Abstract
Food addiction is characterized by poorly controlled intake of highly-palatable, calorically-dense, foods. While previous studies indicate that risk factors for food addiction are similar to substance use disorders (SUD), these studies have looked at food addiction and SUD in independent samples, limiting the ability to directly compare food addiction to SUD. The present study was conducted to assess rates of posttraumatic stress disorder (PTSD), depression, childhood and adult trauma exposure, as well as presence and severity of emotion dysregulation, in a sample of women (N=229) who either meet criteria for no addiction, food addiction only or SUD only. The prevalence of food addiction was 18.3% and the prevalence of SUD was 30.6% in this sample. Women with food addiction and women with SUD endorsed more depression and PTSD symptoms when compared with individuals with no addiction. Individuals with food addiction and SUD had higher total emotion dysregulation scores, specifically with difficulties in goal directed behaviors, non-acceptance of emotional responses, impulse control, limited access to emotion regulation strategies, and lack of emotional clarity, when compared to individuals with no addiction (all p’s<0.05). There were no differences in PTSD and depression symptoms and emotion dysregulation scores between food addiction and SUD groups (all p>0.05). However, women with SUD endorsed higher levels of total childhood (p<0.01) and adulthood trauma (p<0.01) as compared with women with no addiction or food addiction. These results suggest that women with food addiction and those with SUD share similar psychological characteristics and risk factors, with the exception of trauma histories. These findings have implications for the detection of risk for and treatment of these disorders.
Keywords: food addiction, emotion regulation, substance use, trauma, women
Introduction
Food addiction is characterized by the poorly-controlled consumption of highly-palatable foods (Gearhardt, Corbin, & Brownell, 2009). Individuals with food addiction exhibit classic symptoms of addiction, such as a preoccupation with obtaining the desired substance, excessive ingestion of the substance and continued, excessive use, despite adverse biological consequences (Gearhardt, et al., 2009). Food addiction can be diagnosed using the Yale Food Addiction Scale (YFAS), which was developed based on the DSM-IV criteria for substance use disorders (SUD) (Gearhardt, et al., 2009). While the criteria for diagnosis are similar between food addiction and SUD, food addiction has only recently become the subject of clinical investigation. As such, the comorbid psychiatric features of food addiction, such as depression and aspects of emotional dysregulation (e.g., poor impulse control), are not well known. Characterization of differences and commonalities in clinical characteristics between food addiction and SUD would aid in the detection of risk for and treatment of food addiction.
To date, studies focusing on food addiction and SUD have described risk factors and consequences associated with these addictions in independent samples, not allowing for comparisons between the two conditions. For example, food addiction and SUD have both been associated with emotional and maladaptive eating (Davis, et al., 2011; Gearhardt, White, Masheb, & Grilo, 2013; Gearhardt, et al., 2012; Gregorowski, Seedat, & Jordaan, 2013; Hodson, Newcomb, Locke, & Goodyear, 2006). Food addiction has been associated with heightened impulsivity, similar to what has been described in individuals with SUD (Pivarunas & Conner, 2015). More recently, food addiction and SUD have both been associated with emotion dysregulation (Gearhardt, et al., 2013; Pivarunas & Conner, 2015). Emotional regulation refers to an individual’s ability to monitor and appropriately respond to emotions (Thompson, 1994; Wilcox, Pommy, & Adinoff, 2016). Individuals with poor emotion regulation abilities often have poorer decision-making, i.e., a reduced ability to limit impulsive behaviors and adaptively handle unpleasant feelings (Murphy, Ewbank, & Calder, 2012; Weiss, Sullivan, & Tull, 2015). Engaging in maladaptive behaviors, such as substance use and overconsumption of food, have both been described as coping mechanisms for dealing with distressing emotions associated with psychopathology, including depression and posttraumatic stress disorder (PTSD) (Berenson, Laz, Pohlmeier, Rahman, & Cunningham, 2015; Gearhardt, et al., 2012; Hirth, Rahman, & Berenson, 2011; Mason, et al., 2014; Mitchell & Wolf, 2016). Indeed, emotion dysregulation is associated with developing an addiction (Griffin, Lowe, Acevedo, & Botvin, 2015; Simons, Dvorak, & Lau-Barraco, 2009; Wong & Rowland, 2013) and greater SUD severity (Weiss, Tull, Anestis, & Gratz, 2013).
Similar to SUD, exposure to childhood trauma and early life stress and adversity has been shown to be associated with maladaptive eating and food addiction (Imperatori, et al., 2016; Mason, et al., 2014; Michopoulos, et al., 2015). Maltreated children develop eating disorders at higher rates than non-maltreated children (Kong & Bernstein, 2009), and are more likely to engage in emotional eating in adulthood (Michopoulos, et al., 2015). Importantly, exposure to childhood trauma is also linked to development of psychopathology, specifically depression and PTSD (Heim & Nemeroff, 2001; Kessler, Davis, & Kendler, 1997), both of which have been described as risk factors for addictive behaviors (Logrip, Zorrilla, & Koob, 2012).
