Abstract
Objective
To identify risk profiles associated with patterns of problematic cannabis use in early adulthood.
Method
Data came from 1,229 participants in the Great Smoky Mountains Study, a prospective 20-year cohort study from 1993–2015 that is representative of western North Carolina with yearly assessments conducted from ages 9 to 16, and assessments at ages 19, 21, 26, and 30. Patterns of problematic cannabis use (i.e., DSM-5 cannabis use disorder or daily use) in early adulthood included 1) non-problematic use in late-adolescence (ages 19–21) and early adulthood (ages 26–30); 2) limited problematic use in late adolescence only; 3) persistent problematic use in late adolescence and early adulthood; and 4) delayed problematic use in early adulthood only. Multi-nominal logistic regression models examined pairwise associations between these patterns and risk factors in childhood (ages 9–16) and late adolescence (ages 19–21). Risk factors included psychiatric disorders (e.g., anxiety, depressive), other substance use (smoking, alcohol, illicit drugs), and challenging social factors (e.g., low socioeconomic status, family functioning, peers). Sex and race/ethnicity (white, black, American Indian) interactions were tested.
Results
The persistent pattern (6.7% of sample) was characterized by more anxiety disorders across development and more DSM-5 CUD symptoms during late adolescence compared to the limited pattern (13.3%), which, in turn, had more childhood family instability and dysfunction. The delayed pattern (3.7%) was characterized by more externalizing disorders, maltreatment, and peer bullying in childhood compared to non-problematic users. There were no significant sex/race interactions.
Conclusion
Problematic cannabis use patterns during early adulthood have distinctive risk profiles, which may be useful in tailoring targeted interventions.
Keywords: cannabis use disorder, risk factors, adolescence, early adulthood, epidemiology
INTRODUCTION
The prevalence of cannabis use in the US is high, with approximately 70% of the population reporting use by age 30.1, 2 Among active users, 18–30% report problematic cannabis use, characterized by cannabis use disorder (CUD) or daily use.3 Such problematic use peaks at ages 19–21 and subsequently decreases or plateaus,4 and is associated with long-term health and social consequences, including higher risk for altered brain development,5 psychosis and exacerbated symptoms of schizophrenia,6 escalation to harsher drug use,7 and lower educational attainment and employment.8 Substantial progress has been made in identifying risk factors for substance use in the early life course. For problematic cannabis use specifically, the literature points to psychiatric disorders,9 other substance use,10, 11 and challenging economic and social circumstances.12–14 Yet our current understanding of antecedents and correlates of problematic cannabis use in early adulthood is far from complete due, in part, to the heterogeneous developmental patterns of problematic use.
Comparing the existing evidence across studies is difficult because developmental patterns of problematic use can be defined based on the onset, offset, or intensity of cannabis use.15, 16 The most commonly identified developmental patterns include 1) non-problematic use across adolescence and adulthood, 2) problematic use that is limited to adolescence, and 3) problematic use that persists throughout adolescence and adulthood. Finally, there is also growing evidence of a delayed problematic use group that begins in adulthood after the typical peak of cannabis use in the late teens/early twenties.14, 15, 17 Although the number of delayed users is likely to increase in the coming years following cannabis legalization,18 very little is known about this group. To optimize preventions and interventions, it is important to pinpoint the risk profiles that precede and accompany these heterogeneous patterns of problematic cannabis use patterns in early adulthood.
Additional gaps in the literature on problematic cannabis use during early adulthood remain. First, the majority of studies examine cannabis use patterns across adolescence or the college years only, omitting early adulthood, which extends into the thirties. Second, research typically compares problematic cannabis use patterns to patterns of no/low use, but seldom to variations of problematic use. Yet these latter comparisons would be most informative for tailored preventions/interventions. Third, much of the evidence to date does not incorporate the cannabis use disorder (CUD) criteria of the DSM-5.19 Lastly, interactions of race/ethnicity and sex with risk factors across different developmental patterns of problematic cannabis use are poorly understood.20
The current study addresses these gaps using a large, diverse, 20-year cohort that was most recently assessed in 2015. The main objective is to identify how childhood (ages 9–16) and late-adolescent (ages 19–21) risk profiles differ across problematic cannabis use patterns that occur from late adolescence (ages 19–21) until early adulthood (ages 26–30). A secondary objective is to test potential race/ethnicity and sex differences in risk factors for developmental patterns of problematic cannabis use in early adulthood given known race/ethnic and sex differences in terms of age of onset of cannabis use, frequency of use, CUD, and desistance.21, 22 In doing so, we are able to contribute to the growing literature on the development of cannabis use among American Indians.23, 24 Altogether, this work builds on our previous study that examined differences by race/ethnicity and sex for point prevalence of cannabis use, frequencies, and DSM-5 CUD from 9–30 years of age.3
METHOD
Participants
The Great Smoky Mountains Study is a prospective, longitudinal study of the development of psychiatric disorders and need for mental health services among rural and urban youth. A community-representative sample of 1,420 participants was recruited from 11 counties in western North Carolina in 1993, using a household equal probability, accelerated cohort design for three cohorts of children aged 9, 11, and 13 at intake. The study oversampled American Indians, who represented 3% of the community population, but make up nearly a quarter of the study sample (n=350). To ensure that the results were not biased by the oversampling procedure, all enrolled participants were assigned a sampling weight inversely proportional to their probability of selection. More details on recruitment and data collection are published elsewhere.25 Briefly, 80% of those recruited chose to participate at intake. Thereafter, 82.1% of all possible interviews were completed up to age 30 (74%–94% at any particular wave). The maximum possible number of interviews per participant is 11 (youngest cohort of 9 years old at intake), 10 (middle cohort), and 8 (oldest cohort). The mean number of interviews to date is 7.7 (SD 2.3).
