Abstract
Objective
Associations between low socioeconomic status (SES) and poor health outcomes have been demonstrated in a variety of conditions. However, the relationship in patients with sepsis is not well described. We investigated the association of lower household income with in-hospital mortality in patients with sepsis across the United States.
Methods
Retrospective nationwide cohort analysis utilizing the Nationwide Inpatient Sample (NIS) from 2011. Patients aged 18 years or older with sepsis were included. Socioeconomic status was approximated by the median household income of the zip code in which the patient resided. Multivariate logistic modeling incorporating a validated illness severity score for sepsis in administrative data was performed.
Results
A total of 8 023 590 admissions from the 2011 NIS were examined. A total of 671 858 patients with sepsis were included in the analysis. The lowest income residents compared to the highest were younger (66.9 years, standard deviation [SD] = 16.5 vs 71.4 years, SD = 16.1, P < .01), more likely to be female (53.5% vs 51.9%, P < .01), less likely to be white (54.6% vs 76.6%, P < .01), as well as less likely to have health insurance coverage (92.8% vs 95.9%, P < .01). After controlling for severity of sepsis, residing in the lowest income quartile compared to the highest quartile was associated with a higher risk of mortality (odds ratio [OR]: 1.06, 95% confidence interval [CI]: 1.03–1.08, P < .01). There was no association seen between the second (OR: 1.02, 95% CI: 0.99–1.05, P = .14) and third (OR: 0.99, 95% CI: 0.97–1.01, P = .40) quartiles compared to the highest.
Conclusion
After adjustment for severity of illness, patients with sepsis who live in the lowest median income quartile had a higher risk of mortality compared to residents of the highest income quartile. The association between SES and mortality in sepsis warrants further investigation with more comprehensive measures of SES.
Keywords: sepsis, hospital mortality, outcomes, epidemiology
Introduction
The relationship between socioeconomic status (SES) and health outcomes has been widely studied for a variety of health conditions. Robust associations between lower SES and worse outcomes have been demonstrated in heart disease, cancer, stroke, palliative care, access to procedural interventions, and overall mortality.1–7 In critical care, an association between low SES and higher mortality in patients admitted to intensive care units (ICUs) has also been suggested.8,9
Sepsis is the sixth most common reason for hospital admission in the United States, and in critically ill patients, severe sepsis and septic shock remain the leading causes of mortality.10–12 To date, the relationship between SES and sepsis has not been well characterized. Existing studies have been limited by small sample size or lack of an appropriate control for disease severity.13,14 Recently, Goodwin et al demonstrated that living in medically underserved areas (MUAs) in South Carolina was associated with worse outcomes in patients with sepsis.15 However, it has yet to be shown whether this relationship is more broadly generalizable to other areas.
The objective of our study was to examine the relationship between SES, using the surrogate of median household income, and mortality in patients with sepsis across the United States. On the basis of prior research, we hypothesized that lower household income would be associated with higher mortality.
Methods
We report our study in accordance with the STrengthening the Reporting of OBservational studies in Epidemiology statement.16 A waiver of consent was granted from the institutional review board of University of British Columbia (H16-01635). The outcome for this analysis was in-hospital mortality.
Cohort Selection
For this retrospective cohort analysis, the setting was the 2011 Nationwide Inpatient Sample (NIS). The NIS is a national database capturing 20% of all US hospital admissions produced by the Agency for Health Care Quality (AHRQ).17 Using a complex survey design, the NIS allows for estimation of 95% of inpatient care delivered across the United States. The NIS represents data from the entire year 2011 from over 4000 hospitals in 47 states.
