Abstract
Background:
Because of medical advances, metastatic breast cancer (MBC) is now viewed as a chronic disease, rather than an imminent death sentence. Helping women live with this disease requires more than a medical approach to symptoms. Thus, a mentor-based and supportive-expressive program ‘Be Resilient to Breast Cancer’ (BRBC) was designed to help Chinese women with MBC enhance their resilience levels, biopsychosocial functions, and potentially extend their life span.
Methods:
A total of 226 women with MBC were randomly assigned, in a 1 : 1 ratio, to an intervention group (IG) that participated in BRBC or to a control group (CG) that received no intervention. Be Resilient to Breast Cancer was conducted for 120 min once a week. Primary outcomes were cancer-specific survival and secondary outcomes were resilience, Allostatic Load Index (ALI), anxiety, depression, and quality of life (QoL). The Cox proportional-hazards model was used for survival analysis and growth mixture models were performed for secondary outcomes.
Results:
Be Resilient to Breast Cancer did not significantly prolong 3- or 5-year survival (median survival, 36.7 months in IG and 31.5 months in CG). The hazard ratio for death was 0.736 (95% CI, 0.525–1.133, P=0.076; univariate Cox model) and 0.837 (95% CI, 0.578–1.211, P=0.345; multivariate Cox analysis). The IG improved in anxiety (ES=0.85, P<0.001), depression (ES=0.95, P<0.001), QoL (ES=0.55, P<0.001), resilience (ES=0.67, P<0.001), and ALI (ES=0.90, P<0.001) compared to CG.
Conclusions:
BRBC does not improve survival of women with MBC in this study, though longer follow up is warranted. It positively impacts resilience, QoL, ALI, and emotional distress.
Keywords: metastatic breast cancer, BRBC, multidiscipline, mentor-based, resilience, survival, group therapy, psychosocial support
Breast cancer is the most prevalent cancer in women and annually accounts for 10% of new malignancies worldwide (Ferlay et al, 2004). In mainland China, ∼169 000 females are diagnosed with breast cancer every year and constitute 12.2% of the breast cancer incidents worldwide (Fan et al, 2014). Additionally, 30% of early breast cancer turns metastatic, which is often incurable (Redig and McAllister, 2013). Different from women with early breast cancer, women with metastatic breast cancer (MBC) must receive lifelong treatment, experience higher levels of emotional/physical distress, and feel frequent uncertainty about their health/possible death (Vilhauer, 2008; Thorne et al, 2013). They are also challenged to manage distressing adverse effects induced by medical treatments and experience heavy self-care demands (Stanton et al, 2005; Stanton, 2006). Thus, specific interventions to help women with metastatic breast cancer to recover from this traumatic event have been designed, and one of these is supportive-expressive group therapy (SEGT).SEGT has been found to achieve improvement in anxiety, depression, quality of life (QoL), family functioning, and satisfaction with treatment (Goodwin et al, 2001; Spiegel, 2002; Kissane et al, 2004). However, the effect of SEGT on survival is inconsistent. Initial studies examining SEGT have reported a mean survival advantage of 18 months by Spiegel et al (1989), however, these findings could not later be fully replicated in researches of Edelman et al (1999), Kissane and Li, 2008, Goodwin et al (2001), and Spiegel et al (2007). Yet, no study has reported a survival disadvantage for those given SEGT (Edwards et al, 2013). In addition, we found no published articles on the application of SEGT among women with MBC in Mainland China. Owing to this dearth of previous research, it is unclear whether this therapy would exhibit positive effects within Chinese culture. Thus, we developed a ‘Be Resilient to Breast Cancer’ (BRBC) program that is culturally tailored for Chinese females with MBC. This program was adapted from SEGT and is designed to increase resilience (defined as the capacity to bounce back after encountering a traumatic event; Connor and Davidson, 2003; Haglund et al, 2007) and QoL, decrease emotional and physical distress (allostatic load), and eventually prolong longevity. In a multicenter randomised control trial of BRBC, based in Guangzhou, China, we examined 3- and 5-year cancer-specific survival as the primary outcome. The secondary outcomes were anxiety, depression, QoL, resilience, and Allostatic Load Index (ALI, a composite index measured by 14 indicators from different physiological systems),. We hypothesised that BRBC would (a) prolong 3- and 5-year survival, (b) decrease emotional distress (anxiety, depression, pain and so on) and physical distress (allostatic load), and (c) increase the resilience and QoL.
Materials and methods
Study protocol
Trial was conducted at First Affiliated Hospital of Guangzhou University of Chinese Medicine, Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Sun Yat-sen University Cancer Center, and Affiliated Tumor Hospital of Guangzhou Medical University. Patients recruited from these hospitals all provided informed consent, and the study was approved by the ethics committees of all participating centers.
Patients were recruited between 2006 and 2011. Inclusion criteria were (1) women with confirmed MBC (2) metastases outside of the breast and ipsilateral axilla, and (3) fluent in oral Mandarin or Cantonese. Participants were excluded if they exhibited (1) central nervous system metastases, (2) a history of repeated suicidal behavior, (3) active psychosis or severe character disorder, (4) a life expectancy of <3 months (as assessed by primary oncologist), and/or (5) declined to participate in the program. Potentially eligible women were scheduled for an in-office visit to complete consent forms and baseline biopsychosocial assessment (T1), and then were randomised by computer program to IG or CG.
