Abstract
Implant-supported dental prostheses can be retained by a screw or cement. Implant-supported fixed partial dentures have a passive fit. A passive fit means there is an internal gap between the abutment surface and the intaglio of the retainer to insure that there is no lateral pressure on the supporting implants or friction upon seating of the prosthesis. This gap is filled with cement for retention of the prosthesis. Any lateral pressure may cause marginal bone loss or periimplantitis. Also, there is usually a microscopic gap at the margin of a crown retainer that exposes the cement to oral fluids. The solubility of zinc phosphate (ZOP) cement is a definite liability due to the risk for cement dissolution. In fixed prostheses, the dissolution of the cement of one or more retainers would cause a transfer of the occlusal load to the retained unit(s). The resulting rotation and lifting of the cement-retained implants from occlusal and parafunctional loads could cause loss of osseointegration of the abutment-retained implant(s). ZOP cement may not be indicated for implant-supported fixed partial dentures or splints. Cement dissolution in single unit probably only involves re-cementation, if the patient does not swallow or aspirate the crown.
Keywords: passive fit, retention, film thickness, fixed, marginal gap
Video abstract
Introduction
Implant-supported fixed crowns and dentures may be retained by screws or cement. There are several types of cement that may be used for this. Zinc phosphate (ZOP) cement has been used in dentistry since the 1850s and is very familiar to dentists.1 ZOP, however, has been traditionally used as a definitive cement for fixed crowns and partial dentures on natural teeth. ZOP cement was made for tooth-borne fixed partial dentures and crowns. Its properties may not be suitable for passive-fit metal-to-metal cementation that is in implant prostheses. It may be an inappropriate choice for long-term retention of multiple implant-supported prostheses. The solubility of ZOP is a well-known detrimental property.2 This property may make it inappropriate for luting the metal-to-metal or metal oxide surfaces of titanium and zirconia abutments to the metal or metal oxide intaglio of crowns and retainers.
The purpose of this article is to discuss ZOP cement as a definitive luting agent for fixed implant-supported dentures and crowns. Written informed consent for treatment, photographs, and publishing has been obtained from patients for this study.
Case series
Case 1
A 54-year-old female was treated with fixed small diameter implant-supported partial denture at the mandibular right molars. The partial denture was cemented with ZOP cement (Flecks). After several years of uneventful function, the denture became loose at the mesial abutments causing an overloading of the distal implant (Figures 1 and 2). Subsequently, the distal implant fractured. The fractured implant apex was removed, a short, larger diameter implant placed, and a new fixed partial denture fabricated and cemented with a resin-modified glass ionomer (RelyX, ESPE; 3-M, Neuss, Germany). The patient has been functioning uneventfully for 5 years.
Figure 1.
The mesial abutments zinc phosphate cement dissolved, and there was subsequent overload and fracture of the distal implant.
Figure 2.

The fractured fragment was retrieved.
Case 2
A 60-year-old male was treated with a ZOP cement-retained implant-supported fixed partial denture. The denture functioned uneventfully for 5 years, but the cement failed at the mesial abutment causing the distal implant to rotate under load, loose osseointegration, and exfoliate (Figures 3 and 4). The site was retreated a new implant-supported fixed partial denture cemented with a resin-modified glass ionomer (RelyX, ESPE). The patient has now been functioning uneventfully for 7 years.
Figure 3.

The distal abutment zinc phosphate cement dissolved putting more load on the mesial implant.
Note: This caused loss of integration and exfoliation of the fixed splinted restoration.
Figure 4.
The mesial abutment was lost due to mechanical overload from the dissolution of the retaining cement of the distal abutment.
Case 3
A 59-year-old female patient had an implant placed that supported a single crown and cemented with ZOP in 2005. In 2016, the cement had dissolved and the crown dislodged. The crown and abutment were cleaned, and the crown re-cemented with resin-modified glass ionomer (RelyX, ESPE).
