Abstract
Purpose
To describe a possible causal relationship between ocular cicatricial pemphigoid (OCP) and ocular surface squamous neoplasia.
Methods
Two middle aged female patients with already diagnosed OCP were studied in regard to the subsequent onset of conjunctival squamous neoplasia. Their clinical histories, ocular examinations, clinical photographs, and results of biopsies and any ancillary immunofluorescent laboratory evaluation studies were carefully reviewed.
Results
One patient had a pre-invasive squamous dysplasia and the other an invasive squamous cell carcinoma, both in the unequivocal setting of OCP with bilateral conjunctivitis, symblephara, and forniceal foreshortening. The patients had been receiving intensive immunotherapy consisting of some combination of corticosteroids, rituximab and interferon-alpha. Both patients had a positive immunofluorescent study demonstrating immunoreactants at the level of the epithelial basement membrane. Each patient had two earlier negative immunofluorescent studies before a third was positive.
Conclusions
While rare, there is one previous report of an association between OCP and conjunctival squamous neoplasia. The current report provides more data supporting the proposal that this conjunction is more than a random event. Repeat immunofluorescent studies after an initial negative result in a patient with strong clinical signs of OCP are imperative due to the frequency of false negative studies in the context of clinically persuasive disease.
Keywords: ocular cicatricial pemphigoid, conjunctiva, ocular surface squamous neoplasia, squamous cell carcinoma
Introduction
Ocular cicatricial pemphigoid (OCP) is an autoimmune disorder characterized by inflammation and scarring of the conjunctiva. Diagnosis is based on clinical findings and direct immunofluorescent evaluation of a biopsy. Treatment typically consists of a combination of systemic immunosuppressive therapy and surgery.1 Squamous cell dysplasia eventuating in invasive carcinoma (SCC) of the conjunctiva is strongly associated with ultraviolet radiation, human immunodeficiency virus (HIV), and human papillomavirus (HPV).2,3 It most commonly arises in the para-limbal bulbar conjunctiva and is treated with surgical excision and/or topical therapy with interferon alpha-2b or anti-metabolites.4 Two cases are described in this study who had squamous cell neoplasia (a term embracing both dysplasia and carcinoma) of the inferior palpebral conjunctiva developing in the setting of OCP. All collection and evaluation of protected patient health information were HIPAA compliant.
Case Reports
Case 1
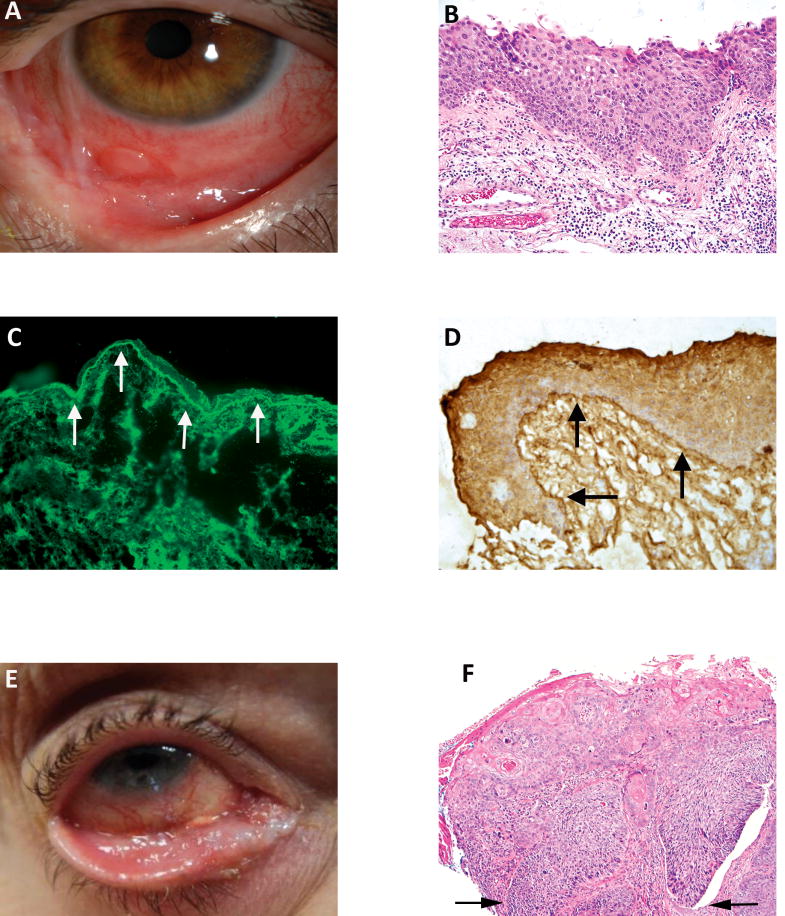
A 53 year-old woman with chronic conjunctivitis of the left eye that was previously treated with topical corticosteroids presented with symblepharon formation of the inferonasal conjunctiva. An incisional biopsy of the conjunctiva revealed chronic inflammation with intraepithelial dysplasia but negative direct immunofluorescence. She was treated with topical corticosteroids and lubrication for 2.5 years. She then developed right eye irritation and was noted to have new symblepharon formation of the right inferior fornix with a patch of keratinized tarsal conjunctiva. Examination of the left eye at this time revealed severe inferior symblephara with significant injection, and a pink, sessile nodular appearance of the entire inferior fornix (Figure 1A) that on biopsy was diagnosed as squamous dysplasia with a negative immunofluorescent study for OCP. A repeat incisional biopsy of the left inferior fornix showed squamous carcinoma in situ (Figure 1B and C) and again a negative direct immunofluorescent study. Given the high suspicion for possible OCP, another biopsy of the left inferior fornix was performed and sent to a different laboratory; on this occasion direct immunofluorescence was positive for OCP with the identification of IgG, IgA and fibrinogen at the level of the epithelial basement membrane (Figure 1E). Confirmatory immunoperoxidase staining was also obtained (Figure 1F). Interferon alpha 2b drops and methotrexate were started with plan for close monitoring.
