Abstract
Aim:
The aim of the study was to compare the clinical and microbiological efficacy of Group I-delmopinol dentifrice, Group II-chlorhexidine, and Group III-triclosan-containing regularly used control dentifrice on plaque formation and gingivitis.
Materials and Methods:
A total of 45 healthy volunteer students fulfilling the inclusion criteria are recruited for this randomized control parallel study. All the individuals were randomly assigned into 3 groups depending on the dentifrice prescribed. After the selection of individuals, thorough scaling and polishing were performed for all the individuals, and in a 4 days' washout period, they were refrained from regular oral hygiene maintenance and 0.9% NaCl (normal saline) rinse was prescribed to obtain plaque regrowth. Microbiological morphotypes were assessed using darkfield microscope.
Statistical Analysis:
The data were analyzed using the SPSS-software 19.00 program. The intragroup comparison of clinical parameters was done using Kruskal–Wallis ANOVA test, and intergroup comparison was done by Mann–Whitney U-test. The intragroup comparison of clinical parameters including modified staining index, the supragingival microbiota such as cocci, bacilli, and spirochetes scores was done at various study intervals using one-way ANOVA, and intergroup comparison was done using Tukey's multiple post hoc test.
Results:
The results showed that statistically significant correlation between Group II and Group III at 15 and 30 days and between Group I and Group II at 30 days with cocci and bacilli but not spirochetes.
Conclusion:
Group II showed better plaque and gingivitis reduction compared to other active groups. To validate the results of the present study, further long-term studies with larger sample size and evaluation using known and proven study designs on gingivitis patients are needed.
Keywords: Chlorhexidine, darkfield microscope, delmopinol, triclosan
INTRODUCTION
Gingivitis is an inflammatory condition of the gums that affects most of the adult population. Maintenance of an effective plaque control is the cornerstone in preventing and controlling gingival and periodontal diseases. The most commonly employed plaque control at home is by tooth brushing.[1] The use of toothpaste has ancient root. Ancient Greeks, Egyptians, and Roman civilizations were known to develop their own tooth powder containing pumice, talcum, coral powder, and alabaster.[2] Delmopinol ((+)-3-(4-propylheptyl)-4-morpholineethanol hydrochloride) inhibits plaque formation by interfering with plaque adhering to the tooth and gingiva by acting at the interface between the plaque bacteria and the tooth or gingival surface and also shows significant effect in penetrating into the existing plaque.[3] Chlorhexidine is a large dicationic molecule, (1,6-di(4-chlorophenyl-diguanido)) hexane, with the positive charge distributed over the nitrogen atoms on either side of the hexamethylene bridge and has ability to absorb into negatively charged surfaces, such as bacterial cell walls, where it exerts its bacteriostatic and bactericidal effects. The reported side effects of chlorhexidine are extrinsic staining of the teeth and tongue, (painful) desquamations of the oral mucosa, and rarely parotid swelling. The most obvious side effect as a result of chlorhexidine is the development of stain.[4] In plaque regrowth studies, plaque accumulation from day 1 (zero level), in the absence of mechanical cleaning and under the influence of the allocated formulation, was scored on day 5.[5] The teeth with gingivitis had a supragingival flora of predominantly filamentous cells and a scanty but distinct subgingival flora. Supragingival plaque control is the effective method of controlling gingivitis and it is important part of periodontal therapy. The mechanical removal of plaque by home care regime is time-consuming and tedious, so the supplementation of chemotherapeutic agents would be beneficial to gingival health. Recently, it has been found that metal ions and essential oils have their own limitations. Thus, the alternative approach has been very much essential for effective plaque control. Hence, the present study was undertaken to compare the clinical and microbiological efficacy of chlorhexidine gluconate, delmopinol-containing dentifrice with the conventional triclosan-containing regularly used control dentifrice on plaque formation and gingivitis.
MATERIALS AND METHODS
After due authorization from the Institutional Ethical Board, a total of 45 healthy volunteer students fulfilling the inclusion criteria were selected for this randomized control group parallel study.
A total of 45 systemically healthy patients (29 males and 16 females), aged between 20 and 30 years with a mean age of 24.42 ± 1.52 years without any systemic diseases and who are able to maintain oral hygiene by their own were included in the study. Patients should also have healthy indexed teeth, and the teeth adjacent to the index teeth should be without dental restorations and prosthesis.
