Abstract
Background
So far, it has not yet been studied whether socioeconomic status is associated with distinct frailty components and for which frailty component this association is the strongest. We aimed to examine the association between socioeconomic status and frailty and frailty components. In addition we assessed the mediating effect of the number of morbidities on the association between socioeconomic status and other frailty components.
Methods
This is a cross-sectional study of pooled data of The Older Persons and Informal Caregivers Survey Minimum DataSet in the Netherlands among community-dwelling persons aged 55 years and older (n = 26,014). Frailty was measured with a validated Frailty Index that consisted of 45 items. The Frailty Index contained six components: morbidities, limitations in activities of daily living (ADL), limitations in instrumental ADL (IADL), health-related quality of life, psychosocial health and self-rated health. Socioeconomic indicators used were education level and neighbourhood socioeconomic status.
Results
Persons with primary or secondary education had higher overall frailty and frailty component scores compared to persons with tertiary education (P < .001). Lower education levels were most consistently associated with higher overall frailty, more morbidities and worse self-rated health (P < .05 in all age groups). The strongest association was found between primary education and low psychosocial health for persons aged 55–69 years and more IADL limitations for persons aged 80+ years. Associations between neighborhood socioeconomic status and frailty (components) also showed inequalities, although less strong. The number of morbidities moderately to strongly mediated the association between socioeconomic indicators and other frailty components.
Conclusion
There are socioeconomic inequalities in frailty and frailty components. Inequalities in frailty, number of morbidities and self-rated health are most consistent across age groups. The number of morbidities a person has play an important role in explaining socioeconomic inequalities in frailty and should be taken into account in the management of frailty.
Introduction
Frailty can be defined as a state of increased vulnerability to external stressors and adverse outcomes such as death and hospitalization[1, 2]. Frailty is a better predictor of adverse outcomes than age[3]. Hence, it is important to identify persons or groups at risk of developing frailty in order to target prevention strategies. Older persons with a low socioeconomic status (SES) are more frail and become more frail over time compared to persons with a high SES[4–6]. Many indicators of SES such as education level, occupation, income and wealth have been linked to frailty[4, 7–9].
A widely used approach to measure frailty is the accumulation-of-deficits approach that results in a Frailty Index (FI)[10, 11]. The FI is calculated by adding up the number of health deficits a person has, divided by the total of possible health deficits included in the index. Theou et al. found that of eight commonly use frailty scales, the FI most accurately predicted mortality[12]. A standard procedure to construct a FI was developed by Searle et al., who recommended to include the following components in the index: morbidities, disability in Activities of Daily Living (ADL) and Instrumental ADL (IADL), restricted activity, impairments in general cognition and physical performance, psychological health and self-rated health (SRH)[13]. In addition to the study of ‘overall’ frailty, the assessment of frailty components could uncover important information about the specific domain in which a person is frail. Recently, Yang et al. have studied the associations of frailty components with mortality and found that IADL and ADL limitations played a greater role in mortality compared to other components[14].
It is not yet studied which frailty component contributes most strongly to socioeconomic inequalities in frailty. By uncovering this, interventions could be directed towards narrowing the gap in frailty between persons with a higher versus a lower SES. In the FI approach and other frailty measures such as the FRAIL scale, morbidities are considered as part of frailty[2, 12]. Theoretically morbidities precede the other frailty components of the FI, as proposed in different health models[15, 16]. Having certain morbidities at a younger age, such as depression or cardiovascular disease, could lead to an increase in ADL and/or IADL limitations at older age[17]. Studies using Fred’s frailty phenotype have showed that both number and specific morbidities such as obesity partly explained why persons with a lower SES were more frail compared to persons with a higher SES[9, 18]. Therefore we hypothesize that the presence of morbidities could mediate the association between SES and other components of the FI.
The aim of this study was, 1) to assess the association between SES indicators and a) ‘overall’ frailty and b) the distinct frailty components (morbidities, ADL, IADL, health-related quality of life (HRQoL), psychosocial health and SRH), and 2) to assess whether and to what extent the number of morbidities mediates the association between SES and the other frailty components (ADL, IADL, HRQoL, psychosocial health and SRH).
Methods
Study design and population
We applied a cross-sectional study design using data from The Older Persons and Informal Caregivers Survey Minimum DataSet (TOPICS-MDS)[19]. TOPICS-MDS is a data-base designed to capture information on the well-being of older persons in the Netherlands. TOPICS-MDS was developed to collect uniform information from studies funded under the National Care for older citizens Programme[20]. Included survey items were based on the recommendations of experts who identified key outcomes in older persons’ health[19]. Data were collected between 2010 and 2013 in 50 studies in the Netherlands. TOPICS-MDS consists of pooled data of these studies which differ across study design, sampling framework, and inclusion criteria. TOPICS-MDS is a fully anonymized data set, and therefore this analysis was exempt from ethical review (Radboud University Medical Centre Ethical Committee review reference number: CMO: 2012/120).
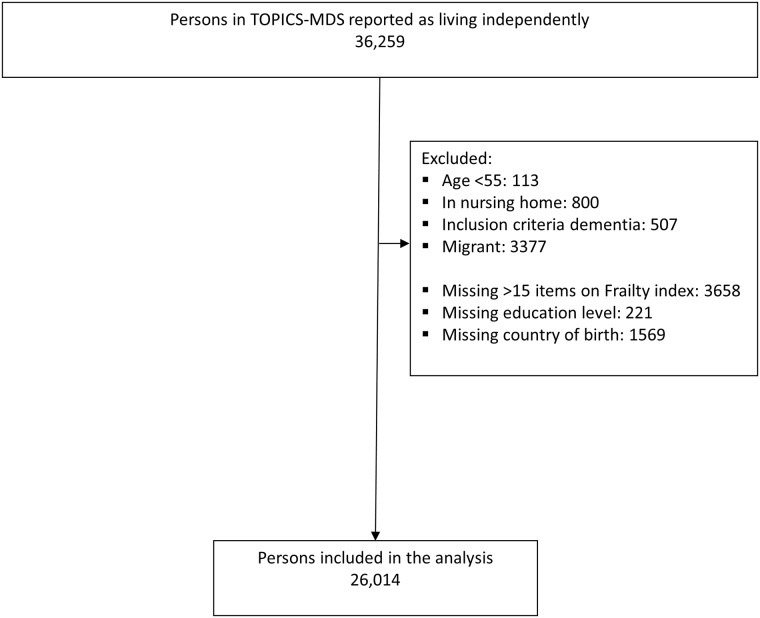
Our analysis was restricted to data from independently living Dutch persons aged 55 years and older. We further excluded persons with more than 15 missing items for the FI (n = 3658), missing education level (n = 221) or country of birth (n = 1569). The final sample comprised of data from 30 studies of 26,014 persons (see Fig 1).