The participants of this study were patients aged 18 years or older who met the Angus definition of sepsis from the 2011 NIS sample.18 The Angus definition has been validated to have a sensitivity of 50.4% and a specificity of 96.3% in identifying patients with sepsis.19 The Angus definition was created by Dr Derek Angus for the use of administrative data in the study of sepsis and has been utilized extensively.18,20,21 In order to be “Angus Positive,” a patient must have the International Classification of Diseases, Ninth Revision (ICD-9) code for severe sepsis (995.92) or septic shock (785.52). A patient can also be Angus Positive if they have an ICD-9 code for infection with an additional code for organ dysfuncton.19 The variables obtained from the data set and used in this analysis were age, gender, race (white, black, Hispanic, and other), length of stay, hospital mortality, insurance status, zip code income quartile, and do not resuscitate (DNR) status (V4986). Diagnostic and procedure codes were collated utilizing the ICD-9, Clinical Modification scheme.
To define SES, we relied on median household income level for the zip code of the patient’s residence. The use of income data as a sole measure of SES is common but not ideal in health outcomes research.22 Ideally, a multilevel analysis would be performed incorporating detailed information on factors such as wealth, education status, and marital status, among others. Unfortunately, the NIS, as with most large administrative data sets, does not contain detailed information on these other factors. Thus for the purposes of this analysis, when we refer to SES we are referring to median household income. For the purpose of univariate analysis, we compared the lowest quartile to the highest quartile of median zip code income. For multivariate modeling, the highest quartile served as the reference value, and data from all quartiles were included in the model. The median household incomes for the zip code quartiles defined by the AHRQ were 1 (USD$1-USD$38 999), 2 (USD$39 000-USD$47 999), 3 (USD$48 000-USD$63 999), and 4 (USD$64 000+).
Severity of Sepsis
In order to compare accurately across levels of SES, we utilized the sepsis severity score developed by Ford et al.23 This validated scoring system uses administrative data to adjust for risk of in-hospital mortality in patients with sepsis. Factors included in the model are age, gender, race, early mechanical ventilation (<2 days since admission), shock, treatment in an ICU, and 24 of the Elixhauser Comorbidity indices (listed later in the article). Shock was defined as the presence of septic shock (785.52) or shock (785.50). As there is no flag variable for ICU admission in the NIS data set, we defined ICU care as the presence of any of these procedures: mechanical ventilation (96.70, 96.71, and 96.72), vasopressor infusion (00.17), arterial line placement (38.91), or central line placement (38.97).
Statistical Analysis
All analyses were performed using SAS version 9.4 (SAS Institute, Cary, North Carolina) using complex survey procedures. Univariate analysis utilized independent t tests for normally distributed data and the Wilcoxon rank sum test for nonnormal data. χ2 testing was used for categorical data. All tests were performed with an α level of .05.
Multivariate logistic regression analysis modeling the outcome of in-hospital mortality was performed. The variables included in the model were selected a priori and included the severity of illness covariates described in the Methods section.23 In order to strengthen the analysis, we also included insurance coverage status, hospital size, hospital teaching status, and DNR status. For testing of linear trend of odds ratio [OR], the Cochran-Armitage trend test was used.
Results
A total of 8 023 590 admissions from the 2011 NIS were examined. There were 671 858 patients who met the Angus definition of sepsis and were included in the analysis (Figure 1). The results of the univariate analysis between the highest zip code income quartile and the lowest are displayed in Table 1. The lowest income residents compared to the highest were younger (66.9 years, standard deviation [SD] = 16.5 vs 71.4 years, SD = 16.1, P < .01), more likely to be female (53.5% vs 51.9%, P < .01), less likely to be white (54.6% vs 76.6%, P < .01), as well as less likely to have health insurance coverage (92.8% vs 95.9%, P < .01). Lower income patients were more likely to receive early mechanical ventilation (13.5% vs 11.3%, P < .01); however, they had a lower incidence of shock (30.0% vs 31.7%, P < .01). There was no difference in unadjusted in-hospital mortality observed between the 2 levels of income (11.0% vs 11.4%, P = .13).
Figure 1.