Patients who are excluded are with periodontal pockets ≥5 mm, with previous history of periodontal therapy within the past 1 year, with a history of hypersensitivity to any of ingredients of test compounds, receiving antibiotics, corticosteroids, anticholinergic, antidepressants, current smokers, pregnant, and lactating women.
All the patients were randomly assigned by computer-generated randomization into three groups (Group I-delmopinol dentifrice), (Group II-chlorhexidine), (Group III-triclosan) depending on the dentifrice prescribed. After the selection of patients, thorough scaling and polishing were performed for all the patients, and in a 4 days' washout period, they were asked to refrain from their regular oral hygiene maintenance (mechanical plaque control), and 0.9% NaCl (normal saline) rinse was prescribed to obtain plaque regrowth.[6] A detailed case history was taken and the following clinical parameters, namely, plaque index (PI),[7] gingival index (GI),[8] staining index,[9,10] and oral malodor using hedonic scale,[11] and microbiological morphotypes such as cocci, bacilli, and spirochetes were assessed using darkfield microscope, after supragingival plaque was collected with a sterile curette. The curette with the collected plaque was dispensed in Eppendorf tube containing normal saline and then immediately sent to laboratory where they were analyzed under darkfield microscope. To minimize clumping and the loss of bacterial motility, samples were prepared and the examination completed within 1 h of their collection.[12] One drop of the suspension was applied to a microscopic slide and coverslipped. Excess fluid was removed by inverting the slide over an absorbent surface and applying moderate pressure. Care was taken to avoid excessive bubbling of air during the dispersion. The slide was examined under darkfield microscopy at a magnification of 10X. A fixed reference line in the ocular was used to count the cells using a manual cell counter, and the cells were counted once only if they are showing movement.
Generally from the 100 bacteria in the selected field were categorized morphologically into three distinct classes such as coccoid cells, rods, and spirochetes. After recording the parameters and sample collection, thorough scaling and polishing were performed and patients were assigned to use respective dentifrices in a modified bass method twice daily. The sample collection was done, and clinical parameters and microbiological morphotypes were recorded again on 15th day and 30th day from baseline and were analyzed and compared.
Statistical analysis
The data were analyzed using the SPSS-software 19.00 program (SPSS Inc., Chicago, IL, USA). The intragroup comparison of PI scores, oral malodor scores, and GI scores was done at various study intervals using Kruskal–Wallis ANOVA test, and intergroup comparison was done using Mann–Whitney U-test. The intragroup comparison of clinical parameters including modified staining index, the supragingival microbiota such as cocci, bacilli, and spirochetes scores were done at various study intervals using one-way ANOVA test, and intergroup comparison was done using Tukey's multiple post hoc test. Differences were considered as statistically significant at P ≤ 0.05.
RESULTS
A total of 45 healthy individuals with a mean age of 24.44 years were selected for this study comprising 29 males and 16 females.
Plaque Index and gingival index scores
The intragroup comparison of PI and GI scores was done between groups at study intervals using Kruskal–Wallis one-way ANOVA test as shown in Table 1. No significant difference was observed in all groups at baseline.
Table 1.
Intragroup comparison of Group I, Group II, and Group III with plaque index and gingival index scores at different time points by Kruskal-Wallis one-way ANOVA test
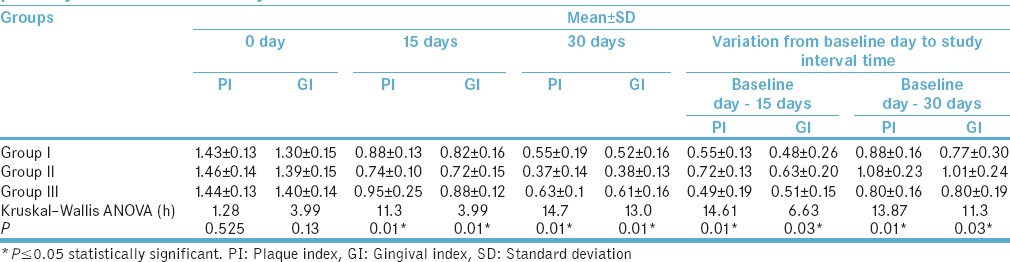
The intergroup comparison of PI and GI scores was done between groups at study intervals using Mann–Whitney U-test as shown in Table 2. The results showed that statistically significant correlation between Group II and Group III at 15 and 30 days and between Group I and Group II at 15 days and 30 days in PI and GI scores, respectively.
