Abstract
Health-related behaviors, such as smoking, alcohol use, exercise, and diet, are major determinants of physical health and health disparities. However, a growing body of experimental research in humans and animals also suggests these behaviors can impact the ways our bodies respond to stress, such that they modulate (that is, serve as a means to self-regulate or cope with) the deleterious impact of stressful experiences on mental health. A handful of epidemiologic studies have investigated the intersection between stress and health behaviors on health disparities (both mental and physical), with mixed results. In this study we use a novel instrument designed to explicitly measure the self-regulatory motivations and perceived effectiveness of eight health-related self-regulatory behaviors (smoking, alcohol, drug use, overeating, prayer, exercise, social support, talking with a counselor) in a subset of the Health and Retirement Study (N=1354, Mean age=67, 54% female). We find that these behaviors are commonly endorsed as self-regulatory stress-coping strategies, with prayer, social support, exercise, and overeating used most frequently. The likelihood of using particular behaviors as self-regulatory strategies varied significantly by sex, with only limited variation by race/ethnicity, education, or wealth. We also find that greater stress exposure is associated with higher likelihood of using these behaviors to self-regulate feelings of emotional distress, particularly health-harming behaviors like smoking, alcohol, and overeating. These findings provide an important link between sociological and psychological theoretical models on stress and empirical epidemiological research on social determinants of health and health disparities.
Keywords: United States, Stress, coping, Health disparities, Epidemiology, Aging, Behavior
Highlights
-
•
Most people engage in a wide range of self-regulatory behaviors.
-
•
Behaviors vary in their perceived effectiveness at reducing emotional distress.
-
•
Women are more likely to engage in self-regulatory behaviors to cope with stress.
-
•
Little variation in use of self-regulatory behaviors by race, education, or wealth.
-
•
Stress was associated with greater use, particularly of health-harming behaviors.
Introduction
The only way to keep your health is to eat what you don’t want, drink what you don’t like, and do what you’d rather not.
Mark Twain
A compelling body of epidemiologic research indicates that exposure to stressful events contributes to poor health and health disparities over the life course (James, 2009, Miller et al., 2009). “Stress” refers to any threat or challenge to homeostasis (McEwen, 2013), and includes a broad range of exposures such as prenatal insults (Hilmert et al., 2008), early life adversity (Miller, Chen, & Parker, 2011), work (e.g., job strain), finances (e.g., poverty, food insecurity), interpersonal events (e.g., divorce, social isolation), trauma (e.g., emotional, physical, or sexual abuse), and experiences of discrimination (Abdou et al., 2016, Turner et al., 1995). While the neurobiological stress response (e.g., hypothalamic-pituitary-adrenal (HPA)-axis, sympathetic nervous system) is well-suited for addressing acute stressors, it is hypothesized that repeated, chronic activation of the body’s stress response (commonly operationalized as “allostatic load,” “weathering,” and related constructs) contributes to the development of cardiovascular and metabolic conditions in mid- and late-life (Geronimus, 1992; McEwen & Seeman, 1999; Miller et al., 2011). This process of “wear and tear” is often cited as an explanation of the large racial/ethnic and socioeconomic disparities in physical health seen in the US population (Geronimus, 1992).
However, this explanation of stress as a direct cause of social disparities in physical health does not account for the fact that socially-disadvantaged groups, particularly African Americans and Hispanics in the US, despite having higher morbidity and mortality, have better mental health relative to non-Hispanic Whites (Jackson et al., 2010, Mezuk et al., 2010, Mezuk et al., 2013). For example, African Americans are less likely to have major depression, anxiety disorders, or substance abuse/dependence relative to non-Hispanic Whites, a finding that has been replicated across numerous nationally-representative samples and measures of psychopathology (Mezuk et al. 2013). Since stress is an established cause of these mental health outcomes, the apparently paradoxical finding that these socially-disadvantaged groups (which are presumably exposed to more stress than socially-advantaged non-Hispanic whites) do not have worse mental health, despite having worse physical health, warrants a reconsideration of the potential pathways linking stress, health behaviors, and health status. Informed by this evidence, we developed the Environmental Affordances Model of Health Disparities (EA Model; Mezuk et al. 2013) a transdisciplinary framework which guides our empirical research on how stress, behavior, and context intersect to influence mental and physical health.
Re-conceptualization of coping behaviors under the EA model
While much is known about the direct effects of stress exposure on health, there has been less focus on how the intersection between stress and coping behaviors (i.e., efforts to self-regulate the body’s stress response) relates to health and health disparities (Ellis and Del Giudice, 2014, Mezuk et al., 2013). Under the conceptualization of stress as a direct cause of poor physical health, behaviors are treated as confounders (i.e., correlates of stress and causally related to health, but not part of the pathway linking the two (Umberson, Liu & Reczek, 2008)). This conceptualization of health behaviors as confounders may stem from an inappropriately narrow scope of coping typologies. Coping is traditionally defined as the “cognitive and behavioral efforts to manage specific external and/or internal demands that are appraised as taxing or exceeding the resources of the person,” (Lazarus & Folkman, 1984, pp. 141), and is generally divided into approach and avoidance typologies (Taylor & Stanton, 2007). Approach-oriented coping involves processes that directly address either the source of stress or the resulting homeostatic imbalance (e.g., cognitive strategies like planning, strategizing, humor, and acceptance), and implicitly focus on coping as a psychological experience. When behaviors are examined as approach-oriented strategies the focus is often on seeking social support (e.g., talking to others or seeking advice). Within this typology, other behaviors (e.g., doing activities as a distraction, disengaging from the situation) are regarded as avoidant coping. The term avoidant invokes processes that prevent individuals from effectively addressing the stressful situation and/or do not address the homeostatic imbalance induced by the stressor. Health-related behaviors (i.e., smoking, drinking alcohol, eating, exercise) are chief among these avoidant strategies (Umberson et al., 2008). For both approach and avoidant coping strategies there is little consideration of the biological underpinnings by which these processes translate into improved mental health; however, all mental experiences are derived from the brain, even if we do not fully understand how this derivation occurs.
A growing body of experimental research (both in animal models and humans) suggests that these “avoidant” health behaviors act on a common set of reward and stress-response pathways and have the same (short-term) salutary impact on restoring homeostasis (both psychological and physiological) as approach-oriented coping behaviors (Mezuk et al., 2013). For example, in a placebo-controlled study of current smokers (i.e., smoking as usual vs. nicotine patch vs. placebo patch), cigarette use reduced the cortisol response to a laboratory stressor, indicating a biological underpinning between stress and relapse from smoking cessation (Wardle, Munafo, & de Wit, 2011). In another example, women randomized to consume high-sugar beverages over a 2-week period had a reduced cortisol response to a laboratory stressor compared to women receiving aspartame-sweetened beverages, suggesting a negative feedback loop between glucose consumption and HPA-axis reactivity (Tryon et al., 2015). There are similar examples of linkages between the HPA-axis and other reinforced behaviors (Koob, 2008) including alcohol use (Stephens & Wand, 2012), eating (Pecoraro, Reyes, Gomez, Bhargava, & Dallman, 2004), drug use (Chaplin et al., 2010), meditation (Rosenkranz et al. 2016), and exercise (Childs & de Wit, 2014). This suggests a need to consider the neuroscience of coping as much as we consider the psychology of coping.