Fig 1. Population of analysis.
Frailty and components
Frailty was measured by the TOPICS-Frailty Index (TOPICS-FI), which was developed and validated using TOPICS-MDS data by Lutomski et al.[21]. In our study we included the 45 item TOPICS-FI, after exclusion of the item measuring prostatism. Searle et al. showed that a FI with 30–40 variables is accurate for predicting adverse outcomes[13, 22]. The TOPICS-FI was calculated when at least 30 items were available. This was done by adding up the number of health deficits a person reported, divided by the total health deficits measured for this person, following Searle et al.[13]. This resulted in a score between 0–1, where higher scores represent higher frailty.
The TOPICS-FI as used in this study consists of 45 items that belong to six components, each measured by validated instruments; morbidities, ADL, IADL, HRQoL, psychosocial health and SRH[13]. The component ‘Morbidities’ was measured by 16 items regarding the self-reported presence (yes/no) of diabetes, stroke, heart failure, cancer, respiratory condition (asthma, chronic bronchitis, lung emphysema or Chronic obstructive pulmonary disease (COPD), incontinence, joint damage of hips or knees, osteoporosis, hip fracture, fractures other than hip, dizziness with falling, depression, anxiety/panic disorder, dementia, hearing problems, vision problems. The component ‘ADL limitations’ was measured by 6 items using a modified version of the Katz instrument[23, 24]. Persons could indicate whether they needed help (yes/no) with the following activities: bathing, dressing, toileting, incontinence, sitting down, eating. The component ‘IADL limitations’ was measured by 9 items using a modified version of the Katz instrument[23, 24]. Persons could indicate whether they needed help (yes/no) with the following activities: using the telephone, travelling, shopping, preparing a meal, cleaning, taking medications, handling finance, brushing hair and walking. The component ‘HRQoL’ was measured by 6 items of the EuroQol 5D+C[25]. Persons could indicate whether they had problems (no/some/extreme) with the following: mobility, self-care, usual activities, pain/discomfort, anxiety/depression and cognition. The component ‘Psychosocial health’ was measured with 5 items of the RAND-36 [26]. Persons could indicate how much of the time in the past month (none/a little/ some/a good bit/most/all) they had been the following: nervous, calm, downhearted, happy and down in the dumps, and how much time (none/a little/some/most/all) health problems had interfered with social activities. The component ‘SRH’ was measured with 2 items of the RAND-36[26], one regarding perceived current health status (poor/fair/good/very good/excellent) and one regarding perceived changes in health in the past year (much worse/slightly worse/about the same/a little better/much better). The score for each component of the TOPICS-FI were calculated analogous to the FI, by adding up the health deficits within the FI component that a person had, divided by the total of possible health deficits included in the component[13]. This resulted in a score between 0–1, where higher scores represent worse health. We accepted no missing variables for SRH and a maximum of 1 of 3 missing variables for other FI component scores.
Indicators of SES
In this study we applied two indicators of SES; education level and neighbourhood SES. TOPICS-MDS used the 1997 International Standard Classification of Education[27] to assess education level; participants were asked whether they had completed: fewer than 6 years of primary school; 6 years of primary school; further uncompleted education; vocational school; secondary professional education or university entrance level or tertiary education. We categorized the education level into “primary education or less”, “secondary education” and “tertiary education or higher”, based on the definition by Statistics Netherlands[28].
For the neighbourhood SES, the 2006 reference scores for area codes were used, as calculated by The Netherlands Institute for Social Research[29] based on the education level, income and labor market position of persons living in each area code. Scores were categorized into quartiles, quartile 1 is the least deprived quartile (high education, high income, high labor market position), while quartile 4 is the most deprived.
Potential confounders
Gender, age, living arrangement, marital status and level of urbanization were incorporated as potential confounders in this study based on literature and availability in TOPICS-MDS. Age was assessed by asking year of birth. Living arrangement was assessed by asking whether participants were living: independent alone, independent with others, care or nursing home. Only persons living independently were included and categorized into “not alone” and “alone”. Marital status was assessed by asking whether participants were: married, divorced, widowed, unmarried, long term cohabitation unmarried. Answers were categorized into “married/cohabitant partners”, “divorced”, “widowed” and “single”. Level of urbanization was based on the density of addresses in an area code and categorized as by Statistics Netherlands into “not urban”, “little urban”, “somewhat urban”, “urban” and “very urban”[30].
Statistical analysis
The statistical significance of differences in socio-demographic characteristics, frailty and frailty components (morbidities, ADL limitations, IADL limitations, psychosocial health, HRQoL and SRH) among persons from different education levels was calculated using chi-squared tests for categorical variables and one-way ANOVA for continues variables.
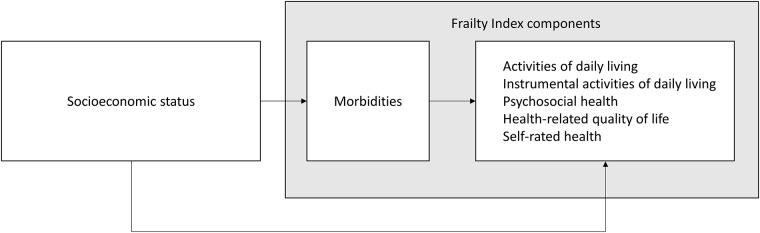
To examine the association between SES, frailty and frailty components (Model 1), we estimated multilevel random-intercept models because data were clustered in studies[31]. As such, dependency between the observations of participants of a study because of sampling design and/or inclusion criteria, was taken into account. Only potential confounders that led to a substantial change in effect estimates (i.e. ≥10% change) were included in models[32]. Subsequently, we examined the presence of mediation by the number of morbidities in the association between SES and other frailty components, by following the causal step approach proposed by Baron and Kenny (Fig 2)[33]. When SES indicators were significantly associated with the morbidities component and when the morbidities component was significantly associated with the other frailty components, the morbidities component was considered a ‘true’ mediator. Only then, the morbidities component was added to Model 1 (Model 2). To assess the mediating effect, the percentages of attenuation of effect estimates were calculated by comparing Model 2 relative to Model 1.
Fig 2. Conceptual framework for the association between socioeconomic status and Frailty Index components, where the morbidities component mediates the association between socioeconomic status and other Frailty Index components.
