Abstract
Whereas hemispheric dominance is well-established for appendicular motor control in humans, the evidence for dominance in axial motor control is still scarce. In Parkinson's disease (PD), unilateral (UL) onset of appendicular motor symptoms corresponds with asymmetric neurodegeneration predominantly affecting contralateral nigrostriatal circuits. Disease progression yields bilateral and axial motor symptoms but the initial appendicular asymmetry usually persists. Furthermore, there is evidence for hemispheric dominance for axial motor dysfunction in some of these patients. Dopaminergic medications improve appendicular symptoms but can also produce motor complications over time. Once these complications develop, bilateral (BL) deep brain stimulation (DBS) of the subthalamic nuclei (STN) can significantly improve appendicular symptoms while reducing medication doses and motor complications. Conversely, axial motor symptoms remain a significant source of disability, morbidity, and mortality for patients with PD. These axial symptoms do not necessarily improve with dopaminergic therapy, might not respond, and could even worsen after BL-DBS. In contrast to medications, DBS provides the opportunity to modify stimulation parameters for each cerebral hemisphere. Identical, BL-DBS of motor circuits with hemispheric dominance in PD might produce overstimulation on one side and/or understimulation on the other side, which could contribute to motor dysfunction. Several studies based on asymmetry of appendicular motor symptoms already support an initial UL rather than BL approach to DBS in some patients. The response of axial motor symptoms to UL versus BL-DBS remains unclear. Nonetheless, UL-DBS, staged BL-DBS, or asymmetric programming of BL-DBS could also be considered in patients with PD.
Keywords: Asymmetric neuromodulation, hemispheric dominance, Parkinson's disease, postural instability and gait dysfunction, subthalamic nucleus deep brain stimulation
INTRODUCTION
Parkinson's disease (PD) is a chronic neurodegenerative disorder associated with loss of dopaminergic neurons in the nigrostriatal pathways. In the U.S., approximately 1 million people have PD and additional 50,000 are diagnosed each year. The prevalence of PD significantly increases with age, ranging from 41 per 100,000 people in the 40–49 years group to 19 per 1,000 people older than 80 years worldwide.[18,57] With the estimated increase in the U.S. population older than 50 years old, the overall PD prevalence of 0.401% in 2005 will increase to approximately 0.535% in the year 2040.[58] Despite promising advances in the understanding of this condition, PD remains a relentlessly progressive condition that significantly impairs motor and nonmotor aspects of daily living.
Appendicular motor dysfunction in early PD is usually unilateral (UL) and includes tremor, rigidity, and bradykinesia. Disease progression yields bilateral (BL) and axial motor symptoms, but the initial UL predominance usually persists. Dopaminergic agents can improve appendicular and some axial symptoms; however, they can also produce significant complications over time (fluctuations, dyskinesia). Once these complications develop, BL deep brain stimulation (DBS) of the subthalamic nuclei (STN) is a safe and effective intervention capable of improving appendicular symptoms while reducing medication requirements and motor complications. Axial motor dysfunction in PD includes dysarthria, dysphagia, postural instability, and gait dysfunction (PIGD) including freezing of gait (FOG). These symptoms remain a significant source of morbidity and mortality in PD. They do not necessarily improve with medications, might not respond, and could even worsen with BL STN-DBS.[69,77,78] In this review, we focus on the evidence for hemispheric dominance of appendicular and axial motor control in PD, and the potential effects of modulating these presumably lateralized circuits with unilateral (UL), symmetric, and asymmetric BL STN-DBS.
LATERALIZATION OF NORMAL MOTOR CONTROL
Certain brain functions are predominantly controlled by one hemisphere (i.e., hemispheric dominance or lateralization). For instance, the right (R) hemisphere is dominant for spatial cognition, body schema, proprioceptive control, and action inhibition,[5,31,83] whereas the left (L) is dominant for verbal processing and motor control.[65] This L-sided dominance for motor control is particularly clear in 90% of humans that are R-handed. In L-handed and ambidextrous people, several studies have shown that brain asymmetries are less pronounced, and thus, it is unclear if the R hemisphere is dominant or if there is lack of the usual L-sided dominance.[26,40]
The mechanism of lateralization for motor control is unknown. Even though a genetic basis could be possible, heritability studies have not been conclusive.[28] Interestingly, this functional segregation might be established during early development, based on the preferential encoding of low-frequency signals representing global information in the R hemisphere, as opposed to high-frequency, local information in the L hemisphere.[38,64]
The L-sided lateralization for motor control is more evident for distal as opposed to proximal tasks, independent of the performing hand. Although motor dominance can be assessed in terms of preference (hand chosen to move) and/or performance (hand most proficient at the movement), it is also evident during bimanual movements. In this case, the dominant hand usually performs distal, fine movements, whereas the nondominant hand serves proximal, postural purposes.[65,72] This pattern is concordant with clinical data suggesting that the L hemisphere is dominant for task-relevant, timing aspects of ballistic, and sequential movements, whereas the R hemisphere is dominant for processing visual and sensory-mediated mechanisms that control final limb position.[6,82]
Though dominance for more proximal and axial motor functions such as posture, balance, and locomotion is not yet well-established, it has been proposed that the R hemisphere controls limb position and posture whereas the L hemisphere controls limb trajectory.[61,82] For instance, the R inferior frontal cortex and STN have been implicated in motor inhibition through suppression of thalamocortical signals.[5] Moreover, internal or previously known stimuli appear to trigger L greater than R-sided motor processing, whereas external or novel stimuli might lead to R greater than L-sided motor processing.[31]
Hemispheric functional differences for motor control have also been observed during learning. The progressive development of “motor expertise” has been associated with a transition from externally to internally generated movement control, along with a shift from R to L hemispheric activation. This phenomenon might be produced by a progressive reduction in the monitoring of global, spatial, and external features, as well as an increased representation of the local, internal motor program with learning.[15,73]
Even though locomotion is considered symmetric, functional gait asymmetries have been observed in normal humans.[59] In fact, normal stride length appears to be longer with the R foot. A possible explanation is that the R leg has greater muscle power and dominates gait propulsion, whereas the L leg has greater power absorption and dominates postural stabilization.[59,60] Therefore, functional gait asymmetry might be associated with the previously mentioned hemispheric asymmetries for motor control. Nevertheless, leg muscle asymmetries might be predominant and thus the origin of gait asymmetry is still controversial.[59,60]
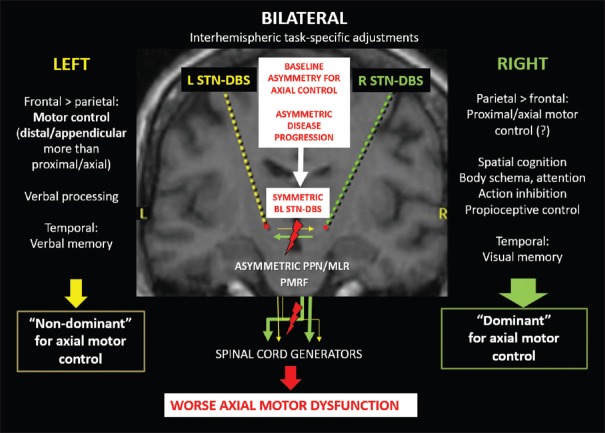
Because the functions preferentially carried out by the R hemisphere (visuospatial orientation, action inhibition, posture) are indispensable for movement,[5,64,65,72] it has also been proposed that hemispheric lateralization of motor control is a dynamic, “interhemispheric” process during which the functional involvement of both hemispheres can adapt to the type and complexity of the task being performed, as well as to the neurological and attentional status of the performer [Figure 1].[6,64] For instance, recent studies in patients with longstanding callosotomies replicated the classic finding that each hemisphere processes sensory information independently, as seen in the acute phase, but also found that the outcomes of those perceptual processes can be unified in one consciousness, regardless of the type and laterality of the response (verbal, L hand, or R hand).[55] Remarkably, these patients have less difficulties than normal controls in simultaneously producing bimanual movements with different directions.[25]
Figure 1.
