Abstract
Background
Individuals with autism spectrum disorder (ASD) frequently demonstrate symptoms of attention-deficit/hyperactivity disorder (ADHD). Previous findings in children with ASD have suggested that these symptoms are associated with an impairment in executive function (EF) abilities. However, studies rarely considered this association within a single framework that controls for other related factors such as Theory of Mind (ToM) abilities and ASD symptoms.
Methods
We used structural equation modeling to explore the relations among EF, ToM, and symptoms of ASD and ADHD, using data from a population-based sample of 100 adolescents with ASD and full-scale IQ ≥ 50 (the Special Needs and Autism Project (SNAP) cohort). The study used a multi-measure and multi-informant approach, where performance of inhibition, planning, switching, and working memory tasks indexed EF and performance on tasks involving mentalizing indexed ToM. Measures of ASD and ADHD symptoms included parent and teacher reports and direct observation of the children. Shared source of symptom reporting was accounted for with a parental rating latent factor indexed by symptom measures reported by parents.
Results
Impairments in EF abilities were specifically associated with ADHD symptoms while impaired ToM was specifically associated with ASD symptoms, when accounting for the associations of each cognitive domain with the other factors. ASD and ADHD symptom latent factors were also correlated, but this association became nonsignificant once the shared source of reporting from parents was accounted for and within a model that also controlled for the correlated pathway between EF and ToM factors. The specific relations between the cognitive domains and behavioral symptoms remained even after controlling for IQ.
Conclusions
In this ASD sample, symptoms of ADHD and ASD are underpinned by separate cognitive domains. The association between EF and ToM impairments is a likely partial explanation for the co-occurrence of ADHD symptoms in ASD, but the role of shared reporting effects is also important and supports the inclusion of independent informants and objective measures in future research.
Electronic supplementary material
The online version of this article (10.1186/s13229-017-0177-1) contains supplementary material, which is available to authorized users.
Keywords: Autism spectrum disorder, Attention-deficit/hyperactivity disorder, Comorbidity, Executive function, Theory of mind, SNAP
Background
Autism spectrum disorder (ASD) is a condition affecting 1–2% children worldwide [1]. Individuals with ASD are impaired in reciprocal social communication and interaction and display various stereotyped and repetitive behaviors [2]. Many children with ASD also meet the criteria for attention-deficit/hyperactivity disorder (ADHD), with rates of approximately 30–60% in community samples [3–5] compared to 5–7% for ADHD in the general population [6]. Both ASD and ADHD are associated with highly overlapping cognitive impairments (e.g., [7–9]). Therefore, neurocognitive approaches can be useful for explaining the mechanisms underpinning the co-occurring ADHD in the ASD population [10–12].
Two disorders can co-occur beyond chance level due to artifactual or non-artifactual reasons [13, 14]. In the clinical setting, the co-occurrence of two disorders can arise due to sampling or ascertainment biases, resulting in artifactual increase of its prevalence. However, these mechanisms cannot be the sole explanation for the co-occurrence of ASD and ADHD because their high rates have been observed in population-based and epidemiological samples [3–5]. Indeed, several models of non-artifactual comorbidity of ASD and ADHD have been proposed recently [10–12, 15]. The “additivity model” is one such model [11]. The model hypothesizes that the co-occurrence of ASD and ADHD arises from separate but correlated risk factors or liabilities and results in the “additive combination of two separate nosologies” [14]. To investigate this model, neurocognitive studies typically use group comparison or factorial design, contrasting individuals with pure ASD or ADHD, combined ASD + ADHD, against those with typical development. In these studies, the pure ASD or ADHD groups are expected to demonstrate unique cognitive profiles, of which combination characterizes the cognitive performance of the ASD + ADHD group. The model thus predicts a double dissociation between the cognitive correlates of ASD and ADHD traits [14].
In the context of cognitive function, impairments of theory of mind (ToM) and executive function (EF) cognitive domains are often reported in children with ASD (e.g., [9, 16–19]). Central to ToM is the ability to mentalize, that is, to attribute mental states such as beliefs, desires, feelings, and intentions of others. Impaired ToM abilities are thought to be developmentally specific to ASD [20, 21] and have been reported to much lesser extent in ADHD (e.g., [9, 22, 23]). Often reported in both disorders are EF impairments, which are usually inferred from performance of inhibition, working memory, cognitive flexibility, and planning tasks (see e.g., [24, 25]). The impairments of EF have been reported especially in ADHD [26–28], and it is uncertain presently if executive dysfunctions truly characterize ASD. Findings of impairments across studies have been heterogeneous (e.g., [17, 29, 30]), and the performance of the EF tasks are rarely correlated with ASD symptom severity, except for between cognitive flexibility deficits and repetitive behavior (e.g., [31–34]). Evidence also suggests that EF impairments in the ASD population are associated with co-occurring ADHD traits. For instance, Corbett et al. [35] found that the inhibitory impairments among ASD children fell to trend level after excluding those with additional ADHD, while Buehler et al. [36] showed increasing motor inhibition impairments in the ASD + ADHD relative to the pure ASD group. Others have also reported increased impairments of sustained attention and working memory in the combined vs. the pure ASD group [11, 12, 15, 37, 38].
Those findings suggest dissociable relations between EF and ToM impairments and the ADHD or ASD traits among individuals with ASD [39], but there are limitations to this interpretation. Firstly, the pattern of increased executive dysfunctions in the combined relative to the pure ASD group have not been observed in every EF subdomain (e.g., in the domains of planning and cognitive flexibility [11, 40, 41]), although presumably, these subdomains have specific characteristics beyond the “common” EF [25, 42] that are unrelated to the ADHD traits. Furthermore, most studies tend to use single measures for defining symptoms of ASD and ADHD, completed typically by a single informant (e.g., parents for pediatric studies). Such approach may increase the magnitude of associations between symptom domains because of the shared source of information, in this case between, ASD and ADHD symptoms [39]. Finally, most studies have tested the links between each domain of cognition (ToM or EF) and behavioral traits in separate studies [39]. Thus, possible influences each factor might have on the relation between the other cognitive domain and behavioral traits might be obscured. Moderating influences could exert for instance through pathways between EF and ToM (e.g., [43–46]) or between the symptom domains of ASD and ADHD (e.g., [47–49]), which should be controlled within one single framework.
We explore the associations among EF, ToM, and symptom domains of ASD and ADHD and address the above challenges in the present study. In line with a recent approach [39], we investigated the dimensional relations between factors within a population-based cohort of children with ASD instead of conducting a group comparison with a factorial design. The study used a structural equation modeling (SEM) framework, enabling the constructions of the latent factors EF and ToM derived from multiple measures, and therefore controlling the specific influences of each task or cognitive subdomain. Symptoms ASD and ADHD were indexed using multiple measures collected from multiple informants including parents, teachers, and the children themselves. Using this approach, we aimed to elucidate the specific and potentially clinically significant patterns of associations among those factors within the ASD population. We hypothesized specific associations between EF impairments and increased ADHD symptoms, and between ToM impairments and increased ASD symptoms.
Methods
Participants
The Special Needs and Autism Project (SNAP) is a population-based cohort of people with ASD who were first ascertained and characterized at the age of 10–12 years (wave 1; [50]). The children received research diagnoses of ASD according to the International Classification of Diseases (ICD-10; [51]), based on the Autism Diagnostic Interview-Revised (ADI-R; [52]) parental interview, the Autism Diagnostic Observation Schedule-Generic (ADOS-G; [53]) and IQ, language, and adaptive behavior. Of the original ASD sample, N = 131 (77%) had full-scale intelligent quotient (FSIQ) ≥ 50 and were followed up at the age of 14–16 years (wave 2). Of these 131 individuals, 19 declined to take part, 11 could not be contacted and one stated interest but could not take part before the end of the study. Thus, in total, 100 adolescents (n = 9 females) participated in the current study. The children did not differ from those who did not take part, although eligible (n = 31), on baseline measures of IQ, the ADOS-G and ADI-R total scores, the Social Responsiveness Scale (SRS; [54]) total score, the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) ADHD symptom numbers, and parent- and teacher-rated hyperactivity/inattention scores on the Strengths and Difficulties Questionnaire (SDQ; [55]) (ts = .32–1.5, ps = .14–.75). The follow-up was conducted in two sessions completed on average in 29 days (SD = 36 days; range = 1–259 days) with 94 participants completing the follow-up session within 2 × SD days from the mean. Tests were divided equally between 2 days, with IQ tests reserved for the first day of testing, in case of participant drop-out. For each testing day, a task order was fixed that enabled presentation of activities to be balanced (e.g., alternating between computerized and pen and paper tasks) and accommodate any constraints (e.g., tasks with a fixed duration). Half of the participants received the tasks in reverse order with some adjustment to account for task constraints. The study was approved by the South-East London Research Ethics Committee (05/MRE01/67). Informed consent was given by the parents and by the participant if their level of understanding was sufficient.
Measures
Measures used in this study are described below and in the supplement. All measures were collected from the young people or parent/teacher over two waves of studies, when the young people were 10–16 years. The measures and timing (wave 1 or 2) are listed in Additional file 1: Table S1.
Cognitive measure
The Wechsler Abbreviated Scale of Intelligence (WASI; [56]) was chosen as a brief but reliable measure of general intellectual ability. The WASI consisted of four subtests, all contributed to an estimate of full-scale IQ (FSIQ).