We explored the presence of interaction between the indicators of SES and sex, age and living arrangement in the association between SES and frailty and frailty components. We also explored interaction between the indicators of SES and morbidities (exposure-mediator interaction) in the association between SES and frailty and frailty components. After applying Bonferroni correction for multiple testing[34], we found significant interactions between SES and age on overall frailty and on all frailty components, and therefore stratified all analyses by age in three groups: 55–69 years, 70–79 years, and 80 years and older.
Percentages of missing values in the potential confounders were 2% or less (Table 1). Missing data on potential confounders were imputed using multiple imputation. We computed five imputation datasets using a fully conditional specified model[35]. Pooled estimates from these datasets were used to report regression coefficients and 95% confidence intervals (CIs). We considered a p-value of .05 or lower to be statistically significant for main analyses and used Bonferroni correction for testing interactions[34]. Descriptive analyses were performed using SPSS version 23.0 (IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp). Multilevel linear regression analysis were performed using R-3.3.2.
Table 1. Socio-demographic characteristics and frailty outcomes by education level of 26,014 persons of The Older Persons and Informal Caregivers Survey Minimum DataSet (TOPICS-MDS).
| Total N = 26,014 |
Education level | P-value* | |||
|---|---|---|---|---|---|
| Tertiary N = 2723 |
Secondary N = 14,762 |
Primary or less N = 8529 |
|||
| Age in years (mean, SD) | 78.0 (6.8) | 76.1 (7.1) | 77.7 (6.7) | 79.3 (6.7) | <0.001 |
| Sex, N (%) | <0.001 | ||||
| Male | 10,825 (41.6) | 1800 (66.1) | 6394 (43.3) | 2631 (30.8) | |
| Female | 15,189 (58.4) | 923 (33.9) | 8268(56.7) | 5898 (69.2) | |
| Living arrangement, N (%) | <0.001 | ||||
| Alone | 11,689 (44.9) | 860 (31.6) | 6377 (43.2) | 4452 (52.2) | |
| With others | 14,325 (55.1) | 1863 (68.4) | 8385 (56.8) | 4077 (47.8) | |
| Marital status, N (%) | <0.001 | ||||
| Married/Cohabitant partners | 13,954 (53.6) | 1836 (67.4) | 8261 (56.0) | 3857 (45.2) | |
| Divorced | 1562 (6.0) | 189 (7.0) | 878 (5.9) | 494 (5.8) | |
| Widowed | 9288 (35.7) | 491 (18.0) | 4940 (33.5) | 3857 (45.2) | |
| Single | 1211 (4.7) | 206 (7.6) | 684 (4.6) | 321 (3.8) | |
| Neighbourhood SES, N (%) | <0.001 | ||||
| First quartile | 7277 (28.5) | 1298 (48.2) | 4369 (30.1) | 1610 (19.4) | |
| Second quartile | 6988 (27.4) | 649 (24.1) | 4012 (27.7) | 2327 (28.0) | |
| Third quartile | 5259 (20.6) | 427 (15.9) | 2958 (20.4) | 1874 (22.6) | |
| Fourth quartile | 5970 (23.4) | 320 (11.9) | 3165 (21.8) | 2485 (30.0) | |
| Level of urbanization, N (%) | <0.001 | ||||
| Not urban | 5802 (22.3) | 592 (21.7) | 3232 (21.9) | 1978 (23.2) | |
| Little urban | 7031 (27.0) | 578 (21.2) | 4177 (28.3) | 2277 (26.7) | |
| Somewhat urban | 4114 (15.8) | 637 (23.4) | 2410 (16.3) | 1067 (12.5) | |
| Urban | 6313 (24.3) | 704 (25.9) | 3497 (23.7) | 2112 (24.8) | |
| Very urban | 2754 (10.6) | 213 (7.8) | 1445 (9.8) | 1096 (12.8) | |
| Overall Frailty mean FI (SD)† | 0.20 (0.12) | 0.16 (0.11) | 0.20 (0.12) | 0.23 (0.13) | <0.001 |
| Morbidities, mean FI (SD)† | 0.17 (0.12) | 0.14 (0.11) | 0.16 (0.12) | 0.18 (0.13) | <0.001 |
| Number morbidities, mean (SD) | 2.61 (1.90) | 2.16 (1.69) | 2.55 (1.87) | 2.88 (1.98) | <0.001 |
| ADL limitations, mean FI (SD)† | 0.11 (0.19) | 0.08 (0.17) | 0.11 (0.19) | 0.13 (0.20) | <0.001 |
| Number ADL limitations, mean (SD) | 0.65 (1.10) | 0.47 (0.97) | 0.62 (1.08) | 0.78 (1.16) | <0.001 |
| IADL limitations, mean FI (SD)† | 0.21 (0.24) | 0.14 (0.21) | 0.20 (0.23) | 0.26 (0.25) | <0.001 |
| Number IADL limitations, mean (SD) | 1.48 (1.67) | 0.96 (1.47) | 1.39 (1.62) | 1.81 (1.74) | <0.001 |
| Psychosocial health, mean FI (SD)† | 0.26 (0.18) | 0.22 (0.16) | 0.25 (0.17) | 0.28 (0.19) | <0.001 |
| Health-related quality of life, mean FI (SD)† | 0.22 (0.17) | 0.18 (0.16) | 0.21 (0.17) | 0.25 (0.17) | <0.001 |
| Self-rated Health, mean FI (SD)† | 0.58 (0.17) | 0.54 (0.17) | 0.57 (0.17) | 0.60 (0.17) | <0.001 |
* P-values are based on Chi-squared test for categorical variables and one-way ANOVA for continues variables.
† Mean FI = mean number of health deficits reported/total health deficits measured in instrument; score between 0–1 where higher scores represent worse health. Missing N (%) for variables: Age = 544 (2%); sex = 8 (<1%); living arrangement = 0 (0%); marital status = 50 (<1%); Neighbourhood SES = 520 (2%); Level of urbanization = 199 (1%); morbidities = 531 (2%); ADL = 45 (<1%); IADL = 124 (<1%); psychosocial health = 281 (1%); Health-related quality of life = 521 (2%); Self-rated health = 100 (<1%). FI = frailty index; (I)ADL = (instrumental) activities of daily living; SES = socioeconomic status.
Non-response analysis
A comparison of persons included in the study (N = 26,014) with persons not included due to missing values for education level, FI and/or country of birth (N = 5448) did not indicate significant differences in terms of sex (p = .882) and living arrangement (p = .113). However, excluded persons were older (p < .001), more often single (p < .05), more often living in rural areas and in deprived neighbourhoods (p < .001) than persons included in the study.