The final analytical sample for the present study consists of 1,229 participants who had relevant data on patterns of cannabis use at ages 19–21 and 26–30. Among these individuals, 134 had missing observations on late-adolescent risk factors (ages 19–21), resulting in 1,095 respondents with complete data. Participants with missing data on late adolescent risk factors were more likely to be male (p<.001) and less likely to have ever used cannabis by age 16 (p<.05), compared to the full analytical sample. There were no differences by race/ethnicity.
Procedures
Before the study began, both the child participant and a parent (83% biological mother) signed informed consent forms. Each respondent received an honorarium for participation. Interviews were conducted separately for both respondents on an annual basis until the participant was 16 years old. Going forward, only the participant was interviewed at ages 19, 21, 26, and 30. The study was approved by the Duke University Medical Center Institutional Review Board.
Assessment
All variables—except criminal offenses and the neglect portion of the maltreatment variable—were assessed using the Child and Adolescent Psychiatric Assessment (CAPA) self- and parent-reports until age 16 and the Young Adult Psychiatric Assessment (YAPA) self-reports thereafter at ages 19, 21, 26, and 30.26, 27 The reference period for all variables was within the past three months immediately preceding the interview to increase the accuracy of the recall. For symptoms of psychiatric disorders and high-risk behaviors such as substance use,28 the reliability of a three-month reference period has been shown to be an improvement over longer (e.g., past six months or past year) recall time frames because estimates using this reference period are less likely to be biased by forgetting or to show inconsistencies in details related to the onset, duration, and intensity of the experiences.29 The structured interviews were coded by trained interviewers; each interview was then checked by a supervisor. Scoring programs, written in SAS by the senior authors, combined information about the date of onset, duration, and intensity of each symptom to contribute to diagnoses according to DSM criteria. Two-week test-retest reliability of endorsed diagnoses is comparable to that of other highly-structured psychiatric interviews.30
Cannabis Involvement
The substance use module of the YAPA assesses cannabis use at ages 19, 21, 26, and 30 according to age of onset, frequency of use, symptoms of DSM-5 CUD, and maladaptive behaviors such as the use of cannabis to improve mood, disinhibited cannabis use, cannabis use first thing in the morning, blackouts, and cannabis-related criminality. For this study, problematic cannabis was defined as either daily cannabis use or meeting full criteria for DSM-5 CUD. Although highly correlated, these constructs are not synonymous (see also our previous publication detailing the point prevalence of CUD and daily use from ages 9 to 30 years).3 Specifically, among the total 415 reports of CUD observed in the weighted sample over the course of the study, 72.1% of the observations coincided with an account of daily use. Conversely, only 57.4% of daily use reports (n=382) overlapped with CUD endorsement. Endorsement of DSM-5 CUD diagnostic criteria required presentation of at least two of 11 symptoms, all of which were routinely collected since study inception in 1993 in the CAPA and later in YAPA prior to DSM-5 updates in 2013. These included: overconsumption, attempts to cut back, excessive time spent acquiring or using, craving, failure to fulfill major roles or obligations, continued use causing problems for interpersonal relationships, reduction in other activities, use in physically hazardous situations (e.g., driving intoxicated), continued use despite observed physical or psychological consequences, increased tolerance, and withdrawal due to cessation.19
Risk Factors
We measured dichotomized variables (0=no, 1=yes) for psychiatric disorders, other substance use, and challenging economic and social circumstances aggregated across ages 9 to 16 in childhood and across ages 19 and 21 in late adolescence. Psychiatric disorders consisted of anxiety disorders, depressive disorders, attention-deficit/hyperactive disorder (ADHD), oppositional defiant disorder (ODD), conduct disorder (CD), suicidality, and comorbidity. Other substance use captured tobacco use, alcohol use, and other illicit drug use. Economic and social challenges were measured by low socioeconomic status, family dysfunction, family instability, caregiver child maltreatment, delinquent or age-inappropriate friends, bullying victimization, and school expulsion in childhood. In late adolescence, economic and social challenges were assessed as material hardship, young parenthood of two or more children, majority of friends being substance users, low educational attainment, and involvement in moderate/violent crime. Detailed descriptions of all variables are provided in the Supplement 1, available online.
Analyses
Problematic cannabis use patterns in early adulthood were selected a priori based on daily use or meeting criteria for DSM-5 CUD diagnosis during four assessments of cannabis use at 19, 21, 26, and 30 years. Problematic use in late adolescence was endorsed if the respondent had an affirmative status at either 19 or 21 years; problematic use in early adulthood was endorsed if the respondent had an affirmative status at either 26 or 30 years. The resulting problematic use patterns consisted of 1) non-problematic use (NP) in late adolescence and early adulthood, which includes non-users and cannabis users who do not meet our definition of problematic use; 2) limited problematic use (LP) in late adolescence only, 3) persistent problematic use (PP) in late adolescence and early adulthood; and 4) delayed problematic use (DP) in early adulthood only. We assessed the potential for misclassification in early adulthood due to the three-month reference periods in late adolescence/early adulthood by comparing assignments generated using available data from ages 9–21 for lifetime history reports of daily cannabis use and cumulative reports of ever reporting any DSM symptoms of CUD based on three-month recall.