Taken together, previous investigations show clear relationships between food addiction and trauma, emotion dysregulation and psychopathology that parallel those described in SUD. However, these studies have looked at food addiction and SUD in independent samples, limiting the ability to directly compare food addiction to SUD (Ziauddeen, Farooqi, & Fletcher, 2012; Ziauddeen & Fletcher, 2013). Therefore, the current study was designed to examine rates of PTSD, depression, childhood and adult trauma exposure, as well as presence and severity of emotion dysregulation, in a sample of traumatized women with food addiction or SUD. We also included a group of traumatized women with no current addiction for comparison. Based on previous literature, we hypothesized that the food addiction and SUD groups would have similar patterns of emotion dysregulation, psychopathology, and trauma exposure. Specifically, we predicted that more severe emotional dysregulation, depression and PTSD symptoms would be observed in both food addiction and SUD groups when compared to controls. We also hypothesized that food addiction and SUD would be associated with greater rates of trauma exposure.
Methods
Participants
Participants were 229 women drawn from a large study of risk factors for PTSD in a low socioeconomic, urban minority population. Women were recruited from waiting rooms in the diabetic, gynecology, and primary care medical clinics Grady Memorial Hospital, a public hospital in Atlanta, Georgia. Eligible participants were between the ages of 18 and 65, English speaking, and able to give informed consent. Of these 229 participants, 42 women had food addiction but not SUD, 70 women had SUD but no food addiction, and 117 women had neither food addiction nor SUD. Women that had comorbid were not included in the current study as our goal was to compare food addiction to SUD. All study procedures were reviewed and approved by the Emory Institutional Review Board and the Grady Hospital Research Oversight Committee. All participants underwent a structured clinical interview and completed all the measures described below.
Measures
Demographic information was collected with a locally developed Demographics Form that collected information on sex, age, self-identified race, education and income (Gillespie, et al., 2009). Body mass index (BMI; kg/m2) was calculated using self-reported height (m) and weight (kg).
The Yale Food Addiction Scale (YFAS) is a 25-item scale designed to assess food addiction symptoms (Gearhardt, et al., 2009). With this measure, food addiction can be measured as a continuous variable (symptom count) and as a categorical variable (presence of absence of food addiction). The symptom count scoring version provides information on the number of symptoms experienced in the last 12 months. The diagnostic scoring version designates a “diagnosis” of food addiction if an individual reports three or more symptoms in the past 12 months with clinically significant distress or impairment.
The Emotional Eating subscale of the Dutch Eating Behavior Questionnaire (DEBQ) was also administered to assess emotional eating severity (Van Strien, Frijters, Vanstaveren, Defares, & Deurenberg, 1986). The DEBQ Emotional Eating subscale assesses desire to eat under different emotional states (e.g., irritated, depressed, lonely, frightened and disappointed) and is scored on a 5-point Likert scale ranging from 0 (“No desire”) to 4 (“A strong desire”). Total emotional eating severity was calculated by summing responses to individual DEBQ questions as described previously (Cronbach’s α=0.92) (Michopoulos, et al., 2015).
The Traumatic Events Inventory (TEI) was used to assess lifetime trauma exposure (childhood and adulthood). The TEI was administered by trained research interviewers. The TEI was developed and validated in our population (Gillespie, et al., 2009), and assesses experiencing and witnessing traumatic events separately. We used this measure to examine adult trauma exposure, using a sum score that indicates the number of types of traumatic events participants experienced during adulthood (Gillespie, et al., 2009).
The short form of the Childhood Trauma Questionnaire (CTQ) validated previously in both general and clinical populations (Forde, Baron, Scher, & Stein, 2012; Paivio & Cramer, 2004) was used to assess childhood exposure to physical, sexual and emotional abuse, as well as physical and emotional neglect (Bernstein, et al., 2003). Higher scores on the measure are indicative of higher reported levels of childhood trauma.
The Beck Depression Inventory II, a 21-item measure of depressive symptoms in the past two weeks, was used to assess current depression symptom severity. This measure provides scores that indicate depressive severity (total score) and a likely diagnosis of depression (score >18) (Beck, Steer, Ball, & Ranieri, 1996). In the current study, the severity items (Likert Scale ranging from 0 to 3) were summed to calculate current depression symptom severity (Cronbach’s α=0.91).
Current PTSD symptoms (in the last two weeks) were assessed via the 17-item self-report, psychometrically valid, modified PTSD Symptom Scale (PSS) for DSM-IV (Falsetti, Resnick, Resick, & Kilpatrick, 1993). We assessed re-experiencing, avoidance and numbing, and hyperarousal symptom severity, as well as overall symptom severity (PSS total score). The PSS is a widely used and psychometrically sound measure; Cronbach’s α=0.90 for the present study.
The Difficulties in Emotion Regulation Scale (DERS) is a 36-item questionnaire that assesses various aspects of emotional dysregulation. This measure has excellent psychometric properties (Gratz & Roemer, 2008); Cronbach’s α=0.81 for the current study. We used the DERS total and subscale scores for this study; subscales assess: non-acceptance of emotional responses (non-acceptance subscale); difficulties engaging in goal oriented behavior (goals subscale); impulse control (impulse subscale); lack of emotional awareness (awareness subscale); limited access to emotion regulation strategies (strategies subscale); and lack of emotional clarity (clarity subscale) (Neumann, van Lier, Gratz, & Koot, 2010; Ruscitti, Rufino, Goodwin, & Wagner, 2016; Wolz, et al., 2015). Higher scores indicate higher levels of emotion dysregulation.
The Mini International Neuropsychiatric Interview (M.I.N.I. 6.0) is a brief, semi-structured clinician-administered interview that was utilized to categorically diagnose the presence of current (in the last 12 months) or past substance abuse or dependence (SUD) based on DSM-IV criteria. For the purposes of this study, we defined the SUD group as those who met criteria for current or lifetime SUD (Sheehan, et al., 1998).