Results
Table 1 shows the characteristics of the study population. Of all persons, 10.5% of the persons had tertiary education, and 32.8% had primary education or less. Compared with persons who received tertiary education, persons who received primary education or less were older, more often female, more often living alone, more often widowed and less often married, single or divorced and more often living in deprived neighbourhoods (P < .001). Frailty was highest in persons who received primary education or less (mean = 0.23; SD = 0.13), followed by persons who received secondary education (mean = 0.20; SD = 0.12) and persons who received tertiary education (mean = 0.16; SD = 0.11).
Education level was significantly associated with frailty; frailty was higher in persons of all age groups with secondary and primary or less education as compared to persons with tertiary education (p < .05; Table 2-Model 1). This was also found for the frailty components morbidities and SRH. Persons with lower education levels generally had higher scores (i.e. worse health) for IADL limitations, psychosocial health and HRQoL, although not significant in all age groups for secondary education. ADL limitations were only worse in persons aged 70–79 years with primary education or less compared to persons with tertiary education (p < .05). Among all frailty components, the association between education level and psychosocial health was strongest in persons aged 55–69 years, while for persons aged 80+ years this was IADL limitations. For frailty and all frailty components except IADL limitations, stronger associations were observed in persons aged 55–69 compared to older age groups. The number of morbidities mediated the association between education level and other frailty components, attenuations ranged between 19% and 80% (Table 2-Model 2).
Table 2. Association of education level with overall frailty and with its six components (Model 1) and change in association of education level with the five other frailty components after adjustment for the morbidities component (Model 2); stratified by age group among 26,014 persons of The Older Persons and Informal Caregivers Survey Minimum DataSet (TOPICS-MDS).
| Overall Frailty | Morbidities | ADL limitations | IADL limitations | Psychosocial health | Health-related quality of life | Self-rated health | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B (95% CI) | B (95% CI) | B (95% CI) | %† | B (95% CI) | %† | B (95% CI) | %† | B (95% CI) | %† | B (95% CI) | %† | |
| Model 1 | ||||||||||||
| Age 55–69 years | ||||||||||||
| Secondary education | 0.016** | 0.019*** | 0.007 | 0.005 | 0.016 | 0.020* | 0.028** | |||||
| (0.005–0.026) | (0.008–0.030) | (-0.008–0.022) | (-0.013–0.023) | (-0.003–0.036) | (0.003–0.038) | (0.011–0.046) | ||||||
| ≤ Primary education | 0.047*** | 0.052*** | 0.013 | 0.034** | 0.074*** | 0.056*** | 0.064*** | |||||
| (0.035–0.059) | (0.039–0.064) | (-0.005–0.030) | (0.013–0.055) | (0.051–0.096) | (0.036–0.076) | (0.044–0.085) | ||||||
| Age 70–79 years | ||||||||||||
| Secondary education | 0.007* | 0.008** | -0.002 | 0.011* | 0.006 | 0.005 | 0.016*** | |||||
| (0.001–0.013) | (0.002–0.014) | (-0.010–0.007) | (0.000–0.021) | (-0.003–0.015) | (-0.004–0.014) | (0.007–0.025) | ||||||
| ≤ Primary education | 0.027*** | 0.022*** | 0.010* | 0.039*** | 0.034*** | 0.029*** | 0.043*** | |||||
| (0.021–0.033) | (0.015–0.028) | (0.000–0.019) | (0.028–0.051) | (0.024–0.044) | (0.019–0.038) | (0.033–0.053) | ||||||
| Age ≥ 80 years | ||||||||||||
| Secondary education | 0.015*** | 0.012** | 0.001 | 0.019* | 0.022*** | 0.018** | 0.014* | |||||
| (0.006–0.024) | (0.003–0.021) | (-0.014–0.016) | (0.001–0.036) | (0.009–0.035) | (0.005–0.031) | (0.001–0.026) | ||||||
| ≤ Primary education | 0.026*** | 0.019*** | 0.012 | 0.044*** | 0.026*** | 0.033*** | 0.022*** | |||||
| (0.017–0.036) | (0.009–0.028) | (-0.003–0.028) | (0.026–0.063) | (0.012–0.040) | (0.019–0.046) | (0.007–0.035) | ||||||
| Model 2 | ||||||||||||
| Age 55–69 years | ||||||||||||
| Secondary education | NA | NA | 0.001 | NA | -0.003 | NA | 0.003 | NA | 0.009 | 55% | 0.017* | 39% |
| (-0.014–0.16) | (-0.021–0.014) | (-0.015–0.022) | (-0.007–0.025) | (0.001–0.034) | ||||||||
| ≤ Primary education | NA | NA | -0.003 | NA | 0.014 | 59% | 0.040*** | 46% | 0.026** | 54% | 0.036*** | 44% |
| (-0.021–0.014) | (-0.007–0.034) | (0.019–0.062) | (0.007–0.044) | (0.016–0.056) | ||||||||
| Age 70–79 years | ||||||||||||
| Secondary education | NA | NA | -0.005 | NA | 0.006 | 45% | 0.002 | NA | 0.001 | NA | 0.013** | 9% |
| (-0.014–0.004) | (-0.004–0.016) | (-0.007–0.011) | (-0.007–0.008) | (0.004–0.021) | ||||||||
| ≤ Primary education | NA | NA | 0.002 | 80% | 0.028*** | 28% | 0.024*** | 29% | 0.016*** | 45% | 0.032*** | 26% |
| (-0.008–0.011) | (0.017–0.039) | (0.014–0.034) | (0.007–0.025) | (0.023–0.042) | ||||||||
| Age ≥ 80 years | ||||||||||||
| Secondary education | NA | NA | -0.005 | NA | 0.011 | 42% | 0.016** | 27% | 0.010 | 44% | 0.008 | 43% |
| (-0.020–0.010) | (-0.006–0.028) | (0.003–0.028) | (-0.002–0.022) | (-0.004–0.020) | ||||||||
| ≤ Primary education | NA | NA | 0.003 | NA | 0.032*** | 27% | 0.017** | 35% | 0.021*** | 36% | 0.013* | 41% |
| (-0.012–0.019) | (0.015–0.050) | (0.003–0.030) | (0.008–0.033) | (0.001–0.025) | ||||||||
Values are derived from multilevel multivariable linear regression, tertiary education is the reference group. Model 1 is adjusted for confounders: age, sex, and living arrangement (alone/not alone). Model 2 is additionally adjusted for morbidities.
