoate and oxantel pamoate on human intestinal nematodes. Korean Journal of Pharmacology. 1976;12:69–73. [Google Scholar]
- Crompton DWT, Nesheim MC, editors. Controlling Disease due to Soil-Transmitted Helminths. Geneva: World Health Organization; (in press) [Google Scholar]
- Desowitz RS, Bell T, Williams J, Cardines R, Tamarua M. Anthelmintic activity of pyrantel pamoate. American Journal of Tropical Medicine and Hygiene. 1970;19:775–778. doi: 10.4269/ajtmh.1970.19.775. [DOI] [PubMed] [Google Scholar]
- Dissanaike AS. A comparative trial of oxantel-pyrantel and mebendazole in multiple helminth infection in school-children. Drugs. 1978;15(supplement 1):73–77. doi: 10.2165/00003495-197800151-00015. [DOI] [PubMed] [Google Scholar]
- Garcia EG. Treatment for trichuriasis with oxantel. American Journal of Tropical Medicine and Hygiene. 1976;25:914–915. doi: 10.4269/ajtmh.1976.25.914. [DOI] [PubMed] [Google Scholar]
- Horton J, Witt C, Ottesen EA, Lazdins JK, Addiss DG, Awadzi K, Beach MJ, Belizario VY, Dunyo SK, Espinel M, Gyapong JO, et al. An analysis of the safety of the single dose, two drug regimens used in programmes to eliminate lymphatic filariasis. Parasitology. 2000;121(supplement):S147–S160. doi: 10.1017/s0031182000007423. [DOI] [PubMed] [Google Scholar]
- Hsieh HC, Chen ER. Treatment of Ascaris, hookworm and Trichuris infections with a single dose of pyrantel pamoate (Combantrin) Southeast Asian Journal of Tropical Medicine and Public Health. 1973;4:407–412. [PubMed] [Google Scholar]
- Ismail MM, Premaratne UN, Suraweera MGW. Comparative efficacy of single dose anthelmintics in relation to intensity of geohelminth infections. Ceylon Medical Journal. 1991;36:162–167. [PubMed] [Google Scholar]
- Ismail MM, Tavakody RL, Weil GJ, Fernando D, De Silva MSG, De Silva GAC, Balasooriya WK. Long-term efficacy of single-dose combinations of albendazole, ivermectin and diethylcarbamazine for the treatment of bancroftian filariasis. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2001;95:332–335. doi: 10.1016/s0035-9203(01)90257-3. [DOI] [PubMed] [Google Scholar]
- Lee SH, Lim JK. A comparative study of the effect of oxantel-pyrantel suspension and mebendazole in mixed infection with Ascaris and Trichuris. Drugs. 1978;15(Supplement 1):95–98. doi: 10.2165/00003495-197800151-00018. [DOI] [PubMed] [Google Scholar]
- Lim JK. Anthelmintic effect of oxantel and oxantel pyrantel in intestinal nematode infections. Drugs. 1978;15(supplement 1):37–41. doi: 10.2165/00003495-197800151-00019. [DOI] [PubMed] [Google Scholar]
- Long Qi X, Ze-Xiao J, Sen-Hai Y, Xiao-Ming D, Xin-Hua B, Hui-Fang Y, Hai-Qing Z, Cheng-Song K, Qing-Wei C, Chang-Hai Z, Ying F, et al. Treatment of soil-transmitted helminth infections by anthelminthics in current use. Chinese Journal of Parasitology and Parasitic Diseases. 1992;10:95–99. [Chinese with abstract in English.] [PubMed] [Google Scholar]
- Marti H, Haji HJ, Savioli L, Chwaya HM, Mgeni AF, Ameir JS, Hatz C. A comparative trial of a single-dose ivermectin versus three days of albendazole for treatment of Strongyloides stercoralis and other soil-transmitted helminth infections in children. American Journal of Tropical Medicine and Hygiene. 1996;55:477–481. doi: 10.4269/ajtmh.1996.55.477. [DOI] [PubMed] [Google Scholar]
