Abstract
Objectives
The aim of this study was to test a hypothesized mediation model to explain associations between mothers’ dental anxiety and children’s dental utilization through the mothers’ own dental utilization.
Methods
Two hundred and twenty three low-income African-American mothers with young children (age 31–59 months) completed a study questionnaire which assessed (i) mothers’ dental anxiety; (ii) mothers’ dental utilization (seeing a dentist at least once a year) and (iii) children’s dental utilization (at least one non-study-related dental visit during the 36-month study period). The hypothesized mediation model consisted of these three elements with both a direct path from mothers’ dental anxiety to children’s dental utilization and an indirect path from mothers’ dental anxiety to children’s dental utilization through mothers’ dental utilization. Mediation analysis with bootstrapping was conducted to test the hypothesized model.
Results
The mediation analysis indicated significant total effect of mothers’ dental anxiety on children’s dental utilization. The standardized total effect of mothers’ anxiety on children’s dental utilization was −0.164 (SE=0.084, p=0.050), and the standardized indirect effect of mothers’ anxiety on children’s dental utilization mediated by mothers’ dental utilization was −0.072 (SE=0.039, p=0.068). The direct effect from mothers’ anxiety to children’s dental utilization was not statistically significant (p=0.313) after adjusting for the mothers’ dental utilization.
Conclusions
In this low-income African-American sample, there was a trend for mothers’ dental anxiety to be associated with children’s dental utilization indirectly through mothers’ own dental utilization, while the direct influence of mothers’ dental anxiety on children’s dental utilization was not seen. This suggests that mothers’ dental utilization might explain how mothers’ dental anxiety impacts children’s early dental utilization.
Keywords: Parents, Child, Poverty, African-American, Questionnaire, Dental Anxiety, Dental Health Services
Introduction
In the United States (U.S.), children from low-income families and those from some minority populations, such as African-Americans, have significantly more dental caries than more affluent and non-minority counterpart populations1–5. A recent review of the U.S. Medical Expenditures Panel Survey (MEPS) found children with Medicaid dental coverage had a very low rate of preventive dental visits (29.2%) in a two-year period (2010–2012)6. In this same study, Hispanic and non-Latino Black children were less likely to receive dental care compared to non-Hispanic White children (34.7% and 34.8% versus 47.3%, respectively). Yang and colleagues7 found several factors associated with poor oral health and high levels of dental caries in U.S. children including identifying as “multi-racial” or “other race’ (p. 498), low family income, low level of maternal education, and poor maternal health. Children from minority populations who also come from low-income families, then, clearly face several barriers to adequate dental care and, by extension, good oral health.
A systematic review by Fisher-Owens and colleagues, designed to develop a conceptual etiological model for children’s dental caries, noted that children’s dental caries is a multi-factorial disease with identified risk factors ranging from the individual microbiological factor, to parental psychological and behavioral factors, to community level factors8. Furthermore, Hooley at al. suggests that negative parental factors, such as dental anxiety, prevent their children from accessing regular dental care, while positive parental factors, such as dental utilization, positively impact children’s dental utilization. Parents’ behaviors, therefore, play an important role in children’s dental caries development in addition to socio-demographic factors9.
The American Academy of Pediatric Dentistry (AAPD) guidelines for the prevention of dental caries recommend that children should visit a dentist at the eruption of the first tooth or by the their first birthday10, 11 and dentists should provide periodic comprehensive examinations, anticipatory guidance, and preventive dental services such as prophylaxis and topical fluoride treatment at these visits12. Previous reports indicated that caregivers’ dental utilization is strongly and positively related to children’s utilization, especially in low-income African-American population13–16. However, Kelly et al. reported that African-American caregivers of Medicaid-insured children had not utilized dental services for their children due to high levels of caregivers’ dental anxiety17.
Dental anxiety clearly acts as a barrier to adequate dental care18–21; approximately 75% of adults have some anxiety about going to the dentist and about 10–20% of adults indicate they have severe dental anxiety22–24. Furthermore, the prevalence of dental anxiety has not significantly changed in the U.S. from the 1960s to 200125.
We hypothesized that the dental anxiety of mothers who are primary caregivers may prevent their children’s dental utilization directly and/or indirectly. However, understanding the pathway of the impact of mothers’ dental anxiety and dental utilization on children’s dental utilization is still limited9. Given the barriers to adequate oral care for low-income African-Americans in the U.S., the understanding of this pathway among this population is an urgent need.