Discussion
There is no consensus as to the most appropriate cement for implant restorations.3,4 There are even variations of preference in and among dental schools.3,4 Nonetheless, dental schools most often choose resin-modified glass ionomer cement (57%) but ZOP is still chosen for ~19% of cementations. ZOP, among other cements, is still being taught in 70% of dental schools and in advanced education programs.3,4 According to one survey, only 2% of private practice clinical dentists use ZOP to retain implant crowns.5 The practical experience of clinicians may be the reason for such a discrepancy.
ZOP is mixed as a powder component incorporated into a liquid component. ZOP should be mixed for low viscosity for definitive cementation and high viscosity for provisional cementation (ANSI-ADA Spec 8).6 The maximum ZOP film thickness should be 25 μm for crown cementation. After 2 minutes of mixing, the cement viscosity will increase dramatically. The ZOP setting time is 5–9 minutes at 37°C. Setting time will be shortened if there is rapid powder incorporation.3 Mixing of ZOP is an exothermic reaction. Thus, incremental slow mixing is done to increase the setting time and prevent excessive heat generation. Slow mixing delays the exothermic reaction. Mixing on a cooled glass slab increases the setting time and allows incorporation of more powder producing a set cement with better retentive and compressive qualities. Adding water to the mix, intentionally or through condensation on the cooled slab, will shorten setting time.3
ZOP shrinks slightly with setting. Any water contact will cause the set cement to swell but this is followed b ~0.05% shrinkage up to 7 days later. Approximately 0.3% shrinkage will occur if setting occurs in air. While the cement is very acidic during mixing, neutrality is reached after ~48 hours. ZOP is a good thermal and electrical insulator, but this is decreased under clinical moisture conditions.3
The main constituent of ZOP powder is zinc oxide, with smaller amounts of magnesium oxide, silicon dioxide, boron oxide, barium oxide and sulfate, and calcium oxide. Tin fluoride may be an additive in some brands for potential chronic fluoride release. The cement liquid comprised aqueous ~50% phosphoric acid with buffering compounds in minor amounts.3
Basically, the mixing reaction is that zinc oxide reacts with phosphoric acid to form ZOP:
After 24 hours, the compressive strength of set ZOP is 80–140 MPa. Most of the final compressive strength is reached at 1 hour after mixing.
ZOP cement has moderately good natural tooth abutment retention when tested for pull-out retention.7 A thin film thickness and an intimate fit of the retainer to a natural tooth is desirable, and the thin ZOP cement film has good retention for crowns on natural teeth.7
ZOP does not perform well as a provisional cement to seal an endodontic access opening.8
Sand blasting of the intaglio of the retainers and abutments, occlusal taper, and cutting internal grooves in the surfaces may increase the retentiveness of ZOP as well as other cements.9
ZOP is generally mixed by hand, which creates variability in the resultant product and its properties.10 Under laboratory conditions, ZOP may easily disintegrate compared to other types of cements.11 Nonetheless, oral conditions may be much less stressful than laboratory conditions.
A systematic review of the clinical failures of restorations retained with ZOP, glass ionomer, resin, and zinc oxide eugenol (ZOE) cements found that the ZOP restorations lost retention most often with the exception of those cemented with ZOE.12
In implant fixed prosthodontics, an intimate fit of the retainer in fixed partial dentures is not desirable.13 A passive fit is more appropriate so there is no lateral frictional force against the supporting implants from tight fitting crown retainers (Figure 5). A passive fit means there is no axial abutment friction or pressure of the retaining crowns. Inter-implant abutment friction or pressure may induce marginal bone loss by pressing the supporting implant fixture against the encasing bone.13 The pressing implant may induce pressure necrosis of the surrounding bone especially the cervical bone and induce periimplantitis.13 Thus the intaglio of the retaining crowns should not press against the inter-implant axial walls of the abutments. A passive fit is attained by fabricating a space between the intaglio of the retainer surface and the abutment surface (Figure 5). This space may minimize the retention quality of ZOP cement. Because the optimal film thickness of ZOP is 25 microns this space will cause the set ZOP to be much thicker and thus reduce the functional qualities of the ZOP.14
Figure 5.