* p<0.05;
** p<0.01;
*** p<0.001.
† % represents the % change in effect estimates relative to model 1 after adjustment for morbidities; this was calculated by: 100x ((Bmodel1-Bmodel2)/Bmodel1). B = effect estimate; CI = confidence interval; (I)ADL = (instrumental) activities of daily living
Neighbourhood SES was significantly associated with frailty, morbidities, IADL limitations, psychosocial health, HRQoL and SRH (p < .05; Table 3-Model 1). Persons living in more deprived neighbourhoods (third or fourth quartile) had higher scores compared to those living in the least deprived neighbourhoods (first quartile). The number of morbidities mediated the association between neighbourhood SES and other frailty components, attenuations ranged between 20% and 90% (Table 3-Model 2).
Table 3. Association of neighbourhood socioeconomic status with overall frailty and with its six components (Model 1) and change in association of neighbourhood socioeconomic status with the five other frailty components after adjustment for the morbidities component (Model 2); stratified by age group among 25,494 persons of The Older Persons and Informal Caregivers Survey Minimum DataSet (TOPICS-MDS).
| Overall Frailty | Morbidities | ADL limitations | IADL limitations | Psychosocial health | Health-related quality of life | Self-rated health | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B (95% CI) | B (95% CI) | B (95% CI) | %† | B (95% CI) | %† | B (95% CI) | %† | B (95% CI) | %† | B (95% CI) | %† | |
| Model 1 | ||||||||||||
| Age 55–69 years | ||||||||||||
| Second quartile | 0.008 | 0.006 | 0.005 | -0.005 | 0.020 | 0.017 | 0.021* | |||||
| (-0.004–0.020) | (-0.007–0.018) | (-0.012–0.022) | (-0.025–0.016) | (-0.002–0.042) | (-0.003–0.036) | (0.0011–0.041) | ||||||
| Third quartile | 0.012* | 0.013 | -0.004 | 0.005 | 0.023* | 0.028** | 0.021* | |||||
| (0.001–0.023) | (-0.001–0.025) | (-0.021–0.012) | (-0.015–0.025) | (0.001–0.044) | (0.010–0.047) | (0.001–0.040) | ||||||
| Fourth quartile | 0.023*** | 0.025*** | -0.002 | 0.016 | 0.043*** | 0.028** | 0.036*** | |||||
| (0.012–0.033) | (0.014–0.036) | (-0.017–0.013) | (-0.002–0.034) | (0.024–0.063) | (0.011–0.045) | (0.018–0.053) | ||||||
| Age 70–79 years | ||||||||||||
| Second quartile | 0.003 | 0.007** | -0.001 | 0.000 | 0.001 | 0.006 | 0.002 | |||||
| (-0.001–0.008) | (0.002–0.012) | (-0.008–0.006) | (-0.009–0.009) | (-0.007–0.009) | (-0.001–0.013) | (-0.006–0.009) | ||||||
| Third quartile | 0.010*** | 0.012*** | 0.002 | 0.007 | 0.010* | 0.013** | 0.008 | |||||
| (0.004–0.015) | (0.006–0.018) | (-0.006–0.010) | (-0.003–0.017) | (0.001–0.018) | (0.005–0.022) | (-0.001–0.017) | ||||||
| Fourth quartile | 0.014*** | 0.015*** | 0.004 | 0.010* | 0.016*** | 0.018*** | 0.025*** | |||||
| (0.008–0.019) | (0.009–0.021) | (-0.005–0.012) | (0.000–0.021) | (0.007–0.025) | (0.009–0.026) | (0.016–0.033) | ||||||
| Age ≥ 80 years | ||||||||||||
| Second quartile | 0.005 | 0.006 | 0.002 | 0.012 | -0.003 | 0.010* | -0.002 | |||||
| (-0.001–0.011) | (-0.001–0.012) | (-0.008–0.013) | (-0.001–0.024) | (-0.012–0.007) | (0.001–0.019) | (-0.011–0.007) | ||||||
| Third quartile | 0.003 | 0.008* | -0.002 | 0.002 | 0.000 | 0.003 | 0.003 | |||||
| (-0.004–0.010) | (0.001–0.015) | (-0.014–0.010) | (-0.012–0.015) | (-0.011–0.010) | (-0.007–0.013) | (-0.007–0.013) | ||||||
| Fourth quartile | 0.012*** | 0.008* | 0.004 | 0.017* | 0.017** | 0.025*** | 0.010* | |||||
| (0.005–0.019) | (0.001–0.015) | (-0.008–0.016) | (0.003–0.030) | (0.006–0.027) | (0.015–0.035) | (0.000–0.020) | ||||||
| Model 2 | ||||||||||||
| Age 55–69 years | ||||||||||||
| Second quartile | NA | NA | 0.003 | NA | -0.007 | NA | 0.015 | NA | 0.014 | NA | 0.019* | NA |
| (-0.014–0.20) | (-0.027–0.013) | (-0.006–0.036) | (-0.005–0.032) | (0.000–0.038) | ||||||||
| Third quartile | NA | NA | -0.007 | NA | 0.001 | NA | 0.015 | NA | 0.023** | NA | 0.015 | NA |
| (-0.023–0.009) | (-0.019–0.020) | (-0.005–0.035) | (0.006–0.040) | (-0.003–0.033) | ||||||||
| Fourth quartile | NA | NA | -0.009 | NA | 0.005 | NA | 0.027** | 37% | 0.014 | 50% | 0.022** | 39% |
| (-0.024–0.006) | (-0.013–0.022) | (0.008–0.045) | (-0.002–0.029) | (0.005–0.039) | ||||||||
| Age 70–79 years | ||||||||||||
| Second quartile | NA | NA | -0.004 | NA | -0.004 | NA | -0.003 | NA | 0.002 | NA | -0.002 | NA |
| (-0.011–0.004) | (-0.013–0.004) | (-0.010–0.005) | (-0.004–0.009) | (-0.010–0.005) | ||||||||
| Third quartile | NA | NA | -0.003 | NA | 0.000 | NA | 0.003 | 70% | 0.006 | 54% | 0.000 | NA |
| (-0.011–0.005) | (-0.010–0.010) | (-0.006–0.011) | (-0.002–0.014) | (-0.008–0.008) | ||||||||
| Fourth quartile | NA | NA | -0.003 | NA | 0.001 | 90% | 0.008 | 50% | 0.008* | 56% | 0.016*** | 36% |
| (-0.011–0.006) | (-0.008–0.011) | (-0.001–0.016) | (0.001–0.016) | (0.007–0.024) | ||||||||
| Age ≥ 80 years | ||||||||||||
| Second quartile | NA | NA | 0.000 | NA | 0.008 | NA | -0.006 | NA | 0.006 | NA | -0.005 | NA |
| (-0.011–0.010) | (-0.004–0.020) | (0.015–0.003) | (-0.002–0.015) | (-0.014–0.003) | ||||||||
| Third quartile | NA | NA | -0.006 | NA | -0.004 | NA | -0.004 | NA | -0.001 | NA | -0.001 | NA |
| (-0.017–0.006) | (-0.017–0.010) | (-0.014–0.006) | (-0.010–0.008) | (-0.011–0.008) | ||||||||
| Fourth quartile | NA | NA | 0.001 | NA | 0.012 | 29% | 0.013** | 24% | 0.020*** | 20% | 0.007 | 30% |
| (-0.010–0.013) | (-0.001–0.026) | (0.003–0.023) | (0.011–0.030) | (-0.003–0.016) | ||||||||
Values are derived from multilevel multivariable linear regression, First Quartile is the reference group. Model 1 is adjusted for confounders: age, sex, and living arrangement (alone/not alone). Model 2 is additionally adjusted for morbidities.
