Abstract
Objective: We aimed to explore correlates and predictors of bereavement severity and persistence (triggered by “loss of a loved one”; referent group partner loss) in the Rotterdam cohort. Method: We used linear regression to examine factors associated with grief severity using a cross-sectional analysis and logistic regression to determine prospective associations. Results: Cross-sectionaly, females, child-lost, higher depressive symptoms, lower education, and difficulties in daily activities were independently associated with a higher bereavement severity. Prospectively (6 years; response rate 71%), the baseline value of the grief severity was the single predictor significantly associated with grief persistence. Discussion: Our results suggest that only grief severity is independently associated with grief persistence. Further studies are needed to confirm our findings.
Keywords: epidemiology, mental health, end of life, families, geriatrics
Introduction
Bereavement has been cited as one of the most traumatic life events (Clark & Georgellis, 2013). Death of a loved one is associated with severe stress and increased risk of occurrence of depressive symptoms, major depressive episodes, anxiety-related disorders (Alexopoulos, 2005; Kreicbergs, Valdimarsdottir, Onelov, Henter, & Steineck, 2004; Mendes de Leon, Kasl, & Jacobs, 1994; Prigerson et al., 1997), impaired immune function (Zisook et al., 1994), lower quality of life (Grimby, 1993), suicide, and increased risk of mortality (Kaprio, Koskenvuo, & Rita, 1987). After 6 to 12 months, most bereaved persons will adapt to the loss with a reduction in grief intensity and a return to a different but meaningful and satisfying life without the deceased (Bonanno et al., 2002; Prigerson et al., 2009). However, for some bereaved individuals, the adaptation might be complicated, slowed, or halted, leading to persistence of grief (Boelen & van den Bout, 2008; Shear et al., 2007). Persistent grief is associated with functional impairment, sleep disturbances, high-risk behaviors, and increased risk of cancer and cardiovascular disease (Simon et al., 2005; Simon et al., 2007). It is therefore important to identify the factors associated with persistent grief to identify the population at risk of developing prolonged or complicated grief in need of support and adequate treatment. Several factors have been suggested to influence the duration and severity of grief. First, the effects of grief on morbidity and mortality are greater for the widowers in the acute grieving period because women benefit more from social support (Stroebe, 2001). Likewise, with respect to gender differences in coping styles, women are more confronted and expressive of their emotions than men. That can be a predisposition for their better recovery (Stroebe & Stroebe, 1983). Second, due to life experience, people develop better coping strategies. Tempestuous emotions tend to be damped down, and it is less common for people to respond excitable to worries. The previous study showed that restlessness symptom was significantly higher in young widows and the irritability symptom showed an interaction effect—high for young (sudden death) and middle-aged (prolonged grief) widows (Ball, 1977). Thirdly, race influenced the grief severity. Previous study (Fitzpatrick & Tran, 2002) revealed that bereavement was a significant factor affecting the health of White Americans, particularly in the youngest and oldest age groups. However, no bereavement effects were observed among African Americans within any of the age groups. These findings raise questions as to the differential effects of bereavement between different races. Fourth, in the acute grieving phase, lower educated people had worse coping skills, while in prolonged grief, education level was no longer significant (Boelen, van den Bout, & de Keijser, 2003). This might be due to lack of intellectual capability to work on a coping system or lack of possibilities to seek comfort in spiritual and intellectual aspects of life and social networks. Fifth, employment might play a role in younger or middle-aged adults, but in elderly, it helps dominantly as an additional source for seeking peers for social networking after a loss event. Also, working people might experience difficulties going back to work while suffering severe grief due to fear of underperforming. Sixth, spousal bereavement increases the grief severity. The previous study shows that elderly participants who lost their spouse had a higher risk of developing complicated grief when compared with participants losing someone else (Fujisawa et al., 2010). Next, bereaved spouses with prolonged grief had difficulty accessing positive memories of the deceased, and higher recalled marital adjustment. (Mancini, Sinan, & Bonanno, 2015). Mood-incongruency effects are due to a mood-regulatory process in which people retrieve memories to repair moods. :: The fact that one is not able to retrieve negative but only positive memories, increases the severity of grief. The same phenomenon is present in the more positive recalled marital adjustment when people tend to forget or repress the negative memories. Rumination keeps refocusing the griever on the thought of the deceased. Equally important for grief severity, experiential avoidance of situations that serve as reminders of the loss is also common. All of the above have been implicated as predictors of prolonged grief (Morina, 2011). Also, studies report severe depressive symptoms to be associated with prolonged grief, but findings have not been consistent (Tsai et al., 2016; Tsuboya et al., 2016). Most of the studies examine factors associated with grief severity and persistence solely on the basis of spousal bereavement, while other types of loss events have not been explored. Although health-related factors, both physical and mental (Onrust, Cuijpers, Smit, & Bohlmeijer, 2007), have been hypothesized to influence duration and severity of grieving, few longitudinal studies have examined their role in grief persistence among older adults. Grieving has been reported to differ by age, given the differential circumstances and mechanisms of adaptation that might occur within individuals at different stages of mental maturation. Mortality risk increases with age. Consequently, the probability of losing a spouse or partner also increases. Loss of a spouse or partner, might result in transferring dependency to others in the family or to the social surrounding .Elderly bereaved often lacks the necessary social support. This desolation further aggravates the grief process. Previous longitudinal studies on this topic had short follow-up (up to 24 months) and did not explore the determinants of grief related to long-term bereavement and different kind of loss (Bonanno et al., 2002; Prigerson et al., 2009; Tsai et al., 2016; Zisook, Paulus, Shuchter, & Judd, 1997; Zisook & Shuchter, 1991; Zisook et al., 1994). Therefore, our aim was to examine cross-sectionally factors associated with grief severity in adults aged 55 years and older taking into account all kind of kinship and also loved ones (not family related). Furthermore, we aimed to determine whether these factors were associated with grief persistence using a longitudinal data.
