Abstract
Despite the importance of cardiorespiratory fitness, no practical method exists to estimate maximal oxygen consumption (VO2max) without a specific exercise protocol. We developed an estimation model of VO2max, using maximal activity energy expenditure (aEEmax) as a new feature to represent the level of physical activity. Electrocardiogram (ECG) and acceleration data were recorded for 4 days in 24 healthy young men, and reference VO2max levels were measured using the maximal exercise test. aEE was calculated using the measured acceleration data and body weight, while heart rate (HR) was extracted from the ECG signal. aEEmax was obtained using linear regression, with aEE and HR as input parameters. The VO2max was estimated from the aEEmax using multiple linear regression modeling in the training group (n = 16) and was verified in the test group (n = 8). High correlations between the estimated VO2max and the measured VO2max were identified in both groups, with a 15-hour recording being sufficient to produce a highly accurate VO2max estimate. Additional recording time did not significantly improve the accuracy of the estimation. Our VO2max estimation method provides a robust alternative to traditional approaches while only requiring minimal data acquisition time in daily life.
Keywords: Cardiorespiratory Fitness, Oxygen Consumption, Energy Expenditure, Maximal Activity Energy Expenditure
Graphical Abstract
INTRODUCTION
Typical physical activity monitoring systems use a multiple axis accelerometer, converting acceleration data to an activity count or calorie expenditure (1,2), with the reliability and feasibility of these accelerometer-based physical activity monitoring systems having been established (3). However, these conventional physical activity monitors only measure the quantity of movement and do not provide information on physical fitness, which is specifically related to the ability or capacity for physical activity. Therefore, the purpose of exercise should be to increase both physical activity and fitness (4) and, hence, monitoring physical fitness is as important as physical activity monitoring.
Cardiorespiratory fitness (CRF), which is one component of physical fitness, is the ability to take in oxygen and to provide this oxygen to the exercising muscles. The importance of CRF in health has been emphasized in previous studies. Blair et al. (5) and Lee et al. (6) have reported that CRF is related to mortality due to all causes, including death due to a cardiovascular event. Moreover, in previously published research, we reported lower CRF to be associated with higher prevalence of renal hyperfiltration, an early marker of chronic kidney disease (7). CRF is influenced not only by non-modifiable factors, such as genetic factors, age, and gender, but also by modifiable factors, including regular aerobic exercise (8,9). Blair et al. (5) indicated that CRF can be enhanced through exercise, lowering the overall risk of mortality from all causes. However, CRF has not received its deserved attention in health care and research (6). The absence of practical and reliable methods to measure CRF is likely to be a contributing factor to this.
The maximal oxygen consumption (VO2max) is a representative index of CRF, with several methods available to measure or estimate VO2max. Metabolic gas analysis during maximal exercise is the gold standard for measuring VO2max (10). However, maximal exercise testing is not safe for high-risk groups due to the high intensity exercise required (6), as well as because of the high level of motivation required to complete the test (11). In addition, these tests require expensive equipment and expertise in aerobic exercise testing. Moreover, repeated maximal exercise test for monitoring of VO2max after modification of life styles is not practical.
To overcome the limitations of maximal exercise testing, submaximal tests (11,12) have been developed. These are based on the linear relationship between oxygen consumption, exercise intensity, and physical responses, such as heart rate (HR). However, like maximal exercise testing, submaximal exercise tests are not suitable for repeated testing and require specific equipment and expertise. Moreover, outcomes of these tests can easily be affected by the familiarity of the exercise (11). Recently, estimation methods of VO2max without the use of a specific exercise protocol in daily life have been developed, using accelerometers with (13,14) or without (15,16) continuous HR monitoring. The non-protocol VO2max estimation methods are based on the relationship between physical activity, HR (response of body to physical activity), and VO2max. Individuals with a higher level of VO2max are assumed to be more active (15,16) and to have greater potential for being active, with a lower HR, compared to individuals with a lower VO2max (13,14). Although the developed methods are simple and safe for high-risk groups, prolonged measurement with an attached sensor for up to 7 days makes these methods impractical in daily life (14).
