Abstract
Background:
Recent evidence shows a delayed return to sport in children and delayed quadriceps recovery in both adults and children who have undergone anterior cruciate ligament (ACL) reconstruction with concomitant femoral nerve blockade (FNB) compared with those who had no blockade. We evaluated the use of adductor canal blockade (ACB), as an alternative to FNB, at the time of ACL reconstruction.
Hypothesis:
Patients who receive ACB will have greater isokinetic strength at 6 months postoperative compared with patients who receive FNB at the time of ACL reconstruction.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective record review was performed at a single academic medical center to identify all patients aged ≥16 years who had undergone ACL reconstruction with blockade between January 2010 and January 2015. Exclusion criteria included (1) non–sports medicine fellowship–trained surgeon performing the procedure, (2) continuous nerve catheter or concurrent epidural used, (3) revision ACL reconstruction or multiligament reconstruction as the index procedure, (4) previous contralateral ACL reconstruction, (5) concurrent microfracture, and (6) additional surgery within the 6-month outcome period that affected recovery. Isokinetic strength testing was performed using a computerized dynamometer, measuring total work at fast speed and peak torque at slow speed at 6 months; results were evaluated as a percentage of the nonoperative side. Multivariate regression analysis was used to evaluate the effect of block type on isokinetic strength outcome variables, controlling for age, sex, body mass index, graft type, and surgeon.
Results:
There were 230 patients receiving FNB and 30 patients receiving ACB included in the study. The multivariate regression analysis identified a greater side-to-side deficit in extension total work for the ACB group compared with the FNB group (P = .040), after controlling for age, sex, body mass index, graft type, and surgeon.
Conclusion:
Compared with FNB, ACB for ACL reconstruction is associated with a persistent fast-activation isokinetic strength deficit at 6 months after surgery. This is the first study to compare FNB to ACB, and results are concerning for patients planning an early return to sport.
Keywords: anesthesia/pain management, ACL, knee ligaments, knee, clinical assessment/grading scales, muscle physiology
Anterior cruciate ligament (ACL) reconstruction is one of the most commonly performed sports medicine procedures in the United States. Nearly all ACL reconstructions are performed in an outpatient setting, heightening the importance of safe and effective postoperative analgesia. Over the past decade, femoral nerve blockade (FNB) has been frequently utilized for this purpose. It has been shown to be efficacious in the early postoperative period, enhancing postoperative pain control.4,6,17 However, the recent literature has associated FNB with a prolonged return of quadriceps strength and a delayed return to sport after ACL reconstruction.10,16 Concern regarding these deleterious long-term effects has led to diminished enthusiasm for its continued use in the athletic population.
Recently, adductor canal blockade (ACB) has been introduced as an alternative to FNB, offering a potential reduction in quadriceps weakness because of the more distal administration of the anesthetic.19 It has found larger popularity in patients undergoing knee arthroplasty, in whom greater quadriceps strength in the acute postoperative period allows earlier ambulation, protects against falls, and facilitates discharge.8,9,14,15 In patients undergoing ACL reconstruction, ACB has been shown to produce less short-term (24 hours) quadriceps weakness compared with FNB, with similar analgesic efficacy.3,7 These short-term benefits suggest the potential utility of ACB as an alternative to FNB in patients undergoing ACL reconstruction. However, the long-term effects of ACB on quadriceps weakness have not yet been reported.
Therefore, we aimed to evaluate the effect of ACB on long-term quadriceps strength in patients undergoing ACL reconstruction. We evaluated isokinetic strength through standardized assessments at 6 months postoperative, comparing results in a group of patients who received single-injection ACB versus a group of patients who received single-injection FNB. We hypothesized improved strength in the setting of ACB versus FNB.