Method
Settings and Study Population
The study was performed within the framework of the Rotterdam Study, a population-based cohort, among persons 55 years and older living in the Ommoord district of Rotterdam, the Netherlands. The rationale and design of the Rotterdam Study is described elsewhere (Hofman et al., 2013). In brief, in 1990 all inhabitants of a well-defined district of Rotterdam were invited (RSI) and in 2000 an additional 3011 participants were enrolled (RSII), consisting of all persons living in the study district who had become 55 years of age. There were no eligibility criteria to enter the Rotterdam Study cohorts except the minimum age and residential area based on ZIP codes. The Rotterdam Study has been approved by the medical ethics committee according to the Population Screening Act: Rotterdam Study, executed by the Ministry of Health, Welfare and Sports of the Netherlands. All participants in the present analysis provided written informed consent to participate and to obtain information from their treating. Baseline measurements were performed in the fourth visit of the first cohort (RSI-4 year 2002-2004, n = 3,554) and the first visit of the second cohort (RSII-2 year 2004-2005; n = 2,468). Overall, there were 6,018 eligible participants (Figure 1). Of these participants, 597 persons did not answer whether they had experienced a death that they were still grieving (consequently, they did not undergo an Inventory of Complicated Grief [ICG] interview). Additionally 1,146 participants were excluded because of cognitive impairment defined as a score ≤26 on the Mini-Mental State Examination (MMSE; Folstein, Folstein, & McHugh, 1975). Of the remaining 4,275 participants, 3,469 were classified as nongrievers: participants who replied negative to the question, “In the past years, have you lost someone who you still grieve over?” or they did not answer sufficiently the ICG interview (less than 75% of the answers was present), leaving 771 (468 from RSI-5 and 303 from RSII-3) persons who constituted the study population. Furthermore, 73 participants died during the follow-up period and out of 698 eligible, 223 persons did not complete the grief questionnaire (lost to follow-up), leaving 475 persons who constituted the follow-up study population. Follow-up measurements were performed in the fifth visit of the first cohort (RSI-5, year 2009-2011) and the second visit of the second cohort (RSII-3 year 2011-2012). The same grief questionnaire was administered at baseline and a follow-up exam with average time of 6.3 years between baseline and follow-up assessment.
Figure 1.
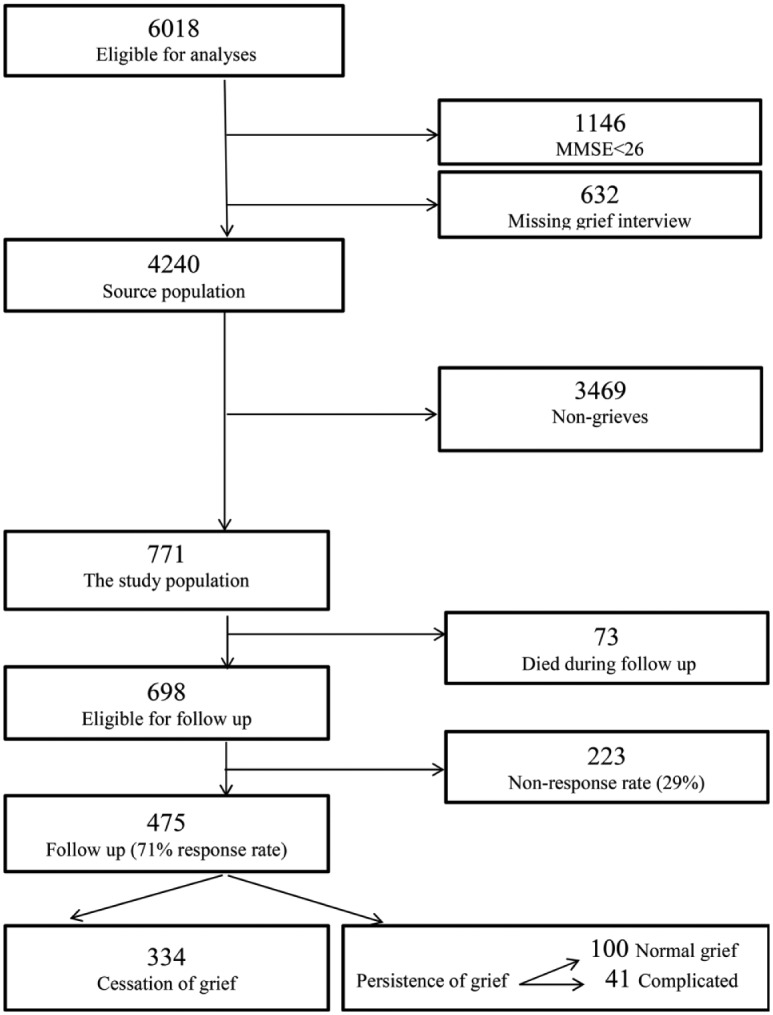
Characteristics of study participants: For cross-sectional and longitudinal analyses.
Note. MMSE = Mini-Mental State Examination.
Assessment of Grief–Interview of Complicated Grief (ICG)
Complicated grief was diagnosed with a Dutch version of the 19-item ICG (Prigerson et al., 1995). Participants underwent face-to-face interviews. They were first asked whether in the past years they had lost someone whom they were still grieving over. If yes, these participants were classified as grievers and were further assessed with the ICG to measure grief severity. Complicated grief symptoms were assessed as present among participants who scored equal or greater than 22 on the ICG score and grieved longer than 6 months (Newson, Boelen, Hek, Hofman, & Tiemeier, 2011; Saavedra Perez et al., 2015). ICG is composed to represent symptoms of complicated grief such as those in the most recent proposed criteria for the condition (Newson et al., 2011; Prigerson et al., 2009; Shear et al., 2011). Among the described symptoms are yearning for the lost person, anger over the death, distrust and detachment from others as a consequence of a death, survivor guilt, and loneliness. The measure has a high internal consistency and convergent and criterion validity, and it is the gold standard for measurement of complicated grief in older adults (Boelen, Van Den Bout, De Keijser, & Hoijtink, 2003). The inventory represents a single underlying construct of complicated grief (Boelen & Hoijtink, 2009). The original ICG consisted of 19 questions. Responses were provided on a 5-point scale to reflect an increase in severity (0 = never, 1 = seldom, 2 = sometimes, 3 = often, 4 = always; Prigerson et al., 1995). In this study, one item from the original inventory, “I feel bitter over this person’s death,” was removed from the original ICG as a pilot study revealed that this sentiment had the same meaning within the Dutch language as the included item, “I feel anger over this person’s death” (Boelen et al., 2003) Two further items (relating to seeing and hearing the deceased) were collapsed into one due to their similarity after a pilot study indicated these symptoms were low in frequency and often overlapped (“I hear the voice of, or see, the person who died”; Boelen et al., 2003). Furthermore, at the baseline we collect the date of the loss event to identify complicated grievers (complicated grief defined as grieving longer than 6 months from the time of the death). No limit for the time since loss was set. : In our pilot study we found that adults may grieve over the loss of a dear one even more than 20 years. This provides the time frame for experienced loss. Information about the deceased person was obtained with question, “Who is the dear one you have lost?” Answers were subdivided into “Loss of the spouse (reference group),” “Loss of the child,” “Loss of the others” (defined as one of the parents, a brother/a sister (Fujisawa et al., 2010), another family member, good friend, another dear person (not described relation-wise so far), multiple deaths (including a spouse and/or child or not including a spouse and/or child; Table 1).