Pairwise comparisons evaluated the relative risk ratios (RRR) of risk factors between all patterns. Adjusted models took into account sex and race/ethnicity. Subsequently, interaction models tested whether the effects of risk factors in the prediction of developmental patterns differed by sex or by race/ethnicity. Race/ethnicity was categorized as non-Hispanic white (reference group), black, and American Indian. Associations were investigated using weighted, multinomial, or binominal logistic regression models that included sampling weights and robust variance estimates to account for the sampling design. Therefore, the reported parameters are representative of the western North Carolina community from which the sample was drawn. For all analyses, two-tailed significance tests were conducted using STATA v1431: p values less than .05 indicated significant results.
RESULTS
Patterns of Problematic Cannabis Use
There was no evidence of misclassification of participants’ problematic cannabis use patterns at 19–21 years. Reports from the three-month recall interviews generated the same assignments as those made from the lifetime history reports of ever using cannabis daily or ever endorsing any symptom of CUD from the ages of 9–21. Based on cumulative reports of ever endorsing any CUD symptoms, five participants with non-problematic cannabis use patterns in early adulthood required further evaluation. Three initiated cannabis use between the ages of 13–14 and ceased by age 16. One had intermittent cannabis use at ages 14, 15, and 20 while another started use at 19 and then stopped; neither of these individuals reported ever using daily or ever having two or more symptoms of CUD between 19 and 21 years of age.
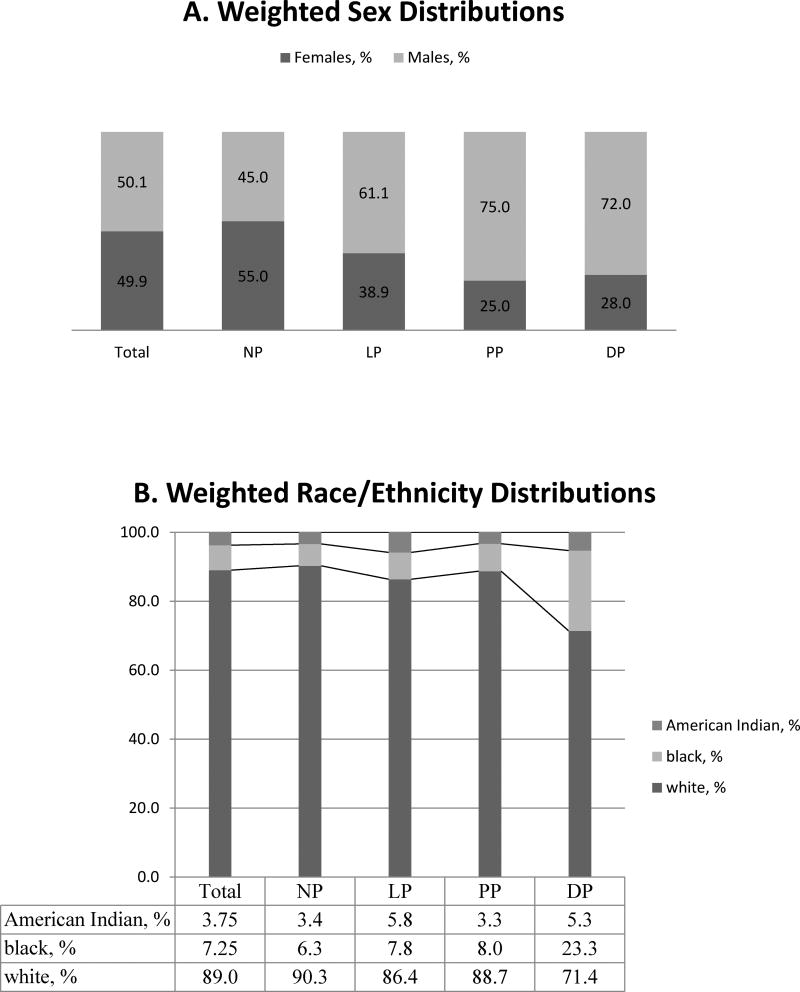
The non-problematic cannabis use pattern was the most common (n=884; 76.3%), followed by limited (n = 200; 13.3%), persistent (n=84; 6.7%), and delayed (n=61; 3.7%) problematic use patterns. Sex and race/ethnicity distributions differed across patterns (see figures 1a–b). More males than females had limited (RRR [CI95] = 1.9 [1.1–3.4], p<.05), persistent (3.7 [1.5–8.7], p<.01), and delayed patterns (3.1 [1.2–8.5], p<.05) as opposed to the non-problematic pattern. Those with limited versus non-problematic use patterns were nearly twice as likely to be American Indian as white (1.8 [1.2–2.7], p<.01). Users with a delayed pattern compared to those with the non-problematic pattern were approximately five times more likely to be black than white participants (4.7 [1.3–16.5], p<.05).
Figure 1.
Weighted sex and race/ethnicity distributions among non-problematic (NP), limited problematic (LP), persistent problematic (PP), and delayed problematic (DP) cannabis use.
Risk Factors for Problematic Cannabis Use
Psychiatric disorders, other substance use, and economic/social challenges were examined for each problematic use pattern as childhood antecedents and late-adolescent correlates. The total number of observed significant tests was six to eight times higher than would be expected by chance alone at an alpha level of 0.05 for childhood risk factors (32 observed: 5 expected) and late-adolescent risk factors (34 observed: 4 expected), suggesting most findings are not due to chance.