Table 2.
Intergroup comparison of Group I, Group II, and Group III with plaque index and gingival index scores at different time points by Mann-Whitney U-test
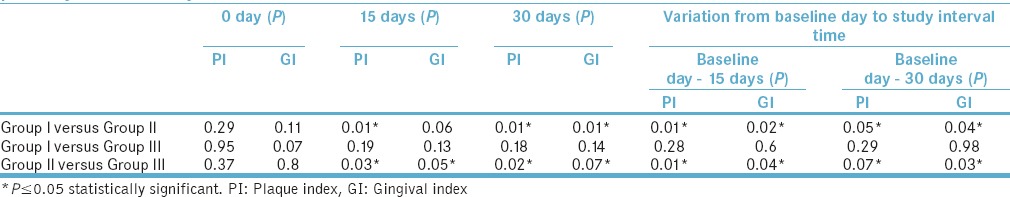
Modified Lobene staining index scores
The intragroup comparison of modified Lobene staining index (MSI) scores was done between groups at study intervals using One-way ANOVA test as shown in Table 3, respectively. Greater extent of staining was increased in Group II which was observed. No significant difference was observed in all groups at baseline. The intergroup comparison of MSI scores done between groups at study intervals using Tukey's multiple post hoc test as shown in Table 4. The results showed that statistically significant correlation was found between Group II and Group III at 15 (P = 0.001) and 30 days (P = 0.01) and between Group I and Group II at 15 days (0.01) and 30 days (P = 0.03).
Table 3.
Intragroup comparison of Group I, Group II, and Group III with modified Lobene staining index and oral malodor scores at different y one-way ANOVA test
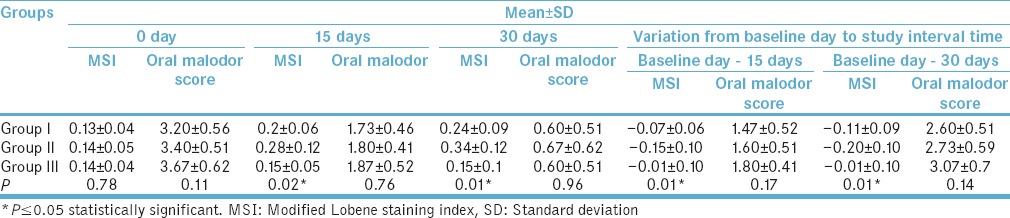
Table 4.
Intergroup comparison of Group I, Group II, and Group III with Modified Lobene staining index and oral malodor scores at different time points by Mann-Whitney U-test
Oral malodor scores
The intragroup comparison oral malodor scores were done using hedonic scale between groups at the study intervals using Kruskal–Wallis one-way ANOVA test as shown in Table 3. Better oral malodor reduction was observed in triclosan group. No significant difference was observed in all groups at baseline. The intergroup comparison of oral malodor scores was done between groups at study intervals using Mann–Whitney U-test as shown in Table 4. The results showed no statistically significant correlation between the groups.
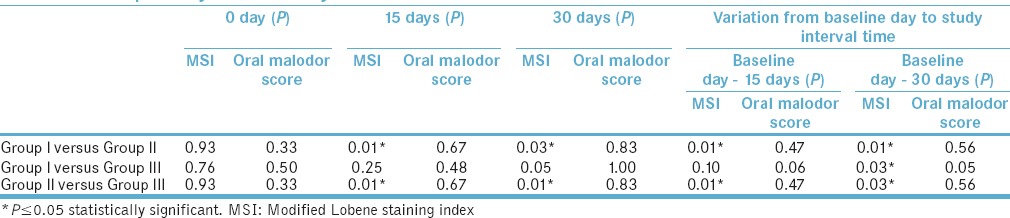
Cocci, bacilli, and spirochetes scores
The intragroup comparison of cocci and bacilli scores was done within the groups at study intervals using one-way ANOVA test as shown in Tables 5–7, respectively. Better improvement in cocci, bacilli, and spirochetes scores was observed in Group II than other groups. No significant difference was observed in all groups at baseline.
Table 5.