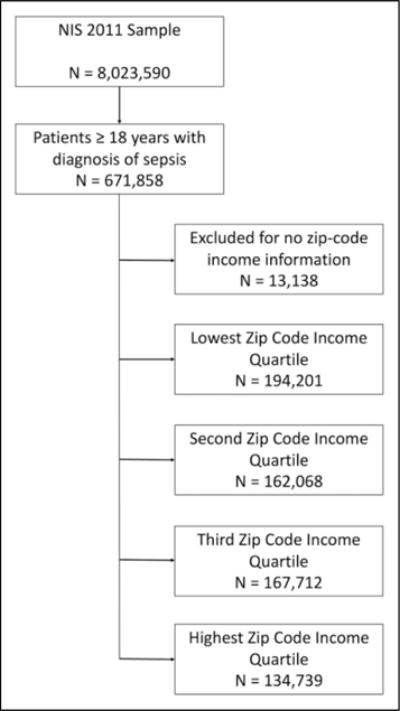
Patient selection flow diagram.
Table 1.
Baseline Demographic and Patient Characteristics for Patients Admitted With Sepsis in the Lowest and Highest Income Quartiles.
| Lowest Income Quartile (n = 194 201) |
Highest Income Quartile (n = 134 739) |
P Value | |
|---|---|---|---|
| Age, years, mean (SD) | 66.9 (16.5) | 71.4 (16.1) | <.01 |
| Length of stay in days, median (IQR) | 6.2 (3.3–11.9) | 5.9 (3.2–11.3) | .04 |
| In-hospital mortality, n (%) | 21 257 (11.0) | 15 329 (11.4) | .13 |
| Female gender, n (%) | 103 394 (53.5) | 69 993 (51.9) | <.01 |
| Race | |||
| White, n (%) | 105 732 (54.6) | 103 273 (76.6) | |
| Black, n (%) | 45 567 (23.4) | 10 376 (7.7) | |
| Hispanic, n (%) | 17 999 (9.3) | 6536 (4.9) | |
| Other, n (%) | 24 897 (12.6) | 14 548 (10.7) | <.01 |
| Insurance coverage, n (%) | 180 077 (92.8) | 129 214 (95.9) | <.01 |
| Early mechanical ventilation, n (%) | 26 184 (13.5) | 15 160 (11.3) | <.01 |
| Shock, n (%) | 58 353 (30.0) | 42 886 (31.7) | <.01 |
| ICU admission, n (%) | 78 740 (40.3) | 53 442 (39.5) | .18 |
| Do not resuscitate status, n (%) | 14 494 (7.4) | 14 855 (10.9) | <.01 |
| Teaching hospital, n (%) | 93 433 (48.8) | 64 520 (48.7) | .85 |
| Hospital size, n (%) | |||
| Small | 17 632 (9.5) | 20 071 (14.7) | |
| Medium | 40 097 (21.5) | 34 352 (26.6) | |
| Large | 133 576 (69.0) | 79 548 (58.5) | <.01 |
Abbreviations: ICU, intensive care unit; IQR, interquartile range; SD, standard deviation.
The results of multivariate logistic regression analysis modeling the outcome of in-hospital mortality are displayed in Table 2. After controlling for severity of sepsis, residing in the lowest income quartile compared to the highest quartile was associated with a higher risk of mortality (OR: 1.06, 95% confidence interval [CI]: 1.03–1.08, P < .01). There was no association seen between the second (OR: 1.02, 95% CI: 0.99–1.05, P = .14) and third (OR: 0.99, 95% CI: 0.97–1.01, P = .40) quartiles compared to the highest. A test for linear trend for the ORs of zip code income quartiles had a P value of <.01, indicating a trend relationship response as income increases. The results of the other covariates in the model are displayed in Table 2.
Table 2.