Methods
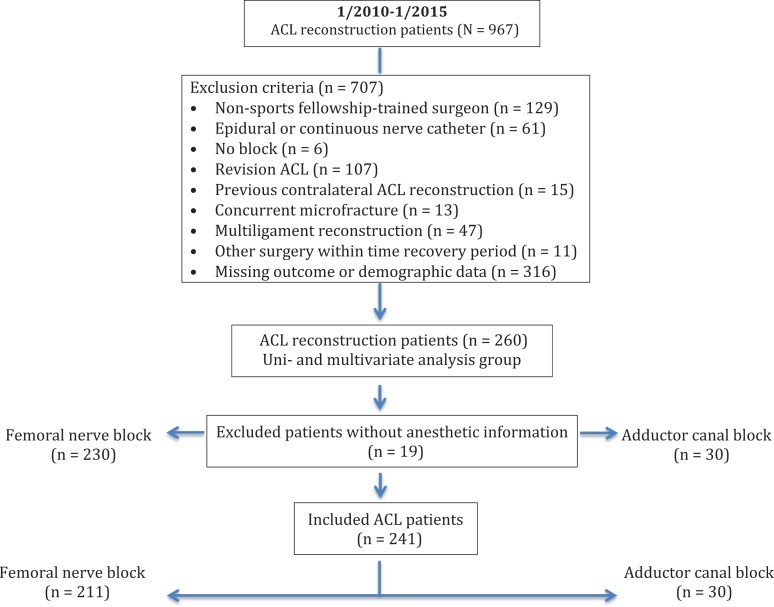
This retrospective record review was performed at a single academic medical center. After institutional review board approval, a data query was performed to identify all patients aged ≥16 years who underwent ACL reconstruction from January 2010 to January 2015. Electronic medical records were reviewed, and patients were excluded from this analysis if (1) surgery was performed by a non–sports medicine fellowship–trained surgeon; (2) surgery was accompanied by an epidural or continuous nerve catheter; (3) surgery was performed without the use of a regional block; (4) the index procedure was revision ACL reconstruction; (5) the patient had a prior contralateral ACL reconstruction, which precluded the use of the contralateral leg as a control for isokinetic strength assessments; (6) there was concurrent microfracture, which has been associated with adverse results; (7) the index procedure was multiligament reconstruction; (8) the patient had additional surgery within the 6-month outcome period that affected recovery (such as contralateral limb surgery); and/or (9) the outcome or baseline demographic data were incomplete. Finally, patients for whom inadequate information regarding the type and amount of anesthetic used (n = 19) were excluded. This yielded 211 patients receiving FNB and 30 patients receiving ACB for inclusion in the analysis, as detailed in Figure 1.
Figure 1.
Inclusion diagram. ACL, anterior cruciate ligament.
Demographic data were collected via an electronic medical record review, recording patient age at surgery, body mass index (BMI), sex, surgeon, graft type, anesthetic type and dose, and isokinetic evaluation at 6-month follow-up. Graft type was based on surgeon and patient preference. Although rehabilitation may have varied because of patient motivation, location, insurance benefits, and/or individual physical therapist expertise or preference, all patients were instructed to follow a standardized progression of exercise using institution-specific rehabilitation guidelines that are readily available online (https://www.uwhealth.org/files/uwhealth/docs/sportsmed/ACL-Protocol.pdf).
Isokinetic testing was performed 6 months postoperatively by a licensed, trained physical therapist using an instrumented dynamometer (Biodex Medical Systems). The testing protocol included a standardized warm-up, followed by flexion and extension assessments that measured total work at fast-activation speeds (240 deg/s) and peak torque at slow-activation speeds (60 deg/s). The patient was given the opportunity to use the machine before the recorded attempt to minimize potential errors associated with the learning curve. Testing was performed for both lower extremities, beginning with the uninjured extremity, and values were calculated for the operative side as a percentage of the nonoperative side, representing the deficit of operative leg strength.
FNB and ACB were administered by, or under the supervision of, a faculty anesthesiologist either preoperatively or immediately postoperatively. The choice of FNB or ACB and the timing of blockade (preoperative vs postoperative) were both based on surgeon preference. These regional blocks were dispensed in addition to general anesthesia and were administered for the purpose of providing postoperative analgesia. Blockade was performed using ultrasound or a nerve stimulator based on the preference of the anesthesiologist. FNB was performed near the inguinal crease, and ACB was performed in the distal thigh at the level of the adductor canal. Regional anesthetic agents included bupivacaine or ropivacaine with or without epinephrine. The volume and amount of anesthetic varied per the preference of the anesthesiologist. Bupivacaine and ropivacaine were treated as equivalent in a 1:1 ratio, and the volume was recorded as a covariate for the current analysis.