In this study, we developed an unobtrusive VO2max estimation model, using maximal activity energy expenditure (aEEmax) as a new feature, to indicate personal physical activity. aEEmax was calculated based on activity energy expenditure (aEE) and HR measured in daily life. Our model decreased the estimation time to reduce discomfort to individuals.
MATERIALS AND METHODS
Participants
Twenty-four healthy young Asian male volunteers participated in this study. All participants had sedentary occupations. All participants signed written informed consent. Participants also completed health evaluations, including medical history related to cardiovascular disease.
Measurement of VO2max
VO2max was measured using a respiration gas analyzer (Vmax Encore System; CareFusion,
San Diego, CA, USA) and an aerobic exercise test system (CASE v6.61; GE Healthcare, Little Chalfont, UK). The modified Bruce protocol was used to determine the VO2max reference value. Twelve-lead electrocardiogram (ECG), blood oxygen saturation (SpO2), and blood pressure were also measured.
First, baseline physiologic measures for all devices used were measured in a standing position after a 5-minute rest period. The modified Bruce protocol was subsequently performed, with the treadmill's velocity and slope increased at 3-minute intervals. The following criteria were used to define VO2max attainment: a respiratory exchange ratio reaching > 1.08; cessation of increase in VO2 with increasing work load; or self-reported volitional fatigue (17). The value of VO2max was expressed in mL/kg/min.
Experimental methods
Participants wore a Shimmer ECG sensor (18), for measurement of 2-lead ECG and tri-axial acceleration (Shimmer platform with ECG sensor module; Shimmer, Dublin, Ireland), for four consecutive days. The sensor was attached to the chest with an elastic chest belt. Participants removed the sensor during sleep or during showering, after which they re-attached the sensor after completing those activities using new ECG electrodes.
An ECG was obtained on the left side of the chest near the left nipple, using a hydrogel Ag/AgCl electrode (2223; 3M, Maplewood, MN, USA) with a 10-cm-sized, square-shaped placement. No adverse skin reactions, such as a rash, were identified. An electrode was not placed at conventional ECG lead positions as the sensor needed to be comfortably placed to avoid disrupting activities of daily living. The acceleration signal was also captured on the chest, with the sensitivity of the accelerometer set to 1.5 g. Ideally, accelerometers should be placed close to the center of body mass, but we placed the sensor on the chest to improve comfort during measurement (19). The X, Y, and Z axes corresponded to the longitudinal axis, the mediolateral axis and the posterior-anterior axis, respectively.
Data obtained from all signals were stored on a micro-SD card at a sampling frequency of 51.2-Hz, which is appropriate for the measurement of physical activity (1), but relatively lower than the standard ECG frequency (20). The sampling frequency was selected to reduce battery consumption without losing signal quality necessary to obtain the R-R intervals (18). The stored data were extracted two times, at 48-hour and 96-hour after initiating measurement.
Signal processing
Whole data sets were reviewed and, if the ECG was inaccurate due to electrode contact problem or sensor detachment, the ECG and the matching accelerometer data were also removed. The tri-axial acceleration was band-pass filtered (0.25 to 7 Hz, 2nd order Butterworth). Filtered acceleration was rectified and integrated over 1-minute sequences to obtain the acceleration count per minute (ACM). A non-linear model for aEE estimation (2) was defined using body mass, gender, and ACM within the following Equations 1 to 7:
| (Equation 1) |
| (Equation 2) |
| (Equation 3) |
| (Equation 4) |
| (Equation 5) |
, where sex = 1 in males and 2 in females
| (Equation 6) |
| (Equation 7) |
The ECG data were band-pass filtered (5 to 20Hz, 4th order Butterworth). The R-R interval was automatically detected from the ECG signal using the R-peak detection algorithm described by Pan and Tomkins (21). The R-R intervals were averaged for 1 minute and converted to an HR (beat per minute). Since previous research showed that the recovery HR after physical activity was heterogeneous (22) and not well correlated to VO2max (23), we used only increasing HR periods in our analysis.