Results of Multivariate Logistic Regression Analysis for Baseline Covariates for the Prediction of In-Hospital Mortality for Patients With Sepsis.a
| Variable | Odds Ratio | Confidence Interval (95%) | Adjusted Odds Ratio | Confidence Interval (95%) | P |
|---|---|---|---|---|---|
| Older age, per 5-year increase | – | – | 1.08 | 1.07–1.09 | <.01 |
| Female gender | 0.87 | 0.85–0.89 | 0.93 | 0.91–0.94 | <.01 |
| White race | 0.99 | 0.95–1.03 | – | – | – |
| Black race | 1.02 | 0.96–1.07 | 1.08 | 1.05–1.11 | <.01 |
| Hispanic race | 1.01 | 0.95–1.07 | 1.03 | 0.99–1.06 | .09 |
| Other race | 0.99 | 0.93–1.06 | 1.15 | 1.12–1.18 | <.01 |
| Zip code income quartile 1 | 1.01 | 0.97–1.05 | 1.06 | 1.03–1.08 | <.01 |
| Zip code income quartile 2 | 0.97 | 0.93–0.99 | 1.02 | 0.99–1.05 | .14 |
| Zip code income quartile 3 | 0.96 | 0.93–0.99 | 0.99 | 0.97–1.01 | .40 |
| Zip code income quartile 4 | 1.06 | 1.01–1.10 | – | – | – |
| Small hospital | 0.99 | 0.91–1.08 | – | – | – |
| Medium hospital | 0.95 | 0.88–1.01 | 0.88 | 0.86–0.91 | <.01 |
| Large hospital | 1.04 | 0.98–1.10 | 0.95 | 0.93–0.98 | <.01 |
| Teaching hospital | 1.09 | 1.02–1.16 | 1.05 | 1.03–1.07 | <.01 |
| Insurance coverage | 1.00 | 0.93–1.07 | 0.78 | 0.75–0.81 | <.01 |
| Shock | 2.73 | 2.64–2.83 | 2.53 | 2.49–2.58 | <.01 |
| ICU admission | 3.40 | 3.20–3.60 | 4.10 | 3.90–4.32 | <.01 |
| Early mechanical ventilation | 3.76 | 3.64–3.90 | 1.01 | 0.96–1.07 | .68 |
| Do not resuscitate status | 4.82 | 4.53–5.13 | 4.24 | 4.15–4.34 | <.01 |
| Alcohol abuse | 1.05 | 1.01–1.10 | 0.87 | 0.84–0.91 | <.01 |
| Anemia | 0.50 | 0.48–0.53 | 0.55 | 0.53–0.58 | <.01 |
| Arthritis | 0.86 | 0.82–0.90 | 1.05 | 1.01–1.10 | .02 |
| Congestive heart failure | 1.36 | 1.32–1.39 | 1.39 | 1.36–1.42 | <.01 |
| Chronic lung disease | 1.00 | 0.97–1.02 | 0.93 | 0.91–0.95 | <.01 |
| Depression | 0.57 | 0.55–0.60 | 0.67 | 0.65–0.69 | <.01 |
| Diabetes | 0.72 | 0.70–0.74 | 0.82 | 0.81–0.84 | <.01 |
| Drug abuse | 0.52 | 0.48–0.56 | 0.58 | 0.55–0.61 | <.01 |
| HIV infection | 1.26 | 1.09–1.45 | 1.46 | 1.33–1.61 | <.01 |
| Hypertension | 0.82 | 0.80–0.84 | 0.82 | 0.80–0.85 | <.01 |
| Hypothyroid | 0.80 | 0.77–0.82 | 0.81 | 0.79–0.83 | <.01 |
| Liver disease | 2.17 | 2.10–2.24 | 2.48 | 2.42–2.55 | <.01 |
| Lymphoma | 1.74 | 1.66–1.82 | 1.93 | 1.84–2.03 | <.01 |
| Metastatic cancer | 2.55 | 2.46–2.65 | 1.94 | 1.86–2.01 | <.01 |
| Nonmetastatic cancer | 2.04 | 1.98–2.10 | 1.48 | 1.44–1.53 | <.01 |
| Neurological disorders | 1.51 | 1.46–1.55 | 1.35 | 1.33–1.38 | <.01 |
| Obesity | 0.61 | 0.58–0.63 | 0.81 | 0.78–0.83 | <.01 |
| Paralysis | 1.02 | 0.97–1.07 | 0.98 | 0.93–1.02 | .29 |
| Peripheral vascular disease | 1.15 | 1.11–1.19 | 1.22 | 1.19–1.26 | <.01 |
| Peptic ulcer | 0.77 | 0.71–0.83 | 0.76 | 0.71–0.85 | <.01 |
| Psychiatric disease | 0.57 | 0.53–0.61 | 0.66 | 0.62–0.70 | <.01 |
| Pulmonary circulatory disease | 1.32 | 1.28–1.37 | 1.34 | 1.30–1.38 | <.01 |
| Renal failure | 0.89 | 0.87–0.91 | 1.12 | 1.09–1.16 | <.01 |
| Weight loss | 1.80 | 1.74–1.87 | 1.38 | 1.36–1.41 | <.01 |
Abbreviation: ICU, intensive care unit.
For race analysis, white is the reference. For zip code income quartile, the highest quartile serves as the reference. For hospital size, small hospitals serve as the reference. All variables displayed in the table were included in the final logistic regression model.
Discussion
In this nationwide analysis, we observed an association between household income level and risk of in-hospital mortality in patients with sepsis. Compared to the highest income quartile, residing in the lowest quartile of median household income was associated with a higher risk of death for patients admitted with sepsis. These disparities were evident after adjustment for severity of sepsis using a validated scoring tool that controlled for factors such as race, comorbidities, and ICU admission.