Statistical Analysis
Isokinetic strength data provided the outcome variables of primary interest. We report patient demographics, surgeon, graft type, anesthetic used, and isokinetic strength data as means and SDs, evaluating for differences between the groups using the t test and Fisher exact test. Univariate regression analysis assessed the effect of group on isokinetic strength outcomes. Multivariate analysis evaluated the following covariates: age, sex, BMI, graft type, surgeon, and anesthetic mass/volume; variables with P < .05 were included in the final analysis model. Anesthetic volume and mass were found not to have significance in the final model; therefore, patients for whom anesthetic volume and mass data were unavailable were also included in the main analysis. Data were analyzed using R software version 3.0.1, with significance set at P < .05.
Results
A total of 967 patients underwent ACL reconstruction during the study interval. After exclusion criteria were applied, data from 230 patients receiving FNB and 30 patients receiving ACB were available for analysis (Figure 1). Patient characteristics are reported, divided by block type, in Table 1. In summary, patients who received FNB were younger than those who received ACB (25.4 vs 28.9 years, respectively; P = .043), but there was no significant difference between block groups for sex distribution or BMI. Patients who received ACB were more likely to have a hamstring autograft than any other graft (P = .003). Other grafts included 4 Achilles allografts, 3 quadriceps tendon autografts, and 2 hybrid hamstring autografts with an allograft. Patients of surgeon 2 were more likely to receive FNB than were patients of surgeon 3, and surgeon 3 had a greater percentage of patients who received ACB than did surgeon 2 (P = .001). Patients who received FNB were given a significantly greater amount of regional anesthetic agent, in both volume and mass, than patients who received ACB (P < .001 for both).
TABLE 1.
Patient and Surgical Characteristicsa
| Femoral Nerve Blockade (n = 230) | Adductor Canal Blockade (n = 30) | P Value | |
|---|---|---|---|
| Age, y | 25.4 ± 9.1 | 28.9 ± 8.6 | .043 |
| Body mass index, kg/m2 | 25.8 ± 4.9 | 26.6 ± 4.8 | .404 |
| Female sex, n (%) | 101 (43.9) | 17 (56.7) | .261 |
| Surgeon, n (%) | .001 | ||
| 1 | 147 (63.9) | 18 (60.0) | |
| 2 | 74 (32.2) | 5 (16.7) | |
| 3 | 8 (3.5) | 5 (16.7) | |
| 4 | 1 (0.4) | 2 (6.7) | |
| Graft type, n (%) | .003 | ||
| Hamstring autograft | 135 (58.7) | 25 (83.3) | |
| Patellar autograft | 88 (38.3) | 3 (10.0) | |
| Other | 7 (3.0) | 2 (6.7) | |
| Anesthetic mass, mg | 106 ± 36 | 84 ± 31 | <.001 |
| Anesthetic volume, mL | 24.7 ± 5.4 | 20.9 ± 3.8 | <.001 |
aData are presented as mean ± SD unless otherwise indicated. Bolded P values indicate statistically significant between-group differences. Between-groups differences were determined by the t test and Fisher exact test.
According to the univariate analysis, the ACB group demonstrated greater side-to-side deficits than the FNB group for mean total work (fast activation) in both extension (25.8% vs 16.8%, respectively; P = .008) and flexion (21.4% vs 7.6%, respectively; P = .010), but there was no difference in peak torque percentage deficits (slow activation). According to multivariate analysis, after controlling for the covariates age, sex, BMI, graft type, and surgeon, greater deficits for total work in extension persisted for the ACB group compared with the FNB group (29.5% vs 22.0%, respectively; P = .040). Regression results are presented in Table 2.
TABLE 2.