Graphic representation of the possible contributions of symmetric bilateral subthalamic stimulation to axial motor deterioration in the context of asymmetric circuits for axial motor control and Parkinson's disease progression. (L: left, R: right, BL: bilateral, PPN/MLR: pedunculopontine nucleus/mesencephalic locomotor region, PMRF: pontomedullary reticular formation)
LATERALIZATION OF MOTOR CONTROL IN PARKINSON'S DISEASE
Disease processes such as PD can also produce lateralized dysfunction. In fact, dopaminergic denervation of the striatum in PD begins asymmetrically and gradually becomes BL with disease progression.[37] As a consequence, appendicular motor dysfunction (bradykinesia, tremor, rigidity) usually begins contralateral to the most affected nigrostriatal pathway and later spreads to the opposite side. The cause of this phenomenon is unknown, but there is extensive evidence from clinical, radiological, and pathological studies supporting this initial asymmetry in PD, which can be maintained over the years despite disease progression.[10,14,39,81] Even though there is limited evidence, an underlying asymmetry of nigrostriatal pathways associated with motor control dominance could be responsible for or at least contribute to the initial asymmetry in PD.[30,41] For instance, the degree of R-handedness was found to increase with L putamen dopaminergic dominance.[14] In the same study, bimanual dexterity in R-handed people with and without PD correlated better with R caudate dominance. Therefore, bimanual movements might depend upon simultaneous L putaminal activation of L hemispheric motor circuits and R caudate inhibition of R-sided circuits.[14]
There is also evidence supporting lateralization of axial motor dysfunction in PD, which includes dysarthria, dysphagia, FOG, and PIGD.[11,12,13,23,29] Even though there is conflicting data,[33] PD patients with L-sided predominant appendicular symptoms at onset have been found to be at higher risk of developing FOG in a large cohort of 250 patients (hazard ratio 1.55).[29] This suggests that R-hemisphere predominant PD is associated with more frequent and earlier derangement of gait control. Interestingly, specific lack of gait coordination and symmetry might be more important than motor control asymmetry for FOG in PD.[56] Given that normal stride length appears to be longer with the R foot,[59,60] L-sided predominant PD might make this normal asymmetry more exaggerated by reducing stride length with the L foot. This asymmetry might then explain the higher risk for FOG in L-sided predominant PD.
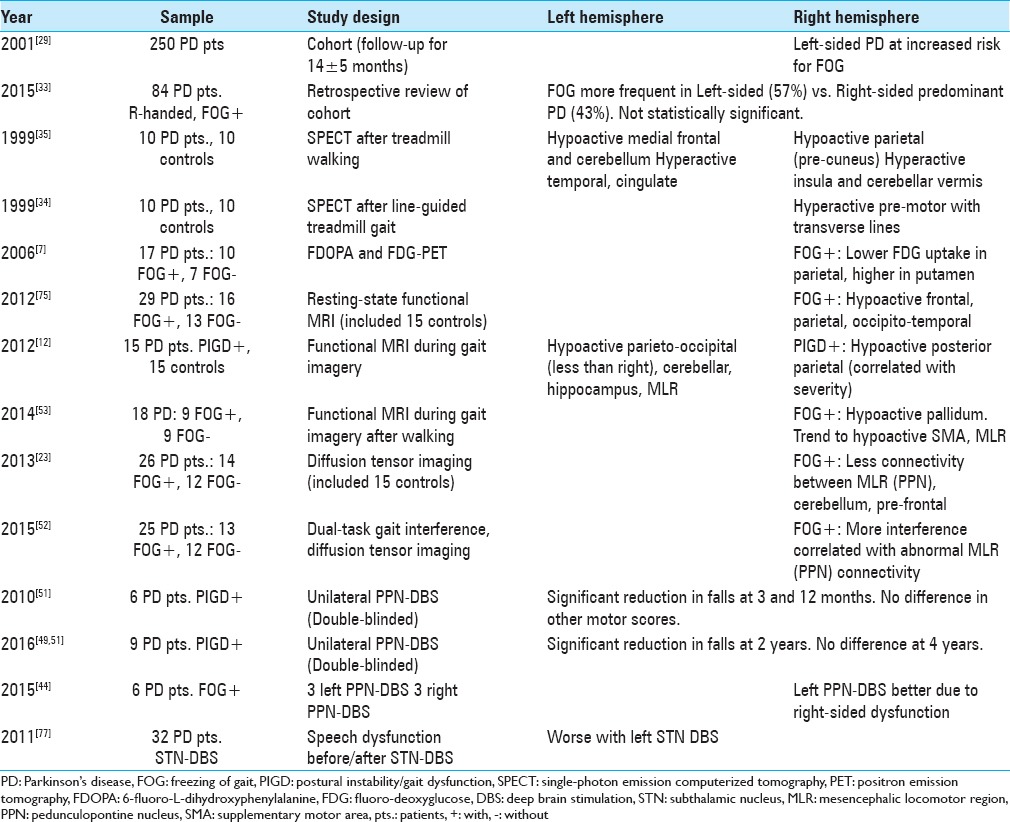
Patients with PD and FOG also appear to have abnormally reduced structural connectivity on diffusion tensor imaging (DTI) and functional MRI (fMRI) signals preferentially affecting R-sided motor circuits during gait imagery tasks.[12,23,52,53] In these patients, hypoactive fMRI signals were seen within the BL parieto-occipital, L posterior hippocampal, L cerebellar, and L mesencephalic regions, including the pedunculopontine nucleus/mesencephalic locomotor region (PPN/MLR). Within this network, decreased activation of the R posterior parietal cortex strongly correlated with the severity of gait disturbances.[12] In another fMRI study of patients with PD and FOG, gait imagery of quiet standing, simple forward walking, and complex locomotor tasks showed significantly lower signals in the R pallidum and trends towards lower signals in other R hemisphere regions involved with locomotion (supplementary motor area, PPN/MLR).[52,53] These abnormalities within the R hemisphere consistently involve the PPN/MLR, and the executive-attention network including prefrontal and parietal regions.[12,23,52,53] A previous single-photon emission CT study also reported that treadmill gait-induced cerebral activity in PD remained low in the R precuneus of the superior parietal lobe when compared to controls.[35] Walking guided by transverse lines increased activation of posterior parietal and cerebellar regions in these PD patients, with greater activation of the R premotor area.[34] In addition, decreased resting-state activity in the R parietal cortex in PD patients with FOG has been described with positron emission tomography.[7] These data, along with other studies that specifically implicate R hemispheric alterations in subjects with PD and FOG,[8,75] suggest that axial dysfunction in PD is associated with abnormalities of R greater than L hemispheric circuits involved in locomotion [Table 1]. Despite imaging studies being unable to distinguish between excitatory or inhibitory circuits, these findings are concordant with the previously reviewed data pointing towards a possible R-sided hemispheric dominance for axial motor control in humans.[15,32,61,73,82]