Our results are generally congruent with the existing literature on the effect of SES on mortality in sepsis. A Danish population–based study found that, compared to persons in the highest income tertile, those in the lowest income tertile were 2.77 times more likely to have community-acquired bacteremia.13 A second Danish study looked prospectively at 387 patients admitted to a general tertiary care ICU and found that, after controlling for disease severity and comorbidities, patients with lower personal income and lower levels of education had a greater risk of both 30- and 180-day mortality, as well as a greater risk of hospital readmission.14 Most recently, Goodwin et al examined the association of residing in an MUA in South Carolina on the incidence and outcomes of sepsis.15 They found an increased incidence of sepsis hospitalizations (8.6 vs 6.8 cases/1000 people, P < .01) as well as an increased risk of mortality after adjustment for severity of sepsis. These findings likely explain the uneven distribution of sepsis across zip code income quartiles seen in our analysis.
The deleterious effect income level on mortality in sepsis is likely multifactorial. Social factors such as lack of appropriate housing, overcrowding, poor nutrition, and decreased access to preventative health-care measures such as vaccinations have all been shown to negatively impact health in low SES groups.24,25 These groups have also been shown to have higher rates of chronic diseases and increased health-care utilization, reflecting poorer baseline health.7,26,27 Furthermore, immunosuppressive conditions such as HIV, which are more common in low-income individuals, may directly relate to increased incidence of sepsis.28 Interestingly, however, Koch et al found that less than half of the discrepancy they observed in rates of bacteremia between persons of high versus low income could be accounted for by differing rates of chronic disease and substance abuse, suggesting that the effect of income on health is profound and multifaceted.13 As an example, the higher rates of DNR status in the highest income quartile likely reflect increased access to primary care as well as palliative care.6,29
In our study, we used median zip code income as a surrogate marker for SES. Although this metric has been widely used in other analyses of SES, it fails to capture other components of SES that are relevant to health care. The concept of MUAs used by Goodwin et al reflects the rate of primary care physicians per capita, the infant mortality rate, the fraction of the population who are aged older than 65 years, and the percentage of the population below the poverty line. In their recent article, they found residence in an MUA to be associated with mortality in patients with severe sepsis, whereas there was no association with traditional zip code–based surrogates.15 There are several possible reasons for the discrepancy with our findings. The composite MUA score captures additional factors that may negatively impact health care, which may have generated a significant association with mortality in a small-scale study. Goodwin et al looked only at patients in South Carolina; it is therefore possible that there are significant regional variations in the impact of income on mortality in sepsis. Furthermore, their cohort focused exclusively on patients with severe sepsis, while our analysis used the Angus definition to capture a broader population.19 Regrettably, data on MUAs, and other key pieces of information such as educational level attained, are difficult to access in many regions. Our findings of an OR of 1.06 for increased mortality in sepsis for patients in the lowest income quartile are thought provoking; however, the clinical utility of this value is unclear. The day-to-day management of these patients should not differ based on their income; however, this finding may reflect systemic differences in care for poorer patients. Further research into health outcomes from sepsis in low-income patients needs to be undertaken.