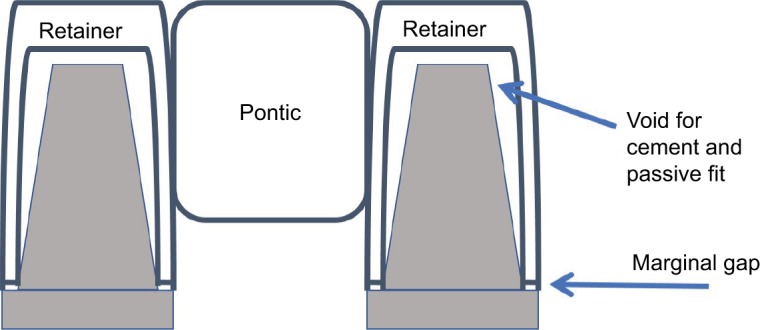
Implant-supported fixed restorations are fabricated for a passive fit.
Notes: This means there is no binding of the retainer intaglio against the abutment surface. Also, there would be a space between the intaglio of the retainer and the abutment surface. The interceding space and any marginal gap may expose the cement to oral fluids and result in dissolution of a soluble cement. If the cement does dissolve under one abutment and the other retainer is held by the cement, there may be an overload of the other supporting implant. This may cause a loss of integration.
The powder-to-liquid ratio of ZOP significantly can influence the amount of marginal cement excess.15 Nonetheless ZOP is the easiest to remove from titanium abutments compared to many cements.15
A beneficial point of ZOP is its radio-opacity that enables scrupulous excess removal.16 It is dramatically more radio-opaque than any of the resin cements.16 In fact, many resin cements are not detectable on radiographs.16 However, zinc oxide cements, eugenol or noneugenol containing, are more radio-opaque than ZOP.16
ZOP can have very effective retention properties especially when the abutment is sandblasted with 5 μm aluminum oxide.17 Nonetheless, the brittle nature of ZOP may not make it to be the most appropriate definitive cement for implant-supported prostheses.3,4
The acceptable maximal marginal gap for crowns and retainers on implant abutments is 250 μm. This generally means that there may be an open margin between the crown margin and the abutment margin. This gap allows salivary fluids access to the cement. Since there is a fabricated built-in intaglio space for a passive fit, there can be cement dissolution over time. The space may allow more and continuous fluid access to the cement as it dissolves. The loss of cement retention will result in a loose abutment. One loose abutment in a multiple unit fixed partial denture will place more load and rotation on the remaining cemented units, thus risking loss of integration.
Cement dissolution may only be important in multiple unit fixed partial dentures. Cement dissolution in single units only involves re-cementation, if the patient does not swallow or aspirate the crown. Since ZOP is soluble in water, it can erode over time from the crown margins.2 Thus, over time a crown retainer is at risk for dislodging. ZOP does not seal margins of zirconia implant crown retainers as well as resin cement does.18,19 Thus, ZOP may not be appropriate for zirconia implant crowns.
The retention of all cemented crowns on implant abutments is influenced by the number and position of abutment axial walls, which increases retention of fixed prostheses.20 The more abutments in parallel but out-of-linear position then the more retention.21 Increased abutment height adds to retention, but the type of cement effects retention more than abutment height.22
Resin cement may favor the development of suppuration and the growth of periodontal pathogens more than some other cements.23 Since ZOP is soluble, this may make it less likely to induce periimplantitis since it would be dissolved by intrasulcular fluids before any detrimental effects can occur. Resin cement is the most retentive cement, but ZOP is more retentive than glass ionomer and eugenol cements in implant-supported prostheses.14,24
Conclusion
Because implant-supported fixed partial dentures have a passive fit, there is a necessary gap between the abutment and intaglio of the retainer to prevent a push against the supporting implants. A thin film thickness is desirable for ZOP retention on natural teeth, but this is not the case with implant-supported abutments. Because there is a metal-to-metal internal and marginal gaps, the solubility of ZOP is a liability. The gap exposes the cement to oral fluids. If ZOP is used as a definitive cement in multiple unit implant-supported fixed partial dentures, there is a risk for ZOP cement dissolution. The dissolution of the cement of one or more retainers in a multiple unit fixed partial denture would cause a transfer of the occlusal load to the remaining retained units. There would also be rotational force of the cement-retained implants so the occlusal and parafunctional loads would be borne by the abutment-retained implants. Thus, there would be a substantial risk for detrimental rotation, overloading, and loss of integration. ZOP may not be indicated for implant-supported fixed partial dentures or splints. Cement dissolution in single units probably only involves re-cementation, if the patient does not swallow or aspirate the crown. These case reports are not high credibility evidence. There are better contemporary cements than ZOP as a definitive cement for dental implant-fixed prostheses. Randomized blinded controlled testing is required for definitive evidence.