Table 1.
Evidence for lateralization of axial dysfunction in patients with Parkinson's disease
NEUROMODULATION OF LATERALIZED MOTOR CIRCUITS IN PARKINSON'S DISEASE
Dopaminergic agents can improve appendicular symptoms in PD; however, they can also produce motor fluctuations and/or dyskinesias over time. Once these complications develop, BL STN-DBS has emerged as a very effective and relatively safe treatment modality for these motor complications. It is especially effective in controlling appendicular symptoms in PD.[16,43,50] Yet, worsening of axial symptoms after BL STN-DBS can occur in almost 20% of patients in the year following implantation.[19,21,69,77,78]
The widespread BL as opposed to UL strategy for initial implantation of the STN is based on limited evidence. Identical DBS of potentially lateralized motor circuits might be unnecessary in all patients and could even contribute to the axial motor deterioration observed in some of them.[20,47,69,77] Also, although BL STN-DBS is relatively safe, it might carry higher costs and more peri- and postoperative complications such as confusion and cognitive decline when compared to UL procedures.[4,24,36,54] For instance, a recent study suggests that there is higher location variability of the second implanted DBS electrode during BL procedures due to multiple factors, such as brain shift caused by air penetration and/or CSF outflow caused by the first skull penetration. This higher variability was associated with lower threshold for side effects and was predictive of motor outcomes at 1 year.[62] Though there have not been head-to-head comparative trials, a common argument is that BL STN-DBS would allow for greater reduction in dopaminergic medication doses and subsequent improvement in dyskinesia, whereas UL implantation would not permit a similar reduction in medication due to uncontrolled worsening of symptoms on the side contralateral to the nonimplanted hemisphere.
Worsening of axial dysfunction after BL STN-DBS has been attributed to the variable combination of disease progression beyond dopaminergic systems and the unwanted spread of electrical fields beyond the STN.[22,43,76,77] More recently, interference of BL STN-DBS with potentially asymmetric circuits underlying interlimb coordination during locomotion has been suggested as a cause of FOG.[20] Equal stimulation of these asymmetric motor circuits could cause overstimulation of one hemisphere and/or understimulation of the other hemisphere [Figure 1]. For instance, it has been observed that overstimulation and subsequent extension of the electric field can produce complications such as hypokinesia and FOG, particularly with anteromedial and dorsal spread from the STN.[22,76] Furthermore, overstimulation contralateral to the most affected hemibody can impair gait despite improving appendicular symptoms.[20,47] In fact, reducing the amplitude of DBS contralateral to the side with the longer stride length improves FOG through normalization of coordination.[20] These improvements could be associated with the reduction of gait asymmetry initially increased by symmetric BL STN-DBS.[56,59,60]
Interestingly, different patterns of local field potentials in motor networks have been associated with axial and appendicular symptoms. For instance, PIGD has been associated with decreased beta and increased gamma and alpha/theta bands. In contrast, bradykinesia has been associated with increased beta frequencies.[67] Consequently, DBS could improve bradykinesia but worsen PIGD by decreasing beta activity in these motor circuits. Finally, some studies have suggested that decreasing DBS frequency to 60–80 Hz could ameliorate PIGD in PD after BL STN-DBS (usually programmed with BL frequencies higher than 100 Hz). Bilateral “low-frequency” STN-DBS could be useful for patients who develop side effects associated with “high-frequency” BL STN-DBS, including axial motor dysfunction.[17,47,84] The asymmetric programming of DBS frequencies might also become a therapeutic option for these patients with the availability of new DBS technology.