ASD measures
ASD symptoms were indexed by (1) total algorithm score on the ADOS-G, (2) total algorithm score on the ADI-R, and (3) parent ratings on the SRS.
ADHD measures
ADHD symptoms were measured using (1) parent and teacher ratings on the hyperactivity domain of the SDQ, (2) parent report of inattention and hyperactivity/impulsivity symptoms frequency and their impact on everyday functioning on the Profile of Neuropsychiatric Symptoms (PONS; [57]), and (3) the number DSM-IV ADHD symptoms endorsed by parents on the Child and Adolescent Psychiatric Assessment interview (CAPA; [58]).
EF measures
The EF measures included in this study were (1) Opposite Worlds, part of the Test of Everyday Attention for Children [59] and (2) Luria Hand Game [60] as measures of inhibition; (3) Trail Making Test [61] and (4) a card sorting task [62] as measures of cognitive flexibility or switching; (5) a planning drawing task [63] as an index of planning; and (6) numbers (backward), taken from Children’s Memory Scale [64], as a measure of working memory. The measures were selected based on the ADHD literature and a previous model of EF [25, 65].
ToM measures
The ToM measures included in this study were (1) a combined False-Belief story (“The Chocolate Story”), a test of first- and second-order false-belief understanding [66, 67]; (2) Reading the Mind in the Eyes Task [68], an assessment of the ability of an individual to infer emotional state from photographic images of pairs of eyes; (3) Penny Hiding Game [69], a naturalistic nonverbal deception task; (4) Strange Stories Test [70], a verbal test consisting of short stories illustrating complex interaction involving lies, double bluffs, or persuasion; and (5) Frith-Happé Animated Triangles Task [71] that assesses spontaneous attribution of mental states towards animated geometric objects.
Analytical plan
Data preparation and descriptive analyses were undertaken in STATA 11 [72]. Raw data were reversed when necessary, so higher scores reflected greater symptoms or difficulties. Box-Cox transformations were used to normalize skewed data (Table 2), and structural equation modeling (SEM) was used to model the relations among factors. Although the data were collected over 6 years, we modeled their associations within a single cross-sectional design. The analysis was divided in four steps. In step 1, the structure of the latent factors for EF and ToM was investigated using an exploratory factor analysis (EFA) with all indicators entered, employing a Geomin rotation. An EFA was thought more suitable than a confirmatory factor analysis for two reasons: (1) the factor structures of the cognitive domains indexed by the candidate EF and ToM measures were not completely clear as the two domains are usually explored separately (e.g., [25, 73]) and (2) individual neurocognitive measures are not “process pure” [34], often involving a mixture of cognitive domains. For this reason, we contrasted one (i.e., common cognitive factor) against two-factor (i.e., EF and ToM) predictor models, of which model fits were evaluated using χ2 statistics. A two-factor structure fits the EF and ToM factors better and was chosen. To improve the “purity” of the factors, indicators that cross-loaded, for example, significantly loaded to both the EF and ToM factors, or to the factor not expected a priori, and those or with factor loadings ≤ 0.4 were excluded in the first instance.
Table 2.
Bivariate correlations among neurocognitive and symptom measures
| EF measures | ToM measures | ADHD measures | ASD measures | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
| Card sort task (1) | – | ||||||||||||||||
| Luria Hand Game (2) | .28** (.05) |
– | |||||||||||||||
| Trail making (3) | .36*** (.12) |
.26* (.11) |
– | ||||||||||||||
| Opposite Worlds (4) | .31** (.08) |
.17 (.03) |
.38*** (.28**) |
– | |||||||||||||
| Numbers (5) | .51*** (.21*) |
.35*** (.18†) |
.47*** (.21**) |
.37*** (− .20†) |
– | ||||||||||||
| Planning/drawing (6) | .36*** (.21*) |
.20† (.08) |
.17 (.05) |
.18† (.06) |
.17† (− .02) |
– | |||||||||||
| Animated triangle (7) | .33** (.12) |
.10 (.01) |
.02 (− .13) |
.14 (− .003) |
.28** (.06) |
.002 (− .13) |
– | ||||||||||
| Penny hiding game (8) | .27** (.06) |
.45*** (.36***) |
.17 (.04) |
.26* (.15) |
.30** (.12) |
.14 (.02) |
.37*** (.32**) |
– | |||||||||
| RME (9) | .22* (− .19†) |
.39*** (.25*) |
.25* (.04) |
.21* (.01) |
.39*** (.11) |
.06 (− .10) |
.41*** (.25*) |
.47*** (.37***) |
– | ||||||||
| Strange stories (10) | .29** (− .07) |
.22* (.07) |
.18 (− .07) |
.23* (.04) |
.37*** (.07) |
.25* (.14) |
.20† (− .04) |
.29** (.12) |
.29** (− .003) |
– | |||||||
| False belief (11) | .63*** (.30**) |
.53*** (.30**) |
.32** (− .01) |
.25* (− .05) |
.46*** (.05) |
.27** (.06) |
.31** (.02) |
.54*** (.44***) |
.45*** (.11) |
.43*** (.08) |
– | ||||||
| pPONS ADHD (12) | .16 (.06) |
.10 (.05) |
.21† (.16) |
.23* (.18) |
.26* (.19†) |
.21† (.17) |
.10 (.04) |
.24* (.20†) |
.11 (.02) |
.01 (− .09) |
.03 (− .13) |
– | |||||
| pDSM ADHD (13) | .27* (.19) |
.16 (.10) |
.20 (.14) |
.19 (.15) |
.25* (.19) |
.30** (.26*) |
.08 (.03) |
.10 (.04) |
.09 (− .01) |
.09 (− .005) |
.13 (− .06) |
.55*** (.54***) |
– | ||||
| pSDQ ADHD (14) | .17 (.05) |
.22* (.17) |
.31** (.24*) |
.21* (.15) |
.28** (.20†) |
.14 (.08) |
.12 (.01) |
.19† (.12) |
.25* (.16) |
.08 (− .04) |
.08 (− .10) |
.56*** (.54***) |
.46*** (.44***) |
– | |||
| tSDQ ADHD (15) | .24* (.20†) |
.28* (.24*) |
.13 (.06) |
.11 (.04) |
.31** (.33**) |
.14 (.09) |
.12 (.05) |
.30** (.27*) |
.14 (.05) |
− .14 (− .26*) |
.22* (.16) |
.41*** (.39***) |
.50*** (.48***) |
.38*** (.36**) |
– | ||
| pADI-R (16) | .18† (.10) |
.19† (.14) |
− .03 (− .16) |
− .05 (− .14) |
.05 (−.05) |
.14 (.10) |
.29** (.25*) |
.31** (.26*) |
.03 (− .07) |
.08 (.03) |
.28** (.24*) |
.16 (.14) |
.35** (.33**) |
.22* (.17) |
.25* (.23*) |
– | |
| ADOS (17) | .17† (.05) |
.27** (.20*) |
.05 (− .05) |
− .02 (− .13) |
.11 (−.02) |
.19† (.12) |
.38*** (.29**) |
.42*** (.37***) |
.33** (.29**) |
.29** (.26*) |
.36** (.24*) |
− .01 (− .06) |
− .17 (− .21†) |
− .02 (− .09) |
.14 (.12) |
.34*** (.33**) |
– |
| pSRS (18) | .17 (− .04) |
.28** (.20†) |
.27* (.11) |
.14 (.03) |
.18 (.007) |
.12 (.01) |
.15 (.03) |
.25* (.16) |
.29** (.15) |
.20† (.06) |
.20† (.05) |
.50*** (.48***) |
.36** (.32**) |
.38*** (.33**) |
.09 (.05) |
.43*** (.40***) |
.15 (.07) |
Notes. Bivariate correlation coefficients are presented, with uncorrected p values for multiple comparisons. The coefficients in brackets are partialled for FSIQ. The prefix p on the measures indicates parent reports whereas the prefix t indicates a teacher report
Abbreviations of neurocognitive measures: EF executive function, ToM Theory of Mind, RME Reading the Mind in the Eye Tasks. Abbreviations for ASD or ADHD measures: ADOS Autism Diagnostic Observation Schedule Total Score, ADI-R Autism Diagnostic Interview-Revised, SRS Social Responsiveness Scale, DSM ADHD Diagnostic and Statistical Manual of Mental Disorders ADHD symptom numbers, SDQ ADHD Strengths and Difficulties Questionnaire ADHD domain, PONS ADHD Profile of Neuropsychiatric Symptoms ADHD domain
Significant levels †p < .1, *p < .05, **p < .01, and ***p < .001
In step 2, we built the SEM model 1 (Fig. 1a) to assess the relations between the neurocognitive (ToM and EF) and behavioral (ASD and ADHD) latent factors. The model was derived from the available data collected from the young people and parent/teacher over a period of 6 years when the young people were 10–16 years, taking the assumption of ADHD and ASD symptom persistence over the time window [74–76]. The data were modeled with EF and ToM “predicting” the symptom factors. However, the aim was not to test if cognitive factors causally underpin symptom domains, but rather to understand better the pattern of associations between cognition and behavior. The EF and ToM latent factors were allowed to correlate [43, 44] as were the ASD and ADHD factors [38, 39, 47, 77]. The EFA and SEM modeling was conducted in Mplus [78].