Childhood antecedents (ages 9–16)
Table 1 shows the frequencies, unweighted N, and significance of childhood risk factors for problematic cannabis use patterns. Table S1, available online, provides the corresponding adjusted RRR and 95% CIs. Those with non-problematic patterns generally had the lowest rates of psychiatric disorders, other substance use, and economic/social challenges. In contrast, those with persistent patterns often had the highest rates, especially for anxiety and depressive disorders; early smoking and other illicit drug use; and school expulsion. Individuals with limited and delayed patterns also had elevated levels of risks compared to those with non-problematic use. Limited patterns coincided with higher rates of CD, comorbidity, all types of other substance use, family instability, family dysfunction, school expulsion, and delinquent/older peers compared to those with non-problematic patterns. Those with delayed patterns had higher rates of ODD, CD, comorbidity, early tobacco use, and victimization due to caregiver maltreatment and peer bullying than those with non-problematic patterns.
Table 1.
Childhood Risk Factors (Ages 9–16) and Early-Adulthood Problematic Cannabis Use Patterns (n=1,229)
| Non- Problematic n=884 |
Limited Problematic n=200 |
Persistent Problematic n=84 |
Delayed Problematic n=61 |
Significance of Pairwise Comparisonsa |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Psychiatric risk factors | NP, % (N) | LP, % (N) | PP, % (N) | DP,% (N) | LP NP |
PP NP |
DP NP |
PP LP |
LP DP |
PP DP |
| Anxiety disorders | 9.6 (117) | 10.1 (28) | 26.5 (19) | 7.5 (9) | NS | ** | NS | * | NS | * |
| Depressive disorders | 6.9 (70) | 10.2 (28) | 20.9 (18) | 11.5 (12) | NS | ** | NS | NS | NS | NS |
| ODD | 8.2 (119) | 13.2 (51) | 21.3 (25) | 24.7 (18) | NS | * | ** | NS | NS | NS |
| Conduct Disorder | 4.7 (74) | 20.3 (55) | 20.1 (25) | 24.5 (10) | *** | ** | ** | NS | NS | NS |
| ADHD | 2.9 (43) | 5.6 (13) | 3.3 (6) | 6.9 (7) | NS | NS | NS | NS | NS | NS |
| Suicidality | 14.1 (125) | 19.5 (39) | 16.7 (14) | 26.2 (16) | NS | NS | NS | NS | NS | NS |
| Comorbidity: 2 or more | 7.8 (107) | 16.3 (15) | 22.4 (55) | 22.4 (27) | * | ** | * | NS | NS | NS |
| Other substance use risk factors | ||||||||||
| Early tobacco use | 14.1 (176) | 42.8 (104) | 47.0 (42) | 30.5 (19) | ** | *** | * | NS | NS | NS |
| Early alcohol use | 21.0 (180) | 55.9 (111) | 51.6 (47) | 16.5 (11) | *** | *** | NS | NS | ** | * |
| Early illicit drug use | 1.2 (9) | 7.0 (26) | 9.8 (11) | -- | ** | *** | NS | NS | NS | * |
| Economic and social risk factors | ||||||||||
| Family low-SES | 31.4 (388) | 39.6 (97) | 36.0 (37) | 36.7 (29) | NS | NS | NS | NS | NS | NS |
| Family instability | 23.2 (266) | 43.7 (93) | 18.9 (35) | 41.3 (25) | ** | NS | NS | ** | NS | NS |
| Family dysfunction | 24.5 (294) | 47.0 (84) | 23.1 (31) | 36.3 (20) | *** | NS | NS | * | NS | NS |
| Caregiver maltreatment | 27.1 (320) | 39.0 (107) | 44.4 (42) | 53.8 (29) | NS | NS | * | NS | NS | NS |
| School expulsion | 2.0 (33) | 6.4 (31) | 11.8 (17) | -- | ** | ** | NS | NS | NS | NS |
| Bully victimization | 22.9 (256) | 32.1 (58) | 34.9 (28) | 51.6 (24) | NS | NS | * | NS | NS | NS |
| Delinquent/older friends | 22.1 (265) | 46.2 (99) | 46.1 (47) | 31.4 (20) | *** | ** | NS | NS | NS | NS |
Note: Frequencies removed for cell sizes with observations of 5 or less. Data could be made available by contacting primary author.
ADHD = attention-deficit/hyperactivity disorder; NS = not significant; ODD = oppositional defiant disorder; SES = socioeconomic status.
Adjusted models with sampling weights controlled for sex and race.
p<.05;
p<.01;
p<.001
Several childhood risk factors differentiated the problematic patterns that were limited, persistent, and delayed. Rates of childhood anxiety disorders were more than three times as high among those with persistent patterns compared to limited patterns. In turn, rates of family instability and family dysfunction were approximately three-fold higher among those with limited patterns compared to persistent patterns. Finally, those with delayed patterns had lower rates of alcohol use than those with limited and persistent patterns as well as lower rates of anxiety disorders compared to users with persistent patterns.
Late-adolescent correlates (ages 19–21)
Table 2 (and Table S2, available online) shows that participants with non-problematic patterns typically had the lowest rates for many of the late-adolescent risks. Cannabis users with limited and persistent patterns had higher rates of depressive disorders, all types of other substance use, lower educational attainment, many drug-using peers, and moderate/violent criminal offenses. In addition, those with persistent patterns had higher levels of anxiety disorders and suicidality while those with limited patterns had less anxiety, comorbidity, and young parenthood but more material hardship than those with non-problematic patterns. Finally, cannabis users with delayed patterns had more daily tobacco smoking than those with non-problematic patterns.