In addition to PIGD, speech dysfunction can also be accelerated after BL STN-DBS in PD.[19,76] Interestingly, it has been observed that patients who have a medially-displaced and/or high-voltage DBS electrode over the L hemisphere are at a higher risk for speech deterioration in the year following BL STN-DBS surgery.[76] This side effect could be associated with overstimulation of L-sided dominant circuits associated with verbal control.[65]
In contrast to medications, DBS provides the opportunity to modify some stimulation parameters separately for each cerebral hemisphere. In some patients, both appendicular and axial motor improvements achieved with UL and BL STN-DBS are similar.[11,71,79] Several studies have shown that UL STN-DBS can improve motor scores by 20–40% when compared to preoperative scores.[9,27,42,46,68] This motor improvement with UL STN-DBS is mostly related to benefits on the contralateral hemibody, although ipsilateral effects have also been reported.[1,2,3,66,68,74,79] Interestingly, approximately 50% of patients with PD undergoing BL STN-DBS have been found to have a “dominant” STN. This phenomenon was predicted by longer disease duration and tremor predominance.[11] Moreover, basal ganglia phase synchronization studies provide evidence for the existence of interhemispheric networks with lateralized dominant regions. In one of these studies, unilateral motor tasks performed by 4 PD patients with BL STN-DBS led to synchronization of alpha oscillations in both STN. These BL STN alpha oscillations were phase synchronized across hemispheres at the onset of movement, with a flow of synchronization always directed from the R to the L STN, regardless of which side performed the motor task.[13] Finally, UL STN-DBS has been shown to activate BL basal ganglia networks, which is also irrespective of the side of the body that performs the movement.[80] Therefore, optimized neuromodulation of UL “dominant” motor circuits might be able to activate BL networks and ameliorate symptoms bilaterally.
Based on the asymmetry of appendicular motor symptoms in PD, several studies support an initial UL as opposed to BL approach to STN-DBS in some patients [Table 2].[45,71,74,79,80] In a prospective study that followed 82 patients after UL STN-DBS contralateral to the most affected hemibody, only 34% of the patients required contralateral implantation in the following 2 years. Predictors of the need for contralateral DBS were symmetric appendicular motor symptoms, high tremor subscore, and low body weight.[71] Given that motor asymmetry in PD is more pronounced early in the disease, UL implantation might become more frequent in the setting of the recent FDA approval of DBS for earlier PD based on the results of the EARLY-STIM trial.[63]
Table 2.
Results of asymmetric neuromodulation with subthalamic DBS in Parkinson's disease
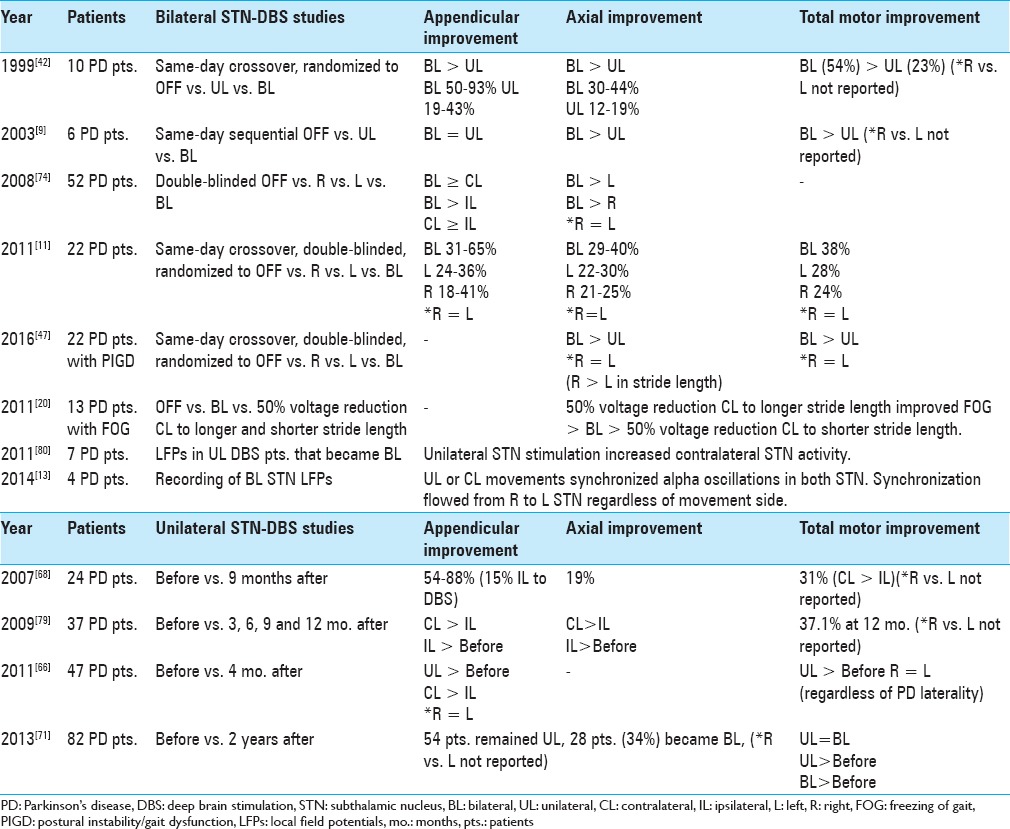
Previous studies have suggested that UL and BL DBS can produce similar effects on axial symptoms in PD; however, BL stimulation appears to yield the maximal benefits.[9,11,42,45,47,74] Given the extensive BL connections of the PPN/MLR, UL PPN-DBS might be enough to produce bilateral effects, and in fact it has been shown to improve PIGD early after implantation in PD.[48,51,70] Though L vs. R differences were not studied, L PPN-DBS yielded greater improvement in axial symptoms in a small sample.[44] The differential effects of R-sided, L-sided, and BL STN-DBS in the context of potentially lateralized axial motor circuits have not been systematically studied. In a recent pilot study of patients with PD who developed axial motor dysfunction after BL STN-DBS,[47] stride length improved by 5 cm more during R versus L STN-DBS and by 7 cm more during BL versus L STN-DBS. The 2-cm difference in favor of BL versus R STN-DBS was not significant. Other gait parameters such as stride velocity and turning time were similar among BL and both UL STN-DBS conditions; however, motor and gait UPDRS scores improved more with BL versus UL STN-DBS. The differences persisted after controlling for asymmetric PD symptoms. These data are consistent with the theory of R-hemispheric dominance for locomotion and other axial functions.
Given the established efficacy of BL STN-DBS and the significant contribution of axial dysfunction to morbidity and mortality in PD patients, it is paramount to identify patients whose axial dysfunction could worsen with BL as opposed to UL or individualized asymmetric programming of BL STN-DBS. A comprehensive presurgical assessment of DBS candidates that includes evaluation of motor lateralization could identify patients who would benefit from an initial UL as opposed to BL DBS paradigm based on both appendicular, axial, and possibly nonmotor symptoms. Although contralateral implantation might be required with disease progression, the initial UL approach could be maintained by asymmetric programming of DBS parameters for each hemisphere (e.g., voltage).[20,47] This asymmetric programming could avoid unnecessary stimulation while maximizing the benefits of BL STN-DBS in appendicular dysfunction [Table 2; Figure 1].