Statistical Analyses
Chi square analysis was used to assess group differences (food addiction only vs. SUD vs. control) on employment, education and income categorical variables. Separate ANOVAs were used to compare the effects of group (food addiction only vs. SUD vs. control) on sociodemographic continuous variables (i.e. age, BMI) as well as emotion regulation scores, depression and PTSD symptom severity, and trauma exposure. Tukey’s post-hoc testing was used to assess between group differences. All the data analyses were conducted using SPSS (v.21). An alpha level of p ≤ 0.05 was considered statistically significant.
Results
Demographics and psychopathology
In this sample, the prevalence of SUD was 30.6%, food addiction was 18% and obesity was 62%. There were no between-group differences in BMI, race, income and highest level of education completed (Table 1). However, SUD and food addiction were associated with greater rates of unemployment compared to controls (p<0.001; Table 1). Women with SUD (p=0.03), but not food addiction (p=0.11), were significantly older than controls.
Table 1.
No differences in BMI, income, and education were observed between controls, food addiction and substance use disorder groups.
| Demographics | N=229 | |||||
|---|---|---|---|---|---|---|
| Controls n=117 (37.5%) |
Food Addiction Only n=42 (18.3%) |
SUD Only n=70 (22.4%) |
||||
| %(n) | χ2 | P- value | ||||
| Employment | 15.49 | <0.001* | ||||
| Employed | 48.7 (57) | 28.6 (12) | 21.4 (15) | |||
| Education | 11.25 | 0.50 | ||||
| < 12th | 15.4 (18) | 23.8 (9) | 28.6 (15) | |||
| 12th or High School Grad; GED | 40.1 (47) | 28.5 (12) | 25.7 (18) | |||
| Some College/Tech School | 22.2 (26) | 28.6 (12) | 27.1 (19) | |||
| College/ Tech School Grad | 18.8 (22) | 14.3 (6) | 17.1 (12) | |||
| Grad School | 3.4 (4) | 4.8 (2) | 1.4 (1) | |||
| Income | 6.80 | 0.55 | ||||
| <$500 | 14.9 (17) | 22.0 (9) | 20 (14) | |||
| $500 – $999 | 31.6 (36) | 24.4 (10) | 30.0 (21) | |||
| $1000–$1999 | 29.8 (34) | 31.7 (13) | 32.9 (23) | |||
| >$2000 | 23.7 (27) | 22.0 (9) | 17.1 (12) | |||
| Mean ± SEM | F-value | p-value | ||||
| Age | 37.9 (1.09) | 42.1 (1.87) | 42.5 (1.41) | 4.05 | 0.01# | |
| BMI | 34.9 (0.75) | 35.7 (1.26) | 33.6 (0.98) | 0.90 | 0.40 | |
Food addiction and SUD are both associated with more unemployment than controls (denoted by *).
SUD is associated with greater age compared to controls (denoted by #).
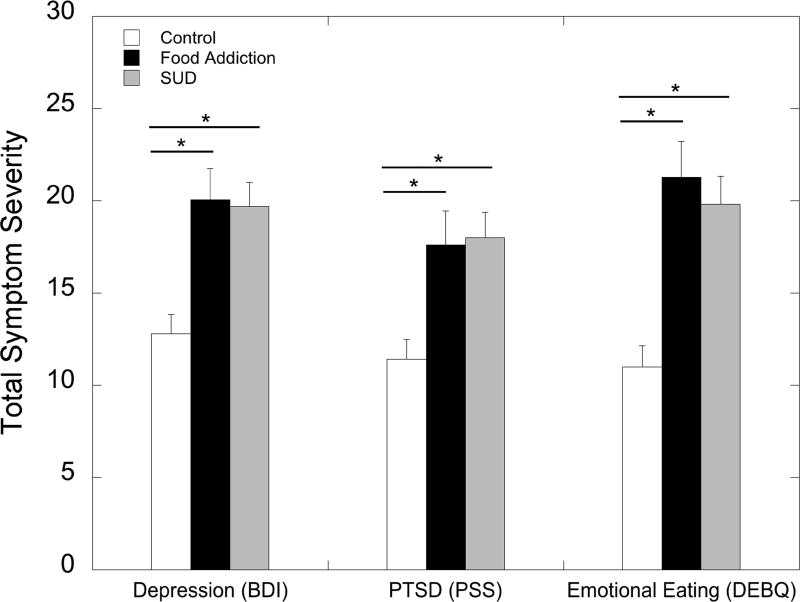
Food addiction and SUD groups were both associated with greater emotional eating severity (DEBQ Emotional Eating subscale score) compared to controls (F2,220= 16.50; p≤0.001; η2=0.13). Food addiction and SUD were both associated with significantly greater depression (F2,224= 12.9; p≤0.001; η2=0.10) and PTSD symptom severity (F2.225= 8.51; p≤0.001; η2= 0.070) as compared to controls (Figure 1). Women with SUD and those with food addiction endorsed higher PTSD re-experiencing (F2,225= 5.14; p≤0.01; η2= 0.044) and avoidance and numbing symptoms (F2,225= 8.30; p≤0.001; η2= 0.069) when compared to controls. SUD, but not food addiction, was associated with somewhat higher PTSD hyperarousal subscale scores as compared to controls (F2,225= 6.65; p≤0.01; η2= 0.056). Emotional eating severity, and depression and PTSD symptom severity were not different between food addiction and SUD groups (all p’s > 0.05; Figure 1).