Fig. 1.
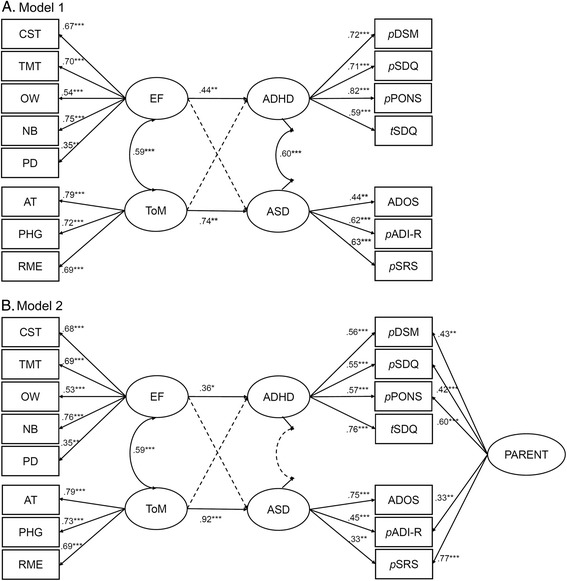
SEM models are presented here with nonsignificant paths shown on dotted lines. Nonsignificant paths in model 1 are between EF and ASD (β = − .11) and between ToM and ADHD factor (β = .07). In model 2, the nonsignificant paths are between EF and ASD (β = − .29), between ToM and ADHD (β = .16), and between ASD and ADHD (r = .03). List of abbreviations: CST card sort task, TMT Trail Making Test, OW Opposite Worlds, NB number backward, PD planning/drawing task, AT animated triangle, PHG penny hiding games, RME Reading the Mind in the Eye tasks, EF executive function, ToM theory of mind. Abbreviations for ASD or ADHD measures: ADOS Autism Diagnostic Observation Schedule, ADI-R Autism Diagnostic Interview-Revised, SRS Social Responsiveness Scale, DSM Diagnostic and Statistical Manual of Mental Disorders, SDQ Strengths and Difficulties Questionnaire, PONS Profile of Neuropsychiatric Symptoms. The prefix p on these behavioral measures indicates parent-based reports whereas the prefix t on the SDQ indicates a teacher-based report. The significant levels are *p < .05, **p < .01, and ***p < .001
Inspection of the residual covariances suggested that accounting for shared information from parents could improve model fit. Therefore, in step 3, we introduced a parental reporting latent factor to account for shared informant influences from parents (model 2; Fig. 1b). The parental latent factor was indexed by symptom measures reported by parents (i.e., excluding the ADOS and the SDQ teacher report). The final form of model 2 was derived in step 4, by systematically removing nonsignificant pathways to increase parsimony and comparing the nested models iteratively. Since many individuals with ASD and ADHD have low IQ (e.g., [79, 80]), we examined in a sensitivity analysis whether the associations among factors remained after controlling for FSIQ in model 2. The ToM, EF, ASD, and ADHD latent factors were regressed on FSIQ in step 5 (Additional file 1: Figure S1A), and the associations between the neurocognitive and symptom factors were inspected. Mindful of the possible changes of ASD or ADHD traits from childhood to adolescence, in step 6, we conducted a sensitivity analysis by modeling the data collected from the children at age 14–16 years, excluding the teacher SDQ hyperactivity domain and DSM-IV ADHD symptoms from the ADHD factor, the total ADOS-G and ADI-R scores from the ASD factor, and the parental latent factor since all behavior scores were parent-rated. In this model, ASD symptoms were indexed by the observed SRS score. The analyses were repeated excluding data from children whose experimental sessions were separated by time window larger than 2 × SD from the mean to see if the extreme testing day separation could have impacted the findings. All models were fitted by maximum likelihood with robust standard error (MLR) which provides unbiased estimates for missing data with missingness assumed at random. The model fit for nested models was evaluated using the likelihood ratio chi-square, comparative fit index (CFI), and the Tucker-Lewis Index (TLI [81]; acceptable fit for both indices ≥ .90), the root mean square error of approximation (RMSEA [82]; acceptable fit ≤ .08). The Bayesian information criterion (BIC) and the Akaike information criterion (AIC) were provided in some cases to allow comparisons of nonnested models.
Results
Descriptive statistics of measures are given in Table 1, and their bivariate correlations, with associated p values uncorrected for multiple comparisons, are in Table 2.
Table 1.
Descriptive statistics of measures
| Mean (SD) | Range | ||
|---|---|---|---|
| IQ measures | |||
| FSIQ | 84.3 (18.0) | 50–119 | |
| VIQ | 80.8 (18.0) | 55–120 | |
| PIQ | 90.4 (18.6) | 53–126 | |
| EF indicators | |||
| Card sort task (98/100)a | 7.2 (6.6) | 1–36 | |
| Luria Hand Game (97/100)b | 2.8 (3.3) | 0–15 | |
| Trail making (88/100)a | 63.4 (44.0) | 13.4–257.1 | |
| Planning/drawing (98/100)a, b | 2.4 (1.7) | 0–6 | |
| Opposite Worlds (98/100)a, b | 8.4 (7.5) | −3.7 – 47.4 | |
| Numbers (99/100)a, b | 7.3 (2.5) | 0–12 | |
| ToM indicators | |||
| RME (94/100)b | 14.0 (4.4) | 6–25 | |
| Penny hiding gameb | 2.3 (2.7) | 0–14 | |
| Strange stories (88/100)b | 4.6 (2.1) | 0–8 | |
| Animated triangle (87/100)a, b | 2.9 (0.9) | 0–4.75 | |
| False belief (99/100)b | 3.3 (2.4) | 0–8 | |
| ADHD symptom indicators | |||
| Parent SDQ hyperactivity (93/100)a | 5.8 (2.5) | 0–10 | |
| Teacher SDQ hyperactivity (85/100) | 5.5 (2.4) | 1–10 | |
| Parent PONS ADHD (89/100)a | 10.7 (6.6) | 0–27 | |
| DSM-IV ADHD symptoms (73/100) | 6.0 (3.6) | 0–14 | |
| ASD symptom indicators | |||
| Parent SRS total raw score (92/100) | 92.5 (29.3) | 21–153 | |
| ADI-R total (99/100) | 21.5 (7.7) | 5–41 | |
| ADOS total | 11.6 (6.1) | 1–27 | |
Notes. Descriptive statistics reported here are based on raw data
Abbreviations: FSIQ Full Scale IQ, VIQ Verbal IQ, PIQ Performance IQ, RME Reading the Mind in the Eye Tasks, SDQ Strengths and Difficulties Questionnaire, PONS Profile of Neuropsychiatric Symptoms, SRS Social Responsiveness Scale, ADI-R Autism Diagnostic Interview-Revised, ADOS Autism Diagnostic Observation Schedule
aBox-Cox transformed during analyses
bReversed scores on this table
Step 1: EFA of predictor factors
The EFA of the ToM and EF indicators better fitted a two-factor (χ2[34] = 49.8, p = .04; CFI = .94; TLI = .91; RMSEA = .07) than a one-factor model (χ2[44] = 81.5, p = .0005; CFI = .87; TLI = .83; RMSEA = .09; Δχ2[10] = 32.5, p < .001). ToM and EF were correlated (r = .62, p < .05). Inspection of this model revealed that several tasks cross-loaded on the “other” neurocognitive domain (Table 3). The Luria Hand Game cross-loaded on ToM (factor loading = .49) and performances on the Strange Stories and False-Belief tasks cross-loaded on EF (factor loadings = .38 and .44, respectively). As they loaded on factors not expected a priori, they were thought to be less “pure” than other indicators and were removed from the subsequent SEM model. The model of the predictors with no cross-loading indicators still fit well to a two-factor model (χ2[13] = 16.2, p = .24; CFI = .98; TLI = .95; RMSEA = .04), but the correlation between EF and ToM was reduced from .62 to .40.
Table 3.
Loading of the measures on factors EF and ToM
| With cross-loading indicators | Without cross-loading indicators | |||
|---|---|---|---|---|
| EF | ToM | EF | ToM | |
| Card sort task | .75* | .003 | .56* | .19 |
| Trail making | .71* | − .07 | .80* | − .09 |
| Opposite Worlds | .47* | .01 | .54* | .005 |
| Luria Hand Gamea | .17 | .49* | – | – |
| Numbers | .66* | .06 | .67* | .00 |
| Planning/drawing | .47* | − .09 | .37* | .06 |
| Animated triangles | .004 | .72* | − .01 | .94* |
| Penny hiding game | − .12 | .84* | .13 | .61* |
| RME | .05 | .65* | .26 | .50* |
| Strange storiesa | .38* | .26 | – | – |
| False beliefa | .44* | .46* | – | – |
Abbreviation: RME Reading the Mind in the Eyes Task
aMeasures which cross-loaded on factors not expected a priori. We excluded these measures from the final model to separate the predictors
*Significant at p = .05 level
Step 2: The associations among EF, ToM, and ASD and ADHD symptoms
Model 1 (Fig. 1a) approached an acceptable fit (χ2[84] = 151.7, p < .0001; CFI = .82; TLI = .77; RMSEA = .09; AIC = 6063.9; BIC = 6196.8). Critically, paths between EF and ADHD (β = .44, p = .005), ToM and ASD (β = .74, p = .007), EF and ToM (β = .59, p < .001), and ASD and ADHD (β = .60, p = .021) were significant. Those between EF and ASD (β = − .11, p = .7) and ToM and ADHD (β = .07, p = .6) were not.