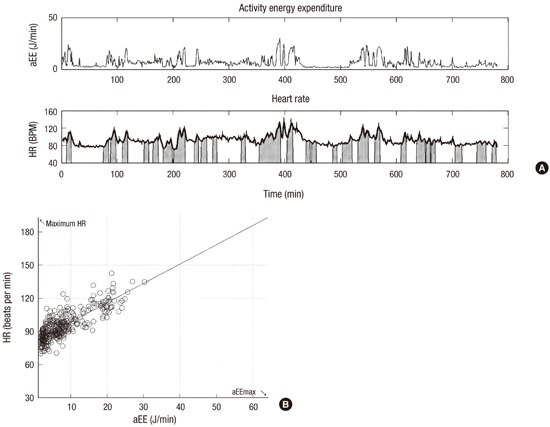
Fig. 1A shows the aEE (upper graph) and HR (lower graph) for a representative participant over time. The gray area under the HR curve indicates periods of increasing HR. As aEE increased, the associated HR increased. The scatter plot of HR and aEE, averaged over 1-minute intervals during periods of increasing HR are shown in Fig. 1B. A simple linear regression equation was developed to estimate aEEmax, using HR and aEE as inputs, with the maximal HR calculated as 220 − age.
Fig. 1.
Signal processing procedure. (A) aEE (in units of J/min), and HR (in units of beats per minute) for one participant. HR data is shown as a thick line and the increasing HR period (at least 4 minutes) is shown in the shadowed region under the smoothed HR curve. (B) Scatter plot of the aEE and HR of the same participant. A simple linear regression was performed to obtain aEEmax at a maximal HR (220 − age).
aEE = activity energy expenditure, HR = heart rate, aEEmax = maximal activity energy expenditure.
Following aEEmax calculation, participants were divided into two subgroups according to aEEmax. The aEEmax values were sorted in ascending order and every third participant was selected to form the test group (n = 8), with other participants forming the training group (n = 16). The aEEmax and anthropometric values were used to develop a multiple linear regression model to estimate the VO2max in the training group.
Statistical analysis
Pearson's correlation coefficient was calculated to evaluate the agreement between the aEEmax and the measured VO2max, as well as between the estimated VO2max and the measured VO2max in both groups. A two-sided P < 0.05 was regarded as significant. Regression equations were evaluated by coefficients of determination (adjusted R2), absolute standard error of the estimate (SEE), and relative SEE (%SEE). A Bland-Altman plot was plotted to determine the differences between measured and estimated VO2max. All signal processing, cross validation, and statistical analyses were performed using MATLAB (MATLAB2014a; Mathworks, Natick, MA, USA).
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of the National Medical Center (IRB. No. M-12111001-001). Informed consent was submitted by all subjects when they were enrolled. Participants also completed health evaluations, including medical history related to cardiovascular disease.
RESULTS
Characteristics of the training and test groups are summarized in Table 1. No between-group differences were evaluated using the Mann-Whitney U test.
Table 1. Characteristics of participants.
| Parameters | Training (n = 16) | Test (n = 8) | P |
|---|---|---|---|
| Age, yr | 27.5 ± 6.6 | 25.1 ± 3.7 | 0.413 |
| Height, cm | 172.6 ± 6.8 | 174.8 ± 6.2 | 0.724 |
| Weight, kg | 70.1 ± 11.2 | 75.0 ± 9.6 | 0.269 |
| The duration of Bruce protocol exercise, sec | 842 ± 89 | 796 ± 107 | 0.272 |
| Measured VO2max, mL/kg/min | 48.5 ± 5.3 | 46.8 ± 4.5 | 0.284 |
| The duration of the measurement using sensor, min | 2,935 ± 767 | 3,319 ± 426 | 0.178 |
All values are mean ± standard deviation. P values were calculated using the Mann-Whitney U test.