The BRBC program consists of education and group discussion, and lasted for 12 months. To better adapt to Chinese culture, we added education hosted by professional staff (e.g., clinical psychologists, dietician, Chinese medicine practitioner and so on) in an effort to foster self-efficacy to combat symptoms (such as pain, fatigue, intrusive thoughts and so on) through knowledge and techniques (such as breath control, meditation and so on), and to help patients gain a sense of control in their life. Second, trained mentors, who were breast cancer survivors themselves, were added to the group discussion to create non-hierarchical, reciprocal relationships through the sharing of experiences with those facing similar challenges (Wong-Kim et al, 2005; Kim et al, 2008). Women in IG attended weekly sessions lasting for 120 min. Education took ∼45 min and covered a variety of topics related to breast cancer (e.g., radio-chemo treatment, depression, traditional Chinese medicine, Taichi, sexual issues, and so on (please see reference for further elaboration; Ye et al, 2016). An outline covering all topics at each session was prepared by researchers as a template, to insure similar materials presented across centers. The group discussion followed the presentation and began with mentors sharing their experience with the topic (e.g., managing chemotherapy induced nausea), followed by participant discussions regarding life changes since diagnosis (e.g., physical, emotional, social, spiritual). Each group consisted of 7–9 patients and 3 leaders (2 mentors and 1 facilitator, including a clinical psychologist, nurse clinician, or social worker). The time of group discussion varied from 45–75 min. All leaders received a 4-day workshop before intervention, including Attention and Interpretation Therapy (AIT), which was designed to teach leaders to pay greater attention to positive things and helped cultivate skills (e.g., forgiveness, acceptance and so on). Leaders from different centers met monthly and discussed therapeutic principles in order to provide consistent intervention delivery. Participants were encouraged to attend as many of the sessions as possible and were considered as dropouts if they missed more than three consecutive sessions. Then, the project nurse would contact the patients, determine the reason for leaving, and encourage them to come back again.
Control group(CG) participants did not receive BRBC. However, a CD containing relaxation therapy (developed by the authors) was provided to every CG participant and monthly telephone follow-up was performed to prevent demoralisation from random assignment.
Randomisation
Stratified by centers, sealed envelopes with random numbers were applied to randomise participants. The sample size was set at 102 per group based on an expected five-year survival of 25% (CG) and 35% (IG). Ratio of assignment was IG:CG=1 : 1, assuming a two-tailed level of 0.05 and 80% power. These also predicted points of an effect size (ES) of 0.80 or greater. Additionally, 7–9 women were randomised to specific centers simultaneously at the beginning of the trial, in order to form an initial group at every center, with newly recruited patients randomised individually.
Masking
Blinding was not designed in the parts of Randomisation. Data were collected by research assistants who were not involved in the design of trial and had no knowledge of participants treatment protocol.
Outcomes
Primary outcome was 3- and 5-year cancer-specific survival. Secondary outcomes were anxiety, depression, QoL, resilience and ALI. Survival data were collected every 1–2 months till the end of the study. Secondary outcomes were only collected at baseline (T1), 2 months (T2), 6 months (T3), and 12 months (T4, after intervention).
Anxiety and depression were measured by the Chinese version of Hospital Anxiety and Depression Scale (HADS; Leung et al, 1993), which contains 7 items for anxiety and 7 items for depression, respectively, scored on a 5-point scale. Higher scores indicate higher levels of anxiety and depression.
QoL was measured by QLQ-C30 core questionnaire of the European Organization for Research and Treatment of Cancer (EORTC; Sprangers et al, 1993), which contains 30 items pertaining to different patient QoL aspects.
Resilience was measured by the 10 item Conner-Davison Resilience Scale (CD-RISC-10; Campbell-Sills and Stein, 2007), which is a self-administered questionnaire based on a 5-point scale, with higher scores reflecting more resilience.
ALI was a composite index measured by 14 indicators from different physiological systems, including body mass index (BMI), waist-hip ratio (WHR), resting pulse (RP), the standard deviation of R-R intervals (SDRR, heartbeat to heartbeat), resting systolic and diastolic blood pressure (SBP and DBP, respectively), white blood cell count (WBC), red blood cell count (RBC), hemoglobin, serotonin, hormone cortisol (HC), C-reactive protein (CRP), interleukin-6 (IL-6) and Cluster of Differentiation 4/Cluster of Differentiation 8(CD4+/CD8+). These indicators were selected to evaluate the functions of sympathetic nervous system (SNS), parasympathetic nervous system (PNS), hypothalamic pituitary adrenal (HPA), cardiovascular, inflammation, and immunisation. If a physical indicator was diagnosed as abnormal (i.e., RP of 107; normal range 60–100), patient would receive 1 point. Higher point totals indicated higher allostatic load. ALI range was from 0 (extremely low) to 14 (extremely high). These approaches to conceptualise physical allostatic load have been applied in previous studies (Seeman et al; 2001; Karlamangla et al, 2006; Seeman et al, 2010). All these data were collected when the patients came back to the hospital for a regular check. BMI, WHR, RP, SBP, and DBP were evaluated by their primary oncologist and SDRR was analysed by a cardiologist. The blood was drawn by the project nurse and biomakers were analysed in the clinical laboratory of the participating hospitals.
Data analysis
Baseline characteristics were examined by Pearson’s χ2-test. Multivariate Cox proportional-hazards models were conducted to assess effects of BRBC on 3- and 5-year cancer-specific survival. Significant influencing factors were enrolled into the Cox model in order to reduce potential impact on the estimations of intervention effect. The main effects of the intervention between the two groups were compared by the ES and two-sample t test. Intent-to-treat analysis was performed at T2, T3, and T4. In addition, a Growth Mixture Model (GMM) was applied to determine the number of potential types of patients existing within groups over the 12-month period (Nylund et al, 2007). We hypothesised that more patients in IG would exhibit ‘resilient’ trajectories of psychosocial and physical outcomes (bounce back to normal in a short time) compared to CG. The bootstrapped likelihood ratio test (BLRT) and Bayesian information criteria (BIC) of the GMM were compared to determine the potential classes within the groups (Muthén et al, 2002). This approach was only applied to the indicators of anxiety, depression, QoL, and ALI, with resilience added as covariant. Missing data except for survival data and demographics was imputed by multiple imputation chained equations (MICE; White et al, 2011). The imputation model included demographics, psychosocial outcomes and survival status (White and Royston, 2009). The statistical significance was set at P=0.05 for all analyses. The software used were the SPSS version 17, STATA version 11, and MPLUS version 7.