The strengths of this analysis lie primarily in its size and generalizability. Examination of patients in 47 of 50 states allows for extrapolation of our findings to care delivery across the United States.17 Our use of the Angus definition of sepsis allowed for a very high specificity and a moderate degree of sensitivity for identifying patients with sepsis. Furthermore, the use of the sepsis severity score developed by Ford et al allowed for adjustment of the severity of sepsis in our modeling, a key component lacking from previous studies.23
This study had several limitations, and its results must be interpreted in the context of study design. The use of large-scale retrospective administrative data comes with inherent risks of coding errors and misclassification bias. As discussed above, the use of median household income by zip code as a measure of SES is not perfect. Ideally, a multilevel analysis incorporating educational attainment and other factors, such as those included in the MUA designation, would better characterize the true SES of patients. Furthermore, median household income may have been biased by differing numbers of individuals per household, for which we were not able to control. It is also possible that there is a more complicated relationship between income and outcomes in sepsis that was not accurately captured by dividing income into quartiles. Unfortunately, the NIS only provides the quartile of household income and not the raw dollar figures which would allow for more complex modeling. Although we were able to control for severity of sepsis in our study using a tool validated in administrative data, a more granular severity of illness indicator such as the Acute Physiology and Chronic Health Evaluation II may have increased the strength of our conclusions.30 Additionally, as the Angus definition of sepsis is only 50% sensitive, we likely did not capture some patients who had sepsis in our analysis. Nevertheless, the high specificity of the Angus definition allowed us to have a very well-defined cohort with sepsis.
Conclusion
In this national cohort analysis, residence in the lowest income median quartile zip code was associated with a higher risk of in-hospital mortality for patients with sepsis when compared to those in the highest income areas, after adjustment for severity of sepsis. These results should be pursued with future work incorporating a more comprehensive measure of SES, as well as granular patient-level data, to further elucidate the impact of SES on mortality in patients with sepsis.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr Russell reports receiving consulting fees from: 1. Cubist Pharmaceuticals (now owned by Merck; formerly was Trius Pharmaceuticals; developing antibiotics), 2. Leading Biosciences (developing a sepsis therapeutic), 3. Ferring Pharmaceuticals (manufactures vasopressin and is developing selepressin), 4. Grifols (sells albumin), 5. La Jolla Pharmaceuticals (developing angiotensin II; Dr Russell chairs the DSMB of a trial of angiotensin II), 6. CytoVale Inc (developing a sepsis diagnostic), 7. Asahi Kesai Pharmaceuticals of America (AKPA) (developing recombinant thrombomodulin). Dr Russell reports having received an investigator-initiated grant from Grifols that is provided to and administered by UBC.