Intra group comparison of Group I, Group II, and Group III with cocci scores at different time points by one-way ANOVA test
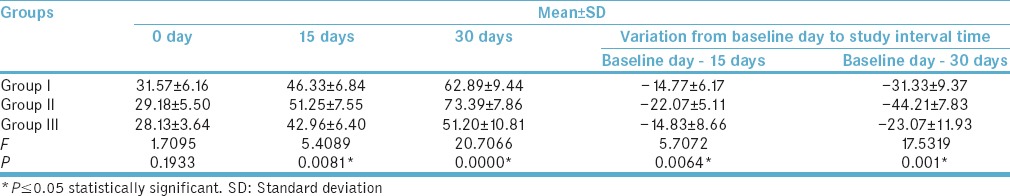
Table 7.
Intra group comparison of Group I, Group II, and Group III with spirochetes scores at different time points by one-way ANOVA test
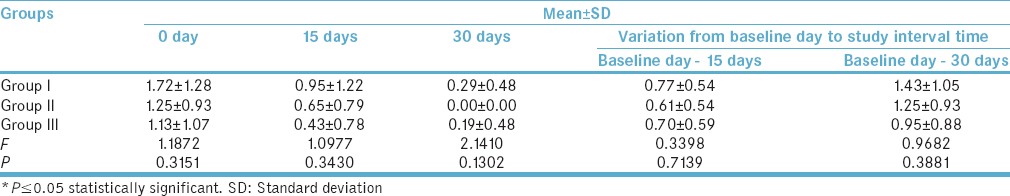
Table 6.
Intragroup Comparison of Group I, Group II, and Group III with bacilli scores at different time points by one-way ANOVA test
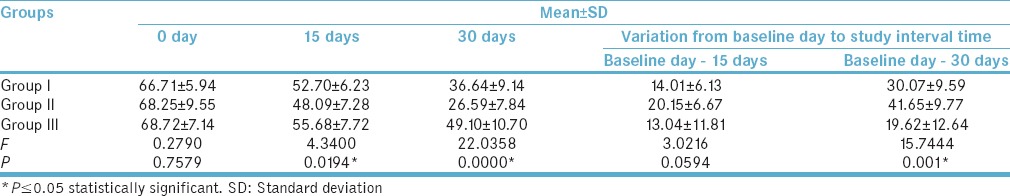
The intergroup comparison of cocci, bacilli, and spirochetes scores done between groups at the study intervals using Tukey's multiple post hoc test as shown in Table 8, respectively. The results of cocci and bacilli showed that statistically significant correlation was found between Group II and Group III at 15 and 30 days and between Group I and Group II at 30 days, whereas the intergroup comparison of spirochete scores done between groups at study intervals showed that there is no statistically significant correlation between all the groups [Figures 1–6].
Table 8.
Intergroup Comparison of Group I, Group II, and Group III with cocci, bacilli, and spirochetes scores at different time points by Tukey's multiple post hoc test
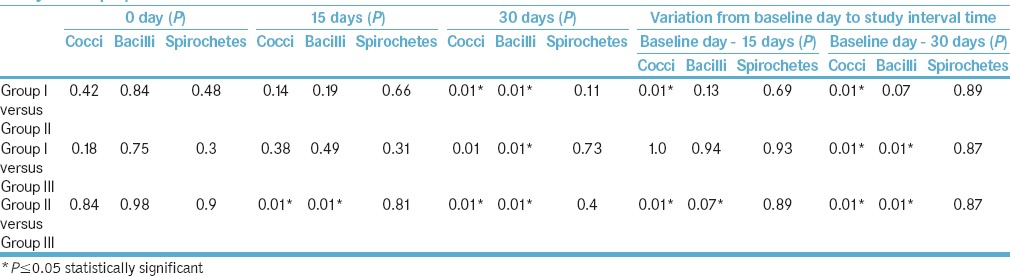
Figure 1.
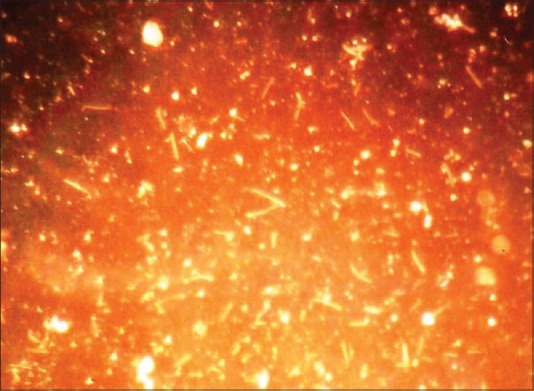
Group I bacterial morphotypes at baseline
Figure 6.