Results
Intervention and follow-up
Of 226 women who were enrolled into the study, 113 were randomly assigned to each group. However, 5 in IG and 9 in CG dropped out prior to intervention commencement. Main reason given for drop-outs was relocation. BRBC session attendance averaged 71.1% (28.4 of 40 possible per person-sessions) and showed no significant difference across centers. Primary reasons for nonattendance given were re-hospitalisation for medical treatment (24.3%), relocation (19.1%), busy (13.6%), and poor condition (17.4%). In addition, 9 of 108 women (8.3%) in IG and 13 of 104 women (12.5%) in CG reported attending support groups outside of the trial (P=0.3201). A total of 90.7% and 80.8% in the IG completed at least one follow-up for psychosocial scales and medical examination, respectively. The rate of completion in IG and CG was 72.1% and 62.5%, respectively. Rate did not differ significantly between groups (P=0.4288 for psychosocial scales; P=0.0853 for medical examination).
Sample characteristics
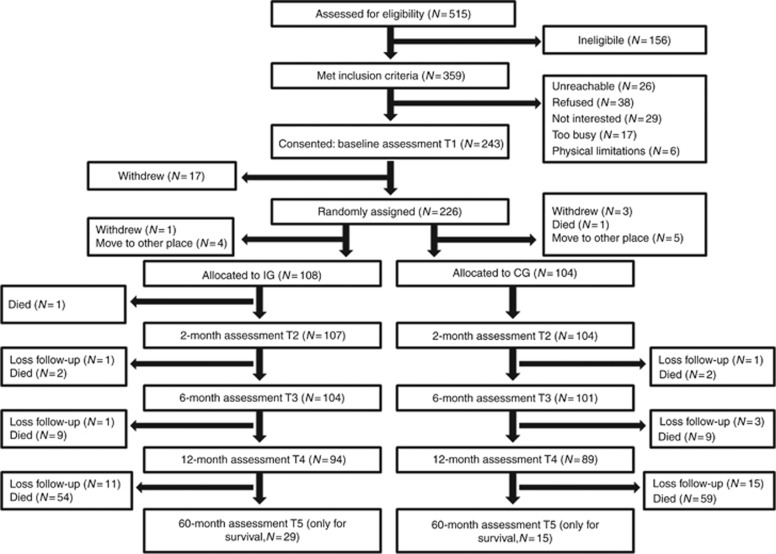
During the 5-year follow-up, 13 participants (12.0%) dropped from IG and 19 (18.3%) from CG (Figure 1). No significant demographic differences between groups were observed, except for income (P=0.0254). Individuals lacking follow-ups were more likely to be minorities (P<0.001 in IG, P=0.0440 in CG) and have a religious affiliation (P=0.0360 in IG, P<0.001 in CG). Other characteristics between follow-ups and non-follow-ups could be found in Table 1.
Figure 1.
Be Resilient to Breast Cancer trial accrual and retention.
Table 1. Demographics and clinical variables of the participants.
| Variable No. (%) | The intervention group (IG, n=95) | Loss of follow up (n=13) | P-value | The control group (CG, n=85) | Loss of follow up (n=19) | P-value | P-value (IG vs CG) |
|---|---|---|---|---|---|---|---|
| Age | 0.0642 | 0.8675 | 0.4451 | ||||
| ⩽40 | 26 (27.4) | 2 (15.4) | 24 (28.2) | 5 (26.4) | |||
| >40 and ⩽60 | 47 (49.5) | 4 (30.8) | 35 (41.2) | 7 (36.8) | |||
| >60 | 22 (23.1) | 7 (53.8) | 26 (30.6) | 7 (36.8) | |||
| Race | <0.001 | 0.0440 | 0.2831 | ||||
| Han | 90 (94.7) | 7 (53.8) | 77 (90.6) | 14 (73.7) | |||
| Other | 5 (5.3) | 6 (46.2) | 8 (9.4) | 5 (26.3) | |||
| Education | 0.7481 | 0.5644 | 0.3185 | ||||
| High school or lower | 54 (56.8) | 8 (61.5) | 42 (49.4) | 8 (42.1) | |||
| Undergraduate or higher | 41 (43.2) | 5 (38.5) | 43 (50.6) | 11 (57.9) | |||
| Income (monthly) | 0.3828 | 0.5364 | 0.0254 | ||||
| ⩽¥5000 | 37 (38.9) | 7 (53.8) | 34 (40.0) | 8 (42.1) | |||
| >¥5000 and ⩽¥10 000 | 41 (43.2) | 3 (23.1) | 23 (27.1) | 7 (36.8) | |||
| >¥10 000 | 17 (17.9) | 3 (23.1) | 28 (32.9) | 4 (21.1) | |||
| Relationship | <0.001 | 0.1331 | 0.3200 | ||||
| Single | 6 (6.3) | 4 (30.8) | 9 (10.6) | 2 (10.5) | |||
| Married | 81 (85.3) | 4 (30.8) | 65 (76.5) | 11 (57.9) | |||
| Divorced or widowed | 8 (8.4) | 5 (38.4) | 11 (12.9) | 6 (31.6) | |||
| Religious affiliation | 0.0360 | <0.001 | 0.1335 | ||||
| Yes | 19 (20.0) | 6 (46.2) | 10 (11.8) | 11 (57.9) | |||
| No | 76 (80.0) | 7 (53.8) | 75 (88.2) | 8 (42.1) | |||