In sum, a growing body of research indicates that the relationships among stress exposure, stress reactivity, and health behaviors are intrinsically linked in two important ways: (1) Stress exposure impacts the likelihood of engaging in health behaviors, and these behaviors, in turn, impact physiological reactivity to subsequent stressors; and (2) These behaviors engage reinforcing (e.g., dopaminergic and opioid) pathways in the brain, which are also connected to the HPA-axis and related stress-response systems. Thus, in the short-term, these health behaviors can serve as effective stress-coping strategies and preserve mental health, just as traditional approach-oriented coping strategies are known to do. However, unlike these traditional coping strategies, over the long-term behaviors such as smoking, excessive alcohol use, and poor diet contribute to disparities in physical health (Lantz et al., 1998). Moreover, sociological studies have shown that the impact of poor health behaviors (e.g., smoking, physical inactivity) on physical health is amplified by stress for individuals with fewer socioeconomic resources (Krueger & Chang, 2008), and that the strength of the relationship between health behaviors and health outcomes varies by race/ethnicity, largely because of racial/ethnic stratification of socioeconomic resources (Krueger, Saint Onge, & Chang, 2011). This illustrates the need for transdisciplinary frameworks like the EA Model that seek to link biology, behavior, and social context.
Limitations of existing research testing the EA model
In this paper we refer to health behaviors as self-regulatory coping behaviors (SRCB) to emphasize that they are coping efforts aimed at addressing the neurobiological stress response and returning the individual to a homeostatic state. As with traditional social psychology theories of coping, the EA Model posits that the specific set of SRCBs prompted in response to stress is influenced by context. By context, we mean the affordances and constraints of the environment, including both physical context (i.e., neighborhood attributes, such as the availability of fast food restaurants) and sociocultural context (i.e., social norms, social integration, social cohesion, and other cultural resources). In this way, structural sources of health disparities (i.e., poverty, residential segregation, social capital) influence health disparities by both acting as a source of stress (i.e., financial strain) and by truncating the opportunities individuals have to cope with stressors (Bird and Rieker, 2008, Link and Phelan, 1995).
However, to date epidemiologic research testing hypotheses of the EA Model has not directly assessed whether health behaviors are actually being used as efforts to self-regulate (i.e., it has been assumed, rather than directly measured, that the behaviors are used to cope with stress) (Boardman and Alexander, 2011, Jackson et al., 2010, Keyes et al., 2011, Mezuk et al., 2010). This is because these analyses have relied on existing data that assessed these behaviors in traditional ways (i.e., asking respondents if, but not why, they smoke, overeat, exercise, etc.). There is also little information known about the perceived effectiveness of these behaviors at reducing feelings of distress in a general population sample (i.e., do individuals experience a reduction in psychological distress as predicted by the biological experimental data, and how does that perceived effectiveness vary across behaviors?) In addition, there has been little attention to how SRCBs that harm physical health (e.g., smoking) relate to SRCBs that promote health (either mental or physical: e.g., exercise). For instance, do people who use health-promoting behaviors avoid health-harming behaviors, or do people who make use of SRCBs in general have a greater likelihood of using all kinds of SRCBs, whether health-promoting or health-harming? In this study we aim to address these limitations of existing research.
Goals and hypotheses of the present study
The goal of this paper is to examine the intersection of stress, context, and health behaviors from a transdisciplinary perspective. Our focus is on a central tenant of the EA Model: that stress prompts use of SRCBs, and that this relationship is influenced by context. In this analysis we do not address whether the interaction of stress and SRCBs relates to disparities in mental and physical health, however these disparities are the underlying motivation for this research.
Our objectives are threefold: First, to describe the nature and distribution of eight SRCBs – smoking, drug use, alcohol use, overeating, exercise, prayer, seeking counsel, and social support – among older adults using a novel instrument we designed explicitly to assess these behaviors as self-regulatory strategies. Second, to assess how context shapes the distribution, content, and perceived effectiveness of SRCB. For this objective we use four proxies of context: education, wealth, sex, and race/ethnicity. These characteristics, while not direct measures of context, are correlated with the resources available to individuals and the social norms and values that shape both individuals’ exposure to stressors, their appraisal of an experience as stressful, and their efforts to cope with perceived stressors (Link & Phelan, 1995). Our hypothesis for this objective is that socially-disadvantaged contexts (i.e., lower education, less wealth, female sex, non-White race/ethnicity) will engage in more health-harming SRCBs as compared to more advantaged contexts. For the third objective, we examined whether greater exposure to stressors (i.e., traumatic experiences, discrimination, and stressful life events) and psychological distress were associated with greater likelihood of engaging in SRCBs. Our hypothesis for this objective is that stress and psychological distress will be more strongly related to engaging in health-harming SRCBs as compared to health-promoting SRCBs. As part of this objective we also explored whether the relationship between stress and SRCBs was moderated by the proxy indicators of context, but these were hypothesis generating, rather than hypothesis testing, analyses.
Methods
Sample
Data come from the Health and Retirement Study (HRS), a nationally-representative steady-state cohort study of US adults over the age of 50. The HRS oversamples African Americans and Hispanics, and the 2008 wave had an overall response rate of 88.4%, which is consistent with prior waves (Sonnega et al., 2014). Additional details of the HRS study design have been described elsewhere (Heeringa & Connor, 1995). While approximately 20,000 individuals are interviewed at each biennial wave of the HRS, our analysis is limited to 1354 respondents who completed an experimental module we developed that was administered as part of the 2008 HRS (see Online Supplement). These experimental modules are administered to a random subset (between 1200 and 1500 people) of the total HRS cohort each wave. This analysis used the RAND (version L) imputed dataset for covariates.
The HRS is approved by the Institutional Review Board at the University of Michigan and all participants provided informed consent.
Measures
Self-regulatory coping behaviors (SRCB)
We examined eight SRCBs (four health-harming and four health-promoting) in the experimental module: alcohol, drugs, eating, smoking, exercise, prayer, social support, and seeking advice from a counselor. This index is adapted from questions originally used in the National Survey of Black Americans (Broman, 1996, Jackson and Gurin, 1987). The specific wording of the items is provided in the Online supplement. The introduction to this part of the module oriented respondents to think about “things you are most likely to do after having what you think is a stressful event or day” (emphasis in original). For each SRCB respondents were asked frequency of using the behavior to cope with stress: “How often do you use [behavior] to help make it easier to bear?” with responses coded using a 5-point Likert scale ranging from Never to Very Often. Additional information regarding the validity and reliability of this index is in the Online supplement. For this analysis we re-categorized the frequency of use to 3 levels: Never=0, Hardly ever/Not often=1, and Fairly often/Very often=2 based on the distributions of these responses to ensure adequate cells sizes for analysis. This frequency was then summed across the SRCB and the average of this summary variable was categorized into tertiles (<1.5, 1.5 to <2, and ≥2) for the descriptive analysis. We also created a summary score of the total number of SRCB endorsed as Fairly often/Very often (range 0–8), number of health-promoting SRCB endorsed (range 0–4) and the total number health-harming SRCB endorsed (0–4).