The aim of this study was to test a hypothesized path model to explain a path between mothers’ dental anxiety and children’s dental utilization through the mothers’ own dental utilization, using a mediation analysis.
Methods
Study Design
This secondary analysis utilized a database from a longitudinal birth cohort study that included dental anxiety and dental utilization information for both mothers (as the primary caregivers) and children. The Institutional Review Board of University Hospitals Case Medical Center reviewed and approved this study protocol.
Study Sample
The original cohort study, which investigated preterm birth and oral health, was conducted in Cleveland, Ohio, an urban city in the U.S.26. A total of 890 mothers who had a live birth from September 2007 through September 2010 were approached consecutively and recruited from two hospitals, University Hospitals Case Medical Center and MetroHealth Medical Center. Three hundred twenty four mothers did not participants or were not eligible according to inclusion and exclusion criteria. e.g. Mothers who had a history of mental illness and/or substance abuse listed in their medical records were not eligible. A total of 566 mothers consented to participate. The participants were asked to bring their children at the age of 8 months, 18–20 months, and 36 months to the research unit at one of the two hospitals. The mothers were asked to complete questionnaires including their own and their children’s demographic information and oral health behavior, while their children received a toothbrush prophylaxis treatment, oral screening examination, fluoride varnish application and oral health instruction three times during the study. The total number of participants who visited the research sites for the original cohort study at 8, 18–20 and 36-month appointments were 410, 406, and 395, respectively.
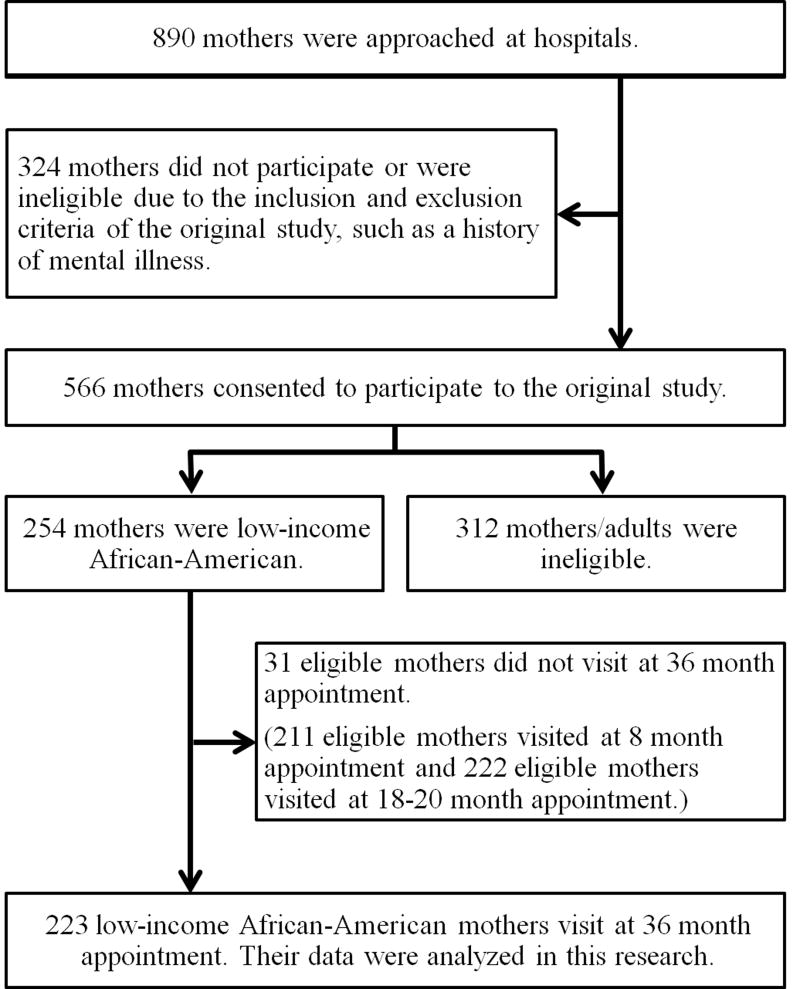
We extracted a sample of low-income African-American mothers receiving Medicaid, who were primary caregivers attending the 36-month appointments, as our target population from the original study. Two hundred fifty-four mothers were eligible for this research at the time of recruitment. Data from 223 mothers and children were collected at the 36-month appointment (children’s mean (s.d.) age = 39.57 (5.45) months, range = 31–59 months) and analyzed for this study. (Figure 1)
Figure 1.