Figure 1.
Food addiction and SUD groups show greater PTSD (PTSD Symptom Scale; PSS), depression symptoms (Beck Depression Inventory II; BDI), and greater emotional eating severity (Dutch Eating Behaviors Questionnaire; DEBQ; denoted by *) compared to the non-addicted, control group. There are no differences between food addiction and SUD on these measures.
Emotion Dysregulation
Significant between-group differences were observed in emotional dysregulation (DERS) total and subscale scores (Figure 2). A significant main effect of group was observed; both the SUD group (p=0.004) and the food addiction group (p≤0.001) had higher total emotion dysregulation scores (DERS total) compared to controls (F2.226= 13.67; p≤0.001; η2= 0.11). There were also significant group effects for five of the six DERS subscales; individuals with either food addiction or SUD endorsed higher scores than controls (all post-hoc test p’s<0.05), on the following DERS subscales: difficulties engaging in goal directed behaviors (F2,226=11.26; p≤0.001; η2= 0.091); non-acceptance of emotional responses (F2,226=2.93; p≤0.05; η2= 0.025); impulse control (F2,226=9.16; p≤0.001; η2= 0.075); limited access to emotion regulation strategies (F2,226=7.87; p≤0.001; η2= 0.065); and lack of emotional clarity (F2,226=15.89; p≤0.001; η2= 0.12). There was no significant between-group difference for lack of emotional awareness (p>0.05). There were also no significant differences between SUD and food addiction groups for any DERS scores (all p’s>0.05).
Figure 2.
Food addiction and SUD are associated with greater (A) overall emotion dysregulation and (B) subscales of DERS scores compared to the non-addicted, control group (denoted by *). There are no differences between food addiction and SUD on DERS total and subscale scores.
Trauma exposure
There was a significant main effect of group on childhood trauma exposure (F2.226= 6.08; p≤0.01; η2= 0.051); individuals with SUD endorsed higher levels of childhood maltreatment (CTQ total score) as compared to controls or individuals with food addiction (p<0.05; Table 2). There were also main effects of group for specific types of childhood maltreatment, including childhood sexual abuse (F2.226= 7.90; p ≤0.001; η2= 0.065), childhood emotional neglect (F2.226= 3.57; p≤0.05; η2= 0.031), and childhood emotional abuse (F2.226= 3.90; p≤0.05; η2= 0.033). More specifically, women with SUD endorsed higher amounts of childhood sexual abuse (p<0.001), childhood emotional neglect (p=0.03), and childhood emotional abuse (p=0.02) when compared women with food addiction (Table 2). Lastly, there was a main effect of group on trauma exposure in adulthood (F2.226= 4.85; p≤0.01; η2= 0.041), such that women with SUD reported greater adulthood trauma exposure compared to women with food addiction (p=0.009; Table 2).
Table 2.
| Demographics | Overall N=229 | |||||
|---|---|---|---|---|---|---|
| Mean ± SEM | ||||||
| Controls n=117 (37.5%) |
Food Addiction Only n=42 (18.3%) |
SUD Only (HX) n=70 (22.4%) |
||||
| F | P- value | |||||
| Childhood Maltreatment Total (CTQ total score) | 40.75 (1.77) | 37.64 (2.96) | 49.23 (2.29) | 6.08 | .003 * # | |
| Emotional Neglect | 9.31 (0.46) | 8.88 (0.77) | 11.10 (0.60) | 3.57 | .03 * | |
| Sexual Abuse | 8.12 (0.50) | 6.76 (0.84) | 10.68 (0.65) | 7.90 | <.001 * # | |
| Physical Abuse | 7.94 (0.43) | 7.33 (0.72) | 9.33 (0.56) | 2.99 | .056 | |
| Emotional Abuse | 8.85 (0.46) | 8.59 (0.77) | 10.78 (0.60) | 3.90 | .02 * | |
| Physical Neglect | 6.53 (0.27) | 6.07 (0.45) | 7.37 (0.35) | 2.95 | .054 | |
| Adult Only Total Experienced (No Child – TEI) | 2.33 (0.16) | 2.66 (0.27) | 3.16 (0.21) | 4.85 | .009 * | |
History of trauma exposure is greater in people with SUD compared to those with food addiction (denoted by *) and non-addicted controls (denoted by #; p≤0.05).
Discussion
The results of our study show that women with SUD or food addiction have similar PTSD and depression symptom profiles, and exhibited more problems with emotional dysregulation as compared to women with no addictions. These findings, generated from a direct comparison between food addiction and SUD, provide critical evidence that these addictions share many clinical characteristics, particularly emotion dysregulation profiles. To our knowledge, only one study has directly compared food addiction to another addiction (alcohol); this study found similar patterns of neural activity (measured via electroencephalography) between the two groups (De Ridder, et al., 2016). Our findings support and extend this research, indicating that these different types of addictions share some common clinical characteristics.
