Abstract
Objectives
This qualitative study describes the experiences of spousal caregivers of a patient with end-stage heart failure (HF) from pre-LVAD to post-LVAD-DT implantation.
Background
LVAD-DTs are implanted as permanent devices for end-stage HF patients with the goal of improving the length and quality of life. LVADs create new demands for both patients and caregivers.
Methods
In-depth, semi-structured interviews of 10 spousal caregivers were thematically analyzed.
Results
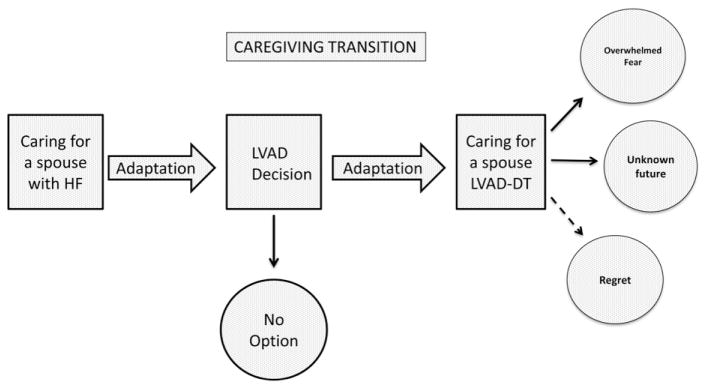
Throughout the process of caregiving, pre-implant through post-implant, all caregivers discussed their ability to adapt within the role as a caregiver. Adaptation as a caregiver occurred through three distinct time frames following the progression of the patient’s HF and subsequent LVAD implantation: caring for a spouse with HF, decision for LVAD implantation made, and caring for a spouse with the LVAD-DT.
Conclusions
Caregivers were able to adapt and develop effective strategies to incorporate the demands of caring for a spouse with an LVAD-DT, but the role remained challenging. The findings underscore the need for continued research that may be translated into effective interventions to support patient and caregivers as they live through this end-of-life trajectory.
Keywords: Heart failure, Caregiving, Left ventricular assist device, Destination therapy, Qualitative
Introduction
Heart failure (HF) is a chronic and progressive disorder impacting approximately 5.8 million Americans.1 Despite advances in technology, as well as risk prevention, the prevalence of HF continues to increase with over 550,000 new cases diagnosed each year.1 There are approximately 50,000–150,000 patients with stage D HF2 who remain symptomatic despite maximal medical management. Patients with end-stage HF have a mortality rate approaching 80% at five years2 and once they become dependent on inotropic support the one year mortality rate approaches 50%.3 The standard of care for the management of HF refractory to medical treatment continues to be cardiac transplantation,4 but with a small number of available donor organs, this option is not attainable for many who do not meet the stringent eligibility criteria.
A left ventricular assist device (LVAD) is a type of mechanical circulatory support that is implanted to restore the physiologic function of the damaged left ventricle in patients with stage D HF. Currently, there are two approved long-term indications: LVAD as a bridge to transplant (BTT) and LVAD as destination therapy (DT). LVAD-DT is a permanent alternative for stage D HF patients who are not transplant candidates. Once implanted, the majority of these patients will live with and die with this device in place. The main goals of destination therapy are to improve the daily function and health-related quality of life, and to improve survival compared to patients who receive optimal medical management.5 Studies have shown a 68% survival rate with an LVAD at 1 year and a 58% increase in survival at 2 years compared to those who are managed medically.6 Based on the current evidence, quality of life also improves post-implant.7–9 Since FDA approval, there has been an exponential increase in the use of LVAD-DT with a ten-fold increase from 2006–2010.6 The implantation of LVADs will continue to increase with improvements in technology, scarcity of donor hearts, and the aging population.