Table 2.
Late-Adolescent Risk Factors (Ages 19–21) and Early-Adulthood Problematic Cannabis Use Patterns (n = 1,095)
| Non- Problematic n=774 |
Limited Problematic n=195 |
Persistent Problematic n=83 |
Delayed Problematic n=43 |
Significance of Pairwise Comparisonsa |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Psychiatric Risk Factors |
NP, % (N) | LP, % (N) | PP, % (N) | DP,% (N) | LP NP |
PP NP |
DP NP |
LP PP |
LP DP |
PP DP |
| Anxiety disorders | 8.7 (48) | 3.6 (17) | 22.9 (13) | -- | * | * | NS | *** | NS | ** |
| Depressive disorders | 4.2 (39) | 9.2 (24) | 11.5 (6) | -- | * | * | NS | NS | NS | * |
| Suicidality | 5.3 (32) | 6.5 (10) | 16.6 (7) | -- | NS | * | NS | NS | NS | NS |
| Comorbidity: 2 or more | 2.5 (47) | 1.6 (34) | 6.6 (19) | -- | * | *** | NS | * | NS | NS |
| Other Substance Use Risk Factors | ||||||||||
| Tobacco smoking-daily | 33.8 (338) | 85.3 (176) | 86.9 (71) | 65.1 (27) | *** | *** | * | NS | NS | NS |
| Alcohol use disorder | 18.4 (138) | 64.9 (111) | 68.0 (48) | 29.3 (8) | *** | *** | NS | NS | ** | * |
| Illicit drug use | 7.0 (60) | 58.3 (122) | 64.2 (57) | 15.3 (6) | *** | *** | NS | NS | * | ** |
| Economic and Social Risk Factors | ||||||||||
| Material hardships | 49.8 (396) | 67.8 (122) | 53.4 (53) | 64.5 (25) | * | NS | NS | NS | NS | NS |
| Low education attainment | 16.1 (181) | 28.7 (86) | 33.1 (46) | 43.6 (16) | * | * | NS | NS | NS | NS |
| Young parent of 2+ kids | 6.8 (63) | 2.1 (13) | 9.5 (11) | -- | ** | NS | NS | ** | NS | NS |
| Most friends use drugs | 15.2 (101) | 53.9 (114) | 79.2 (64) | 35.8 (16) | *** | *** | NS | * | * | *** |
| Moderate-violent crime | 6.4 (72) | 25.9 (48) | 33.1 (34) | 29.9 (10) | *** | *** | NS | NS | NS | NS |
Note: Frequencies removed for cell sizes with observations of 5 or less. Data could be made available by contacting primary author. NS = not significant.
Adjusted models with sampling weights controlled for sex and race.
p<0.05
p<0.01
p<0.001
Among problematic users, higher rates of anxiety disorders were found among persistent patterns compared to limited and delayed patterns. Delayed patterns were characterized by lower rates of alcohol use disorder, other illicit drug use, and drug-using peers than limited and persistent patterns. Also, those with delayed versus persistent patterns of use had lower rates of anxiety and depressive disorders.
DSM-5 CUD Risk Factors
Table 3 (and Table S3, available online) shows that users with limited and persistent patterns did not differ in cannabis use prior to age 16. However, by late adolescence (ages 19–21), differences in CUD symptomology emerged. Specifically, those with persistent patterns had more total symptoms, cannabis overconsumption, excessive time devoted to using, craving, and tolerance than those with limited patterns.
Table 3.
Risks of Cannabis Use, Disorder, and Symptomology for Limited and Persistent Problematic Use Patterns
| Limited Problematic |
Persistent Problematic |
Significancea | |
|---|---|---|---|
| Cannabis Use (Up to age 16) | n=200, % (N) | n=84, % (N) | |
| Ever use | 37.3 (89) | 45.7 (43) | NS |
| Weekly use | 27.1 (64) | 24.3 (25) | NS |
| Daily use | 8.6 (33) | 16.5 (17) | NS |
| CUD | 21.8 (47) | 27.0 (20) | NS |
| CUD Symptomology (ages 19–21) | n = 195, % (N) | n=83, % (N) | |
| Overconsumption | 17.6 (33) | 36.9 (24) | * |
| Attempts to cut back | 41.1 (79) | 55.5 (39) | NS |
| Excessive time spent using | 47.2 (86) | 81.5 (60) | ** |
| Craving | 17.3 (42) | 38.1 (31) | * |
| Failure to fulfill major roles | 10.3 (16) | 23.1 (11) | NS |
| Causes interpersonal problems | 9.0 (11) | -- | NS |
| Causes reduced activities | -- | -- | NS |
| Physically hazardous | 8.4 (17) | 21.8 (13) | NS |
| Causes health problems | 4.2 (11) | 12.6 (8) | NS |
| Increased tolerance | 30.5 (41) | 50.1 (35) | * |
| Withdrawalb | --- | --- | NA |
| Total CUD Symptoms, Mean (SD) | 1.9 (1.6) | 3.2 (1.8) | *** |
Note: Frequencies removed for cell sizes with observations of 5 or less. Data could be made available by contacting primary author. CUD = cannabis use disorder; NA = not available; NS = not significant; SD = Standard Deviation.