VO2max = maximal oxygen consumption.
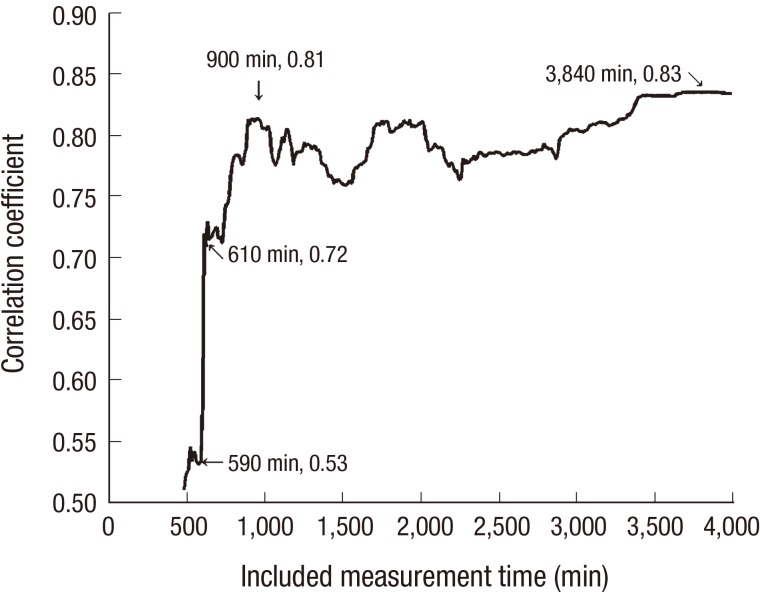
The change in the correlation coefficient between aEEmax and measured VO2max with respect to time is shown in Fig. 2. A significant correlation between aEEmax and the measured VO2max (R = 0.81, P < 0.001) with only 15-hour of recording during daily life. As the correlation coefficient showed little increase with longer duration of measurement, we only used 15-hour of ECG and acceleration data to estimate VO2max.
Fig. 2.
Change of correlation coefficient between aEEmax and measured VO2max. The correlation coefficient was 0.81 at 900 minutes of HR and aEE data analysis to calculate aEEmax. The correlation coefficient fluctuated but did not drastically increase when longer periods were used.
aEEmax = maximal activity energy expenditure, VO2max = maximal oxygen consumption, aEE = activity energy expenditure, HR = heart rate.
The aEEmax and body mass index (BMI) were used to develop a multiple linear regression model to estimate the VO2max using the training data, with the regression formula, expressed as:
VO2max (mL/kg/min) = 0.192 × aEEmax (J/min) − 0.708 × BMI (kg·m−2) + 46.157
The estimated VO2max strongly correlated with the measured VO2max in both groups (Table 2).
Table 2. Performance of multiple linear regression in both groups.
| Statistics | Training group (n = 16) | Test group (n = 8) |
|---|---|---|
| R | 0.81 (P < 0.001) | 0.87 (P < 0.01) |
| Adjusted R2 | 0.63 | 0.74 |
| SEE, mL/kg/min | 4.40 | 5.74 |
| %SEE | 9.53 | 11.85 |
R = correlation coefficient, Adjusted R2 = coefficient of determination, SEE = standard error of the estimate, %SEE = percentage of SEE relative to measured VO2max value, VO2max = maximal oxygen consumption.
The correlation between the estimated and measured VO2max, calculated for all participants, is shown in Fig. 3A, with the Bland-Altman plot shown in Fig. 3B, with the x-axis showing the average of estimated and measured VO2max, with the difference between estimated and measured VO2max (measured VO2max subtracted from estimated VO2max) plotted along the y-axis. The solid line shows the mean value and the dashed line the 1.96 standard deviation (SD) (95% limits of agreement). Values for participants were randomly dispersed within the 1.96 SD range, except for one participant. The mean difference (95% limits of agreement) between the measured and estimated VO2max was 1.26 mL/kg/min (−9.74, 7.22).