Group III bacterial morphotypes after 30 days
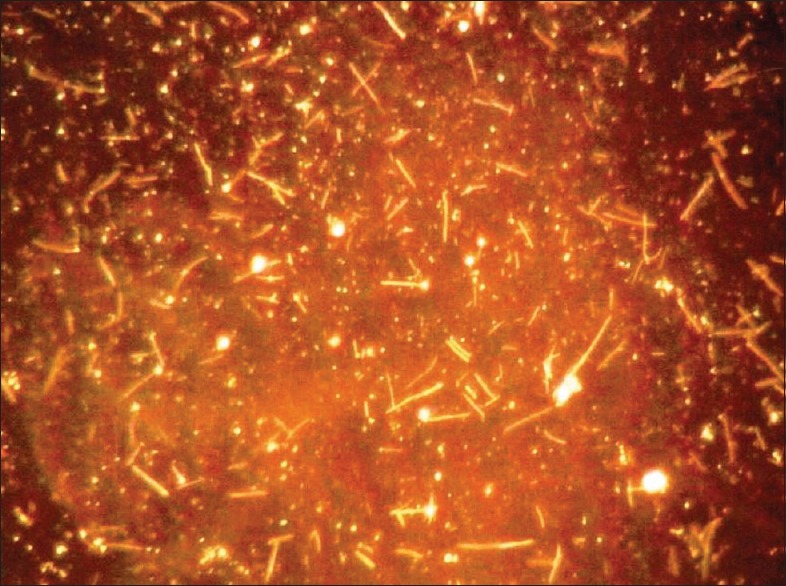
Figure 2.

Group I bacterial morphotypes after 30 days
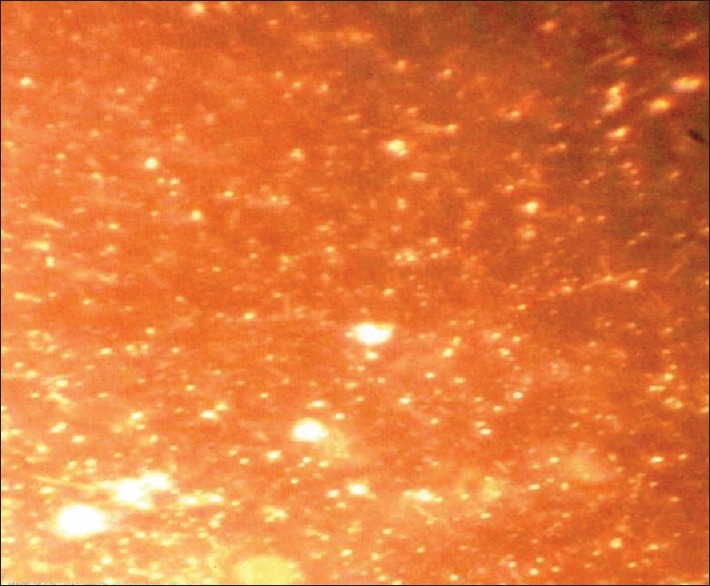
Figure 3.
Group II bacterial morphotypes at baseline
Figure 4.
Group II bacterial morphotypes after 30 days
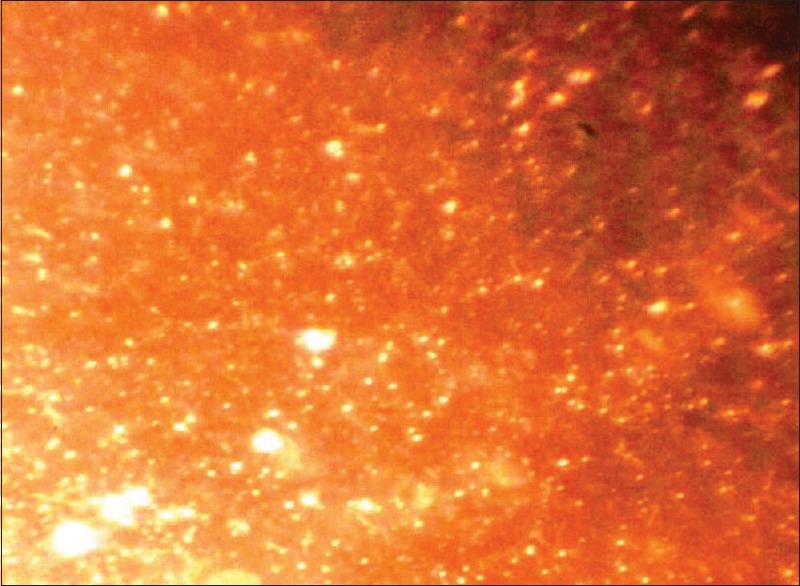
Figure 5.