| Employment | 0.1212 | 0.0528 | 0.1789 | ||||
| Part/full time | 37 (38.9) | 8 (61.5) | 25 (29.4) | 10 (52.6) | |||
| Unemployed | 58 (61.1) | 5 (38.5) | 60 (70.6) | 9 (47.4) | |||
| Menopausal status | 0.4873 | 0.4478 | 0.1030 | ||||
| Premenopausal or perimenopausal | 74 (77.9) | 9 (69.2) | 57 (67.1) | 11 (57.9) | |||
| Postmenopausal | 21 (22.1) | 4 (30.8) | 28 (32.9) | 8 (42.1) | |||
| Type of surgery | 0.3617 | 0.0467 | 0.3843 | ||||
| Mastectomy | 54 (56.8) | 5 (38.5) | 42 (49.4) | 7 (36.8) | |||
| Lumpectomy | 32 (33.7) | 7 (53.8) | 37 (43.5) | 7 (36.8) | |||
| Other | 9 (9.5) | 1 (7.7) | 6 (7.1) | 5 (26.4) | |||
| Chemotherapy | 0.4285 | 0.4698 | 0.7540 | ||||
| Ever | 59 (62.1) | 5 (38.5) | 47 (49.5) | 8 (42.1) | |||
| Current | 67 (70.5) | 9 (69.2) | 58 (68.2) | 14 (73.7) | |||
| Hormone therapy | 0.9160 | 0.7539 | 0.7542 | ||||
| Ever | 56 (58.9) | 5 (38.5) | 54 (63.5) | 12 (63.2) | |||
| Current | 31 (32.6) | 3 (23.1) | 27 (31.8) | 5 (26.3) | |||
| Radiation therapy | 0.7484 | 0.3421 | 0.7737 | ||||
| Ever | 40 (42.1) | 5 (38.5) | 44 (51.8) | 8 (42.1) | |||
| Current | 12 (12.6) | 2 (15.4) | 15 (17.6) | 5 (26.3) | |||
| Oestrogen-receptor status | 0.2280 | 0.1208 | 0.3933 | ||||
| Positive or equivocal | 53 (55.8) | 4 (30.8) | 53 (62.4) | 7 (36.8) | |||
| Negative | 31 (32.6) | 7 (53.8) | 20 (23.5) | 8 (42.1) | |||
| Unknown | 11 (11.6) | 2 (15.4) | 12 (14.1) | 4 (21.1) | |||
| Sites of metastases | 0.0133 | 0.7913 | 0.4736 | ||||
| Any visceral | 32 (33.7) | 9 (69.2) | 33 (38.8) | 8 (42.1) | |||
| Nonvisceral only | 63 (66.3) | 4 (30.8) | 52 (61.2) | 11 (57.9) | |||
| ECOG performance status | 0.0098 | 0.0950 | 0.8105 | ||||
| 0 | 35 (36.8) | 3 (23.1) | 35 (41.2) | 8 (42.1) | |||
| 1 | 48 (50.5) | 4 (30.7) | 39 (45.9) | 5 (26.3) | |||
| 2 | 12 (12.6) | 6 (46.2) | 11 (12.9) | 6 (31.6) | |||
| Estimated survival | 0.8378 | 0.1448 | 0.9867 | ||||
| 6–12 months | 23 (24.2) | 3 (23.0) | 21 (24.7) | 7 (36.8) | |||
| 12–24 moths | 43 (45.3) | 5 (38.5) | 39 (45.9) | 4 (21.1) | |||
| >24 months | 29 (30.5) | 5 (38.5) | 25 (29.4) | 8 (42.1) |
Cancer-specific survival
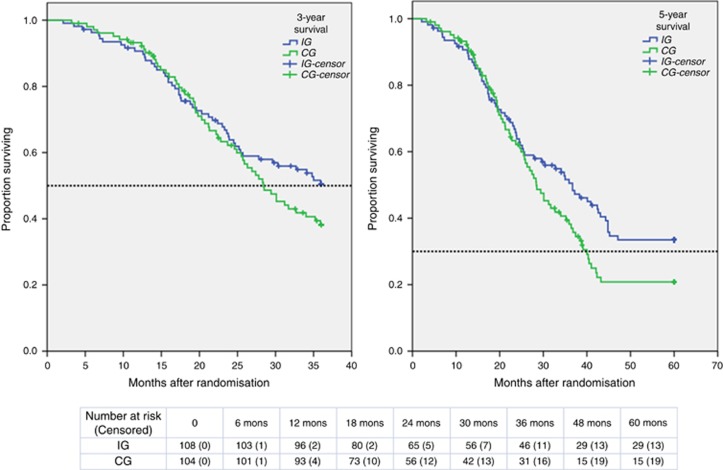
Median 5-year survival was 36.7 months (95% CI, 32.9–40.5) in IG and 31.5 months (95% CI, 28.8–35.9) in CG, according to Kaplan–Meier survival analysis (Figure 2). The Log Rank (Mantel-Cox) for 3-year survival (χ2=1.733, P=0.183) and 5-year survival (χ2=3.171, P=0.075) were not significant, and the hazard ratio (HR) for death in IG was 0.736 (95% CI, 0.525–1.133, P=0.076) compared with CG, based on univariate Cox model. Significant variables recognised by the Cox model were age (HR=1.406, 95% CI, 0.896–2.206, P=0.032), menopausal status (HR=0.648, 95% CI, 0.452–0.928, P=0.018), and oestrogen-receptor status (HR=1.474, 95% CI, 1.014–2.144, P=0.042). No significant effect of the BRBC program on 5-year survival (HR=0.837, 95% CI, 0.578–1.211, P=0.345) was identified after adjustment for significant risks in a multivariate Cox model.
Figure 2.
Kaplan–Meier Survival Curves for women in IG and CG. Black dotted line indicates a survival of 0.50 and 0.30 respectively.