Summary of participant recruitment and retention
Measures
The questionnaire was written in English at approximately a 6th grade reading level. The questionnaire contained the Modified Dental Anxiety Scale (MDAS), questions about mothers’ and children’s dental utilization as well as mothers’ demographic characteristics. The MDAS was used to measure mothers’ dental anxiety with five questions regarding anticipation of a dental visit the next day; scores range from 5–20, with higher scores indicating greater anxiety27, 28. The MDAS is one of the most commonly used measurements of dental anxiety and it has been translated into many languages29–34. The internal consistency of the MDAS (alpha) was 0.7 in people with dental anxiety; the test-retest reliability was more than 0.8. The concurrent and discriminate validities are also high28, 35.
Two dental utilization questions were modified from the National Health and Nutrition Examination Survey III (NHANES III). Question 1, “How often do you see a dentist or dental hygienist?” (At least once a year; every 2 years; less often than every 2 years; whenever needed, no regular schedule; other, or does not go anymore; never), was used to detect the frequency of mothers’ dental utilization. This question was dichotomized into binary answers; whether the mother sees a dentist at least once a year or not. Question 2, “Has your child ever been seen by a dentist?” (yes/no), was used to detect whether the child had a dental visit during the study period. Mothers were instructed by the researcher in the original cohort study not to count the study visits as a dental visit.
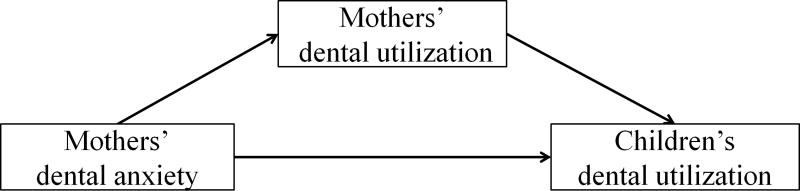
Hypothesized model
A hypothesized model was developed based on previous research results. First, people with dental anxiety avoid dental visits even if they experience dental needs18–21. Second, caregivers’ dental utilization is positively associated with their children’s dental utilization13–16. Third, caregivers’ dental anxiety is negatively associated with their children’s dental utilization36, 37.
The hypothesized model consisted of three variables: (I) mothers’ dental anxiety level as an exposure, (II) mothers’ dental utilization (seeing a dentist at least once per year) as a mediator, and (III) children’s dental utilization (dental visit during the study period) as an outcome (Figure 2).
Figure 2.
The mediation model
Statistical Analyses
After the analyses of participants’ characteristics, student t-tests and chi-square tests were utilized to investigate the relationships among mothers’ dental anxiety and mothers’ and children’s dental utilization.
To test both direct and indirect effects of mothers’ dental anxiety on their children’s dental utilization, a mediation analysis was performed38. The mediation analysis using a probit link for the binary endogenous variables (both mothers’ and children’s dental utilization) was conducted. The probit model can also be conceptualized as a threshold model similar in principal to tetrachoric correlation. Thus, the coefficient/effect size for the pathways between the mothers’ and children’s dental utilization can be interpreted as the effect of latent continuous traits upon each other39. Model coefficients (standardized) were estimated by Weighted Least Squares Means and Variance adjusted with Monte Carlo simulation for numerical integration. Standard errors for the Standardized Indirect Effect and Standardized Direct Effect were calculated using the bootstrap approach. The goodness-of-fit test of this model was not indicated as the model was saturated. The mediation analysis for this study was done by using Mplus Version 7.2 (Muthén & Muthén, Los Angeles, Calif., USA).
Results
Demographic characteristics of the mothers who did not attend the 36-month appointment (n=31) including the average of mothers’ age, education level (graduated from high school or not) and marital status (married, living with partner, or single) were compared with the characteristics of participants (n=223) whose data were analyzed, and found there were no significant differences of the characteristics between them: mothers’ age (t=−1.00, df=252, p=0.316): education level (Pearson Chi-Square=1.25, df=1, p=0.263): marital status (Fisher’s Exact test p=1.000). Mothers’ mean age was 24.9 years (s.d.=4.8; range=17–40 years). Approximately four-fifths of mothers (83.0%) completed high school and 80.3% of mothers were single. The mean MDAS score was 14.51 (s.d.=5.6; range=5–25).