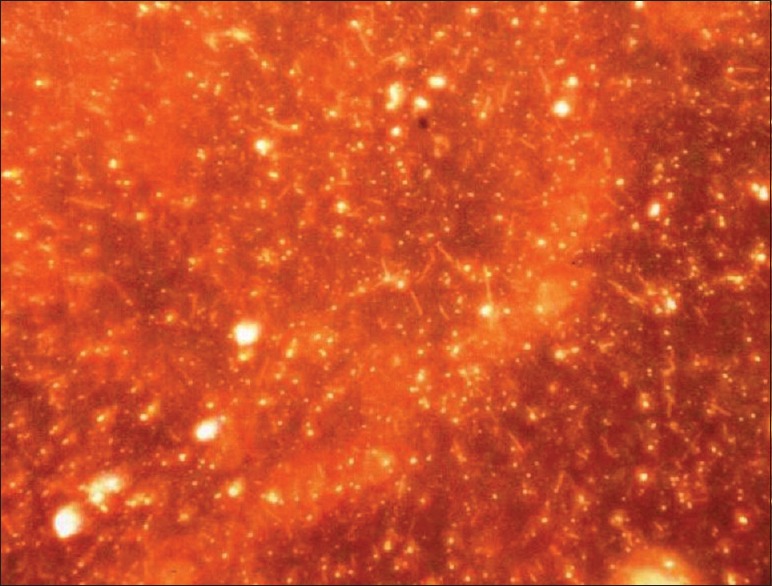
Group III bacterial morphotypes at baseline
DISCUSSION
Bacterial plaque, a kind of specialized biolfilm, is the cause of gingivitis and periodontitis. Bacterial accumulation may cause breath odor. Comparing plaque samples among healthy sites and sites with gingivitis, clear shift in bacterial types were noticed.[13] Gingivitis is an inflammatory condition of the gums that affects most of the adult population. Epidemiological studies revealed a peculiarly high correlation between supragingival plaque levels and chronic gingivitis, and clinical researches led to the proof that plaque was the primary etiological factor in gingival inflammation.[14]
A dentifrice is usually used in combination with tooth brushing with the purpose of facilitating plaque removal and applying agents to the tooth surfaces for therapeutic or preventive reasons.[15] The purpose of the present study was to evaluate the efficacy of chlorhexidine, delmopinol containing dentifrices with regular dentifrice containing triclosan on plaque formation and gingivitis by clinical and microbiological analysis by examination of supragingival plaque sample collected from the patients in a 1 month randomized parallel balanced group study.
Many studies using darkfield microscopy proved that the cocci bacteria were increased in healthy samples, and rods and spirochetes were decreased in diseased samples when using either chlorhexidine[16] or triclosan antiplaque agents. However, in the present study, when the gingival status, Clinical & Microbiologic parameters were compared at baseline between Delmopinol, Chlorhexidine, and Triclosan-containing regular dentifrice groups no significant difference was observed. Statistically significant PI and GI reduction was observed in all groups from baseline day to 30th day. This may be due to all the participants (dental students) in this study who were well aware of brushing techniques and mechanical plaque control. Better plaque and gingivitis reduction was observed in chlorhexidine group.
In the present study, 0.004% chlorhexidine dentifrice group showed mean PI and GI reduction from baseline to each study interval time which is statistically significant. Yates et al.[17] also reported that 1% chlorhexidine dentifrice showed mean PI and GI was reduced significantly at each time in a 6 months' study. These results confirm the findings of an experimental gingivitis study conducted by Jenkins which served to show the activity of the chlorhexidine in the dentifrice formulation. This might be due to the anionic and cationic agents in dentifrice did not have any interactions when they were formulated as a dentifrice, and this improvement in plaque reduction certainly reflected a Hawthorne effect by knowingly involved participants in the present study.