Isokinetic Strength Deficit at 6 Months (Compared With Uninvolved Leg)a
| Femoral Nerve Blockade | Adductor Canal Blockade | P Value | |
|---|---|---|---|
| Univariate analysis | |||
| Extension at 60 deg/s | 25.9 (23.4-28.3) | 28.1 (21.4-34.8) | .537 |
| Flexion at 60 deg/s | 12.1 (10.2-14.0) | 14.6 (9.3-19.9) | .371 |
| Extension at 240 deg/s | 16.8 (14.6-19.1) | 25.8 (19.6-32.1) | .008 |
| Flexion at 240 deg/s | 7.6 (4.0-11.2) | 21.4 (11.5-31.3) | .010 |
| Multivariate analysis | |||
| Extension at 60 deg/s | 27.1 (20.8-33.5) | 31.2 (23.5-38.8) | .261 |
| Flexion at 60 deg/s | 12.3 (6.9-17.7) | 12.6 (6.1-19.1) | .920 |
| Extension at 240 deg/s | 22.0 (15.5-28.4) | 29.5 (21.6-37.3) | .040 |
| Flexion at 240 deg/s | 11.8 (1.8-21.8) | 16.3 (4.2-28.5) | .421 |
aData are presented in percentages as unadjusted (univariate) and adjusted (multivariate) mean (95% CI). Bolded P values indicate statistically significant between-group differences.
Discussion
We compared quadriceps strength at 6 months postoperatively in a group of patients who received ACB versus a larger group of patients who received FNB for perioperative analgesia at the time of ACL reconstruction. Deficits in extension strength were large at both slow-activation (60 deg/s) and fast-activation (240 deg/s) speeds for both groups of patients (17%-26%, unadjusted). After adjusting for age, sex, BMI, graft type, and surgeon, the side-to-side deficit in quadriceps strength at fast speed, as assessed by total work, was 7.5% worse for those who received ACB versus those who received FNB. Thus, in contrast to our hypothesis, ACB produced even greater long-term compromise in muscle function than FNB in this patient population.
For the past 5 years, sports medicine surgeons in our group have utilized FNB to provide perioperative analgesia for nearly all patients undergoing ACL reconstruction. However, recent reports have demonstrated delayed strength recovery after FNB. In pediatric and adolescent patients who received FNB for ACL reconstruction, Luo et al16 identified significant isokinetic deficits in knee extension and flexion strength compared with those who had no block. Patients in the FNB group had deficits in unadjusted isokinetic extension strength at fast speed (17.6% vs 11.2%, respectively; P = .01) and in isokinetic flexion strength at both fast (9.9% vs 5.7%, respectively; P = .04) and slow (13.0% vs 8.5%, respectively; P = .03) speeds; furthermore, patients who received FNB were less likely to meet return-to-sport criteria at 6 months.16 Similarly, in a group of adults who received 48-hour continuous FNB, Krych et al10 identified significant deficits in fast and slow extension strength, vertical jump, and single jump compared with patients who did not receive analgesic blockade (FNB deficit = 22%; no block = 15%, unadjusted). These findings led us to consider substituting ACB for FNB in patients undergoing ACL reconstruction. We hoped to provide the benefit of perioperative analgesia without the detriment of prolonged quadriceps weakness. However, the deficit in fast-speed extension strength identified in the present study is even larger after ACB (25.8%, unadjusted) than FNB (16.8%, unadjusted) and greater in magnitude than the FNB deficits previously reported by Luo et al16 (17.6%) and Krych et al10 (22%).
ACB has become a popular choice for patients undergoing total knee arthroplasty. Compared with FNB, ACB shows less quadriceps weakness in the early postoperative period, leading to fewer falls and a quicker return to postoperative ambulation.8,12 Jaeger et al8 found greater quadriceps strength in a group of patients who received ACB (52% of baseline) compared with those who received FNB (18% of baseline) at 24 hours after total knee arthroplasty. In a study of volunteers assessing quadriceps strength after blockade in the absence of a procedure, Kwofie et al12 identified no significant change from baseline quadriceps strength (99%) at 1 hour after ACB but a 41% deficit in the FNB group. In addition, poor balance, associated with an increased fall risk, was more prevalent in the FNB group. Although we are aware of no studies evaluating medium- or long-term quadriceps strength recovery after ACB in the total knee arthroplasty population, these short-term results suggest that ACB may be muscle sparing, providing the impetus for use in patients undergoing ACL reconstruction.