We observed that women with food addiction endorsed similar problems with emotion dysregulation as compared to those with SUDs, including features such as poor impulse control and emotion interfering with goal-directed behavior, which corroborates and extends previous findings linking emotion dysregulation to food addiction (Gearhardt, et al., 2013; Pivarunas & Conner, 2015). In particular, we found a strong relationship between impulsivity and food addiction, which has been previously suggested to contribute to the development of increased BMI (Raymond & Lovell, 2015). The similar patterns of emotion dysregulation between food addiction and SUD groups may also explain the similarity in emotional eating severity reported by the two groups of women. Our finding that food addiction and SUD were both associated with greater depression and PTSD symptom severity as compared to controls is consistent with previous studies describing associations between depression and PTSD, and food addiction (Berenson, et al., 2015; Gearhardt, et al., 2012; Mitchell & Wolf, 2016) and SUD (Barrett, Teesson, & Mills, 2014; Khoury, Tang, Bradley, Cubells, & Ressler, 2010; McGovern, et al., 2015). Taken together, our data indicate that women with food addiction and SUD do not differ based on their emotion regulation and depression and PTSD symptom profiles. It seems likely that emotion dysregulation plays in the development of both food addiction and SUD; these addictions may serve as maladaptive coping mechanisms in the face of emotional distress. Support for this claim comes from data indicating that maladaptive eating behaviors serve as a form of escape from negative emotions (Brechan & Kvalem, 2015) and that attention bias towards food images increases in the presence of emotionally arousing stimuli (Frayn, Sears, & von Ranson, 2016).
Although emotion dysregulation, and depression and PTSD symptoms were similarly associated with food addiction and SUD in the current study, trauma histories were different between the two groups. Contrary to previous studies that showed an association between food addiction and childhood trauma (Imperatori, et al., 2016), our data indicates that childhood trauma histories were relatively similar for food addicted and non-addicted groups in this highly traumatized sample of women. However, SUD was associated with higher levels of childhood and adulthood trauma as compared to the other two groups. It is possible that higher levels of lifetime psychological stress (including childhood trauma exposure) may lead to greater adaptations in reward circuitry, and thus, a more potent reward stimulus than food (i.e., drugs) may be sought out to experience pleasure or to mute dysregulated affect (Volkow, Wang, Fowler, Tomasi, & Baler, 2012). While longitudinal studies are necessary to characterize the differential impact of childhood and adulthood trauma exposure on reward circuitry and addiction risk (Volkow, et al., 2012), the current data suggest that the timing of trauma exposure may be critical not only for the emergence of specific addictions, but also for the timing of intervention.
The current study sample comprised of economically-underprivileged, African American women presenting for care at an inner-city hospital; this population has historically demonstrated high rates of trauma exposure (Gillespie, et al., 2009; Schwartz, Bradley, Sexton, Sherry, & Ressler, 2005) that have been linked to high rates of SUD and obesity (Gunstad, et al., 2006; Mutlu, Bilgic, Erten, Aras, & Tayfur, 2016; Tucci, Kerr-Correa, & Souza-Formigoni, 2010). In order to identify clinical and demographic characteristics uniquely associated with food addiction, we included women with SUD but no food addiction, women with food addiction and non-addicted controls. Although we found lower prevalence rates of food addiction (~18%) compared to SUD in the current study, the prevalence of either condition within this sample was higher than what was reported in earlier studies (<12%) (Berenson, et al., 2015; Gearhardt, et al., 2009; Gearhardt, et al., 2011), indicating that this sample of women may be at increased risk for addictive disorders (Cross, Crow, Powers, & Bradley, 2015; Gilbert, El-Bassel, Chang, Wu, & Roy, 2012; Patrick, Wightman, Schoeni, & Schulenberg, 2012).
Contrary to other studies that have shown a positive association between food addiction and increased BMI (Flint, et al., 2014; Gearhardt, Boswell, & White, 2014; Pedram, et al., 2013), food addiction was not associated with greater BMI in the current study. However, another study in a similar sample of low SES, reproductive-age women also found no association between BMI and food addiction symptoms (Berenson, et al., 2015); in this study, African American women reported more food addiction symptoms than Hispanic women. This may suggest that sociodemographic factors (i.e. race) may account for the lack of a relationship between food addiction and BMI found here. Additionally, the three groups of women compared in the current study had an average BMI of greater than 33, corroborating previous reports linking low SES to increased rates of obesity, especially in African American women (Harrell & Gore, 1998). Furthermore, low SES has been linked to higher prevalence of SUD (Cross, et al., 2015; Patrick, et al., 2012), which is inversely related to obesity in these low SES populations (Blüml, et al., 2012; Desai, Manley, Desai, & Potenza, 2009; Simon, et al., 2006). However, in the current study we found that there was no association between BMI and SUD. Extant research on other addictions, such as cigarette abuse, also shows equivocal associations with BMI that may be influenced by factors such as age and sex (Barry & Petry, 2009; N'Goran, et al., 2016; Pasch, Velazquez, Cance, Moe, & Lytle, 2012). The lack of an association between food addiction and BMI in the current study underscores the notion that obesity may not be a valid surrogate marker of food addiction as previously described (Ziauddeen, et al., 2012; Ziauddeen & Fletcher, 2013). This notion is also underscored by the current finding that emotional eating severity was similar between food addiction and SUD groups.
Regarding study limitations, we did not assess responses to behavioral measures that incorporated emotional stimuli; thus, we were unable to examine potentially more subtle differences in emotion processing between FA and SUD groups. The cross-sectional nature of our study poses another limitation in terms of understanding how emotion dysregulation patterns influence addiction development. Prospective studies are necessary to understand how trauma exposure and emotion processing patterns increase risk for the development of these addictions. While the exclusion of a comorbid SUD and food addiction group in our sample could also be considered a limitation, we chose to include food addiction only and SUD only groups to examine their unique features. Further, our study did not specifically examine manifestations of eating disorders, such as binge eating, which warrants investigation in future research. The homogeneity of our study sample could also be seen as a limitation, as the results may be less generalizable to other populations. However, we consider this sample homogeneity to be a strength due to the fact that trauma exposure and psychopathology (Gillespie, et al., 2009), as well as food addiction, is highly prevalent in this population.