Adjusted regression models with sampling weights controlled for sex and race.
Withdrawal symptom did not show endorsement (0 cases) across patterns.
p<.05;
p<.01;
p<.001
Moderation by Sex and Race/Ethnicity
There was considerable variation in the weighted frequencies of risk factors by race for the problematic cannabis use patterns (data could be made available by contacting primary author). Yet there were no significant two-way interactions by race or sex for the significant risk factors identified in childhood and late adolescence.
DISCUSSION
This study sought to identify childhood and late-adolescent risk factors associated with patterns of problematic cannabis use in early adulthood. Regardless of the developmental period of onset or offset, individuals with limited, persistent, and delayed problematic use patterns had higher levels of childhood and late-adolescent risk factors than those with non-problematic patterns. In addition, the three problematic patterns were characterized by distinctive risk profiles in relation to one another. These findings could be used to tailor intervention efforts aimed at curbing problematic cannabis use during the early life course.
Consistent with other studies, cannabis users whose problematic use started early and lasted the longest (i.e., persistent use group) generally had the highest rates of childhood and late-adolescent risks for psychiatric disorders, other substance use, and challenging economic and social circumstances.14, 16, 32 Users with persistent patterns had higher rates of anxiety disorders across both childhood and late adolescence compared to users with limited and delayed patterns. In the literature, there are mixed findings on the association between anxiety and cannabis use. A positive association was observed in a recent, nationally-representative study of DSM-5 CUD and anxiety among adults and also in a meta-analysis of longitudinal studies on cannabis use.33, 34 However, other studies have not found an association.9 Our results suggest that the discrepancy may be due to heterogeneity in cannabis use patterns or the use of different developmental periods for risk assessment.
Users with limited patterns were characterized by more risk compared to non-problematic users during both childhood and late-adolescence. In particular, childhood antecedents (e.g., CD, comorbidity, early use of all other substances before 16 years, school expulsion, and delinquent/older peers) indicate that transient problematic cannabis use during adolescence may not simply represent “normative” adolescent deviancy.35 Elevated risks were present well before the onset of problematic cannabis use. Limited users stood out for high levels of childhood family instability and family dysfunction. It is possible that problematic cannabis use among limited users is a reaction to their adverse family circumstances that ceases when they transition to early adulthood. In comparison to those with persistent patterns, users with limited patterns had fewer DSM-5 CUD symptoms (i.e., tolerance, craving) which may have made it easier to decrease or quit use.
Cannabis users with delayed patterns of problematic use after the typical peak years of 19–21 represented a small but unique group that differed from non-problematic users early in development as in other studies.36 In childhood, they had the highest levels of externalizing disorders and comorbidity in our sample, accompanied by the highest exposure to maltreatment and peer victimization (54% and 52%, respectively). Their childhood risk profile of defiance and victimization raises the question as to why problematic use was delayed from starting in late-adolescence.12 Two possible hypotheses are suggested by our findings: 1) having lower levels of involvement with other substances and being less likely to have drug-using friends in late-adolescence could have delayed use; 2) declining socioeconomic status in late adolescence—due to low educational attainment (44%)—could have triggered increased cannabis use frequency later in adulthood.14, 37
In terms of race/ethnicity, there were significant differences in distributions across the patterns of problematic cannabis use. Compared to white users, blacks were more likely to have delayed patterns, and American Indians were more likely to have limited patterns. Nevertheless, risk factors did not strongly distinguish any race/ethnicity group. Part of this null finding is no doubt due to limited statistical power for some comparisons. Because of the small number of observations, especially for those with delayed patterns, inferences could not be drawn from the race/ethnicity frequencies provided for each of the risk factors. Instead, the data served a descriptive purpose. For example, Americans Indians with limited patterns of problematic cannabis use had considerably higher levels of young parenthood compared to white and black users. Future research should seek to better understand this association given that other studies have found young parenthood to be protective against continued cannabis use.38
A number of study limitations are noteworthy. First, the sample is only representative of the western North Carolina community from which it was drawn as opposed to being nationally representative. Black participants and Hispanic-Latinos are underrepresented while American Indians are overrepresented. Furthermore, the Indian tribe studied here is not assumed to be representative of other tribes. Second, the risk factors were collapsed over time and tested as binary variables (yes/no) and therefore did not take into account cumulative exposures. Third, assessments of risk factors and problematic use were typically based on a three-month recall period and thus may miss exposures outside of the assessment window. A final study weakness is that policies, attitudes, cannabis potency, and cannabis use (i.e., modes) have changed dramatically since 1993 when the data were first collected at ages 9–13, although the most recent interview was conducted in 2015. As a result, the magnitude of influence for significant childhood antecedents and late-adolescent correlates could be under- or over-stated compared to more contemporary data.
This study benefited from a prospective, longitudinal design utilizing a diverse, community-representative sample. It provides a comprehensive assessment of psychosocial risk factors preceding and accompanying problematic cannabis use in early adulthood. DSM-5 CUD criteria are used in the definition of problematic cannabis use, and pairwise comparisons are made between four problematic patterns of cannabis use over time (non-problematic, limited, persistent, and delayed). In addition, interactions by race/ethnicity and sex are tested with risk factors across all patterns. The detailed reporting of frequencies for all childhood and late-adolescent risk factors by race/ethnicity and problematic cannabis use patterns fully leverages the oversampling of American Indians to contribute to literature on this under-studied population.
