Abstract
Contrast-induced encephalopathy after cerebral angiography is a rare complication and until now, only few cases have been reported. This paper reports on contras-induced encephalopathy mimicking meningoencephalitis after cerebral angiography by using iodixanol, an iso-osmolar non-ionic contrast agent. A 58-year-old woman underwent cerebral angiography for the evaluation of multiple intracranial aneurysms. A few hours later, she had persistent headache, vomiting, fever, and seizures. Brain computed tomography (CT) showed sulcal obliteration of right cerebral hemisphere and cerebrospinal fluid profile was unremarkable. The next day, she developed left side hemiparesis, sensory loss, and left-sided neglect with drowsy mentality. Brain magnetic resonance imaging (MRI) showed cerebral swelling with leptomeningeal enhancement in the right parieto-occipital lobe without sign of ischemia or hemorrhage. The patient was managed with intravenous dexamethasone, mannitol and anticonvulsant. There was a progressive neurological improvement with complete resolution of the symptoms at day 6. This observation highlights that contrast-induced encephalopathy can be caused by an iso-osmolar non-ionic contrast agent. This rare entity should be suspected if neurologic deterioration after cerebral angiography is not explained by other frequent causes such as acute infarction or hemorrhage.
Keywords: Contrast, Encephalopathy, Angiography
INTRODUCTION
Contrast-induced encephalopathy is a rare complication of cerebral angiography. The reported incidence of transient cortical blindness is 1% or less for vertebral angiography13),20) and 2.9% with endovascular coil treatment of posterior circulation aneurysms.19) Although most cases have been presented with transient cortical blindness in the literature, contrast-induced encephalopathy mimicking meningitis has rarely been reported to our knowledge. Furthermore, only a few cases of contrast-induced encephalopathy using iodixanol, an iso-osmolar non-ionic contrast agent, have been reported up to now.4),11) Here, we describe a case of contrast-induced encephalopathy mimicking meningitis after cerebral angiography by using iodixanol.
CASE REPORT
A 58-year-old woman was found to have multiple intracranial aneurysms on screening brain computed tomography (CT) angiogram. She had past medical histories of hypertension, hypothyroidism, peripheral artery occlusive disease, and depressive disorder. She underwent cerebral angiography and received a total of 220 mL of iodixanol (Visipaque 320, GE Healthcare, Cork, Ireland). Continuous heparinized saline was infused during cerebral angiography. Cerebral angiography showed multiple intracranial aneurysms. There was no complication during the procedure.
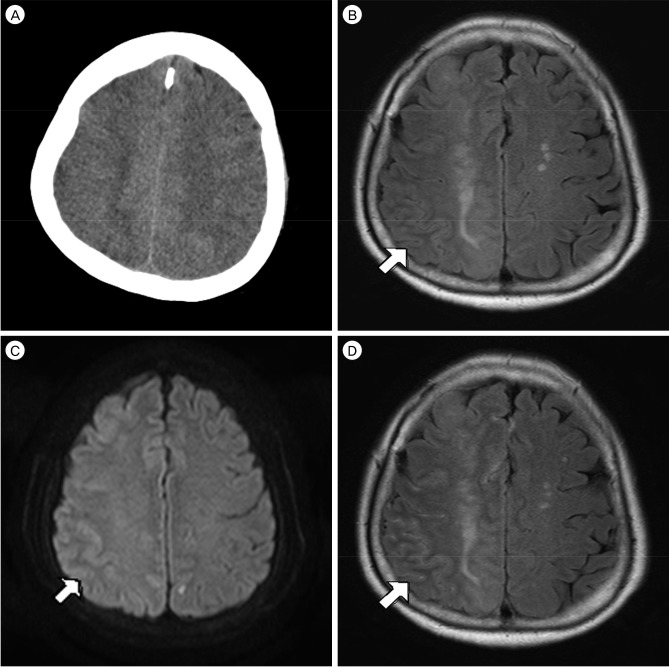
But after the procedure the patient had persistent headache and vomiting. A few hours later, she had fever up to 39.5℃. Non-contrast brain CT showed sulcal obliteration of right cerebral hemisphere (Fig. 1A). And then she developed a generalized tonic-clonic seizure for a few seconds. Laboratory studies showed an increased white blood cell count of 13.0 × 103/µL and a normal level of C-reactive protein. The next day, left hemiparesis involving face, arm and leg (grade 3/5), sensory loss, and left-sided neglect with drowsy mentality were developed. To exclude thromboembolic complications, we performed brain magnetic resonance imaging (MRI). MRI showed gyral swelling and hyperintensity in the right cerebral hemisphere on T2-weighted fluid-attenuated inversion recovery (FLAIR) image (Fig. 1B). The diffusion weighted image (DWI) revealed gyriform hyperintensity (Fig. 1C) in the right cerebral hemisphere, while the apparent diffusion coefficient (ADC) showed no alteration. Gadolinium-enhanced T2-weighted FLAIR image showed diffuse leptomeningeal enhancement of right parieto-occipital lobe (Fig. 1D).