Background
LVAD implantation creates new demands for both the patient and caregiver. Based on the complex care required at home, it is the standard of practice in most mechanical circulatory support programs to designate a member of the patient’s family as the caregiver. This requires an extensive commitment from the dedicated caregiver(s). The caregiver is typically a spouse, immediate family member, or friend who provides around the clock help and support. The responsibilities involved in caregiving vary from simple tasks such as monitoring of vital signs, daily weights, and sterile dressing changes to more complex procedures such as monitoring the LVAD function, troubleshooting alarms, and responding to emergency situations.10 These tasks are complex for a layperson and can be very stressful for caregivers, potentially affecting their health and quality of life.11,12 Compounding the complexity of this caregiving role is the permanency of this care-giving situation. When an LVAD is implanted as a BTT, it is a bridge until a heart for transplantation becomes available.13 Conversely, when an LVAD is implanted as destination therapy, the patient will live with this device until death, increasing the demands placed on the caregiver as the patient lives and dies with this complex device. To date, few researchers have examined the experience of caregivers of patients requiring LVAD support, and even fewer studies have examined caregivers when LVADs are implanted as destination therapy. The primary goal of this study was to explore the caregiving experience, as the patient transitioned from stage D HF to the implantation of an LVAD-DT.
A phenomenological study by Casida10 examined the lived experience of spouses and patients with LVADs. The sample was small (n = 3), but three major themes emerged: emotional distress, determination, and optimism. Marcucculli and Casida14 described the lifestyle adjustments of caregivers for patients with an LVAD as a BTT or DT. The main themes were caregiving as a constant responsibility, coping strategies, and satisfaction. Caregivers described how the adjustments to their new roles became easier over time with the use of effective coping strategies. Baker et al15 described the experiences of caregivers of patients who received an LVAD as a BTT. The main themes in this phenomenological study were sacrifice and moving beyond. Caregivers reported that sacrifices were necessary in terms of family, friends, employment, and their own health as they adjusted to this new role. Although, these studies show effective adaptation over time, the majority of the participants were providing care for patients with an LVAD as a BTT. These caregivers may have had different experiences because they were waiting for a transplant and may not have viewed their caregiving roles as permanent and continuing through death. Although the experience of caring for patients with LVAD-DT may share some of the same characteristics as BTT, there may also be experiences specific to the caregivers of an LVAD-DT that have not be explored. Specifically, patients living with the device long term with no expectation of a transplant and the reality that the patient will die with the device. As the number of LVADs implanted as DT continue to increase, understanding the caregiving experience from the perspective of the spousal caregiver is crucial for healthcare providers who are developing and evaluating care for both patients and their caregivers.
Purpose
The purpose of this qualitative study was to describe the experiences of spousal caregivers of patients with stage D HF from pre-LVAD to post-LVAD-DT implantation. Understanding the experiences of spousal caregivers will provide avenues for the development of caregiver-centered interventions to support these instrumental partners in care. The goal of interventions is to improve the experiences and outcomes for both the patient and the caregiver.
Methods
Design
Data collection and analysis were conducted using a qualitative approach to elucidate spousal experiences of providing care for patients with stage D HF from pre-LVAD to post-LVAD-DT implantation. Qualitative methodology is appropriate for the exploration of this phenomenon as the variables influencing this experience have not been clearly described in the existing literature.16
Sampling and recruitment
Following IRB approval, spousal caregivers of patients with an LVAD-DT were recruited from one large LVAD service in a tertiary medical center. The center was a referral center with an LVAD coordinator on call 24/7 who could answer questions and troubleshoot device issues for patients and their caregivers. This purposive sample was limited to spousal caregivers, because they are caregiving on a daily basis and would be able to provide rich descriptions of the experience. The inclusion criteria for participants included: the ability to speak and understand English; being the spouse/partner residing with the patient and the primary care provider for the spouse/partner following device placement; and without gross evidence of cognitive impairment that may preclude insightful reflection. Spousal caregivers who accompanied LVAD patients to the LVAD clinic over a 6-month period were asked to participate. Sampling continued until thematic saturation was achieved.
Data collection
At a follow-up LVAD clinic appointment, spousal caregivers were asked to participate in the study. If they agreed, informed written consent was obtained. During this visit, sociodemographic data were collected. Due to the length of the clinic visit, the distance most patients lived from the clinic, and limited access to private interview space, face-to-face interviews were not completed at the clinic visit. Following the visit, participants were contacted to set up a mutually convenient time for a phone interview.