Footnotes
Disclosure
The author reports no financial or conflicts of interest in this work and in any product mentioned herein.
References
- 1.Horn HR. The cementation of crowns and fixed partial dentures. Dent Clin North Am. 1965;23:65–81. [PubMed] [Google Scholar]
- 2.Dupuis V, Laviole O, Potin-Gautier M, Castetbon A, Moya F. Solubility and disintegration of zinc phosphate cement. Biomaterials. 1992;13(7):467–470. doi: 10.1016/0142-9612(92)90168-n. [DOI] [PubMed] [Google Scholar]
- 3.Chapter 4: Implant luting cements. In: Wadhwani CPK, editor; Wadhwani CPK, Schwedhelm ER, Tarica DY, Chung K-H, editors. Cementation in Dental Implantology – An Evidence Based Guide. New York: Springer; 2015. pp. 47–82. [Google Scholar]
- 4.Chapter 5: Residual excess cement detection. In: Wadhwani CPK, editor; Wadhwani CPK, Schwedhelm ER, Tarica DY, Chung K-H, editors. Cementation in Dental Implantology – An Evidence Based Guide. New York: Springer; 2015. pp. 83–99. [Google Scholar]
- 5.Christensen GJ. Implant cements: avoiding failure and creating success. Clin Rep. 2016;9(9):3–4. [Google Scholar]
- 6.American National Standards Institute [homepage on the Internet] ADA Specification 8. [Accessed June 9, 2016]. Available from: https://ANSI.org.
- 7.Garg P, Gupta G, Prithviraj DR, Pujari M. Retentiveness of various luting agents used with implant-supported prostheses: a preliminary in vitro study. Int J Prosthodont. 2013;26(1):82–84. doi: 10.11607/ijp.2572. [DOI] [PubMed] [Google Scholar]
- 8.Aledrissy HI, Abubakr NH, Ahmed Yahia N, Eltayib Ibrahim Y. Coronal microleakage for readymade and hand mixed temporary filling materials. Iran Endod J. 2011;6(4):155–159. [PMC free article] [PubMed] [Google Scholar]
- 9.Lewinstein I, Block L, Lehr Z, Ormianer Z, Matalon S. An in vitro assessment of circumferential grooves on the retention of cement-retained implant-supported crowns. J Prosthet Dent. 2011;106(6):367–372. doi: 10.1016/S0022-3913(11)60149-2. [DOI] [PubMed] [Google Scholar]
- 10.McKenna JE, Ray NJ, McKenna G, Burke FM. The effect of variability in the powder/liquid ratio on the strength of zinc phosphate cement. Int J Dent. 2011;2011:679315. doi: 10.1155/2011/679315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gemalmaz D, Pameijer CH, Latta M, Kuybulu F, Alcan T. In vivo disintegration of four different luting agents. Int J Dent. 2012;2012:831508. doi: 10.1155/2012/831508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wittneben JG, Millen C, Brägger U. Clinical performance of screw-versus cement-retained fixed implant-supported reconstructions—a systematic review. Int J Oral Maxillofac Implants. 2014;29(suppl):84–98. doi: 10.11607/jomi.2014suppl.g2.1. [DOI] [PubMed] [Google Scholar]
- 13.Sangeetha A, Padmanabhan TV, Subramaniam R, Ramkumar V. Finite element analysis of stresses in fixed prosthesis and cement layer using a three-dimensional model. J Pharm Bioallied Sci. 2012;4(suppl 2):S384–S389. doi: 10.4103/0975-7406.100291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pattanaik BK, Nagda SJ. An evaluation of retention and marginal seating of Ni-Cr alloy cast restorations using three different luting cements: an in vitro study. Indian J Dent Res. 2012;23(1):20–25. doi: 10.4103/0970-9290.99032. [DOI] [PubMed] [Google Scholar]