Respondents who gave any response other than Never to each SRCB were then asked to report on the perceived effectiveness of the behavior on lessening their distress: “How much did it [the behavior] reduce your feelings of being stressed?” with responses coded using a 4-point Likert scale ranging from Not at all to A great deal (Cronbach’s α for all 8 items: 0.68; for the 4 health-harming items: 0.61; for the 4 health-harming items: 0.57). We recategorized the perceived effectiveness into three levels; Not at all=0, Not very much=1, and Some/A great deal=2, based on the distributions of these responses to ensure adequate cells sizes for analysis.
Proxy indicators of context
We examined variation in SRCBs and their relationship to stressors by three proxy indicators of context: race/ethnicity, sex, and socioeconomic status (SES). To ensure adequate cell sizes for analysis, race/ethnicity was categorized as non-Hispanic white vs. non-White (52.79% (n=199) of which were non-Hispanic Black and 37.14% (n=140) of which were Hispanic); we also conducted a sensitivity analysis using a three-level indicator for race/ethnicity. Sex was categorized as male vs. female. We examine two measures of SES: education (categorized as <high school vs. ≥high school diploma/GED) and wealth, a summary measure derived from total assets (e.g., home ownership, retirement savings, income including from Social Security) minus total debts (e.g., loans, mortgage, credit card balances). Wealth was split at the median (≤$203,811 vs. >203,811). Particularly for older populations, many of whom are retired or only work part-time, wealth is a better measure of current SES than household income or occupation (Robert & House, 1996).
Stressors and psychological distress
A subsample (n=517) of the module respondents also completed the Leave Behind Questionnaire (LBQ), a self-administered psychosocial questionnaire that is administered to a random half of the total HRS at each wave (Clarke, Fisher, House, Smith, & Weir, 2008). We examined three measures of stressors from the LBQ: (a) Lifetime traumatic events, from an 11-item scale of lifetime exposure to traumatic events (Krause, Shaw, & Cairney, 2004); (b) Recent stressful events, from a 6-item index of recent life stressors or situations (Turner et al., 1995), and (c) Experiences of discrimination, from a 7-item measure of discrimination (Williams, Yan, Jackson, & Anderson, 1997). Experience of traumatic events (e.g., being in a natural disaster, being assaulted, having a family member have serious illness, being abused as a child) were each recorded dichotomously (yes/no) and then summed to create a total score (observed range: 0–9). Recent (i.e., within the past 5 years) stressful events (e.g., being fired or laid off, being robbed or having your home burglarized) were recorded dichotomously (yes/no) and then summed to create a total score (observed range: 0–4). Finally, experiences of discrimination (e.g., unfairly dismissed from or not hired for a job, unfairly stopped by the police) were recorded dichotomously (yes/no) and then summed to create a total score (observed range: 0–6). We created a composite index of these measures by summing them (range: 0–13, mean: 2.55).
Because it was available on entire sample (rather than just the subset that received the LBQ), we also examined psychological distress as a predictor of SRCB. Distress was assessed using the 8-item Centers for Epidemiologic Studies - Depression (CESD) scale, which asks about the occurrence (yes/no) of depressive symptoms (e.g., feeling that everything was an effort, difficulty sleeping) in the past week (Turvey, Wallace, & Herzog, 1999); items were summed to create a total score (positive items reverse-coded (range: 0–8, mean: 1.32)).
Other covariates
Age (in years), self-rated health (categorized as excellent/very good (reference group), good, fair, and poor), number of chronic health conditions (e.g., diabetes, cardiovascular disease, cancer, arthritis) (range: 0–8, average: 2.25), and number of functional limitations (e.g., using the phone, managing money, taking medications) (range: 0–5, average: 0.20) were assessed by self-report.
Analysis
For our first objective we used weighted descriptive statistics, paired with ANOVA and Rao-Scott Chi2 tests, to characterize the content of SRCB. As part of this we examined (a) the relationship between frequency of engaging in each SRCB and its perceived effectiveness at reducing stress, and (b) whether engaging in health-harming SRCBs (e.g., smoking) related to the likelihood of engaging in health-promoting SRCBs (e.g., exercise).
For our second objective we used multivariable regression models to estimate the marginal means of the frequency and effectiveness of SCRBs by the four indicates of context (i.e., sex, race/ethnicity, wealth and education). We used Poisson regression models to estimate the marginal mean count of the frequency of SCRBs endorsed (overall, health-harming, and health-promoting). We used logistic regression models to estimate the marginal mean proportion of respondents who Fairly/Very often (vs. less often) used each SRCB and who rated the perceived effectiveness of each SRCB as Some/A great deal (vs. less effective). These marginal means were weighted according to the proportions of each indicator of context (i.e., proportion with low vs. high education) using the LSMeans post-estimation function. Models were adjusted for demographic characteristics, number of health conditions, and functional limitations. Statistically significant differences between the marginal means across levels of each indicator of context (e.g., male vs. female, low vs. high education) were determined by the estimated beta coefficients.
Finally, to examine the intersection between stressors and SRCBs we added the summary stress score in the Poisson models predicting the frequency of engaging in SRCBs; because the stress measure was available on only a subset of the sample, we then refit these models with CESD as an indicator of psychological distress. As a final exploratory analysis, we refit these models with interactions between stress and the four indicators of context (e.g., stress×sex, stress×education) to test whether these indicators modified the relationship between stress and SRCBs.
All analyses accounted for the complex sampling design and all descriptive estimates are weighted to be representative of the US population >50 years old. Analyses were conducted using SAS 9.4 and all p-values refer to two-tailed tests.
Results
Table 1 shows the characteristics of the HRS subsample that completed the experimental module, overall and by number of SRCBs endorsed. Women and individuals with lower wealth were more likely to use SRCBs, but there was no difference by race/ethnicity or education. Stressful events, the composite stress score, and CESD were positively correlated with likelihood of engaging in SRCBs. Finally, greater levels of chronic health conditions and functional limitations were associated with greater use of SRCBs.
Table 1.
Weighted descriptive statistics by number of coping strategies fairly/very often used.
| Overall |
Number of SRCBs fairly/very often used |
X2or F, p-value | |||
|---|---|---|---|---|---|
| None | 1 | 2+ | |||
| N | 1354 | 439 | 470 | 445 | |
| Sociodemographic Characteristics | |||||
| Age (M, SE) | 67.34 (0.35) | 68.38 (0.61) | 67.87 (0.53) | 65.87 (0.52) | 6.24, 0.0036 |
| White Race | 1009 (80.73) | 337 (81.51) | 348 (79.54) | 324 (81.17) | 0.47, 0.7888 |
| Female | 789 (54.44) | 179 (38.19) | 283 (54.57) | 327 (69.22) | 58.53, <0.0001 |
| Education (M, SE) | 12.90 (0.11) | 13.00 (0.21) | 12.81 (0.13) | 12.91 (0.15) | 0.38, 0.6841 |
| Net Worth (M, SE) | 562,683.38 (36, 745.69) | 802,495.98 (84,222.89) | 490,883.63 (40,624.64) | 412,372.60 (40,617.78) | 9.59, 0.0003 |
| Psychological Distress Indicatorsa | |||||
| Stress Events (M, SE) | 0.33 (0.06) | 0.15 (0.04) | 0.40 (0.07) | 0.44 (0.16) | 6.36, 0.0033 |
| Traumatic Events (M, SE) | 1.67 (0.06) | 1.48 (0.13) | 1.73 (0.11) | 1.81 (0.10) | 1.67, 0.1974 |
| Discrimination Events (M, SE) | 0.54 (0.06) | 0.38 (0.07) | 0.53 (0.08) | 0.73 (0.15) | 2.28, 0.1122 |
| Stress Score (M, SE) | 2.55 (0.13) | 2.03 (0.18) | 2.66 (0.19) | 2.99 (0.35) | 4.08, 0.0223 |
| CES-D (M, SE) | 1.32 (0.07) | 0.79 (0.07) | 1.20 (0.08) | 1.92 (0.15) | 33.41, <0.0001 |
| Health Conditions | |||||
| Chronic Conditions (M, SE) | 2.14 (0.05) | 1.92 (0.08) | 2.11 (0.08) | 2.37 (0.10) | 6.46, 0.0030 |
| IADL’s (M, SE) | 0.18 (0.02) | 0.11 (0.02) | 0.15 (0.02) | 0.26 (0.04) | 5.35, 0.0075 |
Stress events, traumatic events, discrimination events, and the standardized sum of these come from the Psychosocial. Leave Behind questionnaire which was completed by a subsample of 2008 respondents (N=517).