Fig. 3.
The correlation between the estimated and measured VO2max. (A) Correlation between the estimated and measured VO2max value of all participants. The thin line is the identity line of the measured and estimated VO2max. (B) Bland-Altman plot (estimated-measured VO2max, n = 24). The solid line represents the mean value, and the dotted line represents the 1.96 SD (95% limit of agreement). With the exception of one participant, the data was randomly distributed among the 1.96 SD range.
VO2max = maximal oxygen consumption, SD = standard deviation
DISCUSSION
In this study, we describe a VO2max estimation model based on the relationship between physical activity (aEE) and corresponding physiological response (HR), using combined ECG and tri-axial accelerometer data in healthy young men. As a strong correlation between the level of physical activity and CRF has been previously found (14,16), and we have added aEEmax as a new feature to quantify personal physical activity. As the VO2max measurement during maximal or submaximal exercise is based on an increase HR in response to physical exercise (24), and knowing that the heterogeneous recovery of HR from physical activity (22) does not strongly correlate with VO2max (23), we used the data corresponding to increased HR in our simple linear regression model to estimate aEEmax.
The estimated VO2max strongly correlated with the measured VO2max in both the training and test groups. The outlier identified on the Bland-Altman plot had the lowest measured VO2max (24.1 mL/kg/min) among all participants. The measured VO2max for this participant was extremely low compared to the average VO2max range (very poor, < 33.0 mL/kg/min) of healthy young male, indicative of a possible error during VO2max measurement or a lower accuracy of the model for participants in the lower range of CRF.
Other CRF estimation methods, using indices of physical activity and physical response, have been reported (13,14,25,26). However, Weyand et al. (25) and Tönis et al. (26) used an exercise protocol to estimate VO2max. Plasqui and Westerterp (13) reported a VO2max estimation method without an exercise protocol using anthropometric values, HR and acceleration data collected over 7 days. The average HR divided by ACM negatively correlated with VO2max, and a multiple linear regression model was developed. After that study, a cross-validation study was conducted to establish a robust regression model (R = 0.86–0.90, R2 = 0.71–0.74, SEE = 341–437 mL/min) (14). Despite the efficacy of this model, the necessity to measure parameters for 7 days would make this method impractical. The separate attachment of an HR sensor and accelerometer could also make the individuals uncomfortable, thus causing behavioral changes. The unified sensor system used in our study appears to be less obtrusive than that of previous studies. Sartor et al. (24) indicated that future non-protocol VO2max estimation should use unobtrusive devices, with the assessment performed using a single day of activity, or even on a single physical activity.
We have improved upon previously available non-protocol based VO2max estimation methods in two ways. First, our method requires only 15-hour of signal measurement, which is the shortest time for VO2max estimation reported to date (14) and allows the possibility of estimating the VO2max using data gathered from activity in one and half days. Many patch-type devices have been developed to measure HR and acceleration, but these devices have not been successful in regular use due to inconvenience in operation. Therefore, by reducing the time taken for VO2max estimation, the proposed method improves upon the current standard. Second, the performance of the estimation regression model using aEEmax as a new feature was comparable to the results of previous studies, despite the reduced signal measurement time.
The limitations of our study need to be acknowledged. First, our participant group was relatively homogenous (healthy young men) and the sample size was not large enough to determine a representative pattern. Therefore, an additional study with a larger, more varied sample group is needed with a revised regression model including additional parameters, such as age and gender. Since age and gender are considered as parameters for calculating aEEmax from maximum HR and energy expenditure, aEEmax is expected to be an effective parameter for VO2max estimation even in a broad age range and gender. Second, changes in participants' VO2max over the long-term should be monitored in a longitudinal study to verify the accuracy of our estimation algorithm. Third, chest-attached sensors, such as the one used in the present study, may not be sufficiently comfortable for use in daily life. Considering the widespread availability of fitness watches and trackers, which are more comfortable to use in daily life, and because these devices provide information regarding both HR and aEE, a follow-up study should be conducted using these devices to verify the accuracy of the proposed algorithm.