A semi-structured interview guide with probes (Table 1) was designed to capture the experience of the spousal caregiver. The interview guide was developed by two qualitative researchers who are experts in qualitative methods and have conducted multiple research studies with HF patients and caregivers. Participants were asked to describe their experiences of caring for a spouse with HF prior to and post-implantation of the LVAD-DT. One interviewer (LK) conducted the in-depth, semi-structured, 45–90 min interviews. Field notes were maintained during the interview to capture data that were not obtained from the transcribed interviews, such as emotional reactions. Interviews were digitally recorded, transcribed verbatim, de-identified, and entered into HyperRESEARCH17 for coding.
Table 1.
LVAD-DT spousal caregiver interview guide.
| Interview questions focus on experience, caregiving tasks pre- and post- implant and how those have changed. |
| Begin with description of illness. Capture both pre- and post-implant. |
| What was your role as a caregiver before the device placement, when your spouse was living with heart failure? |
| What types of tasks did you do for the patient? |
| Tell me what it was like living with a heart failure patient before the device was implanted. |
| Tell me what it has been like living with a heart failure patient with an LVAD-DT. |
| How has life changed since the implant of your spouse’s device for you and your spouse? |
| How would you describe the health status of your spouse since the device placement? Is it better or worse than before the device was implanted? |
| Has the device changed your role as a caregiver? If so, how? |
| What types of caregiving tasks are you performing now that the device is implanted? Has this changed since pre-implant? If so, how? |
| What do you expect from this present treatment? Are these expectations different from before the device was implanted? |
| Have there been services that you have needed as a caregiver that you felt you have not received? |
| What has been the impact on your finances since the device placement? |
| Do you feel all of your healthcare needs are being adequately addressed by the healthcare team? |
| Where do you see yourself in one year? |
| Probes: |
| Can you explain how you felt at that time? |
| Tell me more about that experience. |
Data analysis
A team approach was utilized for analysis. The initial codebook was based on the topics in the interview guide and was developed by three primary coders who met to discuss the coding of data and reach consensus on code labels. An inductive methodology was used for the analysis of the transcribed data. Through the analysis process, raw data were converted into themes. The purpose of the analysis was to reduce large amounts of data into meaningful themes for both the pre-implantation caregiving and post-implantation caregiving, and then to relate the themes to each other in meaningful ways. The process of data collection and analysis proceeded in a cyclic fashion until no new themes were discovered and data saturation was reached.
Trustworthiness of the data was addressed by collecting data utilizing the same researcher and interview guide. Initial coding of the data was completed by two coders, and member checks were performed by one investigator and the coders. Any discrepancies were reviewed by the research team and discussed among the coders and investigators until a consensus was met. An audit trail was documented during each analysis session. The final codes were agreed upon by all investigators in the study. A colleague, who is an expert in qualitative methods and HF, reviewed several transcripts and participated in the analysis session in which an overarching theme of caregiving emerged as well as themes associated with the progression of and changes in caregiving from pre to post-implant.
Results
Demographics
The sample included 10 spousal caregivers (8 females and 2 males), from age 52–73 (mean 62). The majority of participants were Caucasian (90%) and retired (60%). The patients ranged in age from 58 to 76 years of age (mean 67). All of the patients were classified as DT at the time of data collection. The length of time since implant ranged from 5 to 38 months. All of the patients had a Heartmate II non pulsatile flow LVAD (Thoratec Corporation, Pleasanton, California) implanted. Table 2 summarizes the demographic characteristic of the sample. At the time of the caregiver interviews, all of the patients were at home being cared for as outpatients.
Table 2.
Demographics of participants in the study.