CONCLUSIONS
Whereas the L hemisphere appears to be dominant for appendicular movements, there is growing evidence supporting R hemispheric dominance for axial motor control. Recently, theories involving complex interhemispheric relationships are attempting to unify the established models of hemispheric lateralization. In PD, BL STN-DBS is an established treatment modality that can significantly improve appendicular symptoms. Given the usually persistent asymmetry of appendicular symptoms in PD, some patients benefit from an asymmetric approach favoring DBS of the STN contralateral to the worse symptomatic side. Axial symptoms are still a significant contributor to disability, morbidity, and mortality in PD. These symptoms might not respond and can even worsen with BL STN-DBS. The comparative effects of UL or asymmetric programming of BL STN-DBS for axial symptoms have not yet been systematically evaluated, although data consistent with R-sided hemispheric dominance for axial control suggests that both UL and BL STN-DBS could produce similar effects. Thus, an asymmetric approach to STN-DBS implantation or programming could also be considered in PD patients with predominant axial dysfunction to avoid over- or understimulation of potentially asymmetric circuits. The availability of new DBS technology could facilitate the design of individualized asymmetric stimulation parameters that minimize axial impairment while maintaining appendicular symptom control.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Karlo J. Lizarraga, Email: karlo.lizarraga@uhnresearch.ca.
Corneliu C. Luca, Email: cluca@med.miami.edu.
Antonio De Salles, Email: a.desalles@yahoo.com.
Alessandra Gorgulho, Email: a_gorgulho@yahoo.com.
Anthony E. Lang, Email: anthony.lang@uhnresearch.ca.
Alfonso Fasano, Email: alfonso.fasano@uhn.ca.
REFERENCES
- 1.Agostino R, Dinapoli L, Modugno N, Iezzi E, Gregori B, Esposito V, et al. Ipsilateral sequential arm movements after unilateral subthalamic deep-brain stimulation in patients with Parkinson's disease. Mov Disord. 2008;23:1718–24. doi: 10.1002/mds.22203. [DOI] [PubMed] [Google Scholar]
- 2.Alberts JL, Hass CJ, Vitek JL, Okun MS. Are two leads better than one: An emerging case for unilateral subthalamic deep brain stimulation in Parkinson's disease. Exp Neurol. 2008;214:1–5. doi: 10.1016/j.expneurol.2008.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alberts JL, Okun MS, Vitek JL. The persistent effects of unilateral pallidal and subthalamic deep brain stimulation on force control in advanced Parkinson's patients. Parkinsonism Relat Disord. 2008;14:481–8. doi: 10.1016/j.parkreldis.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alberts JL, Voelcker-Rehage C, Hallahan K, Vitek M, Bamzai R, Vitek JL. Bilateral subthalamic stimulation impairs cognitive-motor performance in Parkinson's disease patients. Brain. 2008;131(Pt 12):3348–60. doi: 10.1093/brain/awn238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aron AR, Poldrack RA. Cortical and subcortical contributions to Stop signal response inhibition: Role of the subthalamic nucleus. J Neurosci. 2006;26:2424–33. doi: 10.1523/JNEUROSCI.4682-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bagesteiro LB, Sainburg RL. Nondominant arm advantages in load compensation during rapid elbow joint movements. J Neurophysiol. 2003;90:1503–13. doi: 10.1152/jn.00189.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bartels AL, de Jong BM, Giladi N, Schaafsma JD, Maguire RP, Veenma L, et al. Striatal dopa and glucose metabolism in PD patients with freezing of gait. Mov Disord. 2006;21:1326–32. doi: 10.1002/mds.20952. [DOI] [PubMed] [Google Scholar]
- 8.Bartels AL, Leenders KL. Brain imaging in patients with freezing of gait. Mov Disord. 2008;23(Suppl 2):S461–7. doi: 10.1002/mds.21912. [DOI] [PubMed] [Google Scholar]
- 9.Bastian AJ, Kelly VE, Revilla FJ, Perlmutter JS, Mink JW. Different effects of unilateral versus bilateral subthalamic nucleus stimulation on walking and reaching in Parkinson's disease. Mov Disord. 2003;18:1000–7. doi: 10.1002/mds.10493. [DOI] [PubMed] [Google Scholar]
- 10.Brooks DJ. Morphological and functional imaging studies on the diagnosis and progression of Parkinson's disease. J Neurol. 2000;247(Suppl 2):II11–8. doi: 10.1007/pl00007755. [DOI] [PubMed] [Google Scholar]
- 11.Castrioto A, Meaney C, Hamani C, Mazzella F, Poon YY, Lozano AM, et al. The dominant-STN phenomenon in bilateral STN DBS for Parkinson's disease. Neurobiol Dis. 2011;41:131–7. doi: 10.1016/j.nbd.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 12.Cremers J, D’Ostilio K, Stamatakis J, Delvaux V, Garraux G. Brain activation pattern related to gait disturbances in Parkinson's disease. Mov Disord. 2012;27:1498–505. doi: 10.1002/mds.25139. [DOI] [PubMed] [Google Scholar]
- 13.Darvas F, Hebb AO. Task specific inter-hemispheric coupling in human subthalamic nuclei. Front Hum Neurosci. 2014;8:701. doi: 10.3389/fnhum.2014.00701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de la Fuente-Fernandez R, Kishore A, Calne DB, Ruth TJ, Stoessl AJ. Nigrostriatal dopamine system and motor lateralization. Behav Brain Res. 2000;112:63–8. doi: 10.1016/s0166-4328(00)00165-0. [DOI] [PubMed] [Google Scholar]
- 15.Debaere F, Wenderoth N, Sunaert S, Van Hecke P, Swinnen SP. Changes in brain activation during the acquisition of a new bimanual coordination task. Neuropsychologia. 2004;42:855–67. doi: 10.1016/j.neuropsychologia.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Deuschl G, Schade-Brittinger C, Krack P, Volkmann J, Schafer H, Botzel K, et al. A randomized trial of deep-brain stimulation for Parkinson's disease. N Engl J Med. 2006;355:896–908. doi: 10.1056/NEJMoa060281. [DOI] [PubMed] [Google Scholar]