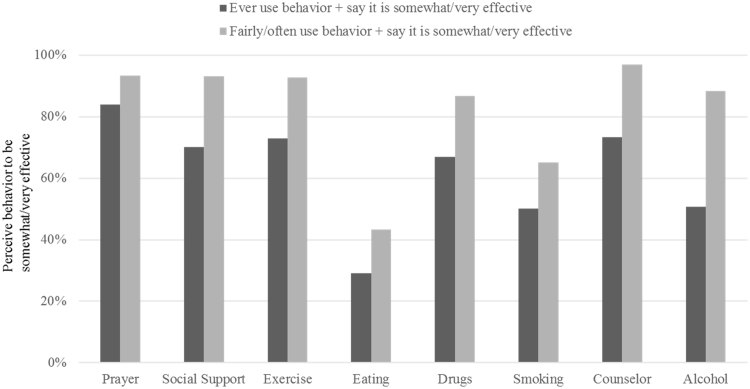
The most frequently reported SRCBs were prayer (73%), social support (50%), overeating (38%), and exercise (27%); the least commonly reported were alcohol (22%), talking to a counselor (19%), drug use (16%), and smoking (10%). Fig. 1 and Supplemental Table 1 provide evidence of the construct validity of the SRCB measure. They show the perceived effectiveness of SRCBs at reducing feelings of stress based on frequency of use. Consistent with the notion that individuals should be more likely to engage in a behavior if they felt it was helpful, individuals who reported that a SRCB was effective at reducing their feelings of stress were more likely to engage in it. For example, only 29% of the people who ever overeat to cope with stress said it was effective at reducing their feelings of distress, as compared to 43% of the people who fairly/very often overeat to cope, a difference of 14 percentage points. Similarly, only 50% of people who ever drink alcohol to cope with stress said it was effective, as compared to 88% of people who fairly/often drink alcohol to cope, a difference of 38 percentage points.
Fig. 1.
Values are weighted percentages who endorse that the behavior is somewhat/very effective at reducing feelings of stress for those who ever use the behavior (dark gray) or frequently use the behavior (light gray).
Table 2 shows the intersection of positive and negative SRCB. Among those who reported at least one negative (i.e., alcohol, drugs, smoking, or eating) SRCB (N=294), a majority also engaged in at least one positive behavior: 14.9% endorsed exercise, 70.1% endorsed prayer, 30.7% endorsed social support, and 13.5% endorsed talking to a counselor. Among those who reported at least one positive SRCB (N=856), 6.4% also endorsed alcohol, 10.7% endorsed drugs, 14.9% endorsed eating, and 6.6% endorsed smoking.
Table 2.
Percent engaging in specific SRCB among those using any positive or negative behavioral coping strategy.
|
Endorse at least one positive SRCB |
Endorse at least one negative SRCB |
|||
|---|---|---|---|---|
| No | Yes | No | Yes | |
| N=498 | N=856 | N=1,060 | N=294 | |
| Alcohol | 10 (2.98) | 38 (6.38) | . | 48 (19.74) |
| Drugs | 13 (1.94) | 85 (10.72) | . | 98 (28.89) |
| Eating | 16 (3.70) | 110 (14.95) | . | 126 (41.79) |
| Smoking | 23 (5.85) | 43 (6.57) | . | 66 (24.27) |
| Exercise | . | 120 (17.50) | 81 (9.69) | 39 (14.88) |
| Prayer | . | 785 (89.61) | 576 (51.67) | 209 (70.58) |
| Social Support | . | 266 (30.27) | 175 (15.01) | 91 (30.73) |
| Counselor | . | 76 (9.38) | 42 (3.25) | 34 (13.54) |
Values are N (weighted column %) of reporting that they “fairly often” or “very often” used each SRCB to cope with stress.
Positive SRCB: exercise, prayer, counselor, social support.
Negative SRCB: smoking, alcohol, drugs, eating.
Note: The two “positive SRCB” columns and the two “negative SRCB” columns each represent total sample (N=1354).
Context and SRCB
Table 3 shows the unadjusted and marginal means of the various metrics of SRCB by the four proxies of context (sex, race/ethnicity, education, and wealth); values in which there is a significant relationship between the contextual factor and SRCB are indicated. Of the four contextual variables examined, only sex was substantially related to the number (total, negative, and positive) of SRCB, with women more likely to report these behaviors relative to men. When this was decomposed into individual behaviors, women were more likely than men to report eating, prayer, social support, and seeing a counselor than men. Women also reported that these behaviors were more effective at relieving feelings of distress than men, including behaviors that they were not significantly more likely to endorse, such as using drugs or alcohol.
Table 3.
The influence of context on frequency, type, and perceived effectiveness of SRCB.