| CG age | CG gender | CG occupation | CG self-reported health status | PT age | PT gender | PT’s length of time with HF (years unless noted) | PT’s Length of time with class III–IV symptoms (years unless noted) | PT’s length of time with LVAD-DT support (months) |
|---|---|---|---|---|---|---|---|---|
| 63 | M | Retired | Good | 65 | F | 10 | 2 months | 5 |
| 72 | M | Retired | Good | 70 | F | 4 | 4 | 24 |
| 62 | F | Retired | Fair | 70 | M | 8 | 3 | 26 |
| 55 | F | Full-time | Good | 76 | M | 15 | 3 | 38 |
| 52 | F | Full-time | Good | 61 | M | 4 | 4 | 6 |
| 58 | F | Full-time | Fair | 58 | M | 7 | 7 | 11 |
| 73 | F | Retired | Fair | 75 | M | 14 | 1 | 6 |
| 67 | F | Retired | Good | 69 | M | 8 | 2 | 13 |
| 65 | F | Full-time | Good | 68 | M | 39 | 2 | 11 |
| 56 | F | Disability | Poor | 58 | M | 2 months | 2 months | 19 |
Themes/time frames
Participants described in detail the impact that HF had on their lives and their roles as caregivers. Throughout the process of caregiving, pre-implant through post-implant, all caregivers discussed their ability to Adapt Within the Role as a Caregiver. Adaptation as a caregiver occurred through three distinct time frames following the progression of the patient’s HF and subsequent LVAD implantation: Caring for a Spouse with HF, Decision for LVAD Implantation Made, and Caring for a Spouse with the LVAD-DT. Fig. 1 depicts a conceptual model of adaptation through the time frames. Table 3 presents exemplar quotes from the spousal care-givers for each of the time frames.
Fig. 1.
Caregiving transition.
Table 3.
Themes and exemplar quotes.
| Excerpts of caregiver comments | |
|---|---|
| Adaptation within the role | “You just accept the changes and adjust.” |
| “It did not matter what I had to do, I learned to do it.” | |
| Caring for a spouse with HF | “The only thing he could do was breathe—that took all of his energy, all he could do is sit in his chair with his oxygen.” |
| “It was all on me, I had to keep working; I carried the insurance, and it was all on memldr;caring for him, the house, the appointments, making sure he had all of his meds at the right time and the right amountmldr;everything. It was overwhelming. It was dragging us all down but we did the best we could.” | |
| “He was doing well, thenmldr;just the ups and downs. He would fill up with fluid and then the next option would be a pacer. He would do well and then the fluid. Next it was the ICD. We were getting back to normal and then he would fill up with fluidmldr;; what a roller coaster. I just kept thinking, ‘what are they going to do next and what if nothing else could be done?’” | |
| Decision made | “Not really an option, he needed it to save his life.” |
| “LVAD or hospice—what would you pick?” | |
| “Not that I would change my decision but I had to make it without him. He was so sick, he was out of it. The times he is not doing well [with the LVAD], I feel guilty, I wonder if he would have made the same decision.” | |
| Caring for a spouse with an LVAD-DT | “I felt like I was a new mom again caring for a newborn, I just hovered; I slept when he did and I was awake when he was.” |
| “I felt prepared to go home when we were in the hospital, but the first time the alarm went off at home, I was in a complete panic. The [health care providers] were not there to help me if I could not get it figured out.” | |
| “I just pray that if something happens, the weather is good and they can fly him to [tertiary medical center]. It is obvious when we come into the emergency room how unfamiliar the staff is with his condition and equipment.” | |
| “I wonder what life would be like for us if he was living with HF.” | |
| “How long is this going to last?” |
Adaptation within the role as a caregiver
As patients transitioned from stage D HF to device placement, spousal caregivers described continual Adaptation Within the Role as a Caregiver. With each transition, from caring for a spouse with stage D HF, to deciding to have the LVAD implanted, to caring for a spouse with the LVAD, spousal caregivers successfully made the necessary adjustments and adopted the needed strategies to provide care. In the later phase post-implant, caregivers also detailed how they had adapted to their new lives with an LVAD and how grateful they were that their spouses had a second chance. However, they all also spoke of their uncertain future, since they were aware there were no further treatment options remaining.
Caring for a spouse with HF
The participants were asked to look back and describe their experiences as caregivers for spouses with stage D HF prior to the LVAD. All of the caregivers described the physical limitations imposed by advanced HF. Spouses were consumed with adapting to the demands of caregiving as they watched the health status of their spouses decline. Many talked of how they “juggled” many tasks to maintain the household. Caregivers spoke of the support systems they had, such as family and friends, and the adjustments they made to their lives to care for a spouse with HF, such as hiring a lawn service or downsizing their home.
All the caregivers detailed strategies for preventing exacerbations. These involved medication management, dietary changes, the flexibility required to change plans, and a hypervigilance in terms of monitoring symptoms. Caregivers talked about how they purchased blood pressure cuffs, scales, and even stethoscopes to monitor for changes. The caregivers also talked about the decline in health status and how quickly their spouses seemed to decompensate.