Fig. 1. Brain CT obtained 10 hours after cerebral angiography shows sulcal obliteration of right cerebral hemisphere (A). Brain MRI shows gyral swelling on T2-weighted fluid-attenuated inversion recovery (FLAIR) image (arrow) (B), and hyperintensity in the right cerebral hemisphere on diffusion weighted image (DWI) (arrow) (C). Gadolinium-enhanced T2-weighted FLAIR image shows leptomeningeal enhancement of right parieto-occipital lobe (arrow) (D). CT = computed tomography; MRI = magnetic resonance imaging.
To rule out the possibility of meningoencephalitis, we also carried out a spinal tapping. An opening pressure was 120 mm H2O and the cerebrospinal fluid (CSF) was clear, with a normal red blood cell count of 0/µL, a normal white blood cell count of 5/µL, a slightly elevated protein level of 93.5 mg/dL and a slightly elevated glucose level of 87 in CSF analysis. Because other causes such as ischemic complication and meningitis were ruled out, the pattern of gyriform swelling and enhancement was interpreted as contrast-induced encephalopathy being caused by extravasation of contrast through disrupted blood-brain barrier.
Due to the progressive neurological deterioration, the patient was sedated and intubated. The patient was managed by hydration with enough fluid, and intravenous dexamethasone, mannitol and anticonvulsant.
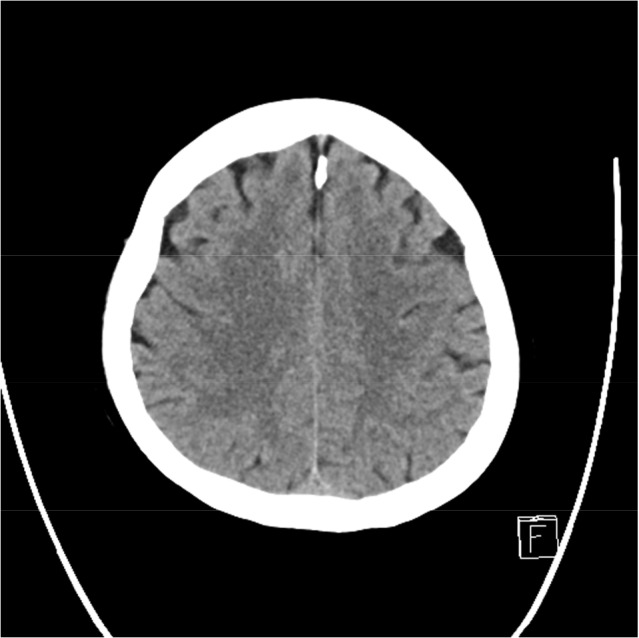
The patient showed a progressive neurological improvement, and on day 6, her mental status, left motor weakness, sensory deficit and left-sided neglect were completely recovered. Follow-up brain CT showed resolution of sulcal obliteration of right hemisphere (Fig. 2).
Fig. 2. Brain CT obtained 6 days after cerebral angiography shows improved sulcal obliteration of right cerebral hemisphere. CT = computed tomography.
DISCUSSION
The mechanism and causes of contrast-induced neurotoxicity is controversial. The blood-brain barrier is impermeable to contrast material under normal conditions. In high concentrations, contrast agents can damage the blood-brain barrier and facilitate its own entry into the brain.3) This disruption of the blood-brain barrier is related to physical or chemical factors of contrast media, such as osmolality, lipid solubility and ionicity, and intraluminal pressure of selective vessel.7),10),16),17) Theoritically, hyperosmolality opens tight junctions between cerebrovascular endothelial cells of the blood-brain barrier by shrinking the cells osmotically through which the contrast media then can enter the brain.17) Furthermore, ionic agents produce further blood-brain barrier disruption than non-ionic agents in animal studies.10) However, osmolality and ionicity are not essential requirements for blood-brain barrier disruption, because encephalopathy has been reported in cases with iodixanol, an iso-osmolar non-ionic contrast agent.4),11) Our case report also strengthens these findings, so the other physical or chemical property such as lipid solubility or the increase in intraluminal pressure caused by injection of the contrast agent may have contributed to blood-brain barrier disruption.