In summary, we have used a new feature, aEEmax, to estimate VO2max during daily activities. The new feature captures the relationship between physical activity and anthropometric values, without requiring a large data set, and successfully estimated VO2max in a small sample of healthy young men. The length of data required for VO2max estimation was only one and half days and the data were measured from a single device. The comparison of measured and estimated VO2max values revealed robust agreement and the correlation coefficient for the VO2max estimation algorithm was shown to be comparable to the values in previous studies.
ACKNOWLEDGMENT
The authors would like to thank all participants.
Footnotes
Funding: This research was supported by a Research Program funded by the National Medical Center, Research Institute (NMC2013-MS-02).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Hwang SH, Yoon HJ. Data curation: Ahn JW, Yoon C. Formal analysis: Ahn JW, Yoon C, Hwang SH, Yoon HJ. Investigation: Ahn JW, Hwang SH, Yoon C, Lee J, Yoon HJ. Writing - review & editing: Ahn JW, Hwang SH, Yoon C, Lee J, Kim HC, Yoon HJ.
References
- 1.Chen KY, Bassett DR., Jr The technology of accelerometry-based activity monitors: current and future. Med Sci Sports Exerc. 2005;37:S490–S500. doi: 10.1249/01.mss.0000185571.49104.82. [DOI] [PubMed] [Google Scholar]
- 2.Chen KY, Sun M. Improving energy expenditure estimation by using a triaxial accelerometer. J Appl Physiol. 1985;1997:2112–2122. doi: 10.1152/jappl.1997.83.6.2112. [DOI] [PubMed] [Google Scholar]
- 3.Plasqui G, Bonomi AG, Westerterp KR. Daily physical activity assessment with accelerometers: new insights and validation studies. Obes Rev. 2013;14:451–462. doi: 10.1111/obr.12021. [DOI] [PubMed] [Google Scholar]
- 4.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- 5.Blair SN, Kampert JB, Kohl HW, 3rd, Barlow CE, Macera CA, Paffenbarger RS, Jr, Gibbons LW. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996;276:205–210. [PubMed] [Google Scholar]
- 6.Lee DC, Artero EG, Sui X, Blair SN. Mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol. 2010;24:27–35. doi: 10.1177/1359786810382057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park M, Ko Y, Song SH, Kim S, Yoon HJ. Association of low aerobic fitness with hyperfiltration and albuminuria in men. Med Sci Sports Exerc. 2013;45:217–223. doi: 10.1249/MSS.0b013e318271b39f. [DOI] [PubMed] [Google Scholar]
- 8.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 9.Helgerud J, Høydal K, Wang E, Karlsen T, Berg P, Bjerkaas M, Simonsen T, Helgesen C, Hjorth N, Bach R, et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc. 2007;39:665–671. doi: 10.1249/mss.0b013e3180304570. [DOI] [PubMed] [Google Scholar]
- 10.Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85:546–562. doi: 10.1016/0002-8703(73)90502-4. [DOI] [PubMed] [Google Scholar]
- 11.Noonan V, Dean E. Submaximal exercise testing: clinical application and interpretation. Phys Ther. 2000;80:782–807. [PubMed] [Google Scholar]
- 12.Kline GM, Porcari JP, Hintermeister R, Freedson PS, Ward A, McCarron RF, Ross J, Rippe JM. Estimation of VO2max from a one-mile track walk, gender, age, and body weight. Med Sci Sports Exerc. 1987;19:253–259. [PubMed] [Google Scholar]