The distal injection site for ACB, by design, affects fewer motor branches of the femoral nerve than those affected by FNB. It is performed at the level of the adductor canal, with infiltration deep to the sartorius muscle. The adductor canal, also known as the Hunter canal, is an intermuscular tunnel in the middle third of the thigh, approximately 12 to 14 cm proximal to the knee. It is triangular in cross-section and is bounded by the vastus medialis, sartorius, and adductor magnus. It is encased by an aponeurosis, and its contents include the femoral artery and vein, a sensory branch of the obturator nerve, the saphenous nerve, and the motor nerve to the vastus medialis.2 Thus, with ACB, paralysis of the vastus medialis is possible. Adoni et al1 demonstrated a 36% decrease in short-term vastus medialis strength in patients who underwent “typical” ACB but no strength reduction in patients who received a more distal saphenous nerve block. These findings may explain the persistent strength deficit seen in our patients who received ACB in the typical location. Prolonged recovery in quadriceps strength after ACB may have been caused by neurotoxicity. Local anesthetics are neurotoxic at clinical doses, and this effect is concentration dependent.1 In our study, the quantity of anesthetic used for ACB was only 15% less than that used for FNB. The much smaller caliber of the nerve to the vastus medialis may have made it more vulnerable to the neurotoxic effects of the anesthetic dose. If so, recovery of this important portion of the quadriceps musculature would be delayed, potentially diminishing quadriceps strength at 6 months postoperatively. Future studies evaluating various anesthetic doses may shed further light on this phenomenon.
Although we found no significant difference between the block groups in slow-speed extension strength deficits, deficits in this parameter were large overall (27%-31%, adjusted) at the 6-month time point assessed in our study. Our findings are similar to those of Luo et al,16 who found deficits in fast but not slow extension strength for FNB versus no block, but dissimilar from those of Krych et al,10 who found deficits in both fast and slow extension strength after 48-hour FNB. In our experience, slow-speed extension strength recovers later than fast-speed extension strength after ACL reconstruction; thus, we suspect that testing at a later time point may have identified differential deficits in slow-speed extension strength for ACB versus FNB patients. Further study, evaluating patients at 9 and/or 12 months postoperatively, is necessary to assess this hypothesis.
Our study is limited by its retrospective nature. Because we did not randomize patients to separate ACB or FNB groups, selection bias may have been influential. The inclusion of patients from 4 surgeons introduced the possibility of differential results based on variations in the surgical technique. However, one surgeon (surgeon 1) performed the majority of procedures, and his patients accounted for a similar percentage of all patients who underwent each block technique (60% of all ACB and 63% of all FNB), minimizing the likelihood that our results were affected by this issue. In addition, our statistical technique (regression analysis) accounted for potential variations related to both surgeon and graft selection. The block groups demonstrated a significant between-group difference in age, with FNB administered in slightly younger patients than ACB. It has been previously shown that younger age is associated with higher isokinetic scores.11 Thus, although age was included as a covariate in our regression analysis, it is possible that our FNB group performed slightly better than the ACB group because they were younger. Finally, we did not include a “no blockade” group in our analysis, as we had an insufficient sample size for this group. Thus, we were only able to compare the ACB group with the FNB group and not with a “no blockade” group. A randomized, controlled prospective study comparing ACB with FNB and no blockade is necessary to fully address these potential issues and associations.
It is important to note that we evaluated patients only at a single time point, approximately 6 months postoperatively. We do not know whether the identified deficit in extension strength was persistent in these patients or whether recovery occurred sometime after the 6-month assessment. Even if the deficit completely cleared in subsequent months, the existence of an extension deficit at 6 months may be clinically significant. The recovery of extension strength is associated with improved function after ACL reconstruction.5,13,18 A delay in strength recovery, even if temporary, is likely to delay functional recovery and, in turn, could delay return to sport. Certainly, the use of an effective perioperative analgesic agent that does not delay recovery is preferred.
In summary, we identified a significantly greater side-to-side deficit in isokinetic extension strength at 6 months postoperatively in patients who received ACB compared with patients who received FNB at the time of ACL reconstruction. Further investigation is needed to explore longer term functional recovery, varying injection dosages, and comparison with no blockade. Nonetheless, these results are concerning and have led to a change in practice among our group of surgeons, who have abandoned the use of ACB, and in some cases all regional blocks, for ACL reconstruction.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the University of Wisconsin–Madison Minimal Risk Institutional Review Board (No. 2015-0479).