Step 3: Adding a parental latent factor
Accounting for the shared parental information resulted in model 2 that approached the threshold of acceptability (χ2[79] = 114.3, p = .006; CFI = .90; TLI = .87; RMSEA = .067; AIC = 6039.8; BIC = 6185.7). The paths of interest between EF and ADHD symptoms (β = .36, p = .049) and ToM and ASD symptoms remained (β = .94, p < .001), and the paths between EF and ASD and ToM and ADHD were nonsignificant. The correlation between ASD and ADHD became nonsignificant (r = .03, p = .94), indicating that the correlation between these symptom domains was partially accounted for by the shared variance of the parent ratings.
Step 4: Derivation of the final model
The final model (Fig. 2) was derived from model 2 with nonsignificant paths systematically removed. The nonsignificant correlation between ASD and ADHD was the first to be removed, as it ceased to be significant upon the addition of parental factor. This resulted in a model of which fit was not significantly worse than the full model (Sattora-Bentler scaled Δχ2[1] = .007, p = .93; CFI = .91; TLI = .88; RMSEA = .064). The removal of a second nonsignificant path between EF and ASD factors also did not significantly change the last model fit (Sattora-Bentler scaled Δχ2[1] = 1.35, p = .25; CFI = .91; TLI = .88; RMSEA = .064). The final removal of the nonsignificant path between ToM and ADHD also did not worsen the model fit (Sattora-Bentler scaled Δχ2[1] = .80, p = .37; CFI = .91; TLI = .88; RMSEA = .064; AIC = 6037.0; BIC = 6175.0). This model showed that EF impairments were associated with increased ADHD symptoms (β = .49, p = .001), ToM impairments were associated with ASD symptoms (β = .75, p < .001), and EF and ToM were correlated (r = .57, p < .001).
Fig. 2.
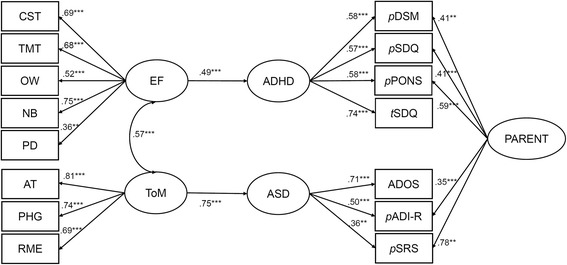
SEM final model is derived from model 2 with nonsignificant paths removed. List of abbreviations: CST card sort task, TMT Trail Making Test, OW Opposite Worlds, NB number backward, PD planning/drawing task, AT animated triangle, PHG penny hiding games, RME Reading the Mind in the Eye tasks, EF executive function, ToM theory of mind. Abbreviations for ASD or ADHD measures: ADOS Autism Diagnostic Observation Schedule, ADI-R Autism Diagnostic Interview-Revised, SRS Social Responsiveness Scale, DSM Diagnostic and Statistical Manual of Mental Disorders, SDQ Strengths and Difficulties Questionnaire, PONS Profile of Neuropsychiatric Symptoms. The prefix p on these behavioral measures indicates parent-based reports whereas the prefix t on the SDQ indicates a teacher-based report. The significant levels are *p < .05, **p < .01, and ***p < .001
Step 5: Sensitivity analysis of a model including FSIQ
By regressing EF, ToM, ASD, and ADHD in full model 2 on FSIQ and removing nonsignificant paths, we arrived at the final parsimonious model (χ2[95] = 138.7, p = .002; CFI = .91; TLI = .88; RMSEA = .07; AIC = 6811.5; BIC = 6960; Additional file 1: Figure S1B), which retained the specific relations between EF and ADHD (β = .40, p = .002) and ToM and ASD (β = .75, p < .001), while controlling for the association between higher IQ and less impairment in EF (β = − .84, p < .001) and ToM (β = − .65, p < .001).
Step 6: Sensitivity analysis using 14–16-year-old data
The fit for the parsimonious model including only the adolescent data was excellent (χ2[51] = 52.7, p = .41; CFI = .99; TLI = .99; RMSEA = .018; AIC = 3914.5; BIC = 4010.9; Additional file 1: Figure S2B), consisting of specific relations between EF and ADHD (β = .38, p = .005) and between ToM and observed ASD symptoms (β = .39, p < .001), while controlling for the association between IQ to EF (β = − .84, p < .001) and ToM impairments (β = − .72, p < .001). The model structure was also preserved when children whose two testing days were separated by more than the 2 × SD days of the mean were excluded from the analyses (see Additional file 1).
Discussion
Although ADHD symptoms are frequently seen in people with ASD, the basis for this association remains poorly understood. This study explored the specificity of relations among executive dysfunction, ToM impairments, and the ASD and ADHD traits using the framework of SEM, in a population-based sample of children with ASD. The primary findings of the study are that poorer EF ability is specifically associated with increased ADHD symptoms, accounting for its association with variation in ToM performance and ASD symptoms. Furthermore, impairments in ToM are specifically associated with ASD symptoms. Taken together, the findings show that ADHD and ASD symptoms in adolescents with ASD have dissociable neurocognitive correlates. The secondary findings are that the observed correlation between ASD and ADHD symptoms in the sample can be explained by shared source of reporting from parents and the correlation between EF and ToM. Finally, the specific relations between each cognitive domain and the behavioral symptoms are retained even when controlling for IQ.
Specific associations between cognitive domains and symptoms
Our model shows that the EF impairments among individuals with ASD are associated with increased ADHD symptoms. This is in line with findings from previous group comparisons reporting increased EF difficulties among children with dual diagnoses of ASD and ADHD compared to children with ASD alone [11, 36–38] and the associations reported between EF deficits and increased ADHD symptoms in ASD samples [39, 83]. In addition, the association between EF impairments and increased ADHD symptoms in this ASD sample is consistent with findings in other samples of individuals with ADHD (e.g., [8, 26, 27, 84]) and in the general populations (e.g., [85–87]). Importantly, we did not detect a significant association between ToM impairments and ADHD symptoms in the model, consistent with a recent meta-analytic finding showing that ToM difficulties are present to a much lesser extent in ADHD than ASD populations [9]. The specific relation between EF and ADHD symptoms in this context may provide an explanation for the mixed findings of EF difficulties in ASD (e.g., [17, 29, 30]), in that, EF difficulties are perhaps more likely to be found among people with ASD who have co-occurring ADHD.
The SEM model also shows that mentalizing abilities are specifically associated with the severity of ASD and not ADHD symptoms. This is consistent with results from previous studies [88–90] and supports the view that ToM impairments are specifically linked to ASD symptoms. These findings contrast with some studies that fail to find an association between ToM and everyday social behavior in people with ASD (e.g., [91–93]), perhaps due to these studies’ reliance on specific measures such as the false belief test, which may not fully capture the breadth of socio-cognitive and perceptual processes related to ToM [92, 94, 95]. We have addressed this potential limitation by using a multi-measure approach to better capture the ToM construct.
Contrary to previous findings of associations between performance of a variety of EF tasks and ASD symptoms [39, 44, 92, 96] and specifically between cognitive flexibility and repetitive behavior symptoms (e.g., [31–34]), no association was found between EF impairments and ASD traits in the SEM model. There could be several explanations for this finding. Firstly, none of these previous studies considered the association between EF and ASD after controlling for ToM impairments. Therefore, the association between EF and ASD symptoms might have been observed in those studies because the covariation of ToM and ASD or EF and ADHD symptoms was not accounted for. Secondly, many studies reporting the associations between EF impairments and ASD symptoms analyzed these relations separately between tasks that may tap different aspects of EF. Thus, the correlations found between task performance and ASD symptoms, notably between cognitive flexibility performance and repetitive behavior symptoms, may reflect relations between properties that are specific to the task or the EF subdomain, rather than the underlying common EF factor, with the ASD symptoms. Lastly, as learnt from the finding in relation to the Luria Hand Game, performance on a task that is traditionally an inhibitory measure may load onto ToM instead of EF factors, thus more associated with ASD symptoms. This could be because the task triggers mentalizing processes when the subjects attempt to guess which hand gesture the experimenter would be giving next. Such interpretation is in line with the Triple-I hypothesis [97], which argues that EF impairments in ASD might be a by-product of mentalizing deficits in the population.
A shared parental rating factor partially accounts for the correlation between ASD and ADHD traits
Several previous studies have found that individuals with ASD (and co-occurring ADHD symptoms) have more severe ASD traits relative to those with ASD alone, judged from parent-rated questionnaires such as the SRS [38, 47, 49]. Autistic trait measures have less specificity when applied to children with ASD and additional behavioral or emotional problems, including ADHD [98, 99]; thus, it is possible that past reports of an association between ASD and ADHD traits were due to a systematic instrument bias, in which those with additional ADHD traits also receive higher ratings of autistic traits. The association between ADHD and ASD trait severity was noticeably absent in previous studies; however, when ASD traits were measured using measures such as the ADI-R, ADOS [38, 47, 48, 75] or clinical symptom counts [74]. Unlike the SRS, which is parent questionnaire, measures such as the ADI-R and clinical symptoms involve clinical judgment, and in the case of ADOS, direct observation of the children. Therefore, the association between the ASD and ADHD traits found in previous studies might be partially dependent on the source and type of reporting.
