Abstract
Oral ulcers are the most common mucosal sign in juvenile-onset systemic lupus erythematosus (JSLE). The ulcers are one of the key clinical features; however, the terminology of oral ulcers, especially in JSLE patients, is often vague and ill-defined. In fact, there are several clinical manifestations of oral ulcers in JSLE, and some lesions occur when the disease is active, indicating that early management of the disease should be started. Oral ulcers are classified as lupus erythematosus (LE) specific, where the lesional biopsy shows a unique pattern of mucosal change in LE, and LE nonspecific, where the ulcers and their histopathological findings can be found in other oral diseases. Here, the clinical manifestations, diagnosis and management of oral ulcers in JSLE patients are reviewed.
Key Points
| Oral ulcers are one of the key clinical features in juvenile-onset systemic lupus erythematosus (JSLE) patients; however, the terminology remains unclear. |
| There are several oral ulcers in JSLE patients that sometimes go unnoticed, and some ulcers indicate that treatment should be started promptly. |
| Lesional biopsy is required when other oral diseases cannot be excluded, such as oral lichen planus and oral lichenoid contact lesions. |
Introduction
Juvenile-onset systemic lupus erythematosus (JSLE) is one of the most common autoimmune diseases in children and has a clinical course ranging from mild, gradual onset to rapid, progressive multi-organ failure [1]. Approximately 20% of systemic lupus erythematosus (SLE) patients are diagnosed in childhood and adolescence, with a median age of 11–12 years [2–5]. The prevalence of JSLE is high in Asian and African populations, with a female predominance (female to male ratio: 4.7:1–6.2:1) [6, 7]. JSLE patients usually present with mucocutaneous lesions, renal involvement, central nervous system (CNS) disorders and hematological abnormalities [4]. The diagnosis of JSLE typically needs four out of 11 criteria based on the revised classification criteria of the American College of Rheumatology (ACR) 1997. However, the new Systemic Lupus International Collaborating Clinics (SLICC) group classification criteria are now widely used in JSLE, and the diagnosis requires at least four out of 17 criteria (including at least one clinical criterion and one immunological criterion), or lupus nephritis with a presence of antinuclear antibody (ANA) or anti-double-stranded DNA (anti-ds DNA) antibodies [8, 9].
Mucocutaneous manifestations are common signs and symptoms in JSLE at diagnosis, and they are found in approximately 70–75% of JSLE populations worldwide [7, 10–14]. According to the ACR revised criteria, four mucocutaneous features are included, one of which is oral ulcers. The terminology of oral ulcers in these criteria is usually “painless oral or nasopharyngeal ulceration observed by a physician”, yet these may be unclear, especially in children [15]. In the new SLICC group classification criteria, oral ulcers remain included. They are defined more specifically as oral ulcers at palate, buccal mucosa or tongue without other causes (e.g., vasculitis or infection) [8]. In fact, there are several types of oral ulcers presented in JSLE patients. Moreover, some ulcers (e.g., palatal erythematous ulcers and aphthous ulcers) occur particularly when disease is active. However, other types of ulcers may appear without being related to disease activity and severity [16, 17].
The mucocutaneous manifestations in JSLE are classified as lupus erythematosus (LE)-specific and LE-nonspecific skin diseases, according to the Gilliam classification of skin lesions associated with LE [18]. Typical oral ulcers in the ACR criteria and SLICC group classification criteria are LE-specific and most lesions are categorized in chronic cutaneous lupus erythematosus (CCLE), such as oral discoid lupus erythematosus (DLE), whilst others are LE-nonspecific (e.g., aphthous ulcers) [10].
We searched for literature reviews and studies in the PubMed database using the following key words: “oral/mucosa/mucosal/mucocutaneous” and “lupus/LE/SLE” and “juvenile/child/childhood/children” (until August 1, 2016). All published articles related to the clinical manifestations of oral ulcers in JSLE patients were reviewed.
Epidemiology
Oral ulcers are the second most common mucocutaneous manifestation in JSLE patients after butterfly rash [11], and they are the most common mucosal sign of JSLE [19]. The incidence of oral ulcers in JSLE is approximately 11.4–37%, which is significantly higher than in adult SLE [4, 5, 20]. In adult patients, males have a lower rate of oral ulcers than females, but there are no reports of gender preference in children [21]. The common oral ulcers in JSLE patients are palatal erythematous ulcers, oral DLE and aphthous ulcers [10, 11].
Clinical Manifestations
Oral mucosa is normally characterized into three types: lining; masticatory and specialized mucosa [22, 23]. The lining mucosa is nonkeratinized epithelium covering buccal mucosa, labial mucosa, alveolar mucosa, soft palate, ventral tongue and the floor of the mouth [24], whereas the masticatory mucosa is keratinized mucosa covering gingiva, attached gingiva and hard palate. The dorsal surface of the tongue is covered with specialized mucosa that consists of taste buds and epithelially derived structures called papillae [22–24]. Understanding of these different types of oral mucosa is important for making a diagnosis, as some lesions tend to affect one type of tissue more than the others. The clinical manifestations of oral ulcers in JSLE patients are summarized in Table 1 [16, 25–30].