References
- 1. Adoni A, Paraskeuopoulos T, Saranteas T, Sidiropoulou T, Mastrokalos D, Kostopanagiotou G. Prospective randomized comparison between ultrasound-guided saphenous nerve block within and distal to the adductor canal with low volume of local anesthetic. J Anaesthesiol Clin Pharmacol. 2014;30(3):378–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Anagnostopoulou S, Anagnostis G, Saranteas T, Mavrogenis AF, Paraskeuopoulos T. Saphenous and infrapatellar nerves at the adductor canal: anatomy and implications in regional anesthesia. Orthopedics. 2016;39(2):259–262. [DOI] [PubMed] [Google Scholar]
- 3. Chisholm MF, Bang H, Maalouf DB, et al. Postoperative analgesia with saphenous block appears equivalent to femoral nerve block in ACL reconstruction. HSS J. 2014;10(3):245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dauri M, Fabbi E, Mariani P, et al. Continuous femoral nerve block provides superior analgesia compared with continuous intra-articular and wound infusion after anterior cruciate ligament reconstruction. Reg Anesth Pain Med. 2009;34(2):95–99. [DOI] [PubMed] [Google Scholar]
- 5. Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Edkin BS, Spindler KP, Flanagan JF. Femoral nerve block as an alternative to parenteral narcotics for pain control after anterior cruciate ligament reconstruction. Arthroscopy. 1995;11(4):404–409. [DOI] [PubMed] [Google Scholar]
- 7. El Ahl MS. Femoral nerve block versus adductor canal block for postoperative pain control after anterior cruciate ligament reconstruction: a randomized controlled double blind study. Saudi J Anaesth. 2015;9(3):279–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jaeger P, Zaric D, Fomsgaard JS, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med. 2013;38(6):526–532. [DOI] [PubMed] [Google Scholar]
- 9. Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesiology. 2014;120(3):540–550. [DOI] [PubMed] [Google Scholar]
- 10. Krych A, Arutyunyan G, Kuzma S, Levy B, Dahm D, Stuart M. Adverse effect of femoral nerve blockade on quadriceps strength and function after ACL reconstruction. J Knee Surg. 2015;28(1):83–88. [DOI] [PubMed] [Google Scholar]
- 11. Krych AJ, Woodcock JA, Morgan JA, Levy BA, Stuart MJ, Dahm DL. Factors associated with excellent 6-month functional and isokinetic test results following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;23(4):1053–1059. [DOI] [PubMed] [Google Scholar]
- 12. Kwofie MK, Shastri UD, Gadsden JC, et al. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk: a blinded, randomized trial of volunteers. Reg Anesth Pain Med. 2013;38(4):321–325. [DOI] [PubMed] [Google Scholar]
- 13. Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2002;17(1):56–63. [DOI] [PubMed] [Google Scholar]
- 14. Li D, Yang Z, Xie X, Zhao J, Kang P. Adductor canal block provides better performance after total knee arthroplasty compared with femoral nerve block: a systematic review and meta-analysis. Int Orthop. 2016;40(5):925–933. [DOI] [PubMed] [Google Scholar]
- 15. Ludwigson JL, Tillmans SD, Galgon RE, Chambers TA, Heiner JP, Schroeder KM. A comparison of single shot adductor canal block versus femoral nerve catheter for total knee arthroplasty. J Arthroplasty. 2015;30(suppl 9):68–71. [DOI] [PubMed] [Google Scholar]
- 16. Luo TD, Ashraf A, Dahm DL, Stuart MJ, McIntosh AL. Femoral nerve block is associated with persistent strength deficits at 6 months after anterior cruciate ligament reconstruction in pediatric and adolescent patients. Am J Sports Med. 2015;43(2):331–336. [DOI] [PubMed] [Google Scholar]
- 17. Mulroy MF, Larkin KL, Batra MS, Hodgson PS, Owens BD. Femoral nerve block with 0.25% or 0.5% bupivacaine improves postoperative analgesia following outpatient arthroscopic anterior cruciate ligament repair. Reg Anesth Pain Med. 2001;26(1):24–29. [DOI] [PubMed] [Google Scholar]
- 18. Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sharma S, Iorio R, Specht LM, Davies-Lepie S, Healy WL. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res. 2010;468(1):135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]