Table 1.
Characteristics of Study Participants: For Cross-Sectional and Longitudinal Analyses.
| Grievers (n = 771) | Cessation of grief (n = 334) | Continuous grief (n = 141) | |
|---|---|---|---|
| Age (years), M (SD) | 72.6 (7.6) | 70.0 (6.6) | 70.0 (6.4) |
| Gender (female), % | 73 | 73 | 81 |
| Education | |||
| Primary, % | 11 | 6 | 11 |
| Intermediate, % | 76 | 79 | 73 |
| High, % | 13 | 15 | 16 |
| Depressive symptoms score, M (SD) | 8.8 (8.6) | 7.1 (7.2) | 10.5 (10.9) |
| Activities of daily living problems score, M (SD) | 0.5 (0.5) | 0.4 (0.4) | 0.5 (0.5) |
| Social support score, M (SD) | 9.2 (1.4) | 9.3 (1.5) | 9.3 (1.3) |
| Diagnosed MDD, % | 4 | 2 | 8 |
| Who died? | |||
| Partner (reference), % | 50 | 56 | 45 |
| Child, % | 11 | 9 | 14 |
| Other, % | 39 | 36 | 41 |
| Psycholepticsa use, yes vs. no, % | 20 | 14 | 24 |
Note. Values are presented as mean (SD) or percentage. MDD = major depressive disorder.
Psycholeptics includes benzodiazepines, antidepressants, neuroleptics, and anticonvulsants.
Assessment of Potential Factors Associated With Grief
Age, sex, education, cognitive functioning, activities of daily living, body mass index (BMI), use of psycholeptics, and the presence of comorbidities and depressive symptoms were considered as potential confounders and assessed at the baseline examination. Education was defined as low (primary education, lower vocational education and/or lower/intermediate general education), intermediate (intermediate vocational education and/or higher general education), or high (higher vocational education or university). Information about the deceased person was obtained with the question: “Who is the dear one you have lost?” Answers were subdivided into loss of a partner, loss of a child, or other. Social support was assessed with social support interview, a self-reported questionnaire (Meltzer, Gill, Pettricrew, & Hinds, 1995). The social support interview consists of five self-rated questions; answers scored equally for each question, on a 3-point scale (0 = not true, 1 = partly true, 2 = certainly true) to yield a global score of maximum 10 points. A higher score indicates the better level of social support. Depressive symptoms were assessed with a valid Dutch version of the Centre for Epidemiological Studies Depression (CES-D) scale (range = 0-60) where people score over 16 points (cutoff defined as score ≥ 16 points) identified persons with the clinically relevant depressive symptom (Beekman, 1997). The ability to perform activities of daily living was measured with the Stanford Health Assessment Questionnaire (Bruce & Fries, 2003; Fries, Spitz, & Young, 1982) that measures disability in eight fields (dressing and grooming, rising, reach, hygiene, eating, walking, grip, and activity). A Disability Index (DI) from 0.50 to 1.00 was considered as mild disability, while a DI of 1.00 or higher was regarded as a severe disability (Odding, Valkenburg, Stam, & Hofman, 2001). Psycholeptic drug use data were obtained from the Rotterdam Study pharmacies network at the baseline. This information was later on verified by a physician/cabinet check. Psycholeptics included benzodiazepines, antidepressants, neuroleptics, and anticonvulsants (Hofman et al., 2013; Stricker & Stijnen, 2010). Cognitive functioning was measured using the MMSE, during the baseline visits (Folstein et al., 1975). Participants with an MMSE score < 26 were excluded from the study. All comorbidities were assessed at the baseline by medical history, home interview, or by a clinician, and later on validated by relevant clinical test (if necessary). Comorbidities were categorized as present or absent and included one or more of the prevalence of diabetes mellitus, heart failure, stroke, myocardial infarction, chronic obstructive pulmonary disease (COPD), and joint problems that include osteoarthritis, rheumatoid arthritis gout, back pain, and ankylosing spondylitis. Diabetes mellitus was defined as a fasting glucose level of ≥7.0 mmol/L or use of blood glucose–lowering medication. Prevalent heart failure at baseline was measured using a validated score that was based on the heart failure definition of the European Society of Cardiology. A history of stroke was determined by interview or proxy informant interview. Confirmation of stroke diagnosis by a treating physician was required. A previous myocardial infarction was determined using an electrocardiogram. Diagnosis of COPD was confirmed by spirometry. Joint problems were obtained from home interview and a physician also measured the participants for joint complaints. Radiographic assessment for the diagnosis of osteoarthritis and rheumatoid arthritis were made at the research center. The presence of major depressive disorder (MDD) was assessed using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) interview. The SCAN is a set of tools created by World Health Organization aimed at diagnosing and measuring mental illness that occur in adult life (Wing et al., 1990). This semistructured clinical interview was performed by trained clinician to determine which participants fulfilled the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association, 1994), criteria for MDD.
Statistical Analyses
Continuous variables were reported as mean ± SD unless stated otherwise, and categorical variables were presented as percentages. Multivariable linear regression models were used to determine the cross-sectional association between potential determinants and ICG score.
In our cross-sectional and longitudinal analyses, each potential factor was first analyzed in models adjusted for age and gender (basic adjusted model), followed by analyses that were additionally adjusted for all potential factors (fully adjusted model). For the longitudinal association on potential predictors of grief persistence, logistic regression models were used (the outcome was dichotomized: complicated grief at follow-up and griever but not-complicated grief at follow-up, the last being the reference group) because standard transformations did not achieve a near normal distribution (more than 70% had an ICG score of 0 at follow-up). No multicollinearity was observed in any of our analysis as assessed by variance inflation factor (all values were <1 and cannot inflate Type I error).