|
Gender |
Race |
Education |
Wealth |
|||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | White | Non-white | Low | High | Low | High | |
| Number of SRCB | ||||||||
| Total SRCB unadjusted mean (SE) marginal mean (SE) |
0.93 (0.06) 0.88 (0.06) |
1.47 (0.05) 1.37(0.05)** | 1.21 (0.04) 1.13 (0.05) |
1.25 (0.08) 1.08 (0.07) |
1.11 (0.10) 1.00 (0.09) |
1.25 (0.04) 1.15 (0.04) |
1.32 (0.06) 1.16 (0.06) |
1.14 (0.05) 1.08 (0.05) |
| Positive SRCB unadjusted mean (SE) marginal mean (SE) |
0.70 (0.04) 0.69 (0.04) |
1.12 (0.04) 1.08 (0.04)** |
0.91 (0.04) 0.87 (0.04) |
1.00 (0.07) 0.94 (0.07) |
0.85 (0.08) 0.78 (0.07) |
0.94 (0.04) 0.90 (0.03) |
0.99 (0.04) 0.92 (0.04) |
0.87 (0.05) 0.84 (0.04) |
| Negative SRCB unadjusted mean (SE) marginal mean (SE) |
0.23 (0.03) 0.18 (0.02) |
0.35 (0.02) 0.27 (0.02)* |
0.31 (0.02) 0.24 (0.02) |
0.25 (0.03) 0.15 (0.02)* |
0.26 (0.04) 0.20 (0.03) |
0.30 (0.02) 0.23 (0.02) |
0.33 (0.03) 0.22 (0.03) |
0.27 (0.03) 0.22 (0.02) |
| Frequency of using individual SRCB Fairly/Very Often to cope with stress | ||||||||
| Alcohol unadjusted % (SE) marginal % (SE) |
6.09 (1.30) 3.61 (1.01) |
4.32 (1.07) 2.67 (0.62) |
5.60 (0.99) 3.35 (0.66) |
3.13 (1.16) 2.10 (0.85) |
2.28 (0.97) 2.40 (1.07) |
5.69 (1.00) 3.21 (0.63) |
3.30 (1.02) 2.22 (0.74) |
6.81 (1.35) 4.12 (0.93) |
| Drugs unadjusted % (SE) marginal % (SE) |
4.72 (1.25) 3.05 (0.86) |
9.80 (1.45) 5.26 (0.79) |
6.95 (1.16) 4.17 (0.78) |
9.70 (1.82) 3.89 (1.06) |
8.13 (2.39) 3.06 (1.17) |
7.36 (1.07) 4.35 (0.69) |
10.31 (1.85) 4.72 (1.05) |
4.88 (0.91) 3.62 (0.90) |
| Eating unadjusted % (SE) marginal % (SE) |
6.00 (1.42) 4.45 (1.08) |
14.81 (1.29) 11.79 (1.20)** |
11.21 (1.01) 8.41 (1.02) |
9.06 (2.45) 5.07 (1.56) |
8.44 (2.68) 6.47 (1.20) |
11.27 (0.97) 7.89 (1.07) |
11.17 (1.54) 7.35 (1.36) |
10.43 (1.24) 7.91 (1.13) |
| Smoke unadjusted % (SE) marginal % (SE) |
5.94 (1.29) 3.25 (0.92) |
6.61 (1.08) 3.77 (0.91) |
6.96 (1.13) 4.57 (1.03) |
3.56 (1.10) 1.16 (0.48)* |
7.36 (2.29) 4.66 (1.72) |
6.11 (1.12) 3.34 (0.88) |
8.03 (1.45) 4.40 (0.99) |
4.72 (1.25) 2.87 (0.96) |
| Exercise unadjusted % (SE) marginal % (SE) |
11.78 (1.75) 7.68 (1.55) |
10.41 (1.66) 7.09 (0.97) |
11.54 (1.34) 7.40 (1.02) |
8.92 (2.21) 7.16 (1.79) |
4.05 (1.16) 4.33 (1.26) |
12.43 (1.36) 8.15 (1.11)* |
6.86 (1.40) 4.98 (1.13) |
14.91 (1.66) 10.44 (1.34)* |
| Prayer unadjusted % (SE) marginal % (SE) |
43.43 (2.11) 44.88 (2.00) |
67.59 (1.85) 68.10 (1.73)** |
55.71 (1.87) 57.06 (1.78) |
60.22 (3.62) 61.46 (3.79) |
53.04 (3.77) 48.73 (3.62) |
57.31 (1.81) 59.68 (1.62)* |
62.44 (2.16) 63.43 (2.26) |
51.18 (2.29) 52.63 (2.27)* |
| Social support unadjusted % (SE) marginal % (SE) |
11.01 (1.46) 10.91 (1.44) |
25.87 (2.09) 25.13 (1.92)** |
18.25 (1.82) 16.90 (1.67) |
22.62 (2.49) 20.16 (2.87) |
18.77 (2.83) 15.45 (2.68) |
19.17 (1.60) 17.92 (1.49) |
21.80 (2.04) 19.23 (2.15) |
16.59 (1.45) 16.01 (1.36) |
| Counselor unadjusted % (SE) marginal % (SE) |
3.64 (1.05) 2.70 (0.84) |
7.82 (1.37) 5.72 (1.12)* |
5.38 (1.05) 3.98 (0.86) |
8.16 (1.92) 4.47 (1.41) |
9.15 (2.54) 6.15 (1.72) |
5.29 (0.91) 3.75 (0.81) |
7.81 (1.56) 4.86 (1.29) |
4.17 (0.97) 3.45 (0.84) |
| Perceived Effectiveness of individual SRCBs at reducing feelings of distress by Some/A Great Deal | ||||||||
| Alcohol unadjusted % (SE) marginal % (SE) |
44.95 (5.19) 42.11 (4.86) |
57.58 (3.26) 57.07 (3.56)* |
52.83 (3.79) 50.75 (4.16) |
41.77 (8.77) 41.20 (8.74) |
46.98 (8.51) 61.50 (10.16) |
51.18 (3.48) 47.12 (3.94) |
50.27 (7.83) 51.51 (7.75) |
50.91 (3.97) 47.36 (4.28) |
| Drugs unadjusted % (SE) marginal % (SE) |
53.26 (7.07) 55.40 (6.86) |
75.38 (4.61) 75.86 (4.31)* |
75.29 (3.57) 80.82 (3.29) |
42.07 (7.87) 24.41 (6.89)** |
59.34 (8.40) 73.09 (6.69) |
69.19 (4.78) 67.31 (5.17) |
68.78 (5.15) 74.79 (4.44) |
64.18 (5.60) 59.04 (6.82) |
| Eating unadjusted % (SE) marginal % (SE) |
21.34 (3.12) 22.05 (3.28) |
33.79 (3.09) 33.04 (3.02)* |
29.85 (2.81) 29.08 (2.79) |
25.89 (4.36) 26.54 (4.78) |
18.77 (4.41) 18.23 (4.55) |
30.66 (2.67) 30.40 (2.71) |
28.67 (2.66) 28.22 (2.90) |
29.65 (3.47) 29.04 (3.60) |
| Smoke unadjusted % (SE) marginal % (SE) |
39.95 (8.09) 41.91 (10.51) |
58.06 (7.35) 60.06 (7.47) |
53.98 (6.43) 54.89 (7.10) |
33.30 (4.98) 40.35 (7.97) |
41.58 (8.89) 46.46 (13.42) |
52.70 (6.52) 53.89 (6.41) |
52.94 (6.67) 59.46 (6.96) |
45.20 (8.29) 39.16 (9.84) |
| Exercise unadjusted % (SE) marginal % (SE) |
69.13 (4.65) 70.71 (4.71) |
76.69 (3.06) 78.75 (2.82) |
75.69 (2.85) 72.69 (3.02) |
61.67 (7.69) 83.46 (4.84) |
35.18 (7.60) 47.12 (9.40) |
77.98 (2.58) 77.93 (2.63)* |
59.75 (4.72) 62.28 (5.53) |
81.28 (3.17) 81.40 (3.08)* |
| Prayer unadjusted % (SE) marginal % (SE) |
75.46 (2.68) 77.45 (2.43) |
89.51 (1.61) 90.27 (1.44)** |
84.75 (1.80) 86.74 (1.70) |
80.43 (3.45) 83.73 (2.81) |
78.30 (3.70) 78.70 (4.16) |
84.92 (1.73) 87.31 (1.49)* |
85.73 (1.88) 88.15 (1.65) |
81.91 (2.45) 83.78 (2.30) |
| Social support unadjusted % (SE) marginal % (SE) |
57.86 (3.12) 57.35 (2.96) |
77.88 (2.50) 78.65 (2.50)** |
70.83 (2.20) 70.68 (2.37) |
67.14 (4.91) 73.73 (4.30) |
62.98 (6.10) 69.51 (5.06) |
71.36 (2.11) 71.64 (2.29) |
66.27 (2.30) 67.80 (2.13) |
74.23 (2.78) 74.91 (3.08)* |
| Counselor unadjusted % (SE) marginal % (SE) |
70.73 (6.02) 70.89 (5.54) |
75.08 (3.82) 76.25 (4.01) |
72.51 (3.70) 73.34 (3.90) |
76.34 (6.29) 77.08 (6.73) |
83.15 (5.02) 84.69 (5.13) |
71.63 (3.41) 71.95 (3.34)* |
74.37 (4.15) 74.47 (4.10) |
72.05 (4.49) 73.82 (4.69) |
* p<.05, **p<.0001. P-values are testing for differences in means (number of SRCBs) or proportions (frequency and perceived effectiveness) comparing across the two levels of each contextual variable (e.g., men vs. women, white vs. non-white, low vs. high education, and low vs. high wealth).