Anxiety and depression
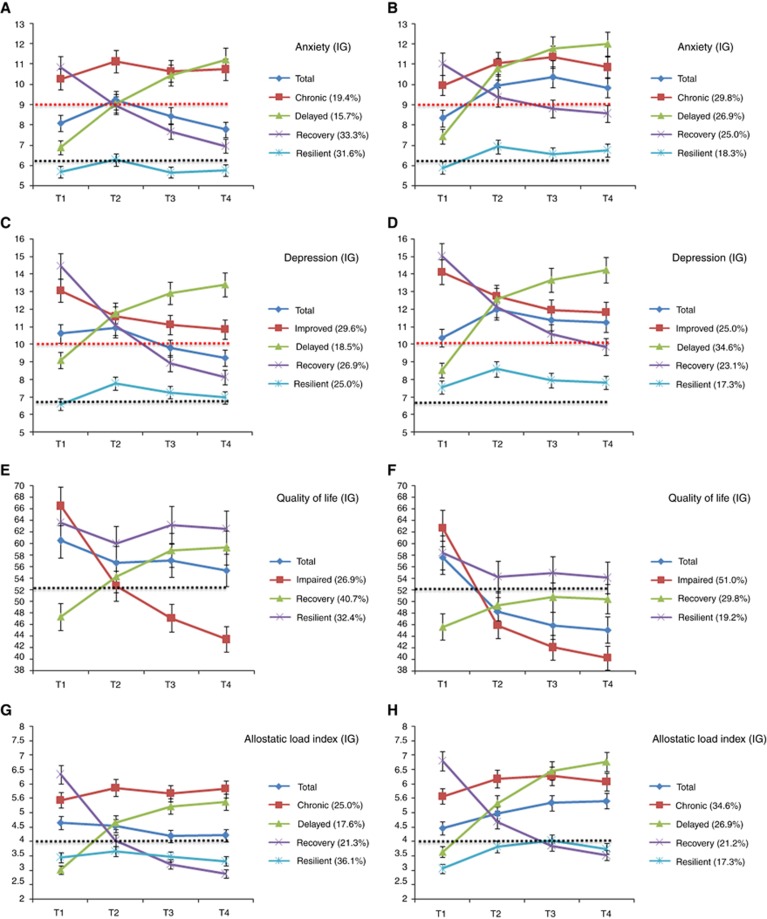
At baseline, no difference was detected in psychological measures between groups (P=0.6985 for anxiety, P=0.3810 for depression, Table 2). Two months from start of intervention (T2), IG showed a significant reduction in both anxiety (ES=0.39, P=0.0226) and depression (ES=0.58, P=0.0024). At T3, the level of anxiety (ES=0.82, P<0.0001) and depression (ES=0.87, P<0.0001) were further decreased in IG. At T4, the level of anxiety (ES=0.85, P<0.0001) and depression (ES=0.95, P<0.0001) were quiet stable compared with T3 (Table 3). GMM recognised 4 potential classes of anxiety trajectories (BICmin=1782.89 for IG and BICmin=1813.22 for CG) and depression trajectories (BICmin=1694.23 for IG and BICmin=1712.45 for CG) respectively. These four specific trajectories (Figure 3A–D) were named as ‘Chronic’(high and stable), ‘Delayed’(from normal to high), ‘Recovery’(from high to normal in a long time), and ‘Resilient’(from normal to high and back to normal in a short time). More participants exhibited ‘Resilient’ types in IG than in CG on anxiety instead of depression (RR=2.06, 95% CI 1.08–3.91, P=0.0264 for anxiety; RR=1.59, 95% CI 0.82–3.11, P=0.1709 for depression).
Table 2. Descriptive statistics of the major variables at baseline (T1).
|
IG (N=108) |
CG (N=104) |
|||||
|---|---|---|---|---|---|---|
| Variable | Possible range | Mean | s.d. | Mean | s.d. | P-value |
| AN | 0–21 | 8.09 | 2.78 | 7.94 | 2.85 | 0.6985 |
| DE | 0–21 | 10.32 | 2.96 | 9.96 | 3.01 | 0.3810 |
| QOL | 0–100 | 60.49 | 19.61 | 57.63 | 18.34 | 0.2744 |
| PF | 0–100 | 67.57 | 22.69 | 70.53 | 25.68 | 0.3744 |
| EF | 0–100 | 45.68 | 12.72 | 48.67 | 15.28 | 0.1225 |
| RF | 0–100 | 40.32 | 12.21 | 42.84 | 13.67 | 0.1580 |
| CF | 0–100 | 49.64 | 13.78 | 47.63 | 16.39 | 0.3342 |
| SF | 0–100 | 42.13 | 14.45 | 44.59 | 12.23 | 0.1831 |
| PA | 0–100 | 62.48 | 17.81 | 65.24 | 18.25 | 0.2664 |
| FA | 0–100 | 46.59 | 15.37 | 48.66 | 17.52 | 0.3610 |
| NV | 0–100 | 34.65 | 9.64 | 31.37 | 9.16 | 0.0119 |
| IN | 0–100 | 76.84 | 24.69 | 73.28 | 26.69 | 0.3143 |
| AL | 0–100 | 68.64 | 20.06 | 69.63 | 17.84 | 0.7049 |
| RE | 0–40 | 17.56 | 6.08 | 17.29 | 5.84 | 0.7421 |
| ALI | 0–12 | 4.75 | 1.43 | 4.47 | 1.61 | 0.1817 |
Abbreviations: AL=appetite loss; ALI=Allostatic Load Index; AN=anxiety; CF=cognitive function; DE=depression; EF=emotional function; FA=fatigue; IN=insomnia; NV=nausea and vomit; PA=pain; PF=physical function; QOL=quality of life; RE=resilience; RF=role function; SF=social function.