To examine whether the presence of a depressive disorder could influence the results, we re-ran all analyses excluding individuals with MDD at baseline. We also examined potential interaction terms before running fully adjusted models. To examine the potential selection bias, we perform sensitivity analysis testing whether there was any significant difference in characteristics between responders and nonresponders at follow-up examination. Furthermore, we explored for potential outliers and whether there was any violation of assumptions, but we did not find any issue related to these two aspects of the analysis. Also, to test the association between more severe bereavement and potential factors, we repeated the prospective logistic regression analyses including only those participants who had complicated grief at baseline (persistence vs. cessation as a reference group). To adjust for the potential bias associated with missing data, we used multiple imputation procedures (n = 5 imputations). Rubin’s method was used for the pooled regression coefficients (β) and 95% Confidence Intervals. The percentage of missing values within the population for the analyses was lower than 3% (ranging from 0% to 2%). The percentage of missing values within our study population was lower than 3% (ranging from 0% to 2%). Age, sex, cognitive score, MDD, CES-D, and comorbidities had no missing values; activities of the daily living score had 0.4%; psycholeptics drugs had 0.5%; and education had 2%. Analyses were performed using SPSS Statistics (version 20; SPSS, Chicago, IL, USA).
Results
Table 1 presents the characteristics of the study population for cross-sectional and longitudinal analyses. Mean age of study participants was 72.7 years. Half of study participants had lost their partner (50%), 11% lost a child, and 39% lost someone else (parent, sibling, cousin, friend, or someone else participants felt close to). MDD was present in 4% participants. The majority of the study participants had depressive symptoms with the value of below 16 points and mild problems in activities of daily living (Table 1).
Table 2 shows the results of the cross-sectional association between potential correlates and ICG score In our fully adjusted models, female sex (β = 1.94, 95% CI: [0.35, 3.52]), loss of the child (β = 4.24, 95% CI: [1.91, 6.58]) or of the other dear person (β = −3.56, 95% CI: [−5.07, −2.04]), higher depressive symptoms score (β = 0.46, 95% CI: [0.37, 0.55]), middle (β = 3.14, 95% CI: [1.04, 5.23]) and primary education level (β = 4.81, 95% CI: [1.89, 7.73]), were associated with higher ICG score. More difficulties in activities of daily living were associated with lower levels of ICG score (β = −2.20, 95% CI: [−3.69, −0.71]).
Table 2.
Factors Associated With Grief Severity: Cross-Sectional Analysis Grief Severity at the Baseline–ICG Score.
| Factors | Model 1a |
Model 2b |
||||
|---|---|---|---|---|---|---|
|
n = 771 |
n = 771 |
|||||
| B | 95% CI | p | B | 95% CI | p | |
| Gender (female) | 0.35 | [−1.30, 2.00] | .68 | 1.94 | [0.35, 3.52] | .02 |
| Age, per year increase | 0.07 | [−0.02, 0.17] | .13 | −0.06 | [−0.16, 0.04] | .24 |
| Grief severity at the baseline, per unit increase | ||||||
| Social support, per unit increase | −0.70 | [−1.23, −0.18] | .009 | −0.28 | [−0.72, 0.26] | .36 |
| Who died? | ||||||
| Partner (reference), % | reference | — | — | reference | — | — |
| Child, % | 2.44 | [−0.01, 4.90] | .05 | 4.24 | [1.91, 6.58] | ≤.001 |
| Other, % | −5.32 | [−6.88, −3.76] | ≤.001 | −3.56 | [−5.07, −2.04] | ≤.001 |
| Depressive symptoms, per 1 point of score | 0.48 | [0.40, 0.56] | ≤.001 | 0.46 | [0.37, 0.55] | ≤.001 |
| Education | ||||||
| High (reference), % | reference | — | — | reference | — | — |
| Middle, % | 3.21 | [0.91, 5.50] | .006 | 3.14 | [1.04, 5.23] | .003 |
| Primary, % | 5.07 | [1.89, 8.26] | .002 | 4.81 | [1.89, 7.73] | .001 |
| Activities of daily living problems, score | 0.19 | [−1.34, 1.73] | .80 | −2.20 | [−3.69, −0.71] | .004 |
| Psycholepticsc use, yes vs. no (%) | −3.70 | [−5.58, −1.81] | ≤.001 | 0.83 | [−0.96, 2.63] | .36 |
| Comorbidities,d yes vs. no %) | 0.49 | [−1.03, 2.01] | .53 | 0.02 | [−1.40, 1.44] | .98 |
| Cognitive functioning, MMSE, score | −0.66 | [−1.27,−0.06] | .03 | −0.30 | [−0.86, 0.26] | .30 |
Note. CI = confidence interval; ICG = Interview of Complicated Grief; MMSE = The Mini-Mental State Examination test for cognitive impairment.
Model 1 was adjusted for gender and age for each covariate.
Model 2 was adjusted for all listed covariates.
Psycholeptics includes benzodiazepines, antidepressants, neuroleptics, and anticonvulsants.
Comorbidities includes the prevalence of myocardial infarction, heart failure, stroke, joint problems that include osteoarthritis, rheumatoid arthritis gout, back pain and ankylosing spondylitis, chronic obstructive pulmonary disease, and diabetes mellitus.
Bolded values represent all significant associations with P ≤ 0.05
After 6 years of follow-up, 475 (71%) of the 698 surviving participants underwent the ICG interview and were, therefore, included in our longitudinal analysis. Out of those, 334 participants reported complete cessation of grief and 141 still grieved. Out of grieving participants, 100 experienced normal grief and 41 complicated grief (Figure 1). In Table 3, we present the results of the prospective association of the correlates of grief severity with grief persistence (cessation as reference). In the age and gender-adjusted analyses, CES-D (OR = 1.04, 95% CI: [1.02, 1.07]) and the baseline value of ICG score were associated with grief persistence (OR = 1.06, 95% CI: [1.04, 1.08]); other correlates were not associated with grief persistence. In the fully adjusted analyses, baseline value of ICG score was associated with grief persistence (OR = 1.05, 95% CI: [1.03, 1.08]), while no association was observed for the other factors examined (Table 3).
Table 3.
Factors Associated With Grief Persistence: A 6-Year Longitudinal Analysis.
| Factors | Model 1a |
Model 2b |
||||
|---|---|---|---|---|---|---|
|
n = 141/475 |
n = 141/475 |
|||||
| OR | 95% CI | p | OR | 95% CI | p | |
| Gender (female) | 0.64 | [0.39, 1.06] | .08 | 0.67 | [0.39, 1.20] | .18 |
| Age, per year increase | 0.99 | [0.96, 1.02] | 0.62 | 0.98 | [0.95, 1.02] | .39 |
| Social support, per unit increase | 1.12 | [0.94, 1.34] | .20 | 1.19 | [0.98, 1.44] | .08 |
| Who died? | ||||||
| Partner (reference), % | reference | — | — | reference | — | — |
| Child, % | 1.22 | [0.61, 2.42] | .57 | 1.40 | [0.67, 2.92] | .65 |
| Other, % | 1.00 | [0.61, 1.63] | .99 | 1.13 | [0.67, 1.91] | .37 |
| Depressive symptoms,c per 1 point of score | 1.02 | [0.99, 1.04] | 0.17 | 1.02 | [0.99, 1.06] | .13 |
| Education | ||||||
| High (reference), % | reference | — | — | reference | — | — |
| Middle, % | 0.67 | [0.36, 1.23] | .20 | 0.72 | [0.38, 1.36] | .31 |
| Primary, % | 1.23 | [0.49, 3.08] | .66 | 1.47 | [0.56, 3.88] | .44 |
| Activities of daily living problems, score | 1.11 | [0.69, 1.81] | .66 | 0.90 | [0.52, 1.56] | .70 |
| Psycholepticsc use, yes vs. no | 0.73 | [0.42, 1.24] | .24 | 1.25 | [0.69, 2.28] | .46 |
| Comorbidities,d yes vs. no (%) | 1.41 | [0.92, 2.16] | .11 | 1.45 | [0.91, 2.29] | .12 |
| Cognitive functioning, MMSE, score | 1.08 | [0.90, 1.28] | .41 | 1.08 | [0.90, 1.30] | .41 |
| Baseline value of ICG, score | 1.06 | [1.04, 1.08] | ≤.001 | 1.05 | [1.03, 1.08] | ≤.001 |
Note. Grief persisted in 141 of 475 participants; 334 persons reported no grief at follow-up (reference category). OR = odds ratio; CI = confidence interval; MMSE = The Mini-Mental State Examination test for cognitive impairment; ICG = Interview of Complicated Grief.
Model 1 was adjusted for gender and age per covariant.
Model 2 was adjusted for all listed covariates.
Psycholeptics includes benzodiazepines, antidepressants, neuroleptics, and anticonvulsants.
Comorbidities includes the prevalence of myocardial infarction, heart failure, stroke, joint problems that include osteoarthritis, rheumatoid arthritis gout, back pain and ankylosing spondylitis, chronic obstructive pulmonary disease, and diabetes mellitus.
Next, we performed a series of sensitivity analyses. First, we excluded persons with major depression from our study population and reran the analysis (Supplement Table A).; our result remained essentially unchanged. Then we limited the cases to those who experienced continuous complicated grief (non grievers as the reference group) and reran the longitudinal analyses(data not shown). Again, our result remained essentially unchanged. Last, to test for selection bias, we tested whether there was any significant difference in characteristics of the population between responders and nonresponders to follow-up exam. Compared with responders, nonresponders were more likely to be men, older age, and lower education; have more depressive symptoms, higher comorbidities, lower activities of daily living score, lower cognitive score, higher ICG score; and reported more use of psycholeptic medications (Supplement Table B).
Discussion
In this population-based study of middle-aged and elderly persons, we investigated the factors related to grief severity in cross-sectional analyses and the determinants of grief persistence in longitudinal analyses. Our cross-sectional findings showed that grief severity was associated with female sex, having low to intermediate education level, the presence of depressive symptoms, and loss of a partner or a child, while more difficulties in daily living activities were associated with less grief severity. In this study of elderly individuals, several factors are associated with grief severity in our cross sectional analyses. These gender differences are based on the fact that females have better compliance and response to the social support/network (Trofimova, 2013).Stroebe et al. (2001) reports gender differences in the efficacy of different types of counseling, showing systematically gender differences in the needs and benefits of bereaved men compared with bereaved women: Widowers benefit more from emotion-focused interventions, while widows benefit more from problem-focused interventions. However, the only determinant of grief persistence after an average follow-up of more than 6 years was a lower severity of baseline grief. Similar to our results, previous studies have reported that women grieve more frequently and in a more complicated way than men (Ofstedal, Reidy, & Knodel, 2004). Beneria and Permanyer (2010) conducted an in-depth analysis of 43 participants (21 males and 22 female) at a Monrovia college fair. Findings revealed that men would rather not talk about grief because talking about the deceased would not help the situation while women thought otherwise. Women considered interiorizing the loss was a bad thing and consider being extroverted about grief a positive way of dealing with it. Moreover, any emotional expressions about a loss were recognized as weakness in men but not in women (Beneria & Permanyer, 2010). Other studies reported a higher level of bereavement among elderly women (Ofstedal et al., 2004). Second, we observed an association between kinship (who died) and grief severity. The spousal bereavement is reported as one of the most stressful events that anyone might experience, although its impact might diminish later in life than when it occurs during young adulthood or middle age (Holmes & Rahe, 1967; Moss, Moss, & Hanson, 2001). Two previous studies reported that even older bereaved spouses have higher rates of mortality and morbidity, impaired immune system, more depressive symptoms, more chronic conditions, and functional disabilities (Buckley et al., 2012; Fiske, Wetherell, & Gatz, 2009; Shahar, Schultz, Shahar, & Wing, 2001). Bonanno et al. (2002) stated that almost everyone experiences an initial increase in grief symptoms, but for most people, these symptoms subside 18 months after the loss. Resilient widows and widowers generally are more accepting of death, more extraverted, more emotionally stable, and less dependent on spouses than their nonresilient peers (Spahni, Morselli, Perrig-Chiello, & Bennett, 2015). As about 50% of our participants experienced loss of the partner, we defined spousal bereavement as the reference group when studying the association between kinship and severity of grief. In the current study, loss of the partner is negatively associated with severity of grief, but we did not find a longitudinal association between kinship and grief persistence. Third, we found that difficulties in activities of daily living were associated with less grief severity. Current literature in the field suggests that the more a person is active prior to spousal death, the easier the adjustment process may be (Utz, Carr, Nesse, & Wortman, 2002). Documenting the effects of widowhood on physical function and activity of older adults is important because significant declines may place individuals at risk for compromised health (Utz et al., 2002). It is important to note that persistent strains prior to spousal loss (caregiving responsibilities) affect the well-being of widowed elders (Schulz et al., 2001) and likely affect their willingness and ability to engage in the activity (Utz et al., 2002).
Differences between our findings and those available in the literature might be due to the timing of measurement of disabilities and grief as the directionality of the presence of both cannot be disentangled adequately at baseline. Furthermore, our results were only observed once we adjusted for depressive symptoms. Thus, our findings must be interpreted as the direct effect of activities of daily living on grief severity once the indirect effect via depressive symptoms is controlled for. Also, there might be other factors explaining these associations that were not collected during baseline examination (e.g., environmental, social capital, networks) and that could add residual confounding to our analyses and results. It is important to note that persistent strains prior to spousal loss (caregiving responsibilities) affect the well-being of widowed elders (Schulz et al., 2001) and likely affect their willingness and ability to engage in activity (Utz et al., 2002). However, more longitudinal studies are needed to examine the levels of physical function and activity prior to spousal death as well as after spousal death in relation to grief severity and persistence. Furthermore, we would like to tackle with several points to raise awareness of the further possibility for research questions. Namely, we would like to point out several possibly relevant predictors of the grief that are not assessed in the current study: coping style, relationship with deceased (not kinship but closeness to the observed/interviewed person), and do on. Also, we noticed that predictors vary by group, that there is interaction triggered by whom you lost, as well as gender. Unfortunately, we have no power to detect mentioned interaction. Furthermore, grief severity captures many aspects and includes information on potential predictors such as depression which opens a “chicken or egg” dilemma—what comes first. Further studies are necessary to assess predictors before bereavement, in particular, complicated grief. In the current study, reverse causality obscures relation that could otherwise have been observed (given the data set availability).
In the longitudinal analysis, we observed that the baseline value of ICG score was independently related to grief persistence, whereas no independent associations were observed between CES-D and other correlates with grief persistence. Contrary to the CES-D questionnaire that assesses overall feelings of sadness and melancholy, the ICG questionnaire assesses specific coping abilities to loss of the loved one. We hypothesize that the baseline severity of grief captures psychological features that predict grief cessation such as poor coping, anger, and detachment from others. Bereaved individuals with good coping abilities might change their lifestyle leading to empowerment of self and present relationships, creating new ones, while preserving health and well-being (Neimeyer, 2006). However, further studies are needed to investigate whether different coping mechanisms are related to grief severity and duration.
Our prospective findings imply that complicated grief is a dynamic condition/state that changes over time. Though the previous study stated that up to 40% of grievers never recover and stay in complicated grief, for the rest of the grievers it is expected that the symptoms get less severe (ICG < 22) or that they even completely stop feeling the grief (Goldsmith, Morrison, Vanderwerker, & Prigerson, 2008; Ott, Lueger, Kelber, & Prigerson, 2007; Piper, Ogrodniczuk, Azim, & Weideman, 2001; Prigerson et al., 1995). Our findings indicate that 7 out of 10 participants did not report any symptoms of complicated grief at follow-up which is in line with previous studies (Goldsmith et al., 2008; Ott et al., 2007; Piper et al., 2001; Prigerson et al., 1995). The major strengths of this study are prospective design and the population-based setting. To the best of our knowledge, this is the study with the longest follow-up to explore the determinants of grief and complicated grief in a population-based study of older adults. Furthermore, this study did not restrict the relationship of the person who died to the participant. We took in an account all kinds of kinship and also loved ones (not family related). We took in an account all kinds of relationships wit dear persons (both familly and not-family). Period after the loss event triggering grief, varies greatly among our participants (oldest date of loss event: was July 15 th, 1947, while the date of the most recent lost event was December 15th, 2011). Within this interval, we have people who grieve over 60 years. This long postdeath period is also a strength of our study because it reflects the variation of the time frame of grief in the general population and there is no evidence for an optimal cutoff to define maximum duration. Also, restriction of our analysis among participants, who scored lower than 26 points on MMSE, limited the possibility of misclassification of grieving status and/or recall bias. Furthermore, the interview was conducted face to face in the privacy of the participant’s own home by trained health care professionals and researchers, thus enhancing the reliability and validity of complicated grief measurement. There are also some limitations to our study that need to be considered. First, the screening question which determined who undertook the ICG allowed participants the opportunity to identify themselves as grievers, which may inadvertently result in an over- or underestimation of the number of grievers. However, in a pilot study, we found that nongrievers cannot meaningfully reply to the questions. We found differences in the group of participants grieving at the follow-up and the one that did not grieve anymore. Our nonresponse analysis showed that older persons and less healthy participants were more likely to be lost to follow-up. We might carefully infer that unhealthy persons were less likely to participate in the follow-up study, compared with the more healthy agers. Therefore, as inherent to all cohort studies, the possibility of health selection bias cannot be ruled out. This selection effect may bias our results and can impact generalizability to older and more frailer populations. Moreover, nearly all participants were of Caucasian descent. Therefore, the generalizability of our findings may be hampered. Another limitation of the current study might be the imprecise definition of grieving (asked within a time frame covering previous years which varies between participants) that did not consider individuals who experience someone’s death but did not feel that they were still grieving (emotional detachment from self as a modus of defend), and therefore selection bias might have been introduced. Also, while in the current study we have defined very precisely the state of complicated grief and persistent grief, there are challenges in operationalizing and distinguishing these conditions. Previous attempts have been taken to tackle this issue and different terms have been suggested, but a consensus has not been achieved yet (Boelen & Hoijtink, 2009). The continuation/persistence of all degrees of severity in grieving process needs more research effort in the future, in order to harmonize the definitions and distinctions between different grief status.
In conclusion, among elderly, grieving is a life event often experienced. Female sex, lower education, depressive symptoms, and loss of a partner or a child were associated with grief severity. Among those grieving approximately 25% had persistent grief after 6 years, which was associated with the severity of bereavement. Further longitudinal studies are needed to confirm and further explore our findings and to identify whether more potential predictors of grief severity and duration exist.
Supplementary Material
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Supplementary Material: The supplements for the article are available online.
References
- Alexopoulos G. S. (2005). Depression in the elderly. The Lancet, 365, 1961-1970. doi: 10.1016/S0140-6736(05)66665-2 [DOI] [PubMed] [Google Scholar]
- Ball J. F. (1977). Widow’s grief: The impact of age and mode of death. Omega: Journal of Death and Dying, 7, 307-333. [Google Scholar]
- Beekman A. T., Deeg D. J., Van Limbeek J., Braam A. W., De Vries M. Z., Van Tilburg W. (1997). Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): Cognition, structural brain changes and complicated grief results from a community-based sample of older subjects in The Netherlands. Psychological Medicine, 27, 231-235. [DOI] [PubMed] [Google Scholar]
- Beneria L., Permanyer I. (2010). The measurement of socio-economic gender inequality revisited. Development and Change, 41, 375-399. doi: 10.1111/j.1467-7660.2010.01648.x [DOI] [Google Scholar]
- Boelen P. A., Hoijtink H. (2009). An item response theory analysis of a measure of complicated grief. Death Studies, 33, 101-129. doi: 10.1080/07481180802602758 [DOI] [PubMed] [Google Scholar]
- Boelen P. A., van den Bout J. (2008). Complicated grief and uncomplicated grief are distinguishable constructs. Psychiatry Research, 157, 311-314. doi: 10.1016/j.psychres.2007.05.013 [DOI] [PubMed] [Google Scholar]
- Boelen P. A., van den Bout J., de Keijser J. (2003). Traumatic grief as a disorder distinct from bereavement-related depression and anxiety: A replication study with bereaved mental health care patients. The American Journal of Psychiatry, 160(7), 1339-1341. doi: 10.1176/appi.ajp.160.7.1339 [DOI] [PubMed] [Google Scholar]
- Boelen P. A., Van Den Bout J., De Keijser J., Hoijtink H. (2003). Reliability and validity of the Dutch version of the Inventory of Traumatic Grief (ITG). Death Studies, 27, 227-247. doi: 10.1080/07481180302889 [DOI] [PubMed] [Google Scholar]
- Bonanno G. A., Wortman C. B., Lehman D. R., Tweed R. G., Haring M., Sonnega J., . . .Nesse R. M. (2002). Resilience to loss and chronic grief: A prospective study from preloss to 18-months postloss. Journal of Personality and Social Psychology, 83, 1150-1164. [DOI] [PubMed] [Google Scholar]
- Bruce B., Fries J. F. (2003). The stanford health assessment questionnaire: A review of its history, issues, progress, and documentation. The Journal of Rheumatology, 30(1), 167-178. [PubMed] [Google Scholar]
- Buckley T., Sunari D., Marshall A., Bartrop R., McKinley S., Tofler G. (2012). Physiological correlates of bereavement and the impact of bereavement interventions. Dialogues in Clinical Neuroscience, 14, 129-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark A. E., Georgellis Y. (2013). Back to baseline in Britain: Adaptation in the British household panel survey. Economica, 80, 496-512. [Google Scholar]
- Fiske A., Wetherell J. L., Gatz M. (2009). Depression in older adults. Annual Review of Clinical Psychology, 5, 363-389. doi: 10.1146/annurev.clinpsy.032408.153621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick T. R., Van Tran T. (2002). Bereavement and health among different race and age groups. Journal of Gerontological Social Work, 37, 77-92. [Google Scholar]
- Folstein M. F., Folstein S. E., McHugh P. R. (1975). “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189-198. [DOI] [PubMed] [Google Scholar]
- Fries J. F., Spitz P. W., Young D. Y. (1982). The dimensions of health outcomes: The health assessment questionnaire, disability and pain scales. The Journal of Rheumatology, 9(5), 789-793. [PubMed] [Google Scholar]
- Fujisawa D., Miyashita M., Nakajima S., Ito M., Kato M., Kim Y. (2010). Prevalence and determinants of complicated grief in general population. Journal of Affective Disorders, 127, 352-358. [DOI] [PubMed] [Google Scholar]
- Goldsmith B., Morrison R. S., Vanderwerker L. C., Prigerson H. G. (2008). Elevated rates of prolonged grief disorder in African Americans. Death Studies, 32, 352-365. [DOI] [PubMed] [Google Scholar]
- Grimby A. (1993). Bereavement among elderly people: Grief reactions, post-bereavement hallucinations and quality of life. Acta Psychiatrica Scandinavica, 87, 72-80. [DOI] [PubMed] [Google Scholar]
- Hofman A., Darwish Murad S., van Duijn C. M., Franco O. H., Goedegebure A., Ikram M. A., . . .Vernooij M. W. (2013). The Rotterdam Study: 2014 objectives and design update. European Journal of Epidemiology, 28, 889-926. doi: 10.1007/s10654-013-9866-z [DOI] [PubMed] [Google Scholar]
- Holmes T. H., Rahe R. H. (1967). The Social Readjustment Rating Scale. Journal of Psychosomatic Research, 11, 213-218. [DOI] [PubMed] [Google Scholar]
- Kaprio J., Koskenvuo M., Rita H. (1987). Mortality after bereavement: A prospective study of 95,647 widowed persons. American Journal of Public Health, 77, 283-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreicbergs U., Valdimarsdottir U., Onelov E., Henter J. I., Steineck G. (2004). Anxiety and depression in parents 4-9 years after the loss of a child owing to a malignancy: A population-based follow-up. Psychological Medicine, 34, 1431-1441. [DOI] [PubMed] [Google Scholar]
- Mancini A. D., Sinan B., Bonanno G. A. (2015). Predictors of prolonged grief, resilience, and recovery among bereaved spouses. Journal of Clinical Psychology, 71, 1245-1258. [DOI] [PubMed] [Google Scholar]
- Meltzer H., Gill B., Pettricrew M., Hinds K. (1995). The prevalence of psychiatric morbidity among adults living in private households (OPCS Survery of Psychiatric Morbidity in Great Britain, Report 1). London, England: Her Majesty’s Stationery Office (HMSO). [Google Scholar]
- Mendes de Leon C. F., Kasl S. V., Jacobs S. (1994). A prospective study of widowhood and changes in symptoms of depression in a community sample of the elderly. Psychological Medicine, 24, 613-624. [DOI] [PubMed] [Google Scholar]
- Morina N. (2011). Rumination and avoidance as predictors of prolonged grief, depression, and posttraumatic stress in female widowed survivors of war. Journal of Nervous and Mental Disease, 199, 921-927. [DOI] [PubMed] [Google Scholar]
- Moss M. S., Moss S. Z., Hanson R. O. (2001). Handbook on bereavement research: Consequences, coping and care. Washington, DC: American Psychological Association. [Google Scholar]
- Neimeyer R. (2006). Making meaning in the midst of loss. Grief Matters: The Australian Journal of Grief and Bereavement, 9, 62-65. [Google Scholar]
- Newson R. S., Boelen P. A., Hek K., Hofman A., Tiemeier H. (2011). The prevalence and characteristics of complicated grief in older adults. Journal of Affective Disorders, 132, 231-238. [DOI] [PubMed] [Google Scholar]
- Odding E., Valkenburg H. A., Stam H. J., Hofman A. (2001). Determinants of locomotor disability in people aged 55 years and over: The Rotterdam Study. European Journal of Epidemiology, 17, 1033-1041. [DOI] [PubMed] [Google Scholar]
- Ofstedal M. B., Reidy E., Knodel J. (2004). Gender differences in economic support and well-being of older Asians. Journal of Cross-Cultural Gerontology, 19, 165-201. [DOI] [PubMed] [Google Scholar]
- Onrust S., Cuijpers P., Smit F., Bohlmeijer E. (2007). Predictors of psychological adjustment after bereavement. International Psychogeriatrics, 19, 921-934. [DOI] [PubMed] [Google Scholar]
- Ott C. H., Lueger R. J., Kelber S. T., Prigerson H. G. (2007). Spousal bereavement in older adults: common, resilient, and chronic grief with defining characteristics. The Journal of Nervous and Mental Disease, 195(4), 332-341 [DOI] [PubMed] [Google Scholar]
- Piper W. E., Ogrodniczuk J. S., Azim H. F., Weideman R. (2001). Prevalence of loss and complicated grief among psychiatric outpatients. Psychiatric Services, 52(8), 1069-1074. [DOI] [PubMed] [Google Scholar]
- Prigerson H. G., Bierhals A. J., Kasl S. V., Reynolds C. F., III, Shear M. K., Day N., . . .Jacobs S. (1997). Traumatic grief as a risk factor for mental and physical morbidity. American Journal of Psychiatry, 154, 616-623. doi: 10.1176/ajp.154.5.616 [DOI] [PubMed] [Google Scholar]
- Prigerson H. G., Horowitz M. J., Jacobs S. C., Parkes C. M., Aslan M., Goodkin K., . . .Maciejewski P. K. (2009). Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Medicine, 6(8), e1000121. doi: 10.1371/journal.pmed.1000121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prigerson H. G., Maciejewski P. K., Reynolds C. F., III, Bierhals A. J., Newsom J. T., Fasiczka A., . . .Miller M. (1995). Inventory of Complicated Grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research, 59, 65-79. [DOI] [PubMed] [Google Scholar]
- Saavedra Perez H. C., Ikram M. A., Direk N., Prigerson H. G., Freak-Poli R., Verhaaren B. F., . . . Tiemeier H. (2015). Cognition, structural brain changes and complicated grief. A population-based study. Psychological Medicine, 45(7), 1389-1399. doi: 10.1017/S0033291714002499 [DOI] [PubMed] [Google Scholar]
- Schulz R., Beach S. R., Lind B., Martire L. M., Zdaniuk B., Hirsch C., . . .Burton L. (2001). Involvement in caregiving and adjustment to death of a spouse: Findings from the caregiver health effects study. Journal of the American Medical Association, 28, 3123-3129. [DOI] [PubMed] [Google Scholar]
- Shahar D. R., Schultz R., Shahar A., Wing R. R. (2001). The effect of widowhood on weight change, dietary intake, and eating behavior in the elderly population. Journal of Aging and Health, 13, 189-199. [DOI] [PubMed] [Google Scholar]
- Shear K., Monk T., Houck P., Melhem N., Frank E., Reynolds C., Sillowash R. (2007). An attachment-based model of complicated grief including the role of avoidance. European Archives Psychiatry and Clinical Neuroscience, 257, 453-461. doi: 10.1007/s00406-007-0745-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon N. M., Pollack M. H., Fischmann D., Perlman C. A., Muriel A. C., Moore C. W., . . .Shear M. K. (2005). Complicated grief and its correlates in patients with bipolar disorder. Journal of Clinical Psychiatry, 66, 1105-1110. [DOI] [PubMed] [Google Scholar]
- Simon N. M., Shear K. M., Thompson E. H., Zalta A. K., Perlman C., Reynolds C. F., . . .Silowash R. (2007). The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Comprehensive Psychiatry, 48, 395-399. doi: 10.1016/j.comppsych.2007.05.002 [DOI] [PubMed] [Google Scholar]
- Spahni S., Morselli D., Perrig-Chiello P., Bennett K. M. (2015). Patterns of psychological adaptation to spousal bereavement in old age. Gerontology, 61, 456-468. doi: 10.1159/000371444 [DOI] [PubMed] [Google Scholar]
- Stricker B. H., Stijnen T. (2010). Analysis of individual drug use as a time-varying determinant of exposure in prospective population-based cohort studies. European Journal of Epidemiology, 25, 245-251. doi: 10.1007/s10654-010-9451-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe M., Stroebe W. (1983). Who suffers more? Sex differences in health risks of the widowed. Psychology Bulletin, 93, 279-301. [PubMed] [Google Scholar]
- Stroebe M. S., Stroebe W., Schut H. A. W. (2001). Gender differences in adjustment to bereavement: An empirical and theoretical review. Review of General Psychology, 5, 62-83. [Google Scholar]
- Trofimova I. (2013). A study of the dynamics of sex differences in adulthood. International Journal of Psychology, 48, 1230-1236. [DOI] [PubMed] [Google Scholar]
- Tsai W. I., Prigerson H. G., Li C. Y., Chou W. C., Kuo S. C., Tang S. T. (2016). Longitudinal changes and predictors of prolonged grief for bereaved family caregivers over the first 2 years after the terminally ill cancer patient’s death. Palliative Medicine, 30, 495-503. [DOI] [PubMed] [Google Scholar]
- Tsuboya T., Aida J., Hikichi H., Subramanian S. V., Kondo K., Osaka K., Kawachi I. (2016). Predictors of depressive symptoms following the Great East Japan earthquake: A prospective study. Social Science & Medicine, 161, 47-54. doi:http://dx.doi.org/10.1016/j.socscimed.2016.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utz R. L., Carr D., Nesse R., Wortman C. B. (2002). The effect of widowhood on older adults’ social participation: An evaluation of activity, disengagement, and continuity theories. The Gerontologist, 42, 522-533. [DOI] [PubMed] [Google Scholar]
- Wing J. K., Babor T., Brugha T., Burke J., Cooper J. E., Giel R., . . .Sartorius N. (1990). Schedules for Clinical Assessment in Neuropsychiatry (SCAN). Archives of General Psychiatry, 47, 589-593. [DOI] [PubMed] [Google Scholar]
- Zisook S., Paulus M., Shuchter S. R., Judd L. L. (1997). The many faces of depression following spousal bereavement. Journal of Affective Disorders, 45, 85-94; discussion 94-85. [DOI] [PubMed] [Google Scholar]
- Zisook S., Shuchter S. R. (1991). Depression through the first year after the death of a spouse. American Journal of Psychiatry, 148, 1346-1352. doi: 10.1176/ajp.148.10.1346 [DOI] [PubMed] [Google Scholar]
- Zisook S., Shuchter S. R., Irwin M., Darko D. F., Sledge P., Resovsky K. (1994). Bereavement, depression, and immune function. Psychiatry Research, 52, 1-10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