- 15.Behr M, Spitzer A, Preis V, Weng D, Gosau M, Rosentritt M. The extent of luting agent remnants on titanium and zirconia abutment analogs after scaling. Int J Oral Maxillofac Implants. 2014;29(5):1185–1192. doi: 10.11607/jomi.3523. [DOI] [PubMed] [Google Scholar]
- 16.Wadhwani C, Hess T, Faber T, Piñeyro A, Chen CS. A descriptive study of the radiographic density of implant restorative cements. J Prosthet Dent. 2010;103(5):295–302. doi: 10.1016/S0022-3913(10)60062-5. [DOI] [PubMed] [Google Scholar]
- 17.Al Hamad KQ, Al Rashdan BA, Abu-Sitta EH. The effects of height and surface roughness of abutments and the type of cement on bond strength of cement-retained implant restorations. Clin Oral Implants Res. 2011;22(6):638–644. doi: 10.1111/j.1600-0501.2010.02011.x. [DOI] [PubMed] [Google Scholar]
- 18.Schäfer L, Winkler C, Brandl G, Eckl S, Preis V, Behr M. The impact of luting agents and stiffness of implant-abutments on marginal adaptation, chipping, and fracture resistance of zirconia crowns. J Mech Behav Biomed Mater. 2014;39:279–291. doi: 10.1016/j.jmbbm.2014.07.021. [DOI] [PubMed] [Google Scholar]
- 19.Rungruanganunt P, Kelly JR. Insights into “bonding” of all-ceramics influenced by cement, sandblasting and water storage time. Dent Mater. 2012;28(9):939–944. doi: 10.1016/j.dental.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Tan KM, Masri R, Driscoll CF, Limkangwalmongkol P, Romberg E. Effect of axial wall modification on the retention of cement-retained, implant-supported crowns. J Prosthet Dent. 2012;107(2):80–85. doi: 10.1016/S0022-3913(12)60028-6. [DOI] [PubMed] [Google Scholar]
- 21.Mayanagi G, Igarashi K, Washio J, Nakajo K, Domon-Tawaraya H, Takahashi N. Evaluation of pH at the bacteria-dental cement interface. J Dent Res. 2011;90(12):1446–1450. doi: 10.1177/0022034511423392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Worni A, Gholami H, Marchand L, Katsoulis J, Mericske-Stern R, Enkling N. Retrievability of implant-supported crowns when using three different cements: a controlled clinical trial. Int J Prosthodont. 2015;28(1):22–29. doi: 10.11607/ijp.4119. [DOI] [PubMed] [Google Scholar]
- 23.Korsch M, Marten S-M, Dötsch A, Jáuregui R, Pieper DH, Obst U. Effect of dental cements on peri-implant microbial community: comparison of the microbial communities inhabiting the peri-implant tissue when using different luting cements. Clin Oral Implants Res. 2016;27(12):e161–e166. doi: 10.1111/clr.12582. [DOI] [PubMed] [Google Scholar]
- 24.Güncü MB, Cakan U, Canay S. Comparison of 3 luting agents on retention of implant-supported crowns on 2 different abutments. Implant Dent. 2011;20(5):349–353. doi: 10.1097/ID.0b013e318225f68e. [DOI] [PubMed] [Google Scholar]