Mothers’ dental anxiety was associated with decreased dental utilization in both mothers and children. Table 1 shows the differences in mothers’ dental anxiety between dental utilization patterns: Mothers who saw a dentist at least once per year had significantly lower MDAS scores than mothers who saw a dentist less than once a year (t=3.01, df=208, p=0.002).
Table 1.
Comparisons of mothers’ dental anxiety by differences in dental utilization
| Dental utilization | Mean (SD) of mother’s MDAS scores |
Statistics |
|---|---|---|
| Mothers’ dental utilizationi | ||
| Yes (n=93) | 13.4 (5.1) | t=3.01, df=208 p=0.002 |
| No (n=117) | 15.7 (5.6) | |
|
| ||
| Children’s dental utilizationii | ||
| Yes (n=113) | 13.8 (5.1) | t=1.94, df=208.8 p=0.054 |
| No (n=107) | 15.3 (6.0) | |
: seeing a dentist at least once a year, n=210, the number of missing data was 13.
: at least one dental visit during the study period, n=220, the number of missing data was 3.
Table 2 shows the relationship between mothers’ and children’s dental utilization. Increased mothers’ dental utilization was strongly associated with increased children’s dental utilization. Mothers who saw a dentist at least once per year took their children to a dentist during the study period significantly more often than mothers who saw a dentist less than once a year (Pearson Chi-Square=7.15, df=1, p=0.008).
Table 2.
Relationship between mothers’ and children’s dental utilization
| Children’s dental utilizationii | |||
|---|---|---|---|
| Yes | No | ||
| Mothers’ dental utilizationi | Yes | 66 (55.9%) | 52 (44.1) |
|
|
|||
| No | 34 (37.0%) | 58 (63.0%) | |
|
| |||
| Pearson Chi-Square=7.15, df=1, p=0.008 | |||
n=210, the number of missing data was 13.
: seeing a dentist at least once a year
: at least one dental visit during the study period
Mediation analysis
Table 3 shows the direct unstandardized effects between all variables and the standardized total, direct, and indirect effects of mothers’ dental anxiety on children’s dental utilization. The indirect effect was defined as the amount of the effect of one variable upon another which explained by intermediate variables (mothers’ dental utilization)40. We have used standardized values for the decomposition of the effects so they can be interpreted on a correlation-like scale. The standardized estimated beta-coefficient of the total effect of mothers’ dental anxiety on the children’s dental visit during the study period was −0.164 (SE=0.084, p=0.050). The indirect effect of mothers’ dental anxiety on children’s dental utilization mediated by mother’s dental utilization indicated a trend of the effect (standardized estimated beta-coefficient = −0.072, SE=0.039, p=0.068) and the mothers’ dental anxiety did not show a significant direct effect on children’s dental utilization (standardized estimated beta-coefficient = −0.092, SE=0.091, p=0.313).
Table 3.
The results of the mediation analysis
| Unstandardized Estimated β-coefficients | S.E. | P-Value (Two-Tailed) | |
|
| |||
| Mothers’ dental anxiety → Mothers’ dental utilization | |||
| −0.049 | 0.016 | 0.002 | |
| Mothers’ dental utilization → Children’s dental utilization | |||
| 0.264 | 0.107 | 0.013 | |
| Mothers’ dental anxiety → Children’s dental utilization | |||
| −0.017 | 0.017 | 0.325 | |
|
| |||
| Standardized Estimated β-coefficients | S.E. | P-Value (Two-Tailed) | |
|
| |||
| Total effects of mothers’ dental anxiety on children’s dental utilization | |||
| −0.164 | 0.084 | 0.050 | |
|
| |||
| Indirect effect: | |||
| Mothers’ dental anxiety → Mothers’ dental utilization → Children’s dental utilization | |||
| −0.072 | 0.039 | 0.068 | |
|
| |||
| Direct effect: | |||
| Mothers’ dental anxiety → Children’s dental utilization | |||
| −0.092 | 0.091 | 0.313 | |
Mothers’ dental anxiety: MDAS score
Mothers’ dental utilization: seeing a dentist at least once a year
Children’s dental utilization: at least one dental visit during the study period
Discussion
Results from this study suggest that children’s early dental visits were associated with mothers’ dental anxiety indirectly, which was mediated by mother’s dental utilization, rather than a direct influence of mothers’ dental anxiety. Parents’ dental anxiety is known to be negatively associated with children’s dental utilization36, 37. During childhood and even adolescence, child dental utilization relies primarily on parental/guardian decision-making and other dental care-seeking behaviors. This time of life is critical in terms of developing good oral health behaviors, such as visiting for regular, preventive dental care.