In 1970 Gjermo and Rolla[18] reported that 0.8% chlorhexidine dentifrice showed mean PI reduction was better in compared to Colgate control dentifrice and in accordance to this study, present study also showed that 0.004% chlorhexidine dentifrice group showed significant PI and GI reduction compared to Colgate control dentifrice. Tooth staining is a well-established side effect of chlorhexidine products.[19,20] Experimental gingivitis study conducted by Yates and Jenkins[18] observed with the use of 1% chlorhexidine dentifrice showed significantly increased staining. The present study also showed that 0.004% chlorhexidine dentifrice cause teeth staining which was significantly more than other two dentifrice groups. The reduction in the PI and GI indices in the present study was also accomplished by shift in the supragingival microbiological flora.
Delmopinol (0.2% w/v) mouthwash in a study conducted by Claydon et al.[21] showed statistically significant reduction in PI, GI scores, and increased staining, and the results of present study were in accordance with it. The reduction in PI and GI scores was also accomplished by the shift in the microbiological flora. Delmopinol (0.2%w/v) dentifrice showed significant increasing in cocci scores and decreased in rods during study intervals.
Palomo et al.[22] reported that triclosan-containing dentifrice alone without copolymers did not showed significant reduction of PI and GI score at any of the examination intervals, as compared to placebo. In the present study, triclosan-containing regular used dentifrice showed significant reduction of PI and GI scores during study intervals. This might be due to all participants in the present study were well aware of mechanical plaque control. Nonnenmacher in an experimental gingivitis study reported that in gingivitis phase, cocci were reduced and rods and spirochetes were increased with triclosan mouth rinse. The present study showed that cocci were increased, rods and spirochetes were decreased during study intervals with using triclosan as dentifrice, but significantly less effective when compared chlorhexidine dentifrice.
Although the hedonic scale may be useful for measuring the effects of compounds that mask malodor, it gives little information about whether or not treatments interfere with the fundamental malodor processes occurring in the mouth that is the biogenic transformation of substrates into volatile compounds (VCs), including volatile sulfur compounds (VSCs).[11] In this present study, no significant reduction was found in any dentifrice group from baseline to study intervals.
SUMMARY AND CONCLUSION
The present study was undertaken to evaluate and compare the efficacy of chlorhexidine, delmopinol containing dentifrices with regularly used triclosan-containing dentifrice on plaque and gingivitis reduction in a 1 month randomized, and parallel group controlled clinical and microbiological study and the results showed that PI and GI was reduced in accomplish with increased cocci and reduced rods and spirochete count in all dentifrice groups and chlorhexidine group showed better plaque and gingivitis reduction compared to other active (delmopinol) and control (triclosan-containing regular used) groups. As all the participants (dental students) in the study were well aware of mechanical plaque control, all groups showed plaque and gingivitis reduction and interaction of anion and cations in chlorhexidine dentifrice might have not occurred.
Clinical and microbial evaluation between the chlorhexidine, delmopinol, and triclosan-containing regular used dentifrices was not done earlier; the results of the present study could not be compared with previous studies and to reconfirm and validate the results of the present study, further long-term studies with larger sample size and evaluation using known and proven study designs on gingivitis patients are needed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflflicts of interest.
REFERENCES
- 1.van der Weijden GA, Hioe KP. A systematic review of the effectiveness of self-performed mechanical plaque removal in adults with gingivitis using a manual toothbrush. J Clin Periodontol. 2005;32(Suppl 6):214–28. doi: 10.1111/j.1600-051X.2005.00795.x. [DOI] [PubMed] [Google Scholar]