Table 1.
Clinical manifestations of oral ulcers in juvenile-onset systemic lupus erythematosus (JSLE) [16, 25]
| Classification | Type of lesions | Locations | Key clinical features |
|---|---|---|---|
| LE-specific oral ulcers | Palatal erythematous ulcer | Masticatory mucosa (especially hard palate) | Painless, single/multiple erythematous ulcer(s) |
| Oral discoid LE | Lining mucosa (especially buccal mucosa and soft palate) | Atrophic plaque with white radiating keratotic striae and painful telangiectasia | |
| Honeycomb plaque | Lining and masticatory mucosa | Chronic, well-circumscribed erythematous plaque with white lacy hyperkeratosis | |
| Verrucous LE | Lining mucosa | Raised, intense keratotic plaque | |
| LE-nonspecific oral ulcers | Aphthous ulcer | Lining mucosa | White to yellow painful ulcer(s) with erythematous halo |
| Lupus cheilitis | Buccal lips (especially lower lip) | Small or diffuse erythematous and edematous lips, or crusty painful ulcer(s) |
LE lupus erythematosus
Lupus Erythematosus (LE)-Specific Oral Ulcers
Palatal Erythematous Ulcers
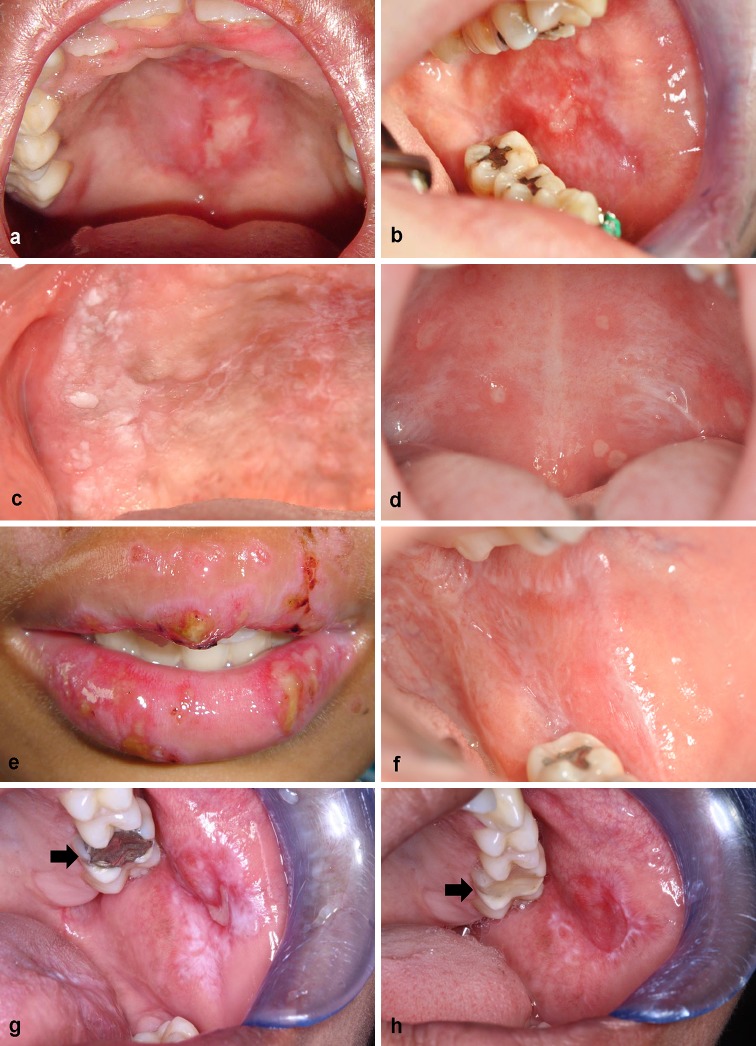
A palatal erythematous ulcer is the typical oral ulcer in the ACR criteria, and it is described as a usually painless, single/multiple lesion(s) at masticatory or keratinized mucosa, especially the hard palate (Fig. 1a). It is an acute sign occurring when disease is active, and sometimes is the first clue of JSLE without skin lesions [26]. The early lesion may be hemorrhaging before developing into the ulcer [10]. If the ulcers are coalesced into a large erythematous patch at the hard palate and extend to the soft palate, the early onset of oral DLE should be considered. Palatal erythematous ulcers are sometimes characterized as acute cutaneous lupus erythematosus (ACLE) of LE-specific skin disease in some reports [16].
Fig. 1.