Table 3. Estimates of changes from baseline (T1) in major variables and their effect size among IG and CG at T2, T3, and T4.
|
2-month change |
6-month change |
12-month change |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | IG (N=107) | CG (N=104) | ES | P | IG (N=105) | CG (N=102) | ES | P | IG (N=96) | CG (N=93) | ES | P |
| AN | 1.12 | 2.30 | 0.39 | 0.0226 | 0.35 | 2.92 | 0.82 | <0.0001 | −0.33 | 2.21 | 0.85 | <0.0001 |
| DE | 0.63 | 2.62 | 0.58 | 0.0024 | −0.74 | 2.20 | 0.87 | <0.0001 | −1.40 | 1.58 | 0.95 | <0.0001 |
| QOL | −2.83 | −9.35 | −0.35 | 0.0005 | −1.88 | −12.26 | −0.58 | <0.0001 | −5.13 | −15.02 | −0.55 | <0.0001 |
| PF | 0.55 | −9.85 | −0.45 | 0.0173 | −2.33 | −13.64 | −0.52 | 0.0024 | −5.21 | −15.87 | −0.47 | 0.0154 |
| EF | 6.63 | −6.16 | −0.82 | 0.0001 | 5.56 | −8.41 | −0.91 | <0.0001 | 7.54 | −5.30 | −0.92 | <0.0001 |
| RF | 2.94 | −6.20 | −0.69 | 0.0008 | 4.95 | −7.28 | −0.94 | <0.0001 | 5.26 | −7.16 | −0.94 | <0.0001 |
| CF | 3.25 | −3.49 | −0.41 | 0.0008 | 4.88 | −7.38 | −0.82 | <0.0001 | 3.38 | −6.11 | −0.63 | <0.0001 |
| SF | 5.74 | −2.03 | −0.53 | 0.0226 | 10.03 | −2.38 | −0.82 | 0.0001 | 12.15 | −0.21 | −0.91 | <0.0001 |
| PA | −2.24 | 5.21 | 0.37 | 0.0018 | −3.87 | 7.34 | 0.54 | <0.0001 | −2.21 | 8.97 | 0.56 | 0.0001 |
| FA | −2.39 | 3.48 | 0.36 | 0.0004 | −0.95 | 9.02 | 0.60 | <0.0001 | 1.64 | 9.68 | 0.47 | 0.0004 |
| NV | 6.67 | 13.89 | 0.65 | 0.0295 | 7.40 | 16.37 | 0.79 | 0.0032 | 5.63 | 15.02 | 0.92 | 0.0006 |
| IN | −8.00 | 1.96 | 0.41 | 0.0555 | −11.59 | 4.21 | 0.60 | 0.0025 | −12.97 | 2.93 | 0.62 | 0.0026 |
| AL | −3.28 | 2.92 | 0.29 | 0.0311 | −5.07 | 5.80 | 0.53 | 0.0002 | −4.13 | 6.95 | 0.57 | 0.0002 |
| RE | 1.56 | −0.45 | −0.31 | 0.0226 | 3.95 | −0.27 | −0.68 | <0.0001 | 4.68 | 0.38 | −0.67 | <0.0001 |
| ALI | −0.22 | 0.49 | 0.45 | 0.1345 | −0.46 | 0.67 | 0.75 | 0.0009 | −0.64 | 0.78 | 0.90 | <0.0001 |
Abbreviations: AL=appetite loss; ALI=Allostatic Load Index; AN=anxiety; CF=cognitive function; DE=depression; EF=emotional function; ES=effect size; FA=fatigue; IN=insomnia; NV=nausea and vomit; PA=pain; PF=physical function; QOL=quality of life; RE=resilience; RF=role function; SF=social function.
Notes: a positive (negative) sign for the ES implies that the T2, T3, or T4 adjusted mean for Major Variables was lower (higher) for IG than CG.
Figure 3.
Growth Mixture Model (GMM) for secondary outcomes between IG and CG. (A–D) Black dotted line indicates a sample of women without breast cancer from our previous study (Ye et al, 2016). Red dotted line indicates a sample with high risk for anxiety and depression symptoms. (E–H) Black dotted line indicates a sample of women with non-metastatic breast cancer from our previous study (Ye et al, 2016).
QoL and resilience
QoL and resilience levels between groups did not differ significantly at baseline, except for dimension of nausea and vomiting (P=0.0119, Table 2). At T2, resilience level in IG increased (ES=0.31, P=0.0226). QoL (ES=0.35, P=0.0005) and its different dimensions (ES varied from 0.41–0.82, P<0.05) in IG had also been improved, or less impaired compared with CG. In addition, some symptoms, (e.g., pain and fatigue) were reduced (ES varied from 0.29–0.65, P<0.05).At T3, the difference of QoL (ES=−0.58, P<0.0001), symptoms (ES varied from 0.53–0.79, P<0.005), and resilience level (ES=−0.68, P<0.0001) between groups were significant compared with T2. At T4, QoL (ES=−0.55, P<0.0001) and resilience (ES=−0.67, P<0.0001) in IG were stable compared to T3. GMM recognised 3 potential classes of QoL trajectories (BICmin=1853.64 for IG and BICmin=1926.74 for CG). These three specific trajectories (Figure 3E and F) were named as ‘Impaired’(from high to low), ‘Recovery’(from low to normal in long time), and ‘Resilient’ (from normal to low and back to normal in a short time) among groups. More IG participants were determined in ‘Resilient’ than in CG (RR=2.01, 95% CI 1.07–3.79, P=0.0290).
ALI
At baseline, the two groups did not show any significant difference in ALI (P=0.1817, Table 2). At T2, ALI had been improved, though the ES was not significant (ES=0.45, P=0.1345). From T2 to T4, ALI was much more enhanced (ES from 0.75–0.90). GMM recognised 4 potential classes of ALI trajectories (BICmin=1686.88 for IG and BICmin=1602.54 for CG). These three specific trajectories (Figure 3G and H) were named as ‘Chronic’ (high and stable), ‘Delayed’ (from normal to high), ‘Recovery’(from high to normal in long time), and ‘Resilient’ (from normal to high and back to normal in a short time) among participants. There were more participants in IG determined in ‘Resilient’ than in CG (RR=2.70, 95% CI 1.42–5.13, P=0.0020).