- Olds GR, King C, Hewlett J, Olveda R, Wu G, Ouma J, Peters I’, McGarvey S, Odhiambo O, Koech D, Liu CY, et al. Double-blind placebo-controlled study of concurrent administration of albendazole and praziquantel in schoolchildren with schistosomiasis and geohelminths. Journal of Infectious Diseases. 1999;179:996–1003. doi: 10.1086/314686. [DOI] [PubMed] [Google Scholar]
- Peldan K, Pitkanen T. Treatment of Trichuris trichiura infection with a single dose of oxantel pamoate. Scandinavian journal of Infectious Diseases. 1982;14:297–299. doi: 10.3109/inf.1982.14.issue-4.10. [DOI] [PubMed] [Google Scholar]
- Pene P, Vincentelli JM, Soula G, Bourderioux C, Rossignol JF. Le zentel (albendazole) dans le traitement des nematodes intestinales. Etude multicentrique en Afrique de l’Ouest. Medecine d’Afrique Noire. 1981;28:483–48s. [Google Scholar]
- Rim HJ, Won CY, Lee SL, Lim JK. Anthelmintic effect of oxantel pamoate and pyrantel pamoate suspension against intestinal nematode infestations. Korean Journal of Parasitology. 1975;13:97–101. doi: 10.3347/kjp.1975.13.2.97. [DOI] [PubMed] [Google Scholar]
- Rim HJ, Chang YS, Ha JH, Lim JK. Anthelmintic effect of oxantel pamoate (CP-14, 445) against trichuriasis. Korean University Medical Journal. 1976;13:205–211. [Google Scholar]
- Rossignol JF, Maissonneuve H. Albendazole: placebo-controlled study in 870 patients with intestinal helminthiasis. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1983;77:707–711. doi: 10.1016/0035-9203(83)90211-0. [DOI] [PubMed] [Google Scholar]
- Sasongko A, Lubis F, Mahaswiati M, Ramawulan D. Practical experience from the primary school based soil-transmitted helminth control program in Jakarta 1987-1999. In: Crompton DWT, Nesheim MC, editors. Controlling Disease due to Soil-Transmitted Helminths. World Health Organization; Geneva: (in press) [Google Scholar]
- Savioli L, Montresor A, Bundy DAP, Albonico M, Renganathan E. Anthelminthic resistance in human helminths: learning from the problem with worm control in livestock-reply. Parasitology Today. 1997;13:156. doi: 10.1016/s0169-4758(97)01024-7. [DOI] [PubMed] [Google Scholar]
- Sinniah B, Sinniah D. The anthelmintic effects of pyrantel pamoate, oxantel-pyrantel pamoate, levamisole and mebendazole in the treatment of intestinal nematodes. Annals of Tropical Medicine and Parasitology. 1981;75:315–321. doi: 10.1080/00034983.1981.11687445. [DOI] [PubMed] [Google Scholar]
- WHO. bench Aids for the Diagnosis of Intestinal Parasites. World Health Organization; Geneva: 1994. [Google Scholar]
- WHO. WHO Model Prescribing Information. Drugs Used in Parasitic Diseases, 2nd edition. World –Health Organization; Geneva: 1995. [Google Scholar]
- WHO. Report of the WHO informal consultation on the use of chemotherapy for the control of morbidity due to soil transmitted nematodes in humans. Geneva 29 April to I May 1996. World Health Organization, Division of Control of Tropical Diseases; Geneva: 1996. WHO/CTD/SIP.96.2. [Google Scholar]
- Zahedi M, Oothuman P, Sabapathy NN, Bakar NA. Intestinal nematode infections and efficacy study of oxantel-pyrantel pamoate among plantation workers. Medical ‘journal of Malaysia. 1980;XXXV(1):31–37. [PubMed] [Google Scholar]
- Zaman V, Sabapaty ‘NNN. Clinical trial with a new anti-trichuris drug? trans-1,4,5,6 tetrahydro-2(3- hydroxystryl)-l-methyl pyrimidine (CP-14,445) Southeast Asian 3oumal of Tropical Medicine and Public Health. 1975;6:103–105. [PubMed] [Google Scholar]