In our case, we used a total of 220 mL of iodixanol due to evaluation of multiple aneurysms, which is relatively large amount in single session cerebral angiography. Some studies have showed a significant relationship between cortical hyperdensity on brain CT and the total amount of contrast material following embolization of intracranial aneurysms.1),2),14) On the contrary, contrast-induced neurotoxicity has been reported in several patients with contrast volumes less than 40 mL.9),15) In these reports, there was no specific contrast dose that led to contrast gyral enhancement. Based on these findings, contrast-induced encephalopathy appears to be an idiosyncratic reaction to contrast rather than dose-related.
Typical CT findings include abnormal cortical and subcortical contrast enhancement, cerebral edema, and subarachnoid contrast enhancement similar to subarachnoid hemorrhage. On MRI, gyral swelling and hyperintensity on T2 FLAIR image and DWI, not accompanied by changes on ADC, have been described in the previously reported cases.5),6),18) Our case also showed radiologic findings coincident with previous reports. If sudden neurologic deterioration is not explained by other cause after contrast injection, CT and MRI may be helpful for differential diagnosis.
Reported demographic risk factors for contrast-induced encephalopathy include hypertension and renal failure.8),12) Chronic hypertension is the most important risk factor. The cerebral autoregulatory capacity in these patients is usually compromised. Our patient had chronic hypertension and peripheral artery occlusive disease. It was likely that her cerebral autoregulatory capacity was also compromised. Since the posterior circulation is more susceptible to damage by blood pressure changes, this phenomenon occurs predominantly in the parieto-occipital cortex like posterior reversible encephalopathy syndrome (PRES). Thus, cortical blindness and seizures are common clinical presentations of contrast-induced encephalopathy. But it should be kept in mind that extravasation of contrast media can also cause chemical meningitis like our patients.
The prognosis of contrast-induced encephalopathy is generally reported as favorable with rapid recovery. It usually occurs and improves within 48-72 hours. But there are several published cases that showed persistent neurologic deficits.12) Although there is no definitive prevention and treatment for this complication, adequate hydration with intra-arterial saline infusion during angiography and intravenous fluids is recommended. Intravenous steroids and mannitol for control of cerebral edema may be helpful for some patients.
CONCLUSION
Our reports and literature show that even iodixanol, an iso-osmolar non-ionic contrast agent, can cause contrast-induced encephalopathy and mimic meningitis. Therefore, contrast-induced encephalopathy should be considered as differential diagnosis for a patient who has an acute neurologic symptom after cerebral angiography, regardless of the type of contras agent. Neurological imaging is essential to rule out other more frequent and severe complications such as acute cerebral infarction or intracranial hemorrhage.
Footnotes
Disclosure: The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Baik SK, Kim YS, Lee HJ, Park J, Kim GC. Immediate CT findings following embolization of cerebral aneurysms: suggestion of blood-brain barrier or vascular permeability change. Neuroradiology. 2008 Mar;50(3):259–266. doi: 10.1007/s00234-007-0332-z. [DOI] [PubMed] [Google Scholar]
- 2.Brisman JL, Jilani M, McKinney JS. Contrast enhancement hyperdensity after endovascular coiling of intracranial aneurysms. AJNR Am J Neuroradiol. 2008 Mar;29(3):588–593. doi: 10.3174/ajnr.A0844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Broman T, Olsson O. The tolerance of cerebral blood-vessels to a contrast medium of the diodrast group: An experimental study of the effect on the blood-brain-barrier. Acta Radiologica. 1948 Jul;30(4-5):326–342. [Google Scholar]
- 4.Chisci E, Setacci F, de Donato G, Setacci C. A case of contrast-induced encephalopathy using iodixanol. J Endovasc Ther. 2011 Aug;18(4):540–544. doi: 10.1583/11-3476.1. [DOI] [PubMed] [Google Scholar]