Oral ulcers in JSLE patients and their differential diagnoses. a–c LE-specific oral ulcers: a a palatal erythematous ulcer at hard palate; b a painful oral discoid LE with well-demarcated radiating white striae at left buccal mucosa; c verrucous LE at alveolar ridge. d–e LE-nonspecific oral ulcers: d multiple aphthous ulcers with erythematous halo at soft palate; e extensive erosive lupus cheilitis at both upper and lower lips. f–h The differential diagnoses: f an oral lichen planus with typical white reticular striae (Wickham striae) at left buccal mucosa and retromolar trigone; g an oral lichenoid contact lesion associated with large amalgam filling at left maxillary first molar (arrow); h clinical improvement 2 weeks after replacement with non-metal restoration. JSLE juvenile-onset systemic lupus erythematosus, LE lupus erythematosus
Oral Discoid Lupus Erythematosus
Oral DLE is a well-defined, atrophic plaque with white radiating keratotic striae and telangiectasia at lining mucosa, especially buccal mucosa and the soft palate (Fig. 1b) [16, 26]. JSLE patients often develop an erythematous lesion with painful telangiectasia, and keratotic scaling occurs afterward. The lesion eventually transforms into an atrophic lesion with keratotic border [31]. The typical oral DLE is composed of (a) white papule/plaque, (b) central erythema, (c) a border zone of irradiating white striae and (d) peripheral telangiectasia [27, 28]. Although the lesion appears at lining mucosa, the masticatory mucosa may be involved without radiating striae (e.g., hard palate) [28]. The dental alveolar process is another location that should be carefully inspected, as oral DLE is easily overlooked. Of note, the radiating white striae sometimes resemble the Wickham striae of oral lichen planus (OLP); therefore, a lesional biopsy should be performed if a definite diagnosis is required. Other locations of oral DLE are not common, such as vermilion borders of buccal lips and specialized mucosa (tongue) [10, 31].
Honeycomb Plaques
A honeycomb plaque is described as a chronic, well-circumscribed plaque with white lacy hyperkeratosis and buccal erythema [16, 25, 32]. The lesion usually occurs at both lining and masticatory tissues, but the lesion at the lining part (e.g., soft palate) is less hyperkeratotic [25]. Some reports suggest that this lesion is a morphological variant or a late stage of oral DLE [18]. The incidence of honeycomb plaque in JSLE is very rare.
Verrucous LE
Verrucous LE is a rare type of CCLE-specific oral ulcer that has been reported in adult SLE and JSLE [16, 33–35]. The lesion is a raised, intense keratotic plaque normally found at lining mucosa, such as the buccal mucosa and lips. However, the hard palate (e.g., alveolar ridge) may be involved (Fig. 1c) [33].
LE-Nonspecific Oral Ulcers
Aphthous Ulcers
An aphthous ulcer is described as a white to yellow painful ulcer with a surrounding red rim. The lesion is usually presented with multiple lesions or in a group, and tends to involve primarily lining tissue: the soft palate, buccal and labial mucosa. Aphthous ulcers are more common in JSLE patients than in adult SLE and usually occur when disease is active [36]. There are four types of aphthous ulcer, classified as (a) minor ulcers, smaller than 1 cm, usually healing without scar; (b) major ulcers, larger than 1 cm, often healing with scar; (c) herpetiform ulcers, a group of small ulcers (more than ten lesions); and (d) severe ulcers, a continuous minor ulcer lasting months [37]. In our observations, the most common type of aphthous ulcer in JSLE patients is multiple minor ulcers and less than ten lesions (Fig. 1d).
Lupus Cheilitis
Lupus cheilitis is an inflammation of the buccal lips. The typical lesion is small or diffuse, erythematous and edematous, and may turn into crusty painful ulcers [29]. Cheilitis often involves the vermilion zone of the lower lip (typical lupus cheilitis) [30]. As the lesion is found in the sun-exposed area, lupus cheilitis is usually associated with photosensitivity in JSLE patients [25]. Extensive erosive lupus cheilitis that involves both upper and lower lips has also been reported in JSLE patients and appears in active disease (Fig. 1e) [38].
Other LE-Nonspecific Oral Lesions
Bullous SLE is a rare clinical manifestation developed by circulating antibodies against type VII collagen at the sub-epidermis. It typically presents with multiple tense bullae at the face, neck and trunk [39]. Bullous LE at buccal mucosa has been reported in adult SLE and JSLE patients [40, 41].
Diagnosis
Clinical evaluation and follow-up is usually sufficient for making a diagnosis of oral ulcers. However, atypical ulcers are sometimes difficult to diagnose, particularly when the patients cannot fulfill the ACR criteria or the new SLICC group classification criteria. In these circumstances, histopathology and immunofluorescence studies are helpful. The histopathology of LE-specific oral ulcers (DLE) shows hyperkeratosis with keratotic plugs. The rete ridge of the mucosa becomes atrophic with deep dermal inflammatory cell infiltration and edematous lamina propria. Positive periodic acid-Schiff staining is found at the juxta-epithelial site in a thick continuous or a patchy pattern [42–44]. In contrast, the histopathology of LE-nonspecific oral ulcers is varied, and no such specific pattern can be identified, as similar findings are also seen in other oral diseases. Direct immunofluorescence of LE-specific oral ulcers shows a band-like deposition of immunoglobulin (IgG, IgM or IgA) at the basement membrane of the lesion [45, 46], in contrast to pemphigoid diseases, where linear deposits can be seen [47].