With regard to mothers’ dental anxiety and their own dental utilization, there is extensive evidence in the literature that people who are afraid of dentists avoid regular dental visits18–21. This study also found that mothers with higher dental anxiety showed significantly less utilization of dental care than mothers with less dental anxiety.
The American Dental Association and American Academy of Pediatric Dentistry (AAPD) recommend that the first dental visit should be at the emergence of the first tooth or by the child’s first birthday10, 11. Mothers in the original cohort study were provided with recommendations to seek an early preventive dental visit for their children. Only half of the children, however, had a dental visit during the 36-month study period. Given that maternal dental utilization is associated with child dental utilization, one way increase dental visits for young children may be to work with mothers to improve their own utilization of oral health services on a regular basis.14–16.
Other factors than dental anxiety, of course, can help explain the link between mothers’ and children’s dental utilization. A concept of “dental home”, which was introduced by AAPD, is a dentist who provide a continuous dental care by family-centered way41. A number of studies42–44 have aimed to increase mothers’ and pregnant women’s association with a “dental home,” under the assumption that mothers with a dental home would be more likely to take their children to a dentist. Given this argument, it is possible that some mothers may not have taken their children to a dentist due to a lack of a dental home.
Previous studies indicated that mothers who are afraid of receiving dental care tend to avoid taking their children to the dentist36, 37. In this study, mothers who did not take their children to a dentist reported higher levels of dental anxiety than mothers who took their children to the dentist (Table 1). However, after controlling for mothers’ dental utilization, the phenomenon disappeared; mothers’ dental anxiety influenced children’s dental utilization, mediated by mothers’ dental utilization.
Children in the original study received oral examinations, fluoride varnish applications, and recommendations for dental visits. Thus, the mothers were exposed to pediatric dentists when the children visited the research site for 8 and 18–20 month appointments before the data were collected that were used in this study. Those exposures could increase the mothers’ behavior, taking their children to a dentist before the 36-month appointment for both fearful and nonfearful mothers. It has weakened the direct influence of mothers’ dental anxiety on children’s dental utilization. Nevertheless, this study showed a trend of indirect influence of mothers’ dental anxiety on children’s dental utilization.
Mothers’ dental anxiety was associated indirectly with children’s dental utilization: a mother’s high dental anxiety may lead her to delay in taking her child to a dentist. This delay might lead to an increase in a child’s dental caries incidence and subsequent invasive treatment, which might contribute to onset of the child’s dental anxiety. Furthermore, previous surveys indicate that 50–85% of adults with dental anxiety reported their anxiety began in childhood24, 45. Although further investigations are needed, dental anxiety on the part of the parent may contribute to the child’s dental anxiety due, in part, by this delay in receiving dental care46, 47. Increasing parents’ dental utilization might help increase children’s dental utilization, which in turn could prevent or reduce childhood dental caries as well as children’s dental anxiety.
As a secondary data analysis, some limitations exist in the interpretation of these results. Participants were recruited from two hospitals in a city in a nonrandomized way. Thus, participants may have some volunteer biases such as higher education level; in fact, the high school graduation rate in the current sample was higher (83%) than the rate in this general Cleveland area (59.3%)48. Higher parental educational level increases both parents’ and children’s dental utilization49. Lastly, the data were from a self-reported and cross-sectional questionnaire. The responses might be influenced by recall and social desirability bias. It is impossible to eliminate these biases without interventions. More definitive conclusions require an intervention study.
Conclusion
Among low-income African-American mothers, there was a trend for mothers’ dental anxiety to be associated indirectly with children’s dental utilization through the mediating influence of the mothers’ own dental utilization. We did not see a direct association with mothers’ dental anxiety on children’s dental utilization after controlling for mothers’ own dental utilization. Increasing mothers’ dental utilization might lead to children’s greater use of dental services.