- 17.di Biase L, Fasano A. Low-frequency deep brain stimulation for Parkinson's disease: Great expectation or false hope? Mov Disord. 2016;31:962–7. doi: 10.1002/mds.26658. [DOI] [PubMed] [Google Scholar]
- 18.Dorsey ER, Constantinescu R, Thompson JP, Biglan KM, Holloway RG, Kieburtz K, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68:384–6. doi: 10.1212/01.wnl.0000247740.47667.03. [DOI] [PubMed] [Google Scholar]
- 19.Fasano A, Aquino CC, Krauss JK, Honey CR, Bloem BR. Axial disability and deep brain stimulation in patients with Parkinson disease. Nat Rev Neurol. 2015;11:98–110. doi: 10.1038/nrneurol.2014.252. [DOI] [PubMed] [Google Scholar]
- 20.Fasano A, Herzog J, Seifert E, Stolze H, Falk D, Reese R, et al. Modulation of gait coordination by subthalamic stimulation improves freezing of gait. Mov Disord. 2011;26:844–51. doi: 10.1002/mds.23583. [DOI] [PubMed] [Google Scholar]
- 21.Ferraye MU, Debu B, Fraix V, Xie-Brustolin J, Chabardes S, Krack P, et al. Effects of subthalamic nucleus stimulation and levodopa on freezing of gait in Parkinson disease. Neurology. 2008;70(16 Pt 2):1431–7. doi: 10.1212/01.wnl.0000310416.90757.85. [DOI] [PubMed] [Google Scholar]
- 22.Fleury V, Pollak P, Gere J, Tommasi G, Romito L, Combescure C, et al. Subthalamic stimulation may inhibit the beneficial effects of levodopa on akinesia and gait. Mov Disord. 2016;31:1389–97. doi: 10.1002/mds.26545. [DOI] [PubMed] [Google Scholar]
- 23.Fling BW, Cohen RG, Mancini M, Nutt JG, Fair DA, Horak FB. Asymmetric pedunculopontine network connectivity in parkinsonian patients with freezing of gait. Brain. 2013;136(Pt 8):2405–18. doi: 10.1093/brain/awt172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frank MJ, Samanta J, Moustafa AA, Sherman SJ. Hold your horses: Impulsivity, deep brain stimulation, and medication in parkinsonism. Science. 2007;318:1309–12. doi: 10.1126/science.1146157. [DOI] [PubMed] [Google Scholar]
- 25.Franz EA, Eliassen JC, Ivry RB, Gazzaniga MS. Dissociation of spatial and temporal coupling in the bimanual movements of callosotomy patients. Psychol Sci. 1996;7:306–10. [Google Scholar]
- 26.Galaburda AM, LeMay M, Kemper TL, Geschwind N. Right-left asymmetries in the brain. Science. 1978;199:852–6. doi: 10.1126/science.341314. [DOI] [PubMed] [Google Scholar]
- 27.Germano IM, Gracies JM, Weisz DJ, Tse W, Koller WC, Olanow CW. Unilateral stimulation of the subthalamic nucleus in Parkinson disease: A double-blind 12-month evaluation study. J Neurosurg. 2004;101:36–42. doi: 10.3171/jns.2004.101.1.0036. [DOI] [PubMed] [Google Scholar]
- 28.Geschwind N, Galaburda AM. Cerebral lateralization: Biological mechanisms, associations and pathology. Cambridge (MA): MIT Press; 1987. [DOI] [PubMed] [Google Scholar]
- 29.Giladi N, McDermott MP, Fahn S, Przedborski S, Jankovic J, Stern M, et al. Freezing of gait in PD: Prospective assessment in the DATATOP cohort. Neurology. 2001;56:1712–21. doi: 10.1212/wnl.56.12.1712. [DOI] [PubMed] [Google Scholar]
- 30.Glick SD, Ross DA, Hough LB. Lateral asymmetry of neurotransmitters in human brain. Brain Res. 1982;234:53–63. doi: 10.1016/0006-8993(82)90472-3. [DOI] [PubMed] [Google Scholar]
- 31.Goble DJ, Brown SH. The biological and behavioral basis of upper limb asymmetries in sensorimotor performance. Neurosci Biobehav Rev. 2008;32:598–610. doi: 10.1016/j.neubiorev.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 32.Goldberg E, Podell K, Lovell M. Lateralization of frontal lobe functions and cognitive novelty. J Neuropsychiatry Clin Neurosci. 1994;6:371–8. doi: 10.1176/jnp.6.4.371. [DOI] [PubMed] [Google Scholar]
- 33.Hall JM, Gilat M, Lewis SJ, Shine JM. Does dominant pedunculopontine nucleus exist? Probably not. Brain. 2015;138(Pt 5):e346. doi: 10.1093/brain/awu315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hanakawa T, Fukuyama H, Katsumi Y, Honda M, Shibasaki H. Enhanced lateral premotor activity during paradoxical gait in Parkinson's disease. Ann Neurol. 1999;45:329–36. doi: 10.1002/1531-8249(199903)45:3<329::aid-ana8>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 35.Hanakawa T, Katsumi Y, Fukuyama H, Honda M, Hayashi T, Kimura J, et al. Mechanisms underlying gait disturbance in Parkinson's disease: A single photon emission computed tomography study. Brain. 1999;122(Pt 7):1271–82. doi: 10.1093/brain/122.7.1271. [DOI] [PubMed] [Google Scholar]
- 36.Hershey T, Revilla FJ, Wernle A, Gibson PS, Dowling JL, Perlmutter JS. Stimulation of STN impairs aspects of cognitive control in PD. Neurology. 2004;62:1110–4. doi: 10.1212/01.wnl.0000118202.19098.10. [DOI] [PubMed] [Google Scholar]
- 37.Hornykiewicz O. Dopamine (3-hydroxytyramine) and brain function. Pharmacol Rev. 1966;18:925–64. [PubMed] [Google Scholar]
- 38.Ivry RB, Roberson LC. The Two Sides of Perception. Cambridge (MA): MIT Press; 1998. [Google Scholar]
- 39.Kempster PA, Gibb WR, Stern GM, Lees AJ. Asymmetry of substantia nigra neuronal loss in Parkinson's disease and its relevance to the mechanism of levodopa related motor fluctuations. J Neurol Neurosurg Psychiatry. 1989;52:72–6. doi: 10.1136/jnnp.52.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim SG, Ashe J, Hendrich K, Ellerman JM, Merkle H, Ugurbil K, et al. Functional magnetic resonance imaging of motor cortex: Hemispheric asymmetry and handedness. Science. 1993;261:615–7. doi: 10.1126/science.8342027. [DOI] [PubMed] [Google Scholar]