Footnotes
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Dr Russell reports patents owned by the University of British Columbia (UBC) that are related to PCSK9 inhibitor(s) and sepsis and related to the use of vasopressin in septic shock. Dr Russell is an inventor on these patents. Dr Russell is a founder, Director and shareholder in Cyon Therapeutics Inc (developing a sepsis therapy). Dr Russell has share options in Leading Biosciences Inc. Dr Russell is a shareholder in Molecular You Corp. Dr Walley reports patents owned by the University of British Columbia (UBC) that are related to PCSK9 inhibitor(s) and sepsis and related to the use of vasopressin in septic shock. Dr Walley is an inventor on these patents. Dr Walley is a founder, Director and shareholder in Cyon Therapeutics Inc (developing a sepsis therapy). Dr Boyd reports patents owned by the University of British Columbia (UBC) that are related to PCSK9 inhibitor(s) and sepsis and related to the use of vasopressin in septic shock. Dr Boyd is an inventor on these patents. Dr Boyd is a founder, Director and shareholder in Cyon Therapeutics Inc (developing a sepsis therapy).
References
- 1.Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med. 1999;341(18):1359–1367. doi: 10.1056/NEJM199910283411806. [DOI] [PubMed] [Google Scholar]
- 2.Kapral MK, Wang H, Mamdani M, Tu JV. Mortality after stroke. Stroke. 2002;33(1):268–275. doi: 10.1161/hs0102.101169. [DOI] [PubMed] [Google Scholar]
- 3.Anderson GM, Grumbach K, Luft HS, Roos LL, Mustard C, Brook R. Use of coronary artery bypass surgery in the United States and Canada. Influence of age and income. JAMA. 1993;269(13):1661–1666. [PubMed] [Google Scholar]
- 4.Katz S. Hospital utilization in Ontario and the United States: the impact of socioeconomic status and health status. Can J Public Heal. 1996;87(4):253–256. [PubMed] [Google Scholar]
- 5.Sharrocks K, Spicer JF, Camidge DR, Papa S. The impact of socioeconomic status on access to cancer clinical trials. Br J Cancer. 2014;111(9):1684–1687. doi: 10.1038/bjc.2014.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rush B, Hertz P, Bond A, McDermid RC, Celi LA. Use of palliative care in patients with end-stage COPD and receiving home oxygen: national trends and barriers to care in the United States. Chest. 2017;151(1):41–46. doi: 10.1016/j.chest.2016.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murray CJL, Kulkarni SC, Michaud C, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med. 2006;3(9):1513–1524. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Latour J. Inequalities in health in intensive care patients. J Clin Epidemiol. 1991;44(9):889–894. doi: 10.1016/0895-4356(91)90051-a. [DOI] [PubMed] [Google Scholar]
- 9.Welch CA, Harrison DA, Hutchings A, Rowan K. The association between deprivation and hospital mortality for admissions to critical care units in England. J Crit Care. 2010;25(3):382–390. doi: 10.1016/j.jcrc.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Elixhauser A, Friedman B, Stranges E. 2009 HCUP Statistical Brief #122. Rockville, MD: Agency for Healthcare Research and Quality (US); 2011. Septicemia in U.S. Hospitals. [PubMed] [Google Scholar]
- 11.Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013;41(5):1167–1174. doi: 10.1097/CCM.0b013e31827c09f8. [DOI] [PubMed] [Google Scholar]
- 12.Brun-Buisson C, Meshaka P, Pinton P, Vallet B, EPISEPSIS Study Group EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med. 2004;30(4):580–588. doi: 10.1007/s00134-003-2121-4. [DOI] [PubMed] [Google Scholar]
- 13.Koch K, Søgaard M, Nørgaard M, Thomsen RW, Schønheyder HC; Danish Collaborative Bacteremia Network Socioeconomic inequalities in risk of hospitalization for community-acquired bacteremia: a Danish population-based case-control study. Am J Epidemiol. 2014;179(9):1096–1106. doi: 10.1093/aje/kwu032. [DOI] [PubMed] [Google Scholar]