Indeed, the final SEM model showed that information obtained from the same source (i.e., parents in this case) on ASD and ADHD traits moderated their correlation. That is, ratings by the same informant on different measures are more highly correlated than those from different informants. There are multiple possible explanations for this finding. Informants, in this case, parents, may have a specific response style, such as a tendency to rate all behaviors as high or low, that influences their responses across measures [100]. Furthermore, children’s behavior may differ across settings [101, 102]. As in many studies, parents were the predominant source of information regarding symptoms in this study. Because no other information source was shared across ASD and ADHD measures, it was not possible to test whether these effects are specific to parents or applies to other sources, such as teachers or direct observation. Nevertheless, our findings underline the importance of obtaining multiple sources of information [103].
Explaining the co-occurrence of ADHD symptoms among ASD children
In line with the comorbidity literature, our model showed that artifactual and non-artifactual mechanisms could explain the increased co-occurrence of ADHD traits in the ASD children population. Firstly, ADHD traits might be reported at increased rates, presumably in those with more severe ASD, due to shared reporting source effects from parents. These cases, which do not express true comorbidity, one hopes are few and can be differentiated from true comorbidity cases during clinical observations, corroborated by non-parental source of information. Aside from this artifactual reason, our model provides preliminary supports for the cognitive mechanisms underlying the true comorbidity of ADHD traits in children with ASD. We have shown in this study that the cognitive correlates of the ASD and ADHD traits in children are dissociable, which supports the additive model for the co-occurrence of ADHD traits on ASD symptoms. Furthermore, from our model, the co-occurrence of the separable ASD and ADHD traits could be explained partially by the moderate correlation between EF and ToM impairments (.56), indicating that individuals with both ASD and ADHD symptoms constitute those who are “doubly hit” by both EF and ToM impairments.
Due to the limitations posed by the available data, the support our model gives to the additive model is preliminary. To satisfactorily adhere to the additive comorbidity model, we believe that the ADHD traits found in our ASD population must be phenomenologically equivalent, both in presentations and their associations to the cognitive factors, with symptoms found in the pure ADHD population. While previous findings suggest that ADHD symptoms in clinical ASD and ADHD populations have similar presentations (inattentive, hyperactive, and combined [104, 105]) with only subtle differences in few symptoms [106, 107], and although the association found between executive dysfunction and ADHD traits in our sample is consistent with other findings in ADHD population (e.g., [8, 26, 27, 84]), neither could be directly observed in this study due to the lack of ADHD comparison sample.
Strengths and limitations
The inclusion of a well-characterized sample of children with ASD is an advantage for this study. Although the sample is not ASD population representative due to the exclusion of individuals with IQ below 50, it is still population-based and is free from clinical sampling biases. In fact, the comparisons we made between eligible individuals who did and did not take part in the study suggested that the study participants had representative ASD and ADHD traits for ASD children with IQ of 50 and above, therefore substantively extending previous neurocognitive findings in this topic which typically excluded children with learning disability. The inclusion of multiple measures from multiple informants gives an advantage over the typical approach of using single measures. The study includes multiple measures of ADHD psychopathology including the SDQ, a well-recognized screening instrument for children and adolescents, and the diagnostic instrument CAPA. Furthermore, the ADOS and the ADI-R, used to index autistic traits in the model, are considered “gold-standard” research instruments for assessing ASD [108].
One limitation of the study is that factors were modeled with EF and ToM predicting the ADHD and ASD symptoms, in line with the idea that EF and ToM deficits are endophenotypes that mediate the link between genes and behavioral symptoms (see [10] for alternative models that do not assume this directionality). However, the study design does not allow a strong test of causal direction. Therefore, the links between factors in the present model are best understood as associations rather than predictions. Secondly, we have modeled associations between factors indexed by measures collected over a 6-year period, thus assuming the stability of behavioral traits within the time window, which was supported by findings of persisting ASD and ADHD traits from childhood to adolescents reported in previous studies [74–76]. Furthermore, the additional analyses including only data collected during the adolescent years preserve the specificity of relations between the factors EF and ADHD and between ToM and observed ASD symptoms in the model. Finally, the small number of girls in the study may limit the generalizability of the results among females with ASD.
Conclusions
This study adds to the growing literature that explores the cognitive underpinnings of ADHD symptoms in the ASD population. We found that there is a specific association between EF and ADHD symptoms that remained even after controlling for their associations with variations in ToM abilities and ASD symptoms, which supports the additive hypothesis of ADHD symptoms of ASD in the comorbid cases. Within the clinical context, this finding improves our understanding of how impairments in distinct cognitive domains contribute to the phenotypic variations of ASD, which often include additional presentation of ADHD. Our findings also suggest similarities in the cognitive correlates of ADHD symptoms in ASD as in pure ADHD [35, 39], although this remains to be tested by comparing the model in both ASD and ADHD populations. Importantly, the association between EF and ToM impairments could provide a partial explanation for the co-occurrence of ADHD symptoms in ASD. Finally, shared reporting effects from parents should be considered when examining ADHD symptoms in the ASD population.
Acknowledgements
We are grateful to the adolescents and families who took part in this study. With thanks to Anita Marsden, Jeni Tregay, and Rebecca Phillips for their help with the data collection.
Funding
The research was supported by awards from the Medical Research Council (G0400065) and the NIHR Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the funders, NHS, NIHR, or the UK Department of Health.
Availability of data and materials
The datasets generated by the current study are not available publicly and are currently being further analyzed by the research group, but they are available on reasonable request from individual researchers who wish to use the data in their investigation.
Abbreviations
- ADHD
Attention-deficit/hyperactivity disorder
- ADI-R
Autism Diagnostic Interview-Revised
- ADOS-G
Autism Diagnostic Observation Schedule-Generic
- AIC
Akaike information criterion
- ASD
Autism spectrum disorder
- AT
Animated triangle task
- BIC
Bayesian information criterion
- CAPA
Child and Adolescent Psychiatric Assessment
- CFI
Comparative fit index
- CST
Card sorting task
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- EF
Executive function
- EFA
Exploratory factor analysis
- FSIQ
Full Scale IQ
- ICD-10
International Classification of Diseases
- NB
Numbers (backward)
- OW
Opposite Worlds
- PD
Planning drawing task
- PHG
Penny hiding game
- PIQ
Performance IQ
- PONS
Profile of Neuropsychiatric Symptoms
- RME
Reading the Mind in the Eyes
- RMSEA
Root mean square error of approximation
- SDQ
Strengths and Difficulties Questionnaire
- SEM
Structural equation modeling
- SNAP
Special Needs and Autism Project
- SRS
Social Responsiveness Scale
- TLI
Tucker-Lewis Index
- TMT
Trail Making Test
- ToM
Theory of mind
- VIQ
Verbal IQ
- WASI
Wechsler’s Abbreviated Scale of Intelligence
- WISC
Wechsler Intelligence Scale for Children
Additional file
Measures, completers, and wave of investigations. Figure S1. Controlling for IQ in the final model. Latent factors EF, ToM, ASD, and ADHD were regressed on IQ in the full final model (Figure A), nonsignificant paths were represented by dotted lines. Figure S2. Model including only measures from collected from the adolescents at the age of 14–16 years old. (DOCX 488 kb)
Authors’ contributions
SL made substantial contributions to the conception of the study and its design, the analysis, interpretation of the data, and the drafting of the manuscript. CJ made substantial contributions to the acquisition of data and critical revision of the manuscript for important intellectual content. AP made substantial contributions to the statistical methods and interpretations. GB, FH, and TC made substantial contribution in the critical revision of the manuscript for important intellectual content. ES made substantial contributions to the design, interpretation of the data, and critical revision of the manuscript for important intellectual content and gave final approval of the version to be published. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by the South-East London Research Ethics Committee (05/MRE01/67). Informed consent was given by the parents and by the participant if their level of understanding was sufficient.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s13229-017-0177-1) contains supplementary material, which is available to authorized users.
Contributor Information
Steve Lukito, Email: steve.s.lukito@kcl.ac.uk.
Catherine R. G. Jones, Email: jonescr10@cardiff.ac.uk
Andrew Pickles, Email: andrew.pickles@kcl.ac.uk.
Gillian Baird, Email: gillian.baird@gstt.nhs.uk.
Francesca Happé, Email: francesca.happe@kcl.ac.uk.
Tony Charman, Email: tony.charman@kcl.ac.uk.
Emily Simonoff, Email: emily.simonoff@kcl.ac.uk.