Acknowledgments
This research was supported by NIH NIDCR RO1DE07947-01 and Clinical and Translational Science Collaborative (CTSC) UL1TR 000439. The authors thank Dr. Jeffrey Albert and Dr. Suchitra Nelson who provided critical suggestions and comments during the writing of this article.
Contributor Information
Masahiro Heima, Case Western Reserve University.
Lisa Heaton, University of Washington.
Douglas Gunzler, Case Western Reserve University.
Nathan Morris, Case Western Reserve University.
References
- 1.Dye BA, Vargas CM, Lee JJ, Magder L, Tinanoff N. Assessing the relationship between children's oral health status and that of their mothers. J Am Dent Assoc. 2011;142(2):173–183. doi: 10.14219/jada.archive.2011.0061. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; http://www.surgeongeneral.gov/library/oralhealth/ [Google Scholar]
- 3.Albino JE, Orlando VA. Promising directions for caries prevention with American Indian and Alaska Native children. Int Dent J. 2010;60(3 Suppl 2):216–222. [PubMed] [Google Scholar]
- 4.Slade GD. Epidemiology of dental pain and dental caries among children and adolescents. Community Dent Health. 2001 Dec;18(4):219–227. [PubMed] [Google Scholar]
- 5.Nunn ME, Dietrich T, Singh HK, Henshaw MM, Kressin NR. Prevalence of early childhood caries among very young urban Boston children compared with US children. J Public Health Dent. 2009 Summer;69(3):156–162. doi: 10.1111/j.1752-7325.2008.00116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berdahl T, Hudson J, Simpson L, McCormick MC. Annual Report on Children's Health Care: Dental and Orthodontic Utilization and Expenditures for Children, 2010–2012. Acad Pediatr. 2016;16(4):314–326. doi: 10.1016/j.acap.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 7.Yang AJ, Gromoske AN, Olson MA, Chaffin JG. Single and Cumulative Relations of Social Risk Factors with Children’s Dental Health and Care-Utilization Within Regions of the United States. Matern Child Health J. 2016;20(3):495–506. doi: 10.1007/s10995-015-1847-2. [DOI] [PubMed] [Google Scholar]
- 8.Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader MJ, Bramlett MD, et al. Influences on children's oral health: A conceptual model. Pediatrics. 2007;120:e510–20. doi: 10.1542/peds.2006-3084. [DOI] [PubMed] [Google Scholar]
- 9.Hooley M, Skouteris H, Boganin C, Satur J, Kilpatrick N. Parental influence and the development of dental caries in children aged 0–6 years: a systematic review of the literature. J Dent. 2012 Nov;40(11):873–885. doi: 10.1016/j.jdent.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 10.The American Academy of Pediatric Dentistry. Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. Pediatr Dent. 2014;30(7 Suppl):40–43. [PubMed] [Google Scholar]
- 11.The American Academy of Pediatric Dentistry. Policy on oral health in child care centers. Reference manual. 2011;36:33–4. [Google Scholar]
- 12.The American Academy of Pediatric Dentistry. Guideline on periodicity of examination, preventive dental services, anticipatory guidance/counseling, and oral treatment for infants, children, and adolescents. Pediatric dentistry. 2013;35(5):E148. [PubMed] [Google Scholar]
- 13.Heima M, Lee W, Milgrom P, Nelson S. Caregiver's education level and child's dental caries in African Americans: a path analytic study. Caries Res. 2015;49(2):177–183. doi: 10.1159/000368560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grembowski D, Spiekerman C, Milgrom P. Linking mother and child access to dental care. Pediatrics. 2008 Oct;122(4):e805–814. doi: 10.1542/peds.2008-0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grembowski D, Spiekerman C, Milgrom P. Linking mother access to dental care and child oral health. Community Dent Oral Epidemiol. 2009 Oct;37(5):381–390. doi: 10.1111/j.1600-0528.2009.00486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sohn W, Ismail A, Amaya A, Lepkowski J. Determinants of dental care visits among low-income African-American children. J Am Dent Assoc. 2007 Mar;138(3):309–318. doi: 10.14219/jada.archive.2007.0163. [DOI] [PubMed] [Google Scholar]