- 2.Ciancio SG. Oral hygiene products use: Introduction. Periodontol 2000. 1995;8:7–10. [Google Scholar]
- 3.Steinberg D, Beeman D, Bowen WH. The effect of delmopinol on glucosyltransferase adsorbed on to saliva-coated hydroxyapatite. Arch Oral Biol. 1992;37:33–8. doi: 10.1016/0003-9969(92)90150-7. [DOI] [PubMed] [Google Scholar]
- 4.Jones CG. Oral hygiene products. Chlorhexidine: Is it still the gold standard? Periodontol 2000. 1997;15:55–62. doi: 10.1111/j.1600-0757.1997.tb00105.x. [DOI] [PubMed] [Google Scholar]
- 5.Addy M, Renton-Harper P, Newcombe R. Plaque regrowth studies: Discriminatory power of plaque index compared to plaque area. J Clin Periodontol. 1999;26:110–2. doi: 10.1034/j.1600-051x.1999.260208.x. [DOI] [PubMed] [Google Scholar]
- 6.Pizzo G, Guiglia R, Imburgia M, Pizzo I, D'Angelo M, Giuliana G. The effects of antimicrobial sprays and mouthrinses on supragingival plaque regrowth: A comparative study. J Periodontol. 2006;77:248–56. doi: 10.1902/jop.2006.050116. [DOI] [PubMed] [Google Scholar]
- 7.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 8.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 9.Macpherson LM, Stephen KW, Joiner A, Schäfer F, Huntington E. Comparison of a conventional and modified tooth stain index. J Clin Periodontol. 2000;27:854–9. doi: 10.1034/j.1600-051x.2000.027011854.x. [DOI] [PubMed] [Google Scholar]
- 10.Gründemann LJ, Timmerman MF, Ijzerman Y, van der Weijden GA, van der Weijden GA. Stain, plaque and gingivitis reduction by combining chlorhexidine and peroxyborate. J Clin Periodontol. 2000;27:9–15. doi: 10.1034/j.1600-051x.2000.027001009.x. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg M, Septon I, Eli I, Bar-Ness R, Gelernter I, Brenner S, et al. Halitosis measurement by an industrial sulphide monitor. J Periodontol. 1991;62:487–9. doi: 10.1902/jop.1991.62.8.487. [DOI] [PubMed] [Google Scholar]
- 12.Listgarten MA, Helldén L. Relative distribution of bacteria at clinically healthy and periodontally diseased sites in humans. J Clin Periodontol. 1978;5:115–32. doi: 10.1111/j.1600-051x.1978.tb01913.x. [DOI] [PubMed] [Google Scholar]
- 13.Eschler B. Key Concepts: Bacteria, Plaque/Biolfilm, Gingivitis and Periodontitis Michigan Dental Association (MDA) Annual Session. 2012:1–5. [Google Scholar]
- 14.Loe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol. 1965;36:177–87. doi: 10.1902/jop.1965.36.3.177. [DOI] [PubMed] [Google Scholar]
- 15.Lindhe J, Lang NP, Karring T. Clinical Periodontolgy and Implant Dentistry. 5th ed. Oxford: Black well; 2008. pp. 705–33. [Google Scholar]
- 16.Chikte UM, Pochee E, Rudolph MJ, Reinach SG. Evaluation of stannous fluoride and chlorhexidine sprays on plaque and gingivitis in handicapped children. J Clin Periodontol. 1991;18:281–6. doi: 10.1111/j.1600-051x.1991.tb00429.x. [DOI] [PubMed] [Google Scholar]
- 17.Yates R, Jenkins S, Newcombe R, Wade W, Moran J, Addy M. A 6-month home usage trial of a 1% chlorhexidine toothpaste (1).Effects on plaque, gingivitis, calculus and toothstaining. J Clin Periodontol. 1993;20:130–8. doi: 10.1111/j.1600-051x.1993.tb00327.x. [DOI] [PubMed] [Google Scholar]
- 18.Gjermo P, Rolla G. Plaque inhibition by antibacterial dentifrices. Scand J Dent Res. 1970;78:464–70. doi: 10.1111/j.1600-0722.1970.tb02099.x. [DOI] [PubMed] [Google Scholar]
- 19.Löe H, Schiött CR, Karring G, Karring T. Two years oral use of chlorhexidine in man. I. General design and clinical effects. J Periodontal Res. 1976;11:135–44. doi: 10.1111/j.1600-0765.1976.tb00061.x. [DOI] [PubMed] [Google Scholar]
- 20.Flötra L, Gjermo P, Rölla G, Waerhaug J. Side effects of chlorhexidine mouth washes. Scand J Dent Res. 1971;79:119–25. doi: 10.1111/j.1600-0722.1971.tb02001.x. [DOI] [PubMed] [Google Scholar]
- 21.Claydon N, Hunter L, Moran J, Wade W, Kelty E, Movert R, et al. A 6-month home-usage trial of 0.1% and 0.2% delmopinol mouthwashes (I). Effects on plaque, gingivitis, supragingival calculus and tooth staining. J Clin Periodontol. 1996;23(3 Pt 1):220–8. doi: 10.1111/j.1600-051x.1996.tb02079.x. [DOI] [PubMed] [Google Scholar]
- 22.Palomo F, Wantland L, Sanchez A, Volpe AR, McCool J, DeVizio W. The effect of three commercially available dentifrices containing triclosan on supragingival plaque formation and gingivitis: A six month clinical study. Int Dent J. 1994;44(1 Suppl 1):75–81. [PubMed] [Google Scholar]