Although clinical features are sufficient for making a diagnosis, there are several diseases with appearances that are similar to the oral ulcers seen in JSLE.
Oral Lichen Planus
As mentioned previously, atypical oral DLE may mimic OLP. OLP has multiple clinical appearances, such as reticular, erythematous, plaque-like and erosive types. Oral DLE may resemble the reticular and erythematous types of OLP, which can present as a white lacy patch and erythematous mucosa. However, the most frequent site of involvement in OLP is posterior buccal mucosa (rarely at the palates) (Fig. 1f) [25, 48, 49]. Wickham striae are characteristic of OLP, but a lesional biopsy is sometimes necessary when a definite diagnosis cannot be made. The histopathology shows basal cell degeneration damage and dense subepithelial band-like infiltration of T lymphocytes in the subjacent connective tissue [50]. Direct immunofluorescence is also helpful, as OLP shows positive staining with anti-fibrinogen in the dermoepidermal junction and positive staining with immunoreactive proteins in the colloid bodies [16, 51, 52].
Oral Lichenoid Contact Lesions
An oral lichenoid contact lesion (OLCL) is a white patch or plague at the buccal mucosa, and its appearance is similar to oral DLE and OLP [27, 53] (Fig. 1g, h). The cause of OLCLs is thought to be a delayed-typed hypersensitivity reaction to a component of dental restorative materials, and use of metallic dental fillings can induce this lesion. OLCLs usually disappear when the metallic dental fillings have been removed [27, 53].
Leukoplakia
Leukoplakia is a homogenous or non-homogenous white plague at the buccal mucosa [54]. As there are no specific histological findings in this lesion, other causes need to be excluded [55]. Oral DLE sometimes transforms into a white homogenous plaque when the lesion has persisted for several months. Therefore, it should be considered as one of the differential diagnoses in leukoplakia [56].
Herpetic Gingivostomatitis
The typical lesion comprises a group of multiple painful vesicles on an erythematous base at the buccal lips, oral mucosa or tongue, with red and swollen gingiva. A group of multiple ulcers and aphthous ulcers in JSLE are quite similar. However, the important clues of herpetic gingivostomatitis are prodromal symptoms and a history of herpes simplex virus (HSV) infection. A Tzanck smear, demonstrating cytopathic effects of the virus, is useful for diagnosis. The lesion usually spontaneously resolves within 2 weeks [57]. Therefore, oral ulcers in JSLE should be considered if this lesion still persists beyond 2 weeks.
Management
Topical anti-inflammatory agents are the treatment of choice for oral ulcers in JSLE [58, 59]. Topical corticosteroids (e.g., 0.1% triamcinolone oral paste) are one of the most commonly used medications in JSLE patients, and shorten the course and severity of the ulcers. The duration of corticosteroid usage depends on the severity of the symptoms. If the oral lesions are refractory to the treatment, then more potent (e.g., betamethasone or clobetasol in oral preparation) or systemic drugs may be needed [58]. However, some oral ulcers are very difficult to treat even when high-potency topical corticosteroid is applied, especially palatal erythematous ulcers and oral DLE [26]. Steroid-sparing agents, such as calcineurin inhibitors (e.g., 0.03 or 0.1% tacrolimus) are also applicable when the side effects of corticosteroids are of concern [60, 61]. The other route of corticosteroid administration, intra-lesional injection, is rarely used, especially in children, due to pain. Noticeably, systemic corticosteroids are normally prescribed as a first-line drug for treatment in JSLE because most patients develop multiple-organ involvement and these drugs dramatically improve the clinical signs and symptoms, including oral ulcers [25, 62].
Antimalarial drugs, such as hydroxychloroquine, are usually used as first-line drugs combined with systemic corticosteroids if the patient needs systemic therapy. However, these drugs can be used as a monotherapy in mild cases of JSLE with mucocutaneous manifestations (e.g., malar rash, discoid rash, photosensitivity, including oral ulcers) [63, 64]. Complete blood counts, eye examination and liver function tests should be monitored, as drug toxicities may occur in children.
Avoiding sun exposure, especially in patients with lupus cheilitis and oral DLE at buccal lips, is recommended, as UV light is an aggravating factor [18, 25]. Routine wet dressing can soothe the pain, and keeping chapped lips moist using petrolatum ointment or lip balm (with UV protection) is needed.
A regular dental check-up is also recommended in JSLE patients who present with oral ulcers. Good oral hygiene and prevention of secondary bacterial infection with oral rinses containing chlorhexidine should be advised [58, 59]. An infection should be suspected when the oral ulcers become painful or bleed. Local antibiotics and antifungal agents (e.g., nystatin) should be considered if infection is suspected.