Decision for LVAD implantation made
The time period when the Decision was Made for LVAD Implantation was a time frame that was significant for caregivers and emerged as an important part of the process of caregiving. Caregivers described the experience leading up to device implantation. Although the majority of caregivers had previously discussed an LVAD as a treatment option with their healthcare team, when the “time came” they did not feel like they had any choice, but to consent. In these situations, it was either consenting or death. Some caregivers also detailed their experiences when the spouse was too ill to consent for the LVAD in an emergency situation, and described feelings of guilt or regret, especially if their spouse had complications post-implant.
Caring for a spouse with an LVAD-DT
Participants described how they transitioned from caring for a spouse with HF, to caring for a spouse with an LVAD-DT. In the early months of caring for a spouse with an LVAD, caregivers described an overwhelming sense of fear and anxiety. Many of the patients had declined to such a fragile state of health prior to the surgery, that many caregivers were not sure their spouse would survive surgery. When caregivers first saw their spouse attached to so many machines in the intensive care unit, they expressed being overcome with fear not only for the continued survival of their spouse, but also for what life was going to be like if they made it home. As their spouse recovered, caregivers reported feeling more comfortable and even assisting with care in the hospital under the supervision of the staff. However, this sense of comfort was short lived. As discharge neared, caregivers thought, “Can I really do this?”
Caregivers also described new strategies they adopted that were necessary to adjust for caring for an LVAD. These involved assisting with ADLs, especially bathing and dressing, which are very different with the LVAD in place. Caregivers detailed the “bedtime routine” that was required, including switching from the batteries to the power base unit and ensuring the batteries and back up batteries (in case of a power outage) were charged. It was at times difficult to help their spouse find a comfortable sleeping position.
Caregivers felt their new role was just as significant as caring for their spouse with advanced HF, but now described it as “different, still just as demanding at times, but different.” The new strategies necessary to provide care now involved complex dressing changes to the external drive lines and ensuring that an adequate supply of dressings were on hand.
Many of the caregivers described how they felt more responsible for their spouse now that they had an LVAD. With advanced HF, caregivers felt a sense of helplessness. Conversely, with the LVAD, caregivers felt that when an emergency arose, it was their job to know how to respond and what to do. Many caregivers had concerns throughout this transition regarding the distance to the LVAD center and the fact that in an emergency, the first hospital, in most cases, was not where the LVAD was implanted. In some cases, this heightened the caregiver’s sense of responsibility in caring for the LVAD.
Over time, the caregivers adopted the necessary strategies to adapt to caring for a spouse with an LVAD. This phase was highlighted by the acceptance of their new way of life. Caregivers adjusted to their new roles and developed effective routines. Caregivers reported a new sense of confidence as they managed the device, medications, and dressings. Caregivers were beginning to feel that life was getting back to normal.
Patients were also adjusting to life with an LVAD. The couples were beginning to establish a normal routine and felt comfortable leaving home for longer periods of time. Some patients even returned to work. One spouse described in great detail how her husband was able to ski again. All the participants expressed their gratitude for this “new lease on life.” Although many of the patients still had ups and downs, ranging from device failure, driveline infections, bleeding complications, and strokes, all expressed life with the LVAD was better than the alternative.
As life with the LVAD continued, many patients began to “outlive” the life expectancy of the device. This was conveyed by feelings of uncertainty in the caregivers. Many hoped their spouses would “just keep going as is,” but expressed concerns regarding what the next steps or options would be. Many were very fearful of a device failure, asking, “How long is this going to last?” Although all the participants realized a heart transplant was not an option, when asked about their feeling about the future, the majority felt they would continue “day by day” and “hopefully they can just keep replacing the device.” As the permanency of the decision became apparent, some patients experienced more complications than others, ranging from driveline infections to strokes. Caregivers of patients who did not experience increased quality of life with the device, although thankful that their spouse was still alive, expressed regret over their decision to have the device implanted.