- 17.Kelly SE, Binkley CJ, Neace WP, Gale BS. Barriers to care-seeking for children's oral health among low-income caregivers. Am J Public Health. 2005;95(8):1345–1351. doi: 10.2105/AJPH.2004.045286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wigen TI, Skaret E, Wang NJ. Dental avoidance behaviour in parent and child as risk indicators for caries in 5-year-old children. Int J Paediatr Dent. 2009;19(6):431–437. doi: 10.1111/j.1365-263X.2009.01014.x. [DOI] [PubMed] [Google Scholar]
- 19.Armfield JM. Predicting dental avoidance among dentally fearful Australian adults. Eur J Oral Sci. 2013;121(3 Pt 2):240–246. doi: 10.1111/eos.12036. [DOI] [PubMed] [Google Scholar]
- 20.Freeman R. Barriers to accessing and accepting dental care. Br Dent J. 1999 Jul 24;187(2):81–84. doi: 10.1038/sj.bdj.4800208. [DOI] [PubMed] [Google Scholar]
- 21.ter Horst G, de Wit CA. Review of behavioural research in dentistry 1987–1992: dental anxiety, dentist-patient relationship, compliance and dental attendance. Int Dent J. 1993;43(3 Suppl 1):265–278. [PubMed] [Google Scholar]
- 22.Kleinknecht RA, Thorndike RM, McGlynn FD, Harkavy J. Factor analysis of the dental fear survey with cross-validation. J Am Dent Assoc. 1984;108(1):59–61. doi: 10.14219/jada.archive.1984.0193. [DOI] [PubMed] [Google Scholar]
- 23.Agras S, Sylvester D, Oliveau D. The epidemiology of common fears and phobia. Compr Psychiatry. 1969;10(2):151–156. doi: 10.1016/0010-440x(69)90022-4. [DOI] [PubMed] [Google Scholar]
- 24.Milgrom P, Fiset L, Melnick S, Weinstein P. The prevalence and practice management consequences of dental fear in a major US city. J Am Dent Assoc. 1988;116(6):641–647. doi: 10.14219/jada.archive.1988.0030. [DOI] [PubMed] [Google Scholar]
- 25.Smith TA, Heaton LJ. Fear of dental care Are we making any progress? The Journal of the American Dental Association. 2003;134(8):1101–1108. doi: 10.14219/jada.archive.2003.0326. [DOI] [PubMed] [Google Scholar]
- 26.Nelson S, Albert JM, Geng C, et al. Increased enamel hypoplasia and very low birthweight infants. J Dent Res. 2013 Sep;92(9):788–794. doi: 10.1177/0022034513497751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corah NL. Development of a dental anxiety scale. J Dent Res. 1969;48(4):596. doi: 10.1177/00220345690480041801. [DOI] [PubMed] [Google Scholar]
- 28.Humphris GM, Morrison T, Lindsay SJ. The Modified Dental Anxiety Scale: validation and United Kingdom norms. Community Dent Health. 1995;12(3):143–150. [PubMed] [Google Scholar]
- 29.Ilguy D, Ilguy M, Dincer S, Bayirli G. Reliability and validity of the Modified Dental Anxiety Scale in Turkish patients. J Int Med Res. 2005;33(2):252–259. doi: 10.1177/147323000503300214. [DOI] [PubMed] [Google Scholar]
- 30.Bahammam MA. Validity and reliability of an Arabic version of the state-trait anxiety inventory in a Saudi dental setting. Saudi Med J. 2016;37(6):668–674. doi: 10.15537/smj.2016.6.13935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gupta G, Shanbhag N, Puranik MP. Cross-Cultural Adaptation of Kannada Version of Modified Dental Anxiety Scale Among an Adult Indian Population. J Clin Diagn Res. 2015;9(9):Zc34–38. doi: 10.7860/JCDR/2015/12675.6469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Facco E, Gumirato E, Humphris G, Stellini E, Bacci C, Sivolella S, et al. Modified dental anxiety scale: validation of the italian version. Minerva stomatologica. 2015;64(6):295–307. [PubMed] [Google Scholar]
- 33.Sitheeque M, Massoud M, Yahya S, Humphris G. Validation of the Malay version of the Modified Dental Anxiety Scale and the prevalence of dental anxiety in a Malaysian population. J Investig Clin Dent. 2015;6(4):313–320. doi: 10.1111/jicd.12106. [DOI] [PubMed] [Google Scholar]