Summary
Oral ulcers are commonly found in JSLE patients, and the typical lesion is a painless palatal erythematous ulcer at masticatory or keratinized mucosa, especially the hard palate. However, most ulcers including oral DLE and aphthous ulcers in JSLE patients appear at the lining tissue of the oral cavity (e.g., buccal mucosa, soft palate and tongue) and sometimes are unnoticed. Therefore, understanding of their clinical features and locations is very important. Clinical evaluation and follow-up is normally sufficient for making a diagnosis; however, lesional biopsy is needed particularly when other diseases (such as OLP or OLCL) cannot be ruled out. Topical corticosteroids remain the first-line treatment of oral ulcers, but the steroid-sparing agents (calcineurin inhibitors) can also be used in JSLE patients.
Acknowledgements
We would like to thank all JSLE patients and their families for contributing to the pictures in this review. Special thanks go to Assistant Professor Patnarin Kanjanabuch, DDS, MS and Assistant Professor Pratanporn Arirachakaran, Department of Oral Medicine, Faculty of Dentistry, Chulalongkorn University. Special acknowledgement goes to the Faculty of Medicine and Faculty of Dentistry, Chulalongkorn University, Bangkok, Thailand, the Institute of Integrative Biology and Institute of Translational Medicine, University of Liverpool, Liverpool, UK, and the Department of Paediatric Rheumatology, Alder Hey Children’s NHS Foundation Trust, Liverpool, UK.
Compliance with Ethical Standards
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
Pongsawat Rodsaward, Titipong Prueksrisakul, Tawatchai Deekajorndech, Steven W. Edwards, Michael W. Beresford and Direkrit Chiewchengchol declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual patients and their parents.
References
- 1.Levy DM, Kamphuis S. Systemic lupus erythematosus in children and adolescents. Pediatr Clin North Am. 2012;59(2):345–364. doi: 10.1016/j.pcl.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klein-Gitelman M, Reiff A, Silverman ED. Systemic lupus erythematosus in childhood. Rheumatic diseases clinics of North America. 2002;28(3):561–77, vi–vii. [DOI] [PubMed]
- 3.Li C, Wang B, Zhang J, Tan X. Clinical features, treatment and follow-ups of childhood systemic lupus erythematosus. Zhonghua yi xue za zhi. 2014;94(41):3259–3261. [PubMed] [Google Scholar]
- 4.Livingston B, Bonner A, Pope J. Differences in clinical manifestations between childhood-onset lupus and adult-onset lupus: a meta-analysis. Lupus. 2011;20(13):1345–1355. doi: 10.1177/0961203311416694. [DOI] [PubMed] [Google Scholar]
- 5.Tarr T, Derfalvi B, Gyori N, Szanto A, Siminszky Z, Malik A, et al. Similarities and differences between pediatric and adult patients with systemic lupus erythematosus. Lupus. 2015;24(8):796–803. doi: 10.1177/0961203314563817. [DOI] [PubMed] [Google Scholar]
- 6.Lehman TJ, McCurdy DK, Bernstein BH, King KK, Hanson V. Systemic lupus erythematosus in the first decade of life. Pediatrics. 1989;83(2):235–239. [PubMed] [Google Scholar]
- 7.Huang JL, Yeh KW, Yao TC, Huang YL, Chung HT, Ou LS, et al. Pediatric lupus in Asia. Lupus. 2010;19(12):1414–1418. doi: 10.1177/0961203310374339. [DOI] [PubMed] [Google Scholar]
- 8.Petri M, Orbai AM, Alarcon GS, Gordon C, Merrill JT, Fortin PR, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64(8):2677–2686. doi: 10.1002/art.34473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40(9):1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 10.Chiewchengchol D, Murphy R, Edwards SW, Beresford MW. Mucocutaneous manifestations in juvenile-onset systemic lupus erythematosus: a review of literature. Pediatr Rheumatol Online J. 2015;13:1. doi: 10.1186/1546-0096-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chiewchengchol D, Murphy R, Morgan T, Edwards SW, Leone V, Friswell M, et al. Mucocutaneous manifestations in a UK national cohort of juvenile-onset systemic lupus erythematosus patients. Rheumatology. 2014;53(8):1504–1512. doi: 10.1093/rheumatology/keu137. [DOI] [PubMed] [Google Scholar]