Discussion
This study highlights the challenging role of the spousal caregiver throughout the process of caring for a spouse with HF to caring for a spouse with an LVAD. The spousal caregiver faces unique challenges as the permanency of caring for a spouse with an LVAD is realized; expressed by some as uncertainty in terms of the future, as well as regret. In describing the experience of spousal caregivers caring for a spouse with stage D HF, the findings were similar to previous studies of caregiving with HF. Stage D HF requires a complex physical and psychological process that continues not only during times of exacerbation, but also times of medical stability.18 Caregivers described how little their spouses were able to do in terms of activity, and how it was very distressing when their spouse worked so hard to breath. This finding was similar to results from Bekelman et al’s19 qualitative study describing the major concerns and needs of HF patients and their caregivers. Adjusting to the limitations of the illness was identified as one of the most difficult aspects of living with HF by patients and their informal caregivers. The caregivers also described “juggling” multiple roles from caregiver, to housekeeper, to sole financial provider. This finding was also similar to findings from Kitko et al (Kitko L, Hupcey J, Boehmer, J. The work of spousal caregiving in heart failure. Unpublished manuscript), in which various types of “work” were described by caregivers throughout their experience.
In this study, the distance to the mechanical circulatory support center was approximately 60 min. Distance was not an issue when the patient was in a period of medical stability but became a concern when a complication arose. Specifically, many of the patients had to be transported to a small facility that may not have had expertise with LVADs. This was reported as stressful for the caregivers and their spouses. As mechanical circulatory support programs continue to grow with patients being referred from further distances, the need for outreach on the part of the implantation center will become increasingly salient to ensure a coordinated plan of care for the patients and their caregivers.
As patients’ HF advanced to the point where they were not maintained by optimal medical management, caregivers described the decision to have an LVAD implanted. Many caregivers discussed how the LVAD was presented as a potential option during interactions with healthcare providers but when the “time came,” none felt they had another choice. This finding is consistent with Kirkpatrick et al who found that patients and caregivers were often overwhelmed by their illnesses and had a poor recall of doctor–patient device communication prior to device placement.20 As a result of an overall lack of advance care planning, Swetz et al21 propose proactive palliative medicine consultations for patients being considered for LVAD-DT. The purpose is to delineate goals of care and quality of life preference from pre-implantation to post-implantation, as well as establishing end-of-life preferences with the patient and caregiver; a process the authors call “preparedness planning.” This planning is critical when LVADs are implanted as DT, as the decision will have to be made to deactivate the device at the end-of-life. It is also salient for the caregiver who described “feelings of guilt,” as she was second – guessing her emergent decision to have the LVAD implanted when her husband was too unstable to consent for his own treatment. This ethical challenge with LVAD-DT was highlighted by Rizzieri et al22 who advocate for cautious use of surrogate consent in the absence of first person (patient) consent.
The few studies that have examined the role of the caregiver in the context of caring for an LVAD, indicate that the caregivers were able to transition to their new life of caring for a family member with an LVAD, which supports the findings of this work.10,14,15 What is not clear from the existing research is the price of this adaptation in terms of perceived burden, quality of life, and overall health of the caregiver for patients with an LVAD-DT, and this warrants additional investigation. As the permanency of the device and their new way of life became apparent, caregivers expressed concerns about next steps or options as some patients were approaching the life expectancy of the device and some even expressed regret over the decision to have the device implanted, but none talked about advance care planning. These are new concepts that have not been well explored in the literature. These concerns underscore the need for comprehensive support programs, such as palliative care, throughout this end-of-life trajectory from pre-LVAD through post-LVAD.