Discussion
The BRBC program failed to replicate the survival advantage in Chinese women with MBC. These findings are consistent with those of Kissane and Li (2008) and Goodwin et al (2001). No significant difference in demographics were noted between groups, except for income, however, this influencing factor was not associated with the primary outcome. BRBC attendance was high (71.1%) and only nine women in IG lacked proper follow-ups (missed more than three consecutive sessions) through the first year. Therefore, poor group participation was not identified as a possible reason for missing an intervention effect. However, BRBC did alleviate emotional distress and enhance QoL, which were consistent with reports by Kissane et al (2004) and Spiegel et al (2002). The definition of resilience is debated (Bonanno, 2012) and many researchers regard resilience as a personality trait which is hard to change while we hold that resilience is an ability that can be nurtured and enhanced after learning and training. The GMM analysis confirmed the ability hypothesis that more participants in IG presumably in ‘Delayed’ or ‘Impaired’ followed ‘Resilient’ trajectory (the emotional distress and physical distress of ‘Delayed’ or ‘Impaired’ return to normal in a short time after a elevation), which we believe indicated the BRBC program was effective and did enhance resilience levels. What’s more, based on the result of reduced allostatic load in IG, the potential for psychosocial interventions to influence metastatic breast cancer survivals was also highlighted though the difference between IG and CG was not significant. However, these benefits may have been attributable to Taichi exercise (Ba Duan Jin) performed at the end of each group session. Participants in IG appreciated this light exercise and continued to engage in it post-treatment, which may have lowered neuroendocrine levels, mitigating inflammatory and metastatic processes, via stress response pathways (Lutgendorf et al, 2010).
In order to recruit more mentors into our program to benefit more patients (we would like to make BRBC into a one-to-one mentorship program in the future), we conducted focus group interviews for every mentee who completed the program through the year. These interviews were designed to learn about expectations, satisfaction, gains, needs, difficulties, and suggestions for improving the BRBC program. After the interview, mentees were asked whether they would like to be mentors in the BRBC program. A total of 94 mentees were invited, of which, 33 (35.1%) were willing to be recruited and 27 (28.7%) were willing to do so in the next 2 years. Several themes emerged in the focus group interviews that help explain why Chinese women valued the BRBC program. Most important was that the program reduced stigma and increased a sense of belonging among participants. Some women who were antagonistic and sealing themselves off at the beginning, eventually opened up and became the ‘big sister’ in the group. The second theme was a sense of empowerment, especially an increase in confidence and hope. The participants used the techniques and knowledge learned from the sessions to combat physical and emotional distress, which increased their confidence and self-efficacy.
Some limitations should be considered. First, we did not insure that the psychological benefits of BRBC identified were representative, because we were unable to determine whether the participants willing to be enrolled were more (or less) distressed than the non-participants, as the collection of psychological information of non-participants was unethical. Second, BRBC was culturally tailored for Chinese females in the mainland. Thus, we cannot insure that this program can be generalised to other female groups with different cultural backgrounds. Third, though BRBC is based on the supportive-expressive program, it has been quite different from the original one due to additional components such as mentorship and education. Thus, the benefits of BRBC may not only be attributable to the supportive-expressive component and more researches to isolate the intervention effect of different components are warranted. Finally, we found that the survival difference between IG and CG had been increased from 3- to 5-year, according to univariate Cox model (χ2=1.733, P=0.183 for 3-year survival; χ2=3.171, P=0.075 for 5-year survival). Therefore, a longer follow-up may be needed to recognise the long term effects of BRBC on the survival of women with MBC.
In conclusion, this article reported a very successful project named Be Resilient to Breast Cancer (BRBC) with a sample of females with MBC and provided some latest progress of SEGT in Mainland China. BRBC does not improve survival of women with MBC in this study, though longer follow up is warranted. It does positively impact resilience, QoL, ALI, and emotional distress.
Acknowledgments
This research was funded by grants from State Administration of Traditional Chinese Medicine (No: ZYZC20160901 and ZYZC20160902), Innovative Project of Guangzhou University of Chinese Medicine (No: 2016KYTD08), Department of Education of Guangdong Province (No: 2012JYKY and GDHL201412015), Guangdong Provincial Administration of Traditional Chinese Medicine (No: 20111183), and Science and Technology Department of Guangdong Province (No: 2011B080701081). We are grateful to the oncologists from different hospitals who referred their patients to the study. Also, we gratefully acknowledge the assistance of mentors who participated in the study to help the patients recover and the patients who provide valuable data and comments to help us improve the BRBC program. The contribution made by the hospitals and the university is also acknowledged.
Author contributions
The following authors or their immediate family members have indicated no financial interest. No conflict exists for drugs or devices used in a study if they are not being evaluated as part of the investigation. Research funding: ZJY; HZQ; MZL; MLL. Conception and design: ZJY; HZQ; MZL. Administrative support: ZJY; HZQ; MLL. Provision of study materials or patients: MZL; PFL; PC; ZS; YLY; SNW; ZZ; KLL; CFP; HH; GYH; YFZ; ZZ; QH; JJZ. Collection and assembly of data: MZL; PFL; PC; ZS; YLY; SNW; ZZ; KLL; CFP; HH; GYH; YFZ; ZZ; QH; JJZ. Data analysis and interpretation: ZJY; HZQ; MZL. Manuscript preparation: ZJY; HZQ; MZL; MLL. Manuscript writing: ZJY; MZL; HZQ; MLL. Final approval of manuscript: all authors.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
The authors declare no conflict of interest.