- 12.Ramirez Gomez LA, Uribe Uribe O, Osio Uribe O, Grisales Romero H, Cardiel MH, Wojdyla D, et al. Childhood systemic lupus erythematosus in Latin America. The GLADEL experience in 230 children. Lupus. 2008;17(6):596–604. doi: 10.1177/0961203307088006. [DOI] [PubMed] [Google Scholar]
- 13.Supavekin S, Chatchomchuan W, Pattaragarn A, Suntornpoch V, Sumboonnanonda A. Pediatric systemic lupus erythematosus in Siriraj Hospital. J Med Assoc Thailand = Chotmaihet thangphaet. 2005;88(Suppl 8):S115–S123. [PubMed] [Google Scholar]
- 14.Bader-Meunier B, Armengaud JB, Haddad E, Salomon R, Deschenes G, Kone-Paut I, et al. Initial presentation of childhood-onset systemic lupus erythematosus: a French multicenter study. J Pediatr. 2005;146(5):648–653. doi: 10.1016/j.jpeds.2004.12.045. [DOI] [PubMed] [Google Scholar]
- 15.Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25(11):1271–1277. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 16.Nico MM, Vilela MA, Rivitti EA, Lourenco SV. Oral lesions in lupus erythematosus: correlation with cutaneous lesions. EJD. 2008;18(4):376–381. doi: 10.1684/ejd.2008.0388. [DOI] [PubMed] [Google Scholar]
- 17.Khatibi M, Shakoorpour AH, Jahromi ZM, Ahmadzadeh A. The prevalence of oral mucosal lesions and related factors in 188 patients with systemic lupus erythematosus. Lupus. 2012;21(12):1312–1315. doi: 10.1177/0961203312454589. [DOI] [PubMed] [Google Scholar]
- 18.Mi C, Rd S, et al. Lupus erythematosus. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, et al., editors. Fitzpatrick’s dermatology in general medicine. 8. New York: McGraw Hill Medical; 2012. pp. 1909–1925. [Google Scholar]
- 19.Hiraki LT, Benseler SM, Tyrrell PN, Hebert D, Harvey E, Silverman ED. Clinical and laboratory characteristics and long-term outcome of pediatric systemic lupus erythematosus: a longitudinal study. J Pediatr. 2008;152(4):550–556. doi: 10.1016/j.jpeds.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 20.Choi JH, Park DJ, Kang JH, Yim YR, Lee KE, Lee JW, et al. Comparison of clinical and serological differences among juvenile-, adult-, and late-onset systemic lupus erythematosus in Korean patients. Lupus. 2015;24(12):1342–1349. doi: 10.1177/0961203315591024. [DOI] [PubMed] [Google Scholar]
- 21.Murphy G, Isenberg D. Effect of gender on clinical presentation in systemic lupus erythematosus. Rheumatology. 2013;52(12):2108–2115. doi: 10.1093/rheumatology/ket160. [DOI] [PubMed] [Google Scholar]
- 22.Gartner LP. Oral anatomy and tissue types. Semin Dermatol. 1994;13(2):68–73. [PubMed] [Google Scholar]
- 23.Squier CA, Kremer MJ. Biology of oral mucosa and esophagus. J Natl Cancer Inst Monogr. 2001;29:7–15. doi: 10.1093/oxfordjournals.jncimonographs.a003443. [DOI] [PubMed] [Google Scholar]
- 24.Woo S-B, et al. Biology and pathology of oral cavity. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, et al., editors. Fitzpatrick’s dermatology in general medicine. 8. New York: McGraw Hill Medical; 2012. pp. 827–851. [Google Scholar]
- 25.Burge SM, Frith PA, Juniper RP, Wojnarowska F. Mucosal involvement in systemic and chronic cutaneous lupus erythematosus. Br J Dermatol. 1989;121(6):727–741. doi: 10.1111/j.1365-2133.1989.tb08215.x. [DOI] [PubMed] [Google Scholar]
- 26.Ramakrishna Y, Reddy JS. Systemic lupus erythematosus presenting with oral mucosal lesions—a case report. J Clin Pediatr Dent. 2009;33(3):255–258. doi: 10.17796/jcpd.33.3.h7m84x4450x03768. [DOI] [PubMed] [Google Scholar]
- 27.Schiodt M, Pindborg JJ. Oral discoid lupus erythematosus. I. The validity of previous histopathologic diagnostic criteria. Oral Surg Oral Med Oral Pathol. 1984;57(1):46–51. doi: 10.1016/0030-4220(84)90259-7. [DOI] [PubMed] [Google Scholar]
- 28.Schiodt M, Halberg P, Hentzer B. A clinical study of 32 patients with oral discoid lupus erythematosus. Int J Oral Surg. 1978;7(2):85–94. doi: 10.1016/S0300-9785(78)80052-0. [DOI] [PubMed] [Google Scholar]
- 29.Guillet G, Constant D, Cales D, Helenon R. Cheilitis and labial lesions of lupus in the French Indies. Int J Dermatol. 1985;24(1):66–67. doi: 10.1111/j.1365-4362.1985.tb05370.x. [DOI] [PubMed] [Google Scholar]
- 30.Neville BW, Damm DD. Dermatologic diseases. In: Neville BW, editor. Oral and maxillofacial pathology. 3rd ed. St. Louis: Saunders/Elsevier; 2009. p. 690–760.