Implications
As patients live and die with this device, studies have described the LVAD-DT as an end-of-life trajectory and stress the importance of comprehensive supportive programs, such as palliative care throughout the course of illness.21–24 When asked about the future, none of the caregivers talked about end-of-life decisions, planning, or thoughts about deactivation. It should be noted, the majority of the patients were in a period of medical stability, which may contribute to this finding. But when a complication does occur, it tends to be life threatening such as an infection, stroke, or bleeding, and in some cases may require a decision by the family to discontinue the LVAD-DT support. This highlights the significance of a palliative care consult prior to the implant, so that a rapport can be established. It is imperative that the palliative care relationship continues throughout this end-of-life trajectory, encompassing the time when difficult decisions need to be made, such as device deactivation. Pre-implant preparations and protocols for device deactivation can lessen the burden on caregivers, as well as clinicians, when these decisions need to be made at the end-of-life. As the use of this device continues to grow, a few institutions have developed preparedness plans that address the patient’s wishes at the end-of-life when he or she is still capable of reflection both before and during the decision to implant.25,26
Limitations
A limitation of this study was the homogeneity of the sample; consisting primarily of white female spouses of patients recruited from one academic medical center. Future work should include non-spousal caregivers and a more diverse sample. However, the experiences discussed by the spousal caregivers were consistent with the findings of other HF and LVAD studies. Caregivers were asked to look back and recall their experiences of caring for a spouse with advanced HF prior to an LVAD implant (all patients were living with an LVAD at data collection) and then describe their experiences of caring for an LVAD. Many of the patients had been living with an LVAD for some time and this past reflection may have influenced the caregivers’ descriptions of caring for a spouse with HF. The interviews were conducted over the phone and not face-to-face. This may be viewed as a limitation, but during the phone interviews, the caregivers were in a private location away from their spouse, so were able to talk freely and did not feel rushed to get the patient back home. Based on the rich data that were collected, the phone interview did not impact the quality of the data. However, the investigator did not have the opportunity to observe facial expressions or body language during the interview. Future studies should include mixed methodology, as well as a longitudinal design to capture the experience of the caregiver. In addition, a large, diverse sample from various ethnic groups including different types of caregivers and different settings should be conducted. It is also imperative to study this phenomenon not only from the perspective of the caregiver, but the patient as well.
Conclusions
As mechanical circulatory support technology improves and the number of patients with stage D HF continues to increase, the number of LVADs implanted as DT will continue to grow. This study is the largest qualitative study to date intended specifically to examine the experiences of spousal LVAD-DT caregivers. These caregivers face unique challenges when devices are implanted as DT as compared to BTT. LVAD-DTs are implanted as a permanent EOL treatment and the majority of patients will live and die with this device in place. This has the potential to increase caregiver burden and decrease quality of life as well as complicate the end-of-life decision making for the patient and caregiver. In this study, caregivers were able to adapt and develop effective strategies to incorporate the demands of caring for a spouse with an LVAD-DT into their daily lives, but the role remained challenging and demanding. The findings of the study build on the currently available evidence, and highlight the essential and demanding role of the caregiver, underscoring the need for continued research in this area that may be translated into effective interventions to support patient and caregivers as they live through this end-of-life trajectory.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics – 2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ammar KA, Jacobsen SJ, Mahoney DW, et al. Prevalence and prognostic significance of heart failure stages: application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation. 2007;115(12):1563–1570. doi: 10.1161/CIRCULATIONAHA.106.666818. [DOI] [PubMed] [Google Scholar]
- 3.Hershberger RE, Nauman D, Walker TL, Dutton D, Burgess D. Care processes and clinical outcomes of continuous outpatient support with inotropes (COSI) in patients with refractory end stage heart failure. J Card Fail. 2003;9(3):180–187. doi: 10.1054/jcaf.2003.24. [DOI] [PubMed] [Google Scholar]