- 5.Frontera JA, Pile-Spellman J, Mohr JP. Contrast-induced neurotoxicity and selective cortical injury. Cerebrovasc Dis. 2007;24(1):148–151. doi: 10.1159/000103621. [DOI] [PubMed] [Google Scholar]
- 6.Guimaraens L, Vivas E, Fonnegra A, Sola T, Soler L, Balaguer E, et al. Transient encephalopathy from angiographic contrast: a rare complication in neurointerventional procedures. Cardiovasc Intervent Radiol. 2010 Apr;33(2):383–388. doi: 10.1007/s00270-009-9609-4. [DOI] [PubMed] [Google Scholar]
- 7.Hansson HA, Johansson B, Blomstrand C. Ultrastructural studies on cerebrovascular permeability in acute hypertension. Acta Neuropathol. 1975 Aug;32(3):187–198. doi: 10.1007/BF00696568. [DOI] [PubMed] [Google Scholar]
- 8.Kocabay G, Karabay CY, Kalayci A, Akgun T, Guler A, Oduncu V, et al. Contrast-induced neurotoxicity after coronary angiography. Herz. 2014 Jun;39(4):522–527. doi: 10.1007/s00059-013-3871-6. [DOI] [PubMed] [Google Scholar]
- 9.Lantos G. Cortical blindness due to osmotic disruption of the blood-brain barrier by angiographic contrast material: CT and MRI studies. Neurology. 1989 Apr;39(4):567–571. doi: 10.1212/wnl.39.4.567. [DOI] [PubMed] [Google Scholar]
- 10.Latchaw RE. The use of nonionic contrast agents in neuroangiography. A review of the literature and recommendations for clinical use. Invest Radiol. 1993 Nov;28(Suppl 5):S55–S59. doi: 10.1097/00004424-199311001-00017. discussion S60-1. [DOI] [PubMed] [Google Scholar]
- 11.Law S, Panichpisal K, Demede M, John S, Marmur JD, Nath J, et al. Contrast-Induced Neurotoxicity following Cardiac Catheterization. Case Rep Med. 2012;2012:267860. doi: 10.1155/2012/267860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leong S, Fanning NF. Persistent neurological deficit from iodinated contrast encephalopathy following intracranial aneurysm coiling. A case report and review of the literature. Interv Neuroradiol. 2012 Mar;18(1):33–41. doi: 10.1177/159101991201800105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mani RL, Eisenberg RL. Complications of catheter cerebral arteriography: analysis of 5,000 procedures. III. Assessment of arteries injected, contrast medium used, duration of procedure, and age of patient. AJR Am J Roentgenol. 1978 Nov;131(5):871–874. doi: 10.2214/ajr.131.5.871. [DOI] [PubMed] [Google Scholar]
- 14.Ozturk A, Saatci I, Pamuk AG, Erdogan C, Akmangit I, Geyik S, et al. Focal increased cortical density in immediate postembolization CT scans of patients with intracranial aneurysms. AJNR Am J Neuroradiol. 2006 Oct;27(9):1866–1875. [PMC free article] [PubMed] [Google Scholar]
- 15.Potsi S, Chourmouzi D, Moumtzouoglou A, Nikiforaki A, Gkouvas K, Drevelegas A. Transient contrast encephalopathy after carotid angiography mimicking diffuse subarachnoid haemorrhage. Neurol Sci. 2012 Apr;33(2):445–448. doi: 10.1007/s10072-011-0765-3. [DOI] [PubMed] [Google Scholar]
- 16.Rapoport SI, Levitan H. Neurotoxicity of X-ray contrast media. Relation to lipid solubility and blood-brain barrier permeability. Am J Roentgenol Radium Ther Nucl Med. 1974 Sep;122(1):186–193. doi: 10.2214/ajr.122.1.186. [DOI] [PubMed] [Google Scholar]
- 17.Rapoport SI, Thompson HK, Bidinger JM. Equi-osmolal opening of the blood-brain barrier in the rabbit by different contrast media. Acta Radiol Diagn (Stockh) 1974 Jan;15(1):21–32. doi: 10.1177/028418517401500103. [DOI] [PubMed] [Google Scholar]
- 18.Saigal G, Bhatia R, Bhatia S, Wakhloo AK. MR findings of cortical blindness following cerebral angiography: is this entity related to posterior reversible leukoencephalopathy? AJNR Am J Neuroradiol. 2004 Feb;25(2):252–256. [PMC free article] [PubMed] [Google Scholar]
- 19.Shinoda J, Ajimi Y, Yamada M, Onozuka S. Cortical blindness during coil embolization of an unruptured intracranial aneurysm--case report. Neurol Med Chir (Tokyo) 2004 Aug;44(8):416–419. doi: 10.2176/nmc.44.416. [DOI] [PubMed] [Google Scholar]
- 20.Wishart DL. Complications in vertebral angiography as compared to non-vertebral cerebral angiography in 447 studies. Am J Roentgenol Radium Ther Nucl Med. 1971 Nov;113(3):527–537. doi: 10.2214/ajr.113.3.527. [DOI] [PubMed] [Google Scholar]