Marginal values are adjusted for age, sex (for all models but gender), race/ethnicity (for all models but race), education (for all models but education), wealth (for all models but wealth), number of chronic conditions and IALDs. Values are weighted and account for the complex sampling study design.
Non-whites were less likely to endorse using negative SRCBs, a result that was driven by smoking. Results using a three-level indicator for race (Whites, Blacks, and other non-Whites) showed similar findings (Supplemental Table 2), with the main difference in that using this categorization being that Blacks were more likely than Whites to use positive strategies (a result largely driven by social support and seeking counsel), whereas those of other non-White race were less likely than Whites to use these strategies. Blacks also reported that exercise, prayer, and social support were more effective at relieving distress relative to Whites, whereas other non-Whites generally reported that these positive strategies were less effective. Finally, higher education and wealth were related to greater endorsement of two positive SRCBs, exercise and prayer, relative to lower education and lower wealth.
Stress and SRCB
Table 4 shows the results of the Poisson regression models assessing the relationship between the stress score (and psychological distress) and count of SRCB (total, negative, and positive). Higher levels of stress were significantly associated with greater number of SRCBs, particularly for negative behaviors (i.e., smoking, alcohol). For example, for every one unit increase in stress, the number of negative SRCBs endorsed increased by a factor 1.14 (95% Confidence Interval: 1.07, 1.22). Findings were similar when using CESD as an alternative indicator of psychological distress.
Table 4.
Relationship between stressors, psychological distress, and number of SRCB.
|
Stress sum score |
Psychological distress (CESD) |
|||
|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | |
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Total SRCB | 1.08 (1.04, 1.12) | 1.07 (1.04, 1.12) | 1.13 (1.10, 1.16) | 1.11 (1.08, 1.13) |
| Positive SRCB | 1.05 (1.00, 1.09) | 1.05 (1.01, 1.10) | 1.09 (1.06, 1.12) | 1.07 (1.04, 1.10) |
| Negative SRCB | 1.17 (1.09, 1.24) | 1.14 (1.07, 1.22) | 1.25 (1.20, 1.30) | 1.21 (1.16, 1.27) |
| N | 517 | 517 | 1354 | 1354 |
Values are adjusted for age, sex, race/ethnicity, education, wealth, number of chronic conditions, and number of IALDs.
IRR: Incidence rate ratio. CI: Confidence Interval.
Estimates are weighted and account for the complex sampling design.
Turning to our exploratory analyses of moderation of the stress X SRCB relationship, there was little evidence that the relationship between stress (or CESD) and SRCB was moderated by the indicators of context (Supplemental Table 3). All the interaction terms between stress and these variables had p-values >0.15 with the exceptions of stress X education on positive SRCB (Beta=-0.077, P=0.037, indicating that the relationship between stress and positive behaviors was weaker among those with higher education). Turning to CESD, all the interaction terms were non-significant with the exception of CESD X race for total and positive SRCB (Beta=-0.063 (p=0.005) and Beta=-0.062 (p=0.035), respectively) indicating that relationship between CESD and total number and number of positive SRCBs is weaker among non-whites.
Discussion
In this paper we presented and evaluated a novel conceptualization and quantitative assessment of health behaviors as self-regulatory strategies with differential implications for mental and physical health. For our first objective, we found that the majority of older adults endorsed at least one SRCB, and that frequency of engaging in these behaviors was related to their perceived effectiveness at relieving distress. For our second objective, sex was the only proxy indicator of context examined that was consistently associated with these coping strategies, with women both more likely to engage in SRCBs and to perceive them to be effective at reducing feelings of distress than men. Finally, for our third objective examining the intersection of stress and SRCB, findings were broadly consistent with the predictions of our theoretical framework for understanding health disparities (Mezuk et al. 2013) in that higher levels of stress (or psychological distress) were associated with greater number of SRCBs, particularly those that harm physical health. This suggests that there is value in broadening both our typologies of coping, and the conceptualization of health behaviors as more than simply confounding variables, in disparities research. We discuss each of these main conclusions in turn.
One of the main innovations of this assessment of SRCB was the explicit incorporation of both stress-reduction as a motivation for engaging in the behavior and the perceived effectiveness of that behavior at relieving emotional distress. This stands in sharp contrast to most epidemiologic work on stress as a determinant of health disparities, which rarely capture the roles of stress perception, appraisal, and response in this relationship (Concha & Mezuk, 2015). We found that people tend to engage in both health-harming and health-promoting SRCBs (i.e., prayer and overeating, exercise and drinking), consistent with work on traditional approaches to coping which finds that the same people use different strategies in different situations (Lazarus & Folkman, 1984). Finally, our measure emphasizes that individuals are (or at least can be) consciously aware of explicitly using these behaviors to cope with stress, as opposed to simply engaging in the behavior without conscious awareness as to why or as merely a distraction. That stress is a motivator for engaging in behaviors that “promote” mental health via coping (even if they harm physical health) means that this connection can be used as a target for intervention to reduce the impact of stress on health (and health disparities).
For our second objective, we examined four proxy indicators of context (sex, race/ethnicity, education, and wealth) but only sex consistently moderated both the frequency and content of SRCB, with relatively modest variation by the latter three indicators. Prior work has indicated sex differences in both which experiences tend to be considered stressful and in coping styles, with women scoring higher than men on emotional and avoidance coping (Matud, 2004). This is consistent with our finding that women were more likely to endorse SRCBs, if these are conceptualized as avoidance strategies. However, these findings can be considered inconsistent with psychosocial theory which posits that because of socialization women are more likely to use expressive and emotion-focused coping behaviors relative to men (Ptacek, Smith & Dodge, 1994). If these findings are replicated in other studies, they suggest the role of sex in coping is more nuanced than currently posited. Our findings, since they address behaviors that have known consequences for physical health, may have implications for understanding trajectories of sex disparities over the life course in which women have higher risk of morbidity and disability but lower risk of mortality relative to men (Case & Paxson, 2005).