Figure 1.
A. Case 1. Mild symblepharon formation with sparing of the cornea and diffuse epibulbar inflammation in a 53 year old woman with OCP. Note the nodule lateral to the symblepharon as well as others in the inferior fornix.
B. Thickening of the conjunctival epithelium with neoplastic cells at the stage of carcinoma in situ. There is underlying lymphocytic and eosinophilic infiltration in the substantia propria.
C. Immunofluorescent microscopy demonstrates immunoreactant fibrinogen deposition along the epithelial basement membrane (arrows).
D. Immunohistochemical demonstration of IgG deposition at the epithelial basement membrane level employing the Avidin-Biotin-Complex (ABC) method.
E. Case 2. Severe right ocular symblepharon formation with foreshortening of the fornix. There is a background inflammation that led to the diagnosis of ocular cicatricial pemphigoid (OCP) in a 66 year old woman. The nodular surface irregularity intimates the possibility of coexistent neoplasia.
F. The cells in the epithelium are arranged in a disorderly fashion with pleomorphic nuclei and there is invasion of the substantia propria (arrows).
(B and F, hematoxylin and eosin; B, 20×; F, 10×; C, immunofluorescence 20×; D, avidin-biotin-complex, 20×)
Case 2
A 66 year-old woman with a 2-year history of OCP managed with dapsone, rituximab, and intravenous immunoglobulin (IVIG) was noted by her managing ophthalmologist to have a persistent right lower lid (RLL) lesion. On examination, there was an elevated, pink, nodular lesion on the medial margin of the RLL with extension of similar lumps onto the tarsal conjunctiva towards the inferior fornix (Figure 1E). Additional cicatricial changes and symblephara were noted in bilateral inferior fornices, consistent with OCP. An incisional biopsy of the RLL lesion showed squamous cell carcinoma in situ extending to the margins. The patient was started on interferon alpha-2b drops (1 million International Units (IU)/cc) with close monitoring. She tolerated therapy without complications. After 6 months, however, repeat biopsy was performed due to the presence of persistent lesions. Histopathology confirmed invasive SCC and the decision was made to begin further therapy with intralesional injection of interferon alpha-2b (10 million IU/cc). Two separate immunofluorescent studies separated by 4 years were negative for OCP and a third subsequent study conducted at a different laboratory was positive for OCP.
Discussion
OCP is a systemic autoimmune disorder caused by type II immune reaction that leads to cicatrizing conjunctivitis and symblepharon formation and compromise of the ocular surface and cornea.1 Symptoms at the time of onset are often nonspecific and insidious, and require a high index of suspicion for diagnosis. Direct immunofluorescence, while being the gold standard, is also known to have high false negative rates in many laboratories, as exemplified by the present two cases.1 If a negative result is obtained despite classical clinical findings favoring OCP, repeat immunofluorescent testing, preferably in a different laboratory, is mandatory.
Squamous neoplasia of the conjunctiva is associated with UV radiation, HIV, and HPV infections. DNA damage, mutations in the tumor suppressor gene, and immunosuppression impairing tumor immune surveillance are also thought to lead to SCC.2,3,4 There is one prior report in the literature of conjunctival SCC occurring in the setting of OCP.5 We report two additional cases in which unilateral conjunctival neoplasia occurred in the setting of bilateral OCP. The association between the two conditions may be related to the pathophysiology of oncogenesis via immune dysfunction and chronic inflammation. In Case 2, significant systemic immunosuppression with rituximab could have played a role, and in Case 1, longstanding, untreated OCP-induced inflammation with dysregulation of the local immune microenvironment could have been partially responsible for the same outcome.
OCP is characterized as a type II immune reaction with autoantibodies directed towards basement membrane antigens. This immune reaction leads to activation of the complement cascade leading to intense inflammation.1 Such chronic inflammation with chronic antigenic stimulation is known to play a role in the pathogenesis of a number of malignancies such as gastric and ocular adnexal MALT lymphoma and certain cases of non-Hodgkin B-cell lymphoma.