- 31.Andreasen JO. Oral Manifestations in discoid and systemic lupus erythematosus. I. Clinical investigation. Acta odontologica Scandinavica. 1964;22:295–310. doi: 10.3109/00016356409028206. [DOI] [PubMed] [Google Scholar]
- 32.Orteu CH, Buchanan JA, Hutchison I, Leigh IM, Bull RH. Systemic lupus erythematosus presenting with oral mucosal lesions: easily missed? Br J Dermatol. 2001;144(6):1219–1223. doi: 10.1046/j.1365-2133.2001.04236.x. [DOI] [PubMed] [Google Scholar]
- 33.Nico MM, Lourenco SV. Hypertrophic (verrucous) cutaneous lupus erythematosus of the lip and oral cavity: a series of 4 cases. Acta Dermato-venereologica. 2013;93(1):108–109. doi: 10.2340/00015555-1433. [DOI] [PubMed] [Google Scholar]
- 34.Chi AC, Neville BW, Krayer JW, Gonsalves WC. Oral manifestations of systemic disease. Am Fam Physician. 2010;82(11):1381–1388. [PubMed] [Google Scholar]
- 35.Lourenco SV, de Carvalho FR, Boggio P, Sotto MN, Vilela MA, Rivitti EA, et al. Lupus erythematosus: clinical and histopathological study of oral manifestations and immunohistochemical profile of the inflammatory infiltrate. J Cutan Pathol. 2007;34(7):558–564. doi: 10.1111/j.1600-0560.2006.00652.x. [DOI] [PubMed] [Google Scholar]
- 36.Ambrose N, Morgan TA, Galloway J, Ionnoau Y, Beresford MW, Isenberg DA, et al. Differences in disease phenotype and severity in SLE across age groups. Lupus. 2016;25(14):1542–1550. doi: 10.1177/0961203316644333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Woo SB, Greenberg MS. Ulcerative, vesicular and bullous lesions. In: Glick M, editor. Burket’s oral medicine. 12th ed. Shelton, Connecticut: People's Medical Publishing House USA; 2015. p. 57–89.
- 38.Coulson IH, Marsden RA. Lupus erythematosus cheilitis. Clin Exp Dermatol. 1986;11(3):309–313. doi: 10.1111/j.1365-2230.1986.tb00466.x. [DOI] [PubMed] [Google Scholar]
- 39.Fujimoto W, Hamada T, Yamada J, Matsuura H, Iwatsuki K. Bullous systemic lupus erythematosus as an initial manifestation of SLE. J Dermatol. 2005;32(12):1021–1027. doi: 10.1111/j.1346-8138.2005.tb00894.x. [DOI] [PubMed] [Google Scholar]
- 40.Anyanwu CO, Ang CC, Werth VP. Oral mucosal involvement in bullous lupus. Arthritis Rheum. 2013;65(10):2622. doi: 10.1002/art.38051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lourenco DM, Gomes RC, Aikawa NE, Campos LM, Romiti R, Silva CA. Childhood-onset bullous systemic lupus erythematosus. Lupus. 2014;23(13):1422–1425. doi: 10.1177/0961203314544187. [DOI] [PubMed] [Google Scholar]
- 42.Kramer IR, Lucas RB, Pindborg JJ, Sobin LH. Definition of leukoplakia and related lesions: an aid to studies on oral precancer. Oral surgery, oral medicine, and oral pathology. 1978;46(4):518–539. doi: 10.1016/0030-4220(78)90382-1. [DOI] [PubMed] [Google Scholar]
- 43.Jaworsky C. Lupus erythematosus. In: Lever WF, Elder DE, Ovid Technologies Inc., editors. Lever’s histopathology of the skin. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2009.