* p<0.05;
** p<0.01;
*** p<0.001.
† % represents the % change in effect estimates relative to model 1 after adjustment for morbidities; this was calculated by: 100x ((Bmodel1-Bmodel2)/Bmodel1). B = effect estimate; CI = confidence interval; (I)ADL = (instrumental) activities of daily living
Discussion
This study showed that persons with the lowest SES, e.g. the lowest education level or living in the most deprived neighbourhoods, had the highest overall frailty and frailty component scores. The number of morbidities mediated the association between SES indicators and other frailty components.
In our study, education level was most consistently associated with overall frailty, morbidities and SRH. Former research found that lower educated persons are on average more frail compared to higher educated persons[5–8]. Education level has been associated with frailty components, such as ADL, IADL and SRH, although few studies compare multiple outcomes[36–38]. We found associations of neighborhood SES as indicator of individual SES with frailty and with frailty components, but these were generally less strong. Additionally, we examined the isolated effect of neighbourhood SES after adjustment for individual education level and found consistent associations for the most deprived neighbourhoods (S1 Table). Few studies have investigated the association between neighbourhood SES and frailty[39]. The association between the SES indicators and ADL limitations was not consistent in our study, which might be due to a ceiling effect for the instrument used in a community-dwelling population[40].
We found the strongest association between education level and psychosocial health for persons aged 55–69 years and with IADL limitations for persons aged 80 years and over. Vaughan et al. found that persons who had no cardiovascular disease when aged between 65–80 years maintained good physical functioning over the age of 80 years[17]. As certain morbidities are more prevalent among persons with a lower SES, this could at a younger age result in worse psychosocial health or self-rated health, but may as one ages increasingly impact on functional health[17, 41]. Socioeconomic inequalities in frailty and all frailty components except for IADL limitations, were larger among persons aged 55–69 years compared to older persons. This finding is often explained by a ‘healthy survivor effect’, where unhealthier persons with a low SES have died at a younger age and is found in cross-sectional research for various health outcomes[42–45]. However, longitudinal research has found confirming and contradicting results, depending on the indicator by which SES and health is measured[4, 46]. Further research is needed to understand the mechanisms behind these findings.
The number of morbidities moderately to strongly mediated the association between SES indicators and other frailty components. Former research has found that both specific morbidities and number of morbidities mediate socioeconomic inequalities in frailty[9, 18, 47, 48]. Hoogendijk et al. found that cognitive impairment, obesity, and number of chronic diseases had the largest contributions to socioeconomic inequalities in frailty[18], while Soler-Vila et al. found largest contributions for obesity, depression and musculoskeletal disease[9]. These studies have looked at physical frailty as developed by Fried[49]. A study by Gobbens et al. that used a multidimensional concept of frailty found that multi-morbidity could explain income differences in psychological and physical frailty, but not social frailty[47]. More longitudinal research is needed on the role of specific morbidities and number of morbidities in explaining socioeconomic inequalities in frailty and frailty components. Furthermore, this means that frailty and morbidities more often coexist in persons with a low SES. It is important to manage the progression of morbidities in this group, as the presence of frailty in persons with chronic diseases such as diabetes and COPD has shown to strongly increase mortality[50, 51].
The main strengths of this study are the size and diversity of the study population, this study included data from a large number of older persons from different regions in the Netherlands. Furthermore, we used validated instruments to measure frailty and frailty components. This study has some limitations. First, this study had a cross-sectional design, which limits conclusions regarding causality. Health could also impact a person’s SES, which is defined as health selection, however the effect of health selection is small for education level[52]. Second, there was considerable variation between the 30 included projects regarding sampling frame, inclusion criteria, study design, sample size, and data collection method. We used meta-analyses techniques to correct for clustering between subjects in projects. However, we believe that these pooled data are likely to reflect reality better than data from a single project based on one nonrandom sample. Third, due to item non-response there were some missing data. To deal with this we used multiple imputation methods for potential confounders. A non-response analysis showed that there were some socio-demographic differences between persons who were excluded and who were included, although it is unclear how this could have affected the size of the effect. We additionally performed a series of sensitivity analyses restricted to persons who had a complete number of items for the FI and for each FI component, changes were marginal.
In conclusion, there are socioeconomic inequalities in frailty and frailty components. Inequalities in frailty, number of morbidities and SRH are most consistent across age groups. The number of morbidities a person has play a role in explaining socioeconomic inequalities in frailty and should be considered in the management of frailty.
Supporting information
(DOCX)
Acknowledgments
This study makes use of data generated by the Older Persons and Caregivers Survey Minimum Dataset (TOPICS-MDS). A full list of the investigators is available from www.topics-mds.eu. Funding for the TOPICS-MDS project was provided by the National Care for older citizens Programme on behalf of the Organisation of Health Research and Development (ZonMw—The Netherlands, Grant reference 310300002). Funding was provided to the first author (Carmen B. Franse) by the Organisation of Health Research and Development (ZonMw—The Netherlands, Grant No. 633400009).
Data Availability
Studies using the TOPICS-MDS data are subject to the Dutch law on medical research among humans (Wet Medisch-Wetenschappelijk Onderzoek met mensen, WMO). It is not allowed by the WMO law that de-identified data are provided to others without restriction. The research ethics committee of the Radboud University Medical Center has approved the use of TOPICS-MDS data and supervises research leaders to conduct accordingly. The data are only available upon request after signing a data usage agreement form of the TOPICS-MDS data repository (http://topics-mds.eu/). Applications are assessed by the TOPICS Project Group and TOPICS Societal board, who may be contacted at topics-mds@radboudumc.nl.