References
- 1.Elsabbagh M, Divan G, Koh Y-J, Kim YS, Kauchali S, Marcín C, Montiel-Nava C, Patel V, Paula CS, Wang C, et al. Global prevalence of autism and other pervasive developmental disorders: global epidemiology of autism. Autism Res. 2012;5:160–179. doi: 10.1002/aur.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders: DSM-5. 5. Washington, DC: APA; 2013. [Google Scholar]
- 3.Gjevik E, Eldevik S, Fjæran-Granum T, Sponheim E. Kiddie-SADS reveals high rates of DSM-IV disorders in children and adolescents with autism spectrum disorders. J Autism Dev Disord. 2011;41:761–769. doi: 10.1007/s10803-010-1095-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salazar F, Baird G, Chandler S, Tseng E, O’sullivan T, Howlin P, Pickles A, Simonoff E. Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. J Autism Dev Disord. 2015;45:2283–2294. doi: 10.1007/s10803-015-2361-5. [DOI] [PubMed] [Google Scholar]
- 5.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47:921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 6.Polanczyk G, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol. 2014;43:434–442. doi: 10.1093/ije/dyt261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Craig F, Margari F, Legrottaglie AR, Palumbi R, de Giambattista C, Margari L. A review of executive function deficits in autism spectrum disorder and attention-deficit/hyperactivity disorder. Neuropsychiatr Dis Treat. 2016;12:1191–1202. doi: 10.2147/NDT.S104620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Willcutt EG, Sonuga-Barke EJS, Nigg JT, Sergeant JA. Recent developments in neuropsychological models of childhood psychiatric disorders. In: Banaschewski T, Rohde LA, editors. Advances in biological psychiatry. Basel: Karger; 2008. pp. 195–226. [Google Scholar]
- 9.Bora E, Pantelis C. Meta-analysis of social cognition in attention-deficit/hyperactivity disorder (ADHD): comparison with healthy controls and autistic spectrum disorder. Psychol Med. 2015;41:1–18. [DOI] [PubMed]
- 10.Rommelse NNJ, Geurts HM, Franke B, Buitelaar JK, Hartman CA. A review on cognitive and brain endophenotypes that may be common in autism spectrum disorder and attention-deficit/hyperactivity disorder and facilitate the search for pleiotropic genes. Neurosci Biobehav Rev. 2011;35:1363–1396. doi: 10.1016/j.neubiorev.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 11.Sinzig J, Morsch D, Bruning N, Schmidt MH, Lehmkuhl G. Inhibition, flexibility, working memory and planning in autism spectrum disorders with and without comorbid ADHD-symptoms. Child Adolesc Psychiatry Ment Health. 2008;2:4. doi: 10.1186/1753-2000-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tye C, Asherson P, Ashwood KL, Azadi B, Bolton P, McLoughlin G. Attention and inhibition in children with ASD, ADHD and co-morbid ASD + ADHD: an event-related potential study. Psychol Med. 2014;44:1101–1116. doi: 10.1017/S0033291713001049. [DOI] [PubMed] [Google Scholar]
- 13.Caron C, Rutter M. Comorbidity in child psychopathology: concepts, issues and research strategies. J Child Psychol Psychiatry. 1991;32:1063–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- 14.Banaschewski T, Neale BM, Rothenberger A, Roessner V. Comorbidity of tic disorders & ADHD: conceptual and methodological considerations. Eur Child Adolesc Psychiatry. 2007;16:5–14. doi: 10.1007/s00787-007-1002-8. [DOI] [PubMed] [Google Scholar]
- 15.van der Meer JM, Oerlemans AM, van Steijn DJ, Lappenschaar MG, de Sonneville LM, Buitelaar JK, Rommelse NN. Are autism spectrum disorder and attention-deficit/hyperactivity disorder different manifestations of one overarching disorder? Cognitive and symptom evidence from a clinical and population-based sample. J Am Acad Child Adolesc Psychiatry 2012; 51:1160-1172 e3. [DOI] [PubMed]
- 16.Yirmiya N, Erel O, Shaked M, Solomonica-Levi D. Meta-analyses comparing theory of mind abilities of individuals with autism, individuals with mental retardation, and normally developing individuals. Psychol Bull. 1998;124:283–307. doi: 10.1037/0033-2909.124.3.283. [DOI] [PubMed] [Google Scholar]
- 17.Kuiper MWM, Verhoeven EWM, Geurts HM. The role of interstimulus interval and “stimulus-type” in prepotent response inhibition abilities in people with ASD: a quantitative and qualitative review. Autism Res. 2016;9:1124–1141. doi: 10.1002/aur.1631. [DOI] [PubMed] [Google Scholar]
- 18.Hill EL. Executive dysfunction in autism. Trends Cogn Sci. 2004;8:26–32. doi: 10.1016/j.tics.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 19.Landry O, Al-Taie S. A meta-analysis of the Wisconsin Card Sort Task in autism. J Autism Dev Disord. 2016;46:1220–1235. doi: 10.1007/s10803-015-2659-3. [DOI] [PubMed] [Google Scholar]
- 20.Baron-Cohen S, Leslie AM, Frith U. Does the autistic child have a “theory of mind”? Cognition. 1985;21:37–46. doi: 10.1016/0010-0277(85)90022-8. [DOI] [PubMed] [Google Scholar]
- 21.Senju A. Atypical development of spontaneous social cognition in autism spectrum disorders. Brain and Development. 2013;35:96–101. doi: 10.1016/j.braindev.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Buitelaar JK, van der Wees M, Swaab-Barneveld H, van der Gaag RJ. Theory of mind and emotion-recognition functioning in autistic spectrum disorders and in psychiatric control and normal children. Dev Psychopathol. 1999;11:39–58. doi: 10.1017/S0954579499001947. [DOI] [PubMed] [Google Scholar]
- 23.Mary A, Slama H, Mousty P, Massat I, Capiau T, Drabs V, Peigneux P. Executive and attentional contributions to theory of mind deficit in attention deficit/hyperactivity disorder (ADHD) Child Neuropsychol. 2016;22:345–365. doi: 10.1080/09297049.2015.1012491. [DOI] [PubMed] [Google Scholar]
- 24.Happe F, Booth R, Charlton R, Hughes C. Executive function deficits in autism spectrum disorders and attention-deficit/hyperactivity disorder: examining profiles across domains and ages. Brain Cogn. 2006;61:25–39. doi: 10.1016/j.bandc.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 25.Miyake A, Friedman NP. The nature and organization of individual differences in executive functions: four general conclusions. Curr Dir Psychol Sci. 2012;21:8–14. doi: 10.1177/0963721411429458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lipszyc J, Schachar R. Inhibitory control and psychopathology: a meta-analysis of studies using the stop signal task. J Int Neuropsychol Soc. 2010;16:1064–1076. doi: 10.1017/S1355617710000895. [DOI] [PubMed] [Google Scholar]
- 27.Kasper LJ, Alderson RM, Hudec KL. Moderators of working memory deficits in children with attention-deficit/hyperactivity disorder (ADHD): a meta-analytic review. Clin Psychol Rev. 2012;32:605–617. doi: 10.1016/j.cpr.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Willcutt EG, Pennington BF, Olson RK, Chhabildas N, Hulslander J. Neuropsychological analyses of comorbidity between reading disability and attention deficit hyperactivity disorder: in search of the common deficit. Dev Neuropsychol. 2005;27:35–78. doi: 10.1207/s15326942dn2701_3. [DOI] [PubMed] [Google Scholar]
- 29.Geurts HM, Sinzig J, Booth R, Happé F. Neuropsychological heterogeneity in executive functioning in autism spectrum disorders. Int J Dev Disabil. 2014;60:155–162. doi: 10.1179/2047387714Y.0000000047. [DOI] [Google Scholar]
- 30.Geurts HM, Corbett B, Solomon M. The paradox of cognitive flexibility in autism. Trends Cogn Sci. 2009;13:74–82. doi: 10.1016/j.tics.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D'Cruz A-M, Ragozzino ME, Mosconi MW, Shrestha S, Cook EH, Sweeney JA. Reduced behavioral flexibility in autism spectrum disorders. Neuropsychology. 2013;27:152–160. doi: 10.1037/a0031721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reed P, Watts H, Truzoli R. Flexibility in young people with autism spectrum disorders on a card sort task. Autism. 2013;17:162–171. doi: 10.1177/1362361311409599. [DOI] [PubMed] [Google Scholar]
- 33.Mostert-Kerckhoffs MAL, Staal WG, Houben RH, de Jonge MV. Stop and change: inhibition and flexibility skills are related to repetitive behavior in children and young adults with autism spectrum disorders. J Autism Dev Disord. 2015;45:3148–3158. doi: 10.1007/s10803-015-2473-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brunsdon VE, Happé F. Exploring the ‘fractionation’ of autism at the cognitive level. Autism. 2014;18:17–30. doi: 10.1177/1362361313499456. [DOI] [PubMed] [Google Scholar]
- 35.Corbett BA, Constantine LJ, Hendren R, Rocke D, Ozonoff S. Examining executive functioning in children with autism spectrum disorder, attention deficit hyperactivity disorder and typical development. Psychiatry Res. 2009;166:210–222. doi: 10.1016/j.psychres.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buehler E, Bachmann C, Goyert H, Heinzel-Gutenbrunner M, Kamp-Becker I. Differential diagnosis of autism spectrum disorder and attention deficit hyperactivity disorder by means of inhibitory control and ‘theory of mind’. J Autism Dev Disord. 2011;41:1718–1726. doi: 10.1007/s10803-011-1205-1. [DOI] [PubMed] [Google Scholar]