- 44.Schiodt M. Oral discoid lupus erythematosus. III. A histopathologic study of sixty-six patients. Oral Surg Oral Med Oral Pathol. 1984;57(3):281–293. doi: 10.1016/0030-4220(84)90184-1. [DOI] [PubMed] [Google Scholar]
- 45.Lourenco SV, Nacagami Sotto M, Constantino Vilela MA, Rodrigues Goncalves de Carvalho F, Rivitti EA, Menta Simonsen Nico M. Lupus erythematosus: clinical and histopathological study of oral manifestations and immunohistochemical profile of epithelial maturation. Journal of cutaneous pathology. 2006;33(10):657–62. doi:10.1111/j.1600-0560.2006.00518.x [DOI] [PubMed]
- 46.Schiodt M, Holmstrup P, Dabelsteen E, Ullman S. Deposits of immunoglobulins, complement, and fibrinogen in oral lupus erythematosus, lichen planus, and leukoplakia. Oral Surg Oral Med Oral Pathol. 1981;51(6):603–608. doi: 10.1016/S0030-4220(81)80010-2. [DOI] [PubMed] [Google Scholar]
- 47.Chan LS, Ahmed AR, Anhalt GJ, Bernauer W, Cooper KD, Elder MJ, et al. The first international consensus on mucous membrane pemphigoid: definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch Dermatol. 2002;138(3):370–379. doi: 10.1001/archderm.138.3.370. [DOI] [PubMed] [Google Scholar]
- 48.De Rossi SS, Ciarrocca K. Oral lichen planus and lichenoid mucositis. Dent Clin North Am. 2014;58(2):299–313. doi: 10.1016/j.cden.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 49.Eisen D, Carrozzo M, Bagan Sebastian JV, Thongprasom K. Number V Oral lichen planus: clinical features and management. Oral Dis. 2005;11(6):338–349. doi: 10.1111/j.1601-0825.2005.01142.x. [DOI] [PubMed] [Google Scholar]
- 50.Daoud MS, Pittelkow MR, et al. Lichen planus. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, et al., editors. Fitzpatrick’s dermatology in general medicine. 8. New York: McGraw Hill Medical; 2012. pp. 296–311. [Google Scholar]
- 51.Firth NA, Rich AM, Radden BG, Reade PC. Assessment of the value of immunofluorescence microscopy in the diagnosis of oral mucosal lichen planus. J Oral Pathol Med. 1990;19(7):295–297. doi: 10.1111/j.1600-0714.1990.tb00847.x. [DOI] [PubMed] [Google Scholar]
- 52.Kulthanan K, Jiamton S, Varothai S, Pinkaew S, Sutthipinittharm P. Direct immunofluorescence study in patients with lichen planus. Int J Dermatol. 2007;46(12):1237–1241. doi: 10.1111/j.1365-4632.2007.03396.x. [DOI] [PubMed] [Google Scholar]
- 53.Khudhur AS, Di Zenzo G, Carrozzo M. Oral lichenoid tissue reactions: diagnosis and classification. Expert Rev Mol Diagn. 2014;14(2):169–184. doi: 10.1586/14737159.2014.888953. [DOI] [PubMed] [Google Scholar]
- 54.Duncan KO, Geisse JK, Leffell DJ. Epitherial precancerous lesions. In: Goldsmith LA, Fitzpatrick TB, editors. Fitzpatrick’s dermatology in general medicine. 8. New York: McGraw-Hill Medical; 2012. pp. 1261–1282. [Google Scholar]
- 55.Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36(10):575–580. doi: 10.1111/j.1600-0714.2007.00582.x. [DOI] [PubMed] [Google Scholar]
- 56.Schiodt M, Andersen L, Shear M, Smith CJ. Leukoplakia-like lesions developing in patients with oral discoid lupus erythematosus. Acta Odontol Scand. 1981;39(4):209–216. doi: 10.3109/00016358109162282. [DOI] [PubMed] [Google Scholar]
- 57.Usatine RP, Tinitigan R. Nongenital herpes simplex virus. Am Fam Physician. 2010;82(9):1075–1082. [PubMed] [Google Scholar]
- 58.Schiodt M. Oral manifestations of lupus erythematosus. Int J Oral Surg. 1984;13(2):101–147. doi: 10.1016/S0300-9785(84)80079-4. [DOI] [PubMed] [Google Scholar]
- 59.Munoz-Corcuera M, Esparza-Gomez G, Gonzalez-Moles MA, Bascones-Martinez A. Oral ulcers: clinical aspects. A tool for dermatologists. Part I. Acute ulcers. Clin Exp Dermatol. 2009;34(3):289–294. doi: 10.1111/j.1365-2230.2009.03220.x. [DOI] [PubMed] [Google Scholar]
- 60.Wang X, Zhang L, Luo J, Wu Z, Mei Y, Wang Y, et al. Tacrolimus 0.03% ointment in labial discoid lupus erythematosus: a randomized, controlled clinical trial. J Clin Pharmacol. 2015;55(11):1221–1228. doi: 10.1002/jcph.537. [DOI] [PubMed] [Google Scholar]
- 61.Merola JF, Moschella SL. Overview of cutaneous lupus erythematosus. In: TW P, editor. UpToDate. UpToDate, Waltham, MA. (Accessed on September 20, 2015.).
- 62.Brennan MT, Valerin MA, Napenas JJ, Lockhart PB. Oral manifestations of patients with lupus erythematosus. Dental clinics of North America. 2005;49(1):127–41, ix. doi:10.1016/j.cden.2004.07.006. [DOI] [PubMed]
- 63.Lee LA. Cutaneous lupus in infancy and childhood. Lupus. 2010;19(9):1112–1117. doi: 10.1177/0961203310370347. [DOI] [PubMed] [Google Scholar]
- 64.Thorbinson C, Oni L, Smith E, Midgley A, Beresford MW. Pharmacological management of childhood-onset systemic lupus erythematosus. Paediatr Drugs. 2016;18(3):181–195. doi: 10.1007/s40272-016-0170-8. [DOI] [PubMed] [Google Scholar]