- 41.Kooistra CA, Heilman KM. Motor dominance and lateral asymmetry of the globus pallidus. Neurology. 1988;38:388–90. doi: 10.1212/wnl.38.3.388. [DOI] [PubMed] [Google Scholar]
- 42.Kumar R, Lozano AM, Sime E, Halket E, Lang AE. Comparative effects of unilateral and bilateral subthalamic nucleus deep brain stimulation. Neurology. 1999;53:561–6. doi: 10.1212/wnl.53.3.561. [DOI] [PubMed] [Google Scholar]
- 43.Krack P, Batir A, Van Blercom N, Chabardes S, Fraix V, Ardouin C, et al. Five-year follow-up of bilateral stimulation of the subthalamic nucleus in advanced Parkinson's disease. N Engl J Med. 2003;349:1925–34. doi: 10.1056/NEJMoa035275. [DOI] [PubMed] [Google Scholar]
- 44.Lam S, Moro E, Poon YY, Lozano AM, Fasano A. Does dominant pedunculopontine nucleus exist? Brain. 2015;138(Pt 2):e323. doi: 10.1093/brain/awu225. [DOI] [PubMed] [Google Scholar]
- 45.Liang J, Hu X, Zhou X, Jiang X, Cao Y, Wang L, et al. Five-year follow-up of 23 asymmetrical Parkinson's disease patients treated with unilateral subthalamic nucleus stimulation. Neural Regen Res. 2012;7:1428–35. doi: 10.3969/j.issn.1673-5374.2012.18.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Linazasoro G, Van Blercom N, Lasa A. Unilateral subthalamic deep brain stimulation in advanced Parkinson's disease. Mov Disord. 2003;18:713–6. doi: 10.1002/mds.10407. [DOI] [PubMed] [Google Scholar]
- 47.Lizarraga KJ, Jagid JR, Luca CC. Comparative effects of unilateral and bilateral subthalamic nucleus deep brain stimulation on gait kinematics in Parkinson's disease: A randomized, blinded study. J Neurol. 2016;263:1652–6. doi: 10.1007/s00415-016-8191-3. [DOI] [PubMed] [Google Scholar]
- 48.Mestre TA, Sidiropoulos C, Hamani C, Poon YY, Lozano AM, Lang AE, et al. Long-term double-blinded unilateral pedunculopontine area stimulation in Parkinson's disease. Mov Disord. 2016;31:1570–4. doi: 10.1002/mds.26710. [DOI] [PubMed] [Google Scholar]
- 49.Moreau C, Defebvre L, Destee A, Bleuse S, Clement F, Blatt JL, et al. STN-DBS frequency effects on freezing of gait in advanced Parkinson disease. Neurology. 2008;71:80–4. doi: 10.1212/01.wnl.0000303972.16279.46. [DOI] [PubMed] [Google Scholar]
- 50.Moro E, Scerrati M, Romito LM, Roselli R, Tonali P, Albanese A. Chronic subthalamic nucleus stimulation reduced medication requirements in Parkinson's disease. Neurology. 1999;53:85–90. doi: 10.1212/wnl.53.1.85. [DOI] [PubMed] [Google Scholar]
- 51.Moro E, Hamani C, Poon YY, Al Khairallah T, Dostrovsky JO, Hutchinson WD, et al. Unilateral pedunculopontine stimulation improves falls in Parkinson's disease. Brain. 2010;133(Pt 1):215–24. doi: 10.1093/brain/awp261. [DOI] [PubMed] [Google Scholar]
- 52.Peterson DS, Fling BW, Mancini M, Cohen RG, Nutt JG, Horak FB. Dual-task interference and brain structural connectivity in people with Parkinson's disease who freeze. J Neurol Neurosurg Psychiatry. 2015;86:786–92. doi: 10.1136/jnnp-2014-308840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peterson DS, Pickett KA, Duncan R, Perlmutter J, Earhart GM. Gait-related brain activity in people with Parkinson disease with freezing of gait. PLoS One. 2014;9:e90634. doi: 10.1371/journal.pone.0090634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Petraglia FW, 3rd, Farber SH, Han JL, Verla T, Gallis J, Lokhnygina Y, et al. Comparison of Bilateral vs. Staged Unilateral Deep Brain Stimulation (DBS) in Parkinson's Disease in Patients Under 70 Years of Age. Neuromodulation. 2016;19:31–7. doi: 10.1111/ner.12351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pinto Y, Neville DA, Otten M, Corballis PM, Lamme VA, de Haan EH, et al. Split brain: Divided perception but undivided consciousness. Brain. 2017 doi: 10.1093/brain/aww358. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 56.Plotnik M, Giladi N, Balash Y, Peretz C, Hausdorff JM. Is freezing of gait in Parkinson's disease related to asymmetric motor function? Ann Neurol. 2005;57:656–63. doi: 10.1002/ana.20452. [DOI] [PubMed] [Google Scholar]
- 57.Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson's disease: A systematic review and meta-analysis. Mov Disord. 2014;29:1583–90. doi: 10.1002/mds.25945. [DOI] [PubMed] [Google Scholar]
- 58.Rossi A, Berger K, Chen H, Leslie D, Mailman RB, Huang X. Projection of the prevalence of Parkinson's disease in the coming decades: Revisited. Mov Disord. 2017 doi: 10.1002/mds.27063. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sadeghi H, Allard P, Prince F, Labelle H. Symmetry and limb dominance in able-bodied gait: A review. Gait Posture. 2000;12:34–45. doi: 10.1016/s0966-6362(00)00070-9. [DOI] [PubMed] [Google Scholar]
- 60.Sadeghi H. Local or global asymmetry in gait of people without impairments. Gait Posture. 2003;17:197–204. doi: 10.1016/s0966-6362(02)00089-9. [DOI] [PubMed] [Google Scholar]
- 61.Sainburg RL. Evidence for a dynamic-dominance hypothesis of handedness. Exp Brain Res. 2002;142:241–58. doi: 10.1007/s00221-001-0913-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sammartino F, Krishna V, King NK, Bruno V, Kalia S, Hodaie M, et al. Sequence of electrode implantation and outcome of deep brain stimulation for Parkinson's disease. J Neurol Neurosurg Psychiatry. 2016;87:859–63. doi: 10.1136/jnnp-2015-311426. [DOI] [PubMed] [Google Scholar]
- 63.Schuepbach WM, Rau J, Knudsen K, Volkmann J, Krack P, Timmermann L, et al. Neurostimulation for Parkinson's disease with early motor complications. N Engl J Med. 2013;368:610–22. doi: 10.1056/NEJMoa1205158. [DOI] [PubMed] [Google Scholar]