- 4.Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009;53(15):e1–e90. doi: 10.1016/j.jacc.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Lietz K, Long JW, Kfoury AG, et al. Outcomes of left ventricular assist device implantation as destination therapy in the post-REMATCH era: implications for patient selection. Circulation. 2007;116(5):497–505. doi: 10.1161/CIRCULATIONAHA.107.691972. [DOI] [PubMed] [Google Scholar]
- 6.Kirklin JK, Naftel DC, Kormos RL, et al. The fourth INTERMACS annual report: 4000 implants and counting. J Heart Lung Transplant. 2012;31(2):117–126. doi: 10.1016/j.healun.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Grady KL, Meyer P, Mattea A, et al. Improvement in quality of life outcomes 2 weeks after left ventricular assist device implantation. J Heart Lung Transplant. 2001;20(6):657–669. doi: 10.1016/s1053-2498(01)00253-4. [DOI] [PubMed] [Google Scholar]
- 8.Wray J, Hallas CN, Banner NR. Quality of life and psychological well-being during and after left ventricular assist device support. Clin Transplant. 2007;21(5):622–627. doi: 10.1111/j.1399-0012.2007.00698.x. [DOI] [PubMed] [Google Scholar]
- 9.Allen JG, Weiss ES, Schaffer JM, et al. Quality of life and functional status in patients surviving 12 months after left ventricular assist device implantation. J Heart Lung Transplant. 2010;29(3):278–285. doi: 10.1016/j.healun.2009.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Casida J. The lived experience of spouses of patients with a left ventricular assist device before heart transplantation. Am J Crit Care. 2005;14(2):145–151. [PubMed] [Google Scholar]
- 11.Dew MA, Kormos RL, Winowich S, et al. Quality of life outcomes in left ventricular assist system inpatients and outpatients. ASAIO J. 1999;45(3):218–225. doi: 10.1097/00002480-199905000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Bunzel B, Laederach-Hofmann K, Wieselthaler G, Roethy W, Wolner E. Mechanical circulatory support as a bridge to heart transplantation: what remains? Long-term emotional sequelae in patients and spouses. J Heart Lung Transplant. 2007;26(4):384–389. doi: 10.1016/j.healun.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 13.Shreenivas SS, Rame JE, Jessup M. Mechanical circulatory support as a bridge to transplant or for destination therapy. Curr Heart Fail Rep. 2010;7(4):159–166. doi: 10.1007/s11897-010-0026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marcuccilli L, Casida J. From insiders’ perspectives: adjusting to caregiving for patients with left ventricular assist devices. Prog Transplant. 2011;21(2):137–143. doi: 10.1177/152692481102100209. [DOI] [PubMed] [Google Scholar]
- 15.Baker K, Flattery M, Salyer J, Haugh KH, Maltby M. Caregiving for patients requiring left ventricular assistance device support. Heart & Lung. 2010;39(3):196–200. doi: 10.1016/j.hrtlng.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Creswell JW. Qualitative Inquiry & Research Design: Choosing Among Five Approaches. 2. Thousand Oaks: Sage Publications; 2007. [Google Scholar]
- 17.Hyper RESEARCH 3.0.2 [computer program]. Version Hyper RESEARCH 3.0.22011.
- 18.Hupcey JE, Fenstermacher K, Kitko L, Penrod J. Achieving medical stability: wives’ experiences with heart failure. Clin Nurs Res. 2010;19(3):211–229. doi: 10.1177/1054773810371119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bekelman DB, Nowels CT, Retrum JH, et al. Giving voice to patients’ and family caregivers’ needs in chronic heart failure: implications for palliative care programs. J Palliat Med. 2011;14(12):1317–1324. doi: 10.1089/jpm.2011.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirkpatrick JHS, Kellom K. Pumped up, but not prepared: examining LVAD-DT patients’ comprehension of advance directive specifications. Paper presented at Heart Failure Society of America 2012 Scientfic Meeting; Seattle, WA. September 10, 2012. [Google Scholar]
- 21.Swetz KM, Freeman MR, AbouEzzeddine OF, et al. Palliative medicine consultation for preparedness planning in patients receiving left ventricular assist devices as destination therapy. Mayo Clin Proc. 2011;86(6):493–500. doi: 10.4065/mcp.2010.0747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rizzieri AG, Verheijde JL, Rady MY, McGregor JL. Ethical challenges with the left ventricular assist device as a destination therapy. Philos Ethics Humanit Med. 2008;3:20. doi: 10.1186/1747-5341-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hupcey JE, Fenstermacher K, Penrod J, Boehmer J. The changing face of heart failure: a needs-driven, anticipatory palliative care model. Circulation. 2008;117(21):E425. [Google Scholar]
- 24.Swetz K, Ottenberg A, Freeman M, Mueller P. Palliative care and end-of-life issues in patients treated with left ventricular assist devices as destination therapy. Curr Heart Fail Rep. 2011;8(3):212–218. doi: 10.1007/s11897-011-0060-x. [DOI] [PubMed] [Google Scholar]
- 25.MacIver J, Ross HJ. Withdrawal of ventricular assist device support. J Palliat Care. 2005;21(3):151–156. [PubMed] [Google Scholar]
- 26.Mueller PS, Swetz KM, Freeman MR, et al. Ethical analysis of withdrawing ventricular assist device support. Mayo Clin Proc. 2010;85(9):791–797. doi: 10.4065/mcp.2010.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]