- 37.Andersen PN, Hovik KT, Skogli EW, Egeland J, Øie M. Symptoms of ADHD in children with high-functioning autism are related to impaired verbal working memory and verbal delayed recall. PLoS One. 2013;8:e64842. doi: 10.1371/journal.pone.0064842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yerys BE, Wallace GL, Sokoloff JL, Shook DA, James JD, Kenworthy L. Attention deficit/hyperactivity disorder symptoms moderate cognition and behavior in children with autism spectrum disorders. Autism Res. 2009;2:322–333. doi: 10.1002/aur.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ames CS, White SJ. Brief report: are ADHD traits dissociable from the autistic profile? Links between cognition and behaviour. J Autism Dev Disord. 2011;41:357–363. doi: 10.1007/s10803-010-1049-0. [DOI] [PubMed] [Google Scholar]
- 40.Unterrainer JM, Rauh R, Rahm B, Hardt J, Kaller CP, Klein C, Paschke-Müller M, Biscaldi M. Development of planning in children with high-functioning autism spectrum disorders and/or attention deficit/hyperactivity disorder. Autism Res. 2015;9:739-51. [DOI] [PubMed]
- 41.Yang J, Zhou S, Yao S, Su L, McWhinnie C. The relationship between theory of mind and executive function in a sample of children from mainland China. Child Psychiatry Hum Dev. 2009;40:169–182. doi: 10.1007/s10578-008-0119-4. [DOI] [PubMed] [Google Scholar]
- 42.Friedman NP, Miyake A. The relations among inhibition and interference control functions: a latent-variable analysis. J Exp Psychol. 2004;133:101–135. doi: 10.1037/0096-3445.133.1.101. [DOI] [PubMed] [Google Scholar]
- 43.Pellicano E. Links between theory of mind and executive function in young children with autism: clues to developmental primacy. Dev Psychol. 2007;43:974–990. doi: 10.1037/0012-1649.43.4.974. [DOI] [PubMed] [Google Scholar]
- 44.Joseph RM, Tager-Flusberg H. The relationship of theory of mind and executive functions to symptom type and severity in children with autism. Dev Psychopathol. 2004;16:137-55. [DOI] [PMC free article] [PubMed]
- 45.Ozonoff S, Pennington BF, Rogers SJ. Executive function deficits in high-functioning autistic individuals: relationship to theory of mind. J Child Psychol Psychiatry. 1991;32:1081–1105. doi: 10.1111/j.1469-7610.1991.tb00351.x. [DOI] [PubMed] [Google Scholar]
- 46.Bigham S. Impaired competence for pretense in children with autism: exploring potential cognitive predictors. J Autism Dev Disord. 2010;40:30–38. doi: 10.1007/s10803-009-0820-6. [DOI] [PubMed] [Google Scholar]
- 47.Holtmann M, Bolte S, Poustka F. Attention deficit hyperactivity disorder symptoms in pervasive developmental disorders: association with autistic behavior domains and coexisting psychopathology. Psychopathology. 2007;40:172–177. doi: 10.1159/000100007. [DOI] [PubMed] [Google Scholar]
- 48.Salley B, Gabrielli J, Smith CM, Braun M. Do communication and social interaction skills differ across youth diagnosed with autism spectrum disorder, attention-deficit/hyperactivity disorder, or dual diagnosis? Res Autism Spectr Disord. 2015;20:58–66. doi: 10.1016/j.rasd.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sprenger L, Buehler E, Poustka L, Bach C, Heinzel-Gutenbrunner M, Kamp-Becker I, Bachmann C. Impact of ADHD symptoms on autism spectrum disorder symptom severity. Res Dev Disabil. 2013;34:3545–3552. doi: 10.1016/j.ridd.2013.07.028. [DOI] [PubMed] [Google Scholar]
- 50.Baird G, Simonoff E, Pickles A, Chandler S, Loucas T, Meldrum D, Charman T. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP) Lancet. 2006;368:210–215. doi: 10.1016/S0140-6736(06)69041-7. [DOI] [PubMed] [Google Scholar]
- 51.World Health Organization . The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- 52.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 53.Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, Pickles A, Rutter M. The Autism Diagnostic Observation Schedule-Generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30:205–223. doi: 10.1023/A:1005592401947. [DOI] [PubMed] [Google Scholar]
- 54.Constantino JN. The quantitative nature of autistic social impairment. Pediatr Res. 2011;69:55R–62R. doi: 10.1203/PDR.0b013e318212ec6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Int Rev Psychiatry. 2003;15:166–172. doi: 10.1080/0954026021000046128. [DOI] [PubMed] [Google Scholar]
- 56.Wechsler D. Wechsler Abbreviated Scale of Intelligence (WASI) London: The Psychological Corporation; 1999. [Google Scholar]
- 57.Santosh PJ, Gringras P, Baird G, Fiori F, Sala R. Development and psychometric properties of the parent version of the Profile of Neuropsychiatric Symptoms (PONS) in children and adolescents. BMC Pediatr. 2015;15:62. doi: 10.1186/s12887-015-0376-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Angold A, Prendergast M, Cox A, Harrington R, Simonoff E, Rutter M. The child and adolescent psychiatric assessment (CAPA) Psychol Med. 1995;25:739–753. doi: 10.1017/S003329170003498X. [DOI] [PubMed] [Google Scholar]
- 59.Manly T, Anderson V, Nimmo-Smith I, Turner A, Watson P, Robertson IH. The differential assessment of children’s attention: the Test of Everyday Attention for Children (TEA-Ch), normative sample and ADHD performance. J Child Psychol Psychiatry. 2001;42:1065–1081. doi: 10.1111/1469-7610.00806. [DOI] [PubMed] [Google Scholar]
- 60.Luria AR, Pribram KH, Homskaya ED. An experimental analysis of the behavioral disturbance produced by a left frontal arachnoidal endothelioma (meningioma) Neuropsychologia. 1964;2:257–280. doi: 10.1016/0028-3932(64)90034-X. [DOI] [Google Scholar]
- 61.Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Mot Skills. 1958;8:271-76.
- 62.Tregay J, Gilmour J, Charman T. Childhood rituals and executive functions. Br J Dev Psychol. 2009;27:283–296. doi: 10.1348/026151008X299737. [DOI] [PubMed] [Google Scholar]
- 63.Booth R, Charlton R, Hughes C, Happé F. Disentangling weak coherence and executive dysfunction: planning drawing in autism and attention-deficit/hyperactivity disorder. Philos Trans R Soc Lond Ser B Biol Sci. 2003;358:387–392. doi: 10.1098/rstb.2002.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cohen M. Children’s memory scale. San Antonio, TX: The Psychological Corporation; 1997. [Google Scholar]
- 65.Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry. 2005;57:1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 66.Bowler DM. “Theory of mind” in Asperger’s syndrome. J Child Psychol Psyc. 1992;33:877–893. doi: 10.1111/j.1469-7610.1992.tb01962.x. [DOI] [PubMed] [Google Scholar]
- 67.Baron-Cohen S. The autistic child’s theory of mind: a case of specific developmental delay. J Child Psychol Psychiatry. 1989;30:285–297. doi: 10.1111/j.1469-7610.1989.tb00241.x. [DOI] [PubMed] [Google Scholar]
- 68.Baron-Cohen S, Wheelwright S, Scahill V, Lawson J, Spong A. Are intuitive physics and intuitive psychology independent? A test with children with Asperger syndrome. J Dev Learn Disord. 2001;5:47–78. [Google Scholar]
- 69.Baron-Cohen S. Out of sight or out of mind? Another look at deception in autism. J Child Psychol Psychiatry. 1992;33:1141–1155. doi: 10.1111/j.1469-7610.1992.tb00934.x. [DOI] [PubMed] [Google Scholar]
- 70.Happé FG. An advanced test of theory of mind: understanding of story characters' thoughts and feelings by able autistic, mentally handicapped, and normal children and adults. J Autism Dev Disord. 1994;24:129–154. doi: 10.1007/BF02172093. [DOI] [PubMed] [Google Scholar]
- 71.Castelli F, Frith C, Happé F, Frith U. Autism, Asperger syndrome and brain mechanisms for the attribution of mental states to animated shapes. Brain. 2002;125:1839–1849. doi: 10.1093/brain/awf189. [DOI] [PubMed] [Google Scholar]
- 72.StataCorp LP. Stata: release 11 base reference manual. College Station, TX: Stata Press; 2009. [Google Scholar]
- 73.Bulgarelli D, Testa S, Molina P. Factorial structure of the ‘ToM Storybooks’: a test evaluating multiple components of theory of mind. Br J Dev Psychol. 2015;33:187–202. doi: 10.1111/bjdp.12062. [DOI] [PubMed] [Google Scholar]
- 74.Simonoff E, Jones CRG, Baird G, Pickles A, Happé F, Charman T. The persistence and stability of psychiatric problems in adolescents with autism spectrum disorders: stability of psychiatric symptoms in autism spectrum disorders. J Child Psychol Psyc. 2013;54:186–194. doi: 10.1111/j.1469-7610.2012.02606.x. [DOI] [PubMed] [Google Scholar]
- 75.Louwerse A, Eussen MLJM, Van der Ende J, de Nijs PFA, Van Gool AR, Dekker LP, Verheij C, Verheij F, Verhulst FC, Greaves-Lord KASD. Symptom severity in adolescence of individuals diagnosed with PDD-NOS in childhood: stability and the relation with psychiatric comorbidity and societal participation. J Autism Dev Disord. 2015;45:3908–3918. doi: 10.1007/s10803-015-2595-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cederlund M, Hagberg B, Billstedt E, Gillberg IC, Gillberg C. Asperger syndrome and autism: a comparative longitudinal follow-up study more than 5 years after original diagnosis. J Autism Dev Disord. 2008;38:72–85. doi: 10.1007/s10803-007-0364-6. [DOI] [PubMed] [Google Scholar]
- 77.Tureck K, Matson JL, Cervantes P, Turygin N. Autism severity as a predictor of inattention and impulsivity in toddlers. Dev Neurorehabil. 2013;18:285-9. [DOI] [PubMed]
- 78.Muthén LK, Muthén BO. Mplus: the comprehensive modeling program for applied researchers : user’s guide. Los Angeles: Muthén & Muthén; 2000.