Long-term systemic immunosuppression has also been shown to be associated with OSSN. “Shields et al. reported 13 patients with conjunctival epithelial neoplasia in the setting of systemic immunosuppression from HIV (n=4), organ transplant (renal (n=4), lung (n=2), liver (n=1), and heart (n=1)), and rheumatologic disease (systemic lupus erythematosus (n=1)).7 These cases showed aggressive, uncontrolled invasive tumor growth (n=3) and one patient died from squamous cell carcinoma with brain invasion. The authors suggested that prompt and long-term topical interferon alpha-2b therapy resulted in the greatest degree of tumor control. Ramasubramanian et al.8 reviewed conjunctival SCC in the setting of corneal transplantation in 4 cases and suggested that the chronic local immunosuppression with topical corticosteroid therapy could have led to the development of the malignancy.”
Conjunctival squamous neoplasia has been previously described in patients with chronic immunosuppression. Shields et al. reported 13 patients with conjunctival epithelial neoplasia in the setting of systemic immunosuppression from HIV (n=4), organ transplantation (renal (n=4), lung (n=2), liver (n=1) and heart (n=1)), and rheumatologic disease (systemic lupus erythematosus (n=1)).7 Several cases showed aggressive, uncontrolled invasive tumor growth and one patient died from squamous cell carcinoma with brain invasion. The authors suggested that prompt and long-term topical interferon alpha-2b therapy resulted in the greatest degree of tumor control. Ramasubramanian et al.8 reviewed conjunctival SCC in the setting of corneal transplantation in 4 cases and proposed that chronic local immunosuppression with topical corticosteroid therapy could have been conducive to the development of the malignancy.
Objective clinical examination and surveillance in the setting of chronically inflamed and fibrosed tissue in OCP can be challenging in some cases. Difficulty is sometimes encountered in reliably differentiating between conjunctival changes secondary to SCC and those arising from OCP. The authors therefore recommend having a low threshold for obtaining a tissue biopsy in any patient with chronic OCP who develops atypical conjunctival changes. It should be understood that repeat biopsies may be necessary for diagnosis, including repeat immunofluorescent studies, which can also be used for monitoring response to therapy.
Acknowledgments
The authors thank Dr. Carol L. Shields for followup clinical information on one of the patients and for her helpful suggestions in the preparation of the manuscript.
Sources of public and private financial support to disclose: None
Footnotes
Disclosure
The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in this article. The authors have no financial disclosures or conflicts of interest to report.
References
- 1.Kirzhner M, Jakobiec FA. Ocular cicatricial pemphigoid: a review of clinical features, immunopathology, differential diagnosis, and current management. Semin Ophthalmol. 2011;26(4–5):270–7. doi: 10.3109/08820538.2011.588660. [DOI] [PubMed] [Google Scholar]
- 2.Gichuhi S, Ohnuma S, Sagoo MS, Burton MJ. Pathophysiology of ocular surface squamous neoplasia. Exp Eye Res. 2014;129:172–82. doi: 10.1016/j.exer.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Afrogheh AH, Jakobiec FA, Hammon R, Grossniklaus HE, Rocco J, Lindeman NI, Sadow PM, Faquin WC. Evaluation for high-risk HPV in squamous cell carcinomas and precursor lesions arising in the conjunctiva and lacrimal sac. Am J Surg Pathol. 2016 Apr;40(4):519–28. doi: 10.1097/PAS.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 4.Kiire CA, Srinivasan S, Karp CL. Ocular surface squamous neoplasia. Int Ophthalmol Clin. 2010 Summer;50(3):35–46. doi: 10.1097/IIO.0b013e3181e246e5. [DOI] [PubMed] [Google Scholar]
- 5.Sivalingam V, Shields CL, Shields JA, Pearah JD. Squamous cell carcinoma of the conjunctiva associated with benign mucous membrane pemphigoid. Ann Ophthalmol. 1990;22(3):106–9. [PubMed] [Google Scholar]
- 6.Shah S, Kaliki S, Kim HJ, Lally SE, Shields JA, Shields CL. Topical interferon alpha 2b for management of ocular surface squamous neoplasia in 23 cases: Outcomes based on American Joint Committee on Cancer (AJCC) classification. Arch Ophthalmol. 2012;130:159–64. doi: 10.1001/archophthalmol.2011.385. [DOI] [PubMed] [Google Scholar]
- 7.Shields CL, Ramasubramanian A, Mellen P, Shields JA. Conjunctival squamous cell carcinoma arising in immunosuppressed patients (organ transplant, human immunodeficiency virus infection) Ophthalmology. 2011;118:2133–7. doi: 10.1016/j.ophtha.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Ramasubramanian A, Shields CL, Sinha N, Shields JA. Ocular surface squamous neoplasia after corneal graft. Am J Ophthalmol. 2010;149:62–5. doi: 10.1016/j.ajo.2009.07.026. [DOI] [PubMed] [Google Scholar]