- 34.Appukuttan D, Datchnamurthy M, Deborah SP, Hirudayaraj GJ, Tadepalli A, Victor DJ. Reliability and validity of the Tamil version of Modified Dental Anxiety Scale. J Oral Sci. 2012;54(4):313–320. doi: 10.2334/josnusd.54.313. [DOI] [PubMed] [Google Scholar]
- 35.Newton JT, Edwards JC. Psychometric properties of the modified dental anxiety scale: an independent replication. Community Dent Health. 2005;22(1):40–42. [PubMed] [Google Scholar]
- 36.Goettems ML, Ardenghi TM, Demarco FF, Romano AR, Torriani DD. Children's use of dental services: influence of maternal dental anxiety, attendance pattern, and perception of children's quality of life. Community Dent Oral Epidemiol. 2012;40(5):451–458. doi: 10.1111/j.1600-0528.2012.00694.x. [DOI] [PubMed] [Google Scholar]
- 37.Milgrom P, Mancl L, King B, Weinstein P, Wells N, Jeffcott E. An explanatory model of the dental care utilization of low-income children. Med Care. 1998;36(4):554–566. doi: 10.1097/00005650-199804000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Jeon J. The Strengths and Limitations of the Statistical Modeling of Complex Social Phenomenon: Focusing on SEM, Path Analysis, or Multiple Regression Models. World Academy of Science, Engineering and Technology, Int J Soc Behav Educ Econ Bus Ind Eng. 2015;9(5):1594–1602. [Google Scholar]
- 39.Muthén B. A general structural equation model with dichotomous, ordered categorical, and continuous latent variable indicators. Psychometrika. 1984;49(1):115–132. [Google Scholar]
- 40.Bollen KA. Total, direct, and indirect effects in structural equation models. Sociol Methodol. 1987;17(1):37–69. [Google Scholar]
- 41.Milgrom P, Ludwig S, Shirtcliff RM, Smolen D, Sutherland M, Gates PA, et al. Providing a dental home for pregnant women: a community program to address dental care access–a brief communication. Journal of public health dentistry. 2008;68(3):170–173. doi: 10.1111/j.1752-7325.2007.00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Milgrom P, Sutherland M, Shirtcliff RM, Ludwig S, Smolen D. Children's tooth decay in a public health program to encourage low-income pregnant women to utilize dental care. BMC Public Health. 2010;10(1):1. doi: 10.1186/1471-2458-10-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Milgrom P, Sutherland M, Shirtcliff RM, Ludwig S, Smolen D. Children's tooth decay in a public health program to encourage low-income pregnant women to utilize dental care. BMC Public Health. 2010;10(1):1. doi: 10.1186/1471-2458-10-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Margolis PA, Stevens R, Bordley WC, Stuart J, Harlan C, Keyes-Elstein L, et al. From concept to application: the impact of a community-wide intervention to improve the delivery of preventive services to children. Pediatrics. 2001;108(3):e42–e42. doi: 10.1542/peds.108.3.e42. [DOI] [PubMed] [Google Scholar]
- 45.Locker D, Liddell A, Dempster L, Shapiro D. Age of onset of dental anxiety. J Dent Res. 1999;78(3):790–796. doi: 10.1177/00220345990780031201. [DOI] [PubMed] [Google Scholar]
- 46.Crego A, Carrillo-Diaz M, Armfield JM, Romero M. Applying the Cognitive Vulnerability Model to the analysis of cognitive and family influences on children's dental fear. Eur J Oral Sci. 2013;121(3 Pt 1):194–203. doi: 10.1111/eos.12041. [DOI] [PubMed] [Google Scholar]
- 47.Themessl-Huber M, Freeman R, Humphris G, MacGillivray S, Terzi N. Empirical evidence of the relationship between parental and child dental fear: a structured review and meta-analysis. Int J Paediatr Dent. 2010;20(2):83–101. doi: 10.1111/j.1365-263X.2009.00998.x. [DOI] [PubMed] [Google Scholar]
- 48.The Cleveland Metropolitan School District [Internet] Fact sheet. Cleveland, Ohio: 2015. Available from: http://www.clevelandmetroschools.org/domain/24. Archived by WebCite® at http://www.webcitation.org/6Zu2Ar2VV. [Google Scholar]
- 49.Tchicaya A, Lorentz N. Socioeconomic inequalities in the non-use of dental care in Europe. Int J Equity Health. 2014;13:7. doi: 10.1186/1475-9276-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]