Overall, this study illustrates the merit of parsing out the heterogeneous patterns of cannabis use over time to better understand specific risks. We conclude that each pattern of problematic use in early adulthood has a distinctive risk profile with developmentally specific antecedents and correlates. Future research should seek to confirm these findings in a nationally representative sample with contemporary data to improve generalizability. Also, as a next step, the clinical and social significance of the problematic cannabis use patterns (limited, persistent, and delayed) in early adulthood requires investigation of associated outcomes.
Supplementary Material
Acknowledgments
This research was supported by the National Institutes of Health (NIDA: R01DA036523, R01DA11301, P30DA23026; NIMH: MH094605, MH63970, MH63671, MH48085; NICHD: HD07376) and the William T. Grant Foundation. The content does not necessarily represent the official views of the NIH.
The authors thank the study participants and their parents for their cooperation, and the Great Smoky Mountains Study staff for their help in conducting the study.
Disclosure: Dr. Hill has received research support from the National Institute on Drug Abuse and National Institute of Child Health and Development. Dr. Shanahan has received research support from the National Institute on Drug Abuse and the National Institute of Child Health and Development. Dr. Costello has received research support from the National Institute of Mental Health and the National Institute on Drug Abuse. She is co-author of the following assessment tools: Child and Adolescent Psychiatric Assessment (CAPA), Young Adult Psychiatric Assessment (YAPA), Child and Adolescent Impact Assessment (CAIA), Child and Adolescent Services Assessment (CASA), and Mood and Feelings Questionnaire (MFQ). No personal income is derived from any of these measurements. Dr. Copeland has received research support from the National Institute of Mental Health and the National Institute on Drug Abuse.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Sherika Hill, Duke University, Durham, NC.
Dr. Lilly Shanahan, Jacobs Center for Productive Youth Development, University of Zurich, Zurich, Switzerland.
Dr. E. Jane Costello, Duke University, Durham, NC.
Dr. William Copeland, Duke University, Durham, NC.
References
- 1.NIDA. [Accessed July 15, 2015];Drug Facts: Nationwide Trends. 2013 http://www.drugabuse.gov/publications/drugfacts/nationwide-trends.
- 2.Kann L, Kinchen S, Shanklin SL, et al. Youth Risk Behavior Surveillance — United States, 2013. MMWR Suppl. 2014;63:1–168. [PubMed] [Google Scholar]
- 3.Copeland WE, Hill S, Costello EJ, Shanahan L. Cannabis Use and Disorder From Childhood to Adulthood in a Longitudinal Community Sample With American-Indians. J Am Acad Child Adolesc Psychiatry. 2017;56:124–132.e2. doi: 10.1016/j.jaac.2016.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farmer RF, Kosty DB, Seeley JR, et al. Natural course of cannabis use disorders. Psychol Med. 2015;45:63–72. doi: 10.1017/S003329171400107X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Filbey FM, Aslan S, Calhoun VD, et al. Long-term effects of marijuana use on the brain. Proc Natl Acad Sci U S A. 2014;111:16913–16918. doi: 10.1073/pnas.1415297111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kraan T, Velthorst E, Koenders L, et al. Cannabis use and transition to psychosis in individuals at ultra-high risk: review and meta-analysis. Psychol Med. 2016;46:673–681. doi: 10.1017/S0033291715002329. [DOI] [PubMed] [Google Scholar]
- 7.Swift W, Coffey C, Degenhardt L, Carlin JB, Romaniuk H, Patton GC. Cannabis and progression to other substance use in young adults: findings from a 13-year prospective population-based study. Journal of epidemiology and community health. 2012;66(7):e26. doi: 10.1136/jech.2010.129056. [DOI] [PubMed] [Google Scholar]
- 8.Lee JY, Brook JS, Finch SJ, Brook DW. Trajectories of marijuana use from adolescence to adulthood predicting unemployment in the mid 30s. Am J Addict. 2015;24:452–9. doi: 10.1111/ajad.12240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farmer RF, Seeley JR, Kosty DB, et al. Internalizing and Externalizing Psychopathology as Predictors of Cannabis Use Disorder Onset During Adolescence and Early Adulthood. Psychol Addict Behav. 2015;29:541–51. doi: 10.1037/adb0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fergusson DM, Boden JM, Horwood LJ. The developmental antecedents of illicit drug use: evidence from a 25-year longitudinal study. Drug Alcohol Depend. 2008;96:165–177. doi: 10.1016/j.drugalcdep.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Brook JS, Lee JY, Brook DW. Trajectories of Marijuana Use Beginning in Adolescence Predict Tobacco Dependence in Adulthood. Subst Abus. 2015;36:470–7. doi: 10.1080/08897077.2014.964901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oshri A, Rogosch FA, Burnette ML, Cicchetti D. Developmental pathways to adolescent cannabis abuse and dependence: child maltreatment, emerging personality, and internalizing versus externalizing psychopathology. Psychol Addict Behav. 2011;25:634–644. doi: 10.1037/a0023151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liebregts N, van der Pol P, Van Laar M, de Graaf R, van den Brink W, Korf DJ. The Role of Study and Work in Cannabis Use and Dependence Trajectories among Young Adult Frequent Cannabis Users. Front Psychiatry. 2013;4:85. doi: 10.3389/fpsyt.2013.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Windle M, Wiesner M. Trajectories of marijuana use from adolescence to young adulthood: predictors and outcomes. Dev Psychopathol. 2004;16:1007–1027. doi: 10.1017/s0954579404040118. [DOI] [PubMed] [Google Scholar]