The relatively modest associations with race/ethnicity and SES indicators of context were contrary to our expectations, which were informed by documented health disparities along these dimensions. Our sensitivity analysis using the three-level indicator of race/ethnicity provided evidence that minority status is not consistently associated with greater use, or perceived effectiveness, of positive coping strategies. These results may reflect survival bias if lower educated, less wealthy, or racial/ethnic minorities were less likely to survive to be interviewed in the 2008 wave. The weak relationships between these SRCB and indicators of context may reflect a cohort effect, since these behaviors may represent patterns of coping established earlier in life. Finally, while we examined these contextual factors separately due to sample size limitations, this is not to discount the importance of the intersection of these indicators (i.e., sex and race/ethnicity) for understanding stress and coping (Cole, 2009). For example, future work should examine whether the sex differences observed here are consistent for lower and higher educated groups, as this would inform theoretical models of the sources of variation in heath behavior across socioeconomic strata.
Turning to the third objective, the EA Model posits that stress is positively associated with endorsement with SRCBs, particularly negative behaviors (e.g., alcohol, smoking, drugs, eating), and this prediction was supported using two distinct indicators of stress (i.e., a count of stressful life events and psychological distress as measured by the CESD). The finding was stronger in magnitude for the CESD measure of stress; this may reflect measurement limitations, such as more variation in this measure due to the larger sample size for this analysis, or the fact that the CESD asks about contemporaneous (i.e., past two weeks) feelings, as opposed to the stress score which asks about events in the past (including in childhood). However, it may also suggest something more fundamental about the psychological sequela of self-regulatory coping. Regardless, this finding adds to the growing body of experimental research (e.g., Chaplin et al., 2010; Childs & de Wit, 2014; Koob, 2008; Stephens & Wand, 2012; Tryon et al., 2015; Wardle et al., 2011) supporting this framework as an integrative approach to understand how stress and behaviors intersect to influence mental and physical health. That is, when it comes to understanding the role of stress as a potential cause of health disparities, researchers need to carefully consider how what role health behaviors play in this relationship; these findings demonstrate that simply adjusting for these variables as confounders is unwarranted, as they are intimately linked to the stress-coping process. Finally, it is important to acknowledge that the SRCBs can become conditioned responses that are decoupled from stress-coping efforts over time, which is hypothesized to be one etiologic pathway for substance dependence syndromes (Koob & Volkow, 2016).
These findings can also inform existing typologies of coping by suggesting a path to move beyond avoidant vs. approach strategies to explore three additional dimensions: (a) motivations and perceived effectiveness, (b) kinetics (i.e., the timeliness and half-life of perceived relief from distress), and (c) consequences of coping in terms of short-term emotional relief vs. long-term health. We could only address the first of these in the present study, but future work should explore the utility of these other aspects. Doing so requires drawing on ideas of human behavior from disciplines like neuroscience, psychology, and sociology but applying these in epidemiologic research on health disparities. For example, the results for perceived effectiveness demonstrate that not all health behaviors are equal in terms of reducing psychological distress, and that there is variation in this metric even across the crude proxies of context examined here. This variation may be informative in efforts to “personalize” public health efforts to reduce disparities along these dimensions of context (Bayer & Galea, 2015).
Findings should be interpreted in light of study limitations and strengths. Limitations included the reliance on a predominantly white sample over the age of 50, which limited our ability to examine variation by race/ethnicity (including examining variation within groups) and age. We only had data on a subset of potential SRCB (e.g., we did not assess meditation or using the internet or other media). This study also has important strengths, including the use of a nationally-representative sample and assessment of multiple indicators of stress across the life course. We explicitly tested the relationship between stress and these behaviors that heretofore had only been inferred. Finally, we drew from an interdisciplinary theoretical framework to develop a novel assessment of coping that includes perceived effectiveness of each behavior.
If stress is to be considered a primary determinant of health disparities and potential target for reducing them, these findings demonstrate a need to reorient research to address the complex relationships between stress, behavior, and context. The results here suggest some avenues to explore in future research. If stress is a primary determinant for engaging in an unhealthy diet, for example, providing more options for healthy affordable foods or nutrition education are unlikely to have a substantial impact on this behavior, consistent with the notion of constrained choice via contextual factors like the ones examined here. Instead, multi-modal efforts that leverage the emotional self-regulatory effects of positive behaviors like exercise while attempting to reduce health-harming behaviors through structural changes are worth exploring.
Acknowledgements
The Health and Retirement Study is supported by the National Institute on Aging (NIA U01AG009740) and the Social Security Administration. B. Mezuk, S. Ratliff, J.A. Rafferty, and J.S. Jackson are supported by the University of Michigan Center for Integrative Approaches to Health Disparities (P60-MD002249). B. Mezuk is also supported by grant 1-16-ICTS-082 from the American Diabetes Association and grant K01-MH093642 from the National Institute of Mental Health. The sponsors had no role in the design, analysis, or decision to publish these findings.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2017.05.004.
Appendix A. Supplementary material
Supplementary material
Supplementary material
Supplementary material
Supplementary material
Supplementary material
References
- Abdou C.M., Fingerhut A.W., Jackson J.S., Wheaton F. Healthcare stereotype threat in older adults in the health and retirement study. American Journal of Preventive Medicine. 2016;50:191–198. doi: 10.1016/j.amepre.2015.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayer R., Galea S. Public health in the precision-medicine era. The New England Journal of Medicine. 2015;373:499–501. doi: 10.1056/NEJMp1506241. [DOI] [PubMed] [Google Scholar]
- Bird C.E., Rieker P.P. Cambridge University Press; New York, NY: 2008. Gender and health: The effects of constrained choices and social policies. [Google Scholar]
- Boardman J.D., Alexander K.B. Stress trajectories, health behaviors, and the mental health of black and white young adults. Social Science & Medicine. 2011;72:1659–1666. doi: 10.1016/j.socscimed.2011.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broman C. Coping with personal problems. In: Neighbors H.W., Jackson J.S., editors. Mental health in Black America. Sage Publications; Thousand Oaks, CA: 1996. pp. 117–129. [Google Scholar]
- Case A., Paxson C. Sex differences in morbidity and mortality. Demography. 2005;42:189–214. doi: 10.1353/dem.2005.0011. [DOI] [PubMed] [Google Scholar]
- Chaplin T.M., Hong K., Fox H.C., Siedlarz K.M., Bergquist K., Sinha R. Behavioral arousal in response to stress and drug cue in alcohol and cocaine addicted individuals versus healthy controls. Human Psychopharmacology. 2010;25:368–376. doi: 10.1002/hup.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs E., de Wit H. Regular exercise is associated with emotional resilience to acute stress in healthy adults. Frontiers in Physiology. 2014;5:161. doi: 10.3389/fphys.2014.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, P., Fisher, G., House, J., Smith, J., Weir, D. (2008). Guide to content of the HRS Psychosocial Leave-Behind Participant Lifestyle Questionnaires: 2004 & 2006. 〈http://hrsonline.isr.umich.edu/sitedocs/userg/HRS2006LBQscale.pdf〉 Accessed 16 september 2001.