- 13.Plasqui G, Westerterp KR. Accelerometry and heart rate as a measure of physical fitness: proof of concept. Med Sci Sports Exerc. 2005;37:872–876. doi: 10.1249/01.mss.0000161805.61893.c0. [DOI] [PubMed] [Google Scholar]
- 14.Plasqui G, Westerterp KR. Accelerometry and heart rate as a measure of physical fitness: cross-validation. Med Sci Sports Exerc. 2006;38:1510–1514. doi: 10.1249/01.mss.0000228942.55152.84. [DOI] [PubMed] [Google Scholar]
- 15.Cao ZB, Miyatake N, Higuchi M, Ishikawa-Takata K, Miyachi M, Tabata I. Prediction of VO2max with daily step counts for Japanese adult women. Eur J Appl Physiol. 2009;105:289–296. doi: 10.1007/s00421-008-0902-8. [DOI] [PubMed] [Google Scholar]
- 16.Cao ZB, Miyatake N, Higuchi M, Miyachi M, Ishikawa-Takata K, Tabata I. Predicting VO2max with an objectively measured physical activity in Japanese women. Med Sci Sports Exerc. 2010;42:179–186. doi: 10.1249/MSS.0b013e3181af238d. [DOI] [PubMed] [Google Scholar]
- 17.Kaminsky LA American College of Sports Medicine. ACSM's Health-Related Physical Fitness Assessment Manual. 3rd ed. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2010. [Google Scholar]
- 18.Burns A, Greene BR, McGrath MJ, O'Shea TJ, Kuris B, Ayer SM, Stroiescu F, Cionca V. SHIMMER™ - a wireless sensor platform for noninvasive biomedical research. IEEE Sens J. 2010;10:1527–1534. [Google Scholar]
- 19.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37:S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 20.Kligfield P, Gettes LS, Bailey JJ, Childers R, Deal BJ, Hancock EW, van Herpen G, Kors JA, Macfarlane P, Mirvis DM, et al. Recommendations for the standardization and interpretation of the electrocardiogram: part I: the electrocardiogram and its technology: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation. 2007;115:1306–1324. doi: 10.1161/CIRCULATIONAHA.106.180200. [DOI] [PubMed] [Google Scholar]
- 21.Pan J, Tompkins WJ. A real-time QRS detection algorithm. IEEE Trans Biomed Eng. 1985;32:230–236. doi: 10.1109/TBME.1985.325532. [DOI] [PubMed] [Google Scholar]
- 22.Bosquet L, Gamelin FX, Berthoin S. Reliability of postexercise heart rate recovery. Int J Sports Med. 2008;29:238–243. doi: 10.1055/s-2007-965162. [DOI] [PubMed] [Google Scholar]
- 23.Campos EZ, Bastos FN, Papoti M, Freitas IF, Junior, Gobatto CA, Balikian P., Junior The effects of physical fitness and body composition on oxygen consumption and heart rate recovery after high-intensity exercise. Int J Sports Med. 2012;33:621–626. doi: 10.1055/s-0031-1295442. [DOI] [PubMed] [Google Scholar]
- 24.Sartor F, Vernillo G, de Morree HM, Bonomi AG, La Torre A, Kubis HP, Veicsteinas A. Estimation of maximal oxygen uptake via submaximal exercise testing in sports, clinical, and home settings. Sports Med. 2013;43:865–873. doi: 10.1007/s40279-013-0068-3. [DOI] [PubMed] [Google Scholar]
- 25.Weyand PG, Kelly M, Blackadar T, Darley JC, Oliver SR, Ohlenbusch NE, Joffe SW, Hoyt RW. Ambulatory estimates of maximal aerobic power from foot -ground contact times and heart rates in running humans. J Appl Physiol. 1985;2001:451–458. doi: 10.1152/jappl.2001.91.1.451. [DOI] [PubMed] [Google Scholar]
- 26.Tönis TM, Gorter K, Vollenbroek-Hutten MM, Hermens H. Comparing VO2max determined by using the relation between heart rate and accelerometry with submaximal estimated VO2max. J Sports Med Phys Fitness. 2012;52:337–343. [PubMed] [Google Scholar]