- 15.Swift W, Coffey C, Carlin JB, Degenhardt L, Patton GC. Adolescent cannabis users at 24 years: trajectories to regular weekly use and dependence in young adulthood. Addiction. 2008;103:1361–1370. doi: 10.1111/j.1360-0443.2008.02246.x. [DOI] [PubMed] [Google Scholar]
- 16.van der Pol P, Liebregts N, de Graaf R, Korf DJ, van den Brink W, van Laar M. Three-year course of cannabis dependence and prediction of persistence. Eur Addict Res. 2015;21:279–290. doi: 10.1159/000377625. [DOI] [PubMed] [Google Scholar]
- 17.Arria AM, Caldeira KM, Bugbee BA, Vincent KB, O'Grady KE. Marijuana use trajectories during college predict health outcomes nine years post-matriculation. Drug Alcohol Depend. 2016;159:158–165. doi: 10.1016/j.drugalcdep.2015.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palamar JJ, Ompad DC, Petkova E. Correlates of intentions to use cannabis among US high school seniors in the case of cannabis legalization. Int J Drug Policy. 2014;25:424–435. doi: 10.1016/j.drugpo.2014.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.APA. Diagnostic and Statistical Manual of Mental Disorders. Fifth. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 20.Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: gender and racial/ethnic differences. J Adolesc Health. 2012;50:154–163. doi: 10.1016/j.jadohealth.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown TL, Flory K, Lynam DR, Leukefeld C, Clayton RR. Comparing the developmental trajectories of marijuana use of African American and Caucasian adolescents: patterns, antecedents, and consequences. Exp Clin Psychopharmacol. 2004;12(1):47–56. doi: 10.1037/1064-1297.12.1.47. [DOI] [PubMed] [Google Scholar]
- 22.Juon HS, Fothergill KE, Green KM, Doherty EE, Ensminger ME. Antecedents and consequences of marijuana use trajectories over the life course in an African American population. Drug Alcohol Depend. 2011;118:216–223. doi: 10.1016/j.drugalcdep.2011.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stanley LR, Harness SD, Swaim RC, Beauvais F. Rates of substance use of American Indian students in 8th, 10th, and 12th grades living on or near reservations: update, 2009–2012. Public Health Rep. 2014;129:156–163. doi: 10.1177/003335491412900209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whitesell NR, Asdigian NL, Kaufman CE, et al. Trajectories of substance use among young American Indian adolescents: patterns and predictors. J Youth Adolesc. 2014;43(3):437–453. doi: 10.1007/s10964-013-0026-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Costello EJ, Angold A, Burns BJ, et al. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 26.Angold A, Cox A, Prendergast M, et al. The Young Adult Psychiatric Assessment (YAPA) Durham, NC: Duke University Medical Center; 1999. [Google Scholar]
- 27.Angold A, Costello E. The Child and Adolescent Psychiatric Assessment (CAPA) J Am Acad Child Adolesc Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- 28.Hjorthoj CR, Hjorthoj AR, Nordentoft M. Validity of Timeline Follow-Back for self-reported use of cannabis and other illicit substances--systematic review and meta-analysis. Addict Behav. 2012;37:225–233. doi: 10.1016/j.addbeh.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 29.Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health. 2003;33:436–457. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 30.Angold A, Costello EJ. The Child and Adolescent Psychiatric Assessment (CAPA) J Am Acad Child Adolesc Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- 31.Stata Statistical Software: Release 14 [computer program] College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 32.Wittchen HU, Frohlich C, Behrendt S, et al. Cannabis use and cannabis use disorders and their relationship to mental disorders: a 10-year prospective-longitudinal community study in adolescents. Drug Alcohol Depend. 2007;88(Suppl 1):S60–70. doi: 10.1016/j.drugalcdep.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 33.Kedzior KK, Laeber LT. A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population- a meta-analysis of 31 studies. BMC Psychiatry. 2014;14:136–136. doi: 10.1186/1471-244X-14-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hasin DS, Kerridge BT, Saha TD, et al. Prevalence and Correlates of DSM-5 Cannabis Use Disorder, 2012–2013: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry. 2016;173:588–599. doi: 10.1176/appi.ajp.2015.15070907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roisman GI, Monahan KC, Campbell SB, Steinberg L, Cauffman E. Is adolescence-onset antisocial behavior developmentally normative? Dev Psychopathol. 2010;22:295–311. doi: 10.1017/S0954579410000076. [DOI] [PubMed] [Google Scholar]
- 36.Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. Early adolescent through young adult alcohol and marijuana use trajectories: early predictors, young adult outcomes, and predictive utility. Dev Psychopathol. 2004;16(1):193–213. doi: 10.1017/s0954579404044475. [DOI] [PubMed] [Google Scholar]
- 37.Brook JS, Lee JY, Brown EN, Finch SJ, Brook DW. Developmental trajectories of marijuana use from adolescence to adulthood: personality and social role outcomes. Psychol Rep. 2011;108:339–357. doi: 10.2466/10.18.PR0.108.2.339-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kerr DC, Capaldi DM, Owen LD, Wiesner M, Pears KC. Changes in At-Risk American Men's Crime and Substance Use Trajectories Following Fatherhood. J Marriage Fam. 2011;73:1101–1116. doi: 10.1111/j.1741-3737.2011.00864.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.