References
- Bonanno GA (2012) Uses and abuses of the resilience construct: Loss, trauma, and health-related adversities. Soc Sci Med 74: 753–756. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR (2003) Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 18: 76–82. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Stein MB (2007) Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress 20: 1019–1028. [DOI] [PubMed] [Google Scholar]
- Edelman S, Lemon J, Bell DR, Kidman AD (1999) Effects of group CBT on the survival time of patients with metastatic breast cancer. Psychooncology 8: 474–481. [DOI] [PubMed] [Google Scholar]
- Edwards AG, Hailey S, Maxwell M (2013) Psychological interventions for women with metastatic breast cancer. Cochrane Database Syst Rev 6: CD004253–CD004253. [DOI] [PubMed] [Google Scholar]
- Ferlay J, Bray F, Pisani P, Parkin DM (2004) Cancer Incidence, Mortality and Prevalence Worldwide. GLOBOCAN, IARC Cancer Base No. 5, version 2.0. IARC Press: Lyon, France. [Google Scholar]
- Fan L, Strasser-Weippl K, Li JJ St, Louis J, Finkelstein DM, Yu KD, Chen WQ, Shao ZM, Goss PE (2014) Breast cancer in china. Lancet Oncol 15: 279–289. [DOI] [PubMed] [Google Scholar]
- Goodwin PJ, Leszcz M, Ennis M, Koopmans J, Vincent L, Guther H, Drysdale E, Hundleby M, Chochinov HM, Navarro M, Speca M, Hunter J (2001) The effect of group psychosocial support on survival in metastatic breast cancer. N Engl J Med 345: 1719–1726. [DOI] [PubMed] [Google Scholar]
- Haglund ME, Nestadt PS, Cooper NS, Southwick SM, Charney DS (2007) Psychobiological mechanisms of resilience: relevance to prevention and treatment of stress-related psychopathology. Dev Psychopathol 19: 889–920. [DOI] [PubMed] [Google Scholar]
- Karlamangla AS, Singer BH, Seeman TE (2006) Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosom Med 68: 500–507. [DOI] [PubMed] [Google Scholar]
- Kissane DW, Love A, Hatton A, Bloch S, Smith G, Clarke DM, Miach P, Ikin J, Ranieri N, Snyder RD (2004) Effect of cognitive existential group therapy on survival in early-stage breast cancer. J Clin Oncol 22: 4255–4260. [DOI] [PubMed] [Google Scholar]
- Kim HS, Sherman DK, Taylor SE (2008) Culture and social support. Am Psychol 63: 518–526. [DOI] [PubMed] [Google Scholar]
- Kissane D, Li YL (2008) Effects of supportive-expressive group therapy on survival of patients with metastatic breast cancer: a randomised prospective trial. Cancer 112: 443–444. [DOI] [PubMed] [Google Scholar]
- Leung CM, Ho S, Kan CS (1993) Evaluation of the Chinese version of the Hospital Anxiety and Depression Scale. A cross-cultural perspective. Int J Psychosom 40: 29–34. [PubMed] [Google Scholar]
- Lutgendorf SK, Sood AK, Antoni MH (2010) Host factors and cancer progression: biobehavioral signaling pathways and interventions. J Clin Oncol 28: 4094–4099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Brown CH, Masyn K, Jo B, Khoo ST, Yang CC, Wang CP, Kellam SG, Carlin JB, Liao J (2002) General growth mixture modeling for randomised preventive interventions. Biostatistics 3: 459–475. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Model 14: 535–569. [Google Scholar]
- Redig AJ, McAllister SS (2013) Breast cancer as a systemic disease: a view of metastasis. J Intern Med 274: 113–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, McEwen BS, Rowe JW, Singer BH (2001) Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci USA 98: 4770–4775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel D (2002) Effects of psychotherapy on cancer survival. Nat Rev Cancer 2: 383–389. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Bloom JR, Kraemer HC, Gottheil E (1989) Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet 2: 888–891. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Butler LD, Giese-Davis J, Koopman C, Miller E, DiMiceli S, Classen CC, Fobair P, Carlson RW, Kraemer HC (2007) Effects of supportive-expressive group therapy on survival of patients with metastatic breast cancer: a randomised prospective trial. Cancer 110: 1130–1138. [DOI] [PubMed] [Google Scholar]
- Sprangers MA, Cull A, Bjordal K, Groenvold M, Aaronson NK (1993) The European Organization for Research and Treatment of Cancer. Approach to quality of life assessment: guidelines for developing questionnaire modules. EORTC Study Group on Quality of Life. Qual Life Res 2: 287–295. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Ganz PA, Kwan L, Meyerowitz BE, Bower JE, Krupnick JL, Rowland JH, Leedham B, Belin TR (2005) Outcomes from the moving beyond cancer psychoeducational, randomised, controlled trial with breast cancer patients. J Clin Oncol 23: 6009–6018. [DOI] [PubMed] [Google Scholar]
- Stanton AL (2006) Psychosocial concerns and interventions for cancer survivors. J Clin Oncol 24: 5132–5137. [DOI] [PubMed] [Google Scholar]
- Seeman T, Epel E, Gruenewald T, Karlamangla A, McEwen BS (2010) Socio-economic differentials in peripheral biology: cumulative allostatic load. Ann N Y Acad Sci 1186: 223–239. [DOI] [PubMed] [Google Scholar]
- Thorne SE, Oliffe JL, Oglov V, Gelmon K (2013) Communication challenges for chronic metastatic cancer in an era of novel therapeutics. Qual Health Res 23: 863–875. [DOI] [PubMed] [Google Scholar]
- Vilhauer RP (2008) A qualitative study of the experiences of women with metastatic breast cancer. Palliat Support Care 6: 249–258. [DOI] [PubMed] [Google Scholar]
- Wong-Kim E, Sun A, Merighi JR, Chow EA (2005) Understanding quality-of-life issues in Chinese women with breast cancer: A qualitative investigation. Cancer Control 12(Suppl): 6–12. [DOI] [PubMed] [Google Scholar]
- White IR, Royston P (2009) Imputing missing covariate values for the Cox model. Stat Med 28: 1982–1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White IR, Royston P, Wood AM (2011) Multiple imputation using chained equations: issues and guidance for practice. Stat Med 30: 377–399. [DOI] [PubMed] [Google Scholar]
- Ye ZJ, Liang MZ, Qiu HZ, Liu ML, Hu GY, Zhu YF, Zeng Z, Zhao JJ, Quan XM (2016) Effect of a multidiscipline mentor-based program, Be Resilient to Breast Cancer (BRBC), on female breast cancer survivors in mainland China—a randomised, controlled, theoretically-derived intervention trial. Breast Cancer Res Treat 158: 1–14. [DOI] [PubMed] [Google Scholar]