- 79.Charman T, Pickles A, Simonoff E, Chandler S, Loucas T, Baird G. IQ in children with autism spectrum disorders: data from the Special Needs and Autism Project (SNAP) Psychol Med. 2011;41:619–627. doi: 10.1017/S0033291710000991. [DOI] [PubMed] [Google Scholar]
- 80.Postorino V, Fatta LM, Sanges V, Giovagnoli G, De Peppo L, Vicari S, Mazzone L. Intellectual disability in autism spectrum disorder: investigation of prevalence in an Italian sample of children and adolescents. Res Dev Disabil. 2016;48:193–201. doi: 10.1016/j.ridd.2015.10.020. [DOI] [PubMed] [Google Scholar]
- 81.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. doi: 10.1037/0033-2909.88.3.588. [DOI] [Google Scholar]
- 82.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newburry Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- 83.Bishop DVM, Norbury CF. Executive functions in children with communication impairments, in relation to autistic symptomatology 2: response inhibition. Autism. 2005;9:29–43. doi: 10.1177/1362361305049028. [DOI] [PubMed] [Google Scholar]
- 84.Wood AC, Rijsdijk F, Johnson KA, Andreou P, Albrecht B, Arias-Vasquez A, Buitelaar JK, McLoughlin G, Rommelse NN, Sergeant JA, et al. The relationship between ADHD and key cognitive phenotypes is not mediated by shared familial effects with IQ. Psychol Med. 2011;41:861–871. doi: 10.1017/S003329171000108X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kuntsi J, Andreou P, Ma J, Börger N, Van Der Meere J. Testing assumptions for endophenotype studies in ADHD: reliability and validity of tasks in a general population sample. BMC Psychiatry. 2005;5:40. [DOI] [PMC free article] [PubMed]
- 86.Kuntsi J, Wood AC, Van Der Meere J, Asherson P. Why cognitive performance in ADHD may not reveal true potential: findings from a large population-based sample. J Int Neuropsychol Soc. 2009;15:570–579. doi: 10.1017/S135561770909081X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bezdjian S, Baker LA, Lozano DI, Raine A. Assessing inattention and impulsivity in children during the Go/NoGo task. Br J Dev Psychol. 2009;27:365–383. doi: 10.1348/026151008X314919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Frith U, Happé F, Siddons F. Autism and theory of mind in everyday life. Soc Dev. 1994;3:108–124. doi: 10.1111/j.1467-9507.1994.tb00031.x. [DOI] [PubMed] [Google Scholar]
- 89.Nagar Shimoni H, Weizman A, Yoran RH, Raviv A. Theory of mind, severity of autistic symptoms and parental correlates in children and adolescents with Asperger syndrome. Psychiatry Res. 2012;197:85–89. doi: 10.1016/j.psychres.2012.02.021. [DOI] [PubMed] [Google Scholar]
- 90.San José Cáceres A, Keren N, Booth R, Happé F. Assessing theory of mind nonverbally in those with intellectual disability and ASD: the Penny Hiding Game. Autism Res. 2014;7:608–616. doi: 10.1002/aur.1405. [DOI] [PubMed] [Google Scholar]
- 91.Fombonne E, Siddons F, Achard S, Frith U, Happé F. Adaptive behaviour and theory of mind in autism. Eur Child Adolesc Psychiatry. 1994;3:176–186. doi: 10.1007/BF02720324. [DOI] [PubMed] [Google Scholar]
- 92.Pellicano E. Testing the predictive power of cognitive atypicalities in autistic children: evidence from a 3-year follow-up study. Autism Res. 2013;6:258–267. doi: 10.1002/aur.1286. [DOI] [PubMed] [Google Scholar]
- 93.Travis L, Sigman M, Ruskin E. Links between social understanding and social behavior in verbally able children with autism. J Autism Dev Disord. 2001;31:119–130. doi: 10.1023/A:1010705912731. [DOI] [PubMed] [Google Scholar]
- 94.Bloom P, German TP. Two reasons to abandon the false belief task as a test of theory of mind. Cognition. 2000;77:B25–B31. doi: 10.1016/S0010-0277(00)00096-2. [DOI] [PubMed] [Google Scholar]
- 95.Tager-Flusberg H. Evaluating the theory of mind hypothesis of autism. Curr Dir Psychol Sci. 2007;16:311–315. doi: 10.1111/j.1467-8721.2007.00527.x. [DOI] [Google Scholar]
- 96.Kenworthy L, Black DO, Harrison B, Della Rosa A, Wallace GL. Are executive control functions related to autism symptoms in high-functioning children? Child Neuropsychol. 2009;15:425–440. doi: 10.1080/09297040802646983. [DOI] [PubMed] [Google Scholar]
- 97.White SJ. The Triple I hypothesis: taking another(’s) perspective on executive dysfunction in autism. J Autism Dev Disord. 2013;43:114–121. doi: 10.1007/s10803-012-1550-8. [DOI] [PubMed] [Google Scholar]
- 98.Moul C, Cauchi A, Hawes DJ, Brennan J, Dadds MR. Differentiating autism spectrum disorder and overlapping psychopathology with a brief version of the Social Responsiveness Scale. Child Psychiatry Hum Dev. 2015;46:108–117. doi: 10.1007/s10578-014-0456-4. [DOI] [PubMed] [Google Scholar]
- 99.Grzadzinski R, Dick C, Lord C, Bishop S. Parent-reported and clinician-observed autism spectrum disorder (ASD) symptoms in children with attention deficit/hyperactivity disorder (ADHD): implications for practice under DSM-5. Mol Autism. 2016;7:7. [DOI] [PMC free article] [PubMed]
- 100.De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychol Bull. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- 101.Kanne SM, Abbacchi AM, Constantino JN. Multi-informant ratings of psychiatric symptom severity in children with autism spectrum disorders: the importance of environmental context. J Autism Dev Disord. 2009;39:856–864. doi: 10.1007/s10803-009-0694-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Murray DW, Kollins SH, Hardy KK, Abikoff HB, Swanson JM, Cunningham C, Vitiello B, Riddle MA, Davies M, Greenhill LL, et al. Parent versus teacher ratings of attention-deficit/hyperactivity disorder symptoms in the Preschoolers with Attention-Deficit/Hyperactivity Disorder Treatment Study (PATS) J Child Adolesc Psychopharmacol. 2007;17:605–620. doi: 10.1089/cap.2007.0060. [DOI] [PubMed] [Google Scholar]
- 103.Risi S, Lord C, Gotham K, Corsello C, Chrysler C, Szatmari P, Cook EH, Leventhal BL, Pickles A. Combining information from multiple sources in the diagnosis of autism spectrum disorders. J Am Acad Child Adolesc Psychiatry. 2006;45:1094–1103. doi: 10.1097/01.chi.0000227880.42780.0e. [DOI] [PubMed] [Google Scholar]
- 104.Goldstein S, Schwebach AJ. The comorbidity of pervasive developmental disorder and attention deficit hyperactivity disorder: results of a retrospective chart review. J Autism Dev Disord. 2004;34:329–339. doi: 10.1023/B:JADD.0000029554.46570.68. [DOI] [PubMed] [Google Scholar]
- 105.Johnston K, Dittner A, Bramham J, Murphy C, Knight A, Russell A. Attention deficit hyperactivity disorder symptoms in adults with autism spectrum disorders. Autism Res. 2013;6:225–236. doi: 10.1002/aur.1283. [DOI] [PubMed] [Google Scholar]
- 106.Hofvander B, Delorme R, Chaste P, Nyden A, Wentz E, Stahlberg O, Herbrecht E, Stopin A, Anckarsater H, Gillberg C, et al. Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry. 2009;9:35. doi: 10.1186/1471-244X-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Joshi G, Faraone SV, Wozniak J, Tarko L, Fried R, Galdo M, Furtak SL, Biederman J. Symptom profile of ADHD in youth with high-functioning autism spectrum disorder: a comparative study in psychiatrically referred populations. J Atten Disord. 2014;21:846-55. [DOI] [PMC free article] [PubMed]
- 108.Falkmer T, Anderson K, Falkmer M, Horlin C. Diagnostic procedures in autism spectrum disorders: a systematic literature review. Eur Child Adolesc Psychiatry. 2013;22:329–340. doi: 10.1007/s00787-013-0375-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated by the current study are not available publicly and are currently being further analyzed by the research group, but they are available on reasonable request from individual researchers who wish to use the data in their investigation.