In conclusion, the findings of the present study outline common features of food addiction and SUD, particularly, of PTSD, depression, and patterns of emotion dysregulation. It is possible that food addiction and SUD have similar neurobiological signatures, including abnormalities in reward pathways, and may respond to similar types of treatment; this is worthy of future investigation as most neuroimaging studies have focused on obesity as their outcome phenotype of interest (Volkow, et al., 2012). Our study highlights the need for further research on food addiction, particularly research that uses a multi-method approach to elucidate the various psychological, behavioral and neurobiological characteristics that are unique to food addiction.
Acknowledgments
The current study was supported by MH096764, MH071537, MH070129, MH101380, HD085850, the Emory Medical Care Foundation, the Emory and Grady Memorial Hospital General Clinical Research Center, NIH National Centers for Research Resources (M01RR00039), the Research and Woodruff Health Sciences IT Division (UL1 TR000424), the Atlanta Clinical Translational Science Institute, the NIH National Centers for Research Resources (M01 RR00039), and the Emory University General Clinical Research Center at Grady Hospital. Support for this publication was provided by a grant from the Robert Wood Johnson Foundation Health Policy Research Scholars program (RH, NF). This study would not have been possible without the research expertise and technical assistance of Angelo Brown, Alex Rothbaum, Abigail Powers, Cherita Clendinen, Dorthie Mokdad, Becky Roffman, Allen Graham, and all the staff, volunteers, and participants of the Grady Trauma Project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barrett EL, Teesson M, Mills KL. Associations between substance use, post-traumatic stress disorder and the perpetration of violence: A longitudinal investigation. Addict Behav. 2014;39:1075–1080. doi: 10.1016/j.addbeh.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Barry D, Petry NM. Associations between body mass index and substance use disorders differ by gender: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addict Behav. 2009;34:51–60. doi: 10.1016/j.addbeh.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Berenson AB, Laz TH, Pohlmeier AM, Rahman M, Cunningham KA. Prevalence of Food Addiction Among Low-Income Reproductive-Aged Women. J Womens Health (Larchmt) 2015;24:740–744. doi: 10.1089/jwh.2014.5182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Blüml V, Kapusta N, Vyssoki B, Kogoj D, Walter H, Lesch OM. Relationship between substance use and body mass index in young males. The American Journal on Addictions. 2012;21:72–77. doi: 10.1111/j.1521-0391.2011.00192.x. [DOI] [PubMed] [Google Scholar]
- Brechan I, Kvalem IL. Relationship between body dissatisfaction and disordered eating: mediating role of self-esteem and depression. Eat Behav. 2015;17:49–58. doi: 10.1016/j.eatbeh.2014.12.008. [DOI] [PubMed] [Google Scholar]
- Cross D, Crow T, Powers A, Bradley B. Childhood trauma, PTSD, and problematic alcohol and substance use in low-income, African-American men and women. Child Abuse Negl. 2015;44:26–35. doi: 10.1016/j.chiabu.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C, Curtis C, Levitan RD, Carter JC, Kaplan AS, Kennedy JL. Evidence that 'food addiction' is a valid phenotype of obesity. Appetite. 2011;57:711–717. doi: 10.1016/j.appet.2011.08.017. [DOI] [PubMed] [Google Scholar]
- De Ridder D, Manning P, Leong SL, Ross S, Sutherland W, Horwath C, Vanneste S. The brain, obesity and addiction: an EEG neuroimaging study. Sci Rep. 2016;6:34122. doi: 10.1038/srep34122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai RA, Manley M, Desai MM, Potenza MN. Gender differences in the association between body mass index and psychopathology. CNS Spectr. 2009;14:372–383. doi: 10.1017/s1092852900023026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falsetti SA, Resnick HS, Resick PA, Kilpatrick DG. The Modified PTSD Symptom Scale: A brief self-report measure of posttraumatic stress disorder. Behaviour Therapist. 1993:161–161. [Google Scholar]
- Flint AJ, Gearhardt AN, Corbin WR, Brownell KD, Field AE, Rimm EB. Food-addiction scale measurement in 2 cohorts of middle-aged and older women. Am J Clin Nutr. 2014;99:578–586. doi: 10.3945/ajcn.113.068965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forde DR, Baron SW, Scher CD, Stein MB. Factor structure and reliability of the childhood trauma questionnaire and prevalence estimates of trauma for male and female street youth. J Interpers Violence. 2012;27:364–379. doi: 10.1177/0886260511416461. [DOI] [PubMed] [Google Scholar]
- Frayn M, Sears CR, von Ranson KM. A sad mood increases attention to unhealthy food images in women with food addiction. Appetite. 2016;100:55–63. doi: 10.1016/j.appet.2016.02.008. [DOI] [PubMed] [Google Scholar]
- Gearhardt AN, Boswell RG, White MA. The association of "food addiction" with disordered eating and body mass index. Eat Behav. 2014;15:427–433. doi: 10.1016/j.eatbeh.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009;52:430–436. doi: 10.1016/j.appet.2008.12.003. [DOI] [PubMed] [Google Scholar]