Funding Statement
Funding for the TOPICS-MDS project was provided by the National Care for older citizens Programme on behalf of the Organisation of Health Research and Development (ZonMw—The Netherlands, Grant reference 310300002). Funding was provided to the first author (Carmen B. Franse) by the Organisation of Health Research and Development (ZonMw—The Netherlands, Grant No. 633400009). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62. Epub 2013/02/12. doi: 10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–7. Epub 2013/06/15. doi: 10.1016/j.jamda.2013.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Romero-Ortuno R, Kenny RA. The frailty index in Europeans: association with age and mortality. Age Ageing. 2012;41(5):684–9. doi: 10.1093/ageing/afs051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stolz E, Mayerl H, Waxenegger A, Rasky E, Freidl W. Impact of socioeconomic position on frailty trajectories in 10 European countries: evidence from the Survey of Health, Ageing and Retirement in Europe (2004–2013). J Epidemiol Community Health. 2016. doi: 10.1136/jech-2016-207712 . [DOI] [PubMed] [Google Scholar]
- 5.Chamberlain AM, St Sauver JL, Jacobson DJ, Manemann SM, Fan C, Roger VL, et al. Social and behavioural factors associated with frailty trajectories in a population-based cohort of older adults. BMJ Open. 2016;6(5):e011410 doi: 10.1136/bmjopen-2016-011410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hajizadeh M, Mitnitski A, Rockwood K. Socioeconomic gradient in health in Canada: Is the gap widening or narrowing? Health Policy. 2016;120(9):1040–50. doi: 10.1016/j.healthpol.2016.07.019 . [DOI] [PubMed] [Google Scholar]
- 7.Harttgen K, Kowal P, Strulik H, Chatterji S, Vollmer S. Patterns of frailty in older adults: comparing results from higher and lower income countries using the Survey of Health, Ageing and Retirement in Europe (SHARE) and the Study on Global AGEing and Adult Health (SAGE). PLoS One. 2013;8(10):e75847 doi: 10.1371/journal.pone.0075847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romero-Ortuno R. Frailty Index in Europeans: association with determinants of health. Geriatr Gerontol Int. 2014;14(2):420–9. doi: 10.1111/ggi.12122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soler-Vila H, Garcia-Esquinas E, Leon-Munoz LM, Lopez-Garcia E, Banegas JR, Rodriguez-Artalejo F. Contribution of health behaviours and clinical factors to socioeconomic differences in frailty among older adults. J Epidemiol Community Health. 2016;70(4):354–60. doi: 10.1136/jech-2015-206406 . [DOI] [PubMed] [Google Scholar]
- 10.Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal. 2001;1:323–36. doi: 10.1100/tsw.2001.58 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–7. . [DOI] [PubMed] [Google Scholar]
- 12.Theou O, Brothers TD, Mitnitski A, Rockwood K. Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc. 2013;61(9):1537–51. Epub 2013/09/14. doi: 10.1111/jgs.12420 . [DOI] [PubMed] [Google Scholar]
- 13.Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:24 Epub 2008/10/02. doi: 10.1186/1471-2318-8-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang F, Gu D. Predictability of frailty index and its components on mortality in older adults in China. BMC Geriatr. 2016;16:145 doi: 10.1186/s12877-016-0317-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health O. International classification of functioning, disability and health: ICF. Geneva: World Health Organization; 2001. [Google Scholar]
- 16.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273(1):59–65. . [PubMed] [Google Scholar]
- 17.Vaughan L, Leng X, La Monte MJ, Tindle HA, Cochrane BB, Shumaker SA. Functional Independence in Late-Life: Maintaining Physical Functioning in Older Adulthood Predicts Daily Life Function after Age 80. J Gerontol A Biol Sci Med Sci. 2016;71 Suppl 1:S79–86. doi: 10.1093/gerona/glv061 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoogendijk EO, van Hout HP, Heymans MW, van der Horst HE, Frijters DH, Broese van Groenou MI, et al. Explaining the association between educational level and frailty in older adults: results from a 13-year longitudinal study in the Netherlands. Ann Epidemiol. 2014;24(7):538–44 e2. doi: 10.1016/j.annepidem.2014.05.002 . [DOI] [PubMed] [Google Scholar]
- 19.Lutomski JE, Baars MA, Schalk BW, Boter H, Buurman BM, den Elzen WP, et al. The development of the Older Persons and Informal Caregivers Survey Minimum DataSet (TOPICS-MDS): a large-scale data sharing initiative. PLoS One. 2013;8(12):e81673 doi: 10.1371/journal.pone.0081673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.BeterOud. Nationaal Programma Ouderenzorg 2017. http://www.beteroud.nl/ouderen/nationaal-programma-ouderenzorg-npo.html.
- 21.Lutomski JE, Baars MA, van Kempen JA, Buurman BM, den Elzen WP, Jansen AP, et al. Validation of a frailty index from the older persons and informal caregivers survey minimum data set. J Am Geriatr Soc. 2013;61(9):1625–7. doi: 10.1111/jgs.12430 . [DOI] [PubMed] [Google Scholar]
- 22.Mitnitski A, Song X, Skoog I, Broe GA, Cox JL, Grunfeld E, et al. Relative fitness and frailty of elderly men and women in developed countries and their relationship with mortality. J Am Geriatr Soc. 2005;53(12):2184–9. doi: 10.1111/j.1532-5415.2005.00506.x . [DOI] [PubMed] [Google Scholar]
- 23.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of Illness in the Aged. The Index of Adl: A Standardized Measure of Biological and Psychosocial Function. JAMA. 1963;185:914–9. . [DOI] [PubMed] [Google Scholar]
- 24.Laan W, Zuithoff NP, Drubbel I, Bleijenberg N, Numans ME, de Wit NJ, et al. Validity and reliability of the Katz-15 scale to measure unfavorable health outcomes in community-dwelling older people. J Nutr Health Aging. 2014;18(9):848–54. doi: 10.1007/s12603-014-0479-3 . [DOI] [PubMed] [Google Scholar]
- 25.Krabbe PF, Stouthard ME, Essink-Bot ML, Bonsel GJ. The effect of adding a cognitive dimension to the EuroQol multiattribute health-status classification system. J Clin Epidemiol. 1999;52(4):293–301. . [DOI] [PubMed] [Google Scholar]
- 26.Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. . [PubMed] [Google Scholar]
- 27.Organisation for Economic C-o, Development. Classifying educational programmes: manual for ISCED-97 implementation in OECD countries. Paris: Organisation for Economic Co-operation and Development; 1999. [Google Scholar]
- 28.Statistics Netherlands (CBS). Standaard Onderwijsindeling. Voorburg [etc.]: Centraal Bureau voor de Statistiek; 1999.