- Cole E.R. Intersectionality and research in psychology. American Psychologist. 2009;64:170–180. doi: 10.1037/a0014564. [DOI] [PubMed] [Google Scholar]
- Concha J.B., Mezuk B. Neighborhoods and risk of diabetes mellitus: person and place or person in place? JAMA Internal Medicine. 2015;175:2002. doi: 10.1001/jamainternmed.2015.6686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis B.J., Del Giudice M. Beyond allostatic load: Rethinking the role of stress in regulating human development. Development and Psychopathology. 2014;26:1–20. doi: 10.1017/S0954579413000849. [DOI] [PubMed] [Google Scholar]
- Geronimus, A.T. (1992). The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis, 2, 207-221. Health and Retirement Study, 2011. Sample size and response rates. Available at: 〈http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf〉. (Accessed 07 March 2017). [PubMed]
- Heeringa, S. G., and Connor, J. (1995). Technical description of the health and retirement study sample design. Retrieved from 〈http://hrsonline.isr.umich.edu/sitedocs/userg/HRSSAMP.pdf〉.
- Hilmert C.J., Schetter C.D., Dominguez T.P., Abdou C., Hobel C.J., Glynn L., Sandman C. Stress and blood pressure during pregnancy: Racial differences and associations with birthweight. Psychosomatic Medicine. 2008;70:57–64. doi: 10.1097/PSY.0b013e31815c6d96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson, J.S., and Gurin, G. (1987). National Survey of Black Americans, 1979-1980: Ann Arbor, MI: Inter-university Consortium for Political and Social Research, Institute for Social Research.
- Jackson J.S., Knight K.M., Rafferty J.A. Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health. 2010;100:933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James S.A. Epidemiologic research on health disparities: Some thoughts on history and current developments. Epidemiologic Reviews. 2009;31:1–6. doi: 10.1093/epirev/mxp010. [DOI] [PubMed] [Google Scholar]
- Keyes K.M., Barnes D.M., Bates L.M. Stress, coping, and depression: Testing a new hypothesis in a prospectively studied general population sample of U.S.-born Whites and Blacks. Social Science & Medicine. 2011;72:650–659. doi: 10.1016/j.socscimed.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob G.F. A role for brain stress systems in addiction. Neuron. 2008;59:11–34. doi: 10.1016/j.neuron.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob G.F., Volkow N.D. Neurobiology of addiction: A neurocircuitry analysis. Lancet Psychiatry. 2016;3:760–773. doi: 10.1016/S2215-0366(16)00104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause N., Shaw B.A., Cairney J. A descriptive epidemiology of lifetime trauma and the physical health status of older adults. Psychology and Aging. 2004;19:637–648. doi: 10.1037/0882-7974.19.4.637. [DOI] [PubMed] [Google Scholar]
- Krueger P.M., Chang V.W. Being poor and coping with stress: Health behaviors and the risk of death. American Journal of Public Health. 2008;98:889–896. doi: 10.2105/AJPH.2007.114454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger P.M., Saint Onge J.M., Chang V.W. Race/ethnic differences in adult mortality: The role of perceived stress and health behaviors. Social Science & Medicine. 2011;73:1312–1322. doi: 10.1016/j.socscimed.2011.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantz P.M., House J.S., Lepkowski J.M., Williams D.R., Mero R.P., Chen J. Socioeconomic factors, health behaviors, and mortality: Results from a nationally representative prospective study of US adults. Journal of the American Medical Association. 1998;279:1703–1708. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- Lazarus R.S., Folkman S. Springer; New York: 1984. Stress, appraisal and coping. [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995:80–94. [PubMed] [Google Scholar]
- Matud M.P. Gender differences in stress and coping styles. Personality and Individual Differences. 2004;37:1401–1415. [Google Scholar]
- McEwen B.S. The brain on stress: toward an integrative approach to brain, body, and behavior. Perspectives on Psychological Science. 2013;8:673–675. doi: 10.1177/1745691613506907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B.S., Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- Mezuk B., Abdou C.M., Hudson D., Kershaw K.N., Rafferty J.A., Lee H., Jackson J.S. “White Box” epidemiology and the social neuroscience of health behaviors: The environmental affordances model. Society & Mental Health. 2013;3:79–95. doi: 10.1177/2156869313480892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B., Rafferty J.A., Kershaw K.N., Hudson D., Abdou C.M., Lee H., Eaton W.W., Jackson J.S. Reconsidering the role of social disadvantage in physical and mental health: Stressful life events, health behaviors, race, and depression. American Journal of Epidemiology. 2010;172:1238–1249. doi: 10.1093/aje/kwq283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller G., Chen E., Cole S.W. Health psychology: Developing biologically plausible models linking the social world and physical health. Annual Review of Psychology. 2009;60:501–524. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- Miller G.E., Chen E., Parker K.J. Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137:959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecoraro N., Reyes F., Gomez F., Bhargava A., Dallman M.F. Chronic stress promotes palatable feeding, which reduces signs of stress: Feed forward and feedback effects of chronic stress. Endocrinology. 2004;145:3754–3762. doi: 10.1210/en.2004-0305. [DOI] [PubMed] [Google Scholar]
- Ptacek J.T., Smith R.E., Dodge K.L. Gender differences in coping with stress: When stressor and appraisals do not differ. Personality and Social Psychology Bulletin. 1994;20:421–430. [Google Scholar]
- Robert S., House J.S. SES differentials in health by age and alternative indicators of SES. Journal of Aging and Health. 1996;8:359–388. doi: 10.1177/089826439600800304. [DOI] [PubMed] [Google Scholar]
- Rosenkranz M.A., Lutz A., Perlman D.M., Bachhuber D.R., Schuyler B.S., MacCoon D.G., Davidson R.J. Reduced stress and inflammatory responsiveness in experienced meditators compared to a matched healthy control group. Psychoneuroendocrinology. 2016;68:117–125. doi: 10.1016/j.psyneuen.2016.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnega A., Faul J.D., Ofstedal M., Langa K.M., Phillips J.W.R., Weir D.R. Cohort profile: the Health and Retirement Study (HRS) International Journal of Epidemiology. 2014;43:576–585. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens M.A., Wand G. Stress and the HPA axis: Role of glucocorticoids in alcohol dependence. Alcohol Research. 2012;34:468–483. doi: 10.35946/arcr.v34.4.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S.E., Stanton A.L. Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology. 2007;3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- Tryon M.S., Stanhope K.L., Epel E.S., Mason A.E., Brown R., Medici V., Havel P.J., Laugero K.D. Excessive sugar consumption may be a difficult habit to break: A view from the brain and body. Journal of Clinical Endocrinology & Metabolism. 2015;100:2239–2247. doi: 10.1210/jc.2014-4353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner R.J., Wheaton B., Lloyd D.A. The epidemiology of social stress. American Sociological Review. 1995;60:104–125. [Google Scholar]
- Turvey C.L., Wallace R.B., Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatric. 1999;11:139–148. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- Umberson D., Liu H., Reczek C. Stress and health behaviors. In: Turner H., Schiemann S., editors. Advances in life course research: stress processes across the life course. Elsevier; Oxford, England: 2008. pp. 19–44. [Google Scholar]
- Wardle M.C., Munafo M.R., de Wit H. Effect of social stress during acute nicotine abstinence. Psychopharmacology (Berl) 2011;218:39–48. doi: 10.1007/s00213-010-2150-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Yan Y., Jackson J.S., Anderson N.B. Racial differences in physical and mental health: socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Supplementary material
Supplementary material
Supplementary material
Supplementary material