- Gearhardt AN, White MA, Masheb RM, Grilo CM. An examination of food addiction in a racially diverse sample of obese patients with binge eating disorder in primary care settings. Compr Psychiatry. 2013;54:500–505. doi: 10.1016/j.comppsych.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearhardt AN, White MA, Masheb RM, Morgan PT, Crosby RD, Grilo CM. An examination of the food addiction construct in obese patients with binge eating disorder. Int J Eat Disord. 2012;45:657–663. doi: 10.1002/eat.20957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68:808–816. doi: 10.1001/archgenpsychiatry.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert L, El-Bassel N, Chang M, Wu E, Roy L. Substance use and partner violence among urban women seeking emergency care. Psychol Addict Behav. 2012;26:226–235. doi: 10.1037/a0025869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, Weiss T, Schwartz AC, Cubells JF, Ressler KJ. Trauma exposure and stress-related disorders in inner city primary care patients. Gen Hosp Psychiatry. 2009;31:505–514. doi: 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2008;30:315–315. [Google Scholar]
- Gregorowski C, Seedat S, Jordaan GP. A clinical approach to the assessment and management of co-morbid eating disorders and substance use disorders. BMC Psychiatry. 2013;13:289. doi: 10.1186/1471-244X-13-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin KW, Lowe SR, Acevedo BP, Botvin GJ. Affective Self-Regulation Trajectories During Secondary School Predict Substance Use Among Urban Minority Young Adults. J Child Adolesc Subst Abuse. 2015;24:228–234. doi: 10.1080/1067828X.2013.812530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunstad J, Paul RH, Spitznagel MB, Cohen RA, Williams LM, Kohn M, Gordon E. Exposure to early life trauma is associated with adult obesity. Psychiatry Res. 2006;142:31–37. doi: 10.1016/j.psychres.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Harrell JS, Gore SV. Cardiovascular risk factors and socioeconomic status in African American and Caucasian women. Res Nurs Health. 1998;21:285–295. doi: 10.1002/(sici)1098-240x(199808)21:4<285::aid-nur2>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- Hirth JM, Rahman M, Berenson AB. The association of posttraumatic stress disorder with fast food and soda consumption and unhealthy weight loss behaviors among young women. J Womens Health (Larchmt) 2011;20:1141–1149. doi: 10.1089/jwh.2010.2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodson C, Newcomb MD, Locke TF, Goodyear RK. Childhood adversity, poly-substance use, and disordered eating in adolescent Latinas: mediated and indirect paths in a community sample. Child Abuse Negl. 2006;30:1017–1036. doi: 10.1016/j.chiabu.2005.10.017. [DOI] [PubMed] [Google Scholar]
- Imperatori C, Innamorati M, Lamis DA, Farina B, Pompili M, Contardi A, Fabbricatore M. Childhood trauma in obese and overweight women with food addiction and clinical-level of binge eating. Child Abuse Negl. 2016;58:180–190. doi: 10.1016/j.chiabu.2016.06.023. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Khoury L, Tang YL, Bradley B, Cubells JF, Ressler KJ. Substance use, childhood traumatic experience, and Posttraumatic Stress Disorder in an urban civilian population. Depress Anxiety. 2010;27:1077–1086. doi: 10.1002/da.20751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong S, Bernstein K. Childhood trauma as a predictor of eating psychopathology and its mediating variables in patients with eating disorders. J Clin Nurs. 2009;18:1897–1907. doi: 10.1111/j.1365-2702.2008.02740.x. [DOI] [PubMed] [Google Scholar]
- Logrip ML, Zorrilla EP, Koob GF. Stress modulation of drug self-administration: implications for addiction comorbidity with post-traumatic stress disorder. Neuropharmacology. 2012;62:552–564. doi: 10.1016/j.neuropharm.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason SM, Flint AJ, Roberts AL, Agnew-Blais J, Koenen KC, Rich-Edwards JW. Posttraumatic stress disorder symptoms and food addiction in women by timing and type of trauma exposure. JAMA Psychiatry. 2014;71:1271–1278. doi: 10.1001/jamapsychiatry.2014.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern MP, Lambert-Harris C, Xie H, Meier A, McLeman B, Saunders E. A randomized controlled trial of treatments for co-occurring substance use disorders and posttraumatic stress disorder. Addiction. 2015;110:1194–1204. doi: 10.1111/add.12943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michopoulos V, Powers A, Moore C, Villarreal S, Ressler KJ, Bradley B. The mediating role of emotion dysregulation and depression on the relationship between childhood trauma exposure and emotional eating. Appetite. 2015;91:129–136. doi: 10.1016/j.appet.2015.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell KS, Wolf EJ. PTSD, food addiction, and disordered eating in a sample of primarily older veterans: The mediating role of emotion regulation. Psychiatry Res. 2016;243:23–29. doi: 10.1016/j.psychres.2016.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy FC, Ewbank MP, Calder AJ. Emotion and personality factors influence the neural response to emotional stimuli. Behavioral and Brain Sciences. 2012;35:156–157. doi: 10.1017/S0140525X11001725. [DOI] [PubMed] [Google Scholar]
- Mutlu H, Bilgic V, Erten S, Aras S, Tayfur M. Evaluation of the Relationship between Childhood Traumas and Adulthood Obesity Development. Ecol Food Nutr. 2016;55:390–401. doi: 10.1080/03670244.2016.1198791. [DOI] [PubMed] [Google Scholar]