- 64.Sergent J. The cerebral balance of power: Confrontation or cooperation? J Exp Psychol Hum Percept Perform. 1982;8:253–72. doi: 10.1037//0096-1523.8.2.253. [DOI] [PubMed] [Google Scholar]
- 65.Serrien DJ, Ivry RB, Swinnen SP. Dynamics of hemispheric specialization and integration in the context of motor control. Nat Rev Neurosci. 2006;7:160–6. doi: 10.1038/nrn1849. [DOI] [PubMed] [Google Scholar]
- 66.Shemisa K, Hass CJ, Foote KD, Okun MS, Wu SS, Jacobson CE, et al. Unilateral deep brain stimulation surgery in Parkinson's disease improves ipsilateral symptoms regardless of laterality. Parkinsonism Relat Disord. 2011;17:745–8. doi: 10.1016/j.parkreldis.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Singh A, Kammermeier S, Plate A, Mehrkens JH, Ilmberger J, Botzel K. Pattern of local field potential activity in the globus pallidus internum of dystonic patients during walking on a treadmill. Exp Neurol. 2011;232:162–7. doi: 10.1016/j.expneurol.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 68.Slowinski JL, Putzke JD, Uitti RJ, Lucas JA, Turk MF, Kall BA, et al. Unilateral deep brain stimulation of the subthalamic nucleus for Parkinson disease. J Neurosurg. 2007;106:626–32. doi: 10.3171/jns.2007.106.4.626. [DOI] [PubMed] [Google Scholar]
- 69.St. George RJ, Nutt JG, Burchiel KJ, Horak FB. A meta-regression of the long-term effects of deep brain stimulation on balance and gait in PD. Neurology. 2010;75:1292–9. doi: 10.1212/WNL.0b013e3181f61329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Strafella A, Lozano AM, Ballanger B, Poon Y, Lang AE, Moro E. rCBF changes associated with PPN stimulation in a patient with Parkinson's disease: A PET study. Mov Disord. 2008;23:1051–4. doi: 10.1002/mds.22055. [DOI] [PubMed] [Google Scholar]
- 71.Sung VW, Watts RL, Schrandt CJ, Guthrie S, Wang D, Amara AW, et al. The relationship between clinical phenotype and early staged bilateral deep brain stimulation in Parkinson disease. J Neurosurg. 2013;119:1530–6. doi: 10.3171/2013.8.JNS122025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Swinnen SP, Jardin K, Meulenbroek R. Between-limb asynchronies during bimanual coordination: Effects of manual dominance and attentional cueing. Neuropsychologia. 1996;34:1203–13. doi: 10.1016/0028-3932(96)00047-4. [DOI] [PubMed] [Google Scholar]
- 73.Swinnen SP. Intermanual coordination: From behavioral principles to neural-network interactions. Nature Rev Neurosci. 2002;3:348–59. doi: 10.1038/nrn807. [DOI] [PubMed] [Google Scholar]
- 74.Tabbal SD, Ushe M, Mink JW, Revilla FJ, Wernle AR, Hong M, et al. Unilateral subthalamic nucleus stimulation has a measurable ipsilateral effect on rigidity and bradykinesia in Parkinson disease. Exp Neurol. 2008;211:234–42. doi: 10.1016/j.expneurol.2008.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tessitore A, Amboni M, Esposito F, Russo A, Picillo M, Marcuccio L, et al. Resting-state brain connectivity in patients with Parkinson's disease and freezing of gait. Parkinsonism Relat Disord. 2012;18:781–7. doi: 10.1016/j.parkreldis.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 76.Tommasi G, Lopiano L, Zibetti M, Cinquepalmi A, Fronda C, Bergamasco B, et al. Freezing and hypokinesia of gait induced by stimulation of the subthalamic region. J Neurol Sci. 2007;258:99–103. doi: 10.1016/j.jns.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 77.Tripoliti E, Zrinzo L, Martinez-Torres I, Frost E, Pinto S, Foltynie T, et al. Effects of subthalamic stimulation on speech of consecutive patients with Parkinson disease. Neurology. 2011;76:80–6. doi: 10.1212/WNL.0b013e318203e7d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.van Neunen BF, Esselink RA, Munneke M, Speelman JD, van Laar T, Bloem BR. Postoperative gait deterioration after bilateral subthalamic nucleus stimulation in Parkinson's disease. Mov Disord. 2008;23:2404–6. doi: 10.1002/mds.21986. [DOI] [PubMed] [Google Scholar]
- 79.Walker HC, Watts RL, Guthrie S, Wang D, Guthrie BL. Bilateral effects of unilateral subthalamic deep brain stimulation on Parkinson's disease at 1 year. Neurosurgery. 2009;65:302–9. doi: 10.1227/01.NEU.0000349764.34211.74. [DOI] [PubMed] [Google Scholar]
- 80.Walker HC, Watts RL, Schrandt CJ, Huang H, Guthrie SL, Guthrie BL, et al. Activation of subthalamic neurons by contralateral subthalamic deep brain stimulation in Parkinson disease. J Neurophysiol. 2011;105:1112–21. doi: 10.1152/jn.00266.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang J, Yang QX, Sun X, Vesek J, Mosher Z, Vasavada M, et al. MRI evaluation of asymmetry of nigrostriatal damage in the early stage of early-onset Parkinson's disease. Parkinsonism Relat Disord. 2015;21:590–6. doi: 10.1016/j.parkreldis.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 82.Winstein CJ, Pohl PS. Effects of unilateral brain damage on the control of goal-directed hand movements. Exp Brain Res. 1995;105:163–74. doi: 10.1007/BF00242191. [DOI] [PubMed] [Google Scholar]
- 83.Wolpert DM, Goodbody SJ, Husain M. Maintaining internal representations: The role of the human superior parietal lobe. Nat Neurosci. 1998;1:529–33. doi: 10.1038/2245. [DOI] [PubMed] [Google Scholar]
- 84.Zibetti M, Moro E, Krishna V, Sammartino F, Picillo M, Munhoz RP, et al. Low-frequency Subthalamic Stimulation in Parkinson's Disease: Long-term Outcome and Predictors. Brain Stimul. 2016;9:774–9. doi: 10.1016/j.brs.2016.04.017. [DOI] [PubMed] [Google Scholar]