- 14.Schnegelsberg A, Mackenhauer J, Nibro HL, Dreyer P, Koch K, Kirkegaard H. Impact of socioeconomic status on mortality and unplanned readmission in septic intensive care unit patients. Acta Anaesthesiol Scand. 2016;60(4):465–475. doi: 10.1111/aas.12644. [DOI] [PubMed] [Google Scholar]
- 15.Goodwin AJ, Nadig NR, McElligott JT, Simpson KN, Ford DW. Where you live matters: the impact of place of residence on severe sepsis incidence and mortality. Chest. 2016;150(4):829–836. doi: 10.1016/j.chest.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vandenbroucke JP, von Elm E, Altman DG, et al. STROBE initiative Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–835. doi: 10.1097/EDE.0b013e3181577511. [DOI] [PubMed] [Google Scholar]
- 17.Introduction to the HCUP Nationwide Inpatient Sample [Internet] Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project; 2011. https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2011.pdf. Accessed December 31, 2016. [Google Scholar]
- 18.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Iwashyna TJ, Odden A, Rohde J, et al. Identifying patients with severe sepsis using administrative claims: patient-level validation of the angus implementation of the international consensus conference definition of severe sepsis. Med Care. 2014;52(6):e39–e43. doi: 10.1097/MLR.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Donnelly JP, Hohmann SF, Wang HE. Unplanned readmissions after hospitalization for severe sepsis at academic medical center-affiliated hospitals. Crit Care Med. 2015;43(9):1916–1927. doi: 10.1097/CCM.0000000000001147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barnato AE, Alexander SL, Linde-Zwirble WT, Angus DC. Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med. 2008;177(3):279–284. doi: 10.1164/rccm.200703-480OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shavers VL. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc. 2007;99(9):1013–1023. [PMC free article] [PubMed] [Google Scholar]
- 23.Ford DW, Goodwin AJ, Simpson AN, Johnson E, Nadig N, Simpson KN. A severe sepsis mortality prediction model and score for use with administrative data. Crit Care Med. 2015;(16):12–15. doi: 10.1097/CCM.0000000000001392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baker MG, Barnard LT, Kvalsvig A, et al. Increasing incidence of serious infectious diseases and inequalities in New Zealand: a national epidemiological study. Lancet. 2012;379(9821):1112–1119. doi: 10.1016/S0140-6736(11)61780-7. [DOI] [PubMed] [Google Scholar]
- 25.Cohen S. Social status and susceptibility to respiratory infections. Ann N Y Acad Sci. 1999;896:246–253. doi: 10.1111/j.1749-6632.1999.tb08119.x. [DOI] [PubMed] [Google Scholar]
- 26.Esper AM, Moss M, Lewis CA, Nisbet R, Mannino DM, Martin GS. The role of infection and comorbidity: factors that influence disparities in sepsis. Crit Care Med. 2006;34(10):2576–2582. doi: 10.1097/01.CCM.0000239114.50519.0E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Droomers M, Westert GP. Do lower socioeconomic groups use more health services, because they suffer from more illnesses? Eur J Public Health. 2004;14(3):311–313. doi: 10.1093/eurpub/14.3.311. [DOI] [PubMed] [Google Scholar]
- 28.An Q, Prejean J, Harrison KM, Fang X. Association between community socioeconomic position and HIV diagnosis rate among adults and adolescents in the United States, 2005 to 2009. Am J Public Health. 2013;103(1):120–126. doi: 10.2105/AJPH.2012.300853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewis JM, DiGiacomo M, Currow DC, Davidson PM. Dying in the margins: understanding palliative care and socioeconomic deprivation in the developed world. J Pain Symptom Manage. 2011;42(1):105–118. doi: 10.1016/j.jpainsymman.2010.10.265. [DOI] [PubMed] [Google Scholar]
- 30.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. [PubMed] [Google Scholar]