- 29.Knol F. Van hoog naar laag; van laag naar hoog: de sociaal-ruimtelijke ontwikkeling van wijken tussen 1971–1995. Den Haag: Sociaal en Cultureel Planbureau; 1998. [Google Scholar]
- 30.Statistics Netherlands (CBS). Kerncijfers postcodegebieden (2008–2010). Den Haag/Heerlen: 2012.
- 31.Snijders TAB, Bosker RJ. Multilevel analysis: an introduction to basic and advanced multilevel modeling. Los Angeles: SAGE; 2012. [Google Scholar]
- 32.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129(1):125–37. . [DOI] [PubMed] [Google Scholar]
- 33.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82. . [DOI] [PubMed] [Google Scholar]
- 34.McDonald JH, University of D. Handbook of biological statistics. Baltimore, Maryland: Sparky House Publishing; 2009. [Google Scholar]
- 35.Greenland S, Finkle WD. A critical look at methods for handling missing covariates in epidemiologic regression analyses. Am J Epidemiol. 1995;142(12):1255–64. . [DOI] [PubMed] [Google Scholar]
- 36.Palacios-Cena D, Jimenez-Garcia R, Hernandez-Barrera V, Alonso-Blanco C, Carrasco-Garrido P, Fernandez-de-Las-Penas C. Has the prevalence of disability increased over the past decade (2000–2007) in elderly people? A Spanish population-based survey. J Am Med Dir Assoc. 2012;13(2):136–42. doi: 10.1016/j.jamda.2010.05.007 . [DOI] [PubMed] [Google Scholar]
- 37.Leopold L, Engelhardt H. Education and physical health trajectories in old age. Evidence from the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Public Health. 2013;58(1):23–31. doi: 10.1007/s00038-012-0399-0 . [DOI] [PubMed] [Google Scholar]
- 38.Tsai Y. Education and disability trends of older Americans, 2000–2014. J Public Health (Oxf). 2016. doi: 10.1093/pubmed/fdw082 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lang IA, Hubbard RE, Andrew MK, Llewellyn DJ, Melzer D, Rockwood K. Neighborhood deprivation, individual socioeconomic status, and frailty in older adults. J Am Geriatr Soc. 2009;57(10):1776–80. doi: 10.1111/j.1532-5415.2009.02480.x . [DOI] [PubMed] [Google Scholar]
- 40.Lutomski JE, Krabbe PF, den Elzen WP, Olde-Rikkert MG, Steyerberg EW, Muntinga ME, et al. Rasch analysis reveals comparative analyses of activities of daily living/instrumental activities of daily living summary scores from different residential settings is inappropriate. J Clin Epidemiol. 2016;74:207–17. doi: 10.1016/j.jclinepi.2015.11.006 . [DOI] [PubMed] [Google Scholar]
- 41.Edjolo A, Proust-Lima C, Delva F, Dartigues JF, Peres K. Natural History of Dependency in the Elderly: A 24-Year Population-Based Study Using a Longitudinal Item Response Theory Model. Am J Epidemiol. 2016;183(4):277–85. doi: 10.1093/aje/kwv223 . [DOI] [PubMed] [Google Scholar]
- 42.Huisman M, Kunst AE, Mackenbach JP. Socioeconomic inequalities in morbidity among the elderly; a European overview. Soc Sci Med. 2003;57(5):861–73. . [DOI] [PubMed] [Google Scholar]
- 43.Enroth L, Raitanen J, Hervonen A, Nosraty L, Jylha M. Is socioeconomic status a predictor of mortality in nonagenarians? The vitality 90+ study. Age Ageing. 2015;44(1):123–9. doi: 10.1093/ageing/afu092 . [DOI] [PubMed] [Google Scholar]
- 44.Gobbens RJ, van Assen MA, Schalk MJ. The prediction of disability by self-reported physical frailty components of the Tilburg Frailty Indicator (TFI). Arch Gerontol Geriatr. 2014. Epub 2014/07/22. doi: 10.1016/j.archger.2014.06.008 . [DOI] [PubMed] [Google Scholar]
- 45.Bell CL, Chen R, Masaki K, Yee P, He Q, Grove J, et al. Late-life factors associated with healthy aging in older men. J Am Geriatr Soc. 2014;62(5):880–8. doi: 10.1111/jgs.12796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Benzeval M, Green MJ, Leyland AH. Do social inequalities in health widen or converge with age? Longitudinal evidence from three cohorts in the West of Scotland. BMC Public Health. 2011;11:947 doi: 10.1186/1471-2458-11-947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gobbens RJ, van Assen MA, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Determinants of frailty. J Am Med Dir Assoc. 2010;11(5):356–64. doi: 10.1016/j.jamda.2009.11.008 . [DOI] [PubMed] [Google Scholar]
- 48.Etman A, Kamphuis CB, van der Cammen TJ, Burdorf A, van Lenthe FJ. Do lifestyle, health and social participation mediate educational inequalities in frailty worsening? Eur J Public Health. 2014. Epub 2014/07/26. doi: 10.1093/eurpub/cku093 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56. Epub 2001/03/17. . [DOI] [PubMed] [Google Scholar]
- 50.Cacciatore F, Testa G, Galizia G, Della-Morte D, Mazzella F, Langellotto A, et al. Clinical frailty and long-term mortality in elderly subjects with diabetes. Acta Diabetol. 2013;50(2):251–60. doi: 10.1007/s00592-012-0413-2 . [DOI] [PubMed] [Google Scholar]
- 51.Galizia G, Cacciatore F, Testa G, Della-Morte D, Mazzella F, Langellotto A, et al. Role of clinical frailty on long-term mortality of elderly subjects with and without chronic obstructive pulmonary disease. Aging Clin Exp Res. 2011;23(2):118–25. . [DOI] [PubMed] [Google Scholar]
- 52.Kroger H, Pakpahan E, Hoffmann R. What causes health inequality? A systematic review on the relative importance of social causation and health selection. Eur J Public Health. 2015;25(6):951–60. doi: 10.1093/eurpub/ckv111 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
Studies using the TOPICS-MDS data are subject to the Dutch law on medical research among humans (Wet Medisch-Wetenschappelijk Onderzoek met mensen, WMO). It is not allowed by the WMO law that de-identified data are provided to others without restriction. The research ethics committee of the Radboud University Medical Center has approved the use of TOPICS-MDS data and supervises research leaders to conduct accordingly. The data are only available upon request after signing a data usage agreement form of the TOPICS-MDS data repository (http://topics-mds.eu/). Applications are assessed by the TOPICS Project Group and TOPICS Societal board, who may be contacted at topics-mds@radboudumc.nl.