- N'Goran AA, Studer J, Deline S, Henchoz Y, Baggio S, Mohler-Kuo M, Daeppen JB, Gmel G. Bidirectional relationship between the body mass index and substance use in young men. Subst Abus. 2016;37:190–196. doi: 10.1080/08897077.2015.1013204. [DOI] [PubMed] [Google Scholar]
- Neumann A, van Lier PA, Gratz KL, Koot HM. Multidimensional assessment of emotion regulation difficulties in adolescents using the Difficulties in Emotion Regulation Scale. Assessment. 2010;17:138–149. doi: 10.1177/1073191109349579. [DOI] [PubMed] [Google Scholar]
- Paivio SC, Cramer KM. Factor structure and reliability of the Childhood Trauma Questionnaire in a Canadian undergraduate student sample. Child Abuse Negl. 2004;28:889–904. doi: 10.1016/j.chiabu.2004.01.011. [DOI] [PubMed] [Google Scholar]
- Pasch KE, Velazquez CE, Cance JD, Moe SG, Lytle LA. Youth substance use and body composition: does risk in one area predict risk in the other? J Youth Adolesc. 2012;41:14–26. doi: 10.1007/s10964-011-9706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Wightman P, Schoeni RF, Schulenberg JE. Socioeconomic status and substance use among young adults: a comparison across constructs and drugs. J Stud Alcohol Drugs. 2012;73:772–782. doi: 10.15288/jsad.2012.73.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedram P, Wadden D, Amini P, Gulliver W, Randell E, Cahill F, Vasdev S, Goodridge A, Carter JC, Zhai G, Ji Y, Sun G. Food addiction: its prevalence and significant association with obesity in the general population. PLoS One. 2013;8:e74832. doi: 10.1371/journal.pone.0074832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pivarunas B, Conner BT. Impulsivity and emotion dysregulation as predictors of food addiction. Eat Behav. 2015;19:9–14. doi: 10.1016/j.eatbeh.2015.06.007. [DOI] [PubMed] [Google Scholar]
- Raymond KL, Lovell GP. Food addiction symptomology, impulsivity, mood, and body mass index in people with type two diabetes. Appetite. 2015;95:383–389. doi: 10.1016/j.appet.2015.07.030. [DOI] [PubMed] [Google Scholar]
- Ruscitti C, Rufino K, Goodwin N, Wagner R. Difficulties in emotion regulation in patients with eating disorders. Borderline Personal Disord Emot Dysregul. 2016;3:3. doi: 10.1186/s40479-016-0037-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz AC, Bradley RL, Sexton M, Sherry A, Ressler KJ. Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatr Serv. 2005;56:212–215. doi: 10.1176/appi.ps.56.2.212. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63:824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Lau-Barraco C. Behavioral inhibition and activation systems: differences in substance use expectancy organization and activation in memory. Psychol Addict Behav. 2009;23:315–328. doi: 10.1037/a0015834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RA. Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev. 1994;59:25–52. [PubMed] [Google Scholar]
- Tucci AM, Kerr-Correa F, Souza-Formigoni ML. Childhood trauma in substance use disorder and depression: an analysis by gender among a Brazilian clinical sample. Child Abuse Negl. 2010;34:95–104. doi: 10.1016/j.chiabu.2009.07.001. [DOI] [PubMed] [Google Scholar]
- Van Strien T, Frijters JER, Vanstaveren WA, Defares PB, Deurenberg P. The Predictive-Validity of the Dutch Restrained Eating Scale. International Journal of Eating Disorders. 1986;5:747–755. [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, Tomasi D, Baler R. Food and drug reward: overlapping circuits in human obesity and addiction. Curr Top Behav Neurosci. 2012;11:1–24. doi: 10.1007/7854_2011_169. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Sullivan TP, Tull MT. Explicating the role of emotion dysregulation in risky behaviors: A review and synthesis of the literature with directions for future research and clinical practice. Curr Opin Psychol. 2015;3:22–29. doi: 10.1016/j.copsyc.2015.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Anestis MD, Gratz KL. The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug Alcohol Depend. 2013;128:45–51. doi: 10.1016/j.drugalcdep.2012.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox CE, Pommy JM, Adinoff B. Neural Circuitry of Impaired Emotion Regulation in Substance Use Disorders. Am J Psychiatry. 2016;173:344–361. doi: 10.1176/appi.ajp.2015.15060710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolz I, Aguera Z, Granero R, Jimenez-Murcia S, Gratz KL, Menchon JM, Fernandez-Aranda F. Emotion regulation in disordered eating: Psychometric properties of the Difficulties in Emotion Regulation Scale among Spanish adults and its interrelations with personality and clinical severity. Front Psychol. 2015;6:907. doi: 10.3389/fpsyg.2015.00907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Rowland SE. Self-determination and substance use: is effortful control a mediator? Alcohol Clin Exp Res. 2013;37:1040–1047. doi: 10.1111/acer.12062. [DOI] [PubMed] [Google Scholar]
- Ziauddeen H, Farooqi IS, Fletcher PC. Obesity and the brain: how convincing is the addiction model? Nat Rev Neurosci. 2012;13:279–286. doi: 10.1038/nrn3212. [DOI] [PubMed] [Google Scholar]
- Ziauddeen H, Fletcher PC. Is food addiction a valid and useful concept? Obes Rev. 2013;14:19–28. doi: 10.1111/j.1467-789X.2012.01046.x. [DOI] [PMC free article] [